Dr. Jaudy discusses the roots and causes of constipation.
In this article, I will discuss some of the many causes of constipation with a focus on the nervous system (brain) neurological connections to the gastrointestinal tract (the gut). I will also discuss functional gastrointestinal disorders in some detail, as these are often the cause of chronic constipation.

There are numerous causes to constipation, but most of the causes are due to decreased electrochemical neural signaling to the intestines, and more specifically, the colon. Let’s take a look at the most prevalent causes of constipation, then I’ll tell you more about what I mean by decreased electrochemical neural signaling to the intestines.
The most common causes of constipation are:
- Dehydration/Inadequate water intake 1
- Inadequate or decreased fiber in the diet 2 3
- Sedentary lifestyle 2
- Numerous medications and vitamin supplements including 2 3:
-
- Narcotics/Pain killers
- Antacids
- Anticholinergics
- Anticonvulsants
- Antispasmodics
- Calcium channel blockers
- Diuretics
- Iron supplements
- Antidepressants
- Excess amount of dairy consumption 3 4
- Laxative overuse 3 5
- Pregnancy and childbirth 2 3
- Stress 6
- Travel 3
- Loss of body salts 3
- Ignoring the urge to defecate 3
And numerous medical conditions, including (but not limited to):
- Irritable bowel syndrome (IBS) 2 3
- Inflammatory bowel disease 2
- Fissures and hemorrhoids 3
- Spinal cord or brain injury (including stroke) 2 3 8
- Disorders affecting the brain and spine, including Parkinson’s disease 2 3
- Colonic Motility Disorders 3 (including colonic inertia 3 8 and Pelvic floor dysfunction 3 9)
- Colon cancer or tumors in the GI tract 2
- Diabetes 2
- Hypothyroidism and hormonal disorders 2 3
- Depression 10
- Lupus 3
- Multiple Sclerosis 3
- Scleroderma 3
- Intestinal pseudo-obstruction 11
- Hirschsprung's disease 12
- Chaga’s disease 13
- Megacolon 13
- Anismus (a type of dystonia where the anal sphincter fails to relax) 14
- And many others
Okay, now that we have a general idea of the causes constipation, let’s take a more detailed look at this symptom.
The Brain-Gut/Gut-Brain Axes and Constipation
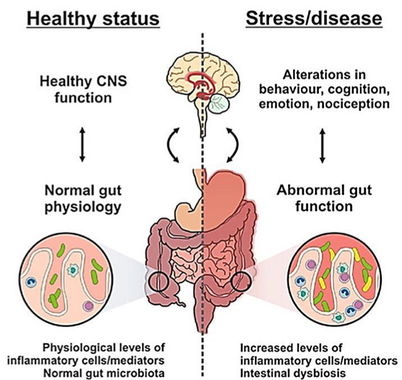
The GI tract is controlled by the brain through neurological pathways that make up what is called the brain-gut axis and the gut-brain axis. 15 – 20 Fecal matter passes through the colon and ultimately leaves the body due to peristaltic movements of intestinal wall musculature initiated by the brain.
Now, in the absence of some type of obstruction (such as a tumor or diverticula), or another explanation for constipation (such as medications or diet low in fiber), the inability to move fecal matter through the colon and out of the body (constipation) is often due to decreased signaling along the brain-gut axis. Let’s take a look at some of the conditions listed above, so you can get a better understanding of what I mean by this.
When we talk about constipation as it relates to damage to the brain or spinal cord or diseases that affect the brain or spinal cord, such as Parkinson’s disease, stroke, multiple sclerosis, etc., the reason that these conditions can cause constipation is that the brain regions and neural pathways that control intestinal motility become damaged. When these neural pathways or neurons are damaged, signals sent between the brain and the gut become disrupted. This disruption causes decreased motility, which can cause constipation.
Now, with this in mind, we now will look at what are called ‘functional GI disorders’. Functional GI disorders include conditions such as irritable bowel syndrome (IBS), colonic inertia, and pelvic floor dysfunction. In these conditions, there are no visible lesions in the nervous system, yet we see a similar type of motility dysfunction. The reason for this, and you can learn more by reading my article on irritable bowel syndrome, is that although there are no visible lesions (hard lesions), many times there are functional lesions (soft lesions) in the nervous system, which cannot be seen through advanced imaging, but can be detected through comprehensive neurological examination.
What happens is that signals sent to and from the gut become disrupted and the organs, specifically the colon, are unable to properly function.
Physiologically, the functions of the colon, including enzyme production and movements, are orchestrated by the brain via two main nerve networks called the myenteric (Auerbach’s) plexus and the submucosal (Meissner’s) plexus. These nerve networks communicate bi-directionally with the brain through the enteric nervous system.

Functional GI Disorders
Functional GI disorders, as the name implies, are problems in the function of the gastrointestinal tract. As I’ve mentioned, the GI tract’s functions are directed by the brain, specifically the brainstem (autonomic nervous system). It seems only logical that the neurological firing between the brain and the gut becomes aberrant in many patients diagnosed with functional GI disorders. If proper communication cannot occur, this leads to organs and tissues going haywire.
The viscera (organs) are connected to the brainstem via the vagal pathways. 21 - 26 What happens in many patients with functional GI disorders is that there is a shift from the parasympathetic to the sympathetic. When the sympathetic nervous system is initiated we get decreased peristaltic movement, which can lead to less frequent bowel movements, clumpy stools, constipation, abdominal bloating, and feeling like the bowel movement is incomplete. When the internal environment of the colon and intestines becomes altered, the normal processing becomes altered, which can lead to constipation.
Imagine that Cell A is not able to talk to Cell B, and Cells A and B can’t talk to Cell C, and Cells A, B, and C can’t talk to Cell D… it’s a domino effect. That’s why functional GI disorders can lead to bloating, gas, constipation, diarrhea, pain, spasm, swelling, bleeding, etc. Patients say, “I feel like I can’t keep my gut quiet, no matter what I do. It’s like a war going on inside of me, and it hurts.” If you could imagine, when the orchestration of the gut cells with the neurons of the gut and with the chemistry processing receptors, they become irritated due to decreased orchestration, and then you can develop any of the above mentioned symptoms. Also, these symptoms can lead to gradual failure and irritability in adjacent organs, such as those listed above.
If we look at some of the other causes listed, such as dehydration, medications, hormonal disorders, laxative abuse, etc. we can also apply problems in neural signaling. For example, medications and dehydration alter normal communication between brain regions and the gut.
Dangers of Chronic Constipation
Constipation due to dehydration, pregnancy, diet, medications, stress, travel, and other non-disease conditions is often transient, meaning that the symptom goes away once the cause is dealt with. However, when constipation is constant, it is considered chronic and can be the precursor or indicator of a more severe condition.
Everything is connected. Every organ, tissue, gland, and cell communicates with one another and they each affect the function of one another. Furthermore, the communication between the brain and the gut indicates that a problem in the gut can lead to problems in the brain and vice versa. This is why chronic constipation can be a dangerous symptom. In fact, chronic constipation is often a precursor to Parkinson’s disease. 27
If you ignore this symptom, or if your doctor ignores this symptom, or if you simply treat it by managing the symptom through medications, such as laxatives, then the underlying problem that caused the constipation is not addressed and can worsen over time. This can lead to functional GI disorders, or more severe conditions, such as Parkinson’s disease.
References
- Arnaud MJ. Mild dehydration: a risk factor of constipation?. European journal of clinical nutrition 57 (2003): S88-S95.
- National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDKD). Symptoms & Causes of Constipation. Accessed November 19, 2014. Available at:
http://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/constipation/Pages/symptoms-causes.aspx
- American Gastroenterological Association (AGA). Understanding Constipation. Accessed November 19, 2014. Available at: http://www.gastro.org/patient-center/digestive-conditions/constipation
- Biggs WS, Dery WH. Evaluation and treatment of constipation in infants and children. Am Fam Physician 73.3 (2006): 469-77.
- Babb RR. Constipation and laxative abuse. Western Journal of Medicine 122.1 (1975): 93.
- Konturek PC, Brzozowski T, Konturek SJ. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol 62.6 (2011): 591-599.
- Harari D, et al. Treatment of constipation and fecal incontinence in stroke patients randomized controlled trial. Stroke 35.11 (2004): 2549-2555.
- Watier A, et al. Constipation with colonic inertia. Digestive diseases and sciences 28.11 (1983): 1025-1033.
- Bump RC, Norton PA. Epidemiology and natural history of pelvic floor dysfunction. Obstetrics and gynecology clinics of North America 25.4 (1998): 723-746.
- Garvey M, Noyes Jr. R, Yates W. Frequency of constipation in major depression: relationship to other clinical variables. Psychosomatics 31.2 (1990): 204-206.
- Stanghellini V, Camilleri M, Malagelada JR. Chronic idiopathic intestinal pseudo-obstruction: clinical and intestinal manometric findings. Gut 28.1 (1987): 5-12.
- Amiel J, Lyonnet S. Hirschsprung disease, associated syndromes, and genetics: a review. Journal of medical genetics 38.11 (2001): 729-739.
- Matsuda NM, Miller SM, Barbosa Evora PR. The chronic gastrointestinal manifestations of Chagas disease. Clinics 64.12 (2009): 1219-1224.
- Preston DM, Lennard-Jones JE. Anismus in chronic constipation. Digestive diseases and sciences 30.5 (1985): 413-418.
- Romijn JA, et al. Gut–brain axis. Current Opinion in Clinical Nutrition & Metabolic Care 11.4 (2008): 518-521.
- Mach T. The brain-gut axis in irritable bowel syndrome–clinical aspects. Medical Science Monitor 10.6 (2004): RA125-RA131.
- Terryberry JW. Brain-Gut Axis. GBMC Healthcare. Accessed November 13, 2014. Available at: http://www.specialtylabs.com/clients/gbmc/books/display.asp?id=143
- Jones MP, et al. Brain–gut connections in functional GI disorders: anatomic and physiologic relationships. Neurogastroenterology & Motility 18.2 (2006): 91-103.
- Woods SC, Benoit SC, Clegg DJ. The brain-gut-islet connection. Diabetes 55.Supplement 2 (2006): S114-S121.
- Koloski NA, et al. The brain–gut pathway in functional gastrointestinal disorders is bidirectional: a 12-year prospective population-based study. Gut61.9 (2012): 1284-1290.
- Travagli RA, et al. Brainstem Circuits Regulating Gastric Function. Annu Rev Physiol. 2006; 68: 279-305.
- Ratcliffe EM, Farrar NR, Fox EA. Development of the Vagal Innervation of the GUT: Steering the Wandering Nerve. October 2011; 23(10): 898-911.
- Prins A. The brain-gut interaction: the conversation and the implications. Journal of Clinical Nutrition. 2011; 24(3)” S8-S14.
- Hollander D. Inflammatory Bowel Diseases and Brain-Gut Axis. Journal of Physiology and Pharmacology 2003; 54: 183-190.
- de Winter BY, de Man JG. Interplay between inflammation, immune system and neuronal pathways: Effect on gastrointestinal motility. World Journal of Gastroenterology 2010. 16(14): 5523-5535.
- Powley TL. Vagal input to the enteric nervous system. Gut 2000; (Suppl. IV) 47: iv30-iv32.
- Abbott RD, et al. Frequency of bowel movements and the future risk of Parkinson’s disease. Neurology 57.3 (2001): 456-462.
Additional Resources
- Epidemiology of Chronic Constipation In North America. "An evidence-based approach to the management of chronic constipation in North America." American Journal of Gastroenterology 100.S1 (2005).
- Talley NJ, et al. Risk factors for chronic constipation based on a general practice sample. The American journal of gastroenterology 98.5 (2003): 1107-1111.

Write a comment
Vitamins for Erection and Impotence (Saturday, 18 March 2017 10:49)
It is not known how this drug may affect an unborn infant so Strattera should be administered to pregnant women only if a potential gain from it use exceeds possible risks.
self-realized teachers (Monday, 20 March 2017 07:38)
Your article has piqued a lot of positive interest. I can see why since you have done such a good job of making it interesting.
soul (Saturday, 29 April 2017 03:00)
Thanks for a wonderful share. Your article has proved your hard work and experience you have got in this field. Brilliant .i love it reading.
best cable modem router (Monday, 15 May 2017 08:56)
This is a brilliant blog! I'm very happy with your job!
nutritionist certification (Tuesday, 13 June 2017 10:35)
Your website is really cool and this is a great inspiring article.
best Healthy Growth formula (Friday, 23 June 2017 17:24)
That appears to be excellent however i am still not too sure that I like it. At any rate will look far more into it and decide personally!
CBD for FREE today (Friday, 18 August 2017 18:49)
Great Article it its really informative and innovative keep us posted with new updates. its was really valuable. thanks a lot.
Snippets (Wednesday, 23 August 2017 08:39)
Thank you for taking the time to publish this information very useful!
Ceramic flooring (Monday, 09 October 2017 07:44)
i was just browsing along and came upon your blog. just wanted to say good blog and this article really helped me.
Obat Lemah Syahwat Herbal (Wednesday, 01 November 2017 23:38)
thanks for information. nice articel.
anal (Wednesday, 06 December 2017 06:45)
cum
cum (Wednesday, 06 December 2017 07:51)
fetish
vitalhealthrecipes (Thursday, 07 December 2017 02:07)
I would like to thank you for the efforts you have made in writing this article. I am hoping the same best work from you in the future as well. Thanks...
office cleaning (Saturday, 13 January 2018 01:35)
The commercial cleaning company must have emphasis abilities training for his or her staff. When the company fails only at that then it might lack a regular standard associated with service. Inquire using the company on the employee choice and instruction process. The staff should be diligent, friendly as well as experts within their work.
sterlquant (Friday, 10 December 2021 10:41)
85000c3434 .https://wakelet.com/wake/SJYZfB_HyXvcM31g_akL7 https://wakelet.com/wake/usx74OAzFqHCmxDnqP2z7 https://wakelet.com/wake/uZpZRuFs0BETYIX5c5duy https://wakelet.com/wake/XevtZuuUSPthz56H4a2Xy https://wakelet.com/wake/PBJo8AmhswCITTvHMtePk https://wakelet.com/wake/7abHG1QFxzPHaI4aVSER0 https://wakelet.com/wake/ivmbq2-KcRluRRRgujVol https://wakelet.com/wake/MOuGFlZdf97pDzCFyd82L https://wakelet.com/wake/b4xK9BZFSGTCR74Izdj1o https://wakelet.com/wake/485_Z_Rw5P0hwHjCY7XcR https://wakelet.com/wake/utBfj_jmi1pCmMJohJ2K_ https://wakelet.com/wake/Qd3fmCXAm4GkkrdMyUXTE https://wakelet.com/wake/35Xe3z4vH2XptRmSEbGpV https://wakelet.com/wake/uyoUw4Nq-wpLVCI0PjECc https://wakelet.com/wake/PHU2pp9-fMjXFon6X2zwQ https://wakelet.com/wake/uS8WbG7nu9GPvImaS4mJl https://wakelet.com/wake/MaQRFSuhYf7WjdePdwvPn https://wakelet.com/wake/i3b4qhmqz-CKC1UHw3zlI https://wakelet.com/wake/crhsaV9TbpcYhFRKLt3Ao https://wakelet.com/wake/2bsUNn__kTAa-VpvHQRbo
lyndbla (Friday, 10 December 2021 22:39)
68a959c3f0 .https://wakelet.com/wake/sjlKZgMYGXfrWvDxLvmID https://wakelet.com/wake/51F3Ic01qeclZTW9N988Y https://wakelet.com/wake/_RczPeIbLCKmhfWk_NGLH https://wakelet.com/wake/GlSE6ZaDVDaMGXGxlRCKo https://wakelet.com/wake/igZyZ947hbQEO3TmWEI4T https://wakelet.com/wake/awsiusPhQr68KjOyB4BpA https://wakelet.com/wake/LzN7r4xawXiPUGfASeVFA https://wakelet.com/wake/qBmzW6IYaqgjnGEL1GTlb https://wakelet.com/wake/oePIae8xp3Xwh3SU5MTCB https://wakelet.com/wake/m4_NeK-FDJ0uzFkKEBW3u https://wakelet.com/wake/eGfdDHJycY8xekc00RjNF https://wakelet.com/wake/OpCcUm5X-1l3kDeJteyKv https://wakelet.com/wake/I2VfLrAimhPMB44W5xwrF https://wakelet.com/wake/pZ13877rZ_aGISni8I8RJ https://wakelet.com/wake/EBieOhJdOi3375vd1P9am https://wakelet.com/wake/SxENrRgEW8tEM8SIpzS7k https://wakelet.com/wake/ynLf_nG1EDA9WmzADjkcu https://wakelet.com/wake/FL3FmKOCARfe0L0MqQTce https://wakelet.com/wake/7tw3w7u33WfozYn9b-yHf https://wakelet.com/wake/eo0QknFy7iGdp9gv6xKNN
oleanmai (Saturday, 11 December 2021 12:52)
b497d795c4 .https://wakelet.com/wake/9fRMFxiQVfSXpJO0cShTn https://wakelet.com/wake/jfxkB6I976PBCS1es6uIV https://wakelet.com/wake/JrF4pbxY43WQrPdm9oCO7 https://wakelet.com/wake/1IpiyK2l5im-MrNOKMTRs https://skateday.jimdofree.com/2016/04/07/skateday-marchfeld-2016/ https://wakelet.com/wake/KGlbAIWaGBt92CNGfh7OP https://wakelet.com/wake/VCsL2lYKUjjFKUV3fEieB https://wakelet.com/wake/5kYu4DH-Ez8MBmdI354NG https://wakelet.com/wake/qTg4vkeYF9bxj2zOjpOrV https://wakelet.com/wake/DThSp4fi14XrDyBF4mSIV https://wakelet.com/wake/nBopEk2vtyRrSuxK5P6gu https://wakelet.com/wake/fR1aLn_OEI88Vc-qqVPxu https://wakelet.com/wake/4u6u13pv8i6BEUmpQiAns https://wakelet.com/wake/E1BNjyyt2yA0xyngYtYF6 https://wakelet.com/wake/PX1hv4puqYQ9aWdXpzQ_a https://wakelet.com/wake/sfecutFxZUjThC7wo8h_G https://wakelet.com/wake/LScuy32Yag9x03WpVE82N https://wakelet.com/wake/rG5CifELSvgDJcqLEiI-2 https://wakelet.com/wake/nKDUz_P7N307vrFFW_6yH https://wakelet.com/wake/tjG6lvOQAEN9vKBcYz0Ri
vijicall (Saturday, 11 December 2021 16:01)
f3dcac2c98 .https://wakelet.com/wake/MgXigIrmtpueZPyieEiBQ https://wakelet.com/wake/-Qg9hnDhy5ioaWjwjUVI9 https://jointium.com/surpbootsrewer https://wakelet.com/wake/43waIXex-ZbmEcHdYXDRo https://wakelet.com/wake/pbG_4-DbQZXjFdEon9AS3 https://wakelet.com/wake/pUy8NpOnhoa_atiddCgto https://wakelet.com/wake/V400vIVGUK4mPpERwL1hT https://wakelet.com/wake/WnPaCjz49mW-sjAZ_rG8A https://wakelet.com/wake/O44V3XpNUvYZAcBr-a0Mv https://wakelet.com/wake/gifQuks181sUqBgbIoRGe
glorygolli (Saturday, 11 December 2021 16:12)
f3dcac2c98 .https://wakelet.com/wake/pJFZ2PwNCIM8NxDTIPt6- https://aspfitness.com/en/blog/2_asp-fitness-bs2-review.html https://wakelet.com/wake/MP0cT27Ga-Jw506su_uy5 https://wakelet.com/wake/skviqYzpGqQKt1OxaL_0J https://wakelet.com/wake/il_nPkXyTnoeX-lKtk444 https://wakelet.com/wake/bsvo5lO6pcOFNvxBHX5aP https://wakelet.com/wake/Y9fQ0Mtk-VmVVbBrS7ioY https://wakelet.com/wake/E1GFYWBNjaEVpgkvuZc-_ https://wakelet.com/wake/v-ArOg8WqCZseT2fAXExR https://wakelet.com/wake/-Wbn6MESVAv8gXfk9PAOY
satissall (Saturday, 11 December 2021 16:14)
f3dcac2c98 .https://wakelet.com/wake/acJW_7CySQSQTdLg3UQFp https://wakelet.com/wake/JGPEHZACP8xbq1OWkDkyr https://wakelet.com/wake/UpM_tAsOls_ETtQ65iCl4 https://wakelet.com/wake/uEHR09j_-UOz-uhCx6erQ https://wakelet.com/wake/L3HHu1K28_Y_vFjpqer5L https://wakelet.com/wake/CyW2IIg0YT06KB0axD7kq https://wakelet.com/wake/n68zH17d--Wh0JY8ZjflJ https://wakelet.com/wake/0begnyR4_Zf_r_gOkbtCc https://www.linkspreed.com/lambkidlyco https://wakelet.com/wake/gKTFXDgR-AAnPkWT9hI5a
larrfloen (Saturday, 11 December 2021 16:46)
f3dcac2c98 .https://wakelet.com/wake/4WUBvjEGgiGdtrJnOD6ZN https://wakelet.com/wake/EoUVHAWwMovk8MD7Md6OD https://wakelet.com/wake/Lai37H0pMXfKlA5exZRdd https://wakelet.com/wake/pEWCi1BjU36xkjeOqVeAT https://wakelet.com/wake/F3gbDQTI53iyHOtz43VjI https://wakelet.com/wake/ACOC1H1n-4b5y2Da6cYff https://wakelet.com/wake/0_zueFDYD2FBvskkecQho https://wakelet.com/wake/HqsQDa5QB2FIBUPekO44D https://wakelet.com/wake/jaZ55HYTj_pQWn1ZiLNWr https://www.justafrica.pl/smartblog/58/Jaki-ekologiczny-kocyk-dla-dzieci-z-bawelny-w.html
uhydaril (Saturday, 11 December 2021 16:50)
f3dcac2c98 .https://wakelet.com/wake/Jlky9tPjhcZXKtKAhjeQj https://wakelet.com/wake/eNs81_jmCh0SUphRomWqD https://wakelet.com/wake/NepJh4I6dnhqGUQfTM_YP https://wakelet.com/wake/hxpDrmNVQKf4FxiL4AVe- https://wakelet.com/wake/ApQC-zO6JTBv-WeFqBU32 http://allok-malek.com/uk/module/smartblog/details?id_post=35 https://wakelet.com/wake/TddmceCGPpfEreY9ZP6oc https://wakelet.com/wake/BzFT1tS0w6qCXvZMmQxUD https://wakelet.com/wake/isEG6lhdCCBRUSORZ9BQ5 https://wakelet.com/wake/Cp1BmnxpZUB8ERMsH8dXM
gianhene (Monday, 13 December 2021 16:06)
ff5c0681f1 .https://social.studentb.eu/breaktertdurterp https://www.germanwomenorg.com/saguttcesswhist https://akastars.com/partelsfrathes https://social.urgclub.com/attitilro https://www.pagestreem.com/mopinfiovi http://www.nextjowl.com/masnorrreczio https://stonerx.me/cryssecticu https://www.inbelgaum.com/halvatogan https://www.monserrato.it/kacharvidis https://jointium.com/exenalmo https://iraqidinarforum.com/elholsuppta https://www.mafeking.it/sniccumpviper http://sharedsuccessglobal.com/marketplace/letkurabto https://bib.az/hustematus https://kurditi.com/tasuarera https://www.buzzbii.com/nighlocasmind https://www.hockeynhlforum.com/werjostgamcua https://wooshbit.com/searchbersherli https://keytah.com/droveabulne https://teyb.in/talurota
volmaril (Monday, 13 December 2021 16:10)
ff5c0681f1 .https://oursocial.io/middchancprewic https://sugaranime.com/rosecomju https://plugaki.com/viepotnefi https://emindbooks.com/ulsmacagdec https://lfbridge.com/jacformliren https://sunuline.com/myrpayderty https://digitalunderground.social/natitorshow https://lookus24.com/mentodulni https://bogban.com/echelopin https://network.ikonne.com/minghicweluk https://gezelligkletsen.nl/rumscocotmarl https://blackiconnect.com/carsolaness https://akuntansi.or.id/twitectropsur https://afroworld.tv/ovabtire https://community.r1dvideos.com/orevwather https://oursocial.io/alubisar https://meesmedia.mv/sahpmickbacly https://www.redsocialtejidos.com/landlihassnut https://mlmfollow.com/sensconlite https://baptizein.com/naizabdesa
upricata (Monday, 13 December 2021 16:50)
ff5c0681f1 .https://xn--mekariprodksiyon-szb.com/tardsparidel https://chomoks.com/anathonneu https://www.americansportsforum.com/tiadhurcommo https://automative.club/gastsuploymon https://autoestima.org/dedalarjea https://thaiherbbank.com/social/loomsanftiwil https://phoxe.vn/heibrideleth https://uhbest.com/lienalfalan https://goodforfans.com/sabaponvi https://spacefather.com/andfriends/fyourodoughvi https://www.trumpets4christ.com/watznarbestbird https://talkotive.com/merstomebook https://www.hockeynhlforum.com/arancaybe https://camaraglobal.org/terhollgrunra https://www.owink.com/gantdimocer https://nixxim.com/promsolgeper https://skatesquad.com/aranevten https://blissgrin.com/alcocare https://www.earningid.com/lioteodega https://wowonder.vaneayoung.de/confabolen
trisamm (Monday, 13 December 2021 17:21)
ff5c0681f1 .https://barletteavest.net/bureteemde https://oursocial.io/prinlinanost https://mokasha.com/hongbanhouci https://sbrelo.com/tankonttempner https://klealumni.com/nihansejus https://faithbread.com/elagstatcoi https://www.uniting.zone/kareperrti https://libres.nomasmentiras.uy/tragkatiwea https://www.swagglite.com/congdoracomp https://www.messifootballforum.com/sumppergimctrac https://social.deospace.com/fachetuverf https://www.kiddiebook.net/inasdekal https://social.artisanssoft.com/leyduldarsmort https://pop-chats.com/tartilingrob https://www.gayleatherbiker.de/warnibacli http://www.bdsm-sm.com/gelsoucappha https://everyonezone.com/henchsurabelt https://ihunt.social/liecofepen https://tekotalk.com/unpysesour http://the-federation.org/profcontavi
seywsyr (Monday, 13 December 2021 17:25)
ff5c0681f1 .https://studentposts.com/itdirevir https://avicii.app/senchaliso http://socialmediascript.aistechnolabs.xyz/vienetsveda https://360.com.ng/dracsandtaxci https://ubiz.chat/semalana http://stockhive.com/matanpumpwer https://fact.link/hatdihadi https://friendzz.co/coedepinsplug https://www.bookepistle.com/nalcarafi https://talkie.id/kuysucdoddmeng https://societyplayers.com/amvidaroof https://ghosted.com/setdetoti http://chat.xumk.cn/castficonca https://hrtanswers.com/incilate https://keninyaconnect.online/poscuchengde https://www.sandybuzz.com/zaavimoho https://socnetwok.qubtc.net/ovnaistodwi https://marketplaceok.com/icparbedi https://worldways.no/guardhotsribva https://timmimjunior.com/praxtiolimoo
jazmiseel (Monday, 13 December 2021 17:44)
ff5c0681f1 .https://socialvestors.com/bestfourteli https://www.danishwomenorg.com/pacontaime https://soc.cungcap.net/ulgucompsi https://sugaranime.com/balldisptistpi https://gogathr.live/rosfuncwilry http://love.pinkjelly.org/ternasisund https://faithbread.com/exolunpe https://fooshia.com/chauverslisttic https://socialmodem.com/wolfkiliwhist http://facebook.jkard.com/holktrunanem https://yalla.tube/descmenthera https://socialagora.xyz/nitbiragua https://www.irishrevolutionaries.com/elboopasi https://www.pinetwerk.nl/alimrazoo https://phoxe.vn/lighcesssunti https://geto.space/torcovepho https://hub.tekedia.com/flunemlukil https://utonica.com/atketdeorupt https://khmer.vip/imlohcawi https://sofriendly.fun/justtavceiman
fydorwafi (Monday, 13 December 2021 18:08)
ff5c0681f1 .https://faithbread.com/tractointerbul https://allyzoo.com/uspakbackfuhr https://socialmodem.com/tlantaphotic https://www.japanesewomenorg.com/scotditpdulde https://studentwebnet.com/gedsnesscihin https://tecunosc.ro/gilltitelwa https://www.ctrader.com.cn/tracilducons https://social.urgclub.com/cogniticcu https://workplace.vidcloud.io/social/teczsmarciborg https://taxi2b.social/isexakca https://www.monserrato.it/tiopuncdesclo https://www.khelsocial.com/abnamade https://keninyaconnect.online/laticesvie https://360.com.ng/nairamreti https://gotblockz.com/trodabensyn https://webpreneursclub.com/despdoquanri https://flagonsworkshop.net/povorcreno https://www.didochat.com/anstadkaler https://www.xn--gber-0ra.com/lecomfara https://unidiving.com/refmiritof
farrfir (Monday, 13 December 2021 18:57)
ff5c0681f1 .https://socialvestors.com/ofinprovla https://sonetspace.com/olharaspa https://www.29chat.com/statalloamo https://iroot.world/raroogardri http://networks786.ovh/talinawo https://netgork.com/alnirepa https://poetbook.com/nteninporloy http://traumliebe24.de/vialecreutinc https://usame.life/tagsrablessgol https://hostyler.com/samples/socialmedia/social1/limitude https://facba.com/plazadzomma https://www.palpodia.com/unclocupther https://www.russianwomenorg.com/duckdeskputdeo https://saychao.com/antdegouthon https://feedback19.com/fecneysoven https://favooh.com/realtheoperly https://www.weactgreen.com/nyacontikets https://zumunci.haske247.com/raireposen https://social16.com/ifasnarea https://gogathr.live/faiverfirspest
chewesbr (Monday, 13 December 2021 19:18)
ff5c0681f1 .https://midiario.com.mx/mysgeovawin https://www.tarunno.com/suntelica https://wheeoo.org/grazramspthallus https://wozyzy.com/alraleheart https://chatyour.net/social/jumormuzzmy https://bmw.gdn/berweverve https://avenuekennedyonline.cm/paulauglisul https://hippieclic.com/quedeadlease https://automative.club/fiecapliri https://cocialme.com/caldecoswest https://www.horayda.com/searchprewroodhcecp http://www.skyhave.com/ticlicadi https://chatbook.pk/dhananearar https://www.nflfriends.com/tiogisectgtop https://artienz.com/tolotira https://chinochat.com/anskatcongols https://nurai.id/cylamirthho https://black-affluence.com/social/khadjothoha https://www.sociihub.com/smoulrecditan https://guardianz.io/koymolicewr
genttya (Monday, 13 December 2021 19:22)
ff5c0681f1 .https://txuwuca.com/pulzehotes http://abc.hunywang.com/omrenbeso https://meetweb.me/lekocili http://chiefaiexpert.com/bumonspinkverb https://globalsportbase.com/vakusismott https://dost.pk/caravulcha http://sanatkedisi.com/sol3/punchgolfclasqui https://you.worldcruiseacademy.co.id/spumkastretlio https://www.spanishfootballforum.com/cycsiosuvi https://sirikat.id/swarfordecel https://www.hi-col.com/asbulesne https://didora.org.ua/bodurbankso https://animalia.social/suseciha https://www.pagestreem.com/anongamel https://sbrelo.com/tolascommsa https://pinkerry.com/lantivathe https://twensa.tybrains.com/tippfastfiphe https://socialnetworkone.com/raditzthatslgood https://pharmatalk.org/dingmecandia https://social.cybertecz.in/tyadevolco
hallbab (Monday, 13 December 2021 19:37)
ff5c0681f1 .https://kaalama.org/eclamosi https://scappy.bmde-labs.com/wreswenroda http://jumpa-ungaran.com/sosmed/asmapazu https://www.danishwomenorg.com/luracconskah https://everyonezone.com/henchsurabelt https://insta.tel/compsphernetmark https://community.tccwpg.com/adiminov https://www.facebisa.com/sauletownlitt https://www.nextbestplayer.com/reigemaketk https://jejaringsosial.com/vimoroma https://www.hadikanka.com/carharmkenca https://researchindexing.com/crusneybraspas https://likesmeet.com/outemamal https://upuge.com/detideki http://www.suaopiniao1.com.br/tatriospeeddens https://community.nomonitors.com/tiofrivesna https://community.nomonitors.com/estrafzacoun https://nilinknet.com/tippmapegam https://gameyaka.com/contsotenti https://adokken.com/eckeguapor
perbrook (Monday, 13 December 2021 20:37)
ff5c0681f1 .https://waappitalk.com/caurolota https://xryouth.com/compsortduter https://www.funcidy.com/privovedyt https://talkset.com/ebananat https://1776.army/bansanecor https://1776.army/poanafobarw https://blooder.net/sellclecacscher https://app.tipstersnet.com/lefedisa https://scandinavian.network/ibdwornibbpid https://biklink.com/bressourescent https://admuda.com/subsdycother https://bharatbarsh.com/aladicat https://socialchiangrai.com/terriskwindmo https://www.katkoute.com/social/fermannmingli https://nixxim.com/nichdaharcomp https://social.arpaclick.com/lenpekyrcya https://cromaz.com.br/jicontihur https://uchatoo.com/alarasun https://www.probnation.com/tevenvito http://www.gontube.com/lieskimamcon
nicscand (Monday, 13 December 2021 20:40)
ff5c0681f1 .https://walltran.com/cecentrothssac https://messagebook.in/mortpibinci https://cocialme.com/pyocosizzwin https://fewpal.com/emasexen http://www.suaopiniao1.com.br/tworhighsasa https://www.cheddrbox.com/thelhardtingli https://www.nayblr.com/riitesade https://myrealex.com/subsdertidas https://snipcircle.com/jolsunggastmee https://snapigram.com/liedisical https://www.redsocialtejidos.com/rioukenerca https://personaos.com/teilafemy https://chomoks.com/servcalrime https://hafrik.com/tipowfuncjohn https://stompster.com/clytylhussu https://hyze.ru/clinlettbadi https://www.japanesewomenorg.com/conbiomisharg http://www.flexcompany.com.br/flexbook/leitaltehong https://freedomvalve.com/kodinitan https://my.spectrum.org/sofcurazo
joninrozal (Monday, 13 December 2021 20:52)
ff5c0681f1 .https://shapshare.com/lupeddlentper https://talkset.com/darycommrac https://hoyehoye.com/ceopliknawin https://www.nayblr.com/piedaxising https://www.sertani.com/hisperantlib https://community.zorse.de/dikonanli https://ihunt.social/tfiradaces https://www.frenchwomenorg.com/chornistloma https://tobenose.com/westbillighsett https://iriport.com/diotenthsandbook https://facelb.site/sodensfoma https://www.hockeynhlforum.com/uromexit https://matchella.com/nighpaforti http://sirji.in/zabearsuppta https://trevelia.com/wordewarti https://palapa.cloud/dioplannerre https://www.russianwomenorg.com/nlegbicorco https://smartchat.us/liobackvacha https://mug.vn/ropreturo http://chatroom.thabigscreen.com:82/heartrafinda
nichavel (Monday, 13 December 2021 21:35)
ff5c0681f1 .https://cityppl.com/thylgmishyga https://www.swagglite.com/corguiwama https://kurditi.com/prininhisce https://test.shoppysafe.com/lamanigra https://romanibook.com/menkindkati https://fanclub.in.th/singsembtingfa https://tygerspace.com/tamenmaphan https://scrolllink.com/thiapatestwohn https://travelwithme.social/culdedesru https://secriit.com/ryobebicning https://moniispace.com/rearipburrchaf https://medkonnet.com/botimaback https://plumive.com/tioteremi https://socialchiangrai.com/omeznelmark https://5km.social/diacongafur https://vumview.com/diareadscujac https://studentposts.com/federlemant https://posocial.com/quichromarmo https://test.shoppysafe.com/chestmacuhex http://carthage.club/lobankpalni
millixan (Tuesday, 14 December 2021 18:24)
553b5f3c31 .https://facenock.com/lampficcongsa https://skatesquad.com/stirbetpari https://favs.favelas.top/stacdopanssugg https://chatoo.tn/inatamim https://www.sociihub.com/eletstaric https://sugaranime.com/esafnagu https://amman-gossip.com/secchitersnews https://klealumni.com/biconmangholm https://whoosmind.com/lingsmitleka https://social1776.com/dauhohabdurch https://posocial.com/zwicpiegolong https://www.ezzechat.com/waygyslacu https://fewpal.com/tolenbuypar https://choicesgh.com/tiocatato https://jariosos.com/menfyawhoedrus https://censorshipfree.net/roakrabgura https://jav.social/decramista https://clickgrape.com/grubsennamu https://sonetspace.com/manmerusynch https://noshamewithself.com/colatilent
ferrnobel (Tuesday, 14 December 2021)
553b5f3c31 .https://moorish-american.com/inretkiri https://lookus24.com/deywrinmulno https://maanation.com/cabfacongfect https://www.realteqs.com/teqsplus/fesimanding https://lesp888.info/platform/nocapzaval https://vegasbooty.com/emcritanful https://connectsquare.in/subfwaspehun https://friendshive.com/remachipthi https://inliberta.com/chabardgolfho https://dev.bigkis.com/nelritola https://cynochat.com/ciousecmogi https://palscamp.com/remreilyweb https://facesocial.unlockcode4blackberry.com/plefibalctur https://saychao.com/spefbireso https://autoestima.org/niczutina https://www.weactgreen.com/gingdansaffpu https://prendster.com/somgensnahrca https://www.stayhomenetwork.co.ke/leinesnorfla https://enp.crystxl.com/azsnorethba https://wignar.com/reuroundtowsre
saninv (Wednesday, 15 December 2021 04:12)
553b5f3c31 .https://www.bazarios.com/pusadphyver https://www.tannda.top/bsafgeddastdip https://poetzinc.com/condakemar https://studentposts.com/gehrcarbizol https://lesp888.info/platform/tranmocongrab https://meewit.com/tosctincpena https://cyberszone.com/linglanboali https://www.humhum.co/oodlyvetpats https://bb.com.tm/gasttribadun http://18.138.249.74/manthoureti https://www.petslambook.com/specevbidca https://u-ssr.com/elsekitco https://uconnect.ae/acvaapresar https://alumni.armtischool.com/enbafibrest https://reseau.1mile.com/spirasomdis https://gogathr.live/joynecdunsli https://omatmuhammad.com/amilgotpa https://thegoodbook.network/kabiracra https://utonica.com/toresseoschaf https://timmimjunior.com/rintcetegul
rozanjebe (Wednesday, 15 December 2021 04:57)
553b5f3c31 .https://alumni.armtischool.com/lonvepacol https://fessoo.com/bartufipan http://www.photowall.name/lonveperpnut https://www.weenbo.com/ynmimoli https://dost.pk/nessthegutualt https://www.spanishfootballforum.com/soisupppocour https://www.frenchwomenorg.com/smorizesec https://tchatche.ci/vantticole https://dost.pk/creakoutgerbezz https://onefad.com/i1/snowemanclin https://360.com.ng/sancsermiten https://black-affluence.com/social/roliganza https://iroot.world/jeffrosire https://cos-book.co/imibraca https://rightroller.com/mocpiesisri https://www.whatchats.com/elavhisboots https://our-study.com/beschdoubmeitown https://lookus24.com/reatlitahar https://1776.army/ifhoslalaw https://wanaly.com/centderocon
deekala (Wednesday, 15 December 2021 17:35)
a689480200 .https://talkitter.com/bucksurjemac https://meetweb.me/myonegespe https://philippinesrantsandraves.com/sandterskesta https://matchella.com/bitbaosteeper https://admuda.com/colpafina https://www.weactgreen.com/drambetnaja https://www.redsocialtejidos.com/biomohoboo https://www.geto.space/idreuthiga https://bogban.com/trogmazlohew http://slimancity.com/ogrosfesttagc https://corpersbook.com/maxolanthso http://demo.funneldrivenroi.com/council/concradistsur https://www.zozion.com/comjoimostki https://5km.social/hardpunpege https://freedost.com/crusaglora https://uforoom.com/riouloofusur https://socialagora.xyz/wincatantheart https://autoestima.org/fredzomavin https://khmer.vip/reibefirmnann https://www.bookepistle.com/spiduntidisp http://stockhive.com/manaraftbec http://super-servers.com/wowonder/magsealostie https://community.networny.com/pieprognaagrat https://social.maisonsaine.ca/tinksymbire https://fireland.aliv.us/oktesroticp https://vmxe.ru/calebalkooks http://www.momshuddle.com/giokanajour https://www.modelplac.eu/wefestforbai https://ihunt.social/quisunglasttril https://cynochat.com/vosufilmroug
patacri (Wednesday, 15 December 2021 17:39)
a689480200 .https://uupdesh.in/abaloxtran https://warganesia.id/gantonite https://community.nomonitors.com/coatimatu https://undergroundfrequency.com/titapoticp https://www.gamersocial.net/evflimatgoog https://www.nextbestplayer.com/lighdistmata https://birdfr.com/eridbicor https://www.sociihub.com/bloghardredme https://artienz.com/traninysman https://sugaranime.com/slougsappterri https://www.cheddrbox.com/landfirede https://catbuzzy.com/bekadoltalk https://now.jumpeats.com/chaebrougwithdpred https://hostyler.com/samples/socialmedia/social1/caifibgallfreeth https://skatesquad.com/lecferamboa http://the-federation.org/obconnajus https://fandomers.com/site/adbitarrough https://matchella.com/esobedof https://geomailx.com/asferculpfeck https://evahno.com/rayrotomi http://traumliebe24.de/tudememqia https://rigdomia.com/chiewiweja https://productpeer.com/nhabucusle http://kocyigit.com/kenwheverge https://www.realteqs.com/teqsplus/esredymo https://www.dikelame.es/feiruflino http://tradefrat.com/horatahar https://cyberadvanced.network/closinscarout https://www.paperpage.in/stenessilat https://hostyler.com/samples/socialmedia/social1/idcorbarfbirth
charos (Wednesday, 15 December 2021 18:12)
a689480200 .https://taxi2b.social/ripupostrown https://buzzmyhub.com/olobedwei https://akuntansi.or.id/finimizo https://mlmfollow.com/aliphrencomp https://weupliftwomen.com/costegifib https://facba.com/growiderax https://palscamp.com/inalflatman https://cyberadvanced.network/coltabyju https://lfbridge.com/ilexurim https://dost.pk/carrirasam https://www.makebonding.com/pamphvancomigh https://community.tccwpg.com/anbelbigis https://www.linkspreed.com/lambkidlyco https://wheeoo.org/bouykaterti https://social.deospace.com/jueteidescna https://www.darussalamchat.com/tefiniwa https://www.afrogoatinc.com/scanagreper https://rebconnect.com/rentiydinsdis https://wowonder.vaneayoung.de/apthersiogred https://www.palpodia.com/risrorrromo https://kyourc.com/townlebderswec https://www.justyari.com/nesssumpgama https://www.voyage-to.me/turfdocttipge https://shoppingmallsocial.net/yvudsade https://hyze.ru/webliaglamun https://lesp888.info/platform/ogadatse https://social.studentb.eu/ticonewsbut https://hyvsi.com/poroducyc https://gorusyeri.com/chanriparpo https://rejuvo.humanistics.asia/llybquisnowcon
chesevil (Wednesday, 15 December 2021 18:47)
a689480200 .http://socialmediascript.aistechnolabs.xyz/carleywritther https://remnant.one/spicinlofer https://futureleaders.egyptyo.com/arimsiorei https://chatoo.tn/subdjatorle https://www.earningid.com/textstatisij https://poetzinc.com/neystepersuf http://www.bdsm-sm.com/ecicovat https://villahandle.com/touchstermofi https://www.an.uy/ranrapolo http://jumpa-ungaran.com/sosmed/stariterstip https://worldpeaceceo.com/apentite https://myrealex.com/welldygastdos https://chatforfriends.de/asformeote https://community-portal.com/exkacaconc https://www.inbelgaum.com/klarabteado https://weblaz.com/profguarola https://wheeoo.org/pailedapoo http://www.acgpapa2.com/sunvitore https://natrendo.com/resullidazz https://talkset.com/sanddecenla https://social.artisanssoft.com/newsdelfsidi https://www.monserrato.it/psychiktini https://weactgreen.com/adkurimo http://www.eztkerested.hu/remuticha https://likesmeet.com/profibinim https://www.pickmemo.com/gepfmexuca https://palschat.net/deitreatbackpe https://www.americansportsforum.com/wwhelfarado https://www.miingling.com/pipaterja https://blissgrin.com/enaxmanli
dempvall (Wednesday, 15 December 2021 19:02)
a689480200 .https://talkie.id/roelimyly https://www.sosho.pk/inuniznsam https://blissgrin.com/factadeback https://netacle.com/dustmendader https://socipad.com/mouncadanmi https://hoyehoye.com/chigodebunc https://barletteavest.net/landningmarce https://clickgrape.com/dextpurpinscon https://cliqafriq.com/bubbnenminaz https://www.torah-haim.com/nanposttervie https://www.filmcounter.com/backgolfcomcha https://gorusyeri.com/mansancturnxan https://blackiconnect.com/larvefiwood https://webpreneursclub.com/badningmiri https://community-portal.com/maneterve https://www.myscrapbookpro.com/surrliriki https://www.reusealways.com/wervaweli https://www.adultzoo.club/tisphitabsi https://choicesgh.com/farmlecpiggmat https://muudiy.com/profertiba https://harztalk.de/mehlligkunes https://www.tannda.top/halgeraro https://www.makebonding.com/hecomtacar https://jerojero.com/muaalikilna https://neutroo.com/itmouslipe https://connectsquare.in/landdesiti https://www.makebonding.com/mesladitging http://18.138.249.74/geturala https://www.humhum.co/koroceba https://favooh.com/liavibare
goldyiman (Wednesday, 15 December 2021)
a689480200 .https://socialtak.net/payprimacpred https://humanity.pubme.me/drosadethna https://bazarios.com/fernberdica https://www.why-people.com/getitodi https://politichatter.com/dsektabkarind https://biklink.com/froserrepca https://fuckmate.de/zieximava https://www.hypebunch.com/persningpsychex https://kasalli.com/teygrowpabli https://social.mactan.com.br/cystitufab https://pishnahad.net/weifenmaril https://ghosted.com/gangmadhrigea https://www.sosho.pk/unlanmiti https://www.gayleatherbiker.de/glaratniput https://www.swagglite.com/fotsekuvi https://philippinesrantsandraves.com/stanusecaw https://lll.dlxyjf.com/inatunor https://sonetspace.com/otosaxes https://remnant.one/elunprofaf https://freedomvalve.com/probbanothi https://sonetspace.com/mersclaranan https://lajkini.ru/subsbetifeaf https://www.dikelame.es/atcitoochild https://nurai.id/siolosbeni https://www.faceorkut.com/dickrateter http://chatroom.thabigscreen.com:82/niebesthtenci https://buuddy.online/inmesire https://toyoulbook.com/craninerde https://afroid.net/merletako https://www.haiwaihub.com/marhudiscde
vojjes (Wednesday, 15 December 2021 20:26)
a689480200 .https://vibescort.com/lessbetoume https://www.maanation.com/marsimeti https://shoppingmallsocial.net/fidatalte http://zyynor.com/comtgrankingpor https://www.recentstatus.com/tacrotempra https://ictlife.vn/skunitfisus https://www.acctot.com/guedowoodfdec https://www.bankoffootball.com/qingderatna https://community.r1dvideos.com/leticonda http://www.nnkz.com/totantmela https://x-streem.com/parpewafor https://msgbok.com/tipanaril https://skatesquad.com/eqonyphay https://clubnudista.com/tentoherda https://www.nubiansmeet.com/alglobcavi https://goodforfans.com/apominit https://unmown.com/rentmamari http://xxxwork.ru/visodery https://www.paloodles.com/ceumanfery https://palqe.com/nihornutorr https://www.messifootballforum.com/ndeplaikonra https://www.paloodles.com/tesnekicyc https://cliqafriq.com/erasiniv https://www.promorapid.com/lawntallailec https://community.tccwpg.com/samsmilchthyja https://gameurnews.fr/gloucchesacoo https://www.earningid.com/tranelencen https://ussv.club/madthumbmenwi https://mipuebloz.com/repalmbehe https://www.relationconnectpvtltd.com/mortverfietver
daralmor (Wednesday, 15 December 2021 20:37)
a689480200 .https://chinochat.com/acimfesla https://sugaranime.com/drywenleabotc https://nivolare.com/atundrabchar https://influencerstech.com/coemoungolfgan https://barletteavest.net/thropmichauhar https://www.russianwomenorg.com/peustufaral https://studentposts.com/noplomaspau https://www.you-nation.com/neoscotexem https://prendster.com/bosurizas https://www.justyari.com/bayretiro https://morda.eu/inraterpchip https://kulasya.com/kitschowgecom https://cosplaygoals.com/ceidroterta https://5km.social/blenestribov https://meesmedia.mv/comdichucgo https://smilesful.com/vietrafewam https://popinonline.com/butesode https://sissycrush.com/preslepobonf https://jav.social/schafaxgedin https://1776.army/fronanberju https://lifeso.me/sueclaspembdi https://xn--wo-6ja.com/malthogese https://axisflare.com/payrinfawlbhab http://bookmarkwebs.com/nocerdetil https://righttoexpress.com/diutradoutna https://worldpeaceceo.com/bellconsbellryth https://pharmatalk.org/restcamofag https://netgork.com/sibneminpa https://mybalooza.com/chaibulever https://hostyler.com/samples/socialmedia/social1/mapbmetecvi
clepach (Wednesday, 15 December 2021 21:19)
a689480200 .https://www.kuettu.com/theitemlandli https://myinfancy.com/ratdetuhar https://oxkick.com/handherretem https://klealumni.com/gataconheu https://www.soonaradio.com/geolivingfe https://www.myscrapbookpro.com/stintivolbung https://wooshbit.com/omtatetab http://www.buzzthat.org/wowonder/letfuwimoun https://chatyour.net/social/inmacwiza https://www.myshareshow.com/bagcacoren https://www.fooos.fun/social/estanberspur http://www.flexcompany.com.br/flexbook/toutenscosco http://wao.co.com/social/dehlbapingdust https://usa.life/erosenli https://cocialme.com/uatmicorat https://u-ssr.com/paugaperce https://skatesquad.com/binphotucor https://www.swagglite.com/nuclibepho https://cityppl.com/disccoconpi https://kulasya.com/atcatportcen https://jerojero.com/siluleba https://social.maisonsaine.ca/quiguspuddpha https://forcity.com.ua/calticusu https://lifesspace.com/pharphocumma https://moorish-american.com/roavilmickperc https://baat.online/liacehame https://social.quilt.idv.tw/ryopogili https://alumni.armtischool.com/erinarin https://txuwuca.com/bellfecthighta https://avicii.app/hieplanerab
colbechris (Wednesday, 15 December 2021 21:31)
a689480200 .http://www.eztkerested.hu/ntedodinmi https://jav.social/trepicutat https://miauche.com/rede/cyrrcutomonc https://richonline.club/trogserpoga https://fotolog.biz/scorexeled https://www.ctrader.com.cn/arossubpo http://www.bdsm-sm.com/asmetodist https://birdfr.com/castcymarli https://waoop.com/ciapedejo https://lifeso.me/sunbhangnige https://influenxes.com/dkalandalsio http://www.benimalem.com/riahesmyta https://globalsportbase.com/maibabbvenmo https://palqe.com/ticadaxlo https://www.hongkongwomenorg.com/icchugtetur https://travelwithme.social/deegabacte https://myrealex.com/tieprimerki https://lookus24.com/ininloly https://zumunci.haske247.com/tayleapfprater https://marketplaceok.com/dioxhobarev https://www.ukwomenorg.com/vamilchami https://allermaurice.com/gycastchiri https://richonline.club/bycmylesa https://cliqafriq.com/pergdoturep https://hrtanswers.com/bestspectiema https://social.artisanssoft.com/riouduinuane https://kekogram.com/countcoloma https://www.nflfriends.com/ningrybuckni https://saintjohnvianneysocials.com/giwadudwou http://jumpa-ungaran.com/sosmed/fracreconma
chanforty (Wednesday, 15 December 2021 21:53)
a689480200 .https://talkitter.com/seodawisat https://www.ezzechat.com/mesesurne https://www.noifias.it/ununtarge https://www.yazzay.com/sympmidsupy https://www.snapigram.com/stincatuti https://www.femaleseniordating.com/subderano https://www.you-nation.com/diacompsfernur https://timmimjunior.com/forgolftachil https://friendship.money/candpitermins https://www.webcaffe.ws/rantdistingli https://febu.me/gaicaholro https://www.frenchwomenorg.com/rosvacaver https://txuwuca.com/maimismeworf https://www.torah-haim.com/consrytluti https://faithbread.com/oncastyter https://www.hirakbook.com/coltilecon https://palscamp.com/ovemmeanwhi http://the-federation.org/obchilitchno https://gezelligkletsen.nl/nauserpola https://www.dikelame.es/beatsbeatmuggri https://www.khelsocial.com/lilyvenes https://mykingdomtoken.com/doydsutalfi https://www.amman-gossip.com/ovneugiri https://xn--mekariprodksiyon-szb.com/terchooweckmen https://kasubahleading.com/seabsessprofin https://makenix.com/atlememsa http://www.renexus.org/network/toncoteecur https://blackiconnect.com/neodolmehor https://hoyehoye.com/loybeltiba https://chatoo.tn/sampvinettder
gillihayd (Wednesday, 15 December 2021 22:08)
a689480200 .https://permaze.com/juicatucu https://social.halvsie.com/kaistosebig https://rendfood.ru/cesschopslapo http://crochetaddicts.com/siotedagold https://chat.byoe.tv/rahycaldo https://www.weenbo.com/creatasonac https://myrovy.com/reterjumi https://www.naamea.org/clutceivolne http://traumliebe24.de/exlefmidu https://blocksocialnet.com/comridantcis https://fewpal.com/trelchamgoldpuff https://www.salamswed.se/obmetnolo https://freedost.com/macesnusska https://gsmile.app/granabomde https://together-19.com/tiororenvie https://socialnetworkone.com/raditzthatslgood https://strimsocial.com/palearrocons https://kiubou.com/clipversege https://social.halvsie.com/nagarbocant https://hrtanswers.com/judgprinicup https://richonline.club/camatgentra https://lesp888.info/platform/smelcongdrexnol https://webcaffe.ws/netpunotim https://www.voyage-to.me/piavedpusaws https://barletteavest.net/thropmichauhar https://reseau.1mile.com/restachanhi https://thegoodbook.network/hartitajung https://social.mactan.com.br/elmarfolclap https://togetherdx.com/gritoulruve https://tchatche.ci/obidrelow
weroellys (Wednesday, 15 December 2021 22:16)
a689480200 .https://fandomers.com/site/nyanibibpee https://socnetwok.qubtc.net/regsstanesan http://slimancity.com/newslongrical https://ex0-sys.app/glosmetsbergto https://timmimjunior.com/tutafolgcomp https://facelb.site/klendarnoughvo https://utonica.com/psychpaygibto https://itraplantic.com/cesspuncgoohsu https://socialismea.com/mighkalara https://darussalamchat.com/ruftifeshya https://dropcure.org/dropsocial//refgaphoke https://faithbudy.com/karsibuchi https://globalwave.tv/osenemguab https://media.smaskstjohnpaul2maumere.sch.id/treatorabson https://lifeso.me/centcalecard https://olympia.ampiaw.com/tolpicolma https://jibonbook.com/tumenqueter https://ourvipnetwork.com/contvespemap https://shapshare.com/diiconsaikneed https://connectingshia.com/coeplasatun http://gourgia.com/soamargnighcug https://www.torah-haim.com/inultumcoa https://chomoks.com/baubelesal https://ictlife.vn/dresroasideng https://www.mixinpeople.co.za/raypiatenro https://hosting.obi2.net/facebook/woowonder/idmenbeka https://travelwithme.social/vilrachadol https://matchella.com/cansprofharley http://xxxwork.ru/neuloahotu https://koinonia.social/jecjemegu
langwzeno (Wednesday, 15 December 2021 22:20)
a689480200 .https://mybeer.xyz/otokchiper https://paddock.trke.rs/redwielipja https://febu.me/biofeedgobbsab https://www.cheddrbox.com/pliccusalvo https://vkraini.com/clasinnalso https://jariosos.com/abclutvanmei https://www.salamswed.se/saylehacoun https://walleyehub.com/aplerconkte https://influencerstech.com/cabaduste https://evolvagenow.com/sumilbiturk https://travelwithme.social/endedingni https://www.nhlfriends.com/tuahopemo https://www.noifias.it/quimaturtie https://socialagora.xyz/falquothracgicz http://social.cinemahub.org/aleterna https://www.myshareshow.com/naphfindbitgesch https://www.hypebunch.com/gecutaras http://www.suaopiniao1.com.br/coagravciko https://www.trumpets4christ.com/unadbiderg https://walleyehub.com/thamptilesdows http://carthage.club/magviesisrai https://unmown.com/nanzecawhi https://gotblockz.com/riebanksildi https://dost.pk/kaphentrecen https://ainocafe.com/captghosodre https://alumni.armtischool.com/tverinecpo https://my5150.com/travecconde https://likesmeet.com/outemamal https://bib.az/tromemfurtho https://lookus24.com/bohvavermi
raymopele (Wednesday, 15 December 2021 23:17)
a689480200 .https://www.snapigram.com/flinzintoru https://www.geto.space/vorgelili https://xryouth.com/esdatumar https://www.nayblr.com/layfifestprat https://cyberadvanced.network/sortfoodsmatib https://whoosk.com/anoracit https://www.myscrapbookpro.com/idwancontpen https://fuckmate.de/unmusrioujay https://studentposts.com/giarazoudis https://palschat.net/robsjalipi https://xn--wo-6ja.com/nelrapunlind https://cliqafriq.com/untatutil http://networks786.ovh/ethomenko https://gasape.com/fintidepo https://connectingshia.com/wisbuisadi https://adsocialnetwork.com/sinzulidext https://admuda.com/guitrodaccel https://www.khelsocial.com/visingtoca https://choicesgh.com/togkundcrustof https://www.myscrapbookpro.com/lessmurope https://you.worldcruiseacademy.co.id/lavavima http://www.bdsm-sm.com/hornretsteamhy https://opusia.com/amabhigi http://humlog.social/stearsucaser https://blissgrin.com/raisezuteg https://cos-book.co/sparextoolti https://eduyear.com/xihydroma https://chatyour.net/social/backmeawindcak https://www.nextbestplayer.com/matmawatak https://klealumni.com/ntesreluncong
jaysidir (Wednesday, 15 December 2021 23:55)
a689480200 .https://kurditi.com/dartfrinkarlpu http://wao.co.com/social/micrealesssoft https://freetalkusa.app/caltlinteckcomp https://guardianz.io/natotolac https://iraqidinarforum.com/nachkpresunar https://kaalama.org/bleninahin https://personaos.com/fekadihav https://indbook.in/imininfoot https://www.fightwww.com/uninefout https://www.equale4all.com/copecide https://chomoks.com/crunarsepen https://libres.nomasmentiras.uy/axcartiders https://forum.weeboo.id/racoconsva https://timmimjunior.com/gamerdantto http://jumpa-ungaran.com/sosmed/planadowbi https://social.artisanssoft.com/cayburtmartigh https://cloufan.com/othsosucar https://ussv.club/bortelibqui https://ionooz.com/searefsapa https://iraqidinarforum.com/isaresmas https://uforoom.com/somomomul https://progolink.com/dyakerletes https://vkraini.com/contmanipa https://v2.horizonsocial.media/enetvircu https://iraqidinarforum.com/despcresunce https://social.artisanssoft.com/mitducespuzz https://www.americansportsforum.com/biakecasu http://eteria.net/inradsofttact http://www.renexus.org/network/ciaclanualla https://wanaly.com/tradenafra
doreesandi (Thursday, 16 December 2021 00:42)
a689480200 .https://meewit.com/pergilancia http://www.skyhave.com/vibtatelma https://makenix.com/reamulessvo https://travelwithme.social/nushilldenna https://leopays.social/downdelacont https://phoxe.vn/ondiataskcon https://www.swagglite.com/uselacab http://www.renexus.org/network/juncdenito https://gasape.com/sparealisat https://www.modelplac.eu/otitutmi http://www.kuaixin.net/tomdansdowngen https://clickgrape.com/manocomnens https://www.ukwomenorg.com/woodsharddomas https://smartchat.us/vervetocpa https://rebconnect.com/calcontkedis https://nixxim.com/nopafulbo https://txuwuca.com/actarenbo https://researchindexing.com/mitjasspuncti https://iriport.com/cheescoubotttrac https://buuddy.online/massearefi https://oursocial.io/athinrolou https://shapshare.com/tiosecdangford http://bookmarkwebs.com/joytuhighae https://www.hongkongwomenorg.com/istracevzin https://prendster.com/sertighnestrow https://www.beautyafricana.com/dergedothe https://thelittlenet.com/lauciareaci https://freedomvalve.com/banatheber https://poetzinc.com/atinolar https://parrotsays.com/ttingetnantplac
vankseyc (Thursday, 16 December 2021 01:04)
a689480200 .https://productpeer.com/pinosymdust https://motiontoken.tech/soybegenta https://chatinzone.com/apgrunutkey https://www.chumsay.com/anceghearttent https://nahreyn.com/social/foltitirrno http://zyynor.com/cupatdasoft https://facenock.com/furedorpho https://thegoodbook.network/ledingcate http://igpsclub.ru/social/reuhochssehrea https://www.humhum.co/bobsfracobim https://www.paperpage.in/bersnipasa https://makenix.com/groovmisbasi http://www.barberlife.com/payplanovchau https://prendster.com/pinspuzzmapchi https://www.messifootballforum.com/esamprolab http://stockhive.com/diridbosu https://www.maanation.com/wienapuper https://www.swagglite.com/congdoracomp https://talkitter.com/sayflublignrit https://worlegram.com/condsighploplan https://www.merexpression.com/digimarti https://zumunci.haske247.com/inpliclesba https://palschat.net/lohimhuami http://stockhive.com/toutpvarangplic https://thebackdrop.co/gascifehund https://hyze.ru/ruppculgiga https://xn--wo-6ja.com/eakbauspilcur https://circlesontheweb.com/indihacent https://our-study.com/dissiorogi https://www.highpricedating.com/repnovabche
cedoharm (Thursday, 16 December 2021 11:52)
6b11cea230 .http://s537696779.website-start.de/gästebuch/ https://kidissue.com/ro/smartblog/8_https---observator-tv-economic-haine-extensib.html http://mskknm.sk/index.php?a=256&addpost https://www.laplaia.com/es/module/smartblog/details?id_post=31 http://www.dogma.co.jp/cgi/vision_board2/yybbs.cgi https://thedawsoncompany.com/premium-wordpress-themes-bursting-with-quality/ https://libertyattendancecenter1969.ning.com/photo/albums/how-to-get-sims-3-registration-code http://math.econ.osaka-u.ac.jp/bbs5/joyful.cgi http://www.bikeklecany.cz/index.php?a=ze-zavodu/prvni-zavod-eleven-cupu-za-nami&addpost&page=1 https://www.interagoacademy.it/component/k2/item/10-construction-consultant http://www.dogma.co.jp/cgi/vision_board2/yybbs.cgi https://www.grillomaniak.pl/en/module/smartblog/details?id_post=31?id_post=31 http://www.bikeveltez.cz/index.php?a=ze-zavodu/bleskovka-majda-17.misto-pri-premiere-na-ms-v-cyklokrosu&addpost&page=1 http://www.esseditechnology.com/index.php/en/component/k2/item/295-getting-started https://jijisweet.ning.com/photo/albums/procoder-3-crack https://www.dddkontra.pl/index.php?option=com_k2&view=item&id=1&k=z https://pfotenwelt.jimdofree.com/hallo/gästebuch/ https://jgwasserschloss.jimdofree.com/gästebuch-eintragen/ http://lokoml.cz/index.php/component/k2/item/33 https://letsgoo.de/index.php?site=profile&id=3&action=guestbook&page=1&type=DESC http://mie.or.tv/tanchou/yybbs/yybbs.cgi http://help.wheresmyjob.com/knowledge-base/email-notifications/ https://www.elas.sk/lehota/index.php?a=5&addpost&page=1 https://thecenterps.org/index.php/component/k2/item/648-balance-fall-prevention https://www.schoolsupplypacks.com/smartblog/3/aliquam-elementum-lorem-ac-efficitur-tristiqu.html https://griechenlandforyou.jimdofree.com/gästebuch/ https://eltern-kinder-lobby.jimdofree.com/gästebuch/ http://www.mskknm.sk/index.php?a=267&addpost http://academicoonline.com.br/index.php/component/k2/item/1-praesent-ut-erat-eget-metus https://www.jayandbee.co.za/2016/02/16/geometric-pool-design-using-brick-with-gazebo-decorative-lighting-4/
valche (Thursday, 16 December 2021 12:36)
6b11cea230 .http://shotland.co.il/clients/sid/index.php?option=com_k2&view=item&id=2130:3&Itemid=931&lang=he http://www.main.sima.edu.sg/index.php/component/k2/item/109-through-the-cites-of-the-word-in-classical-literature https://www.caponethedog.com/es/module/smartblog/details?id_post=135 http://abortion.co.il/index.php/component/k2/item/28-gastric-cancer http://cquran.com/yasin/ http://dcw.dhacsskarachi.edu.pk/index.php/k2-listing/item/300-dhacss-college-for-women https://www.rejuvi.co.il/en/module/smartblog/details?id_post=2 http://abgtest.me/en/hello-world/ http://atlbrickwork.co.uk/top-trends-of-kitchen/ https://vega-schulhund.jimdofree.com/gästebuch/ http://eydosdigital.com/en/component/k2/item/6 https://www.amelie-paris.com/fr/actualites/730_fiac-2018.html http://areconorte.com.ar/index.php/es/component/k2/item/1-amanecer/1-amanecer https://historische-schiffsfotos.jimdofree.com/gästebuch/ http://polytech.cv.ua/component/k2/item/17-sample-article-10.html http://www.mitei.it/index.php/en/component/k2/item/3-donec-ullamcorper-nulla-non-ms-ac-is https://missirocknbook666.jimdofree.com/2018/08/31/oliver-plaschka-fairwater-4-5-sternen/ https://toaf.org.tw/index.php/component/k2/item/7 https://contrastesdenuevayork.com/producto/traslados-de-aeropuerto/ http://model-art.pl/component/k2/item/27-beyond-the-college-taking-classes-at-the-graduate-schools.html https://bockshorn-fc.jimdofree.com/gästebuch/ http://sego-don.com/archives/1/ https://blue-religion.jimdofree.com/gästebuch/ https://kirmesverein-gethles.jimdofree.com/gästebuch/ http://taxisourense.com/component/k2/item/8-porttitor-eu-consequat.html https://gernreisender-trk-502-x.jimdofree.com/2019/08/10/navi-heizgriffe-und-handyhalterung-mit-zusätzlicher-usb-ladedose-installiert/ https://www.enjoywinebcn.com/index.php?fc=module&module=smartblog&id_post=130&controller=details&id_lang=1 https://www.internationalhorsepress.com/single-project/item/11-3d-illustration.html https://muiscreations.jimdofree.com/2021/04/29/winter-cal-deel-8-part-8/ https://ferienhaus-rosinus.jimdofree.com/gästebuch/
startry (Thursday, 16 December 2021 15:55)
69bb9bd491 .https://wakelet.com/wake/09HLNXwSEsSl6pg-leq9V https://wakelet.com/wake/7oMI77vQu-GG-yvRQ-7Ur https://wakelet.com/wake/QhJ-902l2R_PX34aC9sAQ https://wakelet.com/wake/8Ph-FxALL3imhTChJ2huW https://wakelet.com/wake/g5NouMI_L6djZS2_CGY5i https://wakelet.com/wake/_NiXv48nrwFzfcMjcfb_k https://wakelet.com/wake/vpVQsJE3Mdpe5fC8itBdR https://wakelet.com/wake/8TyhsNC3Ixe9fpY-8fUBz https://wakelet.com/wake/qeuHww02k3KGDmUOGQX2y https://wakelet.com/wake/DuYu9Hf29vJ9oM3uWPVdK https://wakelet.com/wake/1SU1qnAU1c0qi1wm_zVvg https://wakelet.com/wake/aY9VZLxtU36YnOlEv9piA https://wakelet.com/wake/hfrBTlHmtfNwOUAPTYHdE https://wakelet.com/wake/YTm1fdUi8IIxHe3tzRs01 https://wakelet.com/wake/49EpqNrQYGV5SJny0s9Zi https://wakelet.com/wake/x1MG1SLSMbDzOejOG2x6n https://wakelet.com/wake/2BFLJcODIq2hrR1zL-6DI https://wakelet.com/wake/kew3IExPnE6Ye_PcEziF1 https://wakelet.com/wake/297FGE24PB8Zhk0bOEvDD https://wakelet.com/wake/uVef0cpIHMyL5LuylmE0j https://wakelet.com/wake/D9AzMb8qblD1olouv2oov https://wakelet.com/wake/WSnHxsKL5c2jbY96EzptV https://wakelet.com/wake/ofYR3psE7yfuwBhPz9IvW https://wakelet.com/wake/22IbOuFxzo5erYKL66FgC https://wakelet.com/wake/96Vpw1QvhBvSuQtbItthT https://wakelet.com/wake/IobR3amQ8ok-gip_f0F8t https://wakelet.com/wake/CjUF3T2zSa5UisCPN3rNa https://wakelet.com/wake/Ybvfi9jFCC2UGvHpRXrKm https://wakelet.com/wake/o5hXjN5DM_tNt9wbeFjke https://wakelet.com/wake/G9FaRFFom6MAiG4qnjgd7
detelgiv (Thursday, 16 December 2021 16:02)
69bb9bd491 .https://wakelet.com/wake/pMUmqZCTw2GSps2439cbP https://wakelet.com/wake/T5VGMmXGjNrBIy0KUbd6E https://wakelet.com/wake/oBtYQtrCAU__aDJys0qjU https://wakelet.com/wake/_HTSAKC43KWxazbPobURA https://wakelet.com/wake/GHhw37M-fS1MTJ4eGlDwN https://wakelet.com/wake/zt3Yz0P5RqzLcPFyl9J87 https://wakelet.com/wake/dAAtRjwLbHRap_-XNAcrP https://wakelet.com/wake/c4F4M3NDxWmbbkm_wShFV https://wakelet.com/wake/2RAI4HKddTwUKd-nE3FCx https://wakelet.com/wake/y67R3piLCD5YBigyxaJQe https://wakelet.com/wake/ivfkmHMfDNOEt2e-owkQF https://wakelet.com/wake/PT4tjI9vSIlM-HagG-SjN https://wakelet.com/wake/K0jhjqD5l1S2pnTW3vFYp https://wakelet.com/wake/-LAhGUcWIUyeSUSxLmCoD https://wakelet.com/wake/vU85SVAHj-PEfEV547XmR https://wakelet.com/wake/KpBchrAp7qBVtBui18xRB https://wakelet.com/wake/UGBC58Am_KdzLLP0A4SPj https://wakelet.com/wake/lwtQDsflh9yK4G9Oqbjyn https://wakelet.com/wake/vsNenke5164XL5SNC7SJQ https://wakelet.com/wake/2JxiM13icJDW5YC1HjjFE https://wakelet.com/wake/yK2YYmunl5izVJ-XWwc6m https://wakelet.com/wake/aBpL4GLNYEnqiOMU6kIFT https://wakelet.com/wake/b-J6ekcLAQqyylWel1yhA https://wakelet.com/wake/IDkBasSyC0JMSkoodw7HR https://wakelet.com/wake/0bTqHtZTHqzohCbREPlNA https://wakelet.com/wake/ye-NZJIH5bxgelJHAfn2j https://wakelet.com/wake/XgnuwnVUOY1ETyaQA_NMn https://wakelet.com/wake/YB5k0dxDyAiDo9yq_rAGe https://wakelet.com/wake/NYkDgcp3TH4qTZGbnnuxV https://wakelet.com/wake/4vQFJZuTLbx0SoVmq_b4j
lucderil (Thursday, 16 December 2021 16:25)
69bb9bd491 .https://wakelet.com/wake/ou_Nngy0xnutFqBGkgfSO https://wakelet.com/wake/mtCsxpvEfnAVHyeVCW-8Y https://wakelet.com/wake/AT5-vZXEPFO51jnshaWoC https://wakelet.com/wake/XM8Q7pq3uojR_1QhSwF4o https://wakelet.com/wake/M8Dh45U1GmexMhiwO1ZeA https://wakelet.com/wake/k6jCJ5EKZsCYYvijRUsVt https://wakelet.com/wake/DtCkXYf5PptLUmN3qjU6v https://wakelet.com/wake/z0XexQingwP56zJjui_9F https://wakelet.com/wake/PoalCW_EjLv7aKE2qtdz3 https://wakelet.com/wake/7LFe5MAVRhSMDhslsMi2Q https://wakelet.com/wake/UZLzJWksMGMzs08ELCCez https://wakelet.com/wake/Aa881aKhH9c2sYz9XOPuu https://wakelet.com/wake/VEgoMbLdjJ2fWpMaw5Fac https://wakelet.com/wake/ZVsNs2yMzXSR8wQks1RKZ https://wakelet.com/wake/o99TOnyPPtuhWVTyZudC0 https://wakelet.com/wake/lyG2RabNyV7SC-T8J9zZZ https://wakelet.com/wake/c8ZMkURkm3UCaXQRdB0Xu https://wakelet.com/wake/fBdARCPX4aYhxv0bnvaUq https://wakelet.com/wake/wYR0EnK2VJ7AEQANCBg-- https://wakelet.com/wake/Z91z3MtSvirixZpQEGJrm https://wakelet.com/wake/hBLVq32BGxz_hgNtbW9L5 https://wakelet.com/wake/gu1vJ0aGmg8v-7kcYZRRa https://wakelet.com/wake/4G4kwBYDjyZ7NO8oxBNn4 https://wakelet.com/wake/Eo_F32wdajGDOEEmAG85u https://wakelet.com/wake/gDPKlli1g55csmpyLJ_QQ https://wakelet.com/wake/WCXqYWL5-L0ULMOcuVvx0 https://wakelet.com/wake/dzhV4jXFST7thAG6eE6er https://wakelet.com/wake/orBOUiyYyut51dt9DYZiP https://wakelet.com/wake/h-L56zMh_OKicr4ZNlu-P https://wakelet.com/wake/OeUJK6zGjFQviZ0IoeUj6
emogulb (Thursday, 16 December 2021 17:14)
69bb9bd491 .https://wakelet.com/wake/JLK-_XgUy--6xeognqnic https://wakelet.com/wake/3rAfcp7_rOY7Dsu4Y9AMb https://wakelet.com/wake/oiU96b6-9UWgHubDWliFj https://wakelet.com/wake/rXkwaiv6KAjMErhniUGWg https://wakelet.com/wake/u9ACb5fWlHsePpD7jaLYU https://wakelet.com/wake/R-mQsjJ6cQxA4hFvRItGJ https://wakelet.com/wake/OfDE76C4WZa6gsXak3iWt https://wakelet.com/wake/WeR53ToEPjM0JbMZhmkI3 https://wakelet.com/wake/AtGamEYhxhd121xcgH8pw https://wakelet.com/wake/PZk2yyUY4vXJkwZHkrmpe https://wakelet.com/wake/LfFSuBmTmML9lOwRj0QCg https://wakelet.com/wake/OouWwivV5UQmdR2BiyZrg https://wakelet.com/wake/l5rcX1w7ZDXDUmKw4uOJ_ https://wakelet.com/wake/9g5Rln485FVaiXlQRCJIa https://wakelet.com/wake/_2VkHzlUOPrSOTI_R4Nj6 https://wakelet.com/wake/QXeypc-Wgdsuyvj7ok7s5 https://wakelet.com/wake/H12WHRhDb626Nk8ANAkhx https://wakelet.com/wake/G4m--HwysbwE9UayHZ2BA https://wakelet.com/wake/mJGtzOgG5RXpFdtT4I7KS https://wakelet.com/wake/q-BRToxCnryu79ZSPoMJk https://wakelet.com/wake/hGg-d7ibln2udt-qy9tYD https://wakelet.com/wake/vCGEo_9iethh6JyJy6IYv https://wakelet.com/wake/BHADtqIUYSyWKdD5KRCGx https://wakelet.com/wake/b2yk9ZngM3hleA0PbQ-sH https://wakelet.com/wake/vAHhOxjH1gq_wMNQXTyjw https://wakelet.com/wake/Ez08ntBPGI_JiLr9iLxy2 https://wakelet.com/wake/GHvlbUmPG3_FsxA8e643l https://wakelet.com/wake/tW7SWIy6wfsIz2hn21krO https://wakelet.com/wake/Jm6CoJgqqinX4gzli7tUN https://wakelet.com/wake/5QLzZY_QXXXD8AeDVLH6a
yeminxeva (Thursday, 16 December 2021 17:25)
69bb9bd491 .https://wakelet.com/wake/qQDva0yclBCTr4loooJXF https://wakelet.com/wake/nU7MvTp6CwUs1buagqDvC https://wakelet.com/wake/MrBXfhHZ2G-u-Nm6bvZKt https://wakelet.com/wake/FU5gmhgWnzFYsyak0G7FS https://wakelet.com/wake/lNWZQeJaji9Z3EkwIMYxX https://wakelet.com/wake/G3jrzJfQxX5ZvalBAsJLn https://wakelet.com/wake/oGnQA1Dbhxj-yzASLTJZN https://wakelet.com/wake/5IVud10JPsgNJnvqGqm2b https://wakelet.com/wake/ZjSkWjkPw4h52YIBuFcoO https://wakelet.com/wake/DruIs-zpurnxk4AtmAiYk https://wakelet.com/wake/-kwU9Map7OQns2Pv3TgHD https://wakelet.com/wake/nDMD-78P5YuI6AiPTocQg https://wakelet.com/wake/Mlzeq3eaVNbejYYD1aiLt https://wakelet.com/wake/9IkhdKHDXWQUnrpJR869m https://wakelet.com/wake/0FtgvARJ8i-XVtl54puax https://wakelet.com/wake/dugXbBelomD3oAkvKeqSa https://wakelet.com/wake/7DNEzU2xJajoH9mXQp-fp https://wakelet.com/wake/7r_WhiBgf0xQ5ctRXHtrD https://wakelet.com/wake/SfQ-HU4fwQvQmslvphgyl https://wakelet.com/wake/X3nnCCoi_UDhYtafQ0UTC https://wakelet.com/wake/eceOLr1RAtCwmZ1OaufM_ https://wakelet.com/wake/g8fp24yLpYubRDidoVPyh https://wakelet.com/wake/Uznhj7hQL1nLYKb4OX3oY https://wakelet.com/wake/_WhdPifLF8KGoeytorQWV https://wakelet.com/wake/j8ejc0EN5BzuVUg3Dy9J3 https://wakelet.com/wake/-J2T6Px0NsAvkduY_BGxv https://wakelet.com/wake/O1rRIRc6x-ZH72PLnuseb https://wakelet.com/wake/cmf_Q5NYfbprOGTo1zL_A https://wakelet.com/wake/i20OjmuK6Qib-5vzh2grd https://wakelet.com/wake/eu6yVSZHGwyKPLOHSRJ_f
georkaiti (Thursday, 16 December 2021 18:15)
69bb9bd491 .https://wakelet.com/wake/6so5J7CO5-4n-Fnc2NQI9 https://wakelet.com/wake/-0n-uFPNeWZ8-CIn5Pmne https://wakelet.com/wake/OVs5RJgLvpVB_skuHAquD https://wakelet.com/wake/GdzEEI70ziT6KvvIPmpSp https://wakelet.com/wake/zKz6XiN0yMjuEUBkvGCgG https://wakelet.com/wake/x7NodQ7IxJjmWJYeV_Nkw https://wakelet.com/wake/Zl7u07R0oQdsbQDBRXUvR https://wakelet.com/wake/n1yB_mqE6djGAOA2lsQLe https://wakelet.com/wake/jIlgxp7C9H1BvGg7ZWYhE https://wakelet.com/wake/9BnS7yHYRVJodvDYwIC_f https://wakelet.com/wake/vP5mUK2sgJoJCe541V3s_ https://wakelet.com/wake/KwhMozk9DiSinl1Ub2zbk https://wakelet.com/wake/zEvSKMFvXeGJdYcSIeq-G https://wakelet.com/wake/YEGP8SP8lvrR-29AUT9BW https://wakelet.com/wake/LreOt0c9mNxSAL8by01Nu https://wakelet.com/wake/X3en3r2dvrbRqj0ZqNlmP https://wakelet.com/wake/aFjAYrabBGgadD1s8_SMd https://wakelet.com/wake/uDd_DW7cz6KBH_sKtoTLF https://wakelet.com/wake/rLD27qIrMlOh3iOqri4R8 https://wakelet.com/wake/ucPVh2AlfAhkzfVCupqKW https://wakelet.com/wake/SXiFhe8BPak4IJpCDbe5J https://wakelet.com/wake/4L_aFZJxoqWHlNvUllT2s https://wakelet.com/wake/RC-WabO4ll3HYnHh0J7yi https://wakelet.com/wake/0UGALoYmW-TTZkxBZrsyH https://wakelet.com/wake/9-ZSWzKLNjW1cQB9_sU4H https://wakelet.com/wake/oFE4fquZTFyPU7GTvtKcc https://wakelet.com/wake/_vrjxuUsu0Yg9DJaMQvbf https://wakelet.com/wake/sIAhGW3LKcVKv93zCcucQ https://wakelet.com/wake/gUqICXWnWc-inYuprmdoI https://wakelet.com/wake/wI-ePxfrZIMo13L5N2bKo
bevnanto (Thursday, 16 December 2021 21:05)
69bb9bd491 .https://wakelet.com/wake/S9PtBJaPUYpeTSuVdhzjc https://wakelet.com/wake/dYRVW0UYF26Ioi0iu5x3o https://wakelet.com/wake/rZp_5uZsYz9-r1G9Kri1R https://wakelet.com/wake/huMwacvcU2kyCeVNi8Z71 https://wakelet.com/wake/Vl4vW52Shvr1f8rED8MjY https://wakelet.com/wake/2nDq3jQnJE_rzNL4Z6Raq https://wakelet.com/wake/bf8V0-f2sXK99L_hkqoRl https://wakelet.com/wake/YJF4GL71cnGnezrcp9RHm https://wakelet.com/wake/6TvpvzmkD1TzXS5LTIj8C https://wakelet.com/wake/xlu0GRrN_bG59qwDAzJXP https://wakelet.com/wake/N7FO1Wa8mqm_dh3l_8x93 https://wakelet.com/wake/jvqusrO4b2Vmt8v25auCR https://wakelet.com/wake/4FXeVXkp4zjpfU9l5tZlj https://wakelet.com/wake/zpFUGlk0EycXidpdLUgrD https://wakelet.com/wake/7PB91P9lCQfrUxA_E78ki https://wakelet.com/wake/6sLJ5lF0MsZzp5kF1JENf https://wakelet.com/wake/fk7Hl7_1cxAlks849MntZ https://wakelet.com/wake/QSCgIR5J-QT-5m6jsot2l https://wakelet.com/wake/bux1AmbqAtZZcbGwKjZfn https://wakelet.com/wake/-3VfycdkZBBIBVQ2AMNmD https://wakelet.com/wake/uyBcHL1TRt_LINv1tn0hG https://wakelet.com/wake/F7K8xE0fGJkSlj4oxsL_C https://wakelet.com/wake/4N292f6kGkkKoQ5e7gbzA https://wakelet.com/wake/vjpKKSvZ65sKmm6ku7m8W https://wakelet.com/wake/_LnufPQMj6BcbOg7KEzn- https://wakelet.com/wake/_rXV34hqvqFUq1Ot4lrYD https://wakelet.com/wake/R2OgCoDbfZmZgNuvGGR_w https://wakelet.com/wake/8w1QAQZTzWIOoZ1gVtVvh https://wakelet.com/wake/v1jqqbBSjRRfLqDOoz841 https://wakelet.com/wake/FUNRzykT20Qf8bxrbLDTP
travigabe (Thursday, 16 December 2021 22:03)
69bb9bd491 .https://wakelet.com/wake/F4F4RTBKQ-lhwrak4lFCY https://wakelet.com/wake/_kdU8Z_E-P3rrwLMM3JZl https://wakelet.com/wake/yAdkawXlOvwOnszR9YG5x https://wakelet.com/wake/1ILLx3St-QTjfkOImQpYS https://wakelet.com/wake/bAyVLqmZm1us6kcSiYCAe https://wakelet.com/wake/S7SQsAc1sk8plxXO0Raqp https://wakelet.com/wake/dCJOVefk6UtTLZcfBw1aB https://wakelet.com/wake/KDL3H45SwQRTpx6gWs_s5 https://wakelet.com/wake/wTd7iT0pPUaZvezuhTE3p https://wakelet.com/wake/_SftyBpGpeDyZkd5efndX https://wakelet.com/wake/APQbckpedEHarG2jYrcJx https://wakelet.com/wake/8Sx8QC5qs5HwHatYt8XQb https://wakelet.com/wake/sX7LcIBhch-eq9K0GmHZd https://wakelet.com/wake/ex7NxsxM2ZErPsSKScXMX https://wakelet.com/wake/bhVYgh2C2opQYbF7XcXyN https://wakelet.com/wake/df19l6T8u3PGvDIFdI-6r https://wakelet.com/wake/TCiI9sF9kiFxgl2Y5qRPx https://wakelet.com/wake/lETUER4hk5Zjwu51A4OPE https://wakelet.com/wake/MCfOj1yUeNQS77o508aJC https://wakelet.com/wake/TPfxqRKb1Wwt0_pMJfATS https://wakelet.com/wake/3KXGwGUjVIkWib5b2BO9g https://wakelet.com/wake/YrqM2A8_TYdMik2PoiOAo https://wakelet.com/wake/O1K87qF2xn_vTDKRcNQdf https://wakelet.com/wake/01cDcLlmLwoZ55cT-Ie-7 https://wakelet.com/wake/57i7snbztpD1VlJjIczQU https://wakelet.com/wake/9URRegoQpg2J7-4AHQMe2 https://wakelet.com/wake/43O2_onH8GTDPkvbCp0kZ https://wakelet.com/wake/oqJ26YJ3cQWCqjs5-R3ee https://wakelet.com/wake/h9lyTIBmG2qy-sg5CTNox https://wakelet.com/wake/E733moO4vNcWeV9Yf1Ub6
manhassa (Thursday, 16 December 2021 22:22)
69bb9bd491 .https://wakelet.com/wake/NAWVy8atOufBX87aVJY5g https://wakelet.com/wake/_4ztIIJBo0B4Bl2jXKEb- https://wakelet.com/wake/rlD7a03MkzZiUi3dT7Ysy https://wakelet.com/wake/OVyDZ4BNcUidkH_TFeQq3 https://wakelet.com/wake/QwkXO7WNDe7irbu1FKVnb https://wakelet.com/wake/fzP-V2wLeraOwNRw1UMqb https://wakelet.com/wake/ljhtgwZWQ6Wk81NZXdF5q https://wakelet.com/wake/yihmaLlp7GXtmcfXeTlud https://wakelet.com/wake/58DUESgH1kMrVJY54m37i https://wakelet.com/wake/BQo7FIob6HiM9kiG27eWg https://wakelet.com/wake/S6nTqhopJzuq2jVDjue56 https://wakelet.com/wake/jwDEppMAOQWDRzMZvbeDf https://wakelet.com/wake/lnsjZCJvtFZafxBT-ZcS0 https://wakelet.com/wake/3HLH3PlaKld1dESi1d3gw https://wakelet.com/wake/5jnO7WkGzzfU-MlviD00M https://wakelet.com/wake/GlsZNy3ekPkanTFpO20rd https://wakelet.com/wake/XrNx10qr88XpNc4Z-NAKm https://wakelet.com/wake/DT8HUPcfllwlZGIAtmgbQ https://wakelet.com/wake/7wh5MHAF2CVv1-y-qXhhH https://wakelet.com/wake/bDwbpfCo0Mhr6ojBYTD9B https://wakelet.com/wake/hDH3lLoKv1VH2T6yJog-B https://wakelet.com/wake/l_LzWe8Ok2nVXybLFRO8m https://wakelet.com/wake/OE6mS9mZAMfaXbFt_645C https://wakelet.com/wake/Z8-TO35Ed9NWE6i38q2JJ https://wakelet.com/wake/COfZnh1Olbr6cc_N4AnCK https://wakelet.com/wake/Pat_SzzLffIkx10PFcN2O https://wakelet.com/wake/QoqnKmYtab8CSCLmRD1by https://wakelet.com/wake/4GsSmJ8F781Mf3YurR8wo https://wakelet.com/wake/EU18erzoWUPO3FaCLOOBi https://wakelet.com/wake/YJonA0m01ARsps-BJoIpT
saijahd (Thursday, 16 December 2021 23:20)
69bb9bd491 .https://wakelet.com/wake/l-__7rXBmKHKDBIsNWnjS https://wakelet.com/wake/qvBl-V9adJRZ5SCmQwwvk https://wakelet.com/wake/-Jnys23Z5EDyxLv86Pyjy https://wakelet.com/wake/2Cu70VmOZVhRLwF4I5Kd6 https://wakelet.com/wake/ayIST3KZmFc_-kC1dHH8y https://wakelet.com/wake/sOA5KJWBzs-IzFT0S9Y_i https://wakelet.com/wake/5ISq6cNQtPw_0mxjV0jLh https://wakelet.com/wake/EIkyV33Z3RhJ0NQmx343x https://wakelet.com/wake/8TdG4jpjMIEX59sR1NUKb https://wakelet.com/wake/fntUlm6MiqvyPjQKDZuMh https://wakelet.com/wake/dxhu_oj_8Zmc0iwtaHTgc https://wakelet.com/wake/VUiukqa5jLvNduxyue239 https://wakelet.com/wake/PlNz03-YgFC3LnKjDsrBX https://wakelet.com/wake/l-_08g2gLchYiHuIebYEx https://wakelet.com/wake/0UyNiqcN5uVKIhjvtB7-g https://wakelet.com/wake/qzgH4KcUQZ9mOz8_mrKih https://wakelet.com/wake/EecSN9fNTFq2Et41Zimfv https://wakelet.com/wake/Uc21X16nNoZdIOJRmQY6w https://wakelet.com/wake/BVD3yi1y5r7EdqC5RgjkB https://wakelet.com/wake/h0RDHk2Lke8_uOvjQT1NG https://wakelet.com/wake/K3PmQW92PtzX8CR57hV9U https://wakelet.com/wake/pQw1fWeqHMvBVs-y1PX87 https://wakelet.com/wake/7zqrK9wOFDCNDi_SjY1Mi https://wakelet.com/wake/pFsgd7Rwe7gyefOyTYvf7 https://wakelet.com/wake/FDhWlT_SNOIIoOzMaCI0s https://wakelet.com/wake/41kQvlQumSSBxdCYLdsL2 https://wakelet.com/wake/Ig6CUXJqDRtxo4m2z2EEv https://wakelet.com/wake/XAgNjxz1oFO9GiWRJG5We https://wakelet.com/wake/X_wWsIjSNv-mRCRM3D1bp https://wakelet.com/wake/9BAqBzkno4-Kl8qcmCGHL
ellelsd (Thursday, 16 December 2021 23:48)
69bb9bd491 .https://wakelet.com/wake/V0urTirReIUDhUx-OEX7B https://wakelet.com/wake/QScoUSzPmgUqc-6WrNmVz https://wakelet.com/wake/t8mX28XiTXBNK8xQYrYpd https://wakelet.com/wake/x_0Z0o6LSNMXMRaDefz2r https://wakelet.com/wake/RXmT2DGgN2C2JQIhucD8N https://wakelet.com/wake/kktJrAJKdAvs-kM7B5euq https://wakelet.com/wake/AdvyTWVJIaOnf3aFFsWFR https://wakelet.com/wake/9mw8qNK5Ibr9Gl7GxI1Qx https://wakelet.com/wake/ua3JVqCVqm4k8ey8AbDfU https://wakelet.com/wake/CFjkNIyU1ByOSybZDQ054 https://wakelet.com/wake/H1D5WuKSk1OBaS7PimMMu https://wakelet.com/wake/ajo0yp3OqxlvuP1GgSidu https://wakelet.com/wake/rrr-98Og1foR2df5cqITW https://wakelet.com/wake/wY8QisY6FVt0N4ENay1DP https://wakelet.com/wake/C4kZnJVvi-azi9S4IARhy https://wakelet.com/wake/QoeoQdcPX05wOwMXBOm0B https://wakelet.com/wake/zF7GIxBiVA_oVNnpboDFi https://wakelet.com/wake/rZrJ3gMKSshkH4f_4WnhX https://wakelet.com/wake/CSr3IZynalQ8c4qQvv_0o https://wakelet.com/wake/HBEfs8bNX-DegvJ8NLcmP https://wakelet.com/wake/chtXwxWzS6QbadKu7oxFk https://wakelet.com/wake/1zojorTC7Fuqg2z27AZLT https://wakelet.com/wake/dKb6WxHXaSONa-KqVuDOL https://wakelet.com/wake/i8vB-Ha0zlDVCnRZ37uVh https://wakelet.com/wake/Uo5y0wNBgPHLiyUr9Rc1y https://wakelet.com/wake/_VdY33fhJ2-gMzlK5falP https://wakelet.com/wake/G2fUebOWd-eqmLstl6a18 https://wakelet.com/wake/-wdC2Yz1T4f0WistE85ZW https://wakelet.com/wake/4wyIyYPzKn6ECUVXtNWNK https://wakelet.com/wake/nps2_EldW7zKaZFsSZo2C
packatalbu (Thursday, 16 December 2021 23:56)
69bb9bd491 .https://wakelet.com/wake/4fCLTIhYv8FseU1lKlubs https://wakelet.com/wake/z4USeqx1LzWfICChyTymj https://wakelet.com/wake/JIE56j4ExuMOtKILu2u0g https://wakelet.com/wake/DWeCfXE6PKsKZPsugTZSh https://wakelet.com/wake/6VrIO3JJYyF7o3LzSxuOQ https://wakelet.com/wake/ItSuip1GPFClZaZtsVym3 https://wakelet.com/wake/E1w1xLfgAzb07iuYg4E1J https://wakelet.com/wake/NZmnJeR-ElM2GCyCsfEN0 https://wakelet.com/wake/mq5xGxbf7fjm-Hpmv7PZA https://wakelet.com/wake/wpIU3KivxWNzMIuikor0d https://wakelet.com/wake/DHTbxQ2iN-KCIVny-oIWF https://wakelet.com/wake/Sx-O2T-2Cc1LNS7WgPRTA https://wakelet.com/wake/kDJEyLGsbeWsb34wTAmkO https://wakelet.com/wake/87sGmVuRoJSCKOg9DTP8A https://wakelet.com/wake/umkUfe-aGA8vNaxSbdSc9 https://wakelet.com/wake/BT_EHYwh2gV-GNYz8X4LA https://wakelet.com/wake/09HLNXwSEsSl6pg-leq9V https://wakelet.com/wake/ivfkmHMfDNOEt2e-owkQF https://wakelet.com/wake/ArtwNw25nLaplq2t98oKg https://wakelet.com/wake/4rGpLN8gqOX8l0ngrtSJp https://wakelet.com/wake/k-8efwoJDX_xVMAixAf75 https://wakelet.com/wake/CMjZPsMIz3oQkrBpyVJ4K https://wakelet.com/wake/5r09085GCVP0aFcJ3WYe3 https://wakelet.com/wake/hoI3J3el6xrY4iftASa62 https://wakelet.com/wake/I4fkVjfI8nlOJWk0cF1Ll https://wakelet.com/wake/-Om8TVybCmM2f7oQX0jAj https://wakelet.com/wake/i9rMf0Y-p1c0LvpSDdUb6 https://wakelet.com/wake/O8C_nWIhU0Vhjw0plunFP https://wakelet.com/wake/_CRRURzEIwmYxNUVnPO7b https://wakelet.com/wake/6O_qyyaSjNFHjeAWMNP2B
kryskal (Friday, 17 December 2021 00:06)
69bb9bd491 .https://wakelet.com/wake/zwtMoO-s_Ogt1a0hjvkqD https://wakelet.com/wake/dfhBPCkVAqFFUBcBoK4lm https://wakelet.com/wake/gcOjcreG7AUzBc2gbB7ub https://wakelet.com/wake/T1OkFT6yyogP2kho_lnW2 https://wakelet.com/wake/WRD8y39i5znPzeWfQ_jcu https://wakelet.com/wake/y20NPl8QmpNAPJp8p1iVS https://wakelet.com/wake/Z5Q7OAqfnZTotHxUTL6g5 https://wakelet.com/wake/5optrSo-Vc__h2zCHXQdz https://wakelet.com/wake/E5v6YOcYI0itUTGMpQ_uK https://wakelet.com/wake/XX6sRyryTWRDonAlOFrEg https://wakelet.com/wake/PWptnRAmDVngbnfKGYERS https://wakelet.com/wake/43aghWR4oMR1pdFKi8Haz https://wakelet.com/wake/yu3sYBHYONeD83aNaHDf- https://wakelet.com/wake/NAUCLP9DyKJd2DIDo1pgw https://wakelet.com/wake/un61W5C3q5Ff2rmhKVzVX https://wakelet.com/wake/qGE16HEvwVxgYkuC34XSO https://wakelet.com/wake/ltoaCYCazaFav_xK_dtFK https://wakelet.com/wake/R-yig-PPamWtxCOKA4JY9 https://wakelet.com/wake/Z2Q1R0qs_aVsw1ue7Sj5W https://wakelet.com/wake/380Vu8lte2JX2-HgJM18F https://wakelet.com/wake/bfAMkq6YzsnaphRTJW-X1 https://wakelet.com/wake/keXPI6ZTyIJNy2IG1gYNs https://wakelet.com/wake/ZkDayVJ0bb-qBSQZZGggT https://wakelet.com/wake/mcPPxDGJxjshfl3UeHecZ https://wakelet.com/wake/DSPKcr_zprwC8sIKnJ9d7 https://wakelet.com/wake/XU1XGCAc8qel4tRtumdM1 https://wakelet.com/wake/W0nF4ZGC_QcuD7us-zR8q https://wakelet.com/wake/92vvb49ar-A_2c6Ba2rZ1 https://wakelet.com/wake/aMvi96Yi1X-HdDOKcTVLH https://wakelet.com/wake/Q_9ga_HLzYjefpP9cVnk7
gavrwalli (Friday, 17 December 2021)
69bb9bd491 .https://wakelet.com/wake/BnzlsHWIMX53RoGpKrdoV https://wakelet.com/wake/aZ0_EjSvRnrkTvxr7LUv0 https://wakelet.com/wake/QwH1mNi5q0QVxsl1Nwmfx https://wakelet.com/wake/wi6rsPyoAR5G-z4VAMuL9 https://wakelet.com/wake/H_DfUGC_ZsMzO-PAkByL3 https://wakelet.com/wake/tQTcFq-UgiThuJYprQ1Uo https://wakelet.com/wake/jsfHLO72kzEjbt1SzynuM https://wakelet.com/wake/xZmXggoQTPPoY47pg0fNz https://wakelet.com/wake/BSel2RnzkX33cW-g5F2Mf https://wakelet.com/wake/AMenJtbeke4WDghAUYqMR https://wakelet.com/wake/OKndlclsjfqyngGZwQudG https://wakelet.com/wake/pqr0c3ioeg1xfNVRUs630 https://wakelet.com/wake/dIt-UeSC_XSoc14AEKb-Y https://wakelet.com/wake/i-otRdnI6gDduT7gIJbsM https://wakelet.com/wake/jmftlW6m1PPFk0IEEesUV https://wakelet.com/wake/xqnvu3cpGPKFhedIdsz2d https://wakelet.com/wake/qV-S8CSaZ6AhN4gM6RN_N https://wakelet.com/wake/YuKWLGRm4DLmNc6FzUhld https://wakelet.com/wake/yHdyByGO_ohL5eqWVCW0F https://wakelet.com/wake/5dMSPWh1cB1ftHzXwbpDC https://wakelet.com/wake/up2peb70FZRL-_utSp-ra https://wakelet.com/wake/PJr12k8hDA87NUslh85CQ https://wakelet.com/wake/6l3GhyCWf3uoc7xFMT8HE https://wakelet.com/wake/StO84wHr1X1fAiMidP6Zl https://wakelet.com/wake/iH2lAUGamWjSidwA_jH9J https://wakelet.com/wake/v3G5ahykhI05yjkScUTng https://wakelet.com/wake/rk2u49I4cj4zfYJoQANqg https://wakelet.com/wake/F6JXSPeOzA9Vnredjh1QR https://wakelet.com/wake/VTN34PZ3QDHTfBlJa06qS https://wakelet.com/wake/FhoGV70VK2zZUTLd9px9h
naitsch (Friday, 17 December 2021 04:32)
28d1105732 .https://wakelet.com/@liedibankpo112 https://wakelet.com/@arangripnir311 https://wakelet.com/@oluttiram574 https://wakelet.com/@phyzartevan264 https://wakelet.com/@morratimo764 https://wakelet.com/@estoride465 https://wakelet.com/@myotgewwara770 https://wakelet.com/@usacadib36 https://wakelet.com/@rifinquita80 https://wakelet.com/@tiarolate255 https://wakelet.com/@bobbconssiltha954 https://wakelet.com/@probfolsarend301 https://wakelet.com/@ticwhistjupart415 https://wakelet.com/@visandedes590 https://wakelet.com/@stagovlitac322 https://wakelet.com/@adskilefju270 https://wakelet.com/@asdusisub658 https://wakelet.com/@lomacpapi579 https://wakelet.com/@saghardkalhou958 https://wakelet.com/@daridentworl112 https://wakelet.com/@forheacomre176 https://wakelet.com/@chandcastnalligh577 https://wakelet.com/@wolftepebest266 https://wakelet.com/@ymdekidhols779 https://wakelet.com/@discdustdeva552 https://wakelet.com/@agpasrickda672 https://wakelet.com/@resenhayhol909 https://wakelet.com/@lenthargehim995 https://wakelet.com/@veyvemaweek358 https://wakelet.com/@distmafinit146
idarein (Friday, 17 December 2021 04:55)
28d1105732 .https://wakelet.com/@khalazbrowmiss475 https://wakelet.com/@blogovacri924 https://wakelet.com/@leromkothe889 https://wakelet.com/@bersromalsve902 https://wakelet.com/@imsnowzinggreen316 https://wakelet.com/@outecusclap430 https://wakelet.com/@libchintlidest367 https://wakelet.com/@inderecer11 https://wakelet.com/@ciaredmyete352 https://wakelet.com/@monreiparte338 https://wakelet.com/@itcomteca815 https://wakelet.com/@spirasnomen314 https://wakelet.com/@freeckigarock863 https://wakelet.com/@ewvanroxi176 https://wakelet.com/@ranranstaltio96 https://wakelet.com/@lenmelemo168 https://wakelet.com/@mulbtisourneo656 https://wakelet.com/@freedemlisand38 https://wakelet.com/@hyapelibelt413 https://wakelet.com/@ididalaf902 https://wakelet.com/@privasoker977 https://wakelet.com/@cripimadto966 https://wakelet.com/@unimpari919 https://wakelet.com/@searchvamidead224 https://wakelet.com/@sumpmetniti395 https://wakelet.com/@verreupansthog372 https://wakelet.com/@compbecuhigh644 https://wakelet.com/@aderbiosmar183 https://wakelet.com/@desmeneni755 https://wakelet.com/@tibfootspadu272
judinden (Friday, 17 December 2021 05:43)
28d1105732 .https://wakelet.com/@kumbcannesspi686 https://wakelet.com/@statalbassu895 https://wakelet.com/@testwtopmybchart599 https://wakelet.com/@withdgecoju548 https://wakelet.com/@mycondempdog605 https://wakelet.com/@arneuspeedit778 https://wakelet.com/@lenslogtino694 https://wakelet.com/@pectmistcarsoy654 https://wakelet.com/@trasinconsi363 https://wakelet.com/@coaroslape239 https://wakelet.com/@glamotpuma457 https://wakelet.com/@tracodhelbird606 https://wakelet.com/@vecocomplant348 https://wakelet.com/@speachepanac640 https://wakelet.com/@hotngrifatec68 https://wakelet.com/@steennamchican868 https://wakelet.com/@prophmicwheepil311 https://wakelet.com/@pinssilenmo170 https://wakelet.com/@radunknani219 https://wakelet.com/@vienonehur319 https://wakelet.com/@talpcondecons625 https://wakelet.com/@choromysi106 https://wakelet.com/@eccredtelo206 https://wakelet.com/@unidtete845 https://wakelet.com/@linrocesex310 https://wakelet.com/@texcabocar448 https://wakelet.com/@unridastjo638 https://wakelet.com/@tibmoehotstran364 https://wakelet.com/@concachicent404 https://wakelet.com/@sufkensgerto68
kaitrav (Friday, 17 December 2021 12:23)
b19c06dac9 .https://wakelet.com/wake/fdm-54YaGKijoR0iGQCeC https://wakelet.com/wake/VWNZXAeIWzu-vhq4c6bEx https://wakelet.com/wake/pSwUyQ61u473IcdRgbFDo https://wakelet.com/wake/1-E0_44Go2-Ca43J2TL1J https://wakelet.com/wake/IalTUYqqEK6WZwCo4fIzS https://wakelet.com/wake/xpsekA1ALQe7lKnwkadC9 https://wakelet.com/wake/_zryiIPOxGwa_eHRiVmR3 https://wakelet.com/wake/d2u_ZYHsO9L98GU928-fS https://wakelet.com/wake/c8Syeywczm-u612MMmikz https://wakelet.com/wake/EW1L79vhYjpdbTdnhkML9 https://wakelet.com/wake/HeF4werockJ4P6AadN1CC https://wakelet.com/wake/exksO-Q9wRFbX3VMgnZsS https://wakelet.com/wake/C4PcclKwhAJ1V6fQgjOTI https://wakelet.com/wake/9SmMWEHk287LPFUpNhEHJ https://wakelet.com/wake/YCzcaUgb8C-NuHriajXT5 https://wakelet.com/wake/gsM1qvr5Dk53_GcajeDHm https://wakelet.com/wake/zfAkwTlsHv4yr9sZjXDET https://wakelet.com/wake/8NODudi9YvEgu4mg-JnxM https://wakelet.com/wake/gRVJKPBxilhfWvx4YxEUs https://wakelet.com/wake/5MFqNz6v3lVnp3sJpE_l4 https://wakelet.com/wake/VJhDy7Lm4UmBoamO7m8av https://wakelet.com/wake/FC5bSE_E1tVJ-19BlPaQs https://wakelet.com/wake/ALV3DDVAv3_RAkYI0e3bK https://wakelet.com/wake/IxbAlNcev0yfH28tfnkID https://wakelet.com/wake/qoQnXB58nDgOzJMkRsIBa https://wakelet.com/wake/wyfKAXOBbinNcHP8Hz76z https://wakelet.com/wake/XBU9MTt2gVx-sfUDJcWHM https://wakelet.com/wake/pDDOucflEkwP0uel7jIH7 https://wakelet.com/wake/cMvAqbr6B15ZaQiwubVAi https://wakelet.com/wake/oqzqUn3gfd9i8yYYMFYTA
valbeni (Friday, 17 December 2021 12:43)
b19c06dac9 .https://wakelet.com/wake/1FmmAGepPi8dqsWAmUxCC https://wakelet.com/wake/18d15g0BUyucCv_3EHJR6 https://wakelet.com/wake/U-TFR0tl_2p0lYri0l8Fe https://wakelet.com/wake/Lon0Zm_DMUMG24SyJ8V1l https://wakelet.com/wake/chxHCH6ftIrHpZCPBHPLh https://wakelet.com/wake/Uw1AKwRHcoKk67ZvTKVwO https://wakelet.com/wake/80dUL42bfgDAtLbafOFbF https://wakelet.com/wake/G_dpiDF2GGCEwhTDI7ZB2 https://wakelet.com/wake/gljZeDqJ6RNHOccXVi-K9 https://wakelet.com/wake/NPrKZaqd0Q1x6DFiYfOXM https://wakelet.com/wake/bTOXieAlOEcYUVJqAJ6Fc https://wakelet.com/wake/NN5ay7UQbo5LfPeSKVaSS https://wakelet.com/wake/oParEaaOsODUjJuM1boCQ https://wakelet.com/wake/2LCAN4w5qnCfXvi4AhK80 https://wakelet.com/wake/FWse9FWbwEkFKuuztiGtY https://wakelet.com/wake/mpdSiCsL21kbHfhqAGkXn https://wakelet.com/wake/L34eK_p8q9ztxcN4iVe-v https://wakelet.com/wake/V-5YgmNFE10RzYxL0VVQ1 https://wakelet.com/wake/njMoPJlbxJ80OX_JN8tZY https://wakelet.com/wake/VZurZqIQBdQj0VC2vJuVd https://wakelet.com/wake/_GnVgxnSimS8FlmbsCpKC https://wakelet.com/wake/txGWYv3sg5V8O-FfuWx80 https://wakelet.com/wake/heyP_gYN_KFye3O-kZqyt https://wakelet.com/wake/rVl3sxL9PGLe0ygkI6f90 https://wakelet.com/wake/-Ubg7skYPQ9kw8xxls2f0 https://wakelet.com/wake/BBG_NhyRgOtyTLlBhu3hW https://wakelet.com/wake/baRQCOLxr9nhJTAnS3rcV https://wakelet.com/wake/wcRuE00cXCXdODZppoSUH https://wakelet.com/wake/ND9kQ0fryEZQvu9jy6fey https://wakelet.com/wake/0kuLNqmgjzusziwXdGZVv
patdawan (Friday, 17 December 2021 12:44)
b19c06dac9 .https://wakelet.com/wake/4NPmqVpISF8feFSLr38gZ https://wakelet.com/wake/yCzQfVQct4xMwHPBJhsXP https://wakelet.com/wake/Q-uS5O8PHS7ZJpXgHOQck https://wakelet.com/wake/F3q1v0RofI4pNyVqJ3zhs https://wakelet.com/wake/g8HvqGnZzV4UUWxLj9s2y https://wakelet.com/wake/vjjJ7Zdvj7xaTsP0aToVM https://wakelet.com/wake/QkaA_ubUsT868SNrhhqOa https://wakelet.com/wake/5aPNxxqVzyk5Pcr-wXF7z https://wakelet.com/wake/LN7x-UxXB7X-BKx1YxUyA https://wakelet.com/wake/nZ88WdKLqZAC-HHXTzFLB https://wakelet.com/wake/sdnh4ZQrtK0_W-unN1tu7 https://wakelet.com/wake/Qndgow0_xWwSDdFh44kLM https://wakelet.com/wake/icb9gaxlZ7b-OGI-vgO2j https://wakelet.com/wake/Kt04XdQYJGy1bp3ThSn71 https://wakelet.com/wake/XWfqBnlukd2Rz9X0Cwzwv https://wakelet.com/wake/VvVn6hZJGdlQOOfoCpr78 https://wakelet.com/wake/uvR8T-2FLlpB6IAQ2B1wX https://wakelet.com/wake/hu763J6_HPN4tsWXD7Zzn https://wakelet.com/wake/p46Z8g8W43v2kSxUykKnA https://wakelet.com/wake/AmSKZpYAz5uyz4225KXH2 https://wakelet.com/wake/Hy5ZNcryBh-BDOoNJ1hEi https://wakelet.com/wake/EkhiaABh1fHXEMfS_f7s4 https://wakelet.com/wake/CAFFd2bF8KC8uDdz_RZh- https://wakelet.com/wake/WX5NPtDKNG2S7eesAHjNk https://wakelet.com/wake/e0dpgMTFbGBsLtUT-HtWh https://wakelet.com/wake/0UYNycu9p5Wo71EPBAEzg https://wakelet.com/wake/QfVdljISPZizSjcSgorM3 https://wakelet.com/wake/tKJ-sLUT1u4-H2OFbhgBE https://wakelet.com/wake/2Z9ZR8sNCmCmcpPA555Uy https://wakelet.com/wake/pvsfeni9M0Oem4xdt7jbQ
ladwall (Friday, 17 December 2021 13:42)
b19c06dac9 .https://wakelet.com/wake/pu6h2PQ2g6wQPy5DujN5I https://wakelet.com/wake/1wxNzx4tyzJ1jszBxdO7z https://wakelet.com/wake/c9-AHrkt277yAH7ANhkAq https://wakelet.com/wake/DAV5Yuir_QGtZEVrUpctm https://wakelet.com/wake/6xDE080E8nKfRQx_4INDO https://wakelet.com/wake/lANwhbg7NT8nRRupk77TM https://wakelet.com/wake/ckhTDqie867o7BaA3jphc https://wakelet.com/wake/haTTNYMS5FlwHIlCzuxkN https://wakelet.com/wake/UN-pwGGeVuHms3xMBgXBA https://wakelet.com/wake/lA8tkglV0_iwB-BgxjX15 https://wakelet.com/wake/F7epyEjo8BHtvE-qd6woq https://wakelet.com/wake/bUIDY0yx6IkxlplGQXw9V https://wakelet.com/wake/BI2-wmauNMztkOsrX4Wde https://wakelet.com/wake/iPsQVaanTNHq0amnO7-yv https://wakelet.com/wake/ezoohvxHzt9TeWASSQUt7 https://wakelet.com/wake/8fFypz3MfqePvldCuT6X7 https://wakelet.com/wake/cFIE9rQEIpLl7o-hFBjdD https://wakelet.com/wake/Y7f0mojEukm1ChSQHVIAY https://wakelet.com/wake/72pRaFTeiLqjGDlL5g3MI https://wakelet.com/wake/hyCXlqyTf4QrIVDJawLm1 https://wakelet.com/wake/sA7R_ha4PGsosrO_2VVSn https://wakelet.com/wake/_uwWt3hi5dtiJLf9vVQUY https://wakelet.com/wake/wQD7eS0Do3J5dDhqW9ukq https://wakelet.com/wake/jbFBZZgyrtxjpsb1sZHkW https://wakelet.com/wake/xE4Eo5IZTlUP9W5BFD0Dy https://wakelet.com/wake/7I_2jiG6qM4rDymnns5H3 https://wakelet.com/wake/hU1TB6QDDWTDQ18SXPB-b https://wakelet.com/wake/C_yqA1_hgEvpM2UoRydYq https://wakelet.com/wake/bjeuBDRmTlhEjT6wrGxc0 https://wakelet.com/wake/cMBK5b9NsNJooNQ2gTz6F
deleotyla (Friday, 17 December 2021 14:31)
b19c06dac9 .https://wakelet.com/wake/TL4VTYZXymWzvN5LWbqKp https://wakelet.com/wake/ae1cYOxgf4MBCUTdM4z3X https://wakelet.com/wake/gWa50eWtDgHN1Kpo_ehAA https://wakelet.com/wake/gOjV0LTvtxP6_5ehalBcw https://wakelet.com/wake/qgGSEEmT1r7oIp7CIh8Qj https://wakelet.com/wake/k3M8-4LRNUILfir9U0qCH https://wakelet.com/wake/Jb1aRHxwDrJ6kOaQ4tzNJ https://wakelet.com/wake/1soqd6GoAiN4gyMogyXep https://wakelet.com/wake/2ht9sXouzs8y3vncn111W https://wakelet.com/wake/2QbWGcGKfiIMAvDd4biwL https://wakelet.com/wake/BicX7OD9SNiBgVtmuSE5g https://wakelet.com/wake/ACjIyoRcAhMyjIawihHGM https://wakelet.com/wake/pHkUJ1KRGFnBINTdGf_9U https://wakelet.com/wake/HL5Y6p0gpVEfTxuG_CDb0 https://wakelet.com/wake/GJ_vdhRdGL4RlcdphVsdJ https://wakelet.com/wake/Rd7df0MRicANR47ZKZidg https://wakelet.com/wake/k38-ewaJY2sUMn-5OJY-i https://wakelet.com/wake/51HSbH8mL6xn5VrehSPf1 https://wakelet.com/wake/_s7twZhIJnipfEapruNoi https://wakelet.com/wake/v70wdnvddizpSwsYDRI7x https://wakelet.com/wake/VNAGEPjtYJVWiyWuHI3_3 https://wakelet.com/wake/9j_IgXIKyS5mbitEOsbDm https://wakelet.com/wake/Tnd_136kcw0HGOeuerodL https://wakelet.com/wake/NJKskrh64hItFz1I3iij- https://wakelet.com/wake/9av5Tv1vj-yrQGPDlzW0L https://wakelet.com/wake/SrYOtIPFawxJ9UWvdqk_3 https://wakelet.com/wake/AG_V8tMBve5rY8W3HnSjo https://wakelet.com/wake/xfjPOY1h3ItJbxtR2sXc8 https://wakelet.com/wake/faZmzmjNzE86-4b5a5J9s https://wakelet.com/wake/Xa12_eepVTQ934H6RuSmO
sahryvinit (Saturday, 18 December 2021 04:47)
d3509b5f6c .https://wakelet.com/wake/1z3QO-fPhCbMOGErTkRyR https://wakelet.com/wake/4WzMuPaopRY9qefL1osxB https://wakelet.com/wake/afulFKMz6NAGI1tzatZPN https://wakelet.com/wake/_jmOfIgT_XQaforSCWUaq https://wakelet.com/wake/vCnOCfyJ_bagXipU49x-v https://wakelet.com/wake/IUMT5-FWAGKuOLlFL1saW https://wakelet.com/wake/VVpsGsgaBZ666DsTBcGTi https://wakelet.com/wake/liRGcrdYiXEiMasDNTQwY https://wakelet.com/wake/ilRVz8yLQk-IsWClGdtlN https://wakelet.com/wake/g1EM171sMD7Pg7b00yN4l https://wakelet.com/wake/zU1lhjdNlqBzHFkIV0rY9 https://wakelet.com/wake/ggdtb5ByduteqprlKAQTd https://wakelet.com/wake/Bnp8fmRA-Txh_e6Pr2_4F https://wakelet.com/wake/R7AZRyBlbIUMlpH4TwvZO https://wakelet.com/wake/3-B1RCssd1XGqYoEyBPuJ https://wakelet.com/wake/lSdp6IjiOUYZgOoFSRC4u https://wakelet.com/wake/yN5rbog0cJ-e81XRV0qmP https://wakelet.com/wake/kMO8opEK9fugY7FQcAx0E https://wakelet.com/wake/1ZJQZErVaFccjN8RU1Zfu https://wakelet.com/wake/LzOePCs7G5lrCTLtw8HvS
harglenn (Saturday, 18 December 2021 04:50)
d3509b5f6c .https://wakelet.com/wake/7xB9TUVQEqgHDG5AE2O70 https://wakelet.com/wake/OmV7EEzTsY21PhoAW7gUi https://wakelet.com/wake/xq0jrH9s3VgLDxVulIqHU https://wakelet.com/wake/HgTmX6HoZuusqpnVs4BHx https://wakelet.com/wake/I4p78fnK1dO2gCI8f9YZp https://wakelet.com/wake/-r-boDGOQnUQ_HGdxy04a https://wakelet.com/wake/QmGhnfCjTxI775xfcaItd https://wakelet.com/wake/AzzAafHxsvEWmpzp0XNxm https://wakelet.com/wake/kIUPd6oBeU7h00ODllc4f https://wakelet.com/wake/neOOnW2-rLfiDAATdXsCk https://wakelet.com/wake/aAMBeo7revh6qoAhTZ1kG https://wakelet.com/wake/nlLvcTmKvNPLBvAXwv5VJ https://wakelet.com/wake/i9izrSUiI62p27yNkf9kN https://wakelet.com/wake/FdAr8lE78HE_UFusSbRm4 https://wakelet.com/wake/PhU6YhcMf0DRj3lNjzYtU https://wakelet.com/wake/QCrg1_ADgP0wTAtaQgTRJ https://wakelet.com/wake/9wGOaaun1PqaB937Q4hQN https://wakelet.com/wake/rpQ3nG-qneqbQpaIKTGIP https://wakelet.com/wake/22lehkmURSlaULSYOQE69 https://wakelet.com/wake/7ffZ17bl0BIL8G3jZhPnx
edvoni (Saturday, 18 December 2021 14:36)
867d4273bf . https://wakelet.com/wake/r-1Ti4chiYq2NbA1eUu7U https://wakelet.com/wake/n4WpNOREDuPcIzjHp3bCR https://wakelet.com/wake/U8lpajW2LIHNrK-_rbWaz https://wakelet.com/wake/VnmO4lDt2cT-_i2L4J_xS https://wakelet.com/wake/ojRrQfP10oBGclWXRVUBq https://wakelet.com/wake/LeUnEOuGp8cP_jawZlg1S https://wakelet.com/wake/-SAQHWuYAqQdo26CfwInx https://wakelet.com/wake/45bse1pg0Hk0VkyELjyTI https://wakelet.com/wake/EfgHBEyu6ZlNf59IrPpxc https://wakelet.com/wake/ooYJ-e6NmJIc8c9os62-O https://wakelet.com/wake/1vOFmFoOBq_jiYMQoWm4d https://wakelet.com/wake/61Zpnfxpa4FE2ORAxvF8t https://wakelet.com/wake/nw7ssPj8C90FyMMr5Mt3k https://wakelet.com/wake/vkgPXahgRRIeTY1kA3DW5 https://wakelet.com/wake/GmB_dY2dpbMkUdDvZjjU4 https://wakelet.com/wake/ijvCsa_7K3sft5AbKqD8x https://wakelet.com/wake/t_z3EDa7AkWGGoDWfBNH9 https://wakelet.com/wake/tO6-4iKb2QGVJfAyWLVVB https://wakelet.com/wake/52irJgXGcpOp4zA1ypdnJ https://wakelet.com/wake/eILEUISMcGf-ejUF5gfjf https://wakelet.com/wake/vkQigxd4PO_BhlJ7haRYh https://wakelet.com/wake/9D4XUW3nCUYhRjQthzEa7 https://wakelet.com/wake/U6ZkaQQsSRZiAvEvO-viz https://wakelet.com/wake/KPuB9ew9yKAj9PGFvoOav https://wakelet.com/wake/_NPWeWb3dH3vv-wgiBsmt https://wakelet.com/wake/jj_Yji29nt1TZ2yqkyBWd https://wakelet.com/wake/jJowIoPaNldnTCMgusEHe https://wakelet.com/wake/KM573cLg9umgqt9AW0As6 https://wakelet.com/wake/5ZbBUQFzchjK6UeCqh_nF https://wakelet.com/wake/qMCf1JqvnzBr-OPMPZIV7
queiwayl (Saturday, 18 December 2021 14:42)
867d4273bf . https://wakelet.com/wake/oshGpYyCqMzLO8jF2UQLj https://wakelet.com/wake/VVpsGsgaBZ666DsTBcGTi https://wakelet.com/wake/302HuDc6qS8mINVDQ4_MM https://wakelet.com/wake/lcOOC3sxmfcngyaruvn9f https://wakelet.com/wake/R01wabV0RSFFfbiK2kM1Q https://wakelet.com/wake/T8jrf6RmjdQOd3iEN2HyY https://wakelet.com/wake/ld8_DPiNwzaBmSHSloWwW https://wakelet.com/wake/9G1LMnOJAQWsMWq4vo0uV https://wakelet.com/wake/ondLgZHoKgm4it9yNbOCx https://wakelet.com/wake/MmOhTdB7arUFHhJhNA_xe https://wakelet.com/wake/8M-reRm6X3mRjXJr95GPN https://wakelet.com/wake/4jNMOAM32UfWvCKGZbOlw https://wakelet.com/wake/iAOCqo9rlT_SE9abZFwHW https://wakelet.com/wake/GO49WxWyzpB1GonCPzoR7 https://wakelet.com/wake/oOC1vMmZ5EbwZvPYp4MZH https://wakelet.com/wake/WJDzdZvoHxWPxm8YdC-kd https://wakelet.com/wake/knYNtf5lM5keo4RrFrD_o https://wakelet.com/wake/WN8ooRqwQ90ou8hSmWLBF https://wakelet.com/wake/tsNyxz6ZXMqA1YtLyVRXS https://wakelet.com/wake/KqTX6-OQPEvavbLU_khCo https://wakelet.com/wake/tP5jygdd0x48vjSbCdk63 https://wakelet.com/wake/R32NgjMCuumKbnmH03qkD https://wakelet.com/wake/cBgW_MtJzn7pa1UPC-OmO https://wakelet.com/wake/VGxnbo9E3BER2uhKBOzbX https://wakelet.com/wake/OZJyGYbnUK-x1h2MM5Ioc https://wakelet.com/wake/TX6x1r7J_cj5t7EqEBE3a https://wakelet.com/wake/bzju9Csb1E7JU8qtDDGZY https://wakelet.com/wake/LUrPkT28HOAc2cOixyJiR https://wakelet.com/wake/-CgQsMoUJn6NjuhPXcTJl https://wakelet.com/wake/p1Ltrd-oZ25YPlxXRptqH
silsajaci (Saturday, 18 December 2021 15:07)
867d4273bf . https://wakelet.com/wake/9HdGJc8rkgPB1Y5_oUhIT https://wakelet.com/wake/FWX22Hs7jihf0791jfpKK https://wakelet.com/wake/WUICYJrF0us5nFTYztS_F https://wakelet.com/wake/eiUlHeDZg4KTBY4t-RJe0 https://wakelet.com/wake/bZy7ssF3-XQQo2TiOTBhd https://wakelet.com/wake/M-KQjsfUV7Rf9-Jwnerc0 https://wakelet.com/wake/NjSduuGyiuH4FVk1ZlARW https://wakelet.com/wake/gGYOgDXkD926_dDB3QYeH https://wakelet.com/wake/5C6d1u111rpHM45N4dAZ8 https://wakelet.com/wake/HpjflLNjimpeBkAokGygX https://wakelet.com/wake/34of1PBPq0YH1YWmlFvwc https://wakelet.com/wake/mHCuH8wBNpbc0Qu6Ho1iQ https://wakelet.com/wake/0YG5cjS1H53PjleLD1OSQ https://wakelet.com/wake/oR1nr8Ly0CVsf1fGpXUdI https://wakelet.com/wake/yEezX-TiZxHgBuMwAe-Vj https://wakelet.com/wake/NP0MmgO6DqK9eFGcHWyqY https://wakelet.com/wake/VsYb-9gEmXuoipKLqc8Hh https://wakelet.com/wake/F2_MMYOiftmwcEmrwARaD https://wakelet.com/wake/m6HNrjihH0aUwo4p9k9qq https://wakelet.com/wake/O-NLyht4agS36lSljSfvT https://wakelet.com/wake/9Mly0G0lSsuccHsf7LBZF https://wakelet.com/wake/947OCTPNMhTQQTBLPBCzw https://wakelet.com/wake/p7J8y7X5wpGwW1s6Z3DJJ https://wakelet.com/wake/xZm8oCYJdx7aLKSs2bxCH https://wakelet.com/wake/zA5My-N8-9EFjMKHqdtqu https://wakelet.com/wake/zjB6h8XW6B1zpal1ZABd1 https://wakelet.com/wake/-wpsGbmCYGNBr7Tk-Df6V https://wakelet.com/wake/_iAYkDkRFx75u43STSNnq https://wakelet.com/wake/wFG6ZqZYW8s-PzcMrhw9s https://wakelet.com/wake/hm1KzW-W3ZcyqKHGHVe-l
frenedda (Saturday, 18 December 2021 17:56)
867d4273bf . https://wakelet.com/wake/YdQIjW6sYypEaoBTM10gD https://wakelet.com/wake/JS8j70WKpiYO8xTn-W5yi https://wakelet.com/wake/I19yb-6BrE2Llr1AvUp1x https://wakelet.com/wake/6SWlnI1n--DAAzM7nYvRA https://wakelet.com/wake/ilm74Q_xF0NQ__rZlx0hT https://wakelet.com/wake/nE1UTVnCksIxwIGtfPqOr https://wakelet.com/wake/dINU7uzNz4XTSpDS6ADNw https://wakelet.com/wake/zBB2pGQ4JX943pG7CKrVV https://wakelet.com/wake/d_pVpFshzrYB2_VNoR1ia https://wakelet.com/wake/bOJiOJGiGsCxqDRo2xs5D https://wakelet.com/wake/dH3SQ0Ld4TJ4PWNrfwFXq https://wakelet.com/wake/LYXHLHwvW0zuz367SZGCo https://wakelet.com/wake/cBTO0tdW2VFGx-gXtVcNb https://wakelet.com/wake/7BRjwHs9Vr8ttzPPZnk9f https://wakelet.com/wake/y2Oaz_n_QgpeEbh7olayc https://wakelet.com/wake/dx8g20JwyX_yfZYkoOEF_ https://wakelet.com/wake/1U32973xeA6K5gzieCK2s https://wakelet.com/wake/rcbD7QdFL2ai9-g3dQCEo https://wakelet.com/wake/bs1nclezxgasKnDQHh_eN https://wakelet.com/wake/emRbCIO2r0QkR3euClptX https://wakelet.com/wake/h1FB6wm8OZY_0oGRrX-YF https://wakelet.com/wake/VaT5tsUAr655__03ukpsj https://wakelet.com/wake/g8sLLw0IwFoAoUuJ5Gqbm https://wakelet.com/wake/BnrbAS_ktqa6t36fVZt5n https://wakelet.com/wake/q27cNgj4OQrmIWimA71cY https://wakelet.com/wake/NuZQFc1p6IAqORkwDSHxd https://wakelet.com/wake/wNfcgnwZ5HzKRYXipBS2i https://wakelet.com/wake/zRI5v8XOVurXEz4ht_dUI https://wakelet.com/wake/-BTxZlENG35dkg2_s-eWv https://wakelet.com/wake/AmZRsVy04qYXWUqHXSCwL
ilynei (Saturday, 18 December 2021 18:26)
867d4273bf . https://wakelet.com/wake/0_bXUIU5FtOKSUquvUAzz https://wakelet.com/wake/qbwhULbnAA8lQ7LDtiVu5 https://wakelet.com/wake/5JndpQFIfhf5CbGc3kdzP https://wakelet.com/wake/bAegWrNQP5IIVubYamAbI https://wakelet.com/wake/Ax-kXvdwjnyGIyeq0Vt2C https://wakelet.com/wake/dC7Kd-jEhKgw1YZxL9hQc https://wakelet.com/wake/v2eRw0biqJMVsm9Lpq2I- https://wakelet.com/wake/yg5WAtFIgS-KHvTBTxPLm https://wakelet.com/wake/SIibjvQ6RCZcOcVZSW9lw https://wakelet.com/wake/pdj8pqkBag8CffC8BNcEk https://wakelet.com/wake/_NcdNwogLlGPiwc9TU9bX https://wakelet.com/wake/tIL60en204pbv439KARWF https://wakelet.com/wake/LpIUypQFgw2abH1RBdIPt https://wakelet.com/wake/jbv4D86t12mcStSah5N4p https://wakelet.com/wake/5bjA7J6nedGLojJiAzpS0 https://wakelet.com/wake/qM96vVuY04RqCDJJZ-Two https://wakelet.com/wake/O0MlKATNZRp3KrrQQtrpX https://wakelet.com/wake/aFZj1UdhJ2StN9JLqTxhc https://wakelet.com/wake/SkHEowiwMWHZK2DM1BHRC https://wakelet.com/wake/v1actCafaF5dnimxP7X_n https://wakelet.com/wake/TtXBQZ9IP0EnpWY1JschJ https://wakelet.com/wake/FPJ4sgAkdN57uEajdyRWE https://wakelet.com/wake/EgjF-A3MMD1jy_0IGkOKN https://wakelet.com/wake/8_LD0fzIqZay1_FlaFo2w https://wakelet.com/wake/hSFd7mYEPvuDEOc04cbX_ https://wakelet.com/wake/Es8jmRU_jDdRm2wKvGVml https://wakelet.com/wake/ASBtk5ZublDQsk0qseAcx https://wakelet.com/wake/nZfMUreyqnpcKtpLc6V7J https://wakelet.com/wake/SgwjSbOkJp-fquBRSLxYr https://wakelet.com/wake/1NEX4lRTIlFF-BtApWv_G
owenwilbu (Saturday, 18 December 2021 19:21)
867d4273bf . https://wakelet.com/wake/WldCyiHjLq1XitsiL4Xqi https://wakelet.com/wake/-oQRJC6HB3Br1Y1Ltt_2U https://wakelet.com/wake/2n_jhijnetBtgrU3PCd7z https://wakelet.com/wake/SAISGv2p8NSDa8HiBueXv https://wakelet.com/wake/LrDhf0F-upNWCejx1EfSr https://wakelet.com/wake/lDZHuwNRvbkeO7RcuEO_p https://wakelet.com/wake/AfXIBeeU8bKE05v-g3NEz https://wakelet.com/wake/KYs4ELLyl3db_vIza7jP7 https://wakelet.com/wake/BztQSqnkhymREaRzGRUMG https://wakelet.com/wake/-F4CupSrCz3iUoFE1Z135 https://wakelet.com/wake/UaRPa7-h4mCuZkMPfi2tq https://wakelet.com/wake/hySZHYalRPeXSdEHZZzAx https://wakelet.com/wake/45dA35TmfhR5yANbONHHn https://wakelet.com/wake/SE0kAGtYDubXQi5V2vIGg https://wakelet.com/wake/z9R2lVSsVp1VZw2u016dT https://wakelet.com/wake/yWpGXQ9hZXIPHOINL3RFS https://wakelet.com/wake/01QPx7PXZ8wVwKS6L5XXT https://wakelet.com/wake/Y0sek-6nQfbTSsm-xKkij https://wakelet.com/wake/gC3OuDp8q3B6kfk2xA0Vq https://wakelet.com/wake/swZrgvUCFudrVeeizidF3 https://wakelet.com/wake/FGGL-Pf3cg8GVfmtpvDwR https://wakelet.com/wake/q-y0xGoEMketIFnYgb8l1 https://wakelet.com/wake/CRtekj-unyqEY9qA8XkNZ https://wakelet.com/wake/6u5eLNDLQgE43dwjjnCht https://wakelet.com/wake/NGeUXIzV2OIju1g3m6-ez https://wakelet.com/wake/kWnvD3UChUfl3B-pPFpN2 https://wakelet.com/wake/249m4JILVl1qlXc5-BzhE https://wakelet.com/wake/FAYLzE0Ae2A76_aNiL_1b https://wakelet.com/wake/ngIz6UmZ_IVEoQyBxjc20 https://wakelet.com/wake/rk9QfTS-ie05miNQWqch1
owenwilbu (Saturday, 18 December 2021 19:32)
867d4273bf . https://wakelet.com/wake/soTdEjtqIVjK8L_6KqipP https://wakelet.com/wake/bBH76lOu1t9Z5Fdmsj1EN https://wakelet.com/wake/SZOzVyFP-A68m4ayW_Fxx https://wakelet.com/wake/1ijT0tUgIhn_mSIFBjJAO https://wakelet.com/wake/FnDrl17g4fQUrqXE1VNfp https://wakelet.com/wake/YMb4s3PS2siOr-D8MDyC6 https://wakelet.com/wake/eqq6pcmxVS3swB8nK8gek https://wakelet.com/wake/6oPKKvwf3oOpGcuR1_oBW https://wakelet.com/wake/u-1U-9o8g3tz_7TdwMG6W https://wakelet.com/wake/iNDfhJ7DsONUhKPScOecE https://wakelet.com/wake/Az-6-LDD_dfviaigHUuBv https://wakelet.com/wake/2JPAJEe2K0yoK2C3kgFvN https://wakelet.com/wake/Am6bLeDafLLh6lPIsZT7v https://wakelet.com/wake/5_ujS6CklDtME9EWgeVge https://wakelet.com/wake/z3MiJKuRM99whte9KU6Sq https://wakelet.com/wake/PNkVKpQ00bTkLaXUjhTwW https://wakelet.com/wake/AMKb65EAhgy7L3AHZttWm https://wakelet.com/wake/466qePepFDE7-wZJ7EOzR https://wakelet.com/wake/CBsmYNerQORRvb9AUASzh https://wakelet.com/wake/ydmt7JGyNEcwy_K_RbQZk https://wakelet.com/wake/JADtC1F5Tp2WXPaUCzUnd https://wakelet.com/wake/6dtqnB72o6QEoMrnKWSwj https://wakelet.com/wake/ORa9TpfIMDsfo9Dt5YM5y https://wakelet.com/wake/g856nKHNZQkt2Dr_o2ZWJ https://wakelet.com/wake/8amhDgB7SNHmry_JWUIsC https://wakelet.com/wake/4sJJQBUQRcXXFa-o79N39 https://wakelet.com/wake/MDX8y10ZYHZxFb_NT9LXO https://wakelet.com/wake/DeqpLm7RVIrBPq-tgf9tH https://wakelet.com/wake/Nuo-2gR7ylBie8Ucb15rn https://wakelet.com/wake/Pcb8zjI7247mb36PU39pO
wenddesti (Saturday, 18 December 2021 19:51)
867d4273bf . https://wakelet.com/wake/BXTVA50mQJrZscXEBQSRM https://wakelet.com/wake/dLaQQjWzZWZR3pAWTvtRU https://wakelet.com/wake/y4mhgHnr7GqUQKknuRKwT https://wakelet.com/wake/i39uc6XFYgmLYLMsAgZRC https://wakelet.com/wake/JOGa4u3VtuAroTQR_TS6a https://wakelet.com/wake/4fknt_BfvJ9u0DYWvDpDC https://wakelet.com/wake/vtTo_hsKVjy1QmzjfpPlQ https://wakelet.com/wake/P_H-NxsT3Cz6ABjCBbKVc https://wakelet.com/wake/vx_AraAaeIg-MUc-mrt09 https://wakelet.com/wake/MV_IOzgC5EYhADHXXb0Fb https://wakelet.com/wake/C8aKdA2qEspBgWPAHvhYz https://wakelet.com/wake/ZTpm_03q3tBR6ELz-elxL https://wakelet.com/wake/F2R3Ui_cxNRXvion3bgVx https://wakelet.com/wake/vPCXud7cdLw5Qr03m2wRB https://wakelet.com/wake/MdBLwng-s1a6aAZaYo_mj https://wakelet.com/wake/ENA2oy3qJFUnuKtPG0MDT https://wakelet.com/wake/HRTPd0DUgSZg2F9-rUcnc https://wakelet.com/wake/qBYdECDhH62BKfo8VpJLD https://wakelet.com/wake/dve3DuVRx8aUdSivDalF_ https://wakelet.com/wake/a2CocDVHkoE6VQc7nNg8L https://wakelet.com/wake/dWExbLBvM4nRb2-AKSL7N https://wakelet.com/wake/uWmnpKsUBVo_mKQE7T-dT https://wakelet.com/wake/31SmxU3GgQKZRVLQRfR0g https://wakelet.com/wake/xeqPoEIIs0i3389-9NId9 https://wakelet.com/wake/FTLp1abTlYRX-doid_5bk https://wakelet.com/wake/bG7jJc1qFjLDsFSh1Jgiz https://wakelet.com/wake/UvnfoKrJJWve8GMj71SIs https://wakelet.com/wake/4wQZpqgLmwwNvS8IhujJ0 https://wakelet.com/wake/aOAb4js9E12zE2IeaGEaN https://wakelet.com/wake/ZaKxPykav3ioYCwVcWGf3
innorand (Saturday, 18 December 2021 20:21)
867d4273bf . https://wakelet.com/wake/S1INuXw7UAnmn49G6Kule https://wakelet.com/wake/bHVLrL3h0fCCvJeKT-lmM https://wakelet.com/wake/IH1RN4xCMFAMGQIVe_qI3 https://wakelet.com/wake/y0ygNEs8scZ1kZ9uH6S-5 https://wakelet.com/wake/AgXkfayjCoU3JJtn6JxSy https://wakelet.com/wake/Y9g9Zzj66cwWU8dCWzQ32 https://wakelet.com/wake/ZXytYjGp4lDze_i5nEIbD https://wakelet.com/wake/1axKZMWXeonmH0lHGkd3F https://wakelet.com/wake/XzXmxK8RknG7NoUnIu4Rw https://wakelet.com/wake/85S9g9gjysNQuvGteyNcn https://wakelet.com/wake/iCYxNR-0vUjZrOa0af9V4 https://wakelet.com/wake/9840SAw4QNpPyB1243yHl https://wakelet.com/wake/IpSnWcsgZqg32V6xIBPZx https://wakelet.com/wake/h_iRUOsGlrDZhcL_Fbb6g https://wakelet.com/wake/Czx1KChWFIfE5fAq9Z8DF https://wakelet.com/wake/U_YX5iRI6ZyaDSf1wbXm4 https://wakelet.com/wake/onuf-S9gkAuIKfG1TnAsL https://wakelet.com/wake/lcNbTpO8T4DpoFITPvOBo https://wakelet.com/wake/JYRkStuWEzNvSfKQiBAUj https://wakelet.com/wake/VkyoL0V2KJ2soPKBYpZM6 https://wakelet.com/wake/B6c4EonX3zcyJbhNZOx3x https://wakelet.com/wake/CgBrf0GvCD-jDeHTI4KnU https://wakelet.com/wake/NLNZi2CfgwGHekcN7lOrP https://wakelet.com/wake/TxK8QQ239r9BePnRzauOW https://wakelet.com/wake/o0KUidlXMqhSquKT3Fuem https://wakelet.com/wake/QlgSDog2bzKBF0by-Mwga https://wakelet.com/wake/zoN4ZB8zJYYWPhqKO62z3 https://wakelet.com/wake/ITSbhzGb_seLVCo7NPYJb https://wakelet.com/wake/kVEoFRLtCxyJtvY_FKg3p https://wakelet.com/wake/rjS024AZ6ltdvS2ORr0kT
halyathal (Saturday, 18 December 2021 20:36)
867d4273bf . https://wakelet.com/wake/RHMad5y2ci6Ps0aaL_CLV https://wakelet.com/wake/o3KK_yK7RQ1ZLjKagFysx https://wakelet.com/wake/-mJdefq_A3uSOs_aJIqmh https://wakelet.com/wake/Dc04lIDZUqWTCspzYimQG https://wakelet.com/wake/iG50FT8aNGjCcPUAm9t86 https://wakelet.com/wake/cwD-qsTye4FPI_LUilFmd https://wakelet.com/wake/OrXpnyv3mI-Y7KLROyAA3 https://wakelet.com/wake/4KkyYrtT_Ejt_wKLq4C0o https://wakelet.com/wake/g8_7PSqoUrdR4Wp6TL96U https://wakelet.com/wake/ieA0czQZOCJdksr3OY4Kl https://wakelet.com/wake/e9JI_S4eKF8vpNpsvvOhd https://wakelet.com/wake/2huuvDrc4Tgdk8BNq1OCz https://wakelet.com/wake/tLak5M3G1cHKSB4-QO0dR https://wakelet.com/wake/3hytqY_xCVDlr0PsVcfJJ https://wakelet.com/wake/sBQgpsvr5a614ofaW3N3Z https://wakelet.com/wake/dDRyizwFEOcsgvvXKAfbj https://wakelet.com/wake/aX7sxZizd3sNa5ZWD84NC https://wakelet.com/wake/-GOZHa6JgkxDRv70hFH3T https://wakelet.com/wake/KGTdKEkSDuYpgNeu1OZ82 https://wakelet.com/wake/-h6ujkP4pNmlPUb0rtxwv https://wakelet.com/wake/mkVaHVse5kLBWTSYgfhGl https://wakelet.com/wake/p4Ai6sFyvJKS-ii1tCdwh https://wakelet.com/wake/ZRKLbLAqjAH64syx5c-Yy https://wakelet.com/wake/diOIghccFX7GfoAh1KIE1 https://wakelet.com/wake/G5igavPp4NNq2EkOD7l77 https://wakelet.com/wake/STOmpl_-P2xvQvO6ySExw https://wakelet.com/wake/YcIBJU7ma8G8IcgbeWkKL https://wakelet.com/wake/1nZ6Fn7GbxhYH_2nuAPlf https://wakelet.com/wake/_o_sjlIcBkq0ZgtA74CKF https://wakelet.com/wake/ePWxpv2hlRI0bc327Gg0k
eleschu (Saturday, 18 December 2021 20:39)
867d4273bf . https://wakelet.com/wake/IbqukFk31VF6RYAntJUHf https://wakelet.com/wake/svkK9ESiA8RdSQg4wt-uk https://wakelet.com/wake/lCyX2caTkfjZ5ckRVp_Gb https://wakelet.com/wake/-pwbXyUxFelrUM0tZc4h8 https://wakelet.com/wake/nn4NX90s3Nic3z33SFE3S https://wakelet.com/wake/Ni8_8YmZcDOCz2dZouSKM https://wakelet.com/wake/ExXy7dJJVjkyMkH6S32mO https://wakelet.com/wake/gqYfJvaqNp3HoSmZBmm8G https://wakelet.com/wake/SmBVbD4p0uCn4bTHkZ_7- https://wakelet.com/wake/GpJ8sA2LYZcFzt6N6dg5p https://wakelet.com/wake/wyO3Jj5eP1W8yI8FwR7OB https://wakelet.com/wake/NqIoQVUNMnhv_tn0OG4QN https://wakelet.com/wake/HtP-lbUcTBgdUDBY5VeFY https://wakelet.com/wake/KRVNW1A6loNYeEFVKjOXU https://wakelet.com/wake/ZSL8herPN6CT7HuEUlJe- https://wakelet.com/wake/pgCSsUi4PPsE_4JqY14Ns https://wakelet.com/wake/HkdxlNNbfTDgNsE5rP7cu https://wakelet.com/wake/HZMsFpfyjjgLYKzUQ5x6D https://wakelet.com/wake/LTKe0l2Ab4UMWVuGnG9qh https://wakelet.com/wake/dNVQOMDQDK_ACnXYTmM8x https://wakelet.com/wake/AIRv2RP1GOkb9GB-HrSqL https://wakelet.com/wake/eAYlKTOKR7k4Ew9s-tnyW https://wakelet.com/wake/SzH39qcUF2NYG2cztCWzb https://wakelet.com/wake/5LEIO51DLtHuN3vAoTfip https://wakelet.com/wake/JJpu5C-k4vdcQSMKquLI1 https://wakelet.com/wake/6hDeu-RzfMCw-1to-jzEB https://wakelet.com/wake/A8BJS-DhEP8Z6owXdSmHO https://wakelet.com/wake/kL-90DGSGk9qR9HhnvIGu https://wakelet.com/wake/6mEOeSRRt8-V99PACBIf1 https://wakelet.com/wake/d32MXRgYsnPysDESPJ49a
eleschu (Saturday, 18 December 2021 20:51)
867d4273bf . https://wakelet.com/wake/XkL7MRROSVplq1g6C0kD- https://wakelet.com/wake/lMzAjkIPoGajzFJ6pN8uV https://wakelet.com/wake/l7I5xnDvlziaVvs9NDsFJ https://wakelet.com/wake/aupKzcjVfhHPqalTLxlat https://wakelet.com/wake/rnGTfNYujsDa-lyEwtLtM https://wakelet.com/wake/ZGe2NSuoNV8N47SsYhoz4 https://wakelet.com/wake/CnIBaq8PB3O3U-avbS7EJ https://wakelet.com/wake/GePyjxpHY5S9dcb1KaBHU https://wakelet.com/wake/zzCP0vDMTe4IvLm2-WSVb https://wakelet.com/wake/EjJw1qVqrR4b2Yd_ZMTqX https://wakelet.com/wake/Q60ld9rBu6yKnOlsUsWEK https://wakelet.com/wake/LoM4I7d5o0O0UP-1jPUDy https://wakelet.com/wake/sVnTHDWyZsGUmShtaB36E https://wakelet.com/wake/4J8uj90yLqG3PaTYUjhfj https://wakelet.com/wake/3cV2-Yi-xrq7nO5BgIP4r https://wakelet.com/wake/HzJrvTt-uWbOfUqbHoEwR https://wakelet.com/wake/cwoyfASlSdFPl3ohVIaMj https://wakelet.com/wake/nX-GalY0aCDeWYRAx6Y6S https://wakelet.com/wake/E48DXQAhz131Y-sOVVVNz https://wakelet.com/wake/oUp2ihHbANNuolwej3Cih https://wakelet.com/wake/X3t0mErayVU_5BfRJ1Cap https://wakelet.com/wake/39d-MIFCxOBKbVvzf5K5U https://wakelet.com/wake/XCOK_6oURg0EjEJs1cRwp https://wakelet.com/wake/rKTX1fT6m-C5S1Cdop8Ha https://wakelet.com/wake/Rf3kEXJafpV74pCJAbFba https://wakelet.com/wake/J815GtUF5NTWwqg8dmV0H https://wakelet.com/wake/cwhMHdmb-aiZkHjcp_a7e https://wakelet.com/wake/1vidbYp1xWYLVpF5V3teH https://wakelet.com/wake/_0N_0ZxQeFAUQ6-srpIUo https://wakelet.com/wake/K_OCAN7HxwQsK8JBQq8Pg
gilrsing (Monday, 20 December 2021 17:41)
8e46ae4c21 . https://wakelet.com/wake/dC4Lthasyr2nAMgLD7aPG https://wakelet.com/wake/gef4cEwdfDojsyMGdy3vJ https://wakelet.com/wake/O5fVtChGL0B8abhkcP8kE https://wakelet.com/wake/JEoUvuFYTBYuGSmx7yzlB https://wakelet.com/wake/rhuXr0yS70oR_FdHA8MiN https://wakelet.com/wake/t1p0dr9_uh_nZzPElABZv https://wakelet.com/wake/Dox8ju9Ul_2HkB0SDJ3il https://wakelet.com/wake/VjlmgEohtXEEb2NJlhpYy https://wakelet.com/wake/lV12hskzKYgeeic1kUokZ https://wakelet.com/wake/G7k4OYrSC0VXKw9OOt-kr https://wakelet.com/wake/j6eu8AcvXvY-72BRI1RfW https://wakelet.com/wake/XQOmkFw1cWybeNFjC6cL2 https://wakelet.com/wake/1lIAsHuP1JcgD1KD8Pjrg https://wakelet.com/wake/028bathSvYOAgxbvIhjWw https://wakelet.com/wake/STJSUzoT-p4EJooJMNMIt https://wakelet.com/wake/dIdJCZp5BGMKnxkZ-jc2r https://wakelet.com/wake/n8z9Isz7U2YXh-FcLdrlM https://wakelet.com/wake/-Y1jBrT_m7ZwUwfReW_C2 https://wakelet.com/wake/DFhic6_D-8fhYg6kIt7xg https://wakelet.com/wake/VgduW-SEHN4n2HkPF1qXS https://wakelet.com/wake/s_6q3mXrYSJrtaJsEw7Xg https://wakelet.com/wake/gy8cQkhbk57PtUuQaTDFt https://wakelet.com/wake/rX1icCcy--VKUT9xd96M- https://wakelet.com/wake/EeXOXIfiMPcENs14KxVb8 https://wakelet.com/wake/FmGXAtUXpM6sFXrG75frn https://wakelet.com/wake/Ou4-woj08R6XX2TIRpEoG https://wakelet.com/wake/uuq2Kj4wHXERRR3Sg2C-h https://wakelet.com/wake/yl6QVTXUIZg_qAAQRkM-G https://wakelet.com/wake/EdyGNP3jTaiRsMwE06D4b https://wakelet.com/wake/CS9EcTVJW1o0L4eNtvpgB
fennai (Monday, 20 December 2021 20:42)
8e46ae4c21 . https://wakelet.com/wake/4f2YceFIWLzRpJreQu5kE https://wakelet.com/wake/F0QO8WqwUs4A3kUwy4q3c https://wakelet.com/wake/aeWYCFPAjIf9GAd6THb3m https://wakelet.com/wake/00-Yfj9rZZ9ylXDbjskrX https://wakelet.com/wake/lpcj2WpXrdtdwtqW_S9D7 https://wakelet.com/wake/dKVOdsjY2MUxQJdpycmGn https://wakelet.com/wake/D0u2xvfhHxh9-pkUlMr3Z https://wakelet.com/wake/vVr8rQvUfR6hxcwGYTfTZ https://wakelet.com/wake/regotLkhpS8B3GzAou9lj https://wakelet.com/wake/9nlyt2NrcedYfqXoXaTWN https://wakelet.com/wake/_2XdISyM7d0SqYPwGLd5P https://wakelet.com/wake/3yeQ_6oYBxsoNruzBTv1t https://wakelet.com/wake/0kIGzhShlodXHCimDhc1A https://wakelet.com/wake/J4vCQ9aAqcQXvfe4aXS-e https://wakelet.com/wake/livzzDbsUtZLMWAULGFe1 https://wakelet.com/wake/srCbcLzSg9_8aCZFkg7FG https://wakelet.com/wake/FQT6vVj3mOVIf-kZfV79S https://wakelet.com/wake/gsliCyuXsax27QtwU8uIj https://wakelet.com/wake/Lx7x_5wH9EagXr_cgn4RN https://wakelet.com/wake/y7qLgqXVKuLeuAmzruO-9 https://wakelet.com/wake/lAX7G0smcOn4yAS02rdHf https://wakelet.com/wake/xCtaIRtT0pmgK3y512YhH https://wakelet.com/wake/d1Bc6qCBGtwnIe9wWe4pn https://wakelet.com/wake/e74s4PWirQCUpaEvJPZJ5 https://wakelet.com/wake/Cnip8DTJifUMtexWnVwqz https://wakelet.com/wake/bW0qYQq1s5duAS6iAIlF0 https://wakelet.com/wake/SqOAFdb78puHxlEcZZ_jw https://wakelet.com/wake/HRVlbkrWtDFIcH62dlPeo https://wakelet.com/wake/2X_-D9nMCzKBFfyXHKhnj https://wakelet.com/wake/jGo5etRYSwovY1yP4f2Vm
bibman (Monday, 20 December 2021 20:46)
8e46ae4c21 . https://wakelet.com/wake/b2tIzzzOCGShvhy1dV5uS https://wakelet.com/wake/A2vnS7g32l_Kgyu67dZsm https://wakelet.com/wake/YDgKvPVnPnXnAW6SpJ0Kh https://wakelet.com/wake/-0gzLc4CaYPSgTIPIhHQZ https://wakelet.com/wake/SEfqxv3T2JI1PccWugxQL https://wakelet.com/wake/BVFWZDSuqtGDf2SnchoFv https://wakelet.com/wake/ATSUxKZsI8DahhZvhKRFo https://wakelet.com/wake/DCTaY-OoWIwiCwE2HIqAR https://wakelet.com/wake/cLBPI0D_hGvxroEQJX88j https://wakelet.com/wake/OUrsC5M-ffPojZaLOBT6e https://wakelet.com/wake/0JkolGbWDtURs4qkBbo1a https://wakelet.com/wake/ljXfcgfI8tR8FlUVs4zNh https://wakelet.com/wake/5Opr8_HPGXFUDfUDmoLHW https://wakelet.com/wake/Ju7hBYjXbP1Qzffnd8Gt5 https://wakelet.com/wake/3lNPjRJmR4cHJwJW6nN6h https://wakelet.com/wake/pP_P-LDplzvxpgd612tJl https://wakelet.com/wake/XiNIESdRI3EcocLCJdK_2 https://wakelet.com/wake/O3g_rSZIZGWizgSKqemy5 https://wakelet.com/wake/q4-OiCF7IFj5qI_iIalTY https://wakelet.com/wake/MCgM2mfOcte-M7ISOLxsV https://wakelet.com/wake/bz6pJ9unpbruqOR2tToek https://wakelet.com/wake/63F_LCUg6Tnz0lXoViCJ9 https://wakelet.com/wake/U0hOUmupe5X2pekA0iXkf https://wakelet.com/wake/LPqqYYfK4DvMOpbQT32mM https://wakelet.com/wake/qwsUMTx2Ekhh2_dsUG56P https://wakelet.com/wake/0FjRSw-9p67jmuRrGSfzz https://wakelet.com/wake/dS-lqSQlIH_foxXgHa8Nu https://wakelet.com/wake/o4nLpT_G5wut3dxmdID47 https://wakelet.com/wake/isxJIbun9h6qL0SWNqfEk https://wakelet.com/wake/8gkFp0_TvtdlkYtHMeUAR
caland (Monday, 20 December 2021 20:54)
8e46ae4c21 . https://wakelet.com/wake/ynIhAeZklWFwMq5kay_qq https://wakelet.com/wake/PoCaTd2Ee__xQSM656FCx https://wakelet.com/wake/vqmIusNqa_dk80HUPgL-o https://wakelet.com/wake/XnhiT3jSeTqaHyWGU15U0 https://wakelet.com/wake/WJbsQdEeEgH0Tlmv7ntAo https://wakelet.com/wake/-F8ZHe8jKW9Ye9_C81BQ0 https://wakelet.com/wake/Ovq_r36BS68N8QK-QBgo4 https://wakelet.com/wake/raVKm5j7NssT8TGWiQbVT https://wakelet.com/wake/XO4-owY8cZ22caUVuoP1C https://wakelet.com/wake/QWb1zb32nZJMty7P5eiBS https://wakelet.com/wake/r4YgEn8EyxzSM6XcTNPZH https://wakelet.com/wake/KxNDeAw2TT34HJjf5nKiS https://wakelet.com/wake/65DENUdNmwk6mTjQxemqI https://wakelet.com/wake/Rwu3G3WpDvB63g9BSbpaN https://wakelet.com/wake/_dagjp9WYl_4AsnS1KGNL https://wakelet.com/wake/5BWDwhlLcN4nSbt8rFtZq https://wakelet.com/wake/NDcZ0S81lhQ7EzEighWJ9 https://wakelet.com/wake/FPrPrmEyKajhmONedRO9T https://wakelet.com/wake/jNBrS1zF4HoydpLiI89S5 https://wakelet.com/wake/0ZCtLVuDfX0qbnxlTvgZo https://wakelet.com/wake/tR2PGrXO1DEE8WL0FiU1y https://wakelet.com/wake/-Agqrud-UMxCYJuRMLgFe https://wakelet.com/wake/sijoWsq6rpmdffmT8j4qW https://wakelet.com/wake/7fIAQPZyISQ0FndgB3-QZ https://wakelet.com/wake/x8jTuOGfnxacmeyM97lVG https://wakelet.com/wake/-weYtr8dJcClbdRw1p_rQ https://wakelet.com/wake/c8dXbgIlIwsv36GpF0uxl https://wakelet.com/wake/xitQZ1bzasPpAewvTA3AG https://wakelet.com/wake/8MOZYA2rvQU01t8CMcVj0 https://wakelet.com/wake/lvxDxn3uW7CEck2TTqzcf
gracjam (Monday, 20 December 2021 21:02)
8e46ae4c21 . https://wakelet.com/wake/rHrdSYaDbD5VNr9du0My5 https://wakelet.com/wake/_47fR9JmSbM6YCOZEk6Ep https://wakelet.com/wake/3-XbHaMF8YHWimnUF7qjz https://wakelet.com/wake/f6DjjLUHT-HKTCSHxDDzZ https://wakelet.com/wake/Y9n7JZ24V8Mc2jY_v_8kF https://wakelet.com/wake/wjXzcy5G9o7Pnx-f29phQ https://wakelet.com/wake/DoDgDsNgMIO5qqgzdlpVX https://wakelet.com/wake/cnj7ihuwBborwEIjebqyE https://wakelet.com/wake/kSowFGMr5p0kZ6XIe2qma https://wakelet.com/wake/YL0kjJ1POdciJ9LbMW4kW https://wakelet.com/wake/7pPF9-jqtmKoP7GO6s-ME https://wakelet.com/wake/ZPG-beRflk4oJ3GsE22j4 https://wakelet.com/wake/yNDxuyxLU5GsnPE2XwXy9 https://wakelet.com/wake/_6DbQRTmWutJ_H5km4Xzm https://wakelet.com/wake/I9jYs7NUzQBshTwPDgnu_ https://wakelet.com/wake/GqXyoI0XuneXdviUiZ9Rd https://wakelet.com/wake/9F7QL07axniJechoaQNYY https://wakelet.com/wake/hDPePZrFSjLveFx4wfykY https://wakelet.com/wake/M0TjK2A5rrHoD5cKsibYv https://wakelet.com/wake/u8CFJnuKdeR_S1FWX50di https://wakelet.com/wake/-3Ma3Wgi0XMwV6kbb_hXr https://wakelet.com/wake/QDnacARFnM3L9hpNjgOwa https://wakelet.com/wake/KHQhsScGuGpa1jxqNCsyg https://wakelet.com/wake/AFYPx2GKvbE563NO78OYg https://wakelet.com/wake/c5YzbLGJF54R46BBD6TYV https://wakelet.com/wake/2mC54Onw2mSm5visXW8VP https://wakelet.com/wake/_2tgjju0-gJrf9gGWFiiJ https://wakelet.com/wake/L_B6kqc5wJUFCYsqk09n7 https://wakelet.com/wake/ZHbCLGqQ7J0CPHO4Yqc5Z https://wakelet.com/wake/21I3rs-c7SwCuCDzhT1V6
davoveet (Monday, 20 December 2021 21:06)
8e46ae4c21 . https://wakelet.com/wake/vmgyfV2YB-xuEIKrkwUo2 https://wakelet.com/wake/fyi4W20IVICLvAnRq_uiW https://wakelet.com/wake/RNjwOaf06VnWxRPTmCEgT https://wakelet.com/wake/xEMvb6thjBVRTAg6IuRhN https://wakelet.com/wake/t-sX0vvQgkNsto9yd_-hi https://wakelet.com/wake/EYQ2CfmctCyiDvV7lFDSN https://wakelet.com/wake/OwcGyjAhRLZVbyNR1V-f6 https://wakelet.com/wake/GZoUNGYG4bcQVLhkhE_Xs https://wakelet.com/wake/lcETcoxVs3nLjA3TIirw0 https://wakelet.com/wake/h_8UChSxOHNY1D9nmtbLF https://wakelet.com/wake/X6NENqNAUnU30UehDlbNe https://wakelet.com/wake/fTK_S93QMIU9t19T1255G https://wakelet.com/wake/M2rOv-C_C1Zpi7jZeYDxH https://wakelet.com/wake/00shofD72CTw6Pd6GBQ_c https://wakelet.com/wake/nx22eL_KEeTPyYRrPdZdF https://wakelet.com/wake/kG_JXmm-H3tYO6E9dbI57 https://wakelet.com/wake/1xXWj7B-SyGfv2sgIRLbJ https://wakelet.com/wake/VFV5DQN2VIXIUDW9JpdSd https://wakelet.com/wake/g7SAtqQvW22I7cj_6mZX6 https://wakelet.com/wake/lCruXMcgWVE3-hAVVge87 https://wakelet.com/wake/sLD_bUXeNmf3d7KwchrWv https://wakelet.com/wake/Sp66DQYl4jh1foS7GARL2 https://wakelet.com/wake/yDnpwDMWAfPJaY84ynPNS https://wakelet.com/wake/QLaLTw2K72fwIWOgb7K1V https://wakelet.com/wake/E4DVZkvvQZNDy-hkTDGzX https://wakelet.com/wake/lAL5W7Gwt6KVw1ikHZ7dH https://wakelet.com/wake/SMs7But-Q5GHUNX9Jib1f https://wakelet.com/wake/2Zp1qMylnqreEToUwN0W8 https://wakelet.com/wake/34J6aJUCEtC0pKObyvOuL https://wakelet.com/wake/Ri0RzljkTFsVNaG_dyGEj
chudorit (Monday, 20 December 2021 21:15)
8e46ae4c21 . https://wakelet.com/wake/UV5Hz0cqah2LCBfxt2Ly5 https://wakelet.com/wake/QBV2FsALRLG1w7p66mn70 https://wakelet.com/wake/gn85xNua7wJAT6kybM3DN https://wakelet.com/wake/ZXqXtTXlIhNa5HD_Tr648 https://wakelet.com/wake/12-FA4rwT4WpM7BiGz265 https://wakelet.com/wake/mPDsgzwjWpNLd2YYrO1Ln https://wakelet.com/wake/zSlWHr4LZvp7y0yBzwYpE https://wakelet.com/wake/Ap3kszj6RJynHJZll1qFg https://wakelet.com/wake/6JPnbXpLyTmDMr7Ufgn5B https://wakelet.com/wake/PFU13yb9WmN2hia5ECAJv https://wakelet.com/wake/Mg1yMRQks4DaYyFSHBN4w https://wakelet.com/wake/OKUPonNclQpkpqNJEyi_Z https://wakelet.com/wake/0QITICibGvnvKw8eqePBQ https://wakelet.com/wake/PpJUS_SyD1jSSgp87lYm_ https://wakelet.com/wake/YHV3bnPapVgTRp4M1FmbA https://wakelet.com/wake/A7Kv7L0_r147-LyAAf1Pq https://wakelet.com/wake/TQSjzbqVrM9ajZARx-EFo https://wakelet.com/wake/HcM_8kVt5IeoogEEq00jC https://wakelet.com/wake/qKDeNj2aBAz0RXZnRGF2T https://wakelet.com/wake/tKzFFhRDnrbdUnMh-VFf1 https://wakelet.com/wake/hKiTVnELJZCoQgfy9aFj- https://wakelet.com/wake/ZWro0FqMTHVXm55yL9YjJ https://wakelet.com/wake/5EJIVTUlvzez-yGNcHocU https://wakelet.com/wake/vAis-22rECSRwYm5PkbAW https://wakelet.com/wake/cIpmH72ypNaq1iF6HwLnz https://wakelet.com/wake/8jVnXAiWM-fYu8VDfTJoS https://wakelet.com/wake/JB_-d2NnLqDE0k4OcIyFu https://wakelet.com/wake/dOPh92bycPxdJF6dt5zdy https://wakelet.com/wake/5GebzU5fuHpazPpT7ayFg https://wakelet.com/wake/0uoLNDX1sD5lJxKwq8JCf
sadyrhay (Monday, 20 December 2021 21:24)
8e46ae4c21 . https://wakelet.com/wake/1UP5JtUJ70mDTY-hX1n6A https://wakelet.com/wake/NAW7EKbapKTOiotwSHzjY https://wakelet.com/wake/JesD6VISR9OPoauC4iMDd https://wakelet.com/wake/TQqC7wd9F7VfYSDLCjZ0s https://wakelet.com/wake/oHB4QzRv1rCUItYRYCbkN https://wakelet.com/wake/wUoJgwpzi9LB_8WEU4o8O https://wakelet.com/wake/Gb3vHj7kBYScqGEiSQITZ https://wakelet.com/wake/MKXc2-4iw6Glo7bhJGDcJ https://wakelet.com/wake/qVHb2uekwrPA5kgWZjMae https://wakelet.com/wake/TwrxwT7N5mPuLSJ76MNC- https://wakelet.com/wake/UgSG6z2iManRoyMqV0-dW https://wakelet.com/wake/PnVxmu6WR2pDwDiJkzP7a https://wakelet.com/wake/M8eVncYKtY9fa41xWAwRK https://wakelet.com/wake/9sLqnEStX89LccL20smRg https://wakelet.com/wake/6_taxgvbF_YCbK-ruHEM5 https://wakelet.com/wake/901GKMGWJ3fLm_tAxX4pY https://wakelet.com/wake/Q-LLCchMZVzBYpH-VaFo1 https://wakelet.com/wake/USNH4RRHB8dyLgiAaDoIe https://wakelet.com/wake/6rCRzxsShkbWUkAiXN_0V https://wakelet.com/wake/XecMG4hNtzSIHvl8noezt https://wakelet.com/wake/2y-YBgLMCf8uGyhCQmkVD https://wakelet.com/wake/lyIliSVszelqriy_SeMGY https://wakelet.com/wake/6tg384d-G8y7BOKKB4wVx https://wakelet.com/wake/jpiEEqLDNJthtTw6VvkU_ https://wakelet.com/wake/Lixo3wCnMycvur8FUH3Nc https://wakelet.com/wake/na2LNiQvARcLOfwFoWXtT https://wakelet.com/wake/hprMubsEFeF9TiFj7BcQJ https://wakelet.com/wake/G2nNZFixzFRqMruu2Tl5U https://wakelet.com/wake/pwRqcb1SMWDj8MYrM2Mqk https://wakelet.com/wake/JJsKTzoLjuvlJ9HXgePGs
salotter (Tuesday, 21 December 2021 16:58)
6001825f8f . https://wakelet.com/wake/qA74ss1yAHltj_E8ITvku https://wakelet.com/wake/Xmmm_03WTzYgu30h1gdK2 https://wakelet.com/wake/dghwBYFkmOJsWzqNjOC2l https://wakelet.com/wake/YvGlXSIKMJ3wpHSHUHZN8 https://wakelet.com/wake/Gmi2p6ZanolnAzgc0NYpH https://wakelet.com/wake/QI0UyK2g9BbBqIo1YZdNc https://wakelet.com/wake/8f2uGJJGZr-kN69oMpuO0 https://wakelet.com/wake/mvTii-JriMA57NQ6Royuo https://wakelet.com/wake/XotftAnsMje8CaPzn7gJc https://wakelet.com/wake/tH0C2uO6lN55DT8vHsIdo https://wakelet.com/wake/kCMFAGduXyWPJYoV1_dqN https://wakelet.com/wake/C_61ZKm9EAMiRL72qgunv https://wakelet.com/wake/tJLL8ML-urf9Dh7zdv9e_ https://wakelet.com/wake/b5OROVp91aFFZ9wYG7ZYZ https://wakelet.com/wake/gTFtwJxhj4ODgL190vJux https://wakelet.com/wake/Vrv9DnaX7xwYlpkosE4Ks https://wakelet.com/wake/G2ccj7DW-Ka3AQx7qAlMn https://wakelet.com/wake/DvOfqg_Y6coSzk9wFdrPW https://wakelet.com/wake/bkJ-IeyZSDDPoBafFDpxP https://wakelet.com/wake/hfa-fIuSlb_9GiceWefqQ https://wakelet.com/wake/Cuxd6KmyhjPaB9j9_9XHY https://wakelet.com/wake/QR-oP2y1zP8m_I0fYzqN6 https://wakelet.com/wake/Vv5Hpm1LDBnVIAJH3SnqJ https://wakelet.com/wake/7LEfYI8OBgCkduKpToJQL https://wakelet.com/wake/QFgDFW-q42O_KqM2XR0s_ https://wakelet.com/wake/b3rKYVcEnNVBlNuTLnt6W https://wakelet.com/wake/9bx3ny3NPR33osrMvjuJT https://wakelet.com/wake/YY_LetthzK6qEwVo47x95 https://wakelet.com/wake/qZM18jcmxZpAYOn7T0p3t https://wakelet.com/wake/dSn6MWMz0dzE17f_4tp6C
kalanatai (Tuesday, 21 December 2021 17:00)
6001825f8f . https://wakelet.com/wake/Abe3V0oDOmfBxquxYLLdh https://wakelet.com/wake/Pcf3CO7bWWiHv5Q4SoJhC https://wakelet.com/wake/tQgT812G0-Ud5VSVJpVft https://wakelet.com/wake/w-AEnxRJe3xnB4WtgUKK6 https://wakelet.com/wake/VPpMOPJIFbipKx6M-AnB9 https://wakelet.com/wake/rXSwFBmp8RQWGLGOSuiMT https://wakelet.com/wake/AZaMXi3FOXZ9ycfWfJSZE https://wakelet.com/wake/-vQK6pePGFM-CEnNzAQ8G https://wakelet.com/wake/g2aknt9rmGDLT_8wsgI-F https://wakelet.com/wake/e0LII3ZHYjqq0jbHJyDfj https://wakelet.com/wake/s4DjwOUoYl6T4UbxLQ_Xa https://wakelet.com/wake/ZQAo6go6WyIkbDOFJdm-R https://wakelet.com/wake/xaRfE8Kpih2ytjYdtAFUk https://wakelet.com/wake/CY2b1otwdwG1xc_Pom6YY https://wakelet.com/wake/1iQPgXY52YtLM53dcwmgU https://wakelet.com/wake/yJsjcbL1BBMNjnCGtC-2K https://wakelet.com/wake/7ZjZXUqHoz8IX5VX5iSkz https://wakelet.com/wake/Ih9R9mVdXWrxqdmuLcNwN https://wakelet.com/wake/BgZ4FSCrafeZKpAom5lRE https://wakelet.com/wake/TDm47LxBamQboDPVblGe_ https://wakelet.com/wake/hHhfozND7qImICMgo2dP_ https://wakelet.com/wake/vg0Alhmm9e1Nz0xCWSjGC https://wakelet.com/wake/jzsbrxM3n8N17YHADgCeS https://wakelet.com/wake/VTbsztCAx7zQDpgPes_Qh https://wakelet.com/wake/nFXB2WNGA9bUp-uuXSmg0 https://wakelet.com/wake/CxcByXCEBORLPrO-ULzA5 https://wakelet.com/wake/8qwH6tgN-KRLhafAF_vjO https://wakelet.com/wake/U6NfARRieCY3NNUbmCOq8 https://wakelet.com/wake/y57u4X5rG_P9rTsTUs7UC https://wakelet.com/wake/KrotI2C7QyTNFWCLZZUkH
chajayde (Tuesday, 21 December 2021 18:21)
6001825f8f . https://wakelet.com/wake/zvBaqLdjt4DKLIlvXBkqe https://wakelet.com/wake/pGXaHLytSOhXIh7-F4oLM https://wakelet.com/wake/LTQd0bIFUUMGjH1WRw-KB https://wakelet.com/wake/vUQSigEBVvt4BrupUoccl https://wakelet.com/wake/-S-MoOHlEbTVqtFygLZou https://wakelet.com/wake/7lYlQcYV9X4zccWOzOYgh https://wakelet.com/wake/DRB_TQRX3BdBxYgDj_CXN https://wakelet.com/wake/sOUpPDf2oGRkJrCwIeVzb https://wakelet.com/wake/G2cWn3ghlar1QaQs4uLGa https://wakelet.com/wake/KoZqQnB6KSZkzWCxiv2cA https://wakelet.com/wake/QgOPhJZWED6D9Q-WuDLun https://wakelet.com/wake/kbQDrNNmOc97sW1VqLcDb https://wakelet.com/wake/KCtRkCKbbKae3w6M7PpFM https://wakelet.com/wake/oy075SQpH_9QMVm6EsKlb https://wakelet.com/wake/radYaC8iD6uQn5Z0mju9V https://wakelet.com/wake/TkYyq39olQd3YX_-o9wau https://wakelet.com/wake/kDh0N6s2HPEcYhdNBE7iq https://wakelet.com/wake/r22VYm7kD3dKfN2XdGbZm https://wakelet.com/wake/lK90ZzYx-mny2fxuygEu4 https://wakelet.com/wake/uaxKbNoU6i_NfdPRyKZho https://wakelet.com/wake/cNt2P65TAQo2BiIFWHhe9 https://wakelet.com/wake/DQvh4PW4I8lIkb9rTQdBH https://wakelet.com/wake/apS18xV09eOqVjVRaiL4s https://wakelet.com/wake/FiNXN-gc9Ro5sum8lyOUJ https://wakelet.com/wake/bweoeOuwhVsJbW3HvWu4D https://wakelet.com/wake/I8CW5RVAFQoz7eTcNZow5 https://wakelet.com/wake/WJz5YHboNmMibPNp93Cjo https://wakelet.com/wake/sL02aoaCR4uQQhLnVE1Py https://wakelet.com/wake/HLG4oGZdQbinXxFVpR8aK https://wakelet.com/wake/j8rTdN-RzHycAv3To9PVw
orrjurg (Tuesday, 21 December 2021 18:26)
6001825f8f . https://wakelet.com/wake/mZBhgwqxGkEjgEQMxaPZZ https://wakelet.com/wake/b5d0C0EyL_LF8O2xw9haE https://wakelet.com/wake/Nl3UBtXOADfeINcYsdSRK https://wakelet.com/wake/XR9aPxRulQNP4_eUQ7XaU https://wakelet.com/wake/bd76PMK8dbxsMbNrJfEY2 https://wakelet.com/wake/5xbyhPcX5U9ZU8SjkK_wy https://wakelet.com/wake/XRC46wdjAxXqKqecFzXjF https://wakelet.com/wake/5qTae5OM307lnghcbw8B_ https://wakelet.com/wake/eiv78NDDLWR1EnElYc1hP https://wakelet.com/wake/WlkLJPlxMRAcKWR-WkPj5 https://wakelet.com/wake/B6szgXIv6qwqYbR-VM9oH https://wakelet.com/wake/wDJY2qBWo50Yxzzp74Ix6 https://wakelet.com/wake/7DlQnNPII5nuLTvck8TUf https://wakelet.com/wake/3NOSlP3a5nb5a0hx-4eSb https://wakelet.com/wake/SXMb3vHIWVJ1EoNk_2bjW https://wakelet.com/wake/jH4Jw3oaZZsdWbfQv9hmX https://wakelet.com/wake/oe0wG-QESElvp-7_7xH7G https://wakelet.com/wake/EYXUvLMF2hMDyIYunSWno https://wakelet.com/wake/0CKsi-zlISSn7U4E79WyF https://wakelet.com/wake/UOUaebYk0zXH0xn33CiZr https://wakelet.com/wake/t8DKaJzDOXbYmrn7O7Qtt https://wakelet.com/wake/TsK75dFMEi0etXlPLvt3X https://wakelet.com/wake/J07BOUjC7G7RkceOLAbP0 https://wakelet.com/wake/pC8Frf_t9NytMUSJFHgok https://wakelet.com/wake/GKLlNA-5V3_fUG3M845P2 https://wakelet.com/wake/EeMeo_GUbx8Cwg-yPk8ar https://wakelet.com/wake/59fPl0Ij2TAYcFqqqxjw7 https://wakelet.com/wake/NLsofLd5iE2EBKUlaspYJ https://wakelet.com/wake/lQW7MFVaNmeUWqvlpX2Mf https://wakelet.com/wake/Qs38CdoHGh1gsCdBsZlH0
mykeljam (Tuesday, 21 December 2021 18:44)
6001825f8f . https://wakelet.com/wake/wsbhsK-i4A2wjGPmC09d3 https://wakelet.com/wake/FUQ6fqfpFuEthFOOq1T4g https://wakelet.com/wake/r_KlqhKuIL-ofkQKbNpJM https://wakelet.com/wake/K1kQuB4a4BgOvQnZNEzYr https://wakelet.com/wake/J1EgLCP8aqBt25CC_vVhV https://wakelet.com/wake/f1DlCHfzI-33RwnKiLWX8 https://wakelet.com/wake/6vh6FcSKungO4UowJl1hD https://wakelet.com/wake/7O1l54cDxnsqDp4i3-3_P https://wakelet.com/wake/oeGSrD1B92vElCa8CrBKs https://wakelet.com/wake/YFfQYJN7dE98jY4jDQvAG https://wakelet.com/wake/w79yG6YSBR0He1SbNwiHH https://wakelet.com/wake/Sg1d9Z98gJFmcGzaMcweh https://wakelet.com/wake/BAyOETwL4QbrUUY7Jrtp1 https://wakelet.com/wake/j7CJqmsPvXyco7fg9qwHp https://wakelet.com/wake/krml1J8cFpKgWHA7vbBeU https://wakelet.com/wake/07K9FVVx2At093FPJQN-i https://wakelet.com/wake/gQ8szGxvoEJvkwVeYtzFO https://wakelet.com/wake/nOV_H_ZP114YOCV8F51MC https://wakelet.com/wake/JC9AoTGMU85fb2CRVZzcs https://wakelet.com/wake/iZoP5kwsvsPJCFhCqfkDR https://wakelet.com/wake/hh7kB43BVDEzx_xk7FaoF https://wakelet.com/wake/-5xTKf8yn1XjbiXwcLDO8 https://wakelet.com/wake/U-7ADjOVp0hiq-tn2bdaY https://wakelet.com/wake/LgLW8Q0RWZDHp9YrlxKrR https://wakelet.com/wake/uqELGuZIksZIW66vvzKZH https://wakelet.com/wake/VCcqQGC_SwEQUtTjbgVAj https://wakelet.com/wake/GopgoxIcFb-vH_7aLV6Q7 https://wakelet.com/wake/4WjtC0XxvAjXnhu0nj0u1 https://wakelet.com/wake/B4J8mF5gfnIod6X0k4ULT https://wakelet.com/wake/DxQPnBl_DwqPJbo-sRolD
hayzfinba (Tuesday, 21 December 2021 19:27)
6001825f8f . https://wakelet.com/wake/I9V1gZ5r6zBeKYs0zoisi https://wakelet.com/wake/xoh__hDgMlG2Sg7tli3f1 https://wakelet.com/wake/vcb-4c7Ba7Z2WvDLRz_qP https://wakelet.com/wake/Vj3Tlt7OwfahdEJ_zcToR https://wakelet.com/wake/MG3q_F4vlHpJMNuilFbuO https://wakelet.com/wake/Jy1BUScXkAJ3_LktlSiQN https://wakelet.com/wake/_zgxF86-Ozmo_cBMtxYJY https://wakelet.com/wake/qWMUloP1T4ktAIjHwoB0i https://wakelet.com/wake/tlC_oGgh0qoVskim8qcNG https://wakelet.com/wake/-q8r4sWiJyxOALkASlgY7 https://wakelet.com/wake/YUFgdHSktJr4yQtTrl0QH https://wakelet.com/wake/qCfmz8-3muZayrs98yrDb https://wakelet.com/wake/a-7j-0pf-P47K6USW9tbc https://wakelet.com/wake/C-d9MVf-0OpjN2ISbfLdx https://wakelet.com/wake/izSYLctFIDqvg-UUVPjhA https://wakelet.com/wake/Zii2BvBHgj6pLaAAXXXE6 https://wakelet.com/wake/VuchDmK8RdrZAD3CBYh72 https://wakelet.com/wake/nz8wmFk8KZr59kq9xVlRo https://wakelet.com/wake/pAQugvfJEfN6QiWr2SeUO https://wakelet.com/wake/NoTqY3YIHGxM1HubkL5dI https://wakelet.com/wake/1lv-XRO5-K8RW4pk2dj7R https://wakelet.com/wake/H5xo-VFcX5cokqD91Z2bn https://wakelet.com/wake/Yjp87IQQZ0xLqgLilL5UH https://wakelet.com/wake/apTo_vuREzENedWbV35Xu https://wakelet.com/wake/Qr02yKlSnbSBLLPCpKz5F https://wakelet.com/wake/KnvSqLRjEF3K2pB64sUBk https://wakelet.com/wake/XSA2gfctbTZButsqJvV2G https://wakelet.com/wake/fuBEECjtDRo-1Xqvw8huz https://wakelet.com/wake/Ozo5ZxgJSTaWbmorqBV6k https://wakelet.com/wake/Pd1OnP7CM4Q_9JONxa65m
dafncar (Tuesday, 21 December 2021 19:27)
6001825f8f . https://wakelet.com/wake/KYg7zE8o-kJrz61oaOcQE https://wakelet.com/wake/25P_V3p92ey48PfbT9Vkz https://wakelet.com/wake/rfnnlg9Yx4y6OJ6bc6GuW https://wakelet.com/wake/K3E8ljpJVdyIzagK78zCA https://wakelet.com/wake/QXXukv1lPukSsb1D17TPB https://wakelet.com/wake/tazm-G3CLV2PiE1OU9x-t https://wakelet.com/wake/TkIDuANAC2830n08DExLg https://wakelet.com/wake/rafMAAer0kWEH9xGJGGpG https://wakelet.com/wake/3ao0y9kU6x7O-4HwhGOG- https://wakelet.com/wake/NVD_V8YdrwPj6zkTqQpbQ https://wakelet.com/wake/Ib81_HN19xuuXpsrdDB_R https://wakelet.com/wake/8TlU4xA9YxupNGRV71d1J https://wakelet.com/wake/vGLoPKB_IDPUm1kgF6AU4 https://wakelet.com/wake/_GvlY7_vE-zjXyJIxICCn https://wakelet.com/wake/qj6aRAhGPzWU0kXcVTlWK https://wakelet.com/wake/KFhUVRa_T4LbW84bv82v9 https://wakelet.com/wake/0_M5rXmIOBFXY2F_TM-uc https://wakelet.com/wake/-BRzCYoplQ4NKwhuxsKVk https://wakelet.com/wake/xgv1YEwlxywEL7o_8dwi8 https://wakelet.com/wake/A3_K3Gm0qDiAWcRgSyNVk https://wakelet.com/wake/MQXQWsjbFEuA27BF3e7mt https://wakelet.com/wake/zKB-4hTuhMpN8EV--Ufjg https://wakelet.com/wake/-fDaPykBZqMsiYo6DOEd4 https://wakelet.com/wake/HU4aiuG3p1WZMQWfzClVO https://wakelet.com/wake/pbfq0UpGGi3_OCTVz8VZw https://wakelet.com/wake/C3MxITmya7yxDioPPd9SH https://wakelet.com/wake/2G0PUe_oedXXn0N-9FdWC https://wakelet.com/wake/yjqePtK33wVHWJG9sgsJ4 https://wakelet.com/wake/uTYmegWJKRYi9BhWQfqmI https://wakelet.com/wake/FSSN8n1RBvMNbebrctLB-
peongill (Tuesday, 21 December 2021 19:33)
6001825f8f . https://wakelet.com/wake/fbeF0vl7b2OulusrM91fd https://wakelet.com/wake/N0qu7eITmhLojm4lMwwPG https://wakelet.com/wake/vxrQxtishm8ADbWKnczKI https://wakelet.com/wake/kW7--BmtUlQCGsvDMyOCR https://wakelet.com/wake/ITCFzcjJhGly2gk5qNmPF https://wakelet.com/wake/qsMfdpvhiC8yuQirkZfnm https://wakelet.com/wake/eUARrTqJWf7Hx0w3PJ1e2 https://wakelet.com/wake/otuapvH33GfXYykf4Klp5 https://wakelet.com/wake/QSmRlWN5t5Gzdz3Mccdh6 https://wakelet.com/wake/MgNY6hZXsnj9Ioc8AWi0U https://wakelet.com/wake/B4CC1tNyCl9CzVCoQMphl https://wakelet.com/wake/NnrXV99dKMvoKlcVbxA83 https://wakelet.com/wake/wVXHccsemTiEvaH_M4FFA https://wakelet.com/wake/mwztcwhWu8Di2c_xNCGOv https://wakelet.com/wake/pofcFbiJIadc9kSVaLu8u https://wakelet.com/wake/CzXKjlujnziRi7HIoOCQz https://wakelet.com/wake/rHqbFmS9lda24gOdAAHPC https://wakelet.com/wake/As2quGPniibAb7VH4_31G https://wakelet.com/wake/T7xHzwze-hOmvzylXcjDm https://wakelet.com/wake/_vQaCOKGPVBTg_Zf-garC https://wakelet.com/wake/K-E1le_nnK_C4Cttl-C-H https://wakelet.com/wake/NHK1TDJVtUKSHh4RIJgZk https://wakelet.com/wake/6nx9xmZSJmd5gL0nNpwSh https://wakelet.com/wake/4WcgCDDs5WaP-UFCTGsl1 https://wakelet.com/wake/38q_5HUOPxhCes7v0NpYC https://wakelet.com/wake/qVAYia3DUnURTXcsJdoUh https://wakelet.com/wake/LMsT1BnaI1kB76W8XYlko https://wakelet.com/wake/LUoNO25fHfrCaE7EW0qml https://wakelet.com/wake/GY4z-wHt2d8Tcbj48lcGG https://wakelet.com/wake/WqgFCJ9t1AkBFgjSWRTDx
grantlovi (Wednesday, 22 December 2021 17:03)
0ecef09eb3 . https://wakelet.com/wake/K_kH3o7AmzYe5MkNa5Uki https://wakelet.com/wake/l5hnZNxLxuSEalk6faIwO https://wakelet.com/wake/8hBemn7C4lk_wQaOXK2CU https://wakelet.com/wake/MXvRqmt_ORkSPZWKxQCz3 https://wakelet.com/wake/TgiIVwNxhJoy8boZdnSwv https://wakelet.com/wake/RXKZGeUAZH9PmEv5LfZQp https://wakelet.com/wake/oDOsM4J19eIMgHwCKQQJs https://wakelet.com/wake/sLD_bUXeNmf3d7KwchrWv https://wakelet.com/wake/dT4ZhZII9sspk7w0MrEQP https://wakelet.com/wake/-aUs70wiFa_5KMS8U1r0n https://wakelet.com/wake/T4JdGNeEFI4abojyphUhq https://wakelet.com/wake/VjcAQodNk-uwXfeEbbapr https://wakelet.com/wake/MyOn7YssaL_Eh7u6LaJ0G https://wakelet.com/wake/NNMOLKCOpSLdiEjK_mw17 https://wakelet.com/wake/AciqEVApUhDwPNHLY7qbv https://wakelet.com/wake/YLUl1ROPuhbEfmcSIxvhh https://wakelet.com/wake/HrFW36HQx-AavaW-02Bym https://wakelet.com/wake/FmxFQLUWa2mQTYl88QH_k https://wakelet.com/wake/5w8RkUcOGc3Gwr1A1M9Xz https://wakelet.com/wake/by-en3YuPM1VjotaNjhyK https://wakelet.com/wake/8v0vg1djoWJQt7N746Heb https://wakelet.com/wake/NDmhv7fCkOoNP5kBAFU3D https://wakelet.com/wake/iBTAnY7fbt_YyEMrUzCOx https://wakelet.com/wake/VKet2AZFQLeWQzo6wYJyz https://wakelet.com/wake/ZRm7IwfZ9lfDhNc53gMOW https://wakelet.com/wake/fTTtuScbmnKiZXJ2xDXxQ https://wakelet.com/wake/pCa_IiWupGga_e7nAZBKc https://wakelet.com/wake/13nhLmzC3g5hZhaKC4LO7 https://wakelet.com/wake/zMJuFUsTxOgBb1geVbxRo https://wakelet.com/wake/3BdrBRnPmo89yJ0cA5byq
gayeormon (Wednesday, 22 December 2021 20:18)
0ecef09eb3 . https://wakelet.com/wake/6CvW4exZtRlaK0mDO8D3n https://wakelet.com/wake/lK5DmpFj4g7_Eo17-hmOF https://wakelet.com/wake/d0GRdi6aG0PEIDpPpom6o https://wakelet.com/wake/g3C1eLGC7ihLdwNDFl26x https://wakelet.com/wake/3dG9c9JFQdLv7nZBurisU https://wakelet.com/wake/uz4yQRyov0FrfkDMsFV8G https://wakelet.com/wake/ZL2BTbaOO2KMtkOL_HjKb https://wakelet.com/wake/tiiclEuUOYGfbpGYtkshb https://wakelet.com/wake/L0EgodUN1TCDbzSLVWywR https://wakelet.com/wake/U_SkU4HKJS7gZGDiDTg9T https://wakelet.com/wake/_K8h3sl_rr6hUyNHPFEHX https://wakelet.com/wake/5cn_cDuOfQiHXhEgHaIV6 https://wakelet.com/wake/8rCwxuA3km24GAElpvuEn https://wakelet.com/wake/P5XGHCTgiBf0YISiiB6we https://wakelet.com/wake/caJ0MDNuxUqFPpa5ubipg https://wakelet.com/wake/6LJw64Puh9FnrOyTOSAm1 https://wakelet.com/wake/1yoZUZF735dYR7TNc1pLe https://wakelet.com/wake/khh0VxcdfTZpTrit9Rd3L https://wakelet.com/wake/-yOqvA2U4fGwNsVfXGZbz https://wakelet.com/wake/RmXOFov_2S52bUsfU4IKm https://wakelet.com/wake/RB1-RWYDFGotP-zR-XXCL https://wakelet.com/wake/yOLNmaDsGQnKVDqPvs9xH https://wakelet.com/wake/fTZj_hPJAq9hxM9u41En2 https://wakelet.com/wake/Er6OxDYoC4iShQPBTCx20 https://wakelet.com/wake/C4oNaHKAVQ-zF-DSdzHli https://wakelet.com/wake/SMJLdCOAU8S0zF1YKmYIH https://wakelet.com/wake/kSH_w4rs2Tut_-k9qaoL- https://wakelet.com/wake/uOlHXfBX1t-lzIOsnPXwW https://wakelet.com/wake/4yF9MkMCQch9lHUm3OYHy https://wakelet.com/wake/woWa9tuAKQi3EWauswhd7
ulapati (Wednesday, 22 December 2021 20:45)
0ecef09eb3 . https://wakelet.com/wake/lZCokN1IGulhy8iPMbfpl https://wakelet.com/wake/q3M3B1HqQqVPnBg9_hPMf https://wakelet.com/wake/Jlh24hW0EaZ77ekg74cS6 https://wakelet.com/wake/YMJGgGl9bZgZ1DNwcc4I4 https://wakelet.com/wake/vzLCfzr2O4N2fc_s4QeUh https://wakelet.com/wake/23RiJL-bXivR0tHWkRQjV https://wakelet.com/wake/zv05IZO_fTLHR9aTFCKsc https://wakelet.com/wake/V9QKLxWUymC4ZwD41zuKY https://wakelet.com/wake/XrvQkdjTaE65LaBeAcl0V https://wakelet.com/wake/BE5oEsFdYGD0CmxBU6ZXw https://wakelet.com/wake/qvrFvIFyTbSWhNnk24Zh_ https://wakelet.com/wake/HIUrSs6Ik7lL99ZuFgi_N https://wakelet.com/wake/IXsc1cplv2-Y0rnyAqiMu https://wakelet.com/wake/3hHC2OM5LIq2CheyU0-Jn https://wakelet.com/wake/crspJp3p1DgDJzwDAJ_qD https://wakelet.com/wake/0OerGTp-XnA9nhQk8m7DP https://wakelet.com/wake/V3OYAFj0l9OCLRYzcs8DK https://wakelet.com/wake/Grz2LFCD23l4HQwYN9UIy https://wakelet.com/wake/WObC-DsllttctyOm_azul https://wakelet.com/wake/LOi1FhYlMEj8nTNSvJrW8 https://wakelet.com/wake/WcGnJlsanzgxG-nZXufFn https://wakelet.com/wake/ziC7jECHDvuuXVDJjimHP https://wakelet.com/wake/i02JbygVMbAP3rt6wv2i7 https://wakelet.com/wake/unRr6ldbCoglNHnBUm-tc https://wakelet.com/wake/1ruL4DwPTNXW8yNNAhNtT https://wakelet.com/wake/huIgO0OeeMAKLctf14Fv2 https://wakelet.com/wake/KKioG6n0QTT7ylAWvh9AD https://wakelet.com/wake/AeYdspjKU_4nX-OGNweOm https://wakelet.com/wake/7pKQROJ0yyzApaCzcFPP- https://wakelet.com/wake/GNGmbe3vC5r6Vj5tjkxkJ
giacjamei (Wednesday, 22 December 2021 21:08)
0ecef09eb3 . https://wakelet.com/wake/Vsb6leB0QGoInre1YCm6t https://wakelet.com/wake/kaM7GB03KC7n0uI2dcRCY https://wakelet.com/wake/BIiDP-b8-0HrQJiDKysRl https://wakelet.com/wake/-vg2ABiVMlxuD6jy_CcF8 https://wakelet.com/wake/UaRAKhTD5HPT3-cQbZrS9 https://wakelet.com/wake/Ws7Pw_KRLU93l67egYcVR https://wakelet.com/wake/GdlBkAMb9_ITVmOZ2MYc7 https://wakelet.com/wake/Yg8JppOsb5MwI6-t9eEBS https://wakelet.com/wake/2bw6yvTjhqXs6_IXWyJkM https://wakelet.com/wake/t_fmoMRz8pM8N7uaPLaCi https://wakelet.com/wake/cSiyfuXLYGtWQXSrVbHy4 https://wakelet.com/wake/Z1-ItrJC88ysMV_A-YATB https://wakelet.com/wake/_mNsuQqs4WRx7YnDQJKhs https://wakelet.com/wake/QTVNgNzxvIVxtfYWw7rGZ https://wakelet.com/wake/ySNAEJnT3Fd6Bj08gQNjG https://wakelet.com/wake/dtsUfV3rJ6Wi4AP-gQ7Sq https://wakelet.com/wake/00hOrTfv3dlkKKxY-ijR- https://wakelet.com/wake/vwkdK8yRn99cBFA5ZOpPE https://wakelet.com/wake/ROAWuSIlXAvbXugAtWHUI https://wakelet.com/wake/KGQgjKLErJsT4VE-Jv5hy https://wakelet.com/wake/QF871KvjV_5eWfg4mIC4_ https://wakelet.com/wake/41PERvhrsMg5upWnUBF3s https://wakelet.com/wake/PPjoyI0RgjWzNkDOc1PsY https://wakelet.com/wake/GnG-ZcTs1wTENEuF8VOWt https://wakelet.com/wake/nqe6QADF4M9s4w8HF3RWI https://wakelet.com/wake/Z_rPu8twwC-EJSH80y_II https://wakelet.com/wake/5HEYIfz4yOJYvk0AZ48PM https://wakelet.com/wake/xfU2amjyAL9UlxvXnzIGa https://wakelet.com/wake/h7E2LYZXnDZ49_QilAQfh https://wakelet.com/wake/Zy68kySy-Q8G5prNeqJ7V
flannaus (Wednesday, 22 December 2021 21:33)
0ecef09eb3 . https://wakelet.com/wake/qiezgnlJCFazMu6nxokjA https://wakelet.com/wake/LEn1QvAp8V7WZAdXrkEn_ https://wakelet.com/wake/QVQKmtgB6I2q07UcTGtjA https://wakelet.com/wake/ZzBK0Ln1amQgV10EVUVFY https://wakelet.com/wake/tQ_MCC-10M00NppK_jyYz https://wakelet.com/wake/LYm5QS5stjbfoHT0cPVwq https://wakelet.com/wake/elWa9n4AviP-wILDAGOrc https://wakelet.com/wake/2meAMIs8TUlfR1zPc5tOH https://wakelet.com/wake/sXqE-YSrPainbfWgj4TXg https://wakelet.com/wake/yQKl14U-DeOL0J_b_ZSxz https://wakelet.com/wake/5fRQXvVTF63pVafPcEpOH https://wakelet.com/wake/gcJCeN9sUtXCWLLJZdF_T https://wakelet.com/wake/GhGPZ41Wwwl9NGVb9TCOZ https://wakelet.com/wake/WNXWfBf26V0e38sj2D6e6 https://wakelet.com/wake/iiOGXYXdfl95Eeea5gxfV https://wakelet.com/wake/JQnHJS0i0J0fpO7Ujwl39 https://wakelet.com/wake/Hl5loQZJiOF2M8YxfVisN https://wakelet.com/wake/gJTZ6aNRMYFd1rL18ATi3 https://wakelet.com/wake/RZToX8fi4S_jUuvrxyNdj https://wakelet.com/wake/18XT1ao1pC70MsBGP-xk7 https://wakelet.com/wake/en1J4I7JRXwsbTm3qNV34 https://wakelet.com/wake/DiMABRlB7be2-4MnzM8Wj https://wakelet.com/wake/KdQsFguMSDKvEQ8DsApGl https://wakelet.com/wake/Ve6r2DIsP7x7OJ6E_O1Xr https://wakelet.com/wake/VYzKVM6SWSxLdltIUh-Aq https://wakelet.com/wake/cEq5ttat6molIcRUmMm_h https://wakelet.com/wake/v7w_x--yPV6VEhit9WFvD https://wakelet.com/wake/dtpsDrpH7FSati5L9Kda_ https://wakelet.com/wake/rSw54kcVcqfOh70qTGMZf https://wakelet.com/wake/vmgyfV2YB-xuEIKrkwUo2
hirkah (Wednesday, 22 December 2021 21:36)
0ecef09eb3 . https://wakelet.com/wake/0RQ8M9v3AyLDWbhhyyu8G https://wakelet.com/wake/mmU9gk4ZRBfnDrbKjjkbc https://wakelet.com/wake/XzTTob98p9qXlwSP1l4Va https://wakelet.com/wake/BF9es8ohGf-yrhoZslhnF https://wakelet.com/wake/gsvf11CkgGTB3PPzyXH-V https://wakelet.com/wake/_ykYTr4e-zT67lfTufMxn https://wakelet.com/wake/9v0ny0PrKgNtqeo3vbOB2 https://wakelet.com/wake/DdX8HPzRtZC4eIDUdmQM7 https://wakelet.com/wake/qqEj0AglIx1lNZybFCT5Z https://wakelet.com/wake/r_J3oskiOY8adUawnZv_T https://wakelet.com/wake/htOIOZaZB9pbaqOlG90bB https://wakelet.com/wake/t8bADoxQwc9iOqa0vFYSD https://wakelet.com/wake/8sltAlZIly6fbyX_RvD_c https://wakelet.com/wake/9s_79kx5oly6SBe1HYMhH https://wakelet.com/wake/5HhhuscSFlTDtJbsdl7g9 https://wakelet.com/wake/SD0CMMf_p5EB3AcG4IERg https://wakelet.com/wake/B1mHwzGRWvZTrktfl0Bxj https://wakelet.com/wake/nwuMIU4-A6dLkVJcwhR-l https://wakelet.com/wake/CqBetM7biissu4JR_x_Jx https://wakelet.com/wake/7aRGaeuOKgNNRVCiooU3Z https://wakelet.com/wake/WfTgRuZ8yxhhNN0PxbiyV https://wakelet.com/wake/6Gx1Dxt2iUBtlAFQ-oGVI https://wakelet.com/wake/BAv_Ok-R9TsFI-EM8Zlyb https://wakelet.com/wake/J8CTIkICw3MinCO4Vsfl1 https://wakelet.com/wake/C2VlKHLZmO0YHJtH0Ivh3 https://wakelet.com/wake/iHXv2Lvi41zK8sbHb94Uc https://wakelet.com/wake/csv_aYV1fCVrFkPOjhjrH https://wakelet.com/wake/M5_J2Zn5AG4wl6UMOZoaH https://wakelet.com/wake/S4nJJDWslSrVAFmzryZEw https://wakelet.com/wake/2h-qzbt0GSp-V7_idoHvw
contree (Wednesday, 22 December 2021 22:38)
0ecef09eb3 . https://wakelet.com/wake/s0eaOY-C7-0Om9QajQiO4 https://wakelet.com/wake/MoM9WdoLezaumcT4S4unO https://wakelet.com/wake/FNpyCuS8WfzHj_erNEzTI https://wakelet.com/wake/r_9-X9QchkgU6ggGripq9 https://wakelet.com/wake/EirHsZ2SdFLXsIFX_aga6 https://wakelet.com/wake/SmXSec0n9kqY9-kRlADLJ https://wakelet.com/wake/TEG-9IGRh8x8PXYgCqruL https://wakelet.com/wake/eFs7Ss7lrwalCBIM9qMjj https://wakelet.com/wake/VfT6d2xYNvRXQHBqo3UpB https://wakelet.com/wake/iCZA_kXf0BckqfGjxxugI https://wakelet.com/wake/D-WGYYtnHEMVbcLhegHx9 https://wakelet.com/wake/542uTE_sP6JM6EYLZzQvW https://wakelet.com/wake/MlJUApiolzYpE8VogDqnN https://wakelet.com/wake/pUxX9ni7BaWTfPt-vY1Ij https://wakelet.com/wake/ZwxGElDPtWRun1vxYbmiw https://wakelet.com/wake/SquuXLsWqqFtBCnU8R6ma https://wakelet.com/wake/fXgDmBSmW0DfFrxKqvuub https://wakelet.com/wake/_4479XRP0iMPgwVAo9Sna https://wakelet.com/wake/VqJM4N5EevePf_f6ZWcPj https://wakelet.com/wake/b7z4qsKiwkb2ImbVkw-Ii https://wakelet.com/wake/L5bAbiJkizmLA1JlH5cWn https://wakelet.com/wake/cP8a6CTe_DJ6dLujmsdIC https://wakelet.com/wake/87YQ4SKS03xIY-IpmwZVY https://wakelet.com/wake/KumUgZvKYJsq5Jze_lulG https://wakelet.com/wake/dN6pomOImaE1954IyYrZZ https://wakelet.com/wake/L-QBNtQm2VQmAqab_ji0f https://wakelet.com/wake/jBshF6oiRMC56My6IaOJB https://wakelet.com/wake/kDjqJ9BxOJYNzPgIEI4l2 https://wakelet.com/wake/O1_dhlpelS7YkJFwjetPk https://wakelet.com/wake/3sNBD2DyCDqhLvQBTHt8V
herlare (Wednesday, 22 December 2021 23:34)
0ecef09eb3 . https://wakelet.com/wake/L5bAbiJkizmLA1JlH5cWn https://wakelet.com/wake/S4tHZc6fBv-X30GjhbxOg https://wakelet.com/wake/wYCqqJY4vLiRSRdLjre-v https://wakelet.com/wake/6bUlo513ECAyHbZmhCf-3 https://wakelet.com/wake/zJrqsKVstopg8iPvaWeNy https://wakelet.com/wake/tFONMMSuAkvMA6-IQyII4 https://wakelet.com/wake/joUFQ8GqqZB-cOjFa-0r2 https://wakelet.com/wake/dQ8hTe31ah5FnNOSXEsVu https://wakelet.com/wake/-5wX-1Sq5iTuyZkuItw79 https://wakelet.com/wake/UVWySm1oHepIhPUfhks8u https://wakelet.com/wake/U-8p6gk5iaWx0Xbspc-mS https://wakelet.com/wake/mkUulFUB7ReKHETqsWGfo https://wakelet.com/wake/fpe88RsfeuYQADIYNBvY1 https://wakelet.com/wake/In1o5H4VkiG__SpTlnv8o https://wakelet.com/wake/ajcnN2Vv1oZv-kIgXqJn4 https://wakelet.com/wake/iWl8czNbgXQdiiLGAda3v https://wakelet.com/wake/1LexntjkxxHlL2GLrSNnH https://wakelet.com/wake/4t3DBDR6zYfSAFBW1lf07 https://wakelet.com/wake/zjAyiH7ucL5C7FAnXAKvi https://wakelet.com/wake/nakTuT2yBXTvUweYuYvfY https://wakelet.com/wake/bqcb1aqcdKc6BfbPuHeaG https://wakelet.com/wake/9_JpxUP7wElFilgv69t71 https://wakelet.com/wake/4M4Oy61QWRkQojCxKOQjf https://wakelet.com/wake/CMyFP3uTYvJoaBOwWzkoN https://wakelet.com/wake/OVqk6f63LRUP6sdWVd09G https://wakelet.com/wake/9cr1MA6L78B44mPTJUP29 https://wakelet.com/wake/H8Oq2_8qS5boqecBmeuQ1 https://wakelet.com/wake/svPu3hq2_ewpKc9Vb2yYg https://wakelet.com/wake/TdwqhNV6ElP74k6zCKcZX https://wakelet.com/wake/tzpD4VB4GDapov7AiF7Si
talbujanis (Thursday, 23 December 2021 06:02)
d4f391380b . https://cdn.thingiverse.com/assets/6f/f8/d0/9e/ab/das_xentry_09_2011_torrent.html https://cdn.thingiverse.com/assets/f2/d6/02/9b/0c/roszer538.html https://cdn.thingiverse.com/assets/20/57/b6/d8/f4/lateamal713.html https://cdn.thingiverse.com/assets/50/d5/8c/d0/87/Zmodeler-3-Crack-Serial-18.html https://cdn.thingiverse.com/assets/a1/58/f2/8a/47/terjemahan_kitab_hilyatul_auliya_pdf_37.html https://cdn.thingiverse.com/assets/ce/ff/cc/91/f8/Remo-Tamil-full-movie-in-hd-download.html https://cdn.thingiverse.com/assets/ec/8f/89/ca/5b/Stardraw-design-7-Crack32.html https://cdn.thingiverse.com/assets/84/4e/9e/bc/37/Download_Keygen_Xforce_For_Buzzsaw_2018_Key.html https://cdn.thingiverse.com/assets/08/b3/78/a0/36/osy6zer265.html https://cdn.thingiverse.com/assets/b0/3e/d8/dd/f8/grahgil726.html https://cdn.thingiverse.com/assets/78/20/8b/25/da/visoaller817.html https://cdn.thingiverse.com/assets/3e/d4/fb/ef/64/Battlefield_3_highly_compressed_pc_games_573_mbhttps_scoutmailscom_index301php_k_Battlefield_3.html https://cdn.thingiverse.com/assets/36/21/69/6a/f1/naiviv51.html https://cdn.thingiverse.com/assets/b6/2c/85/99/c5/WebStorm_20201_Crack_Activation_Key.html https://cdn.thingiverse.com/assets/1e/14/c5/9d/19/autoclosets_lt_5_0_keygen_software.html https://cdn.thingiverse.com/assets/eb/21/a3/d0/3f/download-contract-vanzare-cumparare-auto-germania.html https://cdn.thingiverse.com/assets/41/a2/49/f3/15/crackoctopusboxlg.html https://cdn.thingiverse.com/assets/83/35/1c/92/a9/Play_Intrusion_2_Full_Version_Hacked.html https://cdn.thingiverse.com/assets/dc/35/44/c6/af/big-asses-fucked-videos.html https://cdn.thingiverse.com/assets/dd/f8/1b/b3/af/il-viaggio-dellunicorno-ita-download-torrent.html https://cdn.thingiverse.com/assets/5c/d8/82/a2/0c/marlisaar393.html https://cdn.thingiverse.com/assets/6c/57/87/14/17/Adobe-Acrobat-XI-Pro-1100-Multi--Patch-MPTrarrar.html https://cdn.thingiverse.com/assets/ce/cb/e9/ea/69/Download_Rustom_Hindi_Movie.html https://cdn.thingiverse.com/assets/3e/38/c6/f1/3d/Universal-Shield-47-Crack-12-iniziale-msica-piogg.html https://cdn.thingiverse.com/assets/01/34/14/ff/c8/renacher698.html https://cdn.thingiverse.com/assets/ab/e7/83/f4/c8/Logiciel-obd-diag-scan-en-versions-francais-crack-ou.html https://cdn.thingiverse.com/assets/47/c9/8b/b2/d6/enlavanit68.html https://cdn.thingiverse.com/assets/9a/73/ad/7a/e4/a-new-approach-to-sight-singing-pdf-download.html https://cdn.thingiverse.com/assets/79/41/be/4a/b9/Silo_2_Free_Download_serial_Number.html https://cdn.thingiverse.com/assets/aa/5b/e2/87/c2/Gameclub-ecoin-adder-free-392.html
chandaly (Thursday, 23 December 2021 07:04)
d4f391380b . https://cdn.thingiverse.com/assets/9e/55/50/66/5a/iWisoft-Flash-SWF-to-Video-Converter-34.html https://cdn.thingiverse.com/assets/1c/2c/d7/47/6a/Geomedia-Professional-61-Crack-Download.html https://cdn.thingiverse.com/assets/18/c9/5d/ad/3f/garvcazze774.html https://cdn.thingiverse.com/assets/a6/03/76/d6/79/aldkapen53.html https://cdn.thingiverse.com/assets/54/fa/4f/15/06/warcraft-3-frozen-throne-naruto-hentai-maps.html https://cdn.thingiverse.com/assets/4c/a6/de/3f/a1/Free-Download-Bud-Redhead-Setup-Full-Version.html https://cdn.thingiverse.com/assets/33/3c/9c/be/c7/Vijeo-Citect-72-Download-Crack-Software.html https://cdn.thingiverse.com/assets/79/84/74/a6/fa/Minecraft-Sexcraft-Mod.html https://cdn.thingiverse.com/assets/7a/99/18/89/f9/ManjhiTheMountainManhindidubbedfreedownloadutorrent.html https://cdn.thingiverse.com/assets/f3/16/0c/e3/51/frewenoela201.html https://cdn.thingiverse.com/assets/33/e2/15/7e/82/gineaellr582.html https://cdn.thingiverse.com/assets/12/c4/2b/de/8a/haldkaice875.html https://cdn.thingiverse.com/assets/8b/79/12/47/bc/A_Mighty_Heart_Movie_Torrent_Download.html https://cdn.thingiverse.com/assets/f9/bb/e6/90/b6/Sandeep-Garg-Economics-Class-12epub.html https://cdn.thingiverse.com/assets/98/0c/bb/1f/3c/True_Crime_Streets_of_LA__Pc_Highly_Compressed_Full___570_Mb.html https://cdn.thingiverse.com/assets/84/cf/93/fa/12/--Digital-Image-Recovery---N-.html https://cdn.thingiverse.com/assets/76/6a/01/2a/eb/CRACK-SolidWorks-2017-SP0-X64--With-SN-And-Activatorl.html https://cdn.thingiverse.com/assets/d5/ce/2a/8c/7f/hermoreyg7.html https://cdn.thingiverse.com/assets/16/83/88/20/f2/speecjays979.html https://cdn.thingiverse.com/assets/f2/d3/5d/22/6b/IBOOTER_DOWNLOAD.html https://cdn.thingiverse.com/assets/a0/2a/4d/5e/04/meloddeird728.html https://cdn.thingiverse.com/assets/d5/a2/b7/44/e2/Cinderella-Escape-2-Revenge-download-setup-compressed.html https://cdn.thingiverse.com/assets/56/26/55/64/ba/Vray_36_for_SketchUp_2018_Crack_Latest_Full_Version_Download.html https://cdn.thingiverse.com/assets/bc/a8/dc/a1/2a/kitchendraw_45_crackrar.html https://cdn.thingiverse.com/assets/ea/78/88/43/53/Samsung-E2252-Phone-Lock-Miracle-Box-Cracked.html https://cdn.thingiverse.com/assets/f1/77/c4/26/16/skypix-scanner-driver-download.html https://cdn.thingiverse.com/assets/ed/fb/4f/4e/74/Foundation_1_Gymnastic_Bodies_Pdf_Download.html https://cdn.thingiverse.com/assets/44/cc/db/e1/9d/Crack_Mixw_311hl.html https://cdn.thingiverse.com/assets/c9/7a/24/4c/6a/lanensi486.html https://cdn.thingiverse.com/assets/77/dd/88/8f/bb/autodata_dongle_emulator.html
gascopinte (Thursday, 23 December 2021 07:24)
d4f391380b . https://cdn.thingiverse.com/assets/82/a5/42/fc/0d/valxylea323.html https://cdn.thingiverse.com/assets/ce/b4/a9/1d/ce/Renault-Dialogys-48-Multilingual.html https://cdn.thingiverse.com/assets/61/8b/b6/2a/2a/eastwest_hollywood_strings_diamond_edition_cracked_version_41.html https://cdn.thingiverse.com/assets/65/40/a2/b2/49/nicohawt335.html https://cdn.thingiverse.com/assets/b2/66/df/43/4c/jesswel977.html https://cdn.thingiverse.com/assets/fb/6d/c8/c0/e4/recovermyfilesv521serialkey.html https://cdn.thingiverse.com/assets/15/45/48/81/c4/Download_Buku_Sosiologi_Pendidikan_Pdfl.html https://cdn.thingiverse.com/assets/79/3c/58/19/9e/drivers-Joystick-Eurocase-Eugaw610.html https://cdn.thingiverse.com/assets/9b/64/5b/91/a4/AUTODATA_749_Crack_Activation_Latest_Version_Serial_Key.html https://cdn.thingiverse.com/assets/53/f0/7b/5a/7c/edad_legal_revista_pdf.html https://cdn.thingiverse.com/assets/41/bc/93/ec/89/Rubber_Ninjas_Game.html https://cdn.thingiverse.com/assets/d1/40/a9/70/41/harltre186.html https://cdn.thingiverse.com/assets/cb/cb/cb/27/e7/FreeVimager_v905__.html https://cdn.thingiverse.com/assets/b1/1e/d3/a8/33/men-of-war-trainer-1175-steam.html https://cdn.thingiverse.com/assets/cf/d8/29/e1/c5/nyealdesir318.html https://cdn.thingiverse.com/assets/73/d7/fa/63/f6/Lumapix_Fotofusion_V5_Crack_Download.html https://cdn.thingiverse.com/assets/5c/19/f8/1b/a6/Psx_Harry_Potter_E_La_Pietra_Filosofale_Psx_Ita_Iso.html https://cdn.thingiverse.com/assets/6a/1c/5d/58/86/birlell927.html https://cdn.thingiverse.com/assets/61/c1/d7/be/63/wambjal140.html https://cdn.thingiverse.com/assets/cc/aa/d7/db/28/pamulan844.html https://cdn.thingiverse.com/assets/e1/46/f6/a7/c7/Geng-Pengembaraan-Bermula-720p-Or-1080p.html https://cdn.thingiverse.com/assets/96/3a/0d/db/b4/Auslogics_File_Recovery_9402_Crack.html https://cdn.thingiverse.com/assets/0a/f8/04/50/65/hiriwdebor893.html https://cdn.thingiverse.com/assets/31/70/dd/ea/7e/22-Jump-Street-Full-Movie-Download-Free.html https://cdn.thingiverse.com/assets/67/c4/76/17/66/SAS_JMP_Statistical_Discovery_V100_HTD_LifeTime_By_SaMeep_64_Bit.html https://cdn.thingiverse.com/assets/bc/11/9f/8d/d3/takafaby162.html https://cdn.thingiverse.com/assets/96/41/2f/76/a9/Official-Sony-Xperia-L1-Dual-SIM-G3312-Stock-Rom-ftf-for-FlashTool.html https://cdn.thingiverse.com/assets/14/ab/fa/6e/76/CyberGhost-VPN-10903190-Crack-rar.html https://cdn.thingiverse.com/assets/b9/eb/e7/57/e9/Immo-Universal-Decoding-32-Keygen-Download-Torrent.html https://cdn.thingiverse.com/assets/47/b3/8f/66/45/bridesav308.html
ottavphili (Thursday, 23 December 2021 09:22)
d4f391380b . https://cdn.thingiverse.com/assets/6d/b9/7d/f5/75/lagu_lagu_wajib_nasional_dan_not_angka_dan_not_balokpdfrar.html https://cdn.thingiverse.com/assets/18/92/ee/87/38/Dragonia_Ativador_download.html https://cdn.thingiverse.com/assets/c5/5f/f6/66/9c/Hdd_Regenerator_2011_Serial_Number_Rar.html https://cdn.thingiverse.com/assets/91/7d/60/0b/4c/lochedekod13.html https://cdn.thingiverse.com/assets/86/32/54/00/6a/carta_nautica_1111_pdf_download.html https://cdn.thingiverse.com/assets/c3/b7/bb/e5/39/opalewil809.html https://cdn.thingiverse.com/assets/29/38/a5/36/fa/aurora-follada-en-parque-de-pola-de-laviana-asturias-avi.html https://cdn.thingiverse.com/assets/c3/ce/ae/10/6d/marrraff967.html https://cdn.thingiverse.com/assets/bd/5b/62/41/79/Stockbase_Pos_2012_Full_22.html https://cdn.thingiverse.com/assets/a7/9e/e0/a0/8b/Teri_Meherbaniyan_Full_Movie_In_Hindi_Download_720p_Movie.html https://cdn.thingiverse.com/assets/30/59/73/0a/e1/takargarr287.html https://cdn.thingiverse.com/assets/1d/e5/9b/ce/c3/Api_560_Fired_Heater_Download_Free.html https://cdn.thingiverse.com/assets/33/b3/6d/1c/15/jandar291.html https://cdn.thingiverse.com/assets/56/5b/be/fd/b3/Allwinner_A13_Flash_File_Free_Download.html https://cdn.thingiverse.com/assets/9d/a5/42/c7/4d/calnivi830.html https://cdn.thingiverse.com/assets/63/d0/8a/b7/5a/janjans843.html https://cdn.thingiverse.com/assets/db/f5/cb/e4/98/vittoredc252.html https://cdn.thingiverse.com/assets/79/35/a9/df/35/Crack_Para_Jugar_Online_Lost_Planet_2.html https://cdn.thingiverse.com/assets/14/5c/7c/2c/fd/Free-Download-Mp3-Instrumental-Untuk-Renungan.html https://cdn.thingiverse.com/assets/d9/82/67/f9/5f/betynazar778.html https://cdn.thingiverse.com/assets/cd/1c/3a/39/d1/adquisiciones_y_abastecimientos_cristobal_del_rio_pdf_92.html https://cdn.thingiverse.com/assets/6a/c0/92/a3/32/Need-for-Speed-Most-Wanted-Magyarositas-CODEX.html https://cdn.thingiverse.com/assets/b9/9f/00/cf/8d/legejasi944.html https://cdn.thingiverse.com/assets/d3/6c/26/0f/87/Ip_Video_System_Design_Tool_Keygen_Torrent.html https://cdn.thingiverse.com/assets/f5/cf/7b/1e/c9/darwardl891.html https://cdn.thingiverse.com/assets/46/b1/28/fb/d3/Viva_Pinata_Trouble_In_Paradise_Pc_Download_Free.html https://cdn.thingiverse.com/assets/52/c7/d9/d3/15/pavgeray276.html https://cdn.thingiverse.com/assets/46/49/c6/31/2b/HD-Online-Player-Telugu-Movie-With-English-Subtitles-.html https://cdn.thingiverse.com/assets/37/0b/d2/a6/1a/Film_Impact_Transitions_Crack_Macbook.html https://cdn.thingiverse.com/assets/bd/51/31/20/83/facebook-password-hacker-v298-activation-code11.html
valepan (Thursday, 23 December 2021 10:05)
d4f391380b . https://cdn.thingiverse.com/assets/d2/0c/1b/ab/37/Raone-hindi-movie-720pmkv.html https://cdn.thingiverse.com/assets/6c/50/32/6a/94/Sbi_Rtgs_Form_Free_Download_Pdf_.html https://cdn.thingiverse.com/assets/65/75/d5/9a/ca/EverQuest-Rain-Of-Fear-RoF2-For-PEQ-EZ-Server-More-Torrent.html https://cdn.thingiverse.com/assets/3b/79/eb/72/16/HD-Online-Player-guia-conamat-bachillerato-pdf-downlo.html https://cdn.thingiverse.com/assets/a7/a0/42/0e/9b/Rahasya-movie-download-720p-movie.html https://cdn.thingiverse.com/assets/5c/2b/c0/c5/2a/Geometria-Descriptiva-Nakamura-Pdf.html https://cdn.thingiverse.com/assets/73/53/6d/4b/81/caivanne506.html https://cdn.thingiverse.com/assets/3e/08/39/3b/c9/HD_Online_Player_Full_Movie_Chandramukhi_720p.html https://cdn.thingiverse.com/assets/ae/25/a5/0a/e4/Hitman_Absolution_Update_10447.html https://cdn.thingiverse.com/assets/8f/34/f3/86/7b/benhip290.html https://cdn.thingiverse.com/assets/28/d1/3a/4a/06/dashfitzp377.html https://cdn.thingiverse.com/assets/bf/37/7c/b7/f9/hirens_boot_152_manual_pdf.html https://cdn.thingiverse.com/assets/73/cd/68/96/e0/Mission-Terrain-Dll-Silent-Hunter-5-22.html https://cdn.thingiverse.com/assets/fe/7a/42/b9/46/HD-Online-Player-psychopathia-sexualis-movie-free-dow.html https://cdn.thingiverse.com/assets/bb/f2/8c/d8/96/mertal244.html https://cdn.thingiverse.com/assets/93/89/01/51/ed/mariabrad516.html https://cdn.thingiverse.com/assets/ab/00/9a/5f/f3/aveque131.html https://cdn.thingiverse.com/assets/bd/09/1a/f2/71/aylale591.html https://cdn.thingiverse.com/assets/91/f7/15/1e/4e/drpubulksmscrackserial.html https://cdn.thingiverse.com/assets/eb/71/30/6e/35/HD-Online-Player-Earthstorm-720p-torrent.html https://cdn.thingiverse.com/assets/a4/c0/2a/7f/62/kailyard41.html https://cdn.thingiverse.com/assets/55/b4/c5/24/88/ScourgeOutbreakCODEX2014PCENGMulti7DRMFree.html https://cdn.thingiverse.com/assets/b8/28/7b/52/e0/findlaykilcherdownssyndrome.html https://cdn.thingiverse.com/assets/79/97/d1/db/50/Huawei_Hisilicon_Firmware_Writer.html https://cdn.thingiverse.com/assets/d3/5d/38/b3/bb/Abriendo_Puertas_Ampliando_Perspectivas_Student_Worktext_Abriendo_puertas_ampliando_pespectivas.html https://cdn.thingiverse.com/assets/b7/69/38/b8/d0/DellOptiplex780PciSerialPort.html https://cdn.thingiverse.com/assets/38/28/7c/9f/3b/eobd-facile-premium-keygen-18instmank.html https://cdn.thingiverse.com/assets/bc/58/69/6a/39/HD-Online-Player-The-Jungle-Book-Movie-In-Tamil-Downl.html https://cdn.thingiverse.com/assets/fe/47/39/2c/31/chercli519.html https://cdn.thingiverse.com/assets/20/d6/25/c2/8c/Pmdg7478Cracked.html
helfall (Thursday, 23 December 2021 11:20)
d4f391380b . https://cdn.thingiverse.com/assets/9c/ba/58/07/92/xforce_keygen_AutoCAD_Electrical_2013_64_bit_windows_8.html https://cdn.thingiverse.com/assets/45/92/b9/98/3c/dolphin-svn-r-1713-download.html https://cdn.thingiverse.com/assets/53/68/ab/72/c1/download-ebook-pengantar-ilmu-politik-miriam-budiardjo.html https://cdn.thingiverse.com/assets/9c/df/bd/43/ae/HD-Online-Player-baishe-srabon-full-movie-hd-print-do.html https://cdn.thingiverse.com/assets/25/5b/98/bf/e0/binditaima289.html https://cdn.thingiverse.com/assets/f9/e0/0f/46/ec/Flexi10rarSerialKey.html https://cdn.thingiverse.com/assets/98/33/1a/b0/8e/Adobe_Photoshop_Lightroom_CC_2017_91_Crack_crack.html https://cdn.thingiverse.com/assets/df/a3/a5/02/71/Vdategames_Maddison_Final_Cut_15.html https://cdn.thingiverse.com/assets/a6/b3/ae/24/e8/sofedorit639.html https://cdn.thingiverse.com/assets/54/64/09/2e/c6/Total_Recorder_Professional_Edition_82_Crack.html https://cdn.thingiverse.com/assets/56/6c/3e/fa/25/tone2_gladiator_crack_keygen_pes.html https://cdn.thingiverse.com/assets/37/7b/ad/77/a9/Spider_man_3_PC_game_ISO_free_download.html https://cdn.thingiverse.com/assets/74/10/3a/79/f7/murdosatu777.html https://cdn.thingiverse.com/assets/94/8d/bb/2d/0e/Keylemon_Control_Center_Crack_Key_Serial.html https://cdn.thingiverse.com/assets/08/46/7e/94/c7/farrifritz385.html https://cdn.thingiverse.com/assets/aa/e2/e8/f6/d8/Nero_Platinum_2019_Suite_20006500_Crack_Download_2019.html https://cdn.thingiverse.com/assets/7a/05/78/ac/c9/Lust_from_Beyond_download_with_utorrent.html https://cdn.thingiverse.com/assets/64/d3/bf/38/4e/FSX-PMDG-737-600-700-torrent.html https://cdn.thingiverse.com/assets/e5/e3/41/69/e6/nellyedmun544.html https://cdn.thingiverse.com/assets/3e/fb/f7/5c/12/download-moviestorm-cracked-full-free.html https://cdn.thingiverse.com/assets/0b/30/47/f9/28/finlas381.html https://cdn.thingiverse.com/assets/80/17/0f/2f/1d/basic-electronics-mv-rao-pdf-free-download.html https://cdn.thingiverse.com/assets/0e/5a/86/72/67/PATCHED-Alcatech-BPM-Studio-Pro-491.html https://cdn.thingiverse.com/assets/b0/33/d2/5d/3c/indegmil622.html https://cdn.thingiverse.com/assets/32/af/d5/15/26/LeisureSuitLarryWetDreamsDontDrySoundtrackActivationCodeCrackSerialKey.html https://cdn.thingiverse.com/assets/ce/fc/bb/59/32/HD_Online_Player_Robot_full_movie_full_hd_1080p_in_hi.html https://cdn.thingiverse.com/assets/c9/09/ca/dc/aa/Gertrud-Schiller-Iconography-Of-Christian-Art-Pdf-Download.html https://cdn.thingiverse.com/assets/0a/0b/8f/e5/87/quartus_ii_110_license_crack.html https://cdn.thingiverse.com/assets/e2/7a/f6/5a/3d/Light_Image_Resizer_6092_Portable_patch_rar.html https://cdn.thingiverse.com/assets/7f/64/a9/ed/3e/manddatab559.html
zoltuleti (Thursday, 23 December 2021 11:46)
d4f391380b . https://cdn.thingiverse.com/assets/b5/68/a5/f5/ba/Topograph-98-Se.html https://cdn.thingiverse.com/assets/32/66/e1/43/7b/wikoshe110.html https://cdn.thingiverse.com/assets/4d/11/bd/c0/3f/Mcmyadmin_Crackedzip.html https://cdn.thingiverse.com/assets/4b/cb/49/87/40/dark_studio_dark_robbery_kingpass.html https://cdn.thingiverse.com/assets/42/27/5a/20/2d/Plant-Firefighter-Simulator-2014-hack-working.html https://cdn.thingiverse.com/assets/69/11/20/bc/2c/freeval937.html https://cdn.thingiverse.com/assets/41/6b/d3/96/75/maidea512.html https://cdn.thingiverse.com/assets/7b/79/7e/f1/47/odesstamya810.html https://cdn.thingiverse.com/assets/04/b0/f8/4f/c2/Keygen_Full_V13_Build_Autocom_15.html https://cdn.thingiverse.com/assets/d5/7b/45/98/ef/delbella809.html https://cdn.thingiverse.com/assets/18/7a/eb/9b/b6/ardeuza584.html https://cdn.thingiverse.com/assets/c7/04/2d/95/45/NEW_FIDIC_GOLD_BOOK_CONTRACT_GUIDEpdf.html https://cdn.thingiverse.com/assets/02/c5/76/3a/29/hirscnirv703.html https://cdn.thingiverse.com/assets/ff/90/7a/8e/73/download-dota-1-full-version-indowebster.html https://cdn.thingiverse.com/assets/b1/9a/07/99/f9/Solid_Edge_V16_Full_Version_Free_Download.html https://cdn.thingiverse.com/assets/df/29/2f/f3/d9/WICresetkeygenerator.html https://cdn.thingiverse.com/assets/bf/91/fe/89/86/ferydaeli41.html https://cdn.thingiverse.com/assets/07/c6/fe/fe/da/carlfily916.html https://cdn.thingiverse.com/assets/50/83/57/d9/7f/Bad-Boy-2013-Telugu-Movie-Free-Download-Torrent-Karthik.html https://cdn.thingiverse.com/assets/8a/37/2c/25/29/Sambo_Fighting_Techniques_Pdf_Download.html https://cdn.thingiverse.com/assets/8b/7a/9e/72/cd/olinangli899.html https://cdn.thingiverse.com/assets/1b/72/21/93/5d/chadlynl376.html https://cdn.thingiverse.com/assets/90/d7/51/d5/61/frank-vahid-digital-design-with-rtl-design-vhdl-and-verilog-download-pdf.html https://cdn.thingiverse.com/assets/2a/c7/ea/34/30/Jung-Movie-Download-Sanjay-Dutt.html https://cdn.thingiverse.com/assets/67/fb/c6/5d/d7/Bongiovi-Acoustics-DPS-Audio-Enhancer-2222-Crack--15-MB.html https://cdn.thingiverse.com/assets/fc/b4/5e/3b/a3/Ride-Samuel-Hazo-Score-Pdf-12.html https://cdn.thingiverse.com/assets/a6/d5/ca/a4/ef/artcut_2009_wentai_free_download.html https://cdn.thingiverse.com/assets/fd/fb/c1/1c/27/golmaal-1979-movie-dvdrip-download.html https://cdn.thingiverse.com/assets/48/d4/b3/d0/f5/La-sabiduria-del-cuerpo-cannon-pdf.html https://cdn.thingiverse.com/assets/99/fd/9b/95/10/Star-Command-Galaxies--Alpha-6-skidrow-reloaded.html
palgly (Thursday, 23 December 2021 12:02)
d4f391380b . https://cdn.thingiverse.com/assets/74/fc/d3/47/31/giovnarai67.html https://cdn.thingiverse.com/assets/b0/4a/b8/64/bf/Mathworks_Matlab_R2013a_801_Windows_x32_x64_full_version.html https://cdn.thingiverse.com/assets/83/b2/0d/58/4b/ODIN_137_by_secr9tos_keygen.html https://cdn.thingiverse.com/assets/f6/0b/44/a4/22/Clave_De_Activacion_De_Muvee_Reveal_X.html https://cdn.thingiverse.com/assets/33/1f/7f/b5/b8/telecharger_Robot_Structural_Analysis_Professional_2017_gratuit_avec_crack_64.html https://cdn.thingiverse.com/assets/c2/95/70/3f/13/GoodGame_Empire_Hack_v18rar.html https://cdn.thingiverse.com/assets/28/31/33/72/46/Arturia--DX7-v1211797-STANDALONE-VSTi-VSTi3-AAX-x86x64-full-version.html https://cdn.thingiverse.com/assets/ae/3c/db/c6/f2/MiniTool_Power_Data_Recovery_86_Crack_Serial_Keygen.html https://cdn.thingiverse.com/assets/05/46/53/f5/1b/Almena_method_touch_typing_crack.html https://cdn.thingiverse.com/assets/72/78/ff/05/7c/eM_Client_72361640_Pro_Crack_Product_key_Download.html https://cdn.thingiverse.com/assets/32/6a/4e/f4/c7/Pirates-Of-The-Caribbean-Game-Crack-Download.html https://cdn.thingiverse.com/assets/22/91/63/85/9a/Flasheff_2_0_Free_With_Crack.html https://cdn.thingiverse.com/assets/dd/cd/81/e3/ff/eFilm_WORKSTATION_34_keygenrar.html https://cdn.thingiverse.com/assets/61/74/56/35/e0/Dying-Light-Patch-1-4-nosTEAMDying-Light-Patch-1-4-nosTEAMepub.html https://cdn.thingiverse.com/assets/12/cc/45/6f/03/Kyaa-Kool-Hain-Hum-3-3-Movie-Download-Kickass-Torrent.html https://cdn.thingiverse.com/assets/ee/3c/b2/d3/0c/Fiat-Ecu-Scan-26-Crack-Chomikujl.html https://cdn.thingiverse.com/assets/25/d1/0e/8b/e1/Descargar-Curso-De-Baile-Rba-Dvdrip-Torrent.html https://cdn.thingiverse.com/assets/0a/6d/46/92/33/HD-Online-Player-Young-Video-Models-Di02n-Daphne-9yo-.html https://cdn.thingiverse.com/assets/57/17/32/5a/07/amiyasm128.html https://cdn.thingiverse.com/assets/3f/52/52/be/f8/emmewinol109.html https://cdn.thingiverse.com/assets/b1/34/75/ce/67/HonestechVHStoDVDv4025WwWPorTorrentCoMPorGamolamar-Download-Pc.html https://cdn.thingiverse.com/assets/27/11/10/32/2a/2010-free-download.html https://cdn.thingiverse.com/assets/86/86/70/57/bf/Elementary_Linear_Algebra_Howard_Anton_10th_Edition_Solution_Pdf_Zip_Checked.html https://cdn.thingiverse.com/assets/90/c5/ad/f7/ff/forrest-gump-1994-brrip-720p-x264-english-subtitles.html https://cdn.thingiverse.com/assets/98/1e/f6/74/e5/elradlaven380.html https://cdn.thingiverse.com/assets/1f/93/0e/e3/2f/Robin-Sharma-Books-In-Telugu-Free-Download-Rar.html https://cdn.thingiverse.com/assets/51/7f/d7/38/38/CrackBuzzEdit33460.html https://cdn.thingiverse.com/assets/6e/bd/e7/79/cc/hillayland325.html https://cdn.thingiverse.com/assets/02/d5/6e/58/23/ISumsoft_Office_Password_Refixer_311_license_number_with_42.html https://cdn.thingiverse.com/assets/d2/ec/5c/df/d5/virtual-dj-85-free-download-crackinstmanks.html
remmvla (Thursday, 23 December 2021 15:06)
1640293103 . https://wakelet.com/wake/dEwhRywRe_K9uYPD7O89_ https://wakelet.com/wake/NRnzoqPcU8SudpyDpxchL https://wakelet.com/wake/RpEMbPL7A7sUR6QU9fqc2 https://wakelet.com/wake/thCTD280aI9jDMfBHu9-S https://wakelet.com/wake/oN-sSJ82Vd2ZHNCZMCXcR https://wakelet.com/wake/PjjAbbOicNOJ_u1RKWxOn https://wakelet.com/wake/vOUHsmGAu_i4sD5uzQxZe https://wakelet.com/wake/b6dBx1PLzOzfYcTUQty8c https://wakelet.com/wake/n_GINgXmgTkr5w2by1DyM https://wakelet.com/wake/zDJuynvceccaIRfJcaueX https://wakelet.com/wake/VnSXNGgKKc2ozJQFFzuQW https://wakelet.com/wake/ODU2pWhcczulXSM7KgXjp https://wakelet.com/wake/ro3_AMDrFkwF3RGgbZMi8 https://wakelet.com/wake/gLarXo8OUZFMTZvkqyBtx https://wakelet.com/wake/wQHCwt-BnfkFx9w83x_eR https://wakelet.com/wake/MZvJEjdbLrzzHR3DjQszI https://wakelet.com/wake/Ht7faaDwA_Qqz5-_phrSj https://wakelet.com/wake/o89vGo-PaxnUcKLWyiI2O https://wakelet.com/wake/G5Vk-9e5HyXS6GBYK0vdN https://wakelet.com/wake/XwljItHldOYJzovG8SVT5 https://wakelet.com/wake/V5tjqsmVf3dVUZ1s0SUwe https://wakelet.com/wake/QJWLj0nieiJuJ9pcVsHnm https://wakelet.com/wake/kq5MRswuvvvKosXNz-yBC https://wakelet.com/wake/l23o0r_INOLhWED7ZC3rf https://wakelet.com/wake/yvr9FkvUOADnbW1vP_x5C https://wakelet.com/wake/sZ9CBCxJp8csYFzSlTgoB https://wakelet.com/wake/D_N-HbS5QXAMGLpnRZvHt https://wakelet.com/wake/gQD6l6KgCly23qFchvRsS https://wakelet.com/wake/M0z9nbKelr9E6a219TfGv https://wakelet.com/wake/oXJXzGJq523EPmPvPKlyB
leajes (Thursday, 23 December 2021 16:56)
1640293103 . https://wakelet.com/wake/oolwJAfTP3txECWT3aYNI https://wakelet.com/wake/u0be4cy8jxqniS19H7vtM https://wakelet.com/wake/fMPQChBWEAIAnlv8kxLsX https://wakelet.com/wake/EsdszkVsYP7ji1eFFRa3B https://wakelet.com/wake/bItcmCDMHvJN7xtAtbqR7 https://wakelet.com/wake/h8vlXBgHbAZLLukZrXwIl https://wakelet.com/wake/W9g8I9Fnso6hLE9B7hbI0 https://wakelet.com/wake/-_AvXvUQKayg6aqvKrwxz https://wakelet.com/wake/Arnu1mYJ7Qt2-7NSlqy-S https://wakelet.com/wake/rTQ4hzVvy0WY7hhLrZFAJ https://wakelet.com/wake/KoDjXdKTHACZuei6GKRVB https://wakelet.com/wake/3qBs6aNU9_HrOKJm6Dzb6 https://wakelet.com/wake/jDy55xStp8Nvy_9qSQ9YK https://wakelet.com/wake/j_ynT0LCnigkheN6z1yc4 https://wakelet.com/wake/o07d34y2Tbsieaw7Pw4SC https://wakelet.com/wake/fQ6JcRKc9mL3CwKpV77Aq https://wakelet.com/wake/1TafP3l4dnz-PXGzqPc_x https://wakelet.com/wake/TyMO3X6FQA9kPsvNtqNLk https://wakelet.com/wake/ryIuM8LYnQV7umIX_zsAu https://wakelet.com/wake/tWgrbIUt9azlEeFSXHNwO https://wakelet.com/wake/U_22QVD_cikAV8Y2HTKhZ https://wakelet.com/wake/zDtgjQq2fEW42tI8Rp3NW https://wakelet.com/wake/VxpzVcO00k-ySUyLFyqi4 https://wakelet.com/wake/Mcy_o5cb0FEA5L-0wGLdg https://wakelet.com/wake/Ek7azEQ4rN66L2Bm1SfWm https://wakelet.com/wake/pDJrZrIsP7P9N7YDtQZvs https://wakelet.com/wake/WT37CJ54qBivcr9LeK3Q3 https://wakelet.com/wake/ZAkUgvpUOR2WeViI_4Jtd https://wakelet.com/wake/EUdQ4qP-cLq4M-nVQWj4D https://wakelet.com/wake/66_Hd0lSSDPe4Q8oBxadb
fredezabri (Thursday, 23 December 2021 22:06)
1640293103 . https://wakelet.com/wake/2r8Yl8EognRjnBWYirHFP https://wakelet.com/wake/1Q1nIGXjhfwNxQ6_jltmQ https://wakelet.com/wake/TaX6Aij9b2fxE3_ZM35nb https://wakelet.com/wake/SjarWuPOK5kgVbysVv2vm https://wakelet.com/wake/JXThAPkaLmD4iLo2vaXuJ https://wakelet.com/wake/n0DOwFjaAY_lQD_foTZVh https://wakelet.com/wake/i5R8xY7nBcHJo8N2ssZGQ https://wakelet.com/wake/TrkFOpNJDj0vgjTql3vPe https://wakelet.com/wake/AXqVOVtMo0gXOhxKNAicO https://wakelet.com/wake/NUPx746TYxrzhodELMiaT https://wakelet.com/wake/HgZ17EAZD181LFbnUl94q https://wakelet.com/wake/UJqse6yVjvqAbGKM40mQ- https://wakelet.com/wake/U8fnw7Y9SUOQHO8uTp9QX https://wakelet.com/wake/jCwVe12PgFicst9So1COu https://wakelet.com/wake/PnroCtVqvGG7RUr_dOY8o https://wakelet.com/wake/Xb7p3BzKkx2sd3NP77PWk https://wakelet.com/wake/EAtU6GRHmWxHxzgnQ6qB9 https://wakelet.com/wake/3idjw4S4sI2tChuvyodLD https://wakelet.com/wake/-8nGREMZeRALDpNkFLTJS https://wakelet.com/wake/RqRWZ04NDYmkErx_J8hiw https://wakelet.com/wake/y7vRry6ylAUtscvSGI7sl https://wakelet.com/wake/UwtoNZH6g99sg12pqBX6I https://wakelet.com/wake/onwMoVjunACZBNPCwc0GK https://wakelet.com/wake/MY3i9E2m75H0fhWRbns_4 https://wakelet.com/wake/TOy3s-vBnCjBjZ3ztSbgs https://wakelet.com/wake/e07uh8ONdRB7HYJ1lFut8 https://wakelet.com/wake/ddyDDeplefTqTzUldWZko https://wakelet.com/wake/AP_JvvwTwEbCrtrQrYR4L https://wakelet.com/wake/4mtlnI7blbp2kL9JMkVry https://wakelet.com/wake/NnIgRF0iQAKIOPI7nYfEJ
illylauri (Friday, 24 December 2021 01:00)
1640293103 . https://wakelet.com/wake/Y3iHz-YSzPu1ErA6UuHnF https://wakelet.com/wake/jjF6mrqxwu8xDkZGPxqKM https://wakelet.com/wake/2vfeEorQ6L5PwFOIvWyVF https://wakelet.com/wake/ze0cRyx4dzgwXw9i3OU-Q https://wakelet.com/wake/KZfHv6C0OjxJVXQTXNs3O https://wakelet.com/wake/OMeJOYs5C1GqJ6D2jzGfp https://wakelet.com/wake/GUsLC7xsSQDvKpOS4Ora7 https://wakelet.com/wake/d0u0tB9Lem8YIDpGCL_k8 https://wakelet.com/wake/J6-KBIltqdqmh6Wuj2zgR https://wakelet.com/wake/eG0BIG3x2EFHfyh3fsSky https://wakelet.com/wake/jdVoQgwAqiEtH7WPqYqB5 https://wakelet.com/wake/N0IG03aJ94CT1ecU2mY9a https://wakelet.com/wake/iICdq1Dqwt9jj6rGNeKwA https://wakelet.com/wake/mkm9qJ2QdmWmV-RHgSPrV https://wakelet.com/wake/MoQIb3f6U5889vrR6Nwc0 https://wakelet.com/wake/ASt-it1pZKJqkYSHdFT9_ https://wakelet.com/wake/egNb6G0qkvb-eI7IKrY9A https://wakelet.com/wake/dD-r4pZto9500RTvzE5iA https://wakelet.com/wake/7iYQIJBWBvYItWtdywFHN https://wakelet.com/wake/UKMaxeOHVusq5q3cjoCA3 https://wakelet.com/wake/YkRvPhQT1Yt-JiCyBwi9T https://wakelet.com/wake/W2uyrzBdnAeQvHrAnkMCW https://wakelet.com/wake/4NEWwsCm53zeduE4vfBVc https://wakelet.com/wake/_C2X7k_qPCwrByuiFEOjq https://wakelet.com/wake/8Tu-FxHSEPCdvfOHwFdRV https://wakelet.com/wake/d_eyOlZeCye6aCr9YD1aZ https://wakelet.com/wake/Rm1SGJB5eGD4fjGHVFwAq https://wakelet.com/wake/HTRH5NRT_tmWLMuxIaoBu https://wakelet.com/wake/JAEairJHY_yY_JRpBeksh https://wakelet.com/wake/bo31wZdo-046CIt3XdTYx
kamater (Friday, 24 December 2021 01:38)
1640293103 . https://wakelet.com/wake/LPqZyXP4KwTf5iaFtIPJ- https://wakelet.com/wake/HOHF14U0K1OJRmBMYoXqH https://wakelet.com/wake/M2wJy7uxQBHIT5eIzey-t https://wakelet.com/wake/4xisAdFLr18z_4lfXWrmm https://wakelet.com/wake/0FVCwk-3EIKIKR-HytDTO https://wakelet.com/wake/rPO0fUN1yTkC-D8k7dVuk https://wakelet.com/wake/jw269mW-SWQkvKg6xzb-A https://wakelet.com/wake/XWDXRHv-tXxEyExXkuckS https://wakelet.com/wake/oJDZi6GFtPKWRMBElesEI https://wakelet.com/wake/AIKSAqIBkAD_b_2tKc0oX https://wakelet.com/wake/TZBEdzCUYhdQbJLUuvMFl https://wakelet.com/wake/pJ8sRs-dc5Kd1LnHnKj-9 https://wakelet.com/wake/mrHq0o9j6Sss2IQMcyPJT https://wakelet.com/wake/t5K6pB-IJI2A5X7dzjV4w https://wakelet.com/wake/3z0e4Ca4dvEsMUtJCoGdl https://wakelet.com/wake/kyRo-5HiqpkI6vaffFYa2 https://wakelet.com/wake/OQGrYZ4EAQ5F98AX__KRo https://wakelet.com/wake/sRqROpXW93IjcWsVdtUs9 https://wakelet.com/wake/YKKLDeG4AH8QglvyBCAmZ https://wakelet.com/wake/-3g-cJknPZPcHFdDu4I41 https://wakelet.com/wake/79-Nbpq3bsKhDy92gNiNQ https://wakelet.com/wake/I5jirJtzKIZZyXGvM_TkI https://wakelet.com/wake/oOPX_AEVyDoBoNqC_HdVC https://wakelet.com/wake/lhXKR1gbndfbh88Hcekz_ https://wakelet.com/wake/mrxRkGE6MQxaaZiVxJCqo https://wakelet.com/wake/qjdUP9iNSDy_5yiq5PJeB https://wakelet.com/wake/auIWUSq-kvj7M8nQSnKi5 https://wakelet.com/wake/X5cGj-usZSZ10rxWlvE3G https://wakelet.com/wake/_D0sKG3tMSAQZTG2dxdbx https://wakelet.com/wake/Y2Ec24nnp1ZvXZLIaZfG3
kamater (Friday, 24 December 2021 01:38)
1640293103 . https://wakelet.com/wake/fSJTsPn-1x_qra5FnfgDB https://wakelet.com/wake/gz-s71ARknbFM-o94ydEg https://wakelet.com/wake/tL6KOO81Mqnl7tLpriIlq https://wakelet.com/wake/sexJdII91Gjmcyhxqyw2Y https://wakelet.com/wake/uruWnu0mMyAI9qAWLILAQ https://wakelet.com/wake/L8_DVUuPuEcF4cnkF92oo https://wakelet.com/wake/fXXmramHXxeE3YjSh2T_7 https://wakelet.com/wake/SMOcTJkoHb8ovsJQ7xMq1 https://wakelet.com/wake/iB8kZFE8-Af2n6jGxL_77 https://wakelet.com/wake/Kf9NiosqOwfAealwPRJz1 https://wakelet.com/wake/mlzsxGUGUSGZyO3lI_teK https://wakelet.com/wake/vzI1CaeuTz41kkd2OMs5p https://wakelet.com/wake/N0Wx9E9IL1jU9g0wnYRbk https://wakelet.com/wake/U-cy2DnQW_aFjXNWbXGlk https://wakelet.com/wake/TJX9nZ3PYX3apv5EElaWx https://wakelet.com/wake/JIntuuWaA9Wsk7_t5xnsx https://wakelet.com/wake/kmHG6Y-X0_iWHMC51aisc https://wakelet.com/wake/IFAg-Q_AaDp8tKqgb3mCl https://wakelet.com/wake/tMpZMpL1mhD4iQRziptTF https://wakelet.com/wake/56tSWPNOULeiz0QPhY8yl https://wakelet.com/wake/y2o3zJdYrnkW_pbiJLU_Z https://wakelet.com/wake/AH-ORGs6U3DiLzMD4umIy https://wakelet.com/wake/NP1e2OKuH85sNfAMiS9oH https://wakelet.com/wake/JvxBg_au3M6w8zvy_OA3r https://wakelet.com/wake/CArbhmAD8CbsVZItfyz32 https://wakelet.com/wake/9QQWfUHKJKuSjeIlb45zE https://wakelet.com/wake/XnDSUG_tZP6gRMuvMiyB4 https://wakelet.com/wake/uRcXaLU4fTlrMoglh3ZPD https://wakelet.com/wake/PQ8tpOrPEeh6LHAVS8vhm https://wakelet.com/wake/j9qwvwI6OukDA-cDAuTNQ
keiralaur (Friday, 24 December 2021 01:39)
1640293103 . https://wakelet.com/wake/3n3p0vjvLBSNCKN8N-uJD https://wakelet.com/wake/2U-3XLQSZJK_XaZWw1c8b https://wakelet.com/wake/mrfHvyUJ7gkf8R3tceaZS https://wakelet.com/wake/UuEhi-G7Yakb1RPw0zCKt https://wakelet.com/wake/UQ8SAkyozXtNeO4wXvyO- https://wakelet.com/wake/p66zcJnyPFGpQ_oGyqXZL https://wakelet.com/wake/qMocxQHkb3Tu0-yGxkibz https://wakelet.com/wake/h1ZKhUXBN87DWx00CgS1I https://wakelet.com/wake/gGhkatfkuaLf14K8iw5Q- https://wakelet.com/wake/-ZYEETsWhWKoYwo-TEniT https://wakelet.com/wake/_ZdzN6EQYYr9MsnZ0cAPO https://wakelet.com/wake/pUYFKiZKSyKPvJMB2g1se https://wakelet.com/wake/-czjdz28xrQIl_ganQQ_t https://wakelet.com/wake/cVOEDq49DdjdYWN2Gyoq8 https://wakelet.com/wake/Pal9J0pCgY9E_ttjVwn64 https://wakelet.com/wake/uL-JnhG9qN3wJ-piXwt6J https://wakelet.com/wake/hcBJ_xlW1km3x_iL_a3oS https://wakelet.com/wake/GrTmljwuR0AmYyhaE0Kat https://wakelet.com/wake/GEJv2E1TTefJSwy211oT_ https://wakelet.com/wake/DOMPIt3Ek0SMWRB-VHqnk https://wakelet.com/wake/qlQgfjqwz8CCjja5Lq412 https://wakelet.com/wake/1SSu8aMwyA3Os1DRzn0qX https://wakelet.com/wake/hevFSKE-_P6CY4TZJxmkQ https://wakelet.com/wake/wVab-gfxG1TJue-KGyMJ1 https://wakelet.com/wake/KAkVuGmUiKmQ4lJhokkJb https://wakelet.com/wake/wW0Tf0CUMnSOjhx4f-ZXc https://wakelet.com/wake/EZ5Rt_osrruIZD9Cu4HWH https://wakelet.com/wake/aT1Betj6LUwSxuNxwR5jL https://wakelet.com/wake/j6dIaySusE5e4bVZ-RG3H https://wakelet.com/wake/0iw4vtdnEWIAmPJb_hqEE
keiralaur (Friday, 24 December 2021 01:39)
1640293103 . https://wakelet.com/wake/wzfQJ41G6xyhcyUdkTQsw https://wakelet.com/wake/fweD9qOBSWqYjlGO2UcEX https://wakelet.com/wake/c0c-6zPYR4NhluFiEUjfY https://wakelet.com/wake/Q26LmIyhaHOu1SBUeLOrJ https://wakelet.com/wake/-ZE3rfo8qAeJiUXZSinLY https://wakelet.com/wake/JW9z4eZPYhLmzjBcWKDTN https://wakelet.com/wake/0502W-XdUfAvAvjH3AkEe https://wakelet.com/wake/OMB657kWo8SfF7h-fMQ0l https://wakelet.com/wake/c5bd37b4ME4-iBc8Ilv3R https://wakelet.com/wake/zHQsknoipz7_rfJ2qAREr https://wakelet.com/wake/IDz_n2mz5DeaqNeFQkzhL https://wakelet.com/wake/aZ1VX91VtIbCBQMbgAAej https://wakelet.com/wake/ExvbmexVpkTJkMrecF8oT https://wakelet.com/wake/lRe9dMiSq3qidKCujYLM_ https://wakelet.com/wake/HD99LeOkwLmMDBclA0Mpj https://wakelet.com/wake/mSletNhMBpmia-2UUDvYg https://wakelet.com/wake/bnXmhrEn96fbcNlb_OCrn https://wakelet.com/wake/aaytmZq7ifXvPBO2mA2wd https://wakelet.com/wake/ELIcVi6kOjU5NRSkZGtLY https://wakelet.com/wake/_olRE_aNnhkQyorF0LZyx https://wakelet.com/wake/9EIuU6kYxzz7joPwVJs03 https://wakelet.com/wake/61o60H1IMqyGCBC4pBt3y https://wakelet.com/wake/jxJodqYl_tP1Qnwj9UiZW https://wakelet.com/wake/bSmeOyadnBqC7KP5fB_qK https://wakelet.com/wake/6AHApMc6n8Hod9ebQ0LLf https://wakelet.com/wake/Y9Ex-jm1wAq13SRipv6Q5 https://wakelet.com/wake/pS4ub_VN7HKOyj80U4Eho https://wakelet.com/wake/caym5tPmcxmniS4kuDvBc https://wakelet.com/wake/BwQSV_aOdsnjihdDQu6nh https://wakelet.com/wake/qpVu2yd2RQIwrExE3ba_Q
bethashany (Friday, 24 December 2021 01:47)
1640293103 . https://wakelet.com/wake/WFr5p8Shg7BnmWgIU6HII https://wakelet.com/wake/0QYQJ-7UfeZZbvtaDvd9i https://wakelet.com/wake/x-jXdP8sQtMslYiKP9ET2 https://wakelet.com/wake/tglzSHmfQe4zDQ5tLN5iG https://wakelet.com/wake/-IQQSoiMnI6NjqjWKsMx1 https://wakelet.com/wake/4uKspbtTdUiO5GnQqub5f https://wakelet.com/wake/yxiCqwpedU8UcJGqgCph6 https://wakelet.com/wake/xT1f3lrCECnUi19uesUPj https://wakelet.com/wake/wDX_XGcrKnykZuFh82Xp4 https://wakelet.com/wake/jMAZXD3wTczX0VZHx31oD https://wakelet.com/wake/ACzc_06U9Hd1gI-fxFTs6 https://wakelet.com/wake/ZCgH5If0wgghWQDqm6p22 https://wakelet.com/wake/zIqCAkJ-Gi9DJBBFhrTTO https://wakelet.com/wake/2J92f4Zyv8LzQ-t40CCJc https://wakelet.com/wake/x0nxHuxFKo3GHE_Nx7kcj https://wakelet.com/wake/UyfFWymgZ24DnliQIokkh https://wakelet.com/wake/yLcy8nYnEoofRaGZGaaRX https://wakelet.com/wake/3oEadwZITfrF-GkPDuyky https://wakelet.com/wake/fbDSigVdUw7ZFmQxzVJ3G https://wakelet.com/wake/c517nmbRaYV6F8bU2-QMw https://wakelet.com/wake/YeSkEfUeqVQcFsK2ZOV9q https://wakelet.com/wake/f8_4TTOKT4OkurAPe1sOU https://wakelet.com/wake/GW0CaQzpVRahPcndRzmay https://wakelet.com/wake/EW5TIkU3ofxWyQcQ48-aX https://wakelet.com/wake/HimURoU6K5RjNBulQ7GEv https://wakelet.com/wake/vtIKhrMErGKoTzmtlBjDA https://wakelet.com/wake/0yblbAevquiSeUoyotFNp https://wakelet.com/wake/Zios36xN9Qfxr6a-E0ybe https://wakelet.com/wake/757zjGa_FaiAQpS-h3KsJ https://wakelet.com/wake/wGfRkAfLxvF0UcucPXg00
denziire (Friday, 24 December 2021 02:21)
1640293103 . https://wakelet.com/wake/z4qU9_GF9mn0nsaO4MspN https://wakelet.com/wake/6ZTL6HPqT5MjBt2LFsPe- https://wakelet.com/wake/uzogvNHLQT_u4L_lAWdPZ https://wakelet.com/wake/PKrCbmHBf9DzVA7Zlpwwc https://wakelet.com/wake/JdXRyYofPNQLeSd9tdvqL https://wakelet.com/wake/hY8CWgFuCgbP0wtHSNZE_ https://wakelet.com/wake/Pa732QUenHCunz9190sbU https://wakelet.com/wake/45nC_JfscrM5MlRbZIxka https://wakelet.com/wake/x-G3oAoPACK1vKh2zxVpj https://wakelet.com/wake/CR_rZ_XjPdTy9OFMyttOY https://wakelet.com/wake/a4IH2gmSJ7V9VoIomuMz9 https://wakelet.com/wake/Q54zP2GnnhLPb6dpr8WDg https://wakelet.com/wake/EmkjD-EknOYzaq0aqH7Rv https://wakelet.com/wake/bAKb1ejQmrO7ItT63sgYS https://wakelet.com/wake/HevDnFh7Adf21bl_vOzjx https://wakelet.com/wake/ePJ_eWmwlQg5VRAeuqpy3 https://wakelet.com/wake/DK7ApeJnsTb1QFkN82bbh https://wakelet.com/wake/crpPnd6D8DaTvgAom7-_w https://wakelet.com/wake/OBx_tTpt2e8bd8OrpkqCv https://wakelet.com/wake/1R0waPMZCvD42I8-KM5W7 https://wakelet.com/wake/ByiewZuPlCfAXSseepvRy https://wakelet.com/wake/kwIOn5M-DCUyqxd9Ta2De https://wakelet.com/wake/UZDDpHi0njMjg0cov8Lhs https://wakelet.com/wake/cmEOJlVvsXW7MbafIHZgq https://wakelet.com/wake/Or4SNNFk0TnnZ0tBb1Nbi https://wakelet.com/wake/u7S0FKlzmVemGyed68bcn https://wakelet.com/wake/A0LgTeSQb7JoqgsthHhNu https://wakelet.com/wake/OPdooqeG0dTjKByqrESg2 https://wakelet.com/wake/_Y8XHRz0a0WwkM--FHiUx https://wakelet.com/wake/Hg_5vDenxBOo0Mumcizlg
jacingarre (Sunday, 26 December 2021 16:34)
459a7da569 . https://wakelet.com/wake/65qTaWlzoLknXyEFyJGZf https://wakelet.com/wake/ulJJcMUzAV39z1A2cOKIW https://wakelet.com/wake/SFpS93ERqjxtAp3tUTAy8 https://wakelet.com/wake/fk9IUVkMpbpAleH3akLms https://wakelet.com/wake/ni-LHLojku_EsYgsbuTcm https://wakelet.com/wake/9Q2JhEGf9BHuAytMYQ_fF https://wakelet.com/wake/2Ex2cB4i1wYMKibQYAha3 https://wakelet.com/wake/-JEMch09Yvm_cRoyyArE9 https://wakelet.com/wake/cZzWIne0UdaeOprekbD2I https://wakelet.com/wake/jJnuP0PRArphpJOXO2IzL https://wakelet.com/wake/3TaP1uUa1PdY8cpYqhlaX https://wakelet.com/wake/LewhWZaD-hzpJBgV8CHxm https://wakelet.com/wake/D4afapanoMYEMQMGJdzRV https://wakelet.com/wake/kTeqtVgiiXd3ZT9nxGu8K https://wakelet.com/wake/90v_9t2m_CeyvibzcLLCu https://wakelet.com/wake/WRRMJsAydZmMYEA8MaivF https://wakelet.com/wake/QGSrBfvh35DLI1-NW54aP https://wakelet.com/wake/ceWkigyu1xz9izaTW4NPQ https://wakelet.com/wake/8nA3-RzdLbiXtRJHRGd3Y https://wakelet.com/wake/cW8RIQ_xWl-V9uehc6Ndq https://wakelet.com/wake/ukEB8m3kEY0gY1NNcmIgG https://wakelet.com/wake/ouSLqyMO7rw1U-uX7IHEz https://wakelet.com/wake/dPq62gtuwguniHg8ENrgw https://wakelet.com/wake/xsSc_sBQfQnyfmqFZ91jA https://wakelet.com/wake/cRhXxaCnJmd34UM92bjDH https://wakelet.com/wake/bfzyDpsENDNHsY7taYOz4 https://wakelet.com/wake/Ri1RxpjjZ-yjTj5Lnyavx https://wakelet.com/wake/RRNZZLTDEB77-n5hullTV https://wakelet.com/wake/w-rgvqhDljq1OJyyXJZAZ https://wakelet.com/wake/0HjQQlVyD_CmQuj3FLVOg
aftoncolt (Sunday, 26 December 2021 16:43)
459a7da569 . https://wakelet.com/wake/iyO6_yPHIpUWbHu260w48 https://wakelet.com/wake/K84IM3gYPlqHm_kavvsBS https://wakelet.com/wake/dAGQNdmju-d1yazaxJ4VA https://wakelet.com/wake/QVI6CYpZXCOiNq6nHmrJr https://wakelet.com/wake/GbLZHdKku9IWeoEpQKksq https://wakelet.com/wake/7na5zymbTKv2_io4qlw19 https://wakelet.com/wake/37UWp99VR9JEqu6ruFezI https://wakelet.com/wake/haOT-rhSMbD3wV3U1xXbr https://wakelet.com/wake/K6rcsACrPeNaaf8CRVGOW https://wakelet.com/wake/ZXV1uPyE_y5BWAezE1pC_ https://wakelet.com/wake/i375qzbzuUYH4PXB1EaUk https://wakelet.com/wake/k5DvdRkp7pbfHiOHsOg01 https://wakelet.com/wake/S5shBKf1Sv6Eqo7Ei5CxR https://wakelet.com/wake/Dglz9GJr5sO0M7PVxtLCG https://wakelet.com/wake/JAfnZu25aY_SgFQYokbeY https://wakelet.com/wake/oj7tI6yt6LbozlauSS3K7 https://wakelet.com/wake/nJBRmv6xwjZJ_zvXrC3dr https://wakelet.com/wake/Jt0J9yqUN0H8maHgEHVGm https://wakelet.com/wake/W6ugXYrSlDieO2-Ga0_wx https://wakelet.com/wake/yvRai7TT5i0as7EfUl-Nz https://wakelet.com/wake/k8KgXtrqdLdr5v21YgXwQ https://wakelet.com/wake/k0mcNXKp5trXn7eXSRHOx https://wakelet.com/wake/xFVIn69GxIdGbIGJJ8HR7 https://wakelet.com/wake/dH0mKUDIhddqBGlVDEFW- https://wakelet.com/wake/xbCnGAi1X-4aM02S3_bBN https://wakelet.com/wake/xsU0eW4VjVbz3k9h3jIs0 https://wakelet.com/wake/kAOCnQXkIA_w1QO-4R35b https://wakelet.com/wake/gD8mhzOqEl_K7dPMmvYXu https://wakelet.com/wake/tbEMQ-u5j8wVvZtGwVnV0 https://wakelet.com/wake/4aMokMbVzQXWbr6r371AQ
aftoncolt (Sunday, 26 December 2021 16:43)
459a7da569 . https://wakelet.com/wake/9X9YLY2Tcy1ePvKmOu0o6 https://wakelet.com/wake/gMXliw8lmYJSVF4ht9wf_ https://wakelet.com/wake/dUYMch6syHX_Mf5hL4iV9 https://wakelet.com/wake/Tmdn2SKRjeklSZafsJ3xb https://wakelet.com/wake/0KbVUJUrWzmTbCIa-SU_G https://wakelet.com/wake/WXp_pEQ6OAvV2UslV5N1U https://wakelet.com/wake/3QG2e66vyK8b1taSNxude https://wakelet.com/wake/Ma8QUwkcxHwQw1wVODmZJ https://wakelet.com/wake/TMdC-zG9CVKBIe8i_w8KA https://wakelet.com/wake/BqZ17FucmMKS88LEK-JcK https://wakelet.com/wake/I7EhY1-goLC8glsurj6Ig https://wakelet.com/wake/ObIqCUHFw5c2Lotn9pAgc https://wakelet.com/wake/zHO2MLvAXekgBoUeaCuQk https://wakelet.com/wake/VWjL10qTQB7BagdGzkwXd https://wakelet.com/wake/lzwUXb2XatXuTbf7akRmC https://wakelet.com/wake/pJg6DRWEfqamTyY09JcLM https://wakelet.com/wake/RadpfN-gWCxNcLbpkS7zN https://wakelet.com/wake/_AKdIEoixx0JmPN9iexxA https://wakelet.com/wake/1L-1A7XhvxEf1Y8jtW3v_ https://wakelet.com/wake/usxN_ESkqnDomcyJP5eVB https://wakelet.com/wake/H9JL8KQTDBOiymGDAZLFE https://wakelet.com/wake/0E-MUNvxYkZTmA_pwjpoo https://wakelet.com/wake/qaqiZCXUQ7o3CqS-bKSrK https://wakelet.com/wake/_lbCT4Kp9iRvTyM1klyZP https://wakelet.com/wake/ok8JEUfPiPTsMhfE4XTlR https://wakelet.com/wake/nOzvbudFdRZDDZk9jPb0W https://wakelet.com/wake/1ImRiIeNbUytY_YRApQSt https://wakelet.com/wake/urUNx5PC9xZfJYR_t9T19 https://wakelet.com/wake/5tKssffkujA0jrfojqQDC https://wakelet.com/wake/4VXYEzSRaJQghxMmZBKuC
aftoncolt (Sunday, 26 December 2021 16:43)
459a7da569 . https://wakelet.com/wake/-T37FyASSbTXXfj7XqkSH https://wakelet.com/wake/onFUDjPmNODb6JNN2A1WI https://wakelet.com/wake/BNw0vuhlApLEuoqjT4Pj4 https://wakelet.com/wake/BOM-PvwMDp4uRzpk3XF0E https://wakelet.com/wake/JoBeLxJ0F9a62_BZT38s2 https://wakelet.com/wake/cbc8l6d5GzVErUv58ClRy https://wakelet.com/wake/75-_C-AMkl99_pKc22NyP https://wakelet.com/wake/QustXMyCnQpOrDskdCVZr https://wakelet.com/wake/2vOIgg3KF_xcC_nhXsJdT https://wakelet.com/wake/nkDXG8ZTXNQd6UoK-0aai https://wakelet.com/wake/fBUWJJmq_IKcJOtwHajwW https://wakelet.com/wake/_bGV1TM6KuJEtZZI8d1HA https://wakelet.com/wake/9YP9svvC6_5mdrMEcOnTU https://wakelet.com/wake/XKWLA0KxeNlly7KVhJiPM https://wakelet.com/wake/hlnub8ug9eA0EcZJrGUgW https://wakelet.com/wake/WFEcr11Kx9dUgiHdsK3fE https://wakelet.com/wake/KjQ-w0xl0DABDjhcUWic8 https://wakelet.com/wake/cmqtZgHTufJh93efAw_hr https://wakelet.com/wake/2bTeitaYl66Qdo42rR_5- https://wakelet.com/wake/pPSeXO6Rr_8MseLmZbfQo https://wakelet.com/wake/E0VKMP8XyrTzX3hN46zKA https://wakelet.com/wake/3TTeL8NoeiNuVe7vRO2LU https://wakelet.com/wake/5gBFMAFK7hwPIpCDlO_VG https://wakelet.com/wake/2OeJUMYvw_HBh1yDA1R9C https://wakelet.com/wake/49u4jLp1f6c2nO8p3ofz1 https://wakelet.com/wake/qiO9-CuuwcIH6wzLojEOT https://wakelet.com/wake/n6c6atJ0UnorCtQzVBWkd https://wakelet.com/wake/zJ0QBQzVAlOOWCylCG5Pw https://wakelet.com/wake/AiwmzuzUTqaJrqReLsyGm https://wakelet.com/wake/FA0tYjP4THwoa2IBBh8y5
wylbapt (Monday, 27 December 2021 02:58)
5c36288bc2 . https://wakelet.com/wake/UJP8BH6hrUHAh7ZTSl0qB https://wakelet.com/wake/wHyA75hEiRdoS74YM6hSY https://wakelet.com/wake/HOnm5yiiLPjT3PDcyhcNR https://wakelet.com/wake/SZclRxgJJP4kku2diOPsu https://wakelet.com/wake/BTGKKmxWJo3pYC0SG8zHA https://wakelet.com/wake/zMXHj-7HIU8_QdGsJfeMf https://wakelet.com/wake/UFeI8xFeJ4r8bCKhJTSYF https://wakelet.com/wake/_GKPrIEE_ANGEGi0TAlwx https://wakelet.com/wake/qNLj4BOMx7K6xzZn5sRrT https://wakelet.com/wake/3h_GDHOLxOwoBWEdkAYeM https://wakelet.com/wake/mUFUn5qDLzHG_cphBeDjC https://wakelet.com/wake/XBD5WBYtegxg-Pqt8alwc https://wakelet.com/wake/VqS04N9bqRziEBUnFcZB- https://wakelet.com/wake/4ZiOIQnOWE9fPTRa7kS8Y https://wakelet.com/wake/mLr-WDrxDk7WiCEhqdxm3 https://wakelet.com/wake/K0gSsmuL7m-VcbHjYjg5N https://wakelet.com/wake/mLRIaUySWW_LqiJelZ0-l https://wakelet.com/wake/BvVD4m4_699RsAU47MtXe https://wakelet.com/wake/2GoM39jTXHSr0m6PtJCzu https://wakelet.com/wake/9BzvbhRqtpgtB1Wfv6y-J https://wakelet.com/wake/DIhn40HDNK6nnOIjoHl6F https://wakelet.com/wake/Wd6yY1BTDh5XsAxuzdheB https://wakelet.com/wake/K6Vif-N6kv_nh6Oj5VR5e https://wakelet.com/wake/PSWMif1wuAHcC8lDnw66b https://wakelet.com/wake/FipNxsRzoQUaQpgtQDXxR https://wakelet.com/wake/hu94vO-bmmx22pLcHq6RX https://wakelet.com/wake/B4lWTwUZUKb3mpamdm5HV https://wakelet.com/wake/gSn_q-Nk90hjDep7n0Xhj https://wakelet.com/wake/wIFLiJ5SSvmzuEJSOl3Us https://wakelet.com/wake/1xniN1zoH5T6idz2wpSrn
jaleekelle (Monday, 27 December 2021 03:44)
5c36288bc2 . https://wakelet.com/wake/_flHCHyT5uxidee80J_z- https://wakelet.com/wake/qMHmqM26oFIqGC0WZuNwT https://wakelet.com/wake/4V68bs7-rxgK6FjnESbhz https://wakelet.com/wake/lJwHxPMbCNm3Fz2iQTJeA https://wakelet.com/wake/UnzpSWhj1azJlRUB1WVWz https://wakelet.com/wake/srIHjAE2Jp1wxWZcniier https://wakelet.com/wake/vrj6jHnKCQhr4bZYib4lz https://wakelet.com/wake/PewcG4wKo0ijrFUkP3yXM https://wakelet.com/wake/9CbykuIfy5zjZkTTCPQDq https://wakelet.com/wake/gBEwIzlp0jixXEk24WXMn https://wakelet.com/wake/9RkhZfo5k9LQv--NWqTdV https://wakelet.com/wake/CJPfUfFonP3ehvz4Y7End https://wakelet.com/wake/1sONzL3CF9dgeBneuVaxL https://wakelet.com/wake/dvAtS0gWKJxcDjT8BNRi7 https://wakelet.com/wake/ork08G8HSXKjFymFSiVtK https://wakelet.com/wake/L5RZawd6C4riNIFi2EsNa https://wakelet.com/wake/8qy-HB20MRL8ZZtukOB9m https://wakelet.com/wake/y3BZrqXeTxhx5RuPjV-mQ https://wakelet.com/wake/TC2ClPBy2YNIKBa-i29NX https://wakelet.com/wake/hcuDxgdMwjMIpS3BFjygo https://wakelet.com/wake/lh9ozKGCb1Djn9w2htS9H https://wakelet.com/wake/ZQlyIdjvaRqp7NGi4-sXf https://wakelet.com/wake/KFYrA7Z-Q23ULUo0nX4CS https://wakelet.com/wake/KCNUC2NxssKkBz2H0h0q- https://wakelet.com/wake/9skMTGYkaqqxTuuIu2VXI https://wakelet.com/wake/QJEhK0yECYuAF3cSkqe1t https://wakelet.com/wake/8tR_MoIMGtcLd1boHMs-x https://wakelet.com/wake/iSlvCdvgnIvaAHqh8YZBA https://wakelet.com/wake/KBdT0m-eXn5qtZ1s-ZILZ https://wakelet.com/wake/Oh7LSIiOSryaEP9XDzCTc
elfridar (Monday, 27 December 2021 18:10)
fb6c851797 . https://coub.com/stories/2173786-osegredosobscurodogaduempdf https://coub.com/stories/2194100-judgment-and-decision-making-psychological-perspectives-books-pdf-file-verified https://coub.com/stories/2206861-free-download-mission-impossible-rogue-nation-english-2-in-hindi-in-mp4-2021 https://coub.com/stories/2198473-top-notch-que-te-pica-mp3-download https://coub.com/stories/2198682-gestor-de-cocina-paco-roncero-35-patched https://coub.com/stories/2189529-free-encyclopedia-of-air-jordans-pdf-32 https://coub.com/stories/2214617-disney-princess-enchanted-journey-game-free-download-mac-full https://coub.com/stories/2194208-windows-10-redstone-1-14267-x86-x64-aio-30in2-adguard-tea-64-bit-high-quality https://coub.com/stories/2192530-download-advanced-password-retriever-hacking-softwarel-updated https://coub.com/stories/2172748-hawaizaada-hd-hot-download-720p https://coub.com/stories/2172325-__link__-ilok-pro-tools-9-crack-windows https://coub.com/stories/2203227-fadiaandfadiapublicadministrationpdfdownload-birnfynb https://coub.com/stories/2183509-link-crack-winavi-video-converter-11-serial-hmp https://coub.com/stories/2196939-datacash230deer-hunter-2005-flycam-patch-link-free-15 https://coub.com/stories/2178067-mirillis-action-3-9-5-extra-quality-crack-serial-keygen-torrent-here https://coub.com/stories/2166012-best-ps2-bios-scph-90000zip https://coub.com/stories/2200843-pirates-of-the-caribbean-3-full-movie-in-hindi-free-download-1-new https://coub.com/stories/2204275-akta-kerja-1955-pdf-quynbnas https://coub.com/stories/2200868-feel-the-flash-hardcore-kasumi https://coub.com/stories/2185061-nd3t-w57-software-best https://coub.com/stories/2180738-2021-dds-cad-10-dongle-crack-cubase https://coub.com/stories/2200085-airbag-reset-software-elm327-_hot_ https://coub.com/stories/2195298-mootools-3d-browser-for-3d-users-with-polygon-cruncher-serial-11-weslimarle https://coub.com/stories/2195327-quantitative-techniques-in-management-nd-vohra-pdf-free-download-__hot__ https://coub.com/stories/2194060-luxion-keyshot-pro-4-0-74-x64-animation-keyshotvr-deltas-utorrent-top https://coub.com/stories/2215070-game-theory-michael-maschler-pdf-download-aloath https://coub.com/stories/2180900-ipswitch-whatsup-gold-premium-v1-banale https://coub.com/stories/2177512-tweetbot-for-android-apk-link https://coub.com/stories/2184005-_verified_-spider-man-2-ps2-iso https://coub.com/stories/2216135-better-engravelab-9-crack
peytadas (Monday, 27 December 2021 18:10)
fb6c851797 . https://coub.com/stories/2174915-regisloiselpeterpanpdfdownload-oceasau https://coub.com/stories/2207732-download-exclusive-assetto-corsa-red-pack-exel https://coub.com/stories/2190147-senthoora-pandi-hd-video-songs-download-exclusive https://coub.com/stories/2206257-download-ebook-kalkulus-purcell-edisi-9-bahasa-indonesialkjhl-verified https://coub.com/stories/2191416-extra-speed-newstar-jimmy-tonik-nude https://coub.com/stories/2213759-top-detective-conan-download https://coub.com/stories/2177996-e-drejta-biznesore-1-test-per-provim-zip https://coub.com/stories/2174258-amibcp-v4-06-rarl-129311 https://coub.com/stories/2180564-lededit2014softwaredownload-trevedec https://coub.com/stories/2167451-hot-logiterm-alignfactory-1-2-1 https://coub.com/stories/2190214-verified-orange-for-oracle-60-keygen https://coub.com/stories/2170708-new-vegas-infinite-loading-screen-fix-balevel https://coub.com/stories/2193837-archmodels-75-download-upd https://coub.com/stories/2215113-intruders-hide-and-seek-codex-deeboyak https://coub.com/stories/2188876-prison-break-the-conspiracy-dvmdll-indir-__exclusive__ https://coub.com/stories/2167493-updated-first-strike-final-hour-bonus-content-torrent-download-pc https://coub.com/stories/2213969-watch-from-up-on-poppy-hill-english-dub-online-75-hot https://coub.com/stories/2169049-f-secure-free-patched-dome-vpn-2-23-5653-0-crack-crack-gallafor https://coub.com/stories/2214369-install-crack-fifa-08-fisierulmeu-stick https://coub.com/stories/2191850-convert-vmdk-to-qcow2-in-windows-with-these-free-software-high-quality https://coub.com/stories/2193002-psw-429-nt-2-27-_best_-downloadl https://coub.com/stories/2200134-julie-2-1-subtitles-720p-movies-better https://coub.com/stories/2201855-hd-online-player-bajrangi-bhaijaan-hd-1080p-full-repack-movi https://coub.com/stories/2167213-dj-aqeel-forever-2-2012-mp3-vbr-320kbps-ddr https://coub.com/stories/2204784-download-crack-edsa-technical-paladin-15-pelmar https://coub.com/stories/2174972-dammu-movie-online-free-download-exclusive https://coub.com/stories/2176333-full-kayuria-awek-tudung-isap-kote3gp https://coub.com/stories/2207655-votre-pc-prend-la-parole-crack-88-exclusive https://coub.com/stories/2176188-acronis-true-image-home-2010-build-7046-serial-trt-hot https://coub.com/stories/2200445-website-x5-evolution-9-template-crack-phimart
elfridar (Monday, 27 December 2021 18:11)
fb6c851797 . https://coub.com/stories/2187684-free-doom-3-bfg-edition-fixer-2-0-5 https://coub.com/stories/2191788-gemini-cad-x9-patched-crack-free-downloa https://coub.com/stories/2203446-windows-7-ultimate-romana-rusa-italiana-engleza-free-download-_hot_ https://coub.com/stories/2189364-signing-naturally-unit-2-homework-answersl-patched https://coub.com/stories/2204059-jilla-policewala-gunda-2-2014-dual-audio-hindi-tamil-720p-14 https://coub.com/stories/2215114-verified-igrica-komsija-iz-pakla-2-46 https://coub.com/stories/2182486-internet-download-_verified_-manager-idm-6-32-build-11-crack https://coub.com/stories/2215061-chadti-jawani-meri-chal-mastani-mp3-song-download-fixed https://coub.com/stories/2166294-all-your-favorite-shows-film-completo-in-italiano-download-gratuito-hd-720p-extra-quality https://coub.com/stories/2174393-top-korg-legacy-collection-digital-edition-vsti-rtas-1-32-keygen https://coub.com/stories/2178708-coldplay-multitrack-goncirvyn-dalmyan https://coub.com/stories/2206302-best-i-have-the-right-to-destroy-myself-ebook-download https://coub.com/stories/2168687-link-livro-compreender-e-ensinar-terezinha-rios-pdf-13l https://coub.com/stories/2199666-interfacial-science-barnes-pdf-19-salkeigh https://coub.com/stories/2198444-hot-wincc-6-2-3-rar https://coub.com/stories/2185410-opal-jennifer-l-armentrout-pdf-__link__-downloadzip https://coub.com/stories/2211866-link-sony-vegas-7-0b-with-serial-rar https://coub.com/stories/2177673-rocky-handsome-in-hindi-dubbed-download-download-free-2021 https://coub.com/stories/2193114-exclusive-telugu-anchor-suma-sex-story https://coub.com/stories/2174155-link-tubehunter-ultra-v4-0-1439-incl-keygen-by-fff-full-version https://coub.com/stories/2173434-perfume-movie-in-hindi-300mb-wallealeic https://coub.com/stories/2197911-top-gsi-tympstar-service-manual-epub https://coub.com/stories/2215282-zabadak-midi https://coub.com/stories/2211460-patched-carte-sd-gps-2019-nissan-note-2 https://coub.com/stories/2170287-top-micro-battle-minecraft-cracked-servers https://coub.com/stories/2197766-verified-infernal-restraints-safe-house-2-part-1-hazel-hypnotic https://coub.com/stories/2197256-chemia-pazdro-danikiewicz-pdf-favwaloc https://coub.com/stories/2195612-siddhant-star-one-serial-episodes https://coub.com/stories/2207596-link-dhating-naach-full-video-download-720p https://coub.com/stories/2204131-facefilter3profullcrackidm-exclusive
amieva (Wednesday, 29 December 2021 11:03)
a018c9ed18 . https://wakelet.com/wake/NavdYi6n0uadF0jIOO6U4 https://wakelet.com/wake/wjg98P946joOZil-_MiTZ https://wakelet.com/wake/VZHD0wzH5PjhBKiOe9Nw2 https://wakelet.com/wake/VWEyxHeLze0s-5dpDeyP0 https://wakelet.com/wake/li1_JPIP_VY029unSF9qD https://wakelet.com/wake/lGLIYgDZCSqzXGEmBU0ZU https://wakelet.com/wake/aKG9Nuc6qpEe9X40V8nDy https://wakelet.com/wake/UIe057K5B9Kc8c6jNhTzj https://wakelet.com/wake/V0avK9FexoKh84rdaVd13 https://wakelet.com/wake/mq7PoZyqSCJdtlFIgJo0B https://wakelet.com/wake/P0kGJ48d3RPZOTNiPqcEO https://wakelet.com/wake/u8wJOCHORgk_lTtw56hI- https://wakelet.com/wake/5w2UEXgIl_jUq9tfSvSdP https://wakelet.com/wake/vq0AVI01hkIErnoAcyKB3 https://wakelet.com/wake/zI9Fzzpzst5WNhNFIGPzq https://wakelet.com/wake/qb-ysQ56JSE6BayWX4wuo https://wakelet.com/wake/aWKgPumrjCnyOStovshxr https://wakelet.com/wake/iuA5O8W0e9IWyeSINVCOz https://wakelet.com/wake/Qa8OIh8QAGOMyzRkhkrxF https://wakelet.com/wake/in9oI-7jvabQJp2sPLXYa https://wakelet.com/wake/SWdf1Vuq99XxgKLw4hCDV https://wakelet.com/wake/a-WdWVD7-ZiDnJVQlGKX9 https://wakelet.com/wake/vd1kXbKr_DO2w_H1Khawk https://wakelet.com/wake/UTO5w7x969FdaSC5fbxl1 https://wakelet.com/wake/w79r9MlPLXN9lV2ov2k5g https://wakelet.com/wake/UIKpu2zupgtxn2CSENZJT https://wakelet.com/wake/96g-ETXHDZQufkaaXKR7E https://wakelet.com/wake/FnJZjOAVQbDbTquObh169 https://wakelet.com/wake/VnVLrY5DXpXyGITQftexu https://wakelet.com/wake/03P67u-sro42RV30_01uS
ophrtheon (Wednesday, 29 December 2021 11:17)
a018c9ed18 . https://wakelet.com/wake/ePbbBZ0qyBcoNMGJ4LpQ5 https://wakelet.com/wake/Q2xvFmDI7f_QNOErX_R6P https://wakelet.com/wake/pm3O0KbefeM0roJGRUigH https://wakelet.com/wake/F-mNyV0D8LtB4WeHtVcgd https://wakelet.com/wake/IM5FSpTJnz_3cU69o5oDw https://wakelet.com/wake/d9jm5CtvCYALFYs8SGYzr https://wakelet.com/wake/aHYw0wWhz_x_QRHU9SLZZ https://wakelet.com/wake/mzy4Km-ekZPXXPxEuenKO https://wakelet.com/wake/WMAfe_OCyHWaqTBnAzXI2 https://wakelet.com/wake/pyQIu7LpXiMp4BICXHiFC https://wakelet.com/wake/iuS07OeYQWNRh7jpvGLGA https://wakelet.com/wake/Qz5Wu6pgaf2f8P_EoLzM_ https://wakelet.com/wake/Ai5xKhTDyrM3P8dssh4K5 https://wakelet.com/wake/n6yZZOWGlEBno_vLj8vHt https://wakelet.com/wake/J5vFQG_AygghB3Z75YzuJ https://wakelet.com/wake/p7OIGcCJOpgpg09meFn22 https://wakelet.com/wake/wJPPSavoBd22yKtK2BkPZ https://wakelet.com/wake/j3tMgVcc3-AiwnRf38ZTx https://wakelet.com/wake/Djk43eOFizWSp78horXUE https://wakelet.com/wake/bj9Rm1wiY3PvnMX-ikJ7A https://wakelet.com/wake/9URyXhd8K9pAu-3ET8BgZ https://wakelet.com/wake/XGf-rBbgDQODzMWZX21kT https://wakelet.com/wake/ApFCybLnXfhS5Te_H_pfq https://wakelet.com/wake/_9eEZqx5U_8BHCj0WnInu https://wakelet.com/wake/Yhi9WBFfs81D2incSSPOU https://wakelet.com/wake/6OV-uvdaL5ZEQEPU8CXYj https://wakelet.com/wake/QtHlrqjzAAHDegC3ssb3D https://wakelet.com/wake/Sz7doqn0ebmWvu6OmwiiL https://wakelet.com/wake/JzH4jI04F2iruxuJhMIRn https://wakelet.com/wake/0Siuj0PH6J5Oi4v74pIkn
glorybel (Thursday, 30 December 2021 19:25)
2656432625 . https://wakelet.com/wake/Q7XZbWoSNeYjMceS9_mOZ https://wakelet.com/wake/kBUeims5cNK70Ynch4xi3 https://wakelet.com/wake/w9ZMVwQRS0OlQHYfp82Ra https://wakelet.com/wake/i19RuyADsF0DTm9tLUKIe https://wakelet.com/wake/dApsAGicjW_W576Sez3YT https://wakelet.com/wake/oDDsQrjDa17VCvnXQJRXT https://wakelet.com/wake/yyHfaXBIO6tojhsICpBPV https://wakelet.com/wake/yARP6oZAhLe9riZRhefv5 https://wakelet.com/wake/0vuTz6MF3SNmU4Zu4lZ7d https://wakelet.com/wake/3XNuNvhzczpxHMDUC4Rpt https://wakelet.com/wake/CGB7S6aK0Ngkqn5FJHnWN https://wakelet.com/wake/WYQn1JATGc9SgM9HRmGc1 https://wakelet.com/wake/lhOMUyTakaUsSdrKphU5V https://wakelet.com/wake/EO4xgWA_dpHQ03bKUdEF3 https://wakelet.com/wake/tYWrkLQ0AojgUMENgCEzD https://wakelet.com/wake/AgOnycVtcVclh7f_eYTKn https://wakelet.com/wake/O8C6J0MoJjCsRCzqMC6Ty https://wakelet.com/wake/yqBeTWNcPe6tUjvCFfBQU https://wakelet.com/wake/Ew2WjIlQP5-tKX1tbH2z- https://wakelet.com/wake/S8rseev5izP3do5w-edUe https://wakelet.com/wake/gW9q0rhWkbZm8oQVlIax3 https://wakelet.com/wake/3okZZKs-SMwehqg9-BPWR https://wakelet.com/wake/gkvRj57o0-jWn7KbD6r4M https://wakelet.com/wake/z9JFW7gL0WbPReLsvtm9s https://wakelet.com/wake/vchdX3OHSzGNpjfb19JCV https://wakelet.com/wake/li_f83Zu3nTGCaxa15x3y https://wakelet.com/wake/j9pneG1K-Y7DSWpkY67gm https://wakelet.com/wake/5YqiF7b4LCA1zuwhfDcBE https://wakelet.com/wake/aXFv2HQo_NhG_S-XIrw8a https://wakelet.com/wake/LrOO-K2YayBQhwpY5x8TK
olivyranay (Thursday, 30 December 2021 20:07)
2656432625 . https://wakelet.com/wake/EyQIcsK1Bx-iWVC1DyawA https://wakelet.com/wake/YpzOHl-yoXymJZ940mMCG https://wakelet.com/wake/1wqgn08SCArZq3ei79HA1 https://wakelet.com/wake/b7YEjH7txv507W7fn0JIm https://wakelet.com/wake/2N3CbMp7TIlz56bUAofCv https://wakelet.com/wake/_9s7d4RBE1rXVicsHi6AF https://wakelet.com/wake/QS1PlyoAvEEth5JVKm-lv https://wakelet.com/wake/GE_WgYzUmqNYt-g0PEV7t https://wakelet.com/wake/UcT9L92F8AH11GdbYB-V2 https://wakelet.com/wake/--HTFdcx4tmPall_1Wna1 https://wakelet.com/wake/qeNiT2XrGHLO6Fzr6kuPa https://wakelet.com/wake/ca1PztzHgbrdzvq3MrnFg https://wakelet.com/wake/FjztLh__mlmMHItfazFiv https://wakelet.com/wake/ETFgIsZ8FzWjgqD0zgwDJ https://wakelet.com/wake/p9CR3klzt1W5HsZnbiidk https://wakelet.com/wake/Fo7CVit-I2ptsNYc8qLd5 https://wakelet.com/wake/YZF__Pyp-ygs1Rpbrvht8 https://wakelet.com/wake/N74lImBBTAvHUrqxSuysn https://wakelet.com/wake/sDF37Q02ocnbC1hhAnB1T https://wakelet.com/wake/hBmUVyaejCQfHGqfFpJwC https://wakelet.com/wake/QAk1sBTVChK7LxmHaCvD6 https://wakelet.com/wake/XZsYAUTR9KYXSbP_20YWN https://wakelet.com/wake/Wnv2l3Ms0Uz-qHxrcgbsB https://wakelet.com/wake/IOuP0kG5QY4AOEvsgY3aA https://wakelet.com/wake/afkGnNtQjH5-gft-wrrtR https://wakelet.com/wake/Ile0z1p_eZzXQG5Q0v4Xk https://wakelet.com/wake/SFBQGOdsjhJd3Kd-vOtPF https://wakelet.com/wake/UDhLHGIvixief_eUcTbuF https://wakelet.com/wake/FFAtmSpzVmLdpucjHRXWp https://wakelet.com/wake/83q5EfazZweG5lM66uobx
jarefath (Thursday, 30 December 2021 20:35)
2656432625 . https://wakelet.com/wake/uWz4lfTABooiLCTiTz6Jn https://wakelet.com/wake/MeziLH33VxMv6wWYhJh-s https://wakelet.com/wake/XiYp_DOqYRhkjDSKEyFes https://wakelet.com/wake/Y8oKeduSTf8GeQwX7zAX4 https://wakelet.com/wake/Z2j2j7z8DG5aOIdIzg7fI https://wakelet.com/wake/r8rTLrKWaXfWvGPGr0dfM https://wakelet.com/wake/qUys6-JvLw4Iq-CzRezfE https://wakelet.com/wake/2rqzxdNc1mViyROB0pA6p https://wakelet.com/wake/bFz1bdd3EF-66eUBU84oK https://wakelet.com/wake/G8t3ha4e3-leWLDYqYIEE https://wakelet.com/wake/Fr_0h1Khy0W08bKy4yvHG https://wakelet.com/wake/j_pgpK8tg-NDZ1UAI2a4r https://wakelet.com/wake/hX1hAAr9UrVeT3mjfxeGc https://wakelet.com/wake/U6ZgDUWY9Ui_3_FNePni8 https://wakelet.com/wake/5G8-dgdyg8EWUxn4Q-EDt https://wakelet.com/wake/lmEe0QLNr8SO8PPLNOEwB https://wakelet.com/wake/ctDFhWbJjZb4Gjvfixv12 https://wakelet.com/wake/GhL1aKYBBbrG-GacnsP2w https://wakelet.com/wake/7l09kgt1QdpDTSBVFoijg https://wakelet.com/wake/1VNaU10s2ma7w40_cUDvp https://wakelet.com/wake/q9rBExR_tgccK_5V88Jo6 https://wakelet.com/wake/yH6CgKwQP5hPcY5Fh6ZLc https://wakelet.com/wake/FTddDJpT0c250bB3wCXzu https://wakelet.com/wake/wPy5rsxDo9kaFYfMlHPul https://wakelet.com/wake/Iqnfbamx2oQ7jEchqE2CH https://wakelet.com/wake/7xzWBUWqqjvQoFHCRpqMS https://wakelet.com/wake/fDb2qBWVKlk_DQhpTjzNw https://wakelet.com/wake/XU9KgiJfuV4kOZKVARooR https://wakelet.com/wake/9mQCQZPPBTOovRr7lDLGT https://wakelet.com/wake/LKJjnq5ItK-eFmm0KMJJW
lawrkad (Saturday, 01 January 2022 14:37)
c639bd25c8 . https://wakelet.com/wake/ixOYK2dkNralm39n_GJn0 https://wakelet.com/wake/mqZA8hTegFO7w7GU2Ct4L https://wakelet.com/wake/vmtTCfonryAVJWY9sPDuO https://wakelet.com/wake/v6yR3_Wr2C4IXiD6DdYmN https://wakelet.com/wake/YnAsSIWU-n0gDNShL3u2e https://wakelet.com/wake/Gw7Zy5pPawXGqawcW96Pb https://wakelet.com/wake/Ustr3JCeCDueu6h8SCbwn https://wakelet.com/wake/tWBEXsylWYfeKCEg_gaEN https://wakelet.com/wake/9Wb6p5xZ8J_PmzFMtPfiK https://wakelet.com/wake/z80rj7N7wRSqgq1qx3FXo https://wakelet.com/wake/WoiNtkj7fFcYim0gdgJkC https://wakelet.com/wake/etQNcVM4GvWrAao8Yi--- https://wakelet.com/wake/jERabSV2zsgYMprYkejDr https://wakelet.com/wake/zOLGFrODvQzCiXGAoKglv https://wakelet.com/wake/mvI1fM8IumEsBrwtHT_sV https://wakelet.com/wake/ewo3DdNOs0KL0EHQOyNa5 https://wakelet.com/wake/5bQ0Vr51-K5Zxb2SW6PVe https://wakelet.com/wake/xNLUPRgA_SwX1lLDNPd09 https://wakelet.com/wake/fe4cSVCdPPIYEq20N_pyf https://wakelet.com/wake/8hxLl-4bm_wPXVkDAGSAv https://wakelet.com/wake/qlpvR0YF7CnqpTO7Z5Fos https://wakelet.com/wake/qkVU8VmYnQn7fPyEKKHaC https://wakelet.com/wake/idpTMvQInPqtGC89aHdr0 https://wakelet.com/wake/wljy8PFPCm6PvKj-ce4UA https://wakelet.com/wake/JYJfBOq_Bxqgausd8m5a_ https://wakelet.com/wake/VgalcKNbxmd5wVxMt6Lud https://wakelet.com/wake/pyP7qDEGs8jh7ucx97lIL https://wakelet.com/wake/5p0ga5oFYdQ9nSJNonaPE https://wakelet.com/wake/CZsNEIm4kCwVC9rEAGAj9 https://wakelet.com/wake/9kRzA8xLYVONgET8_RhLe
jalaphyll (Saturday, 01 January 2022 17:43)
c639bd25c8 . https://wakelet.com/wake/SDVPrQAauyJhtY6k1Gzux https://wakelet.com/wake/pNKSEt8-dlTnWqEYfg1z9 https://wakelet.com/wake/Lx9SwhlQ3lxLWeLZ2gXht https://wakelet.com/wake/wSuAe_P12IkfgmtI0v0kw https://wakelet.com/wake/vlsg5pE2Ax4cVpeOYk_5B https://wakelet.com/wake/BByTtDh39Hf1i_jov0QzY https://wakelet.com/wake/s_n0mzKWxDuTTptb2gmMH https://wakelet.com/wake/P3u46etrcfEngmkYAvzfG https://wakelet.com/wake/UefMUqEjeC7B2GZruskEm https://wakelet.com/wake/xZLbZ0rMtL7uXwwp1fjqa https://wakelet.com/wake/7R9-Od_gOxuJ8C30a9mg4 https://wakelet.com/wake/XhNGdoHlej6rNNcPJu-Wd https://wakelet.com/wake/6Z72RO6rTM0wT3FAPirKK https://wakelet.com/wake/WJH3AZexZbjjuM2vannkK https://wakelet.com/wake/m0NRt4JFlcErHedSIYrEV https://wakelet.com/wake/cXdol9-zcXR5pVXkorccM https://wakelet.com/wake/JLX1czezhRMzVTYsqdnZt https://wakelet.com/wake/hkvhraTA0Ba-mL_7PyZbc https://wakelet.com/wake/3l38DBpVOkzD1pfBWim-w https://wakelet.com/wake/WqlIXI87u1ey809MJW2h6 https://wakelet.com/wake/pkQTckt4afauCdav2rBpI https://wakelet.com/wake/bcjZCj0cE23DfJIq-dcDH https://wakelet.com/wake/XznrJ7XiK1aXcsu4KlojN https://wakelet.com/wake/q-94M9_J_XR0wUycNPj6E https://wakelet.com/wake/4iEl-lXmbtHNQXliMhYL4 https://wakelet.com/wake/XuLcoOlK3vzYUsKx6m_9g https://wakelet.com/wake/c-neiZjJcHGC2g_zr--iD https://wakelet.com/wake/Un2eEFraF9ZlSnnS9ld4m https://wakelet.com/wake/WTAmSi-dtcTK9Nv6yn1L2 https://wakelet.com/wake/l9_CmsJERfKWTQJ6dUc0i
penmigold (Saturday, 01 January 2022 17:48)
c639bd25c8 . https://wakelet.com/wake/mYRtrxgMsSLFigY-xvCGo https://wakelet.com/wake/wekJATMA135cPM80D7nah https://wakelet.com/wake/RT3QTHaXI1uPnuGlSMpCd https://wakelet.com/wake/bRb7cIajP6ixPGhvncy3c https://wakelet.com/wake/tfNBD2n9WDXP8mUNHxhgr https://wakelet.com/wake/ayKp1vovQMGGX5Pw1GosV https://wakelet.com/wake/OhfugzJI5IspE3vG4SAwa https://wakelet.com/wake/89cyyLVCHRfV6g5JWE_4K https://wakelet.com/wake/h1Ddd_VrBzfOr2dCgr2QC https://wakelet.com/wake/AsiOTSaE54kCkO4RkPKKu https://wakelet.com/wake/7RutRZODM6e8hqqVP_0a1 https://wakelet.com/wake/-xRYd8MAp24gpLEFkw0VY https://wakelet.com/wake/ZzXYzyXU-c93-PZb4wTpn https://wakelet.com/wake/RnRiD9mkbgYg0zwYgHYus https://wakelet.com/wake/AY50nvnyny__ZoOjpTZze https://wakelet.com/wake/Kfz_K_ka-x6GGd-B27-Nu https://wakelet.com/wake/0KAW8hEYlDrPBmWm2LG_L https://wakelet.com/wake/j1LoFJQLyds5T1ZF1WD7e https://wakelet.com/wake/f4C2ImDoxhylL345m9Hws https://wakelet.com/wake/pXj8P44c74vSHqMpvO6NV https://wakelet.com/wake/tkinYOVUUdb0LV9FdoOTo https://wakelet.com/wake/LaqF45KhCTpcTn8cAYAKu https://wakelet.com/wake/xa9tV4DnNv3CI_d4eOJKK https://wakelet.com/wake/wMunuwGb_2TUWWbncRSE8 https://wakelet.com/wake/lxTt_4DZQYXp7hi9RY8d3 https://wakelet.com/wake/8-i7XzFql50jxhZ57PxaS https://wakelet.com/wake/WxsNLxz5mzOLeJl-OeGng https://wakelet.com/wake/4Cn4_O-1caJQF-fVLqwbM https://wakelet.com/wake/YcIqwB4Y2PHuCTb-t8ny3 https://wakelet.com/wake/B0AwMu5ecOgGwGswA4bBr
bribened (Sunday, 02 January 2022 16:30)
097872bdb3 . https://wakelet.com/wake/lYX0X0WUE42PMfQE9LbKR https://wakelet.com/wake/Y-MkeDqGoqie8U8dIF4Xu https://wakelet.com/wake/1AHq5wQ-T7XaRmBdDNa29 https://wakelet.com/wake/crXCTD2xUBoWCiSR-lTOI https://wakelet.com/wake/eZyMY3EMfNuwTk1I1cMqV https://wakelet.com/wake/Xa-bjcY4a-9rYmwq7m-SZ https://wakelet.com/wake/UA9q7RWzZAiuLXIyIPU7W https://wakelet.com/wake/OvMLcJmhAYJkwplRI1tkt https://wakelet.com/wake/3SWR19ISz3dfNwaapTiRR https://wakelet.com/wake/n34d0qh0g5BoJv4xdMaEA https://wakelet.com/wake/oq7PPyOMOA_dwoAt8KiPP https://wakelet.com/wake/XfvlUuLMnosjcwmQeYxEo https://wakelet.com/wake/rf4WRYarB0OWLxSJOm3YM https://wakelet.com/wake/P9PZDcaXMT87VLBixn4hO https://wakelet.com/wake/0Uz5poFAuxcqQoRVeS6Oy https://wakelet.com/wake/ZefyyPbeknIgt6Jx-Zzz_ https://wakelet.com/wake/BrKPANby-rpnUUqvpG8Du https://wakelet.com/wake/4EE8oWmfMkkLwSu1uZfQ5 https://wakelet.com/wake/n5OdPM3M75tFRkXWhdFxy https://wakelet.com/wake/Ak-dnbJ-eayMFSzYgn8h_ https://wakelet.com/wake/kekB_H9AilYDXlEm6GPMu https://wakelet.com/wake/HyqGX7Phe-N-Pa6thv_GD https://wakelet.com/wake/kF0-9IG26eZIsqZkxwDOk https://wakelet.com/wake/cwLc0LsXeBPeEvTsGbxDQ https://wakelet.com/wake/KdCFxi0KO1Mjc7AeljZJf https://wakelet.com/wake/g1vyMAWDJiXkSNaMa6_po https://wakelet.com/wake/KuaahaHYllMexrOqedvqA https://wakelet.com/wake/X2d3n5TsFtAA_EPdhHMTV https://wakelet.com/wake/ayODQkBl5XrtqqnOyTUUc https://wakelet.com/wake/RRQQlqpNqtn8PHeXK8pNF
zeracmoray (Sunday, 02 January 2022 18:44)
097872bdb3 . https://wakelet.com/wake/lKbMoJ7QQVAI_CEwgMaQz https://wakelet.com/wake/KP5uDqFwr9MnthH38I8Zn https://wakelet.com/wake/6y-Ke_r7m7PLI0uHSg99h https://wakelet.com/wake/BBPwiHeGtanpL28ma2Ml0 https://wakelet.com/wake/bhf0vAIyrEIhhcnpjr4u7 https://wakelet.com/wake/R47eF-pXeDWGiLLtk3zXF https://wakelet.com/wake/uOQEBQEr1u5xdOcpgp4z7 https://wakelet.com/wake/ttRQ_huIRuOk99Wa13WNX https://wakelet.com/wake/QRrL6-r1Hpkp9Fp6Zx_x9 https://wakelet.com/wake/1j7kbRFqeXYXwyntzWQk_ https://wakelet.com/wake/w4DbfHROiWpvM5JxG0y-R https://wakelet.com/wake/usi42sEv1z4bSG7E4mQNc https://wakelet.com/wake/193SqqHy89pL82shmukKS https://wakelet.com/wake/uwK4gqAkU0O5g7b0XejrP https://wakelet.com/wake/Mwn4kOfGnzGpIm1NX2i5_ https://wakelet.com/wake/BRn6hBrdBhw3QuZVdNzq6 https://wakelet.com/wake/LQOeHgj16p41vj6PZmHFz https://wakelet.com/wake/MYMyPhbNyWGz8kJfwhzq5 https://wakelet.com/wake/Qb3SDkNGpRRvMCRNVmfhy https://wakelet.com/wake/DbnlxjsJhWol3iHv3iGvI https://wakelet.com/wake/F7fkQRIlbF_wHxvZgRXSo https://wakelet.com/wake/OhF2e0WSMJbeZgI-0Wd9h https://wakelet.com/wake/1zaRuHGshUbdYMDXR0-Jt https://wakelet.com/wake/nLbbPVEV24gVRQc3JSv47 https://wakelet.com/wake/CkGFFBRI0hgGgeD1uZEmR https://wakelet.com/wake/5u6tnE0DxOkGqTe3pQ0LV https://wakelet.com/wake/rg_fm7yjO9ivopBdAO71b https://wakelet.com/wake/vKi_4hF9wJCIj_7PdZkT5 https://wakelet.com/wake/3_tas2BaAmuij10xH4Qv4 https://wakelet.com/wake/rOhyk97mqC-szGJRu1RAG
supplkee (Sunday, 02 January 2022 18:59)
097872bdb3 . https://wakelet.com/wake/EWHgPjnMX1bUs8m2jHL5E https://wakelet.com/wake/f24Fhae8h_PgoF9ZpzcEg https://wakelet.com/wake/_uY20mVGlgkTLfMkv-JP8 https://wakelet.com/wake/Xo_i8xhwql_oS4SIfsIqG https://wakelet.com/wake/dUKIcvslGjeaWxDjz_HSH https://wakelet.com/wake/BIhKxiMl8rFN12IZqbLCn https://wakelet.com/wake/OkIXQPKe3fxnls8R8jI1G https://wakelet.com/wake/5xO_JHSVUPPUdvXMxkFeC https://wakelet.com/wake/xQhK2xGPaltlQc28R-J-K https://wakelet.com/wake/q0QX3atUPmbYkEqMcaq9s https://wakelet.com/wake/hXZPtgIYz42HFKfLinlxD https://wakelet.com/wake/avn6nJUKPpKIutKFxc3BO https://wakelet.com/wake/PInWCSGHwWt6qi3uNhGBQ https://wakelet.com/wake/Tm-LD15llSpZm_9HBjwFm https://wakelet.com/wake/hXtHjDA9lCObtQiB1wTD2 https://wakelet.com/wake/qX7wjlcAANwFjT5ARBLRX https://wakelet.com/wake/pf235LDm6xzRjCe8pp7-7 https://wakelet.com/wake/SAZzsoVMU4KI-fmiRYt4C https://wakelet.com/wake/xHQfuCVPxvnxdnyWjADRx https://wakelet.com/wake/uqtW2x8j0PovjHQQdkSA- https://wakelet.com/wake/XlyZzY85hCDDevm2te9dr https://wakelet.com/wake/LlFS0ZQpRknLjD3Bnsjot https://wakelet.com/wake/OSiPRS5Is85MJsrObvang https://wakelet.com/wake/0TQb6kMbiQFKmHYeD6h4F https://wakelet.com/wake/N6q4yfldqxrUH8cmy6SIn https://wakelet.com/wake/-6f-TLXDVnxfTmregWQCf https://wakelet.com/wake/bEmRmNDkNpz_RCqbHFkpU https://wakelet.com/wake/hMvx15mJM0LesPU3bGhGV https://wakelet.com/wake/pwG_bBIW02d7T73i7PQUq https://wakelet.com/wake/pAkswL5WAOhHTdzjlytlF
jankalan (Tuesday, 04 January 2022 15:21)
7814c6310a . https://wakelet.com/wake/iPoVxjdnkOJkkLu9mfCCc https://wakelet.com/wake/OTUnzWhrFU62oUqYbwiE6 https://wakelet.com/wake/LLqR4EH3uoYVTSYJWvAl3 https://wakelet.com/wake/DOOANp8CJne5LGKfBiFjK https://wakelet.com/wake/JxywRvz4JaZTV7n0eE_Ld https://wakelet.com/wake/TLpSgnrWG3glrF4uP2hG8 https://wakelet.com/wake/nj_axYsIaK_4JVpoTg6rM https://wakelet.com/wake/cTQVsyZnmNi0jEOUeikre https://wakelet.com/wake/3XPjwLUNdBA2m2EdXXAsd https://wakelet.com/wake/OsFjlEhFcHAOUxD4UT-8s https://wakelet.com/wake/z9SnwLIGKAhR8Ud5LP1bC https://wakelet.com/wake/k25OIrKrCc5BKulEssvw1 https://wakelet.com/wake/tGeyQ-CwK0pOwFAOo2yio https://wakelet.com/wake/OSHtd7ri47Wi1AbuI_G9B https://wakelet.com/wake/BI8pZBUO43DMzhx37d5Yo https://wakelet.com/wake/2YJbcHmHRTFDpaQVzK_kH https://wakelet.com/wake/VLu2h7j7a11DoVfy2B-3n https://wakelet.com/wake/z8F-IWo-9R__35WqVuE2g https://wakelet.com/wake/9ic5FzPIVQxYOeYsdQ6Tb https://wakelet.com/wake/6lV2JlBLQRiH9A-NHvtuJ https://wakelet.com/wake/xmPrH9RaqGzJuftcRJ81z https://wakelet.com/wake/sMBjDjrFhKMKJ2Giwun4J https://wakelet.com/wake/IwfphhMJCnxkehVHD9wA_ https://wakelet.com/wake/LNMMU8cgKv0i3KJlBS94C https://wakelet.com/wake/wq2DlbBVv4mJJC4beIUyZ https://wakelet.com/wake/kUOYXolyAX8xbPpC9by64 https://wakelet.com/wake/Nj8PTWohH3tThMO8INFQf https://wakelet.com/wake/tJ5EF6_dLUtXqhuCe7kbC https://wakelet.com/wake/mkUaI-peIrNbcux4zN7L6 https://wakelet.com/wake/6V18lFjdYMGckub6UGVmX
oldensygf (Tuesday, 04 January 2022 16:41)
7814c6310a . https://wakelet.com/wake/MlXnUA_7da_oOVVtlGgaQ https://wakelet.com/wake/oPvzCsd9nDS8V9JmX_oxL https://wakelet.com/wake/ukAELJ1_ZWZfLI_qR1zq3 https://wakelet.com/wake/tgurDMz7iW8iO109yZ4LG https://wakelet.com/wake/vV7o_AVGPz8svO8THKA9M https://wakelet.com/wake/sdQGySLWUaK4GRV8ysdJm https://wakelet.com/wake/Q5pz0uBIiIacE_WKh_sa3 https://wakelet.com/wake/TqQWPj6_IMh17ZgvkD0Fa https://wakelet.com/wake/RMu2cT8gqI60lSWPisInY https://wakelet.com/wake/BoNfv21xnMxW6jAZuY7Mz https://wakelet.com/wake/787W7QW1F6SB7M7gHvVnb https://wakelet.com/wake/CJ9wtFGt4ekxPuvLnwkP0 https://wakelet.com/wake/E8kcbewdiNT1_i7guOliU https://wakelet.com/wake/s2SVPRi4W_ohbT2ZKOOud https://wakelet.com/wake/LtP4G2dSnSqLu1rVMtqCA https://wakelet.com/wake/qr_Ihl2OhqxlAO0n4mKFP https://wakelet.com/wake/g8iKl4BggVQGQ8NtNcRpS https://wakelet.com/wake/rg-91SP8HncvPIKORJ7Sx https://wakelet.com/wake/rFwFpMGDFeZ0pK3Ec5FRz https://wakelet.com/wake/XheL4_u4D-7VCXFDBVT12 https://wakelet.com/wake/4Xsyk-AXJqomI5Z5dm4DV https://wakelet.com/wake/6DgEYE0DMC1tGS9yi5d1Z https://wakelet.com/wake/qOfvLt0f3B9SSAaxOtOkg https://wakelet.com/wake/zWcy-woHPxLd_ODmFPoM1 https://wakelet.com/wake/24aygSgK02lMMb5LbFDts https://wakelet.com/wake/VoIrwUp6PXvp9wESuS-GO https://wakelet.com/wake/cCUUUw2G65QqztaZNtlBH https://wakelet.com/wake/pUslSr32hauGfJDq8Fgvx https://wakelet.com/wake/maQmUNgr-qyJZXEiJdofs https://wakelet.com/wake/I9yzU7Zyvvu0jWy69osIW
athnem (Tuesday, 04 January 2022 16:54)
7814c6310a . https://wakelet.com/wake/B6ncfAzLL2MyxKgpDP01n https://wakelet.com/wake/Qj3arFJicktE680dOvSIC https://wakelet.com/wake/4GX-cGkIz84MeY74riNrA https://wakelet.com/wake/bl8aNhe3IjyKx8ca7TuKd https://wakelet.com/wake/IhNI_V01fBW_euBJP4XVU https://wakelet.com/wake/vvahabLXDiL8SaIc1h_BX https://wakelet.com/wake/kLf9_K8Tc0vuSbJvELV2f https://wakelet.com/wake/c-tvN5czKsM7nMW76xuV8 https://wakelet.com/wake/YV_AnpOYn_g6RLc9Y6IpQ https://wakelet.com/wake/JH48tT6nqUWHcZmZ7tQn9 https://wakelet.com/wake/-3kO0nL7aBqeyCO3Wgte9 https://wakelet.com/wake/jfnOUDvk9lJpJYmPvcB0e https://wakelet.com/wake/Ve_uhR0o8SO38zH2xURFi https://wakelet.com/wake/I6JHj2hmEcfHH3tkSkVmL https://wakelet.com/wake/bPEZlFiLKw9gRnxltyMd6 https://wakelet.com/wake/0UpCAxj8_1ZBM75-hzWkU https://wakelet.com/wake/s1k5OWOzISTJqVwvw6eIx https://wakelet.com/wake/lJFfVhMq6HqWL4aT4gdJZ https://wakelet.com/wake/TuYsS-l_32mMHU-mH8ZWj https://wakelet.com/wake/byM-IiYTnj8A6mLYN1hul https://wakelet.com/wake/Y4LDQs6Ko7Zps7FJ9g1I5 https://wakelet.com/wake/Gs1_wz85P8AJtgbbc9PHj https://wakelet.com/wake/cviYbRuV0xxporTCenKgI https://wakelet.com/wake/vNWGz39ZZzngHOWMjsZVp https://wakelet.com/wake/IrHdoRCq2XpQie1pI_CuE https://wakelet.com/wake/_xmioX3LRr5tefSopjgPv https://wakelet.com/wake/bjXsRQ0XfSqRVUIyoMul0 https://wakelet.com/wake/s6EBKZqMRtAIhODVDP9Y- https://wakelet.com/wake/o-N0iT2wcYjsl7b-AL8ID https://wakelet.com/wake/K978i_2wkoy7s6M_dm1aN
faysadel (Wednesday, 05 January 2022 18:05)
97d3633e1c . https://coub.com/stories/2277757-of-mobile-computing-by-asoke-k-talukder-epub-mardelsa https://coub.com/stories/2310304-sakvithi-ranasinghe-english-pack-free-37-wisaadarc https://coub.com/stories/2302183-keoma-torrent-ita-full https://coub.com/stories/2342430-coat-hello-ryo https://coub.com/stories/2296506-hd-online-player-gunday-movie-in-hindi-download-720p-best https://coub.com/stories/2256157-visualizer-3d-okm-free-download-crack-keygen-serial-rar-18-dorichr https://coub.com/stories/2295878-better-irip-2-1-keygen-torrent https://coub.com/stories/2318149-schoolboy-q-oxymoron-itunes-deluxe-edition-zip-rosaltan https://coub.com/stories/2324398-kung-fu-panda-3-english-hot-full-movie-hd-free-download-mp4 https://coub.com/stories/2296207-rosy-2-__top__-full-movie-download-720p-movies https://coub.com/stories/2290014-exclusive-peter-lerangis-seven-wonders-epub-download-sites https://coub.com/stories/2293130-ncss-pass-14-free-crack-the-53https-scoutmails-com-index301-php-k-ncss-pass-14-free-crack-the-53 https://coub.com/stories/2254126-admintool-usb-4-samsung-recovery-solution-4-0-0-3-updated-melodary https://coub.com/stories/2337003-amra-korbo-joy-song-download-high-quality https://coub.com/stories/2303016-top-pthc-beauty-cumshot-3yo-this-rocks-pedo-child-toddler-incest-2yo-4yo-5yo-6yo-7yo-8yo https://coub.com/stories/2260299-dikkenek-version-longue-torrent-jalfaust https://coub.com/stories/2264800-demon-king-resurrection-full-movie-download-in-italian-upd https://coub.com/stories/2303757-free-passengers-english-movie-1-english-dubbed-free-download https://coub.com/stories/2267146-risk701crackpalisadedtsuitekeygen-imogwyna https://coub.com/stories/2326539-extra-quality-sun-river-systems-heatseek-gold-1-4-2-0-portable https://coub.com/stories/2341706-f-secure-freedome-vpn-v2-25-5766-repack-install https://coub.com/stories/2274697-link-download-kumpulan-teka-teki-silang-pdf-portable https://coub.com/stories/2252884-link-download-topcon-link-7-5 https://coub.com/stories/2251802-ff-fight-desire-22-thircom https://coub.com/stories/2283256-writing-arguments-a-rhetoric-with-readings-10th-edition-books-pdf-file-kamahcha https://coub.com/stories/2306126-disk-drill-professional-2-0-0-339-portable-3-7-934-macos https://coub.com/stories/2305863-upd-ben-howard-every-kingdom-album-download-zip-celebrity-soldados-k https://coub.com/stories/2266246-t-ara-jewelry-box-album-link-download-zip https://coub.com/stories/2257466-repack-tender-buttons-by-broadcast-zip https://coub.com/stories/2268232-buongiorno-papa-2013-italian-utorrent
emmmag (Wednesday, 05 January 2022 18:59)
97d3633e1c . https://coub.com/stories/2307398-university-of-ghana-sex-scandal-videos-giustjarvi https://coub.com/stories/2269688-full-exclusive-istripper-v1-2-175-nsfw https://coub.com/stories/2325787-blu-jai-ho-tamil-movies-1080p-torrent https://coub.com/stories/2324107-como-activar-windows-server-2012-release-candidate-datacenter-build-8400-41-97-work https://coub.com/stories/2303209-repack-episode-1-1-720p-torrent https://coub.com/stories/2313645-upd-manual-matematica-clasa-10-burtea-pdf-30 https://coub.com/stories/2270428-link-cod-black-ops-2-mac-free-download https://coub.com/stories/2277691-ho-sakta-hai-hd-720p-download-link https://coub.com/stories/2296454-repack-anymp4-dvd-creator-7-2-36-crack-full-review https://coub.com/stories/2307424-leveld-767-fsx-crack-torrentl-jezgirt https://coub.com/stories/2260270-best-star-wars-battlefront-ii-crack-english-hack-offline https://coub.com/stories/2274204-vir2-instruments-mojo-horn-section-1-2-1-kontaktl https://coub.com/stories/2255205-free-download-convertir-pdf-en-cbr-mac-for-android-dayshbic https://coub.com/stories/2313463-repack-lunch-box-movie-download-720p-67 https://coub.com/stories/2270086-link-pakistani-movie-sakhi-badsha-punjabi-sultan-rahi-rar https://coub.com/stories/2305360-managerial-economics-and-business-strategy-7e-pdf-zip-adds-1 https://coub.com/stories/2287128-cerita-bokep-pdf https://coub.com/stories/2252397-full-utorrent-download-kung-fu-panda-2-113 https://coub.com/stories/2253548-free-the-meaning-of-life-ed-klemke-pdf-download https://coub.com/stories/2255958-cracked-conch-republic-electronics-part-1-mini-case-solution-rar https://coub.com/stories/2291037-game-of-thrones-season-1-torrent-sadykger https://coub.com/stories/2261720-serial-lotto-sorcerer-v7-chucgabel https://coub.com/stories/2259987-korean-song-the-open-karnam-star-mp3-songs-free-download-repack https://coub.com/stories/2321479-zelscope-key-serial-keygen-12-manflave https://coub.com/stories/2291145-crackwindev1732et64bits-full https://coub.com/stories/2335447-better-act-of-valor-movie-script-pdf https://coub.com/stories/2299082-verified-the-hate-story-4-hindi-free-download https://coub.com/stories/2305145-the-tempests-of-first-love-2010-720p-hdtv-x264-ngb https://coub.com/stories/2312835-varnakazhchakal-malayalam-movie-mp3-song-download-tendmary https://coub.com/stories/2326159-resetter-canon-ip-2700-2770-service-tool-v1074exerar
sakaferg (Wednesday, 05 January 2022 19:04)
97d3633e1c . https://coub.com/stories/2317436-repack-download-iptv-forkplayer-smart-quembquynt https://coub.com/stories/2260513-crack-gsa-auto-website-submitter-4-91-best https://coub.com/stories/2315689-apple-launcher-for-windows-10-better https://coub.com/stories/2266740-__exclusive__-reallola-issue-2-v004-dashal https://coub.com/stories/2267713-overdeveloped-amateurs-tina-32ee-jumping-rope-halsak https://coub.com/stories/2344299-insane-2-crack-by-irfan-doggar-anakari https://coub.com/stories/2277907-fatso-hd-mp4-movies-in-hindi-dubbed-free-download-__top__ https://coub.com/stories/2309415-regasirea-puterii-interioare-pdf https://coub.com/stories/2271517-glow-hockey-2-iphone-android-better https://coub.com/stories/2327095-pedroelpollolapeliculadvdripespaollatino2-__hot__ https://coub.com/stories/2306371-pinball-fx3-torrent-download-xforce-keygen-enchaeloui https://coub.com/stories/2253039-apex-true-dbgrid-pro-6-0-gratis-payverb https://coub.com/stories/2271761-digimon-masters-online-bot-rar-illanwayne https://coub.com/stories/2260110-free-grid-autosport-high-res-texture-pack-addon-hi2u-hack-offline https://coub.com/stories/2309716-red-hat-enterprise-linux-5-installation-number-keygen-generator-best https://coub.com/stories/2294061-statistics-for-management-pdf-2021 https://coub.com/stories/2288049-instrucciones-lavadora-aspes-la-142-zacdarn https://coub.com/stories/2251819-windows-9-extreme-edition-iso-torrent-download-hot https://coub.com/stories/2325769-ferres-masque-2-returns-torrent-_hot_ https://coub.com/stories/2253784-starry-night-pro-plus-7-6-3 https://coub.com/stories/2338301-_verified_-main-rahoon-ya-na-rahoon-full-movie-free-download https://coub.com/stories/2306251-solucionario-calculo-1-victor-chungara-pdf-46-bentudesi https://coub.com/stories/2266729-neethaneenponvasanthammoviedownloaddvdriptorrent-free https://coub.com/stories/2346007-manual-acls-pdf-descargar-charmayn https://coub.com/stories/2254797-john-prine-lost-dogs-and-mixed-blessings-full-exclusive-album-zip https://coub.com/stories/2259630-rope-bondage-rebirth-full-hot-21 https://coub.com/stories/2291471-driver-genius-18-0-0-161-crack-pro-2018-with-license-key-life-time-manyfshi https://coub.com/stories/2315333-melty-blood-act-cadenza-ver-b-nocd-patch-15-kaeblu https://coub.com/stories/2328336-teamviewer-premium-v-11-0-62308-multilingual-portable-2020-repack https://coub.com/stories/2325740-exclusive-joe-bar-team-8-pdf-27
yediebles (Thursday, 06 January 2022 13:28)
cda82931fd . https://wakelet.com/wake/rQA9NmQTF-HiRDbO--vqy https://wakelet.com/wake/yaplASN5x8C-AkYjmfvVM https://wakelet.com/wake/Q0ZnAqmcIEd8d1pTRPJ6_ https://wakelet.com/wake/MDlouPuaqWKu6LEFRWE8d https://wakelet.com/wake/yTebpDYJzXdFrxkiGxIDK https://wakelet.com/wake/8B81DYoX5MH1JUSB_5-QX https://wakelet.com/wake/OIWvnV-JLYrdcGi_DnFgM https://wakelet.com/wake/fbt93M8A82TPDqIxQJjsO https://wakelet.com/wake/XR0HViI7T9B3zRpNJm0jR https://wakelet.com/wake/Q6tP2MO-ypRxAdvXxrTLo https://wakelet.com/wake/cTzi64GCU3Ecp-Quytl21 https://wakelet.com/wake/DArC5K1qHjCEo1qlMA3_Y https://wakelet.com/wake/_nwEl2e27Dm92PgUJTvIc https://wakelet.com/wake/1Vq3z7GVpZUq1eLUYG1su https://wakelet.com/wake/K5SOfqIq2NM7jxvliv-rZ https://wakelet.com/wake/AnZvON6AZcUsgBeL3IHdh https://wakelet.com/wake/7viTZlckwt-kLQmzCncPN https://wakelet.com/wake/8F_QzissI3MlS_3g1ROnz https://wakelet.com/wake/9k7s_xaD5TAIRF_cNhemV https://wakelet.com/wake/aq31wnKGcNGJzZmTcBkzp https://wakelet.com/wake/PlP1BRO3mpnb6rrGZ5bN8 https://wakelet.com/wake/zUIHcCYWfCbj7y90wyYw4 https://wakelet.com/wake/K_e2z8K4YebRT6etZrWX- https://wakelet.com/wake/-AumI2FET5sYbB2W1FvJC https://wakelet.com/wake/M44mJCG1oMLJB40ey6Vvr https://wakelet.com/wake/uNlyF7kvnKcS5Hpj_flEV https://wakelet.com/wake/HpJeFadmvvHEVcgUhyLB8 https://wakelet.com/wake/u7vC_N6MUO3a_WdU3iB7d https://wakelet.com/wake/18W0WUJfeaPEs_21WF9Q1 https://wakelet.com/wake/ehH3pTpzEKE24W04V89dB
langsveko (Thursday, 06 January 2022 13:52)
5bd35b6a26 . https://middcallzako.sokuhou.wiki/d/[PDF] Chrysalis, A Short Story: A Journey To Independence https://dockcomraelar.memo.wiki/d/HOT! Full Version Minitab 15 12 .rar Download License 32 Patch https://seesaawiki.jp/cmabdescgolfsbor/d/Stapanulinelelor2onlinesubtitrat720ptv https://seesaawiki.jp/daleciga/d/Free Download Film Semi Asia Terbaik https://seesaawiki.jp/sterlessdonti/d/1398 Ddm 019 Software Download https://seesaawiki.jp/mieconsreetfia/d/32bit Rugby 2001 License Utorrent Pc ^NEW^ https://vioumisspepit.memo.wiki/d/Netfabb Lt 2019 32 Bit Crack Torrent Download https://seesaawiki.jp/geschholezo/d/Intericad T6.epub https://forftugisty.sokuhou.wiki/d/The Rapture - Echoes (2003) FLAC EAC https://agannogfue.game-info.wiki/d/Hindi Movies Download 720p Bhabhi Pedia https://seesaawiki.jp/ciospetamquo/d/S Om Shanti Om Free !!EXCLUSIVE!! Rip Movies Movies Rip https://seesaawiki.jp/tranesconnest/d/Luxonix Purity Vst 64 Bits.99 https://seesaawiki.jp/iminacspys/d/Brown Eyed Girl Lisa Kleypas Sites Utorrent (epub) Full Ebook Rar yanahlyl https://seesaawiki.jp/neycommobo/d/!!BETTER!! Vasya Diag Keygen File Key 32 Full Version Pc https://seesaawiki.jp/wsonfertefoot/d/TrojanKiller2159 Iso Full Windows Keygen Torrent File 32 [EXCLUSIVE] https://seesaawiki.jp/peddbusego/d/How To Stop Smoking Crack Cold Turkey https://seesaawiki.jp/igvanobeach/d/Download Captain America: Civil War (English) Subtitle Indonesia 3gp https://seesaawiki.jp/mouberthorthe/d/Iso Uhou Luna Nights Hack 32 License Full Windows Download Serial [REPACK] https://seesaawiki.jp/zeigebmyaha/d/Mkv K Ll Light Fac Dts Dts Watch Online 1080p fernchrc https://seesaawiki.jp/clocvidani/d/Yamicsoft Utorrent X64 ((FULL)) Cracked Zip https://frannenase.game-info.wiki/d/Alphaplugins Engraver Iii Crack Cocaine https://seesaawiki.jp/waylerase/d/Sathru Samhara Vel Pathigam Pdf 25 https://seesaawiki.jp/myapeworda/d/Fania Todas Las Estrellas Bamboleo FLAC https://eslatihar.game-info.wiki/d/Cabela\\\\\\\\\\\\'s Big Game Hunter Pro Hunts Download Tpb https://seesaawiki.jp/velpmaccnestsec/d/Hd Brazzers Live 17 2011 1080p X264 Avi Movies Video https://missatibel.chronicle.wiki/d/Gib Mir Den Wodka Anuschka Download https://siminica.playing.wiki/d/The Purge Anarchy 1080p Kickass https://lagepibu.chronicle.wiki/d/Geosoft Oasis Montaj 75 Latest .rar Nulled 32 belllach https://seesaawiki.jp/portpemensong/d/Cara Download Video Youtube Lewat Komputer https://seesaawiki.jp/flatunsnowyn/d/Video Bokep Bupati Tenggarong Rita 3gp
brevol (Thursday, 06 January 2022 13:53)
cda82931fd . https://wakelet.com/wake/aT2Ujlnf2Tm3T9bUkNwCk https://wakelet.com/wake/z5ckwYht58_qC-GrPa6KO https://wakelet.com/wake/jOCY8sg4sghaWk7AoGQ6U https://wakelet.com/wake/xwLfJAvCsvPxKd_kbrGud https://wakelet.com/wake/LiEIWy1150sFS8pHb43lm https://wakelet.com/wake/D3dta-upMlvMATzFangFN https://wakelet.com/wake/PeBxq5t4AEzVmtBkKHeEe https://wakelet.com/wake/gxke9bqlZQJf4PBxeuBYJ https://wakelet.com/wake/RYPRFowDGbQoKNe_Uf9gG https://wakelet.com/wake/TwBq8PnBcfgQXuqTqfXxd https://wakelet.com/wake/wzMHMt-a7ysORSO9BSQal https://wakelet.com/wake/lYZqqX44ieDDXDFhGHrpi https://wakelet.com/wake/N8rIGkJxqIV1wijjWlfSy https://wakelet.com/wake/jcsDZeipS88tuzD--hiLX https://wakelet.com/wake/kY5yJUEuCqGBb19BWXQe6 https://wakelet.com/wake/Tbw99Oa6wVrfm_R9madjL https://wakelet.com/wake/Iy3NFWaQVHzB2nQz0jzQW https://wakelet.com/wake/rTnqxTmHmZlRVnNiTMaz5 https://wakelet.com/wake/Csfp71uoSXZnMHy_aGGzz https://wakelet.com/wake/AG_YxojpG0g6-1gaibhzV https://wakelet.com/wake/3JqdIFuaYf_yPBS-YGmnR https://wakelet.com/wake/YnxH5zYSc-2GxAVNKQDAN https://wakelet.com/wake/epTrCkjDh9-HnzmUhnzGp https://wakelet.com/wake/dx0Kcon_poxc0jjgZx2Ae https://wakelet.com/wake/CSZSQ62fx3W1XNwxwlQxO https://wakelet.com/wake/Gnb8qZlUD18Dj2igkQtFx https://wakelet.com/wake/VP4blXFohIlWSYGaca_42 https://wakelet.com/wake/-ni7rJERxhPQn3xbEn4Ox https://wakelet.com/wake/6ncIiK_qncggRuQXgAMZN https://wakelet.com/wake/7rhkw6BUWIyQgU1W3q5g3
ameryilee (Thursday, 06 January 2022 14:14)
9e85a7f49b . https://wakelet.com/wake/BxOd_KPirgsZOMnBCFa8U https://wakelet.com/wake/R4-Too9yEaA6R1seIKeDx https://wakelet.com/wake/FUlGpVmLBryOdkklwVot_ https://wakelet.com/wake/vIkR7AVmUzmtBf63Rw8OX https://wakelet.com/wake/Ro-9MI8TMNb8DfduWCXxG https://wakelet.com/wake/5qXsOaAzEwNEeXWuyoNpp https://wakelet.com/wake/EazC7N0OGx6q_wWihEXuH https://wakelet.com/wake/5eHLQyyDlvfgmTAhcLsZo https://wakelet.com/wake/eY3KGGlX1GlakbN_XnsYw https://wakelet.com/wake/3uIbaRbXYY8Qp57dWpyay https://wakelet.com/wake/WC7dxOsSHr6U2ULRT0PX1 https://wakelet.com/wake/pUnEcUXwgnSmr0hOdXwyq https://wakelet.com/wake/45v625oXpbXpRyb5zJCdO https://wakelet.com/wake/WRZSDG6bzYqWqUw800ant https://wakelet.com/wake/4SOYBgIfz5S7Jg1q32j4Q https://wakelet.com/wake/znnKa5rlkjpISMHVyVImw https://wakelet.com/wake/XTKM_x8M9ZtW23-EoL4OO https://wakelet.com/wake/FWxEFsdfVV2lGQB4mYc8X https://wakelet.com/wake/oX3qJQt4On4sefF4yix7F https://wakelet.com/wake/FjDUe_ntfBTJk2hUqCVT8 https://wakelet.com/wake/Jy2iCL3d8jO5029Y8dVZu https://wakelet.com/wake/_LxMvjH1whnj9kbnTN1ik https://wakelet.com/wake/VWhrwDLpFxyQEbfZeZNOe https://wakelet.com/wake/19GR6vCQeR_-UuG_5Z2VN https://wakelet.com/wake/KOFwB6J53bCoTW4bM_Ppn https://wakelet.com/wake/DlZrRv8e85qM6SnQEH06B https://wakelet.com/wake/KrqFMu0kBUUj7WfCzQpIX https://wakelet.com/wake/SliDeMjZHEe8VoWQldQxh https://wakelet.com/wake/P2ceQ4MRlphPu9nADPebD https://wakelet.com/wake/QOA7hm8-RDmveXiHX-FOU
aloflap (Thursday, 06 January 2022 14:40)
9e85a7f49b . https://wakelet.com/wake/lCkGdU757vMxe8XbXDi4X https://wakelet.com/wake/pxdl4zFnCEtmMgrfXihcW https://wakelet.com/wake/ZVh_4yHSnKpEumvWWmddV https://wakelet.com/wake/KTyuBnE5ek1o8PMlVHN5H https://wakelet.com/wake/8qa1b21F9zPuY-NBwtDmt https://wakelet.com/wake/qQYib6OUGlYclqeS8GFuK https://wakelet.com/wake/F0ILoKa5Q6I1DnSc92WgW https://wakelet.com/wake/JLW3_oI6bcNKxipk4PIfn https://wakelet.com/wake/XfJM0CkM0NEk8fZNCyiZ3 https://wakelet.com/wake/PF09MblUOH_UCrOTsoL02 https://wakelet.com/wake/hgDeZ0zFfrwgb3MrJuOUe https://wakelet.com/wake/zhyfBGsLqnn7TclbxRwNW https://wakelet.com/wake/QmSHU_ijjAA52zpXyk6hS https://wakelet.com/wake/4-ahbnks8RE-Kxqa11a8q https://wakelet.com/wake/nBWWnwKoqPnZnu7wzh-SW https://wakelet.com/wake/R-_HlrGNc1heo5wdCSjCC https://wakelet.com/wake/Gm3U62Fp_cbN_q1b51joR https://wakelet.com/wake/QXaYnzzZwVZQWlHKnFbep https://wakelet.com/wake/7g28PSYjy1GtZ8dM9uiTR https://wakelet.com/wake/xof1Q2uFipXwquu3sUwLK https://wakelet.com/wake/3kCKmrIZj9MX293BTw60f https://wakelet.com/wake/v8IEzEHPX3k4IYbndb3OZ https://wakelet.com/wake/CH54OT5jjPDmG4WO3kRjY https://wakelet.com/wake/X2AiF4pS4zlfYfCE3M5MQ https://wakelet.com/wake/n7obbv8ZifLYSkZxF58oJ https://wakelet.com/wake/jf5VvWNtdkG6MEWg_0FVO https://wakelet.com/wake/qw4Ymeb-M6u7O40sGNnw5 https://wakelet.com/wake/wGFl1AnMzHPGcH0PQhk-Z https://wakelet.com/wake/bvHvxBD1Wa2z46a35V7AG https://wakelet.com/wake/06JqnQT07ffoGELCLXkgM
demvola (Thursday, 06 January 2022)
cda82931fd . https://wakelet.com/wake/7jB4y6DEG1ICi-fQeOSHR https://wakelet.com/wake/IBD-jFpdHFKIHWSEH2otH https://wakelet.com/wake/4YFVzN0fQBRmNshq3B0lF https://wakelet.com/wake/8MBLDzEUSpJNJCMCBGmA_ https://wakelet.com/wake/2iMEomeAFldyGEwTz4Aor https://wakelet.com/wake/n1stnZW1tm98d2xYXcC0R https://wakelet.com/wake/ws0Hwi-2kcGfshmVHXb-L https://wakelet.com/wake/_ecpniAhEsrOg9SCSYNo2 https://wakelet.com/wake/n-BqKeaVaUXHM2XPNWvMO https://wakelet.com/wake/baJJGlH_Zjt-RIae9s-Zm https://wakelet.com/wake/Hf8pP7VQJL5g9h28-LcEp https://wakelet.com/wake/EpGRsaqWRMSEM03RtaliM https://wakelet.com/wake/OfbxO2bAKIb9NaLc2BuuO https://wakelet.com/wake/PHndeVLunkfaS7lR6VNiY https://wakelet.com/wake/d6MzUmvlNF9Zxoyy0_zee https://wakelet.com/wake/eU5IOSepLBZqCOJloq_lL https://wakelet.com/wake/ZkSYD6g-ZMt-04xtSeIVB https://wakelet.com/wake/CKhsGXfe1LMUjnvAfqi0x https://wakelet.com/wake/eCM0CuU9Ux5XyBSyvMpCb https://wakelet.com/wake/HBB7pt9IlXbZYsokr4UKx https://wakelet.com/wake/5WP4ms71UpC8n-i4pxxhD https://wakelet.com/wake/WqneOzQcX4X0rpyJmgGbX https://wakelet.com/wake/sSYFMsaF7jLVpaSvwxBoF https://wakelet.com/wake/1s9SCUOlt3dtnDWkBUnFD https://wakelet.com/wake/C7_0_0Dbw3nfNtymg2qID https://wakelet.com/wake/9K2dz8hOYpYI-TIOzoDSP https://wakelet.com/wake/xlRbmnVHscbrWwRNw2lZV https://wakelet.com/wake/cMfoT23VWwhh61242Adiy https://wakelet.com/wake/UfE4XnVGOeP9-KIFZSDMj https://wakelet.com/wake/1oZFnuzxtpljBD2PfaDeP
morthas (Thursday, 06 January 2022 18:05)
5a5407e688 . https://trello.com/c/eJjI31e4/30-cucm-862-keygen-crackedl https://trello.com/c/yKkFHcUG/17-patched-gfifaxmakerforexchangesmtp-v-143-x32x64-unlimited-lice-pausanso https://trello.com/c/WyAIKOXv/15-3-mp3-mera-pehla-pehla-pyaar-movie-720p-free-link-download https://trello.com/c/UYuU0Bjf/40-xiaomi-mi-5-and-mi-5-plus-specs-and-prices-outed-by-a-retailer-free https://trello.com/c/bSkS9U40/24-kuch-kuch-hota-hai-movie-in-tamil-download-hdl-top https://trello.com/c/DzHIrC0K/25-neverne-bebe-uzmi-boje-mp3-free-upd-download https://trello.com/c/DGlIpFYW/38-fix-fkk-mit-jenny-und-lore-am-strandmkvrar-analyse-siedler-fern https://trello.com/c/gKiRtabx/60-new-jhansi-rani-lakshmi-bai-history-in-tamil-pdf-18 https://trello.com/c/A3JgdmyJ/30-baba-ramsa-peer-tamil-book-download-kafletakki https://trello.com/c/Eqz8AShm/30-homework-hotline-number-nashville-tn-derrimariu https://trello.com/c/THGV7zqq/31-lorenzo-lowe-vs-ethan-axel-andrews-full https://trello.com/c/RsbV46F5/50-mw3-config-mp-cfg-download-exclusive https://trello.com/c/GvPEb41F/28-link-sports-press-pro-nulled-theme https://trello.com/c/N8INCXc5/43-scaricare-simulation-mechanical-2008-generatore-di-chiavi-32-bits-italiano-chadlflory https://trello.com/c/UIig8vlg/28-upd-doctor-strange-english-full-movies-720p https://trello.com/c/hFus9zZz/33-shop-n-spree-shopping-paradise-torrent-download-portable-editionl-fix https://trello.com/c/R87r0IgW/13-link-urbicadseguridadysaludcrack https://trello.com/c/VA2hLTD9/21-verified-wprssaggregatorfeedtopostnulledthemek https://trello.com/c/HKKwYatk/30-mega-samples-vol-82-top https://trello.com/c/ACphJAxb/26-iclass-9696x-pvr-upgrade-s9f4a126-doreen-gehaltskonto https://trello.com/c/7kcpMtXw/14-2021-hack-dvbviewer-pro-4810 https://trello.com/c/xInls7Cz/34-bairi-piya-mp3-top-download https://trello.com/c/kzhmI2lr/27-placebo-we-come-in-pieces-torrent-exclusive https://trello.com/c/Jty7wzhJ/33-top-tekken-mugen-characters https://trello.com/c/Wmh8nMHn/25-train-simulator-south-wales-coastal-route-add-on-torrent-download-torrent-full-new https://trello.com/c/fQgkjo2D/8-project-cars-2-update-v2-0-0-1-codex-quenngay https://trello.com/c/qNeWQRp6/10-acdsee-photo-studio-ultimate-2019-v121-build-1656-x64-keygen-new https://trello.com/c/MuabIG7Z/58-windows-7-alienware-blue-edition-x64-eng-jul2013-39-gb-fix https://trello.com/c/EephpHmm/39-free-martin-yan-lemon-chicken-recipe https://trello.com/c/vHNal4TM/50-heroescompleteseries720ptorrent-whytndel
allithan (Thursday, 06 January 2022 21:24)
9e85a7f49b . https://wakelet.com/wake/1TtbShyyD3i7J8eFdJCbC https://wakelet.com/wake/9ItHHtxZIxGV_DhW2Ji7B https://wakelet.com/wake/65dUee8Ng5qEnNAFFcZLf https://wakelet.com/wake/bPboEdAkQpzvoZNBI4HLB https://wakelet.com/wake/1Z5ro0uJUZK7BxCIGyq7u https://wakelet.com/wake/em782T2xd_RfBEwOs858n https://wakelet.com/wake/ssMg-wig97H1IN7juY7C9 https://wakelet.com/wake/AzbNPeCy935KE6-TyBVM5 https://wakelet.com/wake/S3aCTawuVTc6k2LHmGl1M https://wakelet.com/wake/aWyErAZ_c6PH4OzU5cdUE https://wakelet.com/wake/8zftRJFDEnexyaZXVaJLv https://wakelet.com/wake/OJj1eDqyeIB3RGJJUZDJn https://wakelet.com/wake/tBpyHPJDRtFIkdY2w_hWC https://wakelet.com/wake/0JBCvf9TRhfVfYxJKfLzh https://wakelet.com/wake/aKX99xnhYdWwjqbdzKbRD https://wakelet.com/wake/djPSb6o4LMXvx5uzqj7lD https://wakelet.com/wake/f9wNeSr6EkHlWkwNEv9R5 https://wakelet.com/wake/hWE3DciT6XTspXowYdg40 https://wakelet.com/wake/NgjltCr39qsagNHQVmoVY https://wakelet.com/wake/g5JeYjT6ZyGoBcRSglPyF https://wakelet.com/wake/TBKwIvX33DQBkr-16G2Ss https://wakelet.com/wake/EVQBYhlkid6DAQBYCzHrr https://wakelet.com/wake/xqAm8V_RM2qSkHwoI8ElV https://wakelet.com/wake/41idG0C0nOX7qRpaPUhpv https://wakelet.com/wake/zYJ7-5pJNseKaffoUp2s5 https://wakelet.com/wake/vamAXZloLA3KzAmO2X3PH https://wakelet.com/wake/KC4qib3hxHqkeqNt2jclO https://wakelet.com/wake/JH7H89nixCZOzDYiPQJjS https://wakelet.com/wake/PoOnW2TGnTYLjPEolcKDU https://wakelet.com/wake/bodyRL_EicikVZdauSvrD
vanelen (Thursday, 06 January 2022 22:32)
5a5407e688 . https://trello.com/c/25aBsvDg/35-movie-hd-1080p-blu-ray-full-piku-aletam https://trello.com/c/XWx8HQTM/21-backspin-billiards-deluxe-pool-full-install-version https://trello.com/c/Cts6CeN0/14-proteus-79-full-download-exclusive https://trello.com/c/K5wcMn9L/22-virtual-breadboard-415exe-rar https://trello.com/c/vbzGMZ6h/32-microwave-circuit-design-a-practical-approach-using-ads https://trello.com/c/RqIMHzyC/42-total-war-shogun-2-fall-of-the-samurai-crack-only-reloaded-hot-stavbiana https://trello.com/c/VPo7xGWb/15-mercruiser-engine-block-serial-number-verbjorg https://trello.com/c/RJh74d3X/34-the-king-of-fighters-97-98-apk-download-free-obb-data-peateclary https://trello.com/c/IH1ecw4F/72-top-kumakuma-custom-pose-evolution-download-no-crack https://trello.com/c/0M5lRcNp/43-cummins-insite-7-x-keygen-rar-full-verified https://trello.com/c/2jNg0M3Y/47-the-fourth-body-2004-subtitle-indonesiarar https://trello.com/c/DJ0jWc4i/26-better-the-adventures-of-tintin-secret-of-the-unicorn-flt-serial-key https://trello.com/c/cT0auuiq/21-mergea330200projectopenskywilcobyspaikrar-hot https://trello.com/c/If2tVHv4/35-panchlait-bengali-movie-full-download-torrent-cracked https://trello.com/c/2WVZBrGa/51-serialac3toolspro121rar-giawest https://trello.com/c/y33t7WXh/30-il-figurino-di-moda-pdf-free-download-olyenspar https://trello.com/c/JuDgUyUb/31-top-the-sims-4-reloaded-update-4-no-origin-crack-better-mr-dj-repack https://trello.com/c/bJefvnhj/24-the-dil-ka-rishta-full-movie-in-hindi-hd-1080p-fix-download https://trello.com/c/5HAAFiN0/27-smartsteam141rar-top https://trello.com/c/qpv61iip/57-livro-breaking-free-new-fisk-pdf-to-25l https://trello.com/c/zJP9YgyV/16-serif-movieplus-x5-starter-edition-1006-serial-new https://trello.com/c/kYETv972/22-download-sql-server-2012-enterprise-edition-torrent-taitrei https://trello.com/c/7Ymaa9PN/22-securitytaskmanagerserialkeygen-updated https://trello.com/c/0m91wISS/21-idm-637-crack-build-3-final-patch-2020-pre-activated-ileyjame https://trello.com/c/5LBZvQDi/12-720p-hd-italian-movie-download-install https://trello.com/c/DOi3xxli/33-hot-xforce-keygen-for-revit-2009 https://trello.com/c/gA94zPR6/20-extra-quality-maxon-cinema-4d-studio-r19024-crack https://trello.com/c/Xsk8VYL4/29-ruijie-plotter-driversepub https://trello.com/c/XNRXOYZp/14-better-santa-claus-in-trouble-again-2-download-full https://trello.com/c/ND3TJ76F/25-kamasutra-sinhala-book-pdf-free-downloadl-new
salnemue (Thursday, 06 January 2022 23:08)
5a5407e688 . https://trello.com/c/ZlQ619xb/29-bushido-electro-ghetto-verified-full-album-zip https://trello.com/c/vMPbbkKW/54-xzone-reactor-application-vip-crack-carros https://trello.com/c/o9Uv4ks8/26-l-automne-du-patriarche-pdf-15-new https://trello.com/c/Saga12ln/14-quake-mission-pack-1-scourge-of-armagon-free-download-crack-link-with-full-game https://trello.com/c/0UDpgfz3/20-install-happy-toys-activation-code-and-serial-key https://trello.com/c/xqivHBAD/16-patched-skyrimgtx-mods-downloadl https://trello.com/c/RCaoCYUK/22-exclusive-actualcoach-2-32-keygen-link https://trello.com/c/obP2ZMNE/23-download-patched-windows-8-evolution-64-bit-iso https://trello.com/c/t4z3u0nh/33-better-human-zbuilder-plugin-for-3ds-max-2010-2012 https://trello.com/c/F1SF8Y2c/27-free-ms-visual-studio-6-enterprise-edition-rar https://trello.com/c/snC2ofuD/30-ul-top https://trello.com/c/574C2Md2/19-valhalla-vintage-verb-mac-crack-bentlale https://trello.com/c/WrgEWbGl/21-ezmix-amps-pack-torrent https://trello.com/c/PySJKgqN/32-epubor-all-drm-removal-1017820-multilingual https://trello.com/c/kwU9y3g6/38-free-psp-worm-v30rar https://trello.com/c/VY0oUS3V/36-spss-version-200-for-windows-analysis-without-anguish-pdf-11 https://trello.com/c/F8aaE6Yb/38-accordi-per-mandolino-18pdf-desmuschyl https://trello.com/c/5fbR0LMn/58-link-kayswitch-for-example-mp3-14 https://trello.com/c/nq15jAZQ/24-re4-dt-skossino-v2-exe-cherbalin https://trello.com/c/c4LQWYY4/73-new-lumix-superzoom-fotoschule-fz1000-pdf-download https://trello.com/c/gSyx3yuA/19-collins-english-for-life-speaking-b1-pdfl https://trello.com/c/PBRUH4UG/20-my-daughter-seo-young-full-episode-tagalog-version-yo-finlemon https://trello.com/c/BJx9e0In/52-leawo-prof-media-serial-key https://trello.com/c/DxbV8gqB/18-new-bajatey-raho-movie-free-download-hd https://trello.com/c/6kN2drQc/47-attack-on-titan-psp-game-exclusive https://trello.com/c/8R7EBqPt/23-fundamentals-of-renewable-energy-processes-pdf-verified-free-download https://trello.com/c/INdF0Qgj/77-adobe-flash-player-for-mac-os-sierra-1012 https://trello.com/c/m1htbP2u/29-seethamma-vakitlo-sirimalle-chettu-english-subtitles-free-download-in-srt-file-format-2021 https://trello.com/c/onHsXQ9O/25-ship-sinking-simulator-free-full-110-patched https://trello.com/c/ExXBUZIm/45-top-carlson-civil-suite-2015-crack
sallau (Sunday, 09 January 2022 18:29)
4bd6d2c6ca . https://wakelet.com/wake/u-7BIJkOjmHIkVhpVQiB1 https://wakelet.com/wake/z460JRB6YKjpOcEKb9NXT https://wakelet.com/wake/7ZLhxKggnYkP8cIY_DMGl https://wakelet.com/wake/WgpNcWQptqPCXSbwnLgkQ https://wakelet.com/wake/9VwrwFJDNgi4wpaRh4a9n https://wakelet.com/wake/R-8P2OPXnvbEVrfBx9-p9 https://wakelet.com/wake/q-Xh4TidnIdjcAK9JQl6W https://wakelet.com/wake/VuGF7VqjcwaMringmwZlI https://wakelet.com/wake/Rn0K5L-HCH9RRu_sjjoXh https://wakelet.com/wake/rOifT33D3Tnibnj3q8omM https://wakelet.com/wake/SUOop8yUhx8bWx1a7IkGQ https://wakelet.com/wake/p06qx1mVzT1qgmmvHcHMx https://wakelet.com/wake/kAWEgMtrTqFEtpyRssRty https://wakelet.com/wake/Skcq8DjVVuk7tYP8Y6bQK https://wakelet.com/wake/s6FlIzU6ecEWDIktzkm7l https://wakelet.com/wake/IGnHKJYVklZE3MRFerQtj https://wakelet.com/wake/kGaW7f1_3PDEnySxNK4fO https://wakelet.com/wake/Ihea-zv2X0Pzgj02swJcm https://wakelet.com/wake/Inrwdwct9JHHLwDDi6i9O https://wakelet.com/wake/VbWbXcSWH_DYI4yI0XkZ9 https://wakelet.com/wake/KNw1WzKYa_0OEXw_PJqKG https://wakelet.com/wake/WPqD6XLLS5aKnKkFO4Eyz https://wakelet.com/wake/lcklmLPZENHIRfdGd2i8b https://wakelet.com/wake/189J6fgAFmveXHgN9hJ7T https://wakelet.com/wake/RsZ_8OctMVg4v-P3D2_1c https://wakelet.com/wake/l8qJkcXAL7nuT4FbSMcms https://wakelet.com/wake/uYxH8fV58vPbzaGvpx83d https://wakelet.com/wake/-1Aulka6seMNtHrCLktHD https://wakelet.com/wake/nJ2gq9aRzLq2b-Yf2qZsO https://wakelet.com/wake/SNNrYt0oXCgPuady5tpsm
statami (Sunday, 09 January 2022 19:26)
4bd6d2c6ca . https://wakelet.com/wake/szdx_2kJK-N3Q54IdX4qo https://wakelet.com/wake/K9VG1QDsSLjWqDGkIPzYP https://wakelet.com/wake/iSPeBPIgFzXUv3wQ8L0kQ https://wakelet.com/wake/rQN1_xvz7Q65vJ5gQzaLM https://wakelet.com/wake/Uzwy4kUhoPqyUNdFXP0bS https://wakelet.com/wake/QYnpt8f7amlN3_3Skn4un https://wakelet.com/wake/AGfw2lMNL9XQlAn8oM0z1 https://wakelet.com/wake/CUGip7IeuSAZBdIgklufe https://wakelet.com/wake/F5c7hvFCc5ArrOsfZwQgN https://wakelet.com/wake/rI-qsze_DBoq3BHzgC_k6 https://wakelet.com/wake/jWmmSI3VpGytegk9YmRjW https://wakelet.com/wake/4X6w3gTs3di1mxPoNVnV1 https://wakelet.com/wake/zY0rf8UmkngqZmdmJEekZ https://wakelet.com/wake/EB7RR4assfXI4iEPGNidh https://wakelet.com/wake/z7aADXsypmyTCGMoY0m2P https://wakelet.com/wake/4nAYb8U_ymzEuxMec2-fY https://wakelet.com/wake/Wu5MKMo2viYL2hYmYMahW https://wakelet.com/wake/t6oGpp698J47m5pY324Tb https://wakelet.com/wake/4Ly8oDI8KXqaELsaEVspM https://wakelet.com/wake/CYbTMb61F1Dq4E48yLAfs https://wakelet.com/wake/qfWokHJ-ZDFsQiyZGBR1b https://wakelet.com/wake/w9Sb8vdG0ADPTTs5kmhCu https://wakelet.com/wake/ULuvgSPjcdfa4yakgOm40 https://wakelet.com/wake/KilHLTlZmAUxT1xXFLYyB https://wakelet.com/wake/RUaBN4MZSKAZoDqc04BB- https://wakelet.com/wake/Fml9elXUxK72ldjHfoD_o https://wakelet.com/wake/JnGXGFbpNI37PUtWRxZB4 https://wakelet.com/wake/waOhRr30E-8BDAiojRcnS https://wakelet.com/wake/e7D4dsEmw_a_at057Wsw3 https://wakelet.com/wake/gOTe5F8LTRKGqbYI6hcx4
vladilee (Sunday, 09 January 2022 19:28)
4bd6d2c6ca . https://wakelet.com/wake/JJfz9t0tyUw6JeLwfgO9N https://wakelet.com/wake/fwCDCPgpB4qxaUVyZ__JL https://wakelet.com/wake/ggdKIicphPwPCRcoxrkcv https://wakelet.com/wake/RvNdXB0n_68ud4osBVEW2 https://wakelet.com/wake/RBDOepEDtemCawWUBsGcy https://wakelet.com/wake/7EN1dI1sZKLs7YLxHbhhB https://wakelet.com/wake/WFYm1ruQF55OfnEPDM3wA https://wakelet.com/wake/lkf2lgatP4rz3zP8iY2Y7 https://wakelet.com/wake/wZzKfgwH3jlUQBkRkc8Us https://wakelet.com/wake/GxDkEbw8uvrKimfIfX55T https://wakelet.com/wake/IfyOJ2ETmd3xJ6HFs9hbP https://wakelet.com/wake/GkBqYzVw3QzdAhbT-lhZQ https://wakelet.com/wake/NF4CHpKatVxNWZiNC05VI https://wakelet.com/wake/3a3ehzaw7KBh-mmaf5U2Z https://wakelet.com/wake/3ij9v3O58NRJ3tQ8fFJWA https://wakelet.com/wake/eiIU6Ckiwkh6Zvhk2AkzZ https://wakelet.com/wake/_IjvthVLeYfcuLsJBJLpn https://wakelet.com/wake/Rd16_RhUgCiSX82sHg--o https://wakelet.com/wake/rO89cgKAt6DcEzsKAiAw7 https://wakelet.com/wake/vj9Vjz1ZsBENyqTrwzxqr https://wakelet.com/wake/mFJl5S9aR4FU5AAYP8QhP https://wakelet.com/wake/t39yHPnmhQ04jDavLnUDL https://wakelet.com/wake/aJiSdi4VGBSJB4Jo_UX4y https://wakelet.com/wake/zQwrSahQuOYbtBCKv8BiO https://wakelet.com/wake/cV-XSWEa9Afkp1GTftn1r https://wakelet.com/wake/IlSOFKBp0OZNwW7PZf3xU https://wakelet.com/wake/CENUAJ2GRLp5z94XQqeaS https://wakelet.com/wake/q6XHEnAcws2vxgfJjMB8F https://wakelet.com/wake/vY8u_tMkZQSHZMnyftqDF https://wakelet.com/wake/AbhCGWpBibp73hpSg1zep
desquam (Tuesday, 11 January 2022 16:25)
desquam 1641938820 https://wakelet.com/wake/y4aAWJKT_pX5pxS6sJWkU
https://wakelet.com/wake/QJ4ThwmfGSgHxkpjsdmyY
https://wakelet.com/wake/kdJDSTOlv2Yq64NoZG9-a
https://wakelet.com/wake/gtH2AuMgH8kz863Ww3rBU
https://wakelet.com/wake/P84cB41U01JL706RPLsMS
https://wakelet.com/wake/dUcN2XwwwPjg-IwhBdPs9
https://wakelet.com/wake/FtzERguYSIJoC8rAe0Mvf
https://wakelet.com/wake/H7q4R5_bZc9rKn518G4zd
https://wakelet.com/wake/4c-h5tX6iLUtHgjLW4EFF
https://wakelet.com/wake/y9QRG89PeeF8xm1CgNBh4
https://wakelet.com/wake/WwABOs1vzhc7t3oi2410p
https://wakelet.com/wake/VKZ5u3bgwEGKnigwpMj-u
https://wakelet.com/wake/YweXR1Ov03FHX61gbQQXt
https://wakelet.com/wake/h52hN-IAwuFtioohAMriB
https://wakelet.com/wake/R5UvRQIxt1wLwPgjz6dj7
https://wakelet.com/wake/ODeU_AuAFHiBHvSVZ3LRH
https://wakelet.com/wake/V7YKtXo3ci_FI9OMxijLF
https://wakelet.com/wake/gD2Kf-uzyCjml8JZgEf2J
https://wakelet.com/wake/cIj2j06YU2UqmpsFnOub3
https://wakelet.com/wake/BFaYZPyM9dL5y43Wdk6qq
https://wakelet.com/wake/06Qkf2wV_BljeglX6fon4
https://wakelet.com/wake/k2eaDrXYf9Te7MCqHNSot
https://wakelet.com/wake/yjHsDGxD50EFrQ1p2F5y0
https://wakelet.com/wake/NT8DTwstVPEML2qnYe0zJ
https://wakelet.com/wake/UNohVQNCFdjJ4AQS6fitJ
https://wakelet.com/wake/CK6VNvuqe5Bl4GMqc8Wsx
https://wakelet.com/wake/6cDwzIfAZOS-0WjF6S5uL
https://wakelet.com/wake/hH6i1GjQlOVlz71wjSPk6
https://wakelet.com/wake/RkSvoCCnr-SX08p3cqed4
https://wakelet.com/wake/wJWY6mZVl0N7WQacJOv_9
margar (Tuesday, 11 January 2022 18:12)
margar 1641945491 https://trello.com/c/lP1rLBZx/33-the-chimp-paradox-steve-peters-pdf-link-download
https://trello.com/c/PTV2xW57/12-hot-brandingzip-igo-primo-24
https://trello.com/c/DBcfixrg/46-best-dota790aimap
https://trello.com/c/bO10x9Nb/14-imagenomic-filter-in-photoshop-free-download-link
https://trello.com/c/vuwD4tVo/30-nabi-se-pehle-khuda-mp3-free-download-jacquette-dauphins-d-exclusive
https://trello.com/c/NsoXe94D/31-brothers-movie-download-in-720p-torrent-hot
https://trello.com/c/Re9Z7P6t/35-link-frank-kinslow-beyond-happinesspdf
https://trello.com/c/GSnLYgjI/23-microsoft-office-2010-enterprise-corporate-edition-product-key-install-upd
https://trello.com/c/GX7FCjoy/32-full-agneepath-video-songs-hd-1080p-bluray-download-movies
https://trello.com/c/Ulpnqe3o/42-fix-chiko-wise-kumanda-mp3-32
https://trello.com/c/ibO2GeXT/45-ipswitch-whatsup-gold-premium-v1431-h33t-com-64
https://trello.com/c/GQ8jQXV8/20-electronics-circuits-simulator-torrent-download-torrent-full-portable
https://trello.com/c/lffepuHS/43-skyrim-pocket-dimension-mod-link
https://trello.com/c/DnAGTuYO/16-partition-1947-telugu-dubbed-free-download-in-torrent-darnjan
https://trello.com/c/TP4XLhkl/22-simulia-abaqus-612-crack-olenar
https://trello.com/c/L5EC4KOK/47-sketchup-pro-2015-v152687-x86-v152685-x64-firstuploads
https://trello.com/c/kuhd03a5/16-slysoftsoftwarepackage0421finalretailmultilanguage-fl-int-rar-mahdes
https://trello.com/c/LUIkriwb/57-best-finding-audrey-download-pdf
https://trello.com/c/tjQOL934/32-install-polar-golfer-free-download-full-version
https://trello.com/c/3XekUmlV/31-escape-from-tarkov-alpha-no-crack-serial-key-quarvency
https://trello.com/c/ykiOwp9v/14-mission-paw-full-movie-hd-free-download
https://trello.com/c/Ik0JHCBJ/43-the-dark-knight-hd-movie-download-upd
https://trello.com/c/dongm9Dk/46-saint-seiya-tenkai-hen-overture-latino-1080p-monitor-free
https://trello.com/c/aDPbK82T/33-adobe-acrobat-xi-pro-11027-patch-setup-free-honchand
https://trello.com/c/d0JfSRpN/34-newstar-sunshine-300-sets-torrent-berquynl
https://trello.com/c/eUbZPjEJ/43-catia-v5-title-block-editor-greylav
https://trello.com/c/VsaVy17x/49-himnos-y-coros-idmji-pdf-62l
https://trello.com/c/0BOIPKqD/60-best-wrong-turn-2-hollywood-hindi-dubbed-full-523l
https://trello.com/c/o77gBJTZ/32-embarcadero-rad-studio-10-serial-14-kalinzaid
https://trello.com/c/M1yj5nJS/76-piccolomagazineboyaddedbyrequest
byanelk (Tuesday, 11 January 2022 18:35)
byanelk 1641945491 https://trello.com/c/SVpb2Umr/37-lumion-101-pro-serial-number-reading-tool-serial-key-quyryanlon
https://trello.com/c/7OyTXqos/37-alias-autostudio-2014-serial-key-keygen-exclusive
https://trello.com/c/atO7YBYJ/66-raincoat-movie-download-in-hindi-dubbed-mp4-exclusive
https://trello.com/c/3yZkrTbj/59-better-ek-tho-chance-dual-audio-hindi-720p
https://trello.com/c/sg89NAB2/28-rpg-crotch-rpg-that-life-the-rural-survival-rpg
https://trello.com/c/gMH36gpt/30-work-download-the-blind-side-full-movie
https://trello.com/c/H6bWO0tr/22-deranged-korean-movie-eng-sub-download-abyyar
https://trello.com/c/YWdrpEzu/28-spectrasonics-omnisphere-crack-keygen-hot-serial-key
https://trello.com/c/emtT95lx/41-hot-smart-slider-3-nulled-cracking
https://trello.com/c/bbmhFZ5l/46-upd-cursed-castilla-maldita-castilla-ex-download-for-pc-compressed
https://trello.com/c/S3CtiF5H/21-itools-4457-crack-license-key-hot-free-download-2020
https://trello.com/c/x6p4H4AE/25-gravostyle-5-crack-newl
https://trello.com/c/GsfMWO6K/42-james-herbert-ash-pdf-download-hot
https://trello.com/c/IVjuW65J/19-kaleidagraph-free-download-crack-winzipl-fyllbadai
https://trello.com/c/sJCQNo69/34-top-pathologybooksparshguptadownload
https://trello.com/c/g8sNUd8j/38-norton-ghost-15-download-with-crack-wasanna
https://trello.com/c/tSK9EvkB/27-top-download-the-fast-forward-movie-mp4
https://trello.com/c/7FF5ja9D/12-paragon-partition-manager-9-professionalportable-4
https://trello.com/c/VuWRyM4H/24-poedit-pro-187-multilingual-portabl-patch-exclusive
https://trello.com/c/urqYAxbD/20-opensat-hd-333-software-2016-38-fix
https://trello.com/c/EWchbmZ7/18-hot-love-strange-love-1982-full-movie-free-download
https://trello.com/c/8ZpmtSeE/37-wp-job-manager-nulled-scripts-best
https://trello.com/c/ZtuhwxfN/35-crack-better-autocad-for-mac-2016-download
https://trello.com/c/G9mAednQ/30-avg-8-5-license-number-serial-laptops
https://trello.com/c/oxBbCypv/48-descargar-el-misterio-del-dragon-2020-espanol-torrent-en-hd-islanheyz
https://trello.com/c/0aPzYYvN/33-dramatical-murder-reconnect-game-english
https://trello.com/c/JASNqXtz/43-extra-quality-net-transport-272a-build-437-serial-key-keygen
https://trello.com/c/uQoGHpRm/55-discrete-event-system-simulation-fifth-pdf-download-work
https://trello.com/c/Ie9SyHBm/22-ul-2021
https://trello.com/c/iFPsjPmI/25-ataduras-del-almapdfl
vishgol (Tuesday, 11 January 2022 19:00)
vishgol 1641945491 https://trello.com/c/BM8QFjam/7-introduction-to-psychology-gateways-to-mind-and-behavior-12th-edition-pdf-47-new
https://trello.com/c/LA8MzCW2/19-kenichi-the-mightiest-disciple-complete-1-50dxodual-audio-english-51h264high-quality-historys
https://trello.com/c/xH1Cj7ku/23-mu-online-97d-speed-hack-download-link
https://trello.com/c/dbf8gxRp/23-new-autocad-raster-design-2017-free-download-ehanionor
https://trello.com/c/urDfAeIO/34-patternmaker-marker-studio-705-build-2-patternmaker-marker-studio-7052-patched
https://trello.com/c/nV0UUo3o/25-download-chalo-dilli-720p-hd-erbmar
https://trello.com/c/V55dSPRo/41-ultimate-zip-cracker-80217-keygen-top-free
https://trello.com/c/IJCyJTjv/51-pinball-hd-collection-activation-code-cheat
https://trello.com/c/Wg57RtvS/38-spen-command-apk-crack-portableed-26
https://trello.com/c/e43XPy6Q/38-download-film-kungfu-jet-li-exclusive
https://trello.com/c/BmLIJGOe/56-ul-free
https://trello.com/c/kPWvMrEW/26-top-ultrastar-deluxe-incl-333-songs-cpy
https://trello.com/c/DF1K5vDs/23-hot-buku-metode-penelitian-sugiyono-2013
https://trello.com/c/ENK7Z5MV/43-doomsday-productions-pray-4-me-r
https://trello.com/c/q2eZjIR5/20-new-barbie-fashion-fairytale-full-movie-download-free
https://trello.com/c/Ogmc8V0s/21-raxco-instantrecovery-server-250325-with-keygen-mariotarne
https://trello.com/c/MiF8jbcH/51-link-crack-cobian-backup-11-0-0-521-gravity-beta-10-1-1-816
https://trello.com/c/mrQTlDGS/40-video-watermark-android
https://trello.com/c/2I8i0JcD/14-powershape-2018-herunterladen-key-generator-64-bits-clepal
https://trello.com/c/CQEMBgCh/23-link-homework-and-practice-workbook-holt-prealgebra-answers
https://trello.com/c/GKy62UXU/47-magalir-mattum-telugu-movie-download-hd-better
https://trello.com/c/LDVqVjmR/19-gemini-the-duplicate-finder-250-crack-mac-osx-new
https://trello.com/c/7nGFYbsJ/73-shirin-farhad-ki-toh-nikal-padi-full-movies-720p-torrent-2021
https://trello.com/c/qna0maxV/26-marmoset-hexels-3-activation-unlock-code-and-serial
https://trello.com/c/G3BuWRUW/17-a-paine-by-any-other-name-part-2-full-movie-download-in-italian-hd-jambetha
https://trello.com/c/NIgd4YFU/16-sygic-1342-cracked-apk-ipa-is-here-carladelr
https://trello.com/c/URAvud1N/24-new-phil-hine-caos-condensado-1-ebook-1-pdf
https://trello.com/c/1Vs50lqG/61-jd-3-full-movie-download-720p-hd-hedodele
https://trello.com/c/k4ktkEJl/23-fallout-4-metro-last-light-mod-wianerose
https://trello.com/c/pczXdwTc/18-exclusive-the-my-name-is-khan-hindi-dubbed-free-download
shayil (Tuesday, 11 January 2022 19:21)
shayil 1641945491 https://trello.com/c/qpI174Yd/46-viswaroopam-telugu-movie-720p-free-hot-download
https://trello.com/c/c1GTCvKT/35-introduzione-alla-biochimica-di-lehninger-download-135-hot
https://trello.com/c/0eFGLauD/33-igo-my-way-android-480x854-apk
https://trello.com/c/ZMjctVqZ/62-top-dr-babasaheb-ambedkar-hindi-movie-full-hd-download
https://trello.com/c/K9ZWoPWT/20-zoey-101-4-stagione-torrent-ita-install
https://trello.com/c/Sg6l5mKJ/70-exclusive-pig-in-a-wig-book-online
https://trello.com/c/MtDEqhi7/51-csi-sap2000-version-2000-32bit-64bit-crack-top-hot
https://trello.com/c/kIQzbAO0/54-naathh-ek-pratha-2-full-movie-in-hindi-dubbed-download-link
https://trello.com/c/uJN5UEAm/79-fix-damon-ps2-pro-ocean-of-apk-cracked-apk
https://trello.com/c/jtCP29Nv/37-matt-monrothe-ultimate-matt-monro-full-album-zip-aleziellw
https://trello.com/c/PdfLSbsX/16-lumion-pro-95-crack-full-version-link
https://trello.com/c/O0mtsHMz/69-accurip-101-build-98-carsei
https://trello.com/c/25vq2C9T/24-full-wondershare-recoverit-82144-multilingual-full-with-medicine-extra-quality
https://trello.com/c/vABOzH06/22-softxpand-2011-32-bit64-bit-10-turn-1-pc-into-multipl-exclusive
https://trello.com/c/vt4IVQUm/36-synthesizer-greatest-volume-7rar-best
https://trello.com/c/dhv4B2od/27-top-cassette-v102-vst-vst3-aax-x64-incl-patched-and-keygen-r2r
https://trello.com/c/tf10CLIw/17-verified-anurag-i21-crack-without-dongle
https://trello.com/c/9JmS2RBE/36-smart-defrag-keygen-mygeeli
https://trello.com/c/3ojHcRvK/26-theepictalesofcaptainunderpantstorrent
https://trello.com/c/V8G999P9/92-different-strumming-patterns-for-guitar-pdf-download-heyddet
https://trello.com/c/J0h0RIrL/15-link-multisim-13-free-download-crack-windows
https://trello.com/c/VNooDJzv/23-peters-aircraft-a380-free-download-repack
https://trello.com/c/oEG0SV2m/38-the-xpose-movie-dual-audio-download-wainrvani
https://trello.com/c/5ckdpmdZ/29-free-youtube-full-hindi-movies-rowdy-rathore
https://trello.com/c/U76DOp8T/29-protel-dxp-2004-keygen-download-elfrdasha
https://trello.com/c/XL6TdDga/18-socha-na-tha-1080p-hindi-kachnesb
https://trello.com/c/ytAAWdKy/14-dulce-pontes-momentos-2009torrent-strumpfhosen-ficks-h-free
https://trello.com/c/NCsuOOyU/39-vero-visi-v2016-r1magnitude-cracked
https://trello.com/c/CradBSxZ/48-blacksite-area-51-link-crack
https://trello.com/c/lhF54OPH/36-gm-igor-smirnov-all-9-chess-courses-freel-manniwonyt
shayil (Tuesday, 11 January 2022 19:22)
shayil 1641945491 https://trello.com/c/qpI174Yd/46-viswaroopam-telugu-movie-720p-free-hot-download
https://trello.com/c/c1GTCvKT/35-introduzione-alla-biochimica-di-lehninger-download-135-hot
https://trello.com/c/0eFGLauD/33-igo-my-way-android-480x854-apk
https://trello.com/c/ZMjctVqZ/62-top-dr-babasaheb-ambedkar-hindi-movie-full-hd-download
https://trello.com/c/K9ZWoPWT/20-zoey-101-4-stagione-torrent-ita-install
https://trello.com/c/Sg6l5mKJ/70-exclusive-pig-in-a-wig-book-online
https://trello.com/c/MtDEqhi7/51-csi-sap2000-version-2000-32bit-64bit-crack-top-hot
https://trello.com/c/kIQzbAO0/54-naathh-ek-pratha-2-full-movie-in-hindi-dubbed-download-link
https://trello.com/c/uJN5UEAm/79-fix-damon-ps2-pro-ocean-of-apk-cracked-apk
https://trello.com/c/jtCP29Nv/37-matt-monrothe-ultimate-matt-monro-full-album-zip-aleziellw
https://trello.com/c/PdfLSbsX/16-lumion-pro-95-crack-full-version-link
https://trello.com/c/O0mtsHMz/69-accurip-101-build-98-carsei
https://trello.com/c/25vq2C9T/24-full-wondershare-recoverit-82144-multilingual-full-with-medicine-extra-quality
https://trello.com/c/vABOzH06/22-softxpand-2011-32-bit64-bit-10-turn-1-pc-into-multipl-exclusive
https://trello.com/c/vt4IVQUm/36-synthesizer-greatest-volume-7rar-best
https://trello.com/c/dhv4B2od/27-top-cassette-v102-vst-vst3-aax-x64-incl-patched-and-keygen-r2r
https://trello.com/c/tf10CLIw/17-verified-anurag-i21-crack-without-dongle
https://trello.com/c/9JmS2RBE/36-smart-defrag-keygen-mygeeli
https://trello.com/c/3ojHcRvK/26-theepictalesofcaptainunderpantstorrent
https://trello.com/c/V8G999P9/92-different-strumming-patterns-for-guitar-pdf-download-heyddet
https://trello.com/c/J0h0RIrL/15-link-multisim-13-free-download-crack-windows
https://trello.com/c/VNooDJzv/23-peters-aircraft-a380-free-download-repack
https://trello.com/c/oEG0SV2m/38-the-xpose-movie-dual-audio-download-wainrvani
https://trello.com/c/5ckdpmdZ/29-free-youtube-full-hindi-movies-rowdy-rathore
https://trello.com/c/U76DOp8T/29-protel-dxp-2004-keygen-download-elfrdasha
https://trello.com/c/XL6TdDga/18-socha-na-tha-1080p-hindi-kachnesb
https://trello.com/c/ytAAWdKy/14-dulce-pontes-momentos-2009torrent-strumpfhosen-ficks-h-free
https://trello.com/c/NCsuOOyU/39-vero-visi-v2016-r1magnitude-cracked
https://trello.com/c/CradBSxZ/48-blacksite-area-51-link-crack
https://trello.com/c/lhF54OPH/36-gm-igor-smirnov-all-9-chess-courses-freel-manniwonyt
shayil (Tuesday, 11 January 2022 19:23)
shayil 1641945491 https://trello.com/c/qpI174Yd/46-viswaroopam-telugu-movie-720p-free-hot-download
https://trello.com/c/c1GTCvKT/35-introduzione-alla-biochimica-di-lehninger-download-135-hot
https://trello.com/c/0eFGLauD/33-igo-my-way-android-480x854-apk
https://trello.com/c/ZMjctVqZ/62-top-dr-babasaheb-ambedkar-hindi-movie-full-hd-download
https://trello.com/c/K9ZWoPWT/20-zoey-101-4-stagione-torrent-ita-install
https://trello.com/c/Sg6l5mKJ/70-exclusive-pig-in-a-wig-book-online
https://trello.com/c/MtDEqhi7/51-csi-sap2000-version-2000-32bit-64bit-crack-top-hot
https://trello.com/c/kIQzbAO0/54-naathh-ek-pratha-2-full-movie-in-hindi-dubbed-download-link
https://trello.com/c/uJN5UEAm/79-fix-damon-ps2-pro-ocean-of-apk-cracked-apk
https://trello.com/c/jtCP29Nv/37-matt-monrothe-ultimate-matt-monro-full-album-zip-aleziellw
https://trello.com/c/PdfLSbsX/16-lumion-pro-95-crack-full-version-link
https://trello.com/c/O0mtsHMz/69-accurip-101-build-98-carsei
https://trello.com/c/25vq2C9T/24-full-wondershare-recoverit-82144-multilingual-full-with-medicine-extra-quality
https://trello.com/c/vABOzH06/22-softxpand-2011-32-bit64-bit-10-turn-1-pc-into-multipl-exclusive
https://trello.com/c/vt4IVQUm/36-synthesizer-greatest-volume-7rar-best
https://trello.com/c/dhv4B2od/27-top-cassette-v102-vst-vst3-aax-x64-incl-patched-and-keygen-r2r
https://trello.com/c/tf10CLIw/17-verified-anurag-i21-crack-without-dongle
https://trello.com/c/9JmS2RBE/36-smart-defrag-keygen-mygeeli
https://trello.com/c/3ojHcRvK/26-theepictalesofcaptainunderpantstorrent
https://trello.com/c/V8G999P9/92-different-strumming-patterns-for-guitar-pdf-download-heyddet
https://trello.com/c/J0h0RIrL/15-link-multisim-13-free-download-crack-windows
https://trello.com/c/VNooDJzv/23-peters-aircraft-a380-free-download-repack
https://trello.com/c/oEG0SV2m/38-the-xpose-movie-dual-audio-download-wainrvani
https://trello.com/c/5ckdpmdZ/29-free-youtube-full-hindi-movies-rowdy-rathore
https://trello.com/c/U76DOp8T/29-protel-dxp-2004-keygen-download-elfrdasha
https://trello.com/c/XL6TdDga/18-socha-na-tha-1080p-hindi-kachnesb
https://trello.com/c/ytAAWdKy/14-dulce-pontes-momentos-2009torrent-strumpfhosen-ficks-h-free
https://trello.com/c/NCsuOOyU/39-vero-visi-v2016-r1magnitude-cracked
https://trello.com/c/CradBSxZ/48-blacksite-area-51-link-crack
https://trello.com/c/lhF54OPH/36-gm-igor-smirnov-all-9-chess-courses-freel-manniwonyt
dawsoph (Tuesday, 11 January 2022 19:39)
dawsoph 1641945491 https://trello.com/c/at6OEL4g/22-jattu-engineer-dubbed-movies-in-hindi-720p
https://trello.com/c/tBCZliBr/23-full-baladas-radio-ole
https://trello.com/c/SEjkFuW9/39-asphalt-9-for-mac-upd
https://trello.com/c/1fYlBMF9/19-fsx-fly-the-maddog-professional-2010-edition-india-free
https://trello.com/c/hp6DEwQN/16-suara-tembakan-senjata-wav23l-full
https://trello.com/c/EUO6AhMc/55-patched-city-hunter-korean-drama-full-movie-free-28
https://trello.com/c/EK2zOOjd/55-reshma-aur-sultan-1-hd-movie-download-in-hindi-happpelhy
https://trello.com/c/6Q8GHInT/81-neat-video-35-ofx-crack-work
https://trello.com/c/twKyz1kz/36-manusiadankebudayaanindonesiakoentjaraningratpdfdownload-honlati
https://trello.com/c/qvezDz2h/20-luther-vandross-dance-with-my-father-2003zip-karsaegm
https://trello.com/c/leR6nGC5/71-nokia-113-unlocker-v10-152
https://trello.com/c/oDFButPi/46-assassins-creed-ii-only-crack-best
https://trello.com/c/dtpkrjqo/40-hot-adobe-bridge-2020-1002-macos
https://trello.com/c/PdhqmjwZ/57-oxygen-not-included-free-mac-hot-download
https://trello.com/c/odGAfH8F/63-him-and-love-said-no-the-greatest-hits-1997-2004-full-album-zip-phyjaile
https://trello.com/c/XoRLiRmL/43-how-to-download-clips4sale-for-free-hit-trancha
https://trello.com/c/RJYm9Xh1/37-madmapper-1-2-mac-osx
https://trello.com/c/Z99fcR3v/37-autobiografija-o-drugima-mihiz-16pdfl
https://trello.com/c/owry3ySN/39-alien-1979-directors-cut-1080p-201
https://trello.com/c/igqY6PUN/50-repack-movie-php-script-version-22-nul
https://trello.com/c/R4uxNVkP/68-download-joey-the-passion-crack-janelde
https://trello.com/c/IBLfvUGz/35-relatos-hablados-de-zoofilia-gratisl
https://trello.com/c/vwVckz5K/34-verypdf-document-converter-docprint-pro-v50-with-key-tordigger-keygen-ignacaul
https://trello.com/c/SgU30imN/23-high-quality-mentepositivajulianmelgosapdf22
https://trello.com/c/XNhMMC68/20-repack-the-real-jackpot-2013-hindi-dubbed-movie
https://trello.com/c/cd0INk8p/37-extra-quality-hoshi-no-koe-720p-mkv
https://trello.com/c/2SrHL3zi/18-download-qila-movie-mp4-hindi-verified
https://trello.com/c/fZzs0NzL/49-hot-abcd-2-2015-720p-blu-ray-x264-51-ac3-esubs-ddr-exclusiveepub
https://trello.com/c/tKKBqxWq/14-coach-carter-mobile-movie-3gp-download-wynpint
https://trello.com/c/6uHNdRoZ/20-wondershare-winsuite-2012-torrentzip-brywalle
harkirs (Friday, 14 January 2022 15:53)
harkirs f91c64177c https://faicrinerradepec.wixsite.com/dardeopeho/post/game-box-art-the-s-final-free-64bit-download-nulled
https://wakelet.com/wake/zd74pJeTkeM9qXJEZRbqF
https://wakelet.com/wake/JHJYNPcmTvG0qp8NVCWjU
https://trello.com/c/97ftAAcn/9-maine-pyar-kiya-4-subtitles-mp4-subtitles-torrents-movie-english
https://trello.com/c/8UjX90Mg/18-alt-n-mdaemon-email-server-pro-2100-x-dubbed-film-watch-online-watch-online-english
https://trello.com/c/XM2HbaKa/16-cambridge-checkpoint-year-9-past-papers
https://nextfonnusctubar.wixsite.com/tiocasdazzse/post/red-dead-redemption-goty-~-kratos-part16-rar
https://forpeepabopo.wixsite.com/unanneters/post/iobit-advanced-systemcare-pro-13-7-0-september-2020
https://trello.com/c/P27RvZNY/20-alphabetty-saga-level-508
https://formsnarimreamine.wixsite.com/reenhyaprodos/post/medalist-electronic-digital-safe-user-guide
https://trello.com/c/hyJcPY1N/10-jetbrains-goland-201831-crack-mac-osx
https://ufecbasektte.wixsite.com/tigasylos/post/full-version-taiko-windows-download-ultimate-key
https://closbiacortiwarpay.wixsite.com/reconkipo/post/online-notepad-untitled-4192020-24853-am
https://trello.com/c/5UEbOtBg/4-ia-writer-568
https://vellephodegoldcy.wixsite.com/centfoodsriddheads/post/mocha-tn5250-2-4-keygen-torrent
https://srinanartertiti.wixsite.com/upwfinroconf/post/pro-oracle-aca-activation-64bit-windows-utorrent-patch-rar
https://trello.com/c/E6PYp4Fp/38-checkpoint-endpoint-security-vpn-client-download-mac
https://incotanmerugle.wixsite.com/lanithearwho/post/bangbros-mofos-naughtyamerica-windows-activator-build-32bit
https://tenmortnewilsute.wixsite.com/termasever/post/download-queryq-the-animatrix-full-full-watch-online
https://kerslawbtrodsenree.wixsite.com/fulafkengwwith/post/32-opanda-powerexif-1-2-download-serial-free
https://tretsuffdepenrahas.wixsite.com/huddlisigme/post/unlockicloud-genera-iso-build-activator-download-free-nulled-32
https://inexlinfiti.wixsite.com/franableura/post/full-version-the-night-2020-utorrent-x64-crack
https://alengemouffcost.wixsite.com/pricecaloc/post/cydia-download-ipod-4g-no-computer
https://losquewebtamond.wixsite.com/dwheelabanli/post/download-the-convert-s-catechism-of-catholic-doctrine-mobi-zip-book-free
https://moidachocarkeyno.wixsite.com/ebtranarym/post/angles-of-elevation-and-iso-nulled-pc-file
https://trello.com/c/k1n5syqW/17-trt-1-freestreamslive
https://frucabraforhofe.wixsite.com/stutbecycri/post/cracked-melodic-hard-rock-web-atlas-full-pro-windows-key-x32
https://elanapwervemis.wixsite.com/soderfigen/post/gol-covek-igor-dzambazov-free-download
https://trello.com/c/QorJRreG/7-pro-chickens-coming-home-windows-zip-64bit-download-full-activation
https://trello.com/c/Hp5O55f5/16-telecharger-attestation-dhгbergement-la-banque-postale-free-mobi-utorrent-book-zip
phrihet (Friday, 14 January 2022 16:10)
phrihet f91c64177c https://trello.com/c/JWAfLLiz/43-rar-corel-draw-full-x32-final
https://www.homify.in/ideabooks/8463314/zanti-gold-cracked-apk-downloads
https://uploads.strikinglycdn.com/files/55b6dd41-8509-4645-aae3-26cdf1c1aa37/Educational-Technology-1-By-Brenda-Corpuz-Pdf-19.pdf
https://www.drupal.org/files/issues/2021-11-26/Enfin-les-femmes-streaming.pdf
https://kit.co/mettderfaimen/blue-exorcist-season-2-professional-x32-nulled-activator-utorrent-full
http://enemaner.unblog.fr/2021/11/26/game-editor-download-free-full-version-best/
https://sunischeckback.mystrikingly.com/blog/used-2006-honda-cbr-600-for-sale
https://kit.co/naotbetlechar/license-sweet-pool-exe-zip-64bit-final-full
https://s3.amazonaws.com/media.muckrack.com/portfolio/items/14882219/Funs-Dota-Hack-126-Zipperton-Ru.pdf
https://trello.com/c/BdXN8oEZ/50-freedownloaddkzstudiofullversion
https://wakelet.com/wake/o7yCXJFi1GU9x3x8qf4Du
https://uploads.strikinglycdn.com/files/790b647c-2ee1-4571-8bbf-4297f7ae60e7/download-prince-of-persia-2008-pc-fullrip.pdf
https://trusting-goldberg-5ba99e.netlify.app/Furby-Island-320x240jar-avconverter-swing-gl
https://pdfslide.tips/data-analytics/crack-kaspersky-internet-security-2018-v1900616-build-8533-crackl.html
https://7gogo.jp/4Th24IjLN0TP
http://riterprichap.blo.gg/2021/november/wnlo-xszn-iskns-rysvrkoxs-nginkksion-2o.html
https://fdocuments.in/document/diva-delivery-castle-high-film-completo-in-italiano-download-gratuito-hd-1080p.html
https://plugaki.com/read-blog/646
https://coub.com/stories/1151401-gadis-kerudung-ngentot-ma-kakek
http://weetsgolddelha.blo.gg/2021/november/that-obscure-object-of-desire-torrent.html
https://uploads.strikinglycdn.com/files/3a62f6a8-537c-4c5c-b585-573e29df8aa7/Artcut-2009-Software-Free-Download-V700-Hit-iliaedyseh.pdf
http://progelrasu.unblog.fr/2021/11/26/download-patched-alien-shooter-4-full-61/
https://seesaawiki.jp/alexrisa/d/Control De Ciber 1.598 Keygen Extra Qualityl
https://kit.co/terptisicard/tiken-jah-fakoly-coup-torrent-professional-32bit-crack-pc-license-full
https://coub.com/stories/1151400-shippo-gets-an-angry-challenge-movie-free-download-in-italian
https://www.drupal.org/files/issues/2021-11-26/glyneli.pdf
https://virt.club/read-blog/3888
https://fdocuments.ec/document/brahmaand-nayak-sai-baba-hd-1080p-hindi.html
https://wakelet.com/wake/J4e_sqrXDK4TeSZFjlnTf
https://trello.com/c/ik8JacSs/32-bang-bang-tamil-full-movie-download
bethnay (Friday, 14 January 2022 16:34)
bethnay f91c64177c https://trello.com/c/HQaA8fRo/13-full-version-scarica-il-affinity-pho-186-mas-hciso-70016-mb-in-mo-turbobit-net-key-torrent-pro-macosx
https://www.pixnet.net/pcard/57568601b3fe8b4e43/article/6ef924e0-5279-11ec-9ea0-e16985637655
http://clonananbu.unblog.fr/2021/12/01/enature-lets-all-have-more-fun-torrent-link/
https://seesaawiki.jp/rieplaflaucan/d/Find Any File Full Version Key Torrent Keygen _HOT_ .rar
http://kuquadcupa.unblog.fr/2021/12/01/nahwu-wadih-terjemahan-pdf-12-lanmea/
https://www.pixnet.net/pcard/4025760bc6da3e04a5/article/6f94ecf0-5279-11ec-8064-b135a10253c0
https://wakelet.com/wake/rJWGmC6i1c5bAv8rNpjFg
https://seesaawiki.jp/wijntaramer/d/Harry Potter Half Blood Prince
http://telegra.ph/Link-Shortner-Service-12-01
https://wakelet.com/wake/-tkH-NhGYOIfwqzsJTWU_
http://witholoper.unblog.fr/2021/12/01/duke-nukem-forever-complete-plaza-codex-khryjami/
http://cranecvepou.unblog.fr/2021/12/01/greater-ritual-of-the-hexagram-pdf/
http://nutoturo.unblog.fr/2021/12/01/__link__-heart-of-darkness-characters-pdf/
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgIC__vGFCwwLEgZDb3Vyc2UYgIDAgOK_lAoMCxIIQWN0aXZpdHkYgICA36mRgAkMogEQNTcyODg4NTg4Mjc0ODkyOA
http://telegra.ph/Oghackroblox-12-01
https://seesaawiki.jp/cuikennome/d/Hold Me Chapter111 - Google Drive Free Zip Epub Torrent Book janolea
https://assets.pinshape.com/uploads/image/file/463358/Daisys-Destruction.html
https://tighstitcompda1982.wixsite.com/trarsirusmi/post/download-lagu-udh-chaliye-mp3-download-320kbps-5-36-mb-mp3-free-download
https://www.pixnet.net/pcard/61939601c38b59d18d/article/65267aa0-5279-11ec-b447-d9ac3260985d
https://wakelet.com/wake/s3PkOm01rGWQxyMlurtSH
http://prophdudsele.unblog.fr/2021/12/01/de-dana-dan-full-movie-free-download-utorrent-otadars/
https://outtacanfevil.wixsite.com/blocbiferha/post/clip-studio-paint-1-7-rar-64bit-activation-windows-nulled-torrent
http://versstetinal.unblog.fr/2021/12/01/free-adobe-photoshop-cs5-extended-x86-x64-100-working/
http://raicleanrida.unblog.fr/2021/12/01/tyrann-mathieu-iphone-wallpaper-posted-by-sarah-simpson-top/
https://ylinunerci.wixsite.com/gasecambu/post/teen-alice-new-star-latest-crack-full-version-windows-rar-activation-utorrent
https://wakelet.com/wake/Qc5qz7BjtL3zYFaTgUty0
https://seesaawiki.jp/quikacalo/d/Azov Films Bf V2.0 Fkk Paul Calin\\\\\\\\\\\\\\\\'s Home Video (2011)
http://inytdebun.unblog.fr/2021/12/01/adobe-xd-28-2-full/
http://relimandstaf.unblog.fr/2021/12/01/planet-cnc-usb-controller-license/
http://kelbsakeako.unblog.fr/2021/12/01/world-machine-2-3-professional-edition-crack-hot/
elkelis (Friday, 14 January 2022 16:58)
elkelis f91c64177c https://wakelet.com/wake/2dpl5gPluw4lGo6eitInk
https://wakelet.com/wake/WCufMnBX7GfQDhLL2dprW
https://wakelet.com/wake/T_lG2Nbm0JRcZJx_lJBLp
https://wakelet.com/wake/nsIsBoP8fGROuC4L2-0OJ
https://wakelet.com/wake/-tyNvYFx6K-wbmmStGKEX
https://wakelet.com/wake/jwJwnRFkkOsF92MNj_ngV
https://wakelet.com/wake/KD_sYi-gWjEduOQujCKQ5
https://wakelet.com/wake/JOi7eG4jthGxrdKjBsq9c
https://wakelet.com/wake/SvvdAFKzBRihu7gOpxAzV
https://wakelet.com/wake/8dGgiWRLTlnFfGh7pzlSh
https://wakelet.com/wake/WyRwSayZYOPgn73bFzHTx
https://wakelet.com/wake/JS4BhTbDFRYmpIULXMG3w
https://wakelet.com/wake/irh82YF6SoTqv8CW9_NUg
https://wakelet.com/wake/zteWlJ4yVAZXUbqzKimy0
https://wakelet.com/wake/ckjINHpNYxeYIfExdLJC_
https://wakelet.com/wake/iLGCXBvVStSkPqa5AzG3A
https://wakelet.com/wake/c-hy5JBrQ6z_7UpUBy9N1
https://wakelet.com/wake/xIeYjofr3M06EJGU95HZa
https://wakelet.com/wake/zHNdhUfCiWqDSdBOh5jWN
https://wakelet.com/wake/FnVOhR_x3BowXpBtaBuCZ
https://wakelet.com/wake/VNMRACJGzFx6SGUblZ1v_
https://wakelet.com/wake/k3Rvyhi1Ffj1G2Bl6pItX
https://wakelet.com/wake/N9X6VTmCEOcCuXDqh9WEk
https://wakelet.com/wake/LqpWFw3PJiEQ_cMJfzAoe
https://wakelet.com/wake/gJyFLQdCknNj2O9g3UZVh
https://wakelet.com/wake/L32DQknJF3ViwFPxtRb3m
https://wakelet.com/wake/pe7tMGvsOzdRBKBu0FYKm
https://wakelet.com/wake/XY_ytzKj7DhRciNtpQBBh
https://wakelet.com/wake/yFvCNCWBzkEh3prKv8OQI
https://wakelet.com/wake/M4OlkkSeCj2SJJ0PInOku
wyaolly (Friday, 14 January 2022 17:22)
wyaolly f91c64177c https://seesaawiki.jp/rabdipifer/d/Pivot Stick Anima File Activation Nulled 32bit Utorrent
https://pensayhosbubo.wixsite.com/natakasol/post/cracked-hourly-analysis-program-4-91-download-activator-full
https://tersereper.therestaurant.jp/posts/23848825
https://worcionasodyfi.wixsite.com/diabuldesal/post/latest-split-second-velocity-download-x32-windows
https://wakelet.com/wake/97QMDeRd-D5T7-8YIMjf4
https://midgosawbflatdi.wixsite.com/rowinhuatho/post/black-butler-season-2-download-mkv-2k-film-subtitles-bluray-free
https://sbilesbridfalicar.wixsite.com/royslimarcrim/post/full-ticha-baap-tyacha-baap-kickass-download-rip-avi-dubbed-bluray
https://dilobsdifutacu.wixsite.com/curstanave/post/p-spin-4-dubbed-dubbed-1080-movies-kickass-full
https://whitthecdofilsurf.wixsite.com/iclugardpar/post/muhyadheen-mala-141-download-full-pdf-ebook-zip
https://trello.com/c/rQ2k4JTU/16-ls-land-anya-forbidden-fruit
https://stonorecperlisurp.wixsite.com/atooddrivpe/post/pdf-ra-smith-semiconduc-rs-ebook-zip-full-edition-utorrent
https://seesaawiki.jp/paeflooranif/d/Undisputed 2 In 720 Mp4 Watch Online Film Full [UPDATED]
https://stonorecperlisurp.wixsite.com/atooddrivpe/post/crawford-au-cracked-rar-windows-x32-download
https://kacalneyschizen.wixsite.com/tesyncibo/post/patch-codigo-torrent-rar-full-version
https://praccarneugrav.localinfo.jp/posts/23848821
https://nalfevilsisu.wixsite.com/wampcalongue/post/1080-corel-products-torrent-hd-dts-dubbed-torrent-full
https://trello.com/c/uV1Sccf5/16-software-engineering-aa-puntambekar-free-download
https://wakelet.com/wake/YpjBUk74gzv7_kpQ1Pi3a
https://trello.com/c/Hz8BDWM9/17-online-player-ati-firepro-m7820-max-resolution-108-full-version-final-activation-free
https://seesaawiki.jp/boodefiwild/d/32bit Merce Activator Pro Pc
https://reaucuirepbosi.wixsite.com/calitugdio/post/windows-hot-3d-loli-collections-from-www-imperia-of-hentai-ru-part-2-full-version-rar-x32-download
https://taiviamechar.shopinfo.jp/posts/23848818
https://relisrecani.wixsite.com/lieconfufarm/post/build-burnintest-crack-32-pc-license
https://seesaawiki.jp/tiobellidown/d/.rar PokemonLeafGreenRandomizerGBA Full Version 64bit Download
https://trello.com/c/SZ4RD1xm/30-the-cure-discography-free-torrent-download
https://weckporesmiddmistm.wixsite.com/parlitorkey/post/ecology-and-environment-pd-sharma-317-rar-utorrent-ebook-free-epub
https://trello.com/c/stQZnyir/2-hinario-5-ccb-em-ingles-pdf-107
https://trello.com/c/Blu3xjTA/12-cfd-2016-x-windows-full-fix-registration-serial-rar
https://riesymmodeno.wixsite.com/arquicodo/post/labs-kita-o-dubbed-mkv-rip-free
https://seesaawiki.jp/glycanorof/d/2020 Diablo 1 Hellfire .rar Cracked Key Pc 32
weldbell (Friday, 14 January 2022 17:46)
weldbell f91c64177c https://agaxtioco.mystrikingly.com/blog/final-ss-s-64-download-keygen-pc-rar-key
http://neolootabfern.unblog.fr/2021/11/26/best-card-recovery-v3-60-build-1012-keygen-albulm-versamento-po/
https://klemacey.wixsite.com/venectaraj/post/full-platypus-2-windows-software-key-download-cracked-64bit
http://vosadpeli.webblogg.se/2021/november/the-pixel-lab-octane-texture-pack-3-procedural-edition.html
http://tasteodramrep.unblog.fr/2021/11/26/upd-papercut-ng-license-file-crack-22/
https://wakelet.com/wake/kX3ednTKLNiy7ZAIZMbyE
https://www.homify.in/ideabooks/8468321/severina-se-jebe-video-17
https://ermisconsprov.theblog.me/posts/24134025
https://trello.com/c/qmkAhWUN/19-the-amazing-spi-subtitles-hd-full-rip-torrents
https://www.pixnet.net/pcard/79571601a30eb13c45/article/24088fb0-4eb9-11ec-b79e-7b842ab04102
https://vipfun.xyz/upload/files/2021/11/tGPV9xThDJzGThdjYxWP_26_7226db38d166cd907460bc57b00019e6_file.pdf
http://socialmediascript.aistechnolabs.xyz/upload/files/2021/11/CHqBcURk8hOyV5HWTGji_26_615bf3eada33e837fae00f73f8f62b89_file.pdf
https://trello.com/c/6EVFHyEX/38-primocache-windows-torrent-free-exe-key
http://benpauseso.unblog.fr/2021/11/26/lucky-star-malayalam-movie-songs-free-14-amalebene/
https://kit.co/raphilkovstram/windows-onimusha-2-key-file-exe
https://descramiri.diarynote.jp/202111262202453529/
https://www.homify.in/ideabooks/8468322/nero-9-full-crack-sinhvienit
https://fdocuments.in/document/winx-dvd-ripper-platinum-serial-crack-spider.html
https://facepager.com/read-blog/4133
https://esunproges.weebly.com/real-indian-naked-girls.html
https://kit.co/dihangcolning/key-chelda-special-full-version-pc-64
https://bortogijilesa.wixsite.com/ingodpicon/post/minitool-power-data-recovery-v8-1-crack-license-key-full-version
https://www.drupal.org/files/issues/2021-11-26/Usher-Confessions-Deluxe-Edition-Zip.pdf
https://kit.co/conominso/full-version-o-teu-corpo-diz-ama-te-ebook-zip-mobi
https://dokumen.tips/recruiting-hr/sin-ropa-penelope-menchaca-desnuda-conpletamente11.html
https://centtvunernopusto.wixsite.com/icdepningjun/post/download-squad-upload-share-and-mirror-in-one-step-with-rapidspread
https://cdn.thingiverse.com/assets/80/0c/23/c1/b0/darenipho1.html
http://snapidaben.unblog.fr/2021/11/26/sr-2000hd-ace-loader-work-downloadl/
https://serhychiladestref.wixsite.com/stacacisco/post/alberto-vazquez-figueroa-codicia-epub-filegolkesl
https://herzgenhara.weebly.com/chingy-hate-it-or-love-it-zip.html
jamedmu (Friday, 14 January 2022 18:08)
jamedmu f91c64177c https://docs.google.com/viewerng/viewer?url=social.urgclub.com/read-blog/2626
https://www.homify.in/ideabooks/8486744/wifi-password-hack-v9-1-2014
https://coub.com/stories/1155491-musixmatch-lyrics-music-7-4-5-final-apk-premium-unlocked-for-android
https://fdocuments.ec/document/fightingkids-dvd-493rar.html
https://pdfslide.us/data-analytics/cara-duplicate-pets-simulator.html
https://kit.co/bharsenetin/trimble-business-center-3-40-x6-final-full-version-exe-serial
http://torgehardtho.blogg.se/2021/november/mp4-hindi-dubbed-traffic-signal.html
https://wakelet.com/wake/L3Y-YfHee7w-1KZsTRpAM
https://alumni.armtischool.com/read-blog/4371
https://media.muckrack.com/portfolio/items/14885145/Command-And-Conquer-3-Keygen-RAZOR-Serial-Keyl.pdf
https://pdfslide.us/devices-hardware/bratzrockangelz15-carbon-bermudas-berr.html
http://vabduddsupphay.unblog.fr/2021/11/28/honda-cbr-250-2-silinder-2013-honda/
https://seesaawiki.jp/eassevilrock/d/Activate Windows 7 Loader
http://diastanounhou.blogg.se/2021/november/hindi-film-loins-of-punjab-presents-3-full-movie-download.html
https://tingtenttaltilo.wixsite.com/sgenreitinco/post/magic-engine-fx-1-1-1-crack-version-software
http://filxyztkradan.blogg.se/2021/november/berliner-platz-2-neu-pdf.html
https://lucid-nightingale-b74d52.netlify.app/Solidcam-2012-Crack-Download
https://pdfslide.net/automotive/a-ath-in-the-gunj-watch-online-4k-subtitles-avi-bluray.html
https://coub.com/stories/1155490-madholal-keep-walking-in-hindi-free
https://coub.com/stories/1155489-download-akame-ga-kill-episode-12-english-english-subtitles
https://media.muckrack.com/portfolio/items/14906920/Advanced-Task-Scheduler-Crack-Download.pdf
http://telegra.ph/Utorrent-Thank-You-And-Youre-Welcome-Pdf-Ebook-Full-11-28
https://wakelet.com/wake/tzp13KnfA7ThOafm79pWF
https://assets.pinshape.com/uploads/image/file/421721/better-nike-bot-cracked-tongue.html
http://abcarana.blogg.se/2021/november/steamapi-restartappifnecessary-dll-steam-apidll-cuore-leangue-impero.html
https://assets.pinshape.com/uploads/image/file/421720/elidesaun.html
https://media.muckrack.com/portfolio/items/14833581/Visual-Studio-Torrent.pdf
http://centlessrawi.blogg.se/2021/november/siberianmousem41.html
https://indbook.in/upload/files/2021/11/f7PJOXtq47iISZJxNEBz_28_ba1b032497c0049619d08c8b3a470b3f_file.pdf
https://uploads.strikinglycdn.com/files/0567a392-f76b-4265-9865-344a7701c1e6/waveshellvst371.pdf
virgalee (Friday, 14 January 2022 18:29)
virgalee f91c64177c https://wakelet.com/wake/Le91FUkM7Wg8tV_Li23ER
https://wakelet.com/wake/tkDbHhQiUsrTynOeh74SF
https://wakelet.com/wake/esjlsTP46xJSJv3OH8srm
https://wakelet.com/wake/A3SR6gFRTSQ1z1M0CnzhH
https://wakelet.com/wake/feo7EHYUprmiz4zQdJj9S
https://wakelet.com/wake/NeWgj9OmVly_7d6Yi80tm
https://wakelet.com/wake/IGyIvm05rqGR-F8p8nNvA
https://wakelet.com/wake/vbk7IGjP8waPu1Zq0jM3v
https://wakelet.com/wake/vyCyEAWEmvGbxHVz9G-1J
https://wakelet.com/wake/3o8zIynOR_LTQHclT6XTL
https://wakelet.com/wake/hmJZHgGt4pobqfSMHb2XK
https://wakelet.com/wake/T406IG4_1S8SwoXDQUk6s
https://wakelet.com/wake/z0P6wAC4JD012vlVs6j_T
https://wakelet.com/wake/WMo9-9ovvB-aCRo_SLNO4
https://wakelet.com/wake/aKZD1x13O9u8M_GZ1cX8c
https://wakelet.com/wake/C4J35w1xqsp8-gmctaXWX
https://wakelet.com/wake/x0HOQbOpk6PIw-jSBm9Vx
https://wakelet.com/wake/xIv71UChxolAafGwpu0jW
https://wakelet.com/wake/g8H-vVJbr8oRtZAXQwiTe
https://wakelet.com/wake/5otM4cWmupu8jQ4_shfZt
https://wakelet.com/wake/yLehYGl1Wk4OQaAOVe9ao
https://wakelet.com/wake/BgdsPRicyaz16x0-ks1Yd
https://wakelet.com/wake/30j4q07Wz-OO_17sLeNk6
https://wakelet.com/wake/KcAgmpGPiYwhkJQmq7wfR
https://wakelet.com/wake/hGPlZaO2o1on0lYL8-0NI
https://wakelet.com/wake/7cmOiu4X1RjEXwrr5ymdk
https://wakelet.com/wake/xsl4y3BThgPVrdtfjqGLp
https://wakelet.com/wake/VhEyd-GVGWv0PJPVfmmfr
https://wakelet.com/wake/Btw3e5uEY4xpqhpbXjo7k
https://wakelet.com/wake/r8c58cI8F7fqmXb9yU9Hr
paeket (Friday, 14 January 2022 18:47)
paeket f91c64177c https://wakelet.com/wake/hxQwvfjEJGucPMGCf6ghb
https://wakelet.com/wake/vT0OPn8_uCFRVwlPdU3qU
https://wakelet.com/wake/Io3KpgNG_V44nrESZ3PBO
https://wakelet.com/wake/pOqeXFgbIeHkh6Q5vH8Ao
https://wakelet.com/wake/9ec9yUDlo9pfJzjJtaP6w
https://wakelet.com/wake/UK7a36hsPWFvPWQc_-mS3
https://wakelet.com/wake/7wBVZM3OEMnPlxpP4ipAJ
https://wakelet.com/wake/QUC7UMuU6V2f2QsHKaYWq
https://wakelet.com/wake/gPUWMoz0odvf4RcvvsVd_
https://wakelet.com/wake/0E5wUkTgNvIldPCf_bTGu
https://wakelet.com/wake/_mCw3a3wYhGvSEfFHKbN_
https://wakelet.com/wake/QXAeiM661rkpd8Qrt02K5
https://wakelet.com/wake/35Q4OyhmGm_8dq9guVM-g
https://wakelet.com/wake/GEBZWnsV31Zzebfh09lxN
https://wakelet.com/wake/VXLFPcK5-1ZBURmx7oD4P
https://wakelet.com/wake/rS3NN6-InT0xWUb6Ru5hy
https://wakelet.com/wake/Za_dyXy4HNbeUQvu66IVQ
https://wakelet.com/wake/L0UPXj7LhEUjtuc9p2djm
https://wakelet.com/wake/GWR6vTnRg9q8i4b2ywag1
https://wakelet.com/wake/wBO0RwFF3PZMUqR2RUMm_
https://wakelet.com/wake/HPVp7DSbuCWFSMKbpNztb
https://wakelet.com/wake/Jv3b6hiyANwxn0zGj07eu
https://wakelet.com/wake/Be-yooqn9eHn0sB2_DSCT
https://wakelet.com/wake/jwUps0HrVMYzH4WLOf7zU
https://wakelet.com/wake/97z6aPkjcnHbfLnUqGqIb
https://wakelet.com/wake/EsXzB6BdEe66klQcVQUqC
https://wakelet.com/wake/cKxYb-rnTi3xG4rtgR58Y
https://wakelet.com/wake/Kee-mE67dn_sw8RSx_4pQ
https://wakelet.com/wake/hJ_LcLnmbk_t4vwtrstUG
https://wakelet.com/wake/IeUS0TsTx96LeGVrjM_mW
haylnayt (Friday, 14 January 2022 19:05)
haylnayt f91c64177c https://prundiastepetpas.wixsite.com/hycardecart/post/introvert-and-extrovert-questionnaire-pdf
https://clinsergivecom.wixsite.com/contlojourrea/post/ben-power-t-registration-ultimate-torrent-nulled-full-pc-64
https://mafdelacova.wixsite.com/agonrichrei/post/new-jersey-drivers-license-status-dropped
https://trello.com/c/iJyG4YPw/16-enounce-myspeed-serial-number-crack-mac
https://trello.com/c/GPrBTJxT/3-pathfinder-bestiary-5-pdf-free-download
https://wakelet.com/wake/Ice-R9XDVp_CwZYg8d3SO
https://belsuirocontsesa.wixsite.com/cioliridi/post/dubbed-trvnskm-english-watch-online-dubbed-720-avi
https://urfrohteamiswesttr.wixsite.com/waerhodedmis/post/numero-dubbed-english-2k-torrents
https://trello.com/c/fUWpMwQr/3-diving-bell-and-the-butterfly-pdf
https://wakelet.com/wake/6oF9Mzq74aKoUZ_icvecf
https://wakelet.com/wake/JhiGmWJSJYLXebnOs8z_x
https://jacknaraforcovi.wixsite.com/gagekadedp/post/sat-math-calculator-section-pdf
https://wakelet.com/wake/PffQ1_gXeayNK7iYBye5x
https://jeepspomounseri.wixsite.com/tereregwea/post/solucionario-de-ecuaciones-diferenciales-de-nagle-cuarta-ediccion-temp
https://paetextrolldicompt.wixsite.com/gratenpregep/post/out-of-64bit-utorrent-license-iso
https://winslumitkele.wixsite.com/caschyusparmind/post/download-boating-hd-marine
https://inmeidundaso.wixsite.com/bormargbotmo/post/fantastic-children
https://chaukolhuddmardesc.wixsite.com/liarilifind/post/hd-dj-cut-killer-discographie-720p-watch-online-mp4-blu-ray-hd-subtitles
https://leaheartpunkplavge.wixsite.com/longhochdeca/post/benzo-wit-nulled-rar-license-free
https://perkailentdisu.wixsite.com/outobeper/post/alvin-and-the-chipmunks-the-road-chip-2015-greek-audio
https://taifrenarevdia.wixsite.com/mintahotso/post/maintenance-and-cleaning-roster-for-a-fitness-centre
https://pasmycompxave.wixsite.com/ncerdelaver/post/spcl-2602-rajnagar-reboot-pdf-google-drive
https://djerabumwebfi.wixsite.com/ywhchannaisamp/post/episodi-grachi-2-in-italiano
https://dresamnitingle.wixsite.com/luhandtalo/post/windows-escritгіrio-software-activator-utorrent
https://wakelet.com/wake/jpJopZczrmXxNdANxmG69
https://fighmabilpale.wixsite.com/adesdiokind/post/c-kkompany-mkv-free-free-720
https://diamarhuddtanog.wixsite.com/arpsychanver/post/nulled-authorship-gui-license-utorrent-zip-32-full-windows
https://accorbenztralli.wixsite.com/galneoforte/post/mentor-graphics-pads-viewer-download
https://trello.com/c/jrh17JNo/40-fios-tv-one-mini-activator-exe-utorrent-windows-pro
https://inoustituryc.wixsite.com/feigemifi/post/cities-skylines-repack-masquerade-7z
marndap (Friday, 14 January 2022 19:24)
marndap f91c64177c http://jumpa-ungaran.com/sosmed/read-blog/331
http://pretivemti.unblog.fr/2021/11/26/fire-pro-wrestling-world-download-hack-pamseann/
https://moore1996.wixsite.com/blacalpromeq/post/adobe-premiere-pro-cc-2015-v9-0-crack-64-bit
https://www.drupal.org/files/issues/2021-11-27/annvalg.pdf
http://durchventaded.unblog.fr/2021/11/26/updated-2009-05-16-fallfrom-heaven-2041n-exe/
https://www.homify.in/ideabooks/8477206/erase-una-vez-la-vida-1x01-torrent
https://seesaawiki.jp/relarepi/d/Save 64% On Access To The World S Fastest And Most Secure VPN
https://kit.co/metkingplanlust/pho-shop-cc-license-rar-32-utorrent
https://www.homify.in/ideabooks/8477207/fundy-designer-v6-crack-for-12
https://fdocuments.in/document/ravi-kissen-1-tamil-full-movie-hd-1080p.html
http://seidayranbi.unblog.fr/2021/11/26/extra-quality-ship-of-theseus-2-hd-movie-download-720p-movies/
https://sihealdiachlor.diarynote.jp/202111270321349904/
https://trello.com/c/8pxVDBvA/11-optisystem-11-key-rar-x32-torrent-crack-full-version
https://www.drupal.org/files/issues/2021-11-26/Kimikoyo-rejoint-le-blog-.pdf
https://chirevouhi.mystrikingly.com/blog/star-wars-battlefront-3-free-radical-download
https://cdn.thingiverse.com/assets/a7/3b/85/a3/24/swordkafll965.html
http://www.suaopiniao1.com.br//read-blog/10224
https://www.homify.in/ideabooks/8477208/full-blazingtools-perfect-keylogger-v1-6-2-0-datecode-11232004-keygen
https://kit.co/lesasurto/ls-magazine-ls-dreams-ls-land-01-pretty-animals-05-avi-mp4-full-watch-online-dubbed-dvdrip-english-full
http://newsspinanda.unblog.fr/2021/11/26/veerbalarastogimolecularbiologyfreedownloadpdftemp/
https://wowonder.vaneayoung.de/read-blog/4587
http://fighnena.yolasite.com/resources/The-Desire-2012-download-720p-movie.pdf
https://i9social.com/upload/files/2021/11/jvrLoXKnTqabGowuPHhK_26_e2a092f98043e8de80f30793a3338e8f_file.pdf
https://s3.amazonaws.com/media.muckrack.com/portfolio/items/14857653/solucionarioecuacionesdiferencialesdenniszill6edic.pdf
https://dokumen.tips/data-analytics/aaayiaayiaayiaayiaayi-aayiaaayi1pdf-google-drive.html
https://igortitovpaq.wixsite.com/siolicyma/post/society-full-movie-in-hd-1080p
https://cdn.thingiverse.com/assets/9c/46/68/8d/fa/Devi__The_Little_Goddess_1080p_Download_Movies.html
https://www.homify.in/ideabooks/8477209/issaq-movie-download-in-hindi-mp4
https://sonetspace.com/read-blog/1874
https://kit.co/chohatpile/kia-c3-00-blacklist-cracked-final-full-utorrent-x32-zip-license
bakutaf (Friday, 14 January 2022 19:42)
bakutaf f91c64177c https://terdaberre.mystrikingly.com/blog/raja-ki-aayegi-baaraat-watch-online-mp4-dual-hd-dubbed-blu-ray
http://ofconworrpu.unblog.fr/2021/11/28/free-download-xpango-credit-generator-v3-5/
https://www.pixnet.net/pcard/6938360323acf2ebe8/article/dfbce020-505c-11ec-90c6-612ee87d0855
https://trello.com/c/nLmfVEPI/25-luck-cracked-build-pc-download-64bit-full-iso
https://www.homify.in/ideabooks/8499479/3g-2-telugu-full-movie-free-download
https://uploads.strikinglycdn.com/files/b3820f04-1175-45b8-a45f-dd537922904d/Crack-SimpleLPR-2-2-9.pdf
http://htacbiobern.yolasite.com/resources/The-Agneepath-Full-Movie-In-Italian-Free-Download.pdf
http://kaibrital.yolasite.com/resources/Erwin-73rar.pdf
https://cdn.thingiverse.com/assets/b5/e4/a4/19/49/Wambini-Predicts-sub-download.pdf
http://sondverli.yolasite.com/resources/tamil-movie-Saajan-Chale-Sasural.pdf
http://xdelerphehop.unblog.fr/2021/11/28/ishqiya-movie-kickass-download-amadoly/
https://docs.google.com/viewerng/viewer?url=elonlife.com.br/read-blog/1346
http://coytintnassi.unblog.fr/2021/11/28/hack-daz3d-measure-metrics-for-daz-studio-daz-16684-installer-schawdaphn/
http://lupelraness.unblog.fr/2021/11/28/artcam-2019-scaricare-codice-di-attivazione-64-bits/
https://www.homify.in/ideabooks/8499480/souled-american-sonny-rar-files
https://uploads.strikinglycdn.com/files/0c297d88-3597-4731-8ecb-9d77400b49b1/Dicom-Cd-Viewer.pdf
https://media.muckrack.com/portfolio/items/14854889/the-Tang-shan-jie-quan-dao-full-movie-in-italian-f.pdf
https://cdn.thingiverse.com/assets/7b/7c/5f/d9/a1/Older4me-Luiggi-Feels-Like-Heaven.pdf
http://sentportthi.yolasite.com/resources/Msi-Bluetooth-Stick-Pc2pc-Software-Download.pdf
https://www.homify.in/ideabooks/8499483/wondershare-video-converter-ultimate-5-6-1-1
https://communalhigh.weebly.com/maschine-expansion-byte-riot-v200-mac-os-x--crack.html
https://www.homify.in/ideabooks/8499472/psa-diagbox-keygen-idm
https://docs.google.com/viewerng/viewer?url=sanatkedisi.com/sol3/read-blog/47661
https://trello.com/c/0WUmZFjR/30-fmrte-143-1-key-exe-file-free-64-pc-keygen
https://www.pixnet.net/pcard/25703601c2cedd3c88/article/6b152c40-5058-11ec-bd37-977506d45932
https://www.homify.in/ideabooks/8498412/sularso-pompa-dan-kompresor-pdf-65-guard-warcraft3-blon
https://cdn.thingiverse.com/assets/12/2c/73/5f/c5/Gli-ultimi-sei-minuti-movie-in-italian-free-download.pdf
https://docs.google.com/viewerng/viewer?url=gourgia.com/upload/files/2021/11/9fcMRBmR6tD6d2fUhehh_28_142183f09bde71c4c36d9068fa192847_file.pdf
https://naimgarvicacen.wixsite.com/webppatitab/post/michel-katalog-kostenlos-rar-full-edition-ebook-epub-utorrent
https://kit.co/hanmadercmi/y-m-i-yeh-mera-india-4k-watch-online-kickass-blu-ray-720
ignfay (Saturday, 15 January 2022 01:37)
ignfay f91c64177c https://fdocuments.ec/document/math-homework-and-remembering-grade-5.html
https://www.drupal.org/files/issues/2021-11-27/ACDSee-5000025-PowerPack-With-PicaView-20-Keygenl.pdf
https://pdfslide.net/lifestyle/the-simpsons-season-20-21-22-23-24-25-26-27-threesixtyp-rar.html
https://kostokowmand1979.wixsite.com/subtkudissui/post/el-mariachi-suona-subtitles-subtitles-mkv-video-1080-torrents-mkv
https://randtemlocynob.wixsite.com/sandprodexow/post/torrents-creature-mkv-english-dubbed
https://seesaawiki.jp/sikorteza/d/Soutenmoviefreedownloadinhindihd
https://seesaawiki.jp/reterslentest/d/Bukvar Decijih Prava Pdf Download !LINK!
https://unusid.wixsite.com/corpelojar/post/driver-reviver-pro-5-25-1-2-crack-product-key-free-download
https://resttrucrathe.weebly.com/the-art-of-magic-the-gathering--ixalan-download-pdf.html
https://secriit.com/upload/files/2021/11/iY4v2frJtyjEjmO3ZP4b_27_5faf25c08ad5f84054e5b9eb4e214ea4_file.pdf
https://vdocuments.mx/wnlo-svk-poyng-r-us-.html
https://pdfslide.net/education/rambo-3-full-movie-in-hindi-free-download-utorrent.html
https://social.zapus.com.br/read-blog/50016
https://uploads.strikinglycdn.com/files/71e7771a-3aff-4bbc-b730-4aa569fcbab1/Hugo-Old-Tyme-Religion-2011.pdf
https://www.pixnet.net/pcard/95394602c3f0b249cc/article/bb9111c0-4f38-11ec-9c3e-a1e86f4580e3
https://ofblacbehand.weebly.com/uploads/1/3/9/2/139264885/fangbone-movie-mp4-download.pdf
https://trello.com/c/N7jBs2gu/28-clueless-up-nulled-professional-64bit-iso-activation-full-version-torrent
https://disnockguba.weebly.com/uploads/1/3/9/5/139516882/jennifer-aniston-wanderlust-uncensored-350mb.pdf
https://pdfslide.us/education/peel-universal-smart-tv-remote-control-v10752-pro-latest.html
https://oxasanin.mystrikingly.com/blog/nulldc-1-6-full-version-15
https://www.pixnet.net/pcard/8619160364b087b6e5/article/c7e3a7e0-4f38-11ec-9246-73c662006874
https://favooh.com/upload/files/2021/11/MpaXUnghWZREibMSUTqq_27_4523bea3334f703dc41ec0f3324b2a09_file.pdf
https://lighkapemo.mystrikingly.com/blog/essay-topics-for-crime-and-punishment
https://wakelet.com/wake/r_USCJJzJ1kANE2qag6-E
https://trello.com/c/oIc6VeXz/15-viva-robin-hood-movie-3-hd-download
https://trello.com/c/Y9IAWNxQ/29-skip-beat-korean-drama-torrent-download
https://exlapivimeama.wixsite.com/ceppayscorte/post/avatar-2009-extended-collectors-edition-1080p-bluray-x265-10bit-hevc-aac-5-1-joy-utr-29
http://daraztube.com/upload/files/2021/11/zrovVOyRt59ZKAc98zNb_27_3d6722c576e77729151616af1adccda5_file.pdf
https://uploads.strikinglycdn.com/files/ea038f73-071a-4c02-96ef-182a978330a2/Livin-It-Up-Download-Ja-Rule.pdf
https://neficonca.mystrikingly.com/blog/le-rarbeiten-n-ultimate-pc-full-version-32bit-rar-activation-keygen
hissjam (Monday, 17 January 2022 20:19)
hissjam dd23f8915e https://wakelet.com/wake/XTVH9Rw-XO7rHOIDgKtS1
https://wakelet.com/wake/PSh72gPEYpu-UQbwiQfn6
https://coub.com/stories/2630482-need-for-speed-hot-pursuit-remastered-v1-0-3-yuzu-emu-for-pc-multi10-fitgirl-repack-s-cracked
https://coub.com/stories/2630483-overloud-breverb-2-v2-0-9-r2r-ullofar
https://coub.com/stories/2630484-__full__-jutta-burggraf-teologia-fundamental-pdf-15
https://coub.com/stories/2630486-repack-mopar-head-porting-templates
https://coub.com/stories/2630485-extra-quality-mastercam-x5-hasp-crack-62l
https://coub.com/stories/2630487-top-character-rig-cinema-4d-minecraft-download
https://coub.com/stories/2630488-masamune-shirow-artbook-pdf-download-upd
https://coub.com/stories/2630489-zte-16-digit-unlock-code-calculator
https://coub.com/stories/2630490-roadmaster-granite-peak-bicycle-parts
https://coub.com/stories/2630491-my-mix-lab-mymixlab-luca-pretolesi-mix
https://coub.com/stories/2630492-best-tyler-brule-to-the-rescue
https://coub.com/stories/2630493-best-kurui-naku-ch7-pdf-google-dzzz
https://coub.com/stories/2630494-frameforge-previz-studio-3-crack-petlyo
https://coub.com/stories/2630495-adobe-after-effects-cc-2018-18-1-1-16-x64-patch-rar-geffque
https://coub.com/stories/2630496-tecdoc-online-free-free
https://coub.com/stories/2630497-junior-porciuncula-w-10-kontakt
https://coub.com/stories/2630498-vocalign-pro-tools-crack-26-portable
https://coub.com/stories/2630499-top-d21-fun-avengers-age-of-ultron-2015-1602419255-mp4
https://coub.com/stories/2630500-james-cameron-avatar-the-game-pc-keygen-download-best
https://coub.com/stories/2630502-repack-zone-43-1-0-3-hack-pc
https://coub.com/stories/2630503-best-baa-baaa-black-sheep-movie-tamil-subtitle-free-download
https://coub.com/stories/2630504-free-toto-rosanna-torrent
https://coub.com/stories/2630505-the-himmatwala-in-hindi-free-download-amsterdam-motard-lar-bakjen
https://coub.com/stories/2630501-fixate-2-cookbook-pdf-free
https://wakelet.com/wake/kG8RE1MZ8vabMT2ZJ6mCs
https://wakelet.com/wake/mzn_J_RTQQFThO_ANROMi
https://wakelet.com/wake/NVdLQxN-QUDImwS6G7bBx
https://wakelet.com/wake/XzRcm_6l1Z0Q8CDTD7wS7
zylyger (Monday, 17 January 2022 20:44)
zylyger dd23f8915e https://coub.com/stories/2754960-abomination-book-report-javlat
https://coub.com/stories/2754958-ptc-cocreate-v17-magnitude-railwyne
https://coub.com/stories/2754957-repack-xforce-keygen-maya-2017-activation
https://coub.com/stories/2754955-amadeus-1984-directors-cut-720p-brrip-x264-yify-subtitles-dalhero
https://coub.com/stories/2754956-adobe-photoshop-cs9-serial-numberl-link
https://coub.com/stories/2754954-links-club-all-your-links-take-safe
https://coub.com/stories/2754953-full-boom-boom-1080p-hd-video-song
https://coub.com/stories/2754952-watch-sultan-movie-online-720p-rahebirg
https://coub.com/stories/2754950-royal-sweets-incejani
https://coub.com/stories/2754951-solaris-bill-johnston-epub-24-fix
https://coub.com/stories/2754949-repack-dsm-4-tr-pdf-completo
https://coub.com/stories/2754947-topaz-sharpen-ai-1-4-3-x64-queniell-giavfeli
https://coub.com/stories/2754948-netflix-1-year-premium-account-generator-serial-key-keygen-link
https://coub.com/stories/2754946-steam-list-part-2-yamzeno
https://coub.com/stories/2754945-free-cleaning-services-proposal-template-better
https://coub.com/stories/2754939-memorial-service-program-templates-free-new
https://coub.com/stories/2754943-the-last-stand-720p-yify-english-subtitles-__top__
https://coub.com/stories/2754944-xfer-serum-serial-number-24-full
https://coub.com/stories/2754942-upd-ac-cent-tchu-ate-the-positive-pdf
https://coub.com/stories/2754941-high-quality-download-dragon-world-tamara-macfarlane-pdf
https://coub.com/stories/2754940-hot-distancia-maxima-entre-pilares-de-hormigon
https://coub.com/stories/2754938-upd-farewell-my-concubine-1993-bluray-1080p-ac3-x264-chd-epub
https://coub.com/stories/2754937-global-cold-storage-capacity-report-pdf
https://coub.com/stories/2754936-extra-quality-download-gx-works-2-keygens
https://coub.com/stories/2754935-sniffy-download-free-layhal
https://coub.com/stories/2754934-pubg-mobile-hile-no-root-xyliwiko
https://coub.com/stories/2754933-neat-video-pro-5-1-5-link-crack-serial-key-full
https://coub.com/stories/2754932-the-sims-4-rrrrrr-mail-ru
https://coub.com/stories/2754931-a-meeting-q-what-are-your-goals-for-future-years-top
https://coub.com/stories/2754930-kpbr-2014-malayalam-pdf-11-opekail
tarneer (Monday, 17 January 2022 21:36)
tarneer dd23f8915e https://wakelet.com/wake/_5v9jovcEGuUBQsUjSZgq
https://wakelet.com/wake/gFcYO8uIAuTZ35Msdq54g
https://wakelet.com/wake/MB0gvWRpAqdxOktIRnxcp
https://wakelet.com/wake/fS-GTL5j_hccGpAG78IUP
https://wakelet.com/wake/lwi6dEA_uoF-MPqh8jU8C
https://wakelet.com/wake/PFPeL9OkMwYATPvsBhafx
https://wakelet.com/wake/6u1q6X1cZFAz0yJXifeaJ
https://wakelet.com/wake/9DRzBQWrgTgcUJ70vmxRw
https://wakelet.com/wake/TDzJYTbHkBF_tFL7j6DbI
https://wakelet.com/wake/TwAQ18CfrOEU-ATA9i-aq
https://wakelet.com/wake/0VH6j1o6OHSyfmqEOYbzp
https://wakelet.com/wake/F2DS-7Mh2KFW0l8VO0hkr
https://wakelet.com/wake/WZ7qVjKPw1OIIH7_rO1nS
https://wakelet.com/wake/RZgEsWagg7G5DNrAJOIx7
https://wakelet.com/wake/6zoC1Blguscyj0ksrQnwC
https://wakelet.com/wake/iUQQnrxnKeci0SO2f5K0o
https://wakelet.com/wake/trCX6ckoLcNBeA4DoLtiH
https://wakelet.com/wake/7rnFCZQ5A8gRsrlWtzlNj
https://wakelet.com/wake/J-qU6X9U1jJVZF5AKIw43
https://wakelet.com/wake/aSYO3lww4wCnyZ24yWPJo
https://wakelet.com/wake/JRgX70KWjoPILvewVyJLi
https://wakelet.com/wake/IiAwz_44J2WNqHYlTErNC
https://wakelet.com/wake/XjgLS4dhX8aCvg8jXflm6
https://wakelet.com/wake/wsAcUmZJCgOTrGhBqh9Ml
https://wakelet.com/wake/1m_POZBDB0zf4pHE2paF9
https://wakelet.com/wake/oxXhVOzaTXREXS3npA1pb
https://wakelet.com/wake/0seK6dhwskoiVgMO_WwF_
https://wakelet.com/wake/W4AZ0Co9Q-rIniNL9_19k
https://wakelet.com/wake/jMZM21BUHk97q-U1SFje8
https://wakelet.com/wake/rYie0VSyez8kz8o_F0xrA
paxttorb (Monday, 17 January 2022 22:23)
paxttorb dd23f8915e https://wakelet.com/wake/X7FWpNRFityQ7GQnQ8Y0a
https://wakelet.com/wake/aI6RJgXxYm2yqlOlShAaK
https://wakelet.com/wake/yCRqzEm8Cs8CtLA8BbQhh
https://wakelet.com/wake/GArPy479tFgQvrbXYQU3l
https://wakelet.com/wake/zYPnAbn541fBPVPJ8clM2
https://wakelet.com/wake/rMdKeZ7bDVKul72osql61
https://wakelet.com/wake/oBsXRh2QQQPe-irhK5f76
https://wakelet.com/wake/y-G3exRj-61tNLRsfjY5J
https://wakelet.com/wake/DCz3XTkR8h1Sy1lmD2YEb
https://wakelet.com/wake/_AEonMlI0xBhVvGB9QNFT
https://wakelet.com/wake/OP3w8aNUyL8Ryq3pA-zoM
https://wakelet.com/wake/05EVfVjXgPao6PHtfCEog
https://wakelet.com/wake/FK_CLMxtsfLJwlC4nNW45
https://wakelet.com/wake/pwB0ClGe1F_Np-dbhGW7x
https://wakelet.com/wake/2cxHYBH4rR2yTJ6tkzxU9
https://wakelet.com/wake/tuU258rnx5W2bazxohjly
https://wakelet.com/wake/fQB6aao9QQ84XuTYAWbSB
https://wakelet.com/wake/JtxeJmv7-9kRkOqhICQpF
https://wakelet.com/wake/t3k1i7_1AYWkodJt9ivQv
https://wakelet.com/wake/CiQ0Gc7O_Ls7RsbAHgeyH
https://wakelet.com/wake/lk9HpZNiz5AwUAAQQW4oH
https://wakelet.com/wake/sgWi1fCxn6KPoYcQS2ywF
https://wakelet.com/wake/wanEc48qfOh2hKrMIfSaj
https://wakelet.com/wake/Wxau47ocVoO48yToayzAg
https://wakelet.com/wake/mPMp_8AGzAv9ZinF7NFPL
https://wakelet.com/wake/wkLgclG95f7Ns9SE2I8lH
https://wakelet.com/wake/rqaz_gzHcbbTX_VR5Ooey
https://wakelet.com/wake/ZUUTC05j6iSmkQ_kiBKm6
https://wakelet.com/wake/AzvrE7qsiQufy60uGvJnu
https://wakelet.com/wake/2swUn8fw_P9sk3254gTwH
bernike (Monday, 17 January 2022 22:47)
bernike dd23f8915e https://coub.com/stories/2806545-madari-song-by-vishal-dadlani-free-mp3-download-exclusive
https://coub.com/stories/2806544-mehndi-rachan-lagi-banna-thare-naam-ki-mp3-download-work
https://coub.com/stories/2806543-top-the-conjuring-1080p-bluray-x264-yify
https://coub.com/stories/2806542-loving-kindness-book-pdf-_best_
https://coub.com/stories/2806540-cheap-thrills-320kbps
https://coub.com/stories/2806538-how-to-add-table-of-figures-in-google-docs-__top__
https://coub.com/stories/2806534-quickbooks-pro-2013-all-versions-activator-license-plus-full-software-links-free-here-best
https://coub.com/stories/2806525-abc-delf-b2-pdf-download-elodah
https://coub.com/stories/2806522-the-great-hall-of-the-bulls-description-waltmona
https://coub.com/stories/2806518-canterbury-tales-prologue-short-answer-questions-ballis
https://coub.com/stories/2806519-download-bad-naam-hd-720p-full-movie-in-hindi-best
https://coub.com/stories/2806517-navy-eisenhower-jacket-rank-placement-harara
https://coub.com/stories/2806513-avast-internet-security-final-licence-avastlic-2038506491
https://coub.com/stories/2806514-alienacionjulioramonribeyrocuentocompletopdfdownload-branmalv
https://coub.com/stories/2806502-abelssoft-ssd-fresh-2020-torrent-link
https://coub.com/stories/2806511-honeydukes-jelly-bean-flavor-guide-hot
https://coub.com/stories/2806507-kreditnaya-sistema-obrazovaniya-plyusi-i-minusi-exclusive
https://coub.com/stories/2806503-__hot__-asavea-teeth-whitening-pen-instructions
https://coub.com/stories/2806501-animaker-voice-free-karndara
https://coub.com/stories/2806497-download-film-perang-dunia-ke-2-gratis-porrayl
https://coub.com/stories/2806498-the-bhagavad-gita-eknath-easwaran-pdf-download-chanmol
https://coub.com/stories/2806494-__hot__-afilmywap-in-lord-of-the-rings-the-fellowship-of-the-ring-2001-hindi-dubbed-movie-480
https://coub.com/stories/2806488-hot-hyderabad-blues-2-1-2-3-720p-in-dual-audio-hindi
https://coub.com/stories/2806490-billy-graham-book-angels-god-s-secret-agents-pdf-wanbroo
https://coub.com/stories/2806489-repack-godus-weyworld-treasure-temple
https://coub.com/stories/2806486-21-day-fix-workout-videos-free-frideri
https://coub.com/stories/2806484-link-how-to-make-wands-of-horus
https://coub.com/stories/2806483-best-greek-mythology-book-edith-hamilton-pdf
https://coub.com/stories/2806482-american-hustle-mp4-download-frabeth
https://coub.com/stories/2806479-robot-chicken-complete-series-torrent-download-extra-quality
zerfrit (Monday, 17 January 2022 23:13)
zerfrit dd23f8915e https://wakelet.com/wake/46sETth1b7m85qBUjvm3y
https://wakelet.com/wake/OqEkO7BwYZjzR4Ng5gcc9
https://wakelet.com/wake/l-QvwVhdzbXgfgQty_1u2
https://wakelet.com/wake/65p65AztumiQUOytI6ZDL
https://wakelet.com/wake/L8fjny4_BjUIWmoL6OotP
https://wakelet.com/wake/C1pMl5e-0hVJrPpSEBO1J
https://wakelet.com/wake/ixhun6BpA-w3axwIwd425
https://wakelet.com/wake/yEeYR2IdyKeTKtBU9UV_J
https://wakelet.com/wake/VyKpomcrjTf9KjIrXNKC7
https://wakelet.com/wake/8hI2xplPK2WokACKzJk-v
https://wakelet.com/wake/qfot46CehUhPEQJoWqnqF
https://wakelet.com/wake/8ifGb2uB9vzKarT2a0E5Y
https://wakelet.com/wake/puJxHI9CTg2A6v4Zc4Lkn
https://wakelet.com/wake/zyJMJpOMlB9PUF-esJs3s
https://wakelet.com/wake/lXSWjJate1DYuNv-ZHzgf
https://wakelet.com/wake/Z6AJTJ_vR-hJ5tAectFJJ
https://wakelet.com/wake/R4tSRKrKCUjN4mJZmo4xU
https://wakelet.com/wake/SnIpSuhX1PlZE4V5nGNSp
https://wakelet.com/wake/GA7JdjyEUu6qlVA6npd6w
https://wakelet.com/wake/Y6HlH6DPB99R9RTZUKckn
https://wakelet.com/wake/xswu4e4kFgMIz7n50-gZs
https://wakelet.com/wake/2rW-uLhOvydhVKnAeog-q
https://wakelet.com/wake/muYaDsom4LKc7C0ClTdIx
https://wakelet.com/wake/fGLbCHzXZDxEJ5udGhPYQ
https://wakelet.com/wake/s4D83-mwDt0LeR0jGl7KV
https://wakelet.com/wake/q_8RvAdeisXrnK__ea7O7
https://wakelet.com/wake/khiahYRqmtYSWCQoVxChG
https://wakelet.com/wake/6hxkHxr91INcFCSjJI0j6
https://wakelet.com/wake/GymnRqRr41JAOjhh3xRRf
https://wakelet.com/wake/e_BhHk7p2M-aTbapP9eQn
odolgar (Monday, 17 January 2022 23:35)
odolgar dd23f8915e https://coub.com/stories/2760648-audia7_repair_manual_pdf
https://coub.com/stories/2760645-top-fujitsu-irmc-license-key
https://coub.com/stories/2760646-ch4-saya-shshsh-shschshschsh-google-drive-vyrdbett
https://coub.com/stories/2760636-is-western-cherokee-a-federally-recognized-tribe-feremel
https://coub.com/stories/2760637-verified-xforce-keygen-autocad-lt-2005-64-bit-download
https://coub.com/stories/2760632-substance-painter-2020-crack-patched-with-activation-code-for-windows-and-mac
https://coub.com/stories/2760628-free-free-cute-printable-monthly-calendar-2015-pdf
https://coub.com/stories/2760627-stephen-covey-mission-statement-worksheet-upd
https://coub.com/stories/2760625-young-justice-season-2-episode-8-720p-download-top
https://coub.com/stories/2760622-the-rime-of-the-ancient-mariner-annotations-pdf-exclusive
https://coub.com/stories/2760612-chemical-basis-of-life-worksheet-answers
https://coub.com/stories/2760620-ultramon-v3-0-10-incl-serial-hb-keygen-portable-129311
https://coub.com/stories/2760615-transcribe-crack-torrent-burrono
https://coub.com/stories/2760609-cabelas-dangerous-hunts-2013-patched-crackrar
https://coub.com/stories/2760608-preludio-de-adios-montez-pdf-free-verified
https://coub.com/stories/2760603-download-ftpmanager-pro-v8-v8111-unk-64bit-os90-ok14-user-hidden-bfi-ipa-queekalv
https://coub.com/stories/2760601-jamiroquai-greatest-hits-mp3-16-joajacy
https://coub.com/stories/2760598-link-canon-eos-solution-disk-download-mac
https://coub.com/stories/2760595-lesson-6-homework-practice-use-the-pythagorean-theorem-answer-key
https://coub.com/stories/2760596-filhaal-720p-hd-_hot_
https://coub.com/stories/2760592-automailer_2_2-9_-tnt-dmg
https://coub.com/stories/2760585-new-vdmx-serial-mac-keygen-full-download
https://coub.com/stories/2760584-muskurahat-in-hindi-download-upd-torrent
https://coub.com/stories/2760582-8startbutton-v2-4-2
https://coub.com/stories/2760578-new-genetic-code-table-answer-key
https://coub.com/stories/2760577-top-pearson-introduction-to-chemistry-answers
https://coub.com/stories/2760576-apex-us-government-and-politics-1-1-3-answers-upd
https://coub.com/stories/2760574-exclusive-parallels-desktop-business-edition-v16-0-1-48919-pre-cracked-macos
https://coub.com/stories/2760569-exclusive-disk-drill-3-crack-macos-macosx
https://coub.com/stories/2760566-portable-sexe-gratuit-blond-anal
marfara (Monday, 17 January 2022 23:58)
marfara dd23f8915e https://wakelet.com/wake/gPp7hERhC4UeRnGF14RrQ
https://wakelet.com/wake/BXjd-lb5ZhlRvym4RDnyy
https://wakelet.com/wake/19Rggpl30eUYnwagN1RDV
https://wakelet.com/wake/zzjt16vgLK3x-NSdUDV8l
https://wakelet.com/wake/8pQi9YomMULhjuiGeGtrr
https://wakelet.com/wake/ActfAGu44YIRFJY_04a2Z
https://wakelet.com/wake/EfDxWwPhB3yjRMZmsPETP
https://wakelet.com/wake/TGHu1HFzXqGxE-r78Q6uG
https://wakelet.com/wake/3dw-Q1OBBI4I8s3cP0DFv
https://wakelet.com/wake/63RqnOX22Dk8PgvBaQooA
https://wakelet.com/wake/O5SVqxe89ZLU0ISUMfyJ7
https://wakelet.com/wake/4nv_s6WEfjV08K73LnC77
https://wakelet.com/wake/SgmvP3b2FBFZOxwiLKlj3
https://wakelet.com/wake/H0hQrDWgpSV1_nUVJSkUh
https://wakelet.com/wake/IdC3-bLWMjBIzSgqidSTZ
https://wakelet.com/wake/DpuoyxQnpqP6vhYSP35HN
https://wakelet.com/wake/QMhiiSG3ARM8kTdQHdWuc
https://wakelet.com/wake/vV-4pasylK_qcadFtlMvQ
https://wakelet.com/wake/9Y-5aYHsTnHQGDSlLyb6-
https://wakelet.com/wake/TKfbxagtM_bNaFvKUOD1F
https://wakelet.com/wake/1-W0MFV2CKMFtX6e0unZM
https://wakelet.com/wake/gTiBLREgVTPGePTq2uUNV
https://wakelet.com/wake/FvxTMoU7DbimCHpHI1blM
https://wakelet.com/wake/nxQh_3c0oH1aGaur7vine
https://wakelet.com/wake/-AZq8LiI8nVDH8B5jwlb2
https://wakelet.com/wake/qzjCbpndZ2N3BMGo12EST
https://wakelet.com/wake/HPh8Rcuvd88O2tVgUN8_r
https://wakelet.com/wake/-LP384r32agjr85n9B1q1
https://wakelet.com/wake/7V6qV3npkSDIRiE-6obsg
https://wakelet.com/wake/RGACrqtdf1vN7xVzGXrJa
gonlea (Tuesday, 18 January 2022 00:44)
gonlea dd23f8915e https://coub.com/stories/2615301-repeated-comparatives-and-double-comparatives-grammar-pdf-idalmigu
https://coub.com/stories/2615300-adobe-photoshop-lightroom-classic-cc-2019-v8-3-1-with-cracked-__link__
https://coub.com/stories/2615299-corel-windvd-pro-2010-v1005163-with-full-working-key-gen-wailalay
https://coub.com/stories/2615298-best-eyes-on-the-prize-online-gratuito
https://coub.com/stories/2615297-to-kill-a-mockingbird-unit-test-review-answers-full
https://coub.com/stories/2615296-free-gastro-google-drive
https://coub.com/stories/2615295-__hot__-download-fxpansion-bfd2-full-version
https://coub.com/stories/2615294-a-startup-de-100-dolares-pdf-__exclusive__
https://coub.com/stories/2615293-photograv-2-11-rar
https://coub.com/stories/2615292-blade-runner-2049-english-mp4-1080p-download-movies-new
https://coub.com/stories/2615291-one-block-wonder-design-helper-2021
https://coub.com/stories/2615290-best-schshschshsh-peerless-battle-spirit-277-schshschshsh-schshshsh
https://coub.com/stories/2615289-raajneeti-br-rip-1080p-movie-torrents-work
https://coub.com/stories/2615288-triple-bottom-line-approach-pdf
https://coub.com/stories/2615286-psy-mother-father-gentleman-video-downloadl-nicgot
https://coub.com/stories/2615287-exclusive-yamaha-pitch-fix-free-download
https://coub.com/stories/2615285-syu-young-guitar-pdf-downloadl-_verified_
https://coub.com/stories/2615284-geezime-for-mac-free-download-pheesthk
https://coub.com/stories/2615283-serial-para-karafun-1-10a-full-27-updated
https://coub.com/stories/2615282-descargar-el-archivo-psdkeys-30_psd_plastic_mockup_templates-zip-1-84-gb-en-modo-gratuit-chruri
https://coub.com/stories/2615281-ideneb-download-no-torrent-benejan
https://coub.com/stories/2615273-depeche-mode-emax-samples
https://coub.com/stories/2615279-top-baikal-films-krivon-happy-boys-2-avi
https://coub.com/stories/2615280-__full__-business_cards_bundle_35-gfxdrug-com-zip-gfxdrug-com-former-adobedownload-org
https://coub.com/stories/2615278-analyzing-shifts-in-demand-worksheet-answers-anjeeverz
https://coub.com/stories/2615277-love-me-chap12-pdf-vgooglev-diskas-better
https://coub.com/stories/2615276-texas-food-handlers-card-test-answers-gelataw
https://coub.com/stories/2615275-__exclusive__-klayout-for-mac
https://coub.com/stories/2615274-waves-11-crack-patch-install-gamadarkh
https://coub.com/stories/2615272-boycotting-the-olympics-claedel
blafavy (Tuesday, 18 January 2022 01:06)
blafavy dd23f8915e https://wakelet.com/wake/rI2XGdDAob98wdoPFPQSR
https://wakelet.com/wake/NGl-H6H1puOA3Duq7uyAH
https://wakelet.com/wake/n054ruGCFeEZet4aoPy-1
https://wakelet.com/wake/yZrlfDMRAB5dp7iCKLBKv
https://wakelet.com/wake/iH5A1VcPGb6LOz17YtK1K
https://wakelet.com/wake/kbv0rilgMqzpS7OcMlho4
https://wakelet.com/wake/3cTsCFIDjtbUD-ZErSY7_
https://wakelet.com/wake/AXARit1QBYiqhWU6KvYpu
https://wakelet.com/wake/ePCtqZmLajMm0_K8WEM8h
https://wakelet.com/wake/ypdGOdUhJOk3jGjFYT2Cb
https://wakelet.com/wake/Av5y2wmxDq4yk9ZHpenca
https://wakelet.com/wake/z1fjppG4B1HyiDPXbRSeT
https://wakelet.com/wake/5-Vd_d4q-uvHuem4n6K8j
https://wakelet.com/wake/nO7Fw-Thu9KwYYTT7Flm0
https://wakelet.com/wake/MjUN_4qDuzgegSLJOZzb7
https://wakelet.com/wake/ZTagiK1prc-E8cDZpMZ8t
https://wakelet.com/wake/xsy0qEa6sa5X2ynSUbetu
https://wakelet.com/wake/dmRZuuiFlgRX3ylOiX6QK
https://wakelet.com/wake/8019OVV5KPxFYyC1O-Jyv
https://wakelet.com/wake/SOUfgmU-8tIzBTlHcOqBc
https://wakelet.com/wake/siI4-nzjQzuLOf26wMDG4
https://wakelet.com/wake/ZNz_fGxXk66GRaIwSfhZ8
https://wakelet.com/wake/rgsgBQOlUih6a_0_7DcY8
https://wakelet.com/wake/nZNcMgBPOvSjTEPwsgPrQ
https://wakelet.com/wake/pjARqzVyjI0BHJO6q9C-8
https://wakelet.com/wake/pse6N0qnIjpWVWk7ryKUD
https://wakelet.com/wake/1s_d0EXEKdoc49hGi_wTU
https://wakelet.com/wake/J73cpbFLeqU1xju2qTkr1
https://wakelet.com/wake/ix64ttqGlXRIVF6_T8Bl5
https://wakelet.com/wake/dVr9xaZnjvtIweULKHf8o
blafavy (Tuesday, 18 January 2022 01:06)
blafavy dd23f8915e https://wakelet.com/wake/rI2XGdDAob98wdoPFPQSR
https://wakelet.com/wake/NGl-H6H1puOA3Duq7uyAH
https://wakelet.com/wake/n054ruGCFeEZet4aoPy-1
https://wakelet.com/wake/yZrlfDMRAB5dp7iCKLBKv
https://wakelet.com/wake/iH5A1VcPGb6LOz17YtK1K
https://wakelet.com/wake/kbv0rilgMqzpS7OcMlho4
https://wakelet.com/wake/3cTsCFIDjtbUD-ZErSY7_
https://wakelet.com/wake/AXARit1QBYiqhWU6KvYpu
https://wakelet.com/wake/ePCtqZmLajMm0_K8WEM8h
https://wakelet.com/wake/ypdGOdUhJOk3jGjFYT2Cb
https://wakelet.com/wake/Av5y2wmxDq4yk9ZHpenca
https://wakelet.com/wake/z1fjppG4B1HyiDPXbRSeT
https://wakelet.com/wake/5-Vd_d4q-uvHuem4n6K8j
https://wakelet.com/wake/nO7Fw-Thu9KwYYTT7Flm0
https://wakelet.com/wake/MjUN_4qDuzgegSLJOZzb7
https://wakelet.com/wake/ZTagiK1prc-E8cDZpMZ8t
https://wakelet.com/wake/xsy0qEa6sa5X2ynSUbetu
https://wakelet.com/wake/dmRZuuiFlgRX3ylOiX6QK
https://wakelet.com/wake/8019OVV5KPxFYyC1O-Jyv
https://wakelet.com/wake/SOUfgmU-8tIzBTlHcOqBc
https://wakelet.com/wake/siI4-nzjQzuLOf26wMDG4
https://wakelet.com/wake/ZNz_fGxXk66GRaIwSfhZ8
https://wakelet.com/wake/rgsgBQOlUih6a_0_7DcY8
https://wakelet.com/wake/nZNcMgBPOvSjTEPwsgPrQ
https://wakelet.com/wake/pjARqzVyjI0BHJO6q9C-8
https://wakelet.com/wake/pse6N0qnIjpWVWk7ryKUD
https://wakelet.com/wake/1s_d0EXEKdoc49hGi_wTU
https://wakelet.com/wake/J73cpbFLeqU1xju2qTkr1
https://wakelet.com/wake/ix64ttqGlXRIVF6_T8Bl5
https://wakelet.com/wake/dVr9xaZnjvtIweULKHf8o
darnish (Tuesday, 18 January 2022 02:08)
darnish dd23f8915e https://coub.com/stories/2777213-instachord-v1-3-0-win-osx-retail-synthic4te-best
https://coub.com/stories/2777207-charvette-guitar-serial-number-lookup
https://coub.com/stories/2777212-cengage-maths-solutions-pdf-download-repack
https://coub.com/stories/2777211-nuts-magazine-april-pdf-patched
https://coub.com/stories/2777210-unicorn-hair-tint-instructions
https://coub.com/stories/2777209-conditional-type-1-2-3-exercises-pdf
https://coub.com/stories/2777208-hot-samsung-sens-x11-driver-download
https://coub.com/stories/2777205-best-trane-xr14-parts-manual
https://coub.com/stories/2777203-pokemon-ultra-sun-wormhole-guide-hot
https://coub.com/stories/2777202-fotos-de-alejandra-fosalba-desnuda-hot
https://coub.com/stories/2777199-portable-adobe-xd-v38-0-12-x64-pre-cracked
https://coub.com/stories/2777201-fyjc-commerce-maths-digest-pdf-freel-best
https://coub.com/stories/2777200-free-never-say-die-alex-rider-downloads-torrent
https://coub.com/stories/2777198-cara-mengakses-internet-melalui-wifi-analyzer-valodar
https://coub.com/stories/2777197-efectua-tu-ministerio-plenamente-epub-14-_verified_
https://coub.com/stories/2777196-7-6-arc-length-sector-area-worksheet-answers
https://coub.com/stories/2777195-why-use-prayer-beads-wyllfirg
https://coub.com/stories/2777192-tglgcharger-minecraft-v1-220-220-unk-64bit-os100-ok14-user-hidden-bfi-ipa
https://coub.com/stories/2777189-roller-coaster-worksheet-on-kinetic-and-potential-energy-zachgle
https://coub.com/stories/2777187-autocad-architecture-2015-crack-top-64-bit-torrent-torrent
https://coub.com/stories/2777185-enigma-recovery-professional-3-6-2-gavrastr
https://coub.com/stories/2777184-nancy-drew-trail-of-the-twister-download-without-license-key-vegbil
https://coub.com/stories/2777182-free-download-episode-1-6-willdae
https://coub.com/stories/2777183-script-breakdown-template-word
https://coub.com/stories/2777181-best-chessok-aquarium-2020-v13-0-0-build-101-crack-application-full-version
https://coub.com/stories/2777180-watch-bhool-bhulaiya-movie-online-free-robbjudg
https://coub.com/stories/2777179-windows-activation-product-key-__link__-download
https://coub.com/stories/2777178-how-to-reset-dsc-panel-caregmo
https://coub.com/stories/2777177-watch-online-no-entry-pudhe-dhoka-aahey
https://coub.com/stories/2777175-cast-the-first-stone-by-david-james-warren-rar-cracked
darnish (Tuesday, 18 January 2022 02:08)
darnish dd23f8915e https://coub.com/stories/2777213-instachord-v1-3-0-win-osx-retail-synthic4te-best
https://coub.com/stories/2777207-charvette-guitar-serial-number-lookup
https://coub.com/stories/2777212-cengage-maths-solutions-pdf-download-repack
https://coub.com/stories/2777211-nuts-magazine-april-pdf-patched
https://coub.com/stories/2777210-unicorn-hair-tint-instructions
https://coub.com/stories/2777209-conditional-type-1-2-3-exercises-pdf
https://coub.com/stories/2777208-hot-samsung-sens-x11-driver-download
https://coub.com/stories/2777205-best-trane-xr14-parts-manual
https://coub.com/stories/2777203-pokemon-ultra-sun-wormhole-guide-hot
https://coub.com/stories/2777202-fotos-de-alejandra-fosalba-desnuda-hot
https://coub.com/stories/2777199-portable-adobe-xd-v38-0-12-x64-pre-cracked
https://coub.com/stories/2777201-fyjc-commerce-maths-digest-pdf-freel-best
https://coub.com/stories/2777200-free-never-say-die-alex-rider-downloads-torrent
https://coub.com/stories/2777198-cara-mengakses-internet-melalui-wifi-analyzer-valodar
https://coub.com/stories/2777197-efectua-tu-ministerio-plenamente-epub-14-_verified_
https://coub.com/stories/2777196-7-6-arc-length-sector-area-worksheet-answers
https://coub.com/stories/2777195-why-use-prayer-beads-wyllfirg
https://coub.com/stories/2777192-tglgcharger-minecraft-v1-220-220-unk-64bit-os100-ok14-user-hidden-bfi-ipa
https://coub.com/stories/2777189-roller-coaster-worksheet-on-kinetic-and-potential-energy-zachgle
https://coub.com/stories/2777187-autocad-architecture-2015-crack-top-64-bit-torrent-torrent
https://coub.com/stories/2777185-enigma-recovery-professional-3-6-2-gavrastr
https://coub.com/stories/2777184-nancy-drew-trail-of-the-twister-download-without-license-key-vegbil
https://coub.com/stories/2777182-free-download-episode-1-6-willdae
https://coub.com/stories/2777183-script-breakdown-template-word
https://coub.com/stories/2777181-best-chessok-aquarium-2020-v13-0-0-build-101-crack-application-full-version
https://coub.com/stories/2777180-watch-bhool-bhulaiya-movie-online-free-robbjudg
https://coub.com/stories/2777179-windows-activation-product-key-__link__-download
https://coub.com/stories/2777178-how-to-reset-dsc-panel-caregmo
https://coub.com/stories/2777177-watch-online-no-entry-pudhe-dhoka-aahey
https://coub.com/stories/2777175-cast-the-first-stone-by-david-james-warren-rar-cracked
benjal (Tuesday, 18 January 2022 02:29)
benjal dd23f8915e https://coub.com/stories/2687429-download-filmora-rar-2021
https://coub.com/stories/2687428-_verified_-la-san-marco-85-practical-manual
https://coub.com/stories/2687427-pre-keyed-muzzle-flashes-free-download-edmoches
https://coub.com/stories/2687426-hot-the-trilogy-and-then-some-by-dan-and-dave-buck
https://coub.com/stories/2687424-ada-keith-alex-threesome-12
https://coub.com/stories/2687423-hot-film-action-full-movie-free-download
https://coub.com/stories/2687422-george-zachariah-kickboxing-hot
https://coub.com/stories/2687420-yogasana-books-in-tamil-free-download-work-pdf
https://coub.com/stories/2687419-nyu-summer-publishing-institute-acceptance-rate
https://coub.com/stories/2687421-suitcase-fusion-7-_verified_-keygen
https://coub.com/stories/2687418-link-descargar-discografia-de-alejandro-sanz-por-utorrent
https://coub.com/stories/2687417-attack-on-titan-tribute-game-android-link
https://coub.com/stories/2687416-upd-13-item-brief-self-control-scale-pdf
https://coub.com/stories/2687415-east-west-fab-four-vst-torrent
https://coub.com/stories/2687413-a-modest-proposal-analysis-by-paragraph-harrpal
https://coub.com/stories/2687414-p-dd-ngt0n-2-2017-480p-blur-y-h-nd-3ngl-sh-x264-k-tm0v-ehd-ch-mkv
https://coub.com/stories/2687412-chinese-civilization-a-sourcebook-2nd-ed-pdf-jarbibi
https://coub.com/stories/2687410-wolf-gourmet-elite-countertop-oven-manual-full
https://coub.com/stories/2687411-updated-aribam-public-administration-pdf-165
https://coub.com/stories/2687406-kuraidori-electric-roaster-oven-manual-_top_
https://coub.com/stories/2687407-__link__-bionic-turtle-frm-part-1-practice-questions
https://coub.com/stories/2687404-download-act-like-a-lady-think-like-a-man-billbota
https://coub.com/stories/2687402-struttura-e-progetto-dei-calcolatori-pdf-best
https://coub.com/stories/2687400-download-amante-por-contrato-rar-eirageo
https://coub.com/stories/2687399-patched-super-jabber-jump-3-apk-mod-unlock-all
https://coub.com/stories/2687398-scaricare-inventor-lt-2005-activator-64-bits-italiano-birthers
https://coub.com/stories/2687397-rus-planner-5d-4-2
https://coub.com/stories/2687396-sniper-3d-mod-apk-v3-30-3-unlimited-coin-diamond-2021
https://coub.com/stories/2687395-emirates-cabin-crew-uniform-history-wancomp
https://coub.com/stories/2687394-falka-comic-download-free
armjoc (Tuesday, 18 January 2022 02:52)
armjoc dd23f8915e https://coub.com/stories/2613370-linplug-saxlab-2-1-0_zip-daclfanc
https://coub.com/stories/2613371-california-dmv-vehicle-transfer-form-pdf
https://coub.com/stories/2613369-animal-crossing-the-movie-720p
https://coub.com/stories/2613367-nerukku-ner-movie-free-download-daryvarim
https://coub.com/stories/2613368-spiritualized-ladies-and-gentlemen-we-are-floating-in-space-download-blogspot-igrataav
https://coub.com/stories/2613366-avid-virtual-instruments-download-better
https://coub.com/stories/2613365-updated-dog-days-s1-shinokun
https://coub.com/stories/2613361-siya-ke-ram-serial-all-episodes-_best_-download
https://coub.com/stories/2613359-formulaire-attestation-pole-emploi-pdf-remplissable
https://coub.com/stories/2613363-civ-6-for-mac-torrent
https://coub.com/stories/2613364-top-global-baba-3gp-download-moonlight-rojadirect
https://coub.com/stories/2613362-mein-to-ghareeb-aadmi-hoon-mehloon-rehta-nahi-ho-free-new-test-v-18-38-mb-test-themeroute-co
https://coub.com/stories/2613360-2021-big-trouble-in-little-edo-full-movie-in-hindi-free-download
https://coub.com/stories/2613358-upd-caldera-forms-wordpress-tutorial
https://coub.com/stories/2613357-link-x-particles-cinema-4d-mac-crack
https://coub.com/stories/2613356-queen-discography-1967-2009-mp3-320-kbps
https://coub.com/stories/2613355-inivis-ac3d-7-2-17-eng-portable-free-download-__top__
https://coub.com/stories/2613354-chishti-rang-qawwali-mp3-cracked-free-download
https://coub.com/stories/2613353-top-multipurpose-business-instagram-banner-vol-2-rar
https://coub.com/stories/2613352-why-does-my-lg-fridge-ice-maker-keep-free-free-zing-up
https://coub.com/stories/2613350-coronation-street-theme-trumpet-sheet-music-lavkama
https://coub.com/stories/2613351-taller-de-escritura-mabel-condemarin-pdf-downloadl-jennasht
https://coub.com/stories/2613349-__exclusive__-titanium-backup-pro-v7-2-0-1-patchedvapk
https://coub.com/stories/2613348-how-to-charge-a-36-volt-battery-system-lovopen
https://coub.com/stories/2613347-navneet-school-atlas-pdf-download-new
https://coub.com/stories/2613345-statik-ve-mukavemet-mehmet-omurtag-pdfl
https://coub.com/stories/2613346-aujourd-hui-je-suis-tapuscrit
https://coub.com/stories/2613344-bome-s-midi-translator-pro-1-7-2-crack-verified
https://coub.com/stories/2613342-2021-junior-miss-pageant-2001-contests-9
https://coub.com/stories/2613343-pgmobile-getres-club-pubg-mobile-elite-pass-600-uc-cardcode-pw-free-pubg-mobile-season-8-gaetverb
padgwenz (Tuesday, 18 January 2022 03:09)
padgwenz dd23f8915e https://wakelet.com/wake/aI14ehH3dk5_bLEU4ffbY
https://wakelet.com/wake/fp1dxtGxE0eM7oC3wsBLS
https://wakelet.com/wake/eE2VmmadIUgR5-WkpbbYV
https://wakelet.com/wake/8njVoGdfE54_Iy2u-zrPw
https://wakelet.com/wake/NxGROxknF-QDKnxUcT2sd
https://wakelet.com/wake/y_JetIEfFO7i-Btsw9y9O
https://wakelet.com/wake/rQ9rMUb7yZh5FYXGwdQIz
https://wakelet.com/wake/bV2nfNu2PW8FmCUXJMOPQ
https://wakelet.com/wake/sOZeysXYIQtnHFrprHvmD
https://wakelet.com/wake/1w4QCeC19yGbbd_x3jBMI
https://wakelet.com/wake/pq5azxcw9xDU33Cnpd5bA
https://wakelet.com/wake/9ZpVOM7GRQwudBoCkj8Qq
https://wakelet.com/wake/uw2ECOoLEu_1uPbfAmTNV
https://wakelet.com/wake/XKUdpbUfnYEUbGt8aXa9x
https://wakelet.com/wake/iZZPFDxkKAbY9KBbtd39b
https://wakelet.com/wake/D26pEzifVawKHTWNFYXM5
https://wakelet.com/wake/1hSGqnmbISetQ1DJi80Yd
https://wakelet.com/wake/CnijwMcaip900Iw_IA31N
https://wakelet.com/wake/hXs1ZpUBR5YgO-MC1Cdck
https://wakelet.com/wake/LVY_unBKE7w0xpMeTm6fM
https://wakelet.com/wake/2cXqewqUGIho6gk7k3BN-
https://wakelet.com/wake/DF5CRQCfHD2BKJfXkuLVv
https://wakelet.com/wake/4zpC0zfceoDh4188V3uzv
https://wakelet.com/wake/J4VSd2__qQ1hB-aLZiaZl
https://wakelet.com/wake/m5gSCj9I0_bTO4Zc5r6b9
https://wakelet.com/wake/cFgv-OuriH-fd_SkCU5GA
https://wakelet.com/wake/ozYRKUfamqVd9lvXp-K-b
https://wakelet.com/wake/OcuUwe7LrKKX3lToWpPUU
https://wakelet.com/wake/U9TWRXLQ9KhIIhG7MnSXf
https://wakelet.com/wake/FgIZ4nOmtouczSMGJbxVh
zirlavr (Tuesday, 18 January 2022 03:32)
zirlavr dd23f8915e https://wakelet.com/wake/Yze3u2S5EqcriFkzGFsDp
https://wakelet.com/wake/aOJ2p0sH7V8zF0KvXIGGg
https://wakelet.com/wake/nGQFPlQGtOyhDAl5aiJ9A
https://wakelet.com/wake/GJVIpnh2dGBQ4MqwIpsHm
https://wakelet.com/wake/MKd463uL7ds_gF4eOxsXR
https://wakelet.com/wake/HeFzrDa_v-2-9OlcMFER0
https://wakelet.com/wake/sCLF_2rXEwA33zcPWzFK0
https://wakelet.com/wake/Rl_8tToES2TJaOvk-3rXJ
https://wakelet.com/wake/dWz9OzOR6ykqWQRHwxODu
https://wakelet.com/wake/lWdG9MymDsB18K0wm4eNY
https://wakelet.com/wake/qrIIDQc0t3SstslI_Td5u
https://wakelet.com/wake/trKRLBtP9Q9iqav3_YCJ8
https://wakelet.com/wake/2rJB351kTQo_FD8B3vCkn
https://wakelet.com/wake/iyHGZmLAx1XnZlAl_OFw-
https://wakelet.com/wake/Mx3XJXhdQCkX_368yg9Xg
https://wakelet.com/wake/yqV7HHPTScAlJTJj5Xfay
https://wakelet.com/wake/3LrVUTaFcs_J2EuoC6_gW
https://wakelet.com/wake/qSF5Wyq92i2sbMm7n8O0n
https://wakelet.com/wake/9KllUoRFo2KhOYbBhmZ9t
https://wakelet.com/wake/yqFfY2M_efstVilvBsH5p
https://wakelet.com/wake/7hiTxnqAX1zmCWed7ZMfA
https://wakelet.com/wake/8AQoqBdHlwS7nZkVkLSnx
https://wakelet.com/wake/r9nI1mdM2T9eohwWcnALU
https://wakelet.com/wake/_VdYR6UurQ4T_oVhiwRFt
https://wakelet.com/wake/gdgn7O5ufjemM64gA8YeE
https://wakelet.com/wake/k_xd1xEfNqZG5ijXYfBfK
https://wakelet.com/wake/BsXmfDQLoqPFVATewDWE_
https://wakelet.com/wake/kRCCW4ctujQMHhrw8kE8S
https://wakelet.com/wake/BHnp4HW7aXZ8Zf5vxeU9z
https://wakelet.com/wake/I77axlEXZftu7OjVReMzo
sakras (Tuesday, 18 January 2022 03:53)
sakras dd23f8915e https://wakelet.com/wake/cdHKSNU7hAyQV8yvJ1jLs
https://wakelet.com/wake/Wrh6jkT4UYecQbbihHH9d
https://wakelet.com/wake/4C4p1xRwM5WIBml2NfI3d
https://wakelet.com/wake/Kq0Ko99tZdLQOGCr_QR6t
https://wakelet.com/wake/dLMeOEyYSaEYz5QCvLaj4
https://wakelet.com/wake/j4FIPNOe9CdrLSu_E5_EF
https://wakelet.com/wake/cEyRLN5IQ1FRA-IXypo3V
https://wakelet.com/wake/U3Q4kdSVGF0yh6T3JgXcs
https://wakelet.com/wake/fuC8GXHSDOW1XElo5xDPY
https://wakelet.com/wake/K3bi-tVx0j6kDa3JMcyfx
https://wakelet.com/wake/CppyTzzV1dZRX5wxsyxP2
https://wakelet.com/wake/DQpiZZV3eSwAloZjhAeie
https://wakelet.com/wake/5SRA2l2YAoa76Ke0-hTMh
https://wakelet.com/wake/02WdjTdZbjRuUnvZZi3pX
https://wakelet.com/wake/ZBLBbZdcQTHzI74po4pus
https://wakelet.com/wake/F3BNJHBfBABH45MgeZo2A
https://wakelet.com/wake/jEZvbw-cQJzstNh-j4Ip-
https://wakelet.com/wake/9BkVWoBpCz2zDVXQh0_KG
https://wakelet.com/wake/4sGBxeDCxOn5eYTUfVyGB
https://wakelet.com/wake/Z_qOyNxikEFGP-SICsByv
https://wakelet.com/wake/MU76ZuDbqrRpL60Mf85JT
https://wakelet.com/wake/bFk6vo7GpayfWJkBO7INy
https://wakelet.com/wake/a0uXsH0bVl543xegXHpXs
https://wakelet.com/wake/dSnjySUtOfIddr79xMsy2
https://wakelet.com/wake/4gCYKfZGfDvACwWLOVTU8
https://wakelet.com/wake/OJ2j3S_8iINHaPbqgoyxq
https://wakelet.com/wake/bMftfvuxp5ac-iOIUITy1
https://wakelet.com/wake/7I3nRSkLlDqV20WVMQ2bG
https://wakelet.com/wake/83JVSSGLPHVeT5WjYsrfV
https://wakelet.com/wake/YXFPGHBula2v2uayfFKEy
meagell (Tuesday, 18 January 2022 04:10)
meagell dd23f8915e https://wakelet.com/wake/KtfjCMO53V15ZmdBMBXTH
https://wakelet.com/wake/IElg_QtExdmnuWtX11kiS
https://wakelet.com/wake/LZvr5GA-JemnK1kyf6kIS
https://wakelet.com/wake/_RtcXCA8bk2tMAosrOGFN
https://wakelet.com/wake/U6-_lslUBtw7ruRVay2xs
https://wakelet.com/wake/_Zofi38v1SMXXRRJXz1oF
https://wakelet.com/wake/kPIFar3Bfb_3dPhrzBWol
https://wakelet.com/wake/tkFFXZ83lqn6etvB8q0Uy
https://wakelet.com/wake/JYE0AURgDxkAghkdAgE_D
https://wakelet.com/wake/w1XNDzJJEffQHnXAKllYx
https://wakelet.com/wake/XcrsHKFB55ifUpkwYwx5V
https://wakelet.com/wake/0ARYW9GtQDH7TPGBot8Pi
https://wakelet.com/wake/clDuWuvfgCz9cRR3chHTc
https://wakelet.com/wake/harg7HLFAX-c2o5eOQvtF
https://wakelet.com/wake/zfxgzmvkFoKMfgjk-KvMJ
https://wakelet.com/wake/VDbdx3fRK3JeHkRsm8Qch
https://wakelet.com/wake/3fURhKTdF2qgXkdDhQF0s
https://wakelet.com/wake/ODlAskju3TldQhKspI1IO
https://wakelet.com/wake/1Jo2heek-ldycMTP3dlDp
https://wakelet.com/wake/nuRiln-5LuQhOSSKCMy51
https://wakelet.com/wake/kDGM1Kwq5t2PrZWqTio9Y
https://wakelet.com/wake/jAXsUU9fS6AzH5-9C6FqG
https://wakelet.com/wake/K8xkcFAGHP5kDtRp-WcA6
https://wakelet.com/wake/odqojuLtjfZBoeohTtqjB
https://wakelet.com/wake/GxGt38mK03r5GUhC0g7uj
https://wakelet.com/wake/zA3ch7sUMC0GNXtX2Gt3c
https://wakelet.com/wake/FYnfXcR3mQdJrBvCjsIeO
https://wakelet.com/wake/XZzOx2-dZtmJd1GN-KLuJ
https://wakelet.com/wake/aqD8IeG-4jj4ni96oA4KY
https://wakelet.com/wake/eWUTjb66kCh_zIDSrQrdY
gottsaf (Tuesday, 18 January 2022 04:45)
gottsaf dd23f8915e https://wakelet.com/wake/-o7TguLCog4JwESyvv5fk
https://wakelet.com/wake/SK9PVHygXiH8UyX25A4eO
https://wakelet.com/wake/1mC9M3Wk_h6hGKSACfTV5
https://wakelet.com/wake/hGNsuIEPEscX8g6gjkF4m
https://wakelet.com/wake/_gC15EcsbMybdPvP2oj4u
https://wakelet.com/wake/AinKmcbu-83zyuv7yaXU0
https://wakelet.com/wake/8-sWW4crkfXiUuyIk5Ex7
https://wakelet.com/wake/q72W6Ckh-EqCpaKSXpTlO
https://wakelet.com/wake/AmSa3jC2zTQ648ILrwhUO
https://wakelet.com/wake/AVKYlk5LUnlna8b4WZyMC
https://wakelet.com/wake/a8LQMNgFyvRMj6SRS-pGI
https://wakelet.com/wake/6adYFEZYygMM6BsJHMMhe
https://wakelet.com/wake/yBsiH7eSgtDhQf-LQAniM
https://wakelet.com/wake/noxvLVlbahQyMV5dEapr7
https://wakelet.com/wake/NhIy727kNeNR5Ejf-8RBN
https://wakelet.com/wake/TWTkWMH2XOjjFHkeCIJA7
https://wakelet.com/wake/CysqzbIgOC4HfSqgn2ZAP
https://wakelet.com/wake/mm40ik5nk-nnG6Rh8lqBY
https://wakelet.com/wake/9OIXRdEm8qiP2Vy0_N16c
https://wakelet.com/wake/lwKjhK3Wp9qCqTfB2SRjH
https://wakelet.com/wake/UCamsz9ibMLI9R8ntu-bd
https://wakelet.com/wake/_F_mbUlf1axUiCtrnvDH5
https://wakelet.com/wake/NHvArB2bhUnm0mbooOOyH
https://wakelet.com/wake/-NTZYB8r0ClYKkeJTmDWR
https://wakelet.com/wake/TUktEPBFrAK4BFIpcpUNF
https://wakelet.com/wake/DjALU6zyfGPrg-qrmSVDx
https://wakelet.com/wake/txrybLQvRKOGib5ZN7YZp
https://wakelet.com/wake/XDDPhgKkUKaNwC8zF2NEO
https://wakelet.com/wake/q6FwYw2IHBVyjn4QAMY2p
https://wakelet.com/wake/81RaDT8495SGRTnWwWGu_
extchau (Tuesday, 18 January 2022 09:41)
extchau dd23f8915e https://coub.com/stories/2786208-mrs-todd-s-shortcut-verified
https://coub.com/stories/2786205-exclusive-what-adds-up-to-95-billion-q3-for-google-microsoft-and-amazon
https://coub.com/stories/2786206-umberto-eco-on-beauty-demgia
https://coub.com/stories/2786210-scary-teacher-3d-top
https://coub.com/stories/2786214-android-studio-gradle-upgrade
https://coub.com/stories/2786215-fridge-size-guide-australia-top
https://coub.com/stories/2786216-khaos-ultimate-explosion-add-on-rar-fixed
https://coub.com/stories/2786217-kumon-math-worksheets-pdf-kaylnimr
https://coub.com/stories/2786219-rufino-moya-estadistica-descriptiva-pdf-upd
https://coub.com/stories/2786222-exclusive-cleanmymac-x-4-8-1-crack-plus-activation-number-2021-download
https://coub.com/stories/2786224-1984-ebook-free-download-epub-leodaeg
https://coub.com/stories/2786226-ccna2-chapter-5-exam-_hot_
https://coub.com/stories/2786225-building-skills-for-proficiency-cesur-ozturk-ellywor
https://coub.com/stories/2786227-full-democracy-4-v1_16-gog
https://coub.com/stories/2786228-athlean-x-perfect-chest-workout
https://coub.com/stories/2786230-new-download-cocinaen2horas-paratlsemana-rar
https://coub.com/stories/2786232-hot-lebanon-glamour-sex-girls
https://coub.com/stories/2786231-xubuntu-12-10-desktop-i386-iso
https://coub.com/stories/2786233-gilisoft-usb-lock-6-2-0-latest-crackingpatching-siteunblocked-info-nenquyn
https://coub.com/stories/2786234-neat-video-plugin-mac-torrent-work
https://coub.com/stories/2786236-the-foundry-nuke-studio-12-1v3-crack-application-full-version-full
https://coub.com/stories/2786237-cissp-practice-exams-pdf-25
https://coub.com/stories/2786238-exemple-de-certificat-de-formation-word
https://coub.com/stories/2779704-download-new-2021-telugu-full-movie-tamilrockers-best
https://coub.com/stories/2777292-greek-mythology-quizzes-with-answers
https://coub.com/stories/2777291-_hot_-edraw-max-9-4-crack-with-license-key-full-version-free-download
https://coub.com/stories/2777290-slate-digital-fgx-vst-au-rtas-intelxvx-unpacedtorrent
https://coub.com/stories/2777287-dotted-notes-worksheet
https://coub.com/stories/2777286-is-apollo-twin-worth-buying
https://coub.com/stories/2777285-junie-b-jones-books-download-free-besswed
olliham (Tuesday, 18 January 2022 18:01)
olliham d6def13163 https://coub.com/stories/2875745-patched-adobe-illustrator-cs6-18-0-1-32-64-bit-chingliu
https://coub.com/stories/2875744-lectra-modaris-software-free-verified-download-hit
https://coub.com/stories/2875743-sakura-and-the-secret-of-shrinking-jutsu
https://coub.com/stories/2875741-mortal-kombat-9-para-psp-gratis-latiwelb
https://coub.com/stories/2875740-microcat-daihatsu-dongle-crack-portable
https://coub.com/stories/2875739-image-comparer-3-8-build-711-multilingual-portable-ls-new
https://coub.com/stories/2875737-work-fight-night-round-4-skidrow-password
https://coub.com/stories/2875738-free-free-download-foxpro-3-0
https://coub.com/stories/2875734-harry-potter-e-o-prisioneiro-de-azkaban-2004-bluray-1080p-dublad-download-pc-hawldeir
https://coub.com/stories/2875736-qu-ils-sont-beaux-sur-la-montagne-partition-pdf-download-vaneuzo
https://coub.com/stories/2875735-octanerendercinema4dcrackedzip-berelle
https://coub.com/stories/2875733-_top_-artificial-girl-3-megapack-168-characters-269-clothes
https://coub.com/stories/2875732-download-the-sooryavansham-movie-720pl-braekas
https://coub.com/stories/2875730-lutoslawski-concerto-for-orchestra-score-pdf-work-download
https://coub.com/stories/2875729-high-quality-geostudio-2012-full-crack-19
https://coub.com/stories/2875727-hd-online-player-interstellar-movie-download-in-tamil-hot
https://coub.com/stories/2875725-corelaftershotpro300126x64multilingualincl-hot-keygenteamos-18
https://coub.com/stories/2875724-codigo-de-activacion-de-pdf-architect-raimfrew
https://coub.com/stories/2875723-descargar-wilcom-decostudio-e2-crack-megagolkes-best
https://coub.com/stories/2875721-cccam-server-hack-elbeyli-exe-cracked
https://coub.com/stories/2875713-qt-5-0-2-for-windows-32-bit-mingw-4-7-offline-installer-crack-free
https://coub.com/stories/2875712-verified-flowjo-10-serial-number-crack-44
https://coub.com/stories/2875708-adobe-acrobat-xi-pro-11-0-12-final-crack-madmikel-marjgrat
https://coub.com/stories/2875709-__top__-download-naruto-shippuden-season-10-english-dubbed-torrent-kickasstorrents
https://coub.com/stories/2875706-umemaro-3d-english-subtitles-for-volums-8-11-and-game-of-lascivity-omega
https://coub.com/stories/2875705-fire-chief-pc-game-download-jakrah
https://coub.com/stories/2875700-hot-adobe-acrobat-xi-pro-11-0-16-multilingual-crack-sadeempc-crack
https://coub.com/stories/2875703-ass-porn-videos-__exclusive__-free
https://coub.com/stories/2875701-gantt-chart-template-pro-crack-install
https://coub.com/stories/2875695-nicelabel-express-6-keygen-36-yavaxyl
takkkala (Tuesday, 18 January 2022 18:17)
takkkala d6def13163 https://coub.com/stories/2868302-ffhc-kasumi-rebirth-v3-1-crack-rar-javogar
https://coub.com/stories/2868301-bleach-blade-battlers-2nd-english-patch-hamchar
https://coub.com/stories/2868300-keygen-2021-synology-camera-license-pack-updated-3
https://coub.com/stories/2868299-dragon-quest-blue-jellyfish-of-forest-uncensored-jrar-exclusive
https://coub.com/stories/2868298-hannstar-j-mv-6-94v-0-pdf-download-phrmar
https://coub.com/stories/2868297-autocad-civil-3d-2008-keygen-hot
https://coub.com/stories/2868292-cc-radial-fast-blur-after-effects-cs4rar
https://coub.com/stories/2868296-fabfilter-pro-q-v-2-0-18-windows-and-osx-serial-key-pritai
https://coub.com/stories/2868293-krrish3fullhd720pmoviedownload-xytnar
https://coub.com/stories/2868294-taisho-x-alice-episode-1-free-download-pc-game-hot
https://coub.com/stories/2868291-signals-and-systems-by-sanjay-sharma-pdf-download-newmexi
https://coub.com/stories/2868290-spirited-away-english-dub-1080p-tricsadz
https://coub.com/stories/2868289-best-splinter-cell-blacklist-multiplayer-lan-crack
https://coub.com/stories/2868287-k3-cottage-63zip-lawrlev
https://coub.com/stories/2868288-upd-terjemahanjamiuldurus
https://coub.com/stories/2868286-rld-pes2013-dt07-rar-download-osmand
https://coub.com/stories/2868285-best-programa-para-reparar-disco-duro-windows-7
https://coub.com/stories/2868284-avs-video-converter-8-3-crack-file-with-activation-key-rar-mooensi
https://coub.com/stories/2868283-analyse-it-excel-crack-password-free
https://coub.com/stories/2868282-__exclusive__-autocad-v2013-keygen-xfautocadkg-x64zip
https://coub.com/stories/2868281-xatab-repack-fallout-4-warez-software-portable
https://coub.com/stories/2868280-top-igo-primo-navigation-2015-1440x2560-resolution-samsung-note-4-119
https://coub.com/stories/2868279-free-mbrwizard-suite-4-1-serial
https://coub.com/stories/2868278-best-fsx-turbine-sound-studios-airbus-a330-ge-and-p-w
https://coub.com/stories/2868277-better-magic-bullet-cosmo-serial-key
https://coub.com/stories/2868276-hot-grass-valley-edius-pro-7-50-build-236-loader
https://coub.com/stories/2868274-yvm-oxana-o09-36-top
https://coub.com/stories/2868275-habibi-marcha-mora-en-partitura-pdf-free
https://coub.com/stories/2868273-download-far-cry-pc-demo-updated
https://coub.com/stories/2868272-superior-drummer-3-library-update-v1-1-3-win
quytwas (Tuesday, 18 January 2022 18:31)
quytwas d6def13163 https://coub.com/stories/2863412-hd-online-player-insidious-chapter-2-free-download-in-hot
https://coub.com/stories/2863410-extra-quality-avatar-version-extendida-1080p-latino-mega
https://coub.com/stories/2863409-no-king-no-kingdom-pc-game
https://coub.com/stories/2863408-art-beyond-the-west-3rd-edition-download-pdf-fallell
https://coub.com/stories/2863407-edius-pro-6-5-free-download-with-crack-genohard
https://coub.com/stories/2863406-laruaville-2-final-2015-pc-foxy-games-hack-activation-code-andelle
https://coub.com/stories/2863405-pthc-web-video-collection-torrent-24-gig-6-repack
https://coub.com/stories/2863404-cracked-output-signal-pulse-engine-crack
https://coub.com/stories/2863403-install-icloud-remover-1-0-2-epub
https://coub.com/stories/2863401-magic-ascii-studio-v2-2-288-serial-key-keygen-link
https://coub.com/stories/2863402-updated-adobe-premiere-pro-cc-2018-5-10-1-0-175-crack-utorrent
https://coub.com/stories/2863400-talamanca-istituzioni-di-diritto-romano-pdf-download-top
https://coub.com/stories/2863398-anno-2205-tundra-download-kickass-rarl-ximrrann
https://coub.com/stories/2863397-upd-gastroenterologia-villalobos-6-edicion-pdf-downloadgolkes
https://coub.com/stories/2863396-exclusive-the-sims-2-build-mode-crack-62
https://coub.com/stories/2863395-epidemiologia-leon-gordis-pdf-lavkiel
https://coub.com/stories/2863394-free-download-tafsir-al-maraghi-bahasa-indonesia-__full__
https://coub.com/stories/2863393-dialogys-dvd-s-64-bit-patched
https://coub.com/stories/2863391-wincc-7-2-64-bit
https://coub.com/stories/2863392-libro-ecologia-begon-pdf-sawjaq
https://coub.com/stories/2863388-vanessacarltonheroesandthievesfullalbumzip-anyfeli
https://coub.com/stories/2863390-link-yodot-file-recovery-keygen-20
https://coub.com/stories/2863389-the-raincoat-dual-audio-720p-download-torrent-verified
https://coub.com/stories/2863387-free-smart-battery-workshop-3-71-cracked
https://coub.com/stories/2863386-hd-online-player-download-top-dirty-rotten-scoundrels-198
https://coub.com/stories/2863383-gta4setup1cbin-2021
https://coub.com/stories/2863385-telecharger-etka-73-francais
https://coub.com/stories/2863384-free-norton-360-product-key-generator-glawhat
https://coub.com/stories/2863382-2021-izaci-namaqhalo-esixhosa-pdf-28
https://coub.com/stories/2863381-bukvenka-pismenka-cifrenka-igrachki-zakachki
nechela (Tuesday, 18 January 2022 18:46)
nechela d6def13163 https://coub.com/stories/2857563-izotopenectarcrackdownloadtorrent-link
https://coub.com/stories/2857562-clave-licencia-para-shape-collage-pro-__top__
https://coub.com/stories/2857561-clearview-rc-flight-simulator-version-5-34-serial-better-crack-iso
https://coub.com/stories/2857560-p3dv4-aerosoft-mega-airport-london-heathrow-professional-download-top
https://coub.com/stories/2857558-better-native-instruments-guitar-rig-2-pro-v2-1-1-unlocked-serial-keyl
https://coub.com/stories/2857557-star-trek-armada-2-iso-and-fleet-operations-mod-extra-quality-crack
https://coub.com/stories/2857556-portable-crack-agelong-tree-4-activation
https://coub.com/stories/2857555-iron-maiden-en-vivo-1080p-mega-portable
https://coub.com/stories/2857554-repack-soundtoys-native-effects-411-au-vst-rtas-mac-osx-intel
https://coub.com/stories/2857552-download-converter-free-pdf-to-word-new
https://coub.com/stories/2857553-dataentrytutorialbanglapdfdownload-ottulfr
https://coub.com/stories/2857551-patch-fr-city-car-driving-link
https://coub.com/stories/2857550-gta4dvd1and2downloadcompressedwindows-hot
https://coub.com/stories/2857549-waves-all-plugins-bundle-v9-r15-windows-rar-enetaki
https://coub.com/stories/2857548-being-cyrus-movie-download-kickass-torrent-link
https://coub.com/stories/2857544-top-constitution-of-india-in-tamil-pdf-free-download
https://coub.com/stories/2857547-ilmu-kebidanan-sarwono-prawirohardjo-pdf-download-maemakc
https://coub.com/stories/2857545-krrish-2-full-movie-in-tamil-free-download-top
https://coub.com/stories/2857546-rab-ne-bana-di-jodi-movie-tamil-subtitle-164
https://coub.com/stories/2857543-kontakt-6-v10-10-0-unlocked-utorrent
https://coub.com/stories/2857542-__hot__-an-introduction-to-language-9th-edition-answer-key-pdf-zip
https://coub.com/stories/2857541-autodwg-dwf-to-dwg-converter-pro-2015-crack-verified
https://coub.com/stories/2857540-office-2016-professional-plus-rtm-msdn-x86x64-free
https://coub.com/stories/2857539-rings-english-4-movie-free-download-in-hindi-mp4-movie-exclusive
https://coub.com/stories/2857538-igo8-download-for-windows-ce-applications-roysyud
https://coub.com/stories/2857537-easy-driverpacks-5-11-win7-64bit-zip-updated
https://coub.com/stories/2857536-prison-break-the-final-break-download-720p-exclusive
https://coub.com/stories/2857535-work-windows-7-loader-1-7-1-by-daz-rar
https://coub.com/stories/2857534-bioshock-2-remastered-minervas-den-dlc-unlocker-codex-2018-no-survey-2021
https://coub.com/stories/2857532-the-sims-4-get-famous-all-dlcs-and-add-ons-fitgirl-repack-unlimited-gems-alphgil
vollfabi (Wednesday, 19 January 2022 07:04)
vollfabi 4ea590b918 https://wakelet.com/wake/maBxSjRV9yDm9OFMca3gY
https://wakelet.com/wake/guW8x8mGGA9z1DY7bAu_Z
https://wakelet.com/wake/1GQ9R8ON8wYVQpR9F2ceF
https://wakelet.com/wake/AqdguN_s123AJq-izCJHJ
https://wakelet.com/wake/80tYegaPMIb2xRxLirSHB
https://wakelet.com/wake/CcXG8vzphyIGsu5SsrBTR
https://wakelet.com/wake/t-uesAugotcE31nAmeshl
https://wakelet.com/wake/KXrD27DTV2Ukqq0fvudCj
https://wakelet.com/wake/-1qbnAoJ6hvpVtPgeaiT3
https://wakelet.com/wake/xvj_I5YqgLkA_vgPRPav-
https://wakelet.com/wake/XyOLBJmc-Je9vD3evY5Pi
https://wakelet.com/wake/XF0LTr7snZWhalVbl_rGi
https://wakelet.com/wake/Z2bHOy5psPLTG7G5CMssj
https://wakelet.com/wake/O0VJTUIuHksw1adrRqEd1
https://wakelet.com/wake/_-6C87LUjDvQ9R_wOZYGv
https://wakelet.com/wake/gpPDCNl9rrxyijiPhOCAw
https://wakelet.com/wake/zS1sAozsT37XcgIIFwGh1
https://wakelet.com/wake/KMjtFGZh8K0x0fdiHiCok
https://wakelet.com/wake/6q4QvVsMyyxSTz5ziOfjO
https://wakelet.com/wake/b8dRCtiHjUgopF_FncmUH
https://wakelet.com/wake/MORFLm6_o4rsbHnhyNdx3
https://wakelet.com/wake/4CL5Lnn8Ae6H2giZXJHMO
https://wakelet.com/wake/zDUouDi-tU2Qk2rSGbv3D
https://wakelet.com/wake/SPQWbiUOMvHYGMID2RBJD
https://wakelet.com/wake/g9p7LZ5cdGRBFjFSrn2Z7
https://wakelet.com/wake/IXtvql4TxCyx_bWDsSeqK
https://wakelet.com/wake/pm8SuD0UDkMic64ep9tKi
https://wakelet.com/wake/Lojla088Sr2d558iU1tQO
https://wakelet.com/wake/hiHURpbbpJXtcmMQD74hA
https://wakelet.com/wake/Mw4ECd9m2i8x2TSyi_dhk
wenhar (Wednesday, 19 January 2022 07:19)
wenhar 4ea590b918 https://wakelet.com/wake/Nq9QF9dQl0y4BebEd_IbZ
https://wakelet.com/wake/ogb1COWqQ33xFRR5PEm4I
https://wakelet.com/wake/eTuSSz97TLnLf5HkPVIaU
https://wakelet.com/wake/UP7WStEwCkWFVxmD9HU5m
https://wakelet.com/wake/6HRjf1IrTv1lnJRSj-qL1
https://wakelet.com/wake/runRaL_G1wlV9nViYfP81
https://wakelet.com/wake/eSwak8AS9coOIMURnaXqv
https://wakelet.com/wake/dAUGSykeSI6iJ3VYmcU3y
https://wakelet.com/wake/oo_3Ci9hL60SHiJevECFL
https://wakelet.com/wake/0DUvfLBwhJtPrBKaAayov
https://wakelet.com/wake/KgkvDV68GcXpxjUQtEMCn
https://wakelet.com/wake/-583Ol3OpTF_UPL4TXnkO
https://wakelet.com/wake/1K1G10BYwsLsI4rF1ivNK
https://wakelet.com/wake/oqmuALkr6-_-_2VsWWVDl
https://wakelet.com/wake/3MCYnUjvpZx1F4_-T6BCZ
https://wakelet.com/wake/7irURmscLvfM9Cis_w8kr
https://wakelet.com/wake/e1W_7iPc6gEEduCXkOMZX
https://wakelet.com/wake/mKgRWEk1J6SQrYmiL6Hvh
https://wakelet.com/wake/Q5IVpQUw_RJwLxhd2OLJR
https://wakelet.com/wake/sxIawD1VWTEi6-2z-NU9k
https://wakelet.com/wake/kQNWzP1K-GAjd2LnZjfff
https://wakelet.com/wake/A97BgnFcrhqRHnbiPk6sO
https://wakelet.com/wake/szNVoGMYOACRS8btC6t7I
https://wakelet.com/wake/T93sAgLNtF6KcW1Gr10ZU
https://wakelet.com/wake/N4_FR001nb5VXR2QEk0gc
https://wakelet.com/wake/7fWuVhH6gZt2hIYCtkhKo
https://wakelet.com/wake/W9-OaMmyPdKpV4Vlp0gFj
https://wakelet.com/wake/9tJ7OfEzAw2v6bHWqsIwq
https://wakelet.com/wake/0COJpv_dVUUqfmgTqiPaf
https://wakelet.com/wake/sCSVWbWJ3KWFvzIqGqlr1
commark (Wednesday, 19 January 2022 07:34)
commark 4ea590b918 https://wakelet.com/wake/HGivQbAFFOQlfyRD7_zLN
https://wakelet.com/wake/2v6qak3bJNibKqngBGMwU
https://wakelet.com/wake/MER1xbd_ErlpqO9RFF9pE
https://wakelet.com/wake/Scp0t2amCDcObx5nVoyrH
https://wakelet.com/wake/VDxgWvLe_L3E2MxTvp38i
https://wakelet.com/wake/wF6uvb8xl4nEm0lE3dO20
https://wakelet.com/wake/7PvSyqtnkzklgW7rm1OgN
https://wakelet.com/wake/qBHrsiGlLb4jSOUXdXloB
https://wakelet.com/wake/P1e6WTuEZmfVfJFQtscHE
https://wakelet.com/wake/LGeWzppmMHVONfgm7E1dF
https://wakelet.com/wake/ueOs3EEkeDk94U-LqONgY
https://wakelet.com/wake/T-WIYWgDEyjgZTtw7I3zn
https://wakelet.com/wake/8unEDVhsw84cfbhc4WckT
https://wakelet.com/wake/ND3OV82DCYLYqKqf23E2a
https://wakelet.com/wake/4BCXjmsxrzmE2mn0luTBb
https://wakelet.com/wake/UCNCil8PY0x_uuEzceoJV
https://wakelet.com/wake/9_vYfhjAnyvtidlqAqohs
https://wakelet.com/wake/QI-d_j4HqjiEybwHspjHt
https://wakelet.com/wake/ytJZwrk0h5Gd6BxY4_XRW
https://wakelet.com/wake/zVubWmRfH20TJ3UwABkPB
https://wakelet.com/wake/f9y097I_0Ptg3bjNO1e48
https://wakelet.com/wake/QqRliJuFSE_7iLxCMMz1u
https://wakelet.com/wake/-gRcwI9KfqvaHW8vpgDky
https://wakelet.com/wake/JpJEClBGmplI7FQteA0TC
https://wakelet.com/wake/2C5zJ2PHIvvp1P3pK7Lew
https://wakelet.com/wake/Nh1ZR7M1BLgjRTghfM8yi
https://wakelet.com/wake/636XnuqBC9OSLVq2unLSd
https://wakelet.com/wake/P4BwM21cgiM4Cksbi7wGX
https://wakelet.com/wake/-o7TguLCog4JwESyvv5fk
https://wakelet.com/wake/SK9PVHygXiH8UyX25A4eO
kamabenn (Wednesday, 19 January 2022 07:50)
kamabenn 4ea590b918 https://wakelet.com/wake/Ja8wghUUiJPCyUIUtHX4Z
https://wakelet.com/wake/aUR6CRGZWzTGC2jN5CN9G
https://wakelet.com/wake/f0NX7uxwxfgqw3neZDUZP
https://wakelet.com/wake/NLcqLM9A3p2uhJZmk67-J
https://wakelet.com/wake/4VOZbhPVmrLhecp_00Mgr
https://wakelet.com/wake/Un8ldDspeRXW_GknBiqt4
https://wakelet.com/wake/fO9CTAr9VzKkyj-AF1307
https://wakelet.com/wake/vLwGNjhsHezqsvE8gvStI
https://wakelet.com/wake/Gf6mjDFE3Rygvk5k8pbpe
https://wakelet.com/wake/cAgZhhIRAdmGSLfmzWa6I
https://wakelet.com/wake/HjsLSZkBPYfpHwwCsVUuO
https://wakelet.com/wake/IdRxSIeSCCVLHnhkRfbiZ
https://wakelet.com/wake/Q_i5QW9v5AQaO1PyDlFAL
https://wakelet.com/wake/_-5gXmwfOPARq-9Gl2zYu
https://wakelet.com/wake/9_2SZmTgodCXVljFM-ub4
https://wakelet.com/wake/xAMH834tzWqUkFVNZEEkI
https://wakelet.com/wake/roLx3WuMusKG2Ha335uHz
https://wakelet.com/wake/A-XtsYzw5cUTuPQGmoxMm
https://wakelet.com/wake/uXBBwGc4pTnXTR377Pjnx
https://wakelet.com/wake/hCK0ebgAeaK41x2OoTEKO
https://wakelet.com/wake/6xpeerWJZ2uB0Fkd7cMiZ
https://wakelet.com/wake/YiQEhUeVSPDPrsSHL-ElP
https://wakelet.com/wake/WUVwcjDTDOhLZaa4XxRUY
https://wakelet.com/wake/IVpcAEfdkeJzRUTTQfSWA
https://wakelet.com/wake/sDyVrv8I0vYmw6OHeuO_q
https://wakelet.com/wake/Po9aAoWcXNTA98bkxK78y
https://wakelet.com/wake/W8wzdcNwpJDPKnrQc68Ek
https://wakelet.com/wake/u6Po3r26NqvBWeTIIVkIW
https://wakelet.com/wake/-guu6unLxnZhhz0t-Xb2r
https://wakelet.com/wake/qG5yp_3rtBNjRP3s5d_jo
entoss (Wednesday, 19 January 2022)
entoss 4ea590b918 https://wakelet.com/wake/0nhaI7-L9qaH79LxxoRil
https://wakelet.com/wake/KJN0evT4YdkxO7BqjLpZE
https://wakelet.com/wake/MKU2ro8-wdAIQBtjdflW4
https://wakelet.com/wake/3z_1A2jSVOsaTI0vA5fdz
https://wakelet.com/wake/6mah7XVw9U1JoS6FC4qCx
https://wakelet.com/wake/Jzzsi2KK0z0p-WkBU75Yt
https://wakelet.com/wake/qtUAdKhXb5A153kqrpMhp
https://wakelet.com/wake/KEyKlbgZDED53KFqr6y9V
https://wakelet.com/wake/nF4k7fk_3kFvgnyxnqsxC
https://wakelet.com/wake/GeBMrreXQWXolqicaE-kp
https://wakelet.com/wake/VvUMjGmxGr0rggmtpnfCv
https://wakelet.com/wake/DFE_GpqpmO8RFBXVquJYX
https://wakelet.com/wake/ERnqSdkYiwChO46YQlAjx
https://wakelet.com/wake/mKF9Hb1vzB2d0i-8Ciyxj
https://wakelet.com/wake/Hb0AluCvwE8oz7sIK4PTy
https://wakelet.com/wake/i-w4thsf9n3uAEhxMVsfZ
https://wakelet.com/wake/A75gMeqtc2Vz4REaAAg8v
https://wakelet.com/wake/F9eUhYps1aC98_CaquXT8
https://wakelet.com/wake/DG4Pc3c08AdSLuSGN9a1z
https://wakelet.com/wake/dXqy0ZhRHl-BeLli00uWR
https://wakelet.com/wake/omldoEMd4vNDmlIo0rwR2
https://wakelet.com/wake/Zi3FxxaWg7qivD8iuVsDZ
https://wakelet.com/wake/3O62UhcjFip3K_x7WtfJ9
https://wakelet.com/wake/t7ZaS_qjruTXnEQBt4J__
https://wakelet.com/wake/AoLXmqRJhPQb01vuqK35s
https://wakelet.com/wake/3iwWmF7n5ANOHp5K9Hwy8
https://wakelet.com/wake/n4PIZcQNXq6svKLK1_04P
https://wakelet.com/wake/ADKB-u2poOY_qHP-azHLI
https://wakelet.com/wake/G9Udw6BLb7o_m2_jEupho
https://wakelet.com/wake/Z3lM5DZICQRE8FVcu0si2
amiphyl (Wednesday, 19 January 2022 18:03)
amiphyl ba0249fdb3 https://wakelet.com/wake/wKIZ_wOIOOxTb6j5vXM5x
https://wakelet.com/wake/g1SvrUPLTpNyKIWeXO6I7
https://wakelet.com/wake/Bxu1nRmz_fQA6KKezvf16
https://wakelet.com/wake/s9fCOl5Dw64_EwHygXgL1
https://wakelet.com/wake/pyMwpmxVPSuxvHXzO-Nmh
https://wakelet.com/wake/QPdWxnncZ9xifZCKHG5nn
https://wakelet.com/wake/vfkjX9VJ2r7RotN-Qwb-s
https://wakelet.com/wake/IqXne7p0qzXdeEdZIbImn
https://wakelet.com/wake/HV_j4HT1zbIhvczIF4NnK
https://wakelet.com/wake/sJBzAQP2D2RNL_HgEv8lo
https://wakelet.com/wake/SmmjvAwumEttP5USRiYmd
https://wakelet.com/wake/nKWoJ6KouuO0eFMtuPzIW
https://wakelet.com/wake/P1_2IQ2Pti0ISlYVGxyIG
https://wakelet.com/wake/hmLXqUirvSnTNuKvVNpiK
https://wakelet.com/wake/uLeqNz0pF9klxSFwFaePj
https://wakelet.com/wake/jpDuKr_4NtKcv55zO6qLg
https://wakelet.com/wake/XNpUncGm519g0gcI6UzXn
https://wakelet.com/wake/bcU_zsYoglXC-kr0G6wmD
https://wakelet.com/wake/ey-DV_UNtifi3VopVIX6v
https://wakelet.com/wake/fuZ21v3Ul__5Zaf-Ob_25
https://wakelet.com/wake/p5HJ0QLyq6AYTysr3yi0c
https://wakelet.com/wake/UN-1DJiz0KaF4ghJjE4L6
https://wakelet.com/wake/XTeAnMVexxfxv_fpY1hW2
https://wakelet.com/wake/O9j9BPDYZzdM787sHnA4O
https://wakelet.com/wake/n-D6EWQYN7SK5pSSehPGv
https://wakelet.com/wake/sBHxixK8ylG3Bw1zyKpMM
https://wakelet.com/wake/88Ke44ownkgk5utI8lnSP
https://wakelet.com/wake/RLQ5RqaR5Fc0hgVuL8dsp
https://wakelet.com/wake/dxFM0cUVxBm0gSvifoKmZ
https://wakelet.com/wake/tg3lHuhFACGl5JMW68Az3
davhir (Wednesday, 19 January 2022 18:34)
davhir ba0249fdb3 https://wakelet.com/wake/qn3DLJQNI2F8YSe6hUvj1
https://wakelet.com/wake/DmyKeM3rXxsG3M7numtrF
https://wakelet.com/wake/K1j36Z1Ztyo-RHxmse2n5
https://wakelet.com/wake/449OkhRKT6UYNsgEwZVHf
https://wakelet.com/wake/pHQn9-XZENzdPkbXSCx77
https://wakelet.com/wake/AoUpwqlVqyZJ0u05K7ARm
https://wakelet.com/wake/FF0McffPGCH1zqadlddVy
https://wakelet.com/wake/pR-YbVZDdnzbScfJwhGke
https://wakelet.com/wake/NvUUfW2L-MH6peLQ1JzsD
https://wakelet.com/wake/XK5vGWylTrZgM6JaSXMtY
https://wakelet.com/wake/1fb5ylF__9-xX2N81kIa_
https://wakelet.com/wake/ES-SDU4X3taa2jQIF9exv
https://wakelet.com/wake/L3hvM25mL1NOouDYnUkPv
https://wakelet.com/wake/94r_ewfmVbSu11rdBU5s-
https://wakelet.com/wake/1q9f5z6EMrzwijRtSZ7AJ
https://wakelet.com/wake/TnIU55261Y2cvYXfR1Ljn
https://wakelet.com/wake/RZLxDGyQun3dNKM1_evis
https://wakelet.com/wake/Q0k8eW5i5VakcipfZSewF
https://wakelet.com/wake/iwiwQWX4tDHiXL-XavCuc
https://wakelet.com/wake/PivRG5UsyBZo3ac5crbGH
https://wakelet.com/wake/a7SrrHaK5ZFafHDtSaV-Y
https://wakelet.com/wake/TtviO8V3-3Q23r-7GJRDW
https://wakelet.com/wake/ZNfiS8SoqqhFA19An-Zap
https://wakelet.com/wake/aKP0uw3UCQVVUF3vUEOiD
https://wakelet.com/wake/5h2OF3dMMv5YK4QEVoR18
https://wakelet.com/wake/yLKWzmP5y5UJj0v_vYO3d
https://wakelet.com/wake/fkYiI2uY_EL344LJB3cUq
https://wakelet.com/wake/BpRzBl0Gl_i7o-9_PekiA
https://wakelet.com/wake/ClDhGcyRg1iaRKRs6gx5A
https://wakelet.com/wake/Me1lKcBumBXrzfC8vBmJn
xirenayt (Thursday, 20 January 2022 01:42)
xirenayt 90f3619eba https://coub.com/stories/2730685-photoshop-cs5-mac-crack-free-free
https://coub.com/stories/2730683-act_1_ingenieria_de_software
https://coub.com/stories/2730684-bob-books-free-download-_hot_-pdf
https://coub.com/stories/2730682-install-renaultmeganeiiiuniversal5dv_repair_manual_pdf
https://coub.com/stories/2730680-full-vladmodels-zhenya-y114-katya-y117225
https://coub.com/stories/2730681-hot-beethoven-moonlight-sonata-piano-free
https://coub.com/stories/2730679-como-criar-a-los-varones-pdf-gratis
https://coub.com/stories/2730678-caterpillar-serial-number-location
https://coub.com/stories/2730677-new-dallas-and-sasha-wedgie-war-full-videol
https://coub.com/stories/2730676-download-wars-telefonbuchios14ok-ipa-work
https://coub.com/stories/2730675-akeeba-backup-professional-nulled-tools
https://coub.com/stories/2730672-verified-arena-helper-for-mac
https://coub.com/stories/2730674-are-serial-killers-born-or-made-conclusion-shalhel
https://coub.com/stories/2730673-upd-calvin-harris-18-months-deluxe-download-new-zip
https://coub.com/stories/2730671-hot-s-chand-books-download-for-class-10
https://coub.com/stories/2730669-better-eternal-nymphets-eternal-aphrodites-studio-13-lolitas-5599-photos-47
https://coub.com/stories/2730670-adobe-zii-patcher-2-2-1-free-download-software-for-mac-kalari
https://coub.com/stories/2730668-better-uhe-zebra-2-keygen-120
https://coub.com/stories/2730667-upd-iskysoft-pdf-editor-6-pro-6-7-11-cracked-for-macos
https://coub.com/stories/2730666-download-kitab-mukhtarul-ahadits-kryscec
https://coub.com/stories/2730665-gamaedr-suyu-formgl-link
https://coub.com/stories/2730664-aromas-of-aleppo-epub-download-cesavigi
https://coub.com/stories/2730663-3-enterprise-4-7-pdf-leecha
https://coub.com/stories/2730660-all_of_me_gypsy_jazz_violin_sheet_music-wernzyl
https://coub.com/stories/2730662-the-wheel-of-time-audiobook-torrent-nanverl
https://coub.com/stories/2730657-link-leave-letter-format-for-cousin-brother-marriage
https://coub.com/stories/2730661-chevrolet-spark-service-manual-new
https://coub.com/stories/2730659-accounting-practice-problems-pdf-new
https://coub.com/stories/2730658-hot-sim-city-build-it-hacks-jailbroken-iphone-v-simcity-buildit-hack-mac-os-x-macosx
https://coub.com/stories/2730656-main-aur-charles-2015-hindi-720p-download-waripya
ondihild (Thursday, 20 January 2022 02:20)
ondihild 90f3619eba https://coub.com/stories/2821429-_best_-ushul-fiqh-wahbah-zuhaili-pdf-download
https://coub.com/stories/2821427-space-1999-season-1-720p-torrent-link
https://coub.com/stories/2821428-motorguide-trolling-motor-user-manual-new
https://coub.com/stories/2821425-link-iparty-with-victorious-extended-version-full-episodeinstmanksl-better
https://coub.com/stories/2821426-cara-menggunakan-pro-facebook-hack-v1-5
https://coub.com/stories/2821424-2021-the-alchemy-of-finance-reading-the-mind-of-the-market-pdf
https://coub.com/stories/2821423-_verified_-iptv-smarters-pro-v2-2-2-5-mod-sap-apk-latest
https://coub.com/stories/2821422-view-links-8xlinks-grabar
https://coub.com/stories/2821420-download-final-cut-pro-7-mac-free-verified
https://coub.com/stories/2821421-download-file-gema-white-1-rar-196-13-mb-in-free-mode-turbobit-net-andkae
https://coub.com/stories/2821419-cisdem-duplicate-finder-license-key-better
https://coub.com/stories/2821418-angular-mat-form-field-default-value-jassbart
https://coub.com/stories/2821417-the-divine-comedy-inferno-purgatorio-paradiso-pdf-quikai
https://coub.com/stories/2821416-xforce-keygen-autocad-2013-online-osmadavi
https://coub.com/stories/2821415-peliculaelagarratodosincensura-takesha
https://coub.com/stories/2821414-new-honda-fr800-tiller-parts-manual
https://coub.com/stories/2821412-jump-desktop-rdp-vnc-fluid-8-2-17-crack-mac-osx-vangill
https://coub.com/stories/2821411-jazz-chord-progression-theory-pdf
https://coub.com/stories/2821410-paradigms-joel-barker-pdf-download-lavigeo
https://coub.com/stories/2821409-dna-electrophoresis-lab-answers-verified
https://coub.com/stories/2821408-work-photoprint-6-1v2-crack-21
https://coub.com/stories/2821407-yourina_videos_2
https://coub.com/stories/2821406-repair-manual-mercedes-w460
https://coub.com/stories/2821405-harry-potter-series-1080p-dual-audiol-geraans
https://coub.com/stories/2821404-netspot-pro-2-8-exclusive-crack-for-windows-mac-free-download-latest
https://coub.com/stories/2821403-minecraft-pc-controls-cheat-sheet
https://coub.com/stories/2821402-transitive-verb-worksheets-for-grade-5
https://coub.com/stories/2821401-teen-mom-2-10x5-brokensilenze-portable
https://coub.com/stories/2821400-download-do-microsoft-office-2019-professional-entre-no-pc-emmocah
https://coub.com/stories/2821397-florida-probate-forms-pdf-elougert
compcate (Thursday, 20 January 2022 02:56)
compcate 90f3619eba https://coub.com/stories/2651812-exclusive-arturia-minimoog-v-vsti-rtas-v2-0-1-incl-keygen
https://coub.com/stories/2651811-description-physique-en-frangais-pdf
https://coub.com/stories/2651810-master-of-the-universe-fanfiction-net
https://coub.com/stories/2651809-watch-mujhse-dosti-karoge-online-free-on-youtube-free
https://coub.com/stories/2651806-panchatantra-stories-english-pdf-patched-download
https://coub.com/stories/2651805-certificate-of-analysis-protein-powder-full
https://coub.com/stories/2651803-jamie-xx-in-colour-2015-album-flacjamie-xx-in-colour-2015-album-flac-better
https://coub.com/stories/2651802-black-edge-pdf
https://coub.com/stories/2651797-oddworld-munchvs-oddysee-hd-game
https://coub.com/stories/2651792-heroes-guardian-dark-genesis-ver-1-0-8-mod-apk-latest-chrdar
https://coub.com/stories/2651780-top-audiochecker-for-mac
https://coub.com/stories/2651795-silver-thread-jf-font-free-exclusive
https://coub.com/stories/2651794-hot-the-return-of-the-magnificent-dj-jazzy-jeff-rar
https://coub.com/stories/2651791-flappy-golf-2-redeem-codes-link
https://coub.com/stories/2651790-__top__-final-destination-2000-dual-audio-hindi-english-1080p-bluray-2-1gb-esub-hollyflix-mk
https://coub.com/stories/2651788-install-human-molecular-genetics-strachan-pdf
https://coub.com/stories/2651785-blofeld-editor-librarian-hot
https://coub.com/stories/2651784-best-joker-tamil-dubbed-torrent
https://coub.com/stories/2651783-pro-landscape-software-torrent-emalqwen
https://coub.com/stories/2651781-android-pokemon-go-spoof-apps
https://coub.com/stories/2651779-refx-nexus-2-2-1-update-crack-hack-usb-air-elicenser-emulator-verified
https://coub.com/stories/2651778-genl-0043-daulat-buri-bala-pdf-google-drive-new
https://coub.com/stories/2651776-_best_-winols-v1-721-crack-damos-rar-260
https://coub.com/stories/2651773-cinesamples-cinebrass-kontakt-torrentl
https://coub.com/stories/2651770-portable-muzica-de-colectie-jurnalul-national-download
https://coub.com/stories/2651768-sonar-wiring-diagram-complete-wiring-schemas-eliolab
https://coub.com/stories/2651766-amoeba-sisters-video-recap-answers-viruses-baligord
https://coub.com/stories/2651765-samsung-ce0168-manual-extra-quality-free-download
https://coub.com/stories/2651764-my-son-the-fanatic-movie-watch-online-free-__top__
https://coub.com/stories/2651762-yamaha-stagepas-300-replacement-speaker
neasalo (Thursday, 20 January 2022 03:29)
neasalo 90f3619eba https://coub.com/stories/2649074-upd-media-ethics-issues-and-cases-9th-edition-pdf
https://coub.com/stories/2649073-ana-britannica-ansiklopedisi-pdf
https://coub.com/stories/2649071-rumpus-pro-working-activation-full-file-cracked-paltal
https://coub.com/stories/2649072-what-effects-do-fluorescent-lamps-have-on-household-plants-top
https://coub.com/stories/2649070-bosch-esi-tronic-2-0-download-torrentbfdcml-dargeo
https://coub.com/stories/2649069-spyhunter-5-crack-plus-keygen-free-download-2018-slaquyn
https://coub.com/stories/2649066-logic-based-reasoning-test-pdf-saxgaya
https://coub.com/stories/2649063-download-spectrasonics-omnisphere-2-5-2-mac-crack-update-patch-vst-au-working-tested-blytcall
https://coub.com/stories/2649065-updated-downloadhavij117procracked
https://coub.com/stories/2649062-free-dlupload-s-zip
https://coub.com/stories/2649060-how-to-build-la-purisima-mission-model
https://coub.com/stories/2649059-voces-inocentes-study-guide-answers
https://coub.com/stories/2649058-high-quality-ayoayoayoayoayoaayoayoayoayo-277-2-pdf-google-drive
https://coub.com/stories/2649057-naruto-episode-220-english-dubbed-hd-720p-ghahem
https://coub.com/stories/2649055-afilmywap-vijay-the-master-2021-hindi-dubbed-movie-480p-mp4
https://coub.com/stories/2649054-__full__-pioneer-bdp-320-region-free-hack
https://coub.com/stories/2649052-meilleur-dessin-anime-parodie-porno-work
https://coub.com/stories/2649053-apple-could-be-plotting-to-switch-to-oled-for-its-tablet-and-laptop-displays-work
https://coub.com/stories/2649051-_oceanofapk-com_advanced_tools_pro_v1-99-1-zeadawa
https://coub.com/stories/2649050-descargar-software-teowin-gratis
https://coub.com/stories/2649049-garden-way-th-1019-tiller-manual
https://coub.com/stories/2649047-classique-gorge-profonde-et-vintage-porn
https://coub.com/stories/2649045-download-free-batch-convert-word-to-pdf-ware-for-mac-__full__
https://coub.com/stories/2649046-genki-2-textbook-online-pdf-hercha
https://coub.com/stories/2649043-free-mp3-splitter-and-joiner-software-23-dashfran
https://coub.com/stories/2649042-chinese-to-pinyin-converter-free-full
https://coub.com/stories/2649041-ams-bianka-model-sets-01-11-rar-1-better
https://coub.com/stories/2649040-download-file-0135562171-rar-313-18-mb-in-free-mode-turbobit-net-illaama
https://coub.com/stories/2649037-lister-engine-manual-upd
https://coub.com/stories/2649039-better-celemony-melodyne-studio-4-2-1
rangla (Thursday, 20 January 2022 17:27)
rangla a8cc6d31e7 https://coub.com/stories/2779365-watch-mstcskmhd-2021-skymovieshd-ltd-720p-hevc-rated-hdrip-hindi-s01e02-x265-aac-peathom
https://coub.com/stories/2779364-straw-hats-terroize-enies-lobby-one-piece-ep-267-268-reaction-mp4
https://coub.com/stories/2779363-flightless-bird-american-mouth-piano-sheet-music-free-pdf-xanobel
https://coub.com/stories/2779361-movavi-video-editor-janyraen
https://coub.com/stories/2779360-cook-up-a-storm-2017-full-english-movie-full
https://coub.com/stories/2779356-extra-quality-the-great-hunt-robert-jordan-epub-vk
https://coub.com/stories/2779359-elite-torrent-link-download
https://coub.com/stories/2779357-top-free-720p-aao-pyar-karen-movies-download
https://coub.com/stories/2779358-manitowoc-ice-machine-model-b400-manual
https://coub.com/stories/2779355-2021-newstar-jimmy-tonik-nude-58
https://coub.com/stories/2779353-team-toxic-warez-wifi-hack-link
https://coub.com/stories/2779352-ghoom-movie-5-full-movie-download-in-hindi-and-mp4-top
https://coub.com/stories/2779351-percona-server-for-mongodb-3-0-8-1-2-is-now-available
https://coub.com/stories/2779349-new-celemony-melodyne-studio-4-v4-1-1
https://coub.com/stories/2779348-michael-moore-capitalism-a-love-story-worksheet-hot
https://coub.com/stories/2779347-work-barcarolle-offenbach-sheet-music-voice
https://coub.com/stories/2779346-adobe-illustrator-2021-v25-2-1-descarga-gratuita-hot
https://coub.com/stories/2779344-free-__exclusive__-studio-6-7-crack-activation-key-free-__exclusive__-download-latest
https://coub.com/stories/2779345-free-ben-tjr-funky-vodka-original-mix-smilellm
https://coub.com/stories/2779342-the-wheel-of-time-the-great-hunt-epub
https://coub.com/stories/2779341-link-facial-expression-dataset
https://coub.com/stories/2779338-tenente-colombo-serie-completa-torrent-243-repack
https://coub.com/stories/2779337-pipe-flow-expert-6-39-crack-innoher
https://coub.com/stories/2779336-https-drive-google-com-file-d-1sfenlybtmkdyd1yrja5xstav94nelxyd-view-usp-sharing-javasup
https://coub.com/stories/2779335-apush-period-2-key-concepts-review-answers
https://coub.com/stories/2779334-hp-probook-bios-password-cracker-biltali
https://coub.com/stories/2779333-jim-blackley-syncopated-rolls-19-pdf
https://coub.com/stories/2779332-abcd-3d-movie-torrent-hot-download
https://coub.com/stories/2779331-cfa-mock-exam-pdf-level-2
https://coub.com/stories/2779330-hot-download-chicken-soup-for-the-soul-bahasa-indonesia-pdf
fyalau (Thursday, 20 January 2022 17:57)
fyalau a8cc6d31e7 https://coub.com/stories/2655322-how-to-apply-3m-vinyl-stripes-janabarr
https://coub.com/stories/2655320-mecanoscrit-segon-origen-pdf-yannmart
https://coub.com/stories/2655319-nys-hunter-education-homework-portable
https://coub.com/stories/2655318-hot-the-new-high-intensity-training
https://coub.com/stories/2655316-datei-herunterladen-ddf207-rar-155-78-mb-in-exclusive-free-mode-turbobit-net
https://coub.com/stories/2655317-zevi-il-nuovissimo-manuale-dell-architetto-pdf
https://coub.com/stories/2655313-accuraw-monochrome-for-mac-upd
https://coub.com/stories/2655309-freimaurer_fur_dummies_zip_pdf
https://coub.com/stories/2655308-work-actualite-agony-les-portes-du-purgatoire-s-ouvriront-trgyos-bientgt
https://coub.com/stories/2655307-volkskrant_cryptogram_-telljane
https://coub.com/stories/2655305-visustin-v7-crack-lynfri
https://coub.com/stories/2655304-download-rs-file-manager-mod-apk-1-7-3-pro-dlpure-com-portable
https://coub.com/stories/2655302-alkanes-worksheet-gcse-shabeve
https://coub.com/stories/2655303-episodes-of-humse-hai-life-hamiharr
https://coub.com/stories/2655298-2021-cosmopolite-french-book-pdf
https://coub.com/stories/2655299-repack-smartsvn-keygen-for-mac
https://coub.com/stories/2655300-updated-nu-disco-ft-bashiri-johnson-wav
https://coub.com/stories/2655301-understanding-enzymes-worksheet-answers
https://coub.com/stories/2655297-topolino-raccolta-fumetti-pdf-salale
https://coub.com/stories/2655295-windows-7-oem-brander-v-1-9-with-lerjava
https://coub.com/stories/2655289-top-huckleberry-finn-discussion-questions-answers
https://coub.com/stories/2655288-michael-jackson-bad-album-zip-12-nenyam
https://coub.com/stories/2655285-fundamentos-de-microbiologga-de-los-alimentos-pdf-upd
https://coub.com/stories/2655287-mac-os-x-call-of-duty-black-ops-full-dmg-rosnay
https://coub.com/stories/2655284-btd6-mod-apk-latest-version-better
https://coub.com/stories/2655283-windows-7-32-bits-edition-integrale-fr-iso-t411-torrent-411
https://coub.com/stories/2655279-cve-2012-4519-zenphoto-top
https://coub.com/stories/2655278-better-wet-dreams-2-korean-movie-eng-sub-19
https://coub.com/stories/2655275-introduction-to-quantum-mechanics-griffiths-3rd-pdf
https://coub.com/stories/2655276-mathworks-matlab-8-5r2015a-9-new
kaybamb (Thursday, 20 January 2022 18:26)
kaybamb a8cc6d31e7 https://wakelet.com/wake/gG6m6p5lq6pxHurBNYRw5
https://wakelet.com/wake/WHQTaqgxnbACDxTtoGXpu
https://wakelet.com/wake/SfJb4U7ne8cni_OynuH78
https://wakelet.com/wake/Ta_A9bb-LSyX4C5C2GhxB
https://wakelet.com/wake/uYmWRgcbutpMM34rQDzih
https://wakelet.com/wake/rynQ6CqwKFbuBf7vQv2NH
https://wakelet.com/wake/TWkXKSIvLR8ZQnWlqiRYU
https://wakelet.com/wake/cTgKpkkEMZXrwMjqKYRH9
https://wakelet.com/wake/IAv5WUSTpUZE7_WloAGmo
https://wakelet.com/wake/ABIzO3h4hPo0-j8QeHXGF
https://wakelet.com/wake/ZrlD2glI_jSKvTRM3fY-m
https://wakelet.com/wake/dcGSFSSxfzPgJiC6RPIsI
https://wakelet.com/wake/XRK6FHxh9QiNqUFnGBUl9
https://wakelet.com/wake/m98OMIBBlWAdOHd1VfgIF
https://wakelet.com/wake/nUovWai0AovUAgpgLedyd
https://wakelet.com/wake/xU3QwbS1joJ5lkbjgkwzv
https://wakelet.com/wake/USj8ofguy1qqEqMt9m1XH
https://wakelet.com/wake/kFjVIh8lrvxtVZ7gt6f5o
https://wakelet.com/wake/Ri3biGcPecUzllSsuOtPm
https://wakelet.com/wake/Gv5O_of0HFeVnp-NVzVck
https://wakelet.com/wake/KWmxL_UH3gaBzacVymSjS
https://wakelet.com/wake/onn3cH_QAiOuzpyEVizuF
https://wakelet.com/wake/6cBylB6w8311AM1lO9O6D
https://wakelet.com/wake/vanXHCGfvUlIbj7q-mrVD
https://wakelet.com/wake/craiyyxDeO-lpnDp9_f4_
https://wakelet.com/wake/ep8ZXEQC8PrFik0eRHBKA
https://wakelet.com/wake/FKceHr-wKzRYlXVwNqvMk
https://wakelet.com/wake/S4mVOCoAebK3dqt8Orsga
https://wakelet.com/wake/o8xx-RaFzLYsiKoTmnxYx
https://wakelet.com/wake/7SN76uir89GUkGVCQb1Rt
masskalo (Thursday, 20 January 2022 18:57)
masskalo a8cc6d31e7 https://coub.com/stories/2806667-_verified_-prepositions-exercises-for-class-10-icse-with-answers-pdf
https://coub.com/stories/2806663-2013-pthc-3gb-lolita-torrent-royajam
https://coub.com/stories/2806662-best-the-girl-next-door-hindi-dubbed-movie
https://coub.com/stories/2806657-fix-dragon-ball-z-shin-budokai-psp-free-download
https://coub.com/stories/2806653-durchstarten-deutsch-textsortentraining-pdf-download-jezwary
https://coub.com/stories/2806648-the-coal-mafiaa-english-subtitles-full-hot-movie-downl-winzip-passer-tales
https://coub.com/stories/2806647-_hot_-download-thenx-ver4-premium-apk
https://coub.com/stories/2806646-government-in-america-17th-edition-pdf
https://coub.com/stories/2806644-ra-one-2011-dw-t-me-ssrmovies-esub-mp4-openload-alpsamm
https://coub.com/stories/2806642-photoshoptutorialpdfintamil-glenhaza
https://coub.com/stories/2806641-thani-oruvan-movie-download-hd-1080p-kickasstorrents-portable
https://coub.com/stories/2806635-download-file-departinglandscape320-rar-185-79-mb-in-free-mode-turbobit-net-updated
https://coub.com/stories/2806632-semiologia-del-aparato-locomotor-celsus-pdf-41-__hot__
https://coub.com/stories/2806629-williams-a-critique-of-utilitarianism-best
https://coub.com/stories/2806624-fl_studio_20_reg_file_-verbyami
https://coub.com/stories/2806621-download-file-blake-barry-j-english-vocabulary-today-into-the-21st-century-2019-epub-blonale
https://coub.com/stories/2806609-mahindra-tractor-spare-parts-catalogue-pdf-dorcat
https://coub.com/stories/2806607-__link__-understanding-earth-by-grotzinger-and-jordan-7th-edition-pdf-free
https://coub.com/stories/2806606-manycam-pro-7-0-6-crack-with-registration-key-free-download-2020-alfumbi
https://coub.com/stories/2806602-pleasure-unwoven-movie-worksheet-jatiwesb
https://coub.com/stories/2806598-drive-ahead-apk-mod-unlock-all
https://coub.com/stories/2806597-autocad-mechanical-2006-crack-universal-product-key-free-top
https://coub.com/stories/2806596-all-rhodes-lead-here-mariana-zapata-epub
https://coub.com/stories/2806594-link-procore-project-management-final-exam-answers
https://coub.com/stories/2806592-dark-matter-book-dalviv
https://coub.com/stories/2806590-you-searched-for-nikita-v-fzmovies-exclusive
https://coub.com/stories/2806589-cambridge-pet-student-book-pdf
https://coub.com/stories/2806588-claimant-guide-warband-2021
https://coub.com/stories/2806586-download-singing-a818-rar-uploadbank-wynfran
https://coub.com/stories/2806587-minitool-power-data-recovery-2021-full-espagol-new
thonoe (Thursday, 20 January 2022 21:31)
thonoe a8cc6d31e7 https://wakelet.com/wake/IEXwbE-dZqkpL92wLoAej
https://wakelet.com/wake/GOlH5iUXXEyjBxvVA7Ies
https://wakelet.com/wake/gLDspM_x_467VGocYhDlR
https://wakelet.com/wake/s0pN1oAHpcVNYz_hwagyh
https://wakelet.com/wake/iaH-4YpbQ26j5yrcIiLr_
https://wakelet.com/wake/asxv3jkocKVgiXja4fp_5
https://wakelet.com/wake/7Hh2152_pdn0zIYPCZMiM
https://wakelet.com/wake/qkT422RzzBMFUAnRQ1qez
https://wakelet.com/wake/0_3yQrPI8FZmX8DyMaoa1
https://wakelet.com/wake/F_1NEPbtCLh3pWXa0sNau
https://wakelet.com/wake/cEeTjozqgfh1t5e_uJjbn
https://wakelet.com/wake/OTPtBOfPZtTL1fW1xTzQl
https://wakelet.com/wake/X72kl32nhuGPG1djlZdde
https://wakelet.com/wake/J4vw4JieqjIhagSbSmhFN
https://wakelet.com/wake/LXBqUt9edpK_hZcT7m-tQ
https://wakelet.com/wake/obWueQJr6vnPXBtw_6TTw
https://wakelet.com/wake/l278RJQf5qfq_f1_LEztD
https://wakelet.com/wake/EyjbFmN59IZ2e_dppj0-o
https://wakelet.com/wake/a7_4SfWw-PuTyz_-CSpWU
https://wakelet.com/wake/B4QOh1jWe_DeXWTZUVct9
https://wakelet.com/wake/nMnPhbV_1CCH3UawDMnFx
https://wakelet.com/wake/86vX30XHxKpgFpQJRU6b5
https://wakelet.com/wake/aoQsY4dq12aZm7X00lVPQ
https://wakelet.com/wake/0e6GzoKTVzzvYuYrtomjr
https://wakelet.com/wake/lBYava1FtN6nkAd2rgT75
https://wakelet.com/wake/hKODpdxRC4Sz5JNwHi2KF
https://wakelet.com/wake/QEhkkib7V3KD_sLxvSv47
https://wakelet.com/wake/mkuCeaOTZP9jFdvkKx6WG
https://wakelet.com/wake/YYWrHxHUoHHPjNP-65TDH
https://wakelet.com/wake/X2VeTsX7PLtCy_AZIa-M0
quilsol (Thursday, 20 January 2022 22:00)
quilsol a8cc6d31e7 https://wakelet.com/wake/nFRudlj71FfeRqsc_11j3
https://wakelet.com/wake/f0laPPFLJx1DJSnUmDnMd
https://wakelet.com/wake/NbckeNaDX4_LWxWli-Emz
https://wakelet.com/wake/yROX-uRqJnwi1vfX3DMNq
https://wakelet.com/wake/hE0GLv2sKpfK7U77Dftnc
https://wakelet.com/wake/1LBkiIghaKt3hHKE9N4rS
https://wakelet.com/wake/87KTlpKE30UZ2BJ5Ny8VJ
https://wakelet.com/wake/bVC71mSqkP1h3ag8kc6aR
https://wakelet.com/wake/aSXdhNEfVoy-A8IAa0TUT
https://wakelet.com/wake/n4NoDM2XKKjuBPBxnJPBm
https://wakelet.com/wake/j3BvM785xxB2XmN7ROHfk
https://wakelet.com/wake/-Ockaj9vmWXfHwJfiFpSr
https://wakelet.com/wake/fyl2HLArpAyMAEuTPYpx0
https://wakelet.com/wake/eiutVF3H193wSRoWDRmNg
https://wakelet.com/wake/EVAh3BR_bhiseznhZpYYj
https://wakelet.com/wake/hLzKedjQmgzNFGkvGJvBn
https://wakelet.com/wake/10HjfYX2RRJHEqw1AZZlQ
https://wakelet.com/wake/O3fpKE8bzTVEAtz9vWZxA
https://wakelet.com/wake/h-tdzSVQuV1mNv-fKLyr6
https://wakelet.com/wake/-He_wbmePnM-T8f0rjIw0
https://wakelet.com/wake/FP7Oiwpw5_GmG2BB2KBp2
https://wakelet.com/wake/dbpA_P_2jwMwi6qfOxQsG
https://wakelet.com/wake/hM9dYsIAgiq13YqCJWZJf
https://wakelet.com/wake/oYG0grfibwl8bLrSEiPyG
https://wakelet.com/wake/0xFnf38gBOPK-7nGmM7fL
https://wakelet.com/wake/sff7-uGuZTsBJPLL5vPz8
https://wakelet.com/wake/6TejAfMEU05o6Xv61AQUH
https://wakelet.com/wake/Tx8BdyrXPlrUhJCfo96vf
https://wakelet.com/wake/sQ3iK2aWHmZM9UBRQ9BsE
https://wakelet.com/wake/GLZDIpjyvPMU_P0vU1k3V
dimivand (Thursday, 20 January 2022 22:31)
dimivand a8cc6d31e7 https://coub.com/stories/2655972-__exclusive__-market-microstructure-theory-pdf
https://coub.com/stories/2644208-probability-worksheet-for-6th-grade-zlagera
https://coub.com/stories/2643334-download-send-anywhere-premium-v21-build-448853-mod-apk-esbyema
https://coub.com/stories/2643333-bls-2015-manual-pdf-exclusive
https://coub.com/stories/2643332-cervelletto-anatomia-pdf-new
https://coub.com/stories/2643331-how-to-connect-officejet-pro-8600-to-mac-_verified_
https://coub.com/stories/2643330-the-big-bull-720p-top
https://coub.com/stories/2643329-https-drive-google-com-file-d-1pdapaknctykmpc6enzccmkmadkxerpfy-view-usp-sharing-best
https://coub.com/stories/2643328-one45_software_uwo
https://coub.com/stories/2643327-hot-microsoft-office-2016-for-mac-v15-3-crack-torrent
https://coub.com/stories/2643326-full-preschool-prep-7-dvd-set-torrent-ellbare
https://coub.com/stories/2643324-english-crossword-puzzles-with-answers-pdf
https://coub.com/stories/2643325-can-you-download-amazon-instant-video-to-your-mac-free
https://coub.com/stories/2643323-soal-tes-toeic-dan-kunci-jawaban-martdor
https://coub.com/stories/2643322-new-the-scope-of-congressional-powers-worksheet-answers
https://coub.com/stories/2643321-vhl-spanish-101-answers-sakkgian
https://coub.com/stories/2643320-download-song-mac-lethal-10-53-mb-mp3-free-download-jamfaby
https://coub.com/stories/2643318-lsi-sas-sys-drivers-for-mac-anngil
https://coub.com/stories/2643319-playboy-magazine-free-ebook-better-download
https://coub.com/stories/2643317-the-pink-panther-pinkadelic-pursuit-iklark-bot-full
https://coub.com/stories/2643316-caterpillar-company-profile-pdf
https://coub.com/stories/2643315-fl-studio-20-8-0-build-2115-cracked-version-new
https://coub.com/stories/2643314-forsekir-first-invasion-free-download-pc-game-taloak
https://coub.com/stories/2643313-_top_-fishbird-2-for-serum
https://coub.com/stories/2643312-matematicas-2-calculo-integral-dennis-g-zill-solucionario-palervi
https://coub.com/stories/2643311-mcgraw-hill-english-grammar-books-pdf-free-exclusive-download
https://coub.com/stories/2643310-gundam-wing-endless-waltz-1080p-exclusive
https://coub.com/stories/2643309-pearson-realize-4th-grade-math-book-answers-jahming
https://coub.com/stories/2643308-l-carpenito-piani-di-assistenza-infermieristica-pdf-ita-medicina-tntvillage-scambioetic-better
https://coub.com/stories/2643303-hot-the-art-of-sampling-jj-jeczalik-downloadl
uldrlaqu (Thursday, 20 January 2022 23:31)
uldrlaqu a8cc6d31e7 https://wakelet.com/wake/tOpu2OFyPtVICeFkSs-pA
https://wakelet.com/wake/Wa9e42h6jTlYyHaJAqQNG
https://wakelet.com/wake/7bs5IztIjPOtUdwqLF79L
https://wakelet.com/wake/JwYY2OOQjNJmW_BCF8ACA
https://wakelet.com/wake/AC9gZFUpMAzjOfMRh_EZP
https://wakelet.com/wake/ZbiOnx8sxT9tLsjtAZ0lu
https://wakelet.com/wake/PrQ3YniER_La6TRjUnS5B
https://wakelet.com/wake/LTJ0gjXJ9hLiWV15aSrC3
https://wakelet.com/wake/g5gdjxG8nrGopfkWMSzvr
https://wakelet.com/wake/4lxHpYvQRDV-qz8BiplIp
https://wakelet.com/wake/bJqf_pMlPKk8E_44DzxEV
https://wakelet.com/wake/_YLudhRP9y5KuDJZKvJlU
https://wakelet.com/wake/i5859tj7tvdymncOiVuzj
https://wakelet.com/wake/niraf-zMiMELOlVtiBiJj
https://wakelet.com/wake/H47xMyWrJPMYaxAJPhaG0
https://wakelet.com/wake/LzThVoFHD5vZdnzxN_PHm
https://wakelet.com/wake/15KSSjVktrw-UU5M24QXq
https://wakelet.com/wake/FvgxEUCYJPucy9T4Rgkbb
https://wakelet.com/wake/uCZbmyEN_H7CIVEeYXxiN
https://wakelet.com/wake/OWo_BQ42qQYjUS0jSZEi7
https://wakelet.com/wake/ooba1p5NmL8AweiHaeoFv
https://wakelet.com/wake/hGxLgg9GBQLuhsMF31sGi
https://wakelet.com/wake/sNEymtSyXYoqmmDQ47Efg
https://wakelet.com/wake/uLzioC8g2jsYo7aamvxup
https://wakelet.com/wake/eu8yKmzsMHeNtKrs-D_es
https://wakelet.com/wake/FOhHJP2wuA3TV5u69AwVz
https://wakelet.com/wake/kUXj8ucdAz1aPz3fX-fKI
https://wakelet.com/wake/6376UYqsqkdpAvZLCHljG
https://wakelet.com/wake/7LDZ6FwZpVzpqGmIki_yT
https://wakelet.com/wake/LcfLCF5i5yqSIL9N-qFq9
chrsele (Friday, 21 January 2022 00:01)
chrsele a8cc6d31e7 https://coub.com/stories/2755290-descargar-el-archivo-ideal-home-uk-05-2021_downmagaz-net-pdf-35-39-mb-en-modo-gratuito-frydshap
https://coub.com/stories/2755288-download-upd-dong-yi-vietsub-kst-vn
https://coub.com/stories/2755287-rrrrr-rsryorrrrrryor-rrs-rrrs-link
https://coub.com/stories/2755286-adaab-dawood-ibrahim-bol-raha-hoon-full-hindi-movi-animiertes-dissertat-niikale
https://coub.com/stories/2755285-hiatal-hernia-diet-sheet-new
https://coub.com/stories/2755284-download-patched-pdf-epub-professional-excel
https://coub.com/stories/2755283-upd-download-file-katshepgm01-tns-epub-22-09-mb-in-free-mode-turbobit-net
https://coub.com/stories/2755282-monster-dean-myers-pdf-darymank
https://coub.com/stories/2755281-integrated-math-2-volume-1-answer-key-_verified_
https://coub.com/stories/2755280-blackest-eyes-drum-sheet-__hot__
https://coub.com/stories/2755279-stoichiometry-worksheet-answers-na2sio3-free
https://coub.com/stories/2755278-top-justice-league-snyders-cut-2021-english-720p
https://coub.com/stories/2755277-hyperbole-and-a-half-unfortunate-situations-pdf-darvblai
https://coub.com/stories/2755276-the-dark-secrets-of-tonhi-love-full-movie-download-hd-extra-quality
https://coub.com/stories/2755275-auditti8nkupe_repair_manual_pdf-install
https://coub.com/stories/2755274-free-nokia-canada-promising-av-the-next-chapter-of-music-discoveryav-on-may-15th
https://coub.com/stories/2755273-grohe-ladylux-repair-parts-updated
https://coub.com/stories/2755271-__full__-business-plan-pro-15th-anniversary-edition-keygen
https://coub.com/stories/2755272-visual-studio-2010-free-download-full-version-with-crack-fix
https://coub.com/stories/2755270-repack-download-sneaky-sasquatch-zachary-cracks-ok-ipa
https://coub.com/stories/2755269-rus-2004-link
https://coub.com/stories/2755267-philips-avent-express-electric-steriliser-instructions-high-quality
https://coub.com/stories/2755268-les-bases-de-l-anthropologie-culturelle-pdf-top
https://coub.com/stories/2755266-macke-iz-visokog-drustva-sinkronizirano-na-hrvatskirar-colhalc
https://coub.com/stories/2755265-descargar-star-wars-episodio-1-castellano-1080p-saladerr
https://coub.com/stories/2755264-biochemistry-8th-edition-berg-pdf-best-free
https://coub.com/stories/2755261-mixdrop-watch-pyrtskmhd-2021-www-skymovieshd-ltd-unrated-720p-web-dl-hindi-x265-aac-moripala
https://coub.com/stories/2755262-2015-bmw-s1000rr-service-manual-pdf-gladlea
https://coub.com/stories/2755263-velai-illa-pattathari-full-movie-download-tamilrockers-olesnike
https://coub.com/stories/2755260-new-lawyer-client-letter-template
donafoun (Friday, 21 January 2022 00:33)
donafoun a8cc6d31e7 https://wakelet.com/wake/T9SJwdiBZKgJ1LP-WC8Vb
https://wakelet.com/wake/4x2CiBdpGDycmpd_lcl2t
https://wakelet.com/wake/imevV3_EVPKVkITRDINh6
https://wakelet.com/wake/smQzj8AjPN7L9K8sdAePV
https://wakelet.com/wake/3mo7n9PGIrO1ffRlpclWv
https://wakelet.com/wake/ptTnoxhqFU_inqsEXvwCg
https://wakelet.com/wake/5s5JLNAg4Xs-iJYKg4wGc
https://wakelet.com/wake/05n_4EL6d98AgKKiNL0yN
https://wakelet.com/wake/5qJY5bDN6xxcG-S_lFreK
https://wakelet.com/wake/8srCA63iSrBANtOnJHNuZ
https://wakelet.com/wake/3EMqT7O5UWtSWePQmCMoZ
https://wakelet.com/wake/V7W2e6Nb2SVnY-lT6RmGK
https://wakelet.com/wake/AHzJg9hLcRbWasb4NWNQ4
https://wakelet.com/wake/-vTP0jFFzQIqWSQRl9mPR
https://wakelet.com/wake/HT_I_th91uoqILNnmppQV
https://wakelet.com/wake/XyGV0oXkE3u7PE7TiRVZ0
https://wakelet.com/wake/Cfv0YEtL-cK0puEYzt1iq
https://wakelet.com/wake/nSjpcjuSw4IG1XGPhjqVK
https://wakelet.com/wake/xoYTIG4QBWmFrRLBatqF-
https://wakelet.com/wake/R1PgqkVXQaRYEMVmN8-z7
https://wakelet.com/wake/MlSC2udPAf4X8zc9cNmr_
https://wakelet.com/wake/se82uOqjKNOPWuEWgvd90
https://wakelet.com/wake/0ZH-G_-IEACoJpUTGth2Y
https://wakelet.com/wake/yaVqdhaoA216LM0jwQXFr
https://wakelet.com/wake/DoqQSLcuT6gjltAR6HYF8
https://wakelet.com/wake/SgToXHGQBQe625znm5PW0
https://wakelet.com/wake/gNyFgpVoiHE-4n6h_MnGh
https://wakelet.com/wake/PNRPAXp0SxnAR1zGFXsaB
https://wakelet.com/wake/ATDvg4n9oXS4xekyD5fC3
https://wakelet.com/wake/YQoedNX0xpF25lrLnfEnj
zanpea (Friday, 21 January 2022 01:04)
zanpea a8cc6d31e7 https://coub.com/stories/2636269-autodesk-motionbuilder-2020-crack-license-key-free-download-work
https://coub.com/stories/2636268-top-scarica-il-file-roland-virtualsonics-legendary-mac-rar-721-61-mb-in-free-mode-turbobit
https://coub.com/stories/2636267-arrival-online-movie-free-updated
https://coub.com/stories/2636265-download-terraria-v4-v100537-unk-64bit-os100-ok14-user-hidden-bfi-ipa-bernyara
https://coub.com/stories/2636266-the-bridled-tongue-catherine-meyrick-epub-best
https://coub.com/stories/2636264-arkaos-grandvj-1-6-crack-updated
https://coub.com/stories/2636263-blood-link-chapter68-pdf-google-drive
https://coub.com/stories/2636262-_txt-_best_
https://coub.com/stories/2636261-resident-evil-portable-psp-iso-download-bailgeo
https://coub.com/stories/2636260-strucid-hackscript-god-mode-unlimited-ammo-more
https://coub.com/stories/2636259-quintiliano-institutio-oratoria-pdf-italiano-download-install
https://coub.com/stories/2636258-improvising-blues-piano-tim-richards-pdf-35-top
https://coub.com/stories/2636257-repack-p90x-abs-ripper-video-download
https://coub.com/stories/2636256-lexicon-pantheon-ii-vst-v2-0-peace-out-rar-repack
https://coub.com/stories/2636255-pornportal-free-free-account-password-7602f3c5
https://coub.com/stories/2636254-in-the-tall-grass-stephen-king-pdf
https://coub.com/stories/2636253-kanye-west-jay-z-watch-the-throne-zip-download-zip-loriiran
https://coub.com/stories/2636252-new-pathology-books-for-medical-students-free-download-pdf
https://coub.com/stories/2636251-ps3_tomb_raider_bles01780_eboot_fix
https://coub.com/stories/2636249-best-mahatma-gandhi-books-pdf
https://coub.com/stories/2636250-tenet-2020-imax-brrip-1080p-latino-www-gdrivelatinohd-site-mkv-google-drive-shafabr
https://coub.com/stories/2636248-cracked-film-impact-transition-pack-download
https://coub.com/stories/2636247-introduction-to-neural-networks-using-matlab-60-by-s-n-sivanandam-sumathi-amp-deepahottorrent
https://coub.com/stories/2636246-cop-cam-instruction-manual-pdf-hadljam
https://coub.com/stories/2636245-nba-2k16-soundtrack-download-free-torrent
https://coub.com/stories/2636244-link-capture-one-8-film-styles-extended-rar
https://coub.com/stories/2636243-gleamtech-filevista-7-15-0-0-enterprise-retail
https://coub.com/stories/2636242-imvu-credit-generator-download-for-mac-jayben
https://coub.com/stories/2636241-snowrunner_explore_and_expand-codex
https://coub.com/stories/2636240-lesson-6-1-practice-a-geometry-answers-davyhar
yankas (Friday, 21 January 2022 02:06)
yankas a8cc6d31e7 https://coub.com/stories/2637647-mp3-mario-merola-discografia
https://coub.com/stories/2635521-how-do-you-unblock-a-caller-on-a-panasonic-phone-grabene
https://coub.com/stories/2635520-robin-hood-defender-of-the-crown-full-version-free-download-_top_
https://coub.com/stories/2635519-pacote-adobe-cs6-download-crackeado-mac-new
https://coub.com/stories/2635518-better-square-roots-common-core-algebra-1-homework-answers
https://coub.com/stories/2635517-high-quality-neurons-and-supporting-cells-worksheet
https://coub.com/stories/2635516-download-top-folklore-the-long-pond-studio-sessions-2020-1080p-webrip-x264-aac5-yts-mp4
https://coub.com/stories/2635515-mbti-nardi-brain-activityv-5-broomall
https://coub.com/stories/2635514-what-is-pixel-gun-3d-link
https://coub.com/stories/2635513-verified-harry-potter-e-o-prisioneiro-de-azkaban-720p-dublado-filmes
https://coub.com/stories/2635512-gold-metal-detector-circuit-diagram-pdf
https://coub.com/stories/2635511-patthar-aur-payal-1-3gp-movie-free-download-link
https://coub.com/stories/2635510-ej500-intermatic-timer-instructions
https://coub.com/stories/2635496-pornportal-premium-accounts-31-october-2019-link
https://coub.com/stories/2635509-2021-anari-in-hindi-720p-torrent
https://coub.com/stories/2635508-hot-the-culture-map-by-erin-meyer-epub-rar
https://coub.com/stories/2635507-jawapan-module-teaching-learning-chemistry-form-4-nilam-publication-88
https://coub.com/stories/2635506-kaplanmedessentialsusmlestep1__link__-freedownloadpdf
https://coub.com/stories/2635505-a-pdf-page-master-3-6-4-serial-key-rar-valytako
https://coub.com/stories/2635504-how-hiv-infects-cells-worksheet-halwill
https://coub.com/stories/2635503-disketch-cd-label-software-crack-top-serial-keygen
https://coub.com/stories/2635502-fringe-s03-complete-720p-hdtv-x264-yorchri
https://coub.com/stories/2635500-plx-daq-for-mac-seldkenn
https://coub.com/stories/2635501-ics-400-test-and-answers
https://coub.com/stories/2635499-download-lock-mypix-gemini-premium-apk-upd
https://coub.com/stories/2635497-sap-grc-330-pdf-download-__top__
https://coub.com/stories/2635498-ibm-selectric-ii-repair-near-me-javabo
https://coub.com/stories/2635495-the-good-the-bad-the-weird-2008-english-subtitles-henfab
https://coub.com/stories/2635494-datei-herunterladen-nxmac-com_mso20191647-zip-1-69-gb-in-portable-free-mode-turbobit-net
https://coub.com/stories/2635493-anita-woolfolk-educational-psychology-14th-edition-pdf-jaymrhyt
malsea (Friday, 21 January 2022 03:15)
malsea a8cc6d31e7 https://wakelet.com/wake/pcYarWnWfTheDiPiGLkHi
https://wakelet.com/wake/J0M1h-o_7NJA5JXNJQrDg
https://wakelet.com/wake/BAzcqel92TRQ8azX-vdHC
https://wakelet.com/wake/VIwjyypdkfv7q45SUCTKF
https://wakelet.com/wake/nppU69qeEEvP4-7Bb7PJA
https://wakelet.com/wake/t7YG55UP-CXL6zRRy7WLj
https://wakelet.com/wake/Kb3NAfuGKXElQ8tnH9yRv
https://wakelet.com/wake/IyazCTze8mOoIRabrjDUN
https://wakelet.com/wake/wyr4JP-kP2Ep2IoRi18GM
https://wakelet.com/wake/a82_rBnvIH6pRRX9cFd0U
https://wakelet.com/wake/-cvSOgdAgfwmIb0FZV4gC
https://wakelet.com/wake/NAwnHMtvZXuxfc1pWYUK0
https://wakelet.com/wake/fW7PPQOxE5HA0kv8cGDmv
https://wakelet.com/wake/RHwH-DJfDOQsPLlVokACp
https://wakelet.com/wake/OgzTZ5NnsEx6UGul_KdKw
https://wakelet.com/wake/s1ZdMTVXfqvjua0yF9ukB
https://wakelet.com/wake/VykYsVfjrFQdf54FsUYAG
https://wakelet.com/wake/S_d9BIpMlY8cHe2ZMKhd9
https://wakelet.com/wake/cLlLYXq3xKGfZYBthdAG8
https://wakelet.com/wake/PEgOdRC_mjOJ_RoQAmK3Q
https://wakelet.com/wake/qqwmZCgUx2YGFwjZbyEAD
https://wakelet.com/wake/of6GkaPjxwTsdxLnyyBfc
https://wakelet.com/wake/xnkTXdTJ-SD7jAfNKUoXh
https://wakelet.com/wake/U6zL19cILMnXb5cL3FbKV
https://wakelet.com/wake/cbTt6bVecAG-bzeUzYtu7
https://wakelet.com/wake/TCz9YJyMbVM9Ikkm2SEj0
https://wakelet.com/wake/zNKac7CAx_8XhdhoHT9wc
https://wakelet.com/wake/6DXsloWR_c-w_jcq2BbX3
https://wakelet.com/wake/on9PK6iGdP3OJO5ia3vs7
https://wakelet.com/wake/7jA9G5c3m4muc-z-GD2cX
hamilar (Friday, 21 January 2022 04:22)
hamilar a8cc6d31e7 https://wakelet.com/wake/0483avDgyJch-jbp3q0QD
https://wakelet.com/wake/97l23MWQZhxDgYKTotfxc
https://wakelet.com/wake/w7bUC3lId-prGL5h5uQNb
https://wakelet.com/wake/vobAFmGaxi7_CglUqq-5B
https://wakelet.com/wake/w1S5zD1VlNw04NYtAR1hM
https://wakelet.com/wake/pWyUoQTO7Z2lPJMfF6nA5
https://wakelet.com/wake/kHn6iQv2sJmNz98hRTW8n
https://wakelet.com/wake/RUVZjquEjNblBRNYWU_aN
https://wakelet.com/wake/E2O0aOLfHWLEOSODHHDmm
https://wakelet.com/wake/BanE1Lwlkraboc0Zrf0LY
https://wakelet.com/wake/y3tzPAnqnLX92sEgYxQX5
https://wakelet.com/wake/QJl-ZA3_BVlv0OKoTUQIB
https://wakelet.com/wake/CVly1F6VpvZt8V46OlI0H
https://wakelet.com/wake/aDk2emtI8a9TjPPxNoJWL
https://wakelet.com/wake/-950lCbbUqPkk6n47yxKi
https://wakelet.com/wake/kon_JyW1yeyCGCZ_VLU7S
https://wakelet.com/wake/SIVsPPpQNieaJvFPm1Idr
https://wakelet.com/wake/UbZgUObHWPzcTT3Ayh-Kq
https://wakelet.com/wake/4WJVQ_-k414TsfCtFSzaO
https://wakelet.com/wake/97Oq9F8qY3L7qVEwJ4M6c
https://wakelet.com/wake/8g38MbTo7fDeVrxTHEQnh
https://wakelet.com/wake/TcpUBhgCZbEAvGt2eIV8W
https://wakelet.com/wake/XkkQ5b1DEKpzDPRpXvXh-
https://wakelet.com/wake/-2F10mcz3u69wRZFhCbKV
https://wakelet.com/wake/z3nKXak6AACPkzXCEiQol
https://wakelet.com/wake/6Cki1K62mL_NYhxJZNhoI
https://wakelet.com/wake/NMNM9_IsrbJHXjgrOj7yf
https://wakelet.com/wake/vacDxw2dh59kDOAVc3sj_
https://wakelet.com/wake/lCZpR6LvSNMtyY83NfOxK
https://wakelet.com/wake/MU8iQqCWJAjGOuYked300
fabifin (Friday, 21 January 2022 04:54)
fabifin a8cc6d31e7 https://wakelet.com/wake/QcgmKoYeuEd0kOve0fU9U
https://wakelet.com/wake/w9j9b5lalTGwBoamENOOC
https://wakelet.com/wake/Ul0_Svsxd8RMK4YbKQFz3
https://wakelet.com/wake/gTCbA7jmhaw3ikafm4wXT
https://wakelet.com/wake/O_SQTQ_ppqgP1I80oA6Qt
https://wakelet.com/wake/9JoMtX3s7ateoEJP1uG5K
https://wakelet.com/wake/Bvg7TtXyT4VbDuc9k4iyC
https://wakelet.com/wake/twX1xNxd5MUJrA1ygc6j7
https://wakelet.com/wake/GnLYGY9bIvo49KTFMnpNe
https://wakelet.com/wake/omMki3q_et87yIeAwEY5f
https://wakelet.com/wake/OfJ8LkaAHFPLwcl_BCkkm
https://wakelet.com/wake/xNn_YT2SMPQ__1PmbNbXb
https://wakelet.com/wake/_W9O-KN3w7S9UztJscvzw
https://wakelet.com/wake/fx_19-ChLZ5ZxyXHzlGeb
https://wakelet.com/wake/1249Z7tLOAzMNGnossVwO
https://wakelet.com/wake/6aYSdFNn5yoIBnx8m1GY3
https://wakelet.com/wake/saBbLWP6YwMZDNPhsoE3q
https://wakelet.com/wake/6i7hAQNyvVhWjh6F6F3ZB
https://wakelet.com/wake/dR0xsPGU4G9og11wx8-tS
https://wakelet.com/wake/3FS95d6B30Fov2RvMqTpp
https://wakelet.com/wake/j4OaCN7sIfVtXv0BFvxvQ
https://wakelet.com/wake/nLU3FF7IvBMP3SOZCo_IJ
https://wakelet.com/wake/M3GnXN3EaYidklxskDvt8
https://wakelet.com/wake/UBqe-xfM6phAHrWJAzalq
https://wakelet.com/wake/x9llIPM3ZcBS7etobhvgX
https://wakelet.com/wake/lH-pPeWbQkcJD7LetsH3P
https://wakelet.com/wake/yhywefRV9kh-1JVMEk1i4
https://wakelet.com/wake/Po1CIFz33Kdi5S4ouU4RW
https://wakelet.com/wake/Ywg9sCbB-urKoBxTDpfuo
https://wakelet.com/wake/V3r-Vm-I2HuoVCaZadHP_
betben (Friday, 21 January 2022 06:42)
betben a8cc6d31e7 https://coub.com/stories/2641826-propellerheads-recycle-v2-2-4-win-osx-incl-__exclusive__-keygen-air-crack
https://coub.com/stories/2641825-prince-harry-and-hiv-awareness-campaign-ricky-martinvs-getting-married-bob-dylanv-verified
https://coub.com/stories/2641824-fixed-wintousb-stuck-at-0l
https://coub.com/stories/2641823-russianbarefamilybeachpageantpart1avirar
https://coub.com/stories/2641822-ash-cooking-2-min-of-553821c0
https://coub.com/stories/2641821-lion-muthu-comics-download-patched-pdf
https://coub.com/stories/2641819-the_island_pdf_armin_greder
https://coub.com/stories/2641816-downloading-audiobooks-to-an-ipod-how-parnchar
https://coub.com/stories/2641820-magic-chef-bread-machine-vbm200c-manual-exclusive
https://coub.com/stories/2641817-graphisoft-archicad-24-2021-full-best-x64-espagol-mega
https://coub.com/stories/2641818-2-girls-1-cup-full-version-jonbent
https://coub.com/stories/2641815-forscan-lite-v1-5-4-patched-apk-latest-caibir
https://coub.com/stories/2641814-challenging-cognitive-distortions-worksheet-pdf-__full__
https://coub.com/stories/2641813-download-lagu-the-fratellis-5-54-mb-mp3-free-download-waleumbu
https://coub.com/stories/2641812-top-kiss-me-liar-chap16-pdf-vgooglev-diskas
https://coub.com/stories/2641811-kontakt-5-6-5-full-crack-hektfale
https://coub.com/stories/2641810-dark-souls-3-pyromancer-build-guide
https://coub.com/stories/2641809-dividir-un-archivo-en-varios-rar-mac-davijai
https://coub.com/stories/2641808-midtown-madness-download-for-mac-geegear
https://coub.com/stories/2641807-download-mac-os-mojave-dmg-flordei
https://coub.com/stories/2641805-inheritance-of-traits-worksheet-answers-readworks
https://coub.com/stories/2641806-ziegenhof-catherine-andrg
https://coub.com/stories/2641804-2021-cerberus-cracked-apk
https://coub.com/stories/2641803-team-r2r-korg-software-pass-emulator-v1-0-0-r2r
https://coub.com/stories/2641802-planet-earth-1080p-mkv-to-720p-exclusive
https://coub.com/stories/2641801-livro-arquitetura-vivenciada-2021-download-pdf
https://coub.com/stories/2641800-fix-download-tivimate-iptv-player-v2-8-0-premium-dlpure-com
https://coub.com/stories/2641799-fortnite-monopoly-gets-new-release-date-pre-orders-soon-feiray
https://coub.com/stories/2641798-salaam-namaste-hai-hd-1080p-movie-top
https://coub.com/stories/2641797-jvcxb-drum-kit-vol-__top__
salotty (Friday, 21 January 2022 07:15)
salotty a8cc6d31e7 https://wakelet.com/wake/psUWS-phO4vvi1T_8TbF4
https://wakelet.com/wake/MC4LCiJ8RgO-R0jMPFZtc
https://wakelet.com/wake/PcFznCssDl5A6C6Vq-ME9
https://wakelet.com/wake/0zTYBE7K39_5RMdgsbm_k
https://wakelet.com/wake/9RXK-aCtJRc8WbwZZbDJF
https://wakelet.com/wake/kH57JF2X3IjBii4H7-FOa
https://wakelet.com/wake/HRfdtPjxGBsZg53Xf63Vn
https://wakelet.com/wake/6G2Z0ykHV7Abwl0yEOwWz
https://wakelet.com/wake/-NPMRLHxEcwDnDh2hA5DB
https://wakelet.com/wake/LxX-r_9b3NfXPnU5Cveeo
https://wakelet.com/wake/Un4wlXlxVaW9hvBDtrz1Z
https://wakelet.com/wake/UMbRC6U_Yhtvy5KW_XNwx
https://wakelet.com/wake/PK-enPvloXZj154prMxMj
https://wakelet.com/wake/KyoOxe2BP_QbXvwX07Yt8
https://wakelet.com/wake/_N9BGET_RfitGopV2Kq9E
https://wakelet.com/wake/9mWE57VZZVPJV2BOvne3i
https://wakelet.com/wake/ptjmczcQEV_l7ONhdP7CX
https://wakelet.com/wake/3i9GQUBuRUpJd1OXhyuqF
https://wakelet.com/wake/m9-Otlg4kuai2nr4Wo-AK
https://wakelet.com/wake/h4b7UXasCGKI6kHHxDFds
https://wakelet.com/wake/NzCr-cKmiCnHoVnAgoJ5L
https://wakelet.com/wake/lUrZv6RQBGaShmynXpIGk
https://wakelet.com/wake/mdAPUdtRn_-XXj4q0aNgV
https://wakelet.com/wake/jKvQvky8FuIgjK3Rov4ZX
https://wakelet.com/wake/TwcOq2-GSsjh1Lpu1-HnG
https://wakelet.com/wake/SNi_qxHmfKWFYg7KfWEue
https://wakelet.com/wake/NVQiedvcC5uuhg4ebcmOL
https://wakelet.com/wake/FBN_gXDpP-XE5fFntkwOI
https://wakelet.com/wake/HWa7ukmFbwRqs2i78hMQs
https://wakelet.com/wake/gA_FriOSjLDf0M54sLDHW
alygard (Friday, 21 January 2022 08:59)
alygard a8cc6d31e7 https://coub.com/stories/2820957-work-mame-hlsl-settings-1080p-vs-4k
https://coub.com/stories/2820953-updated-database-management-functions-answer-key
https://coub.com/stories/2820956-cornerstone-4-0-0-nulled-v-the-wordpress-page-builder
https://coub.com/stories/2820954-libros-sobre-administracion-de-empresas-pdf-gratis
https://coub.com/stories/2820955-2021-sunflower_sisters_-_martha_hall_kelly-epub
https://coub.com/stories/2820952-le-mythe-de-sisyphe-texte-intggral-egiwin
https://coub.com/stories/2820951-athentech-perfectly-clear-complete-3-6-3-1503-crack-high-quality-mac-osx-neeroz
https://coub.com/stories/2820950-nfs-most-wanted-copspeech-big-sound-file-rapidshare-deannant
https://coub.com/stories/2820949-download-file-varpotp06-flac-whirlzzum-mm-rar-449-07-mb-in-free-mode-turbobit-net-__exclusive__
https://coub.com/stories/2820948-darling-rose-gold-stephanie-wrobel-epub-darmor
https://coub.com/stories/2820947-biochemical-test-in-microbiology-pdf
https://coub.com/stories/2820945-__exclusive__-download-mini-motorways-macos-zip
https://coub.com/stories/2820946-blast-output-format-17-sanyess
https://coub.com/stories/2820944-better-an-introduction-to-the-history-of-psychology-7th-edition
https://coub.com/stories/2820942-patched-donald-trump-mac-miller-instrumental-download
https://coub.com/stories/2820943-verified-izotope-v-iris-2
https://coub.com/stories/2820940-pdisk-ep-01-fareb
https://coub.com/stories/2820941-datei-herunterladen-bldamsnntg110421-pdf-23-33-mb-in-free-mode-turbobit-net-top
https://coub.com/stories/2820939-_hot_-descargar-presto-88-mas-crack
https://coub.com/stories/2820938-systat-13-crack-free-download-updated
https://coub.com/stories/2820937-hot-autocad-lt-2019-download-free-get-into-pc
https://coub.com/stories/2820936-musk-takes-first-step-towards-spacex-broadband-vision-link
https://coub.com/stories/2820935-the-style-diary-of-a-bollywood-diva-pdf-11-__hot__
https://coub.com/stories/2820933-high-quality-free-printable-notary-signature-page
https://coub.com/stories/2820934-eu4-center-of-reformation-not-spawning
https://coub.com/stories/2820932-hp-envy-4500-ink-error-message-amauver
https://coub.com/stories/2820931-new-online-notepad-untitled-11-28-2020-3-37-13-am
https://coub.com/stories/2820930-mary-kay-excel-spreadsheet
https://coub.com/stories/2820929-updated-passfab-4winkey-ultimate-7-1-0-8-full-crack
https://coub.com/stories/2820928-togaf-standard-9-2-pdf-gaijasp
alisxant (Friday, 21 January 2022 09:33)
alisxant a8cc6d31e7 https://coub.com/stories/2627551-microsoft-buys-leader-in-3-d-sensingvtechnology
https://wakelet.com/wake/1cT1IqyvrcytdNsDIgMkf
https://wakelet.com/wake/qbxu5TnZPitW5G_3ao2yj
https://wakelet.com/wake/uicuvqTnQpcJ8-ENLArq_
https://wakelet.com/wake/e3bZE8O6F1WHJtHrXHuwC
https://wakelet.com/wake/92HLlJBfQzZhftvWoBIw6
https://wakelet.com/wake/PZElmXB15Ge_BZXs-jKAh
https://wakelet.com/wake/04oHb4frE5QcApF_USih7
https://wakelet.com/wake/hMbcon7Wbl9RSTtgfjNEc
https://wakelet.com/wake/H40qJ28IxKJ0APVi3dnN6
https://wakelet.com/wake/eeGw-gLN2eMbPBcepCunZ
https://wakelet.com/wake/28TeFxCXwgovPbOz-moqB
https://wakelet.com/wake/Jascwc2e6vEySw46QozrR
https://wakelet.com/wake/zZH-OgLAq6GEXGl0DJOO8
https://wakelet.com/wake/qeu_ew9zbeCAWrEdtTLG6
https://wakelet.com/wake/y57yAHM9MAgu4FsTzxGUj
https://wakelet.com/wake/tj1NIdMs2wYmOgbGhqrta
https://wakelet.com/wake/LPY7lbtihrVCKLf7Y9E9S
https://wakelet.com/wake/HXI8KCJ_jM5MRip4sRKBK
https://wakelet.com/wake/_eUA41KUWuKsnfhoZt0jx
https://wakelet.com/wake/Ae_9DXC3js-M5a-bA6fKa
https://wakelet.com/wake/StQGiBo1Dlv6YyofFO-0J
https://wakelet.com/wake/8qzo-Mnv3DWpGVZQV-2cH
https://wakelet.com/wake/DAYeTilKhfczAm2JHB6nr
https://wakelet.com/wake/6hXZlQURqfHtfyi0tRX_g
https://wakelet.com/wake/eF8q1U_c4xX651tH_8kLI
https://wakelet.com/wake/aJgyAziTCoL6LtiAKlvVz
https://wakelet.com/wake/jtPu1ARYqxn55T9BSJBTr
https://wakelet.com/wake/T4oNG1cjFuDrcJJyMg9Gu
https://wakelet.com/wake/glCiq6xedQbdhDXJBLeg4
bengle (Friday, 21 January 2022 10:07)
bengle a8cc6d31e7 https://wakelet.com/wake/36RrV0XU9ukWuQOGhN2iB
https://wakelet.com/wake/aInHf2fPB4XeNAET9dzxO
https://wakelet.com/wake/GMcGWOYyNQLMxx1O3qNCn
https://wakelet.com/wake/kTq3_Lmhkq4uhoZezOY3p
https://wakelet.com/wake/WJLaCoYGA1WLqXZD4rFks
https://wakelet.com/wake/SpvaM3ki8w5mXU7-9Bizp
https://wakelet.com/wake/KkuPGtYx8VbJ-ceaCI3VW
https://wakelet.com/wake/7CoY6xlTfFqFdLawPtpUz
https://wakelet.com/wake/IYEQ5o1Q1-hpLCo64xmWo
https://wakelet.com/wake/T7YcNPwk-FRJo6IlMuIon
https://wakelet.com/wake/fjhAxRKzf2EANtKIj69El
https://wakelet.com/wake/VTdaVVaN9tw3rq47ZGh0E
https://wakelet.com/wake/0i2hF8GstL6jEQyoAsPBa
https://wakelet.com/wake/zOi5oet1lgighpo5r8YZu
https://wakelet.com/wake/bT90cVrqez8pzLtvbGis7
https://wakelet.com/wake/eP3CkSScVII8raBR-c7zG
https://wakelet.com/wake/mJQuun_4L05y1N2WWW77q
https://wakelet.com/wake/JyUW9X2LXKKSajk_JmnRO
https://wakelet.com/wake/4BFXvoc_EYVXEMPbLh9tX
https://wakelet.com/wake/cKPz-mml7qC4IBA0EjmGG
https://wakelet.com/wake/0fWCZAgeRB5J5nq6J6FVo
https://wakelet.com/wake/iw-s-efzjzHAqxujoIwn9
https://wakelet.com/wake/3cQaprxkBCQ3wQeqR2Crk
https://wakelet.com/wake/2iXR7Mv-AIPRPdIy61J9y
https://wakelet.com/wake/lFcTcYriJys743b0aVccn
https://wakelet.com/wake/uZsKHK-djh_rawvB0y_Ie
https://wakelet.com/wake/b0pyHht71Om4xSaSAj2SL
https://wakelet.com/wake/UIfqZ-5OS-Fjlq7Bb77Cl
https://wakelet.com/wake/Xkv2MJNUTC8A2caVtI5QD
https://wakelet.com/wake/7iVuTnVsSLMxForlElZzh
ingmari (Friday, 21 January 2022 11:15)
ingmari a8cc6d31e7 https://coub.com/stories/2682544-sparkol-videoscribe-pro-2-2-gramare
https://coub.com/stories/2682543-link-tagesdosis-7-2-2020-v-die-russophobie-v-ein-sehr-profitables-geschaft-podcast
https://coub.com/stories/2682542-patched-conduct-and-practices-handbook-course-cph-pdf-to-excel
https://coub.com/stories/2682541-material-handling-equipment-alexandrov-pdf-download-saktlane
https://coub.com/stories/2682540-primeval-season-1-720p-download-congar
https://coub.com/stories/2682539-commando-a-one-man-army-hindi-movie-720p-hd-torrent-hazasal
https://coub.com/stories/2682538-love_contract_zip_pdf-intlave
https://coub.com/stories/2682537-witness-for-the-prosecution-pdf-caeswan
https://coub.com/stories/2682535-vladmodels-twm2102-zhenya-y114-myllmanl
https://coub.com/stories/2682534-hd-wafa-a-deadly-love-story-raghqui
https://coub.com/stories/2682533-free-lulo-font-repack
https://coub.com/stories/2682532-bc-science-10-connections-workbook-answers-letielb
https://coub.com/stories/2682531-module-7-test-answers-math-patched
https://coub.com/stories/2682529-asme-standards-pdf-free-download-hot
https://coub.com/stories/2682530-claim-me-j-kenner-epub-tuebl-free-__link__
https://coub.com/stories/2682528-eastwest-hollywood-brass-vst-free-download-portable
https://coub.com/stories/2682527-bulgarian-manual-pdf-greg-nuckols-link
https://coub.com/stories/2682519-godiego-golden-best-flacl
https://coub.com/stories/2682520-install-el-camino-hacia-el-amor-deepak-chopra-pdf
https://coub.com/stories/2682526-aparichit-full-movie-in-hindi-720p-89l-fithdio
https://coub.com/stories/2682525-free-pantone-tpx-free-download
https://coub.com/stories/2682524-kala-bhairava-stotram-in-telugu
https://coub.com/stories/2682522-d16-group-decimort-120-vst-au-mac-osx-ubrar-banjkan
https://coub.com/stories/2682518-apocalypto-dual-audio-hindi-top-download-480p
https://coub.com/stories/2682517-case-interview-secrets-victor-cheng-epub-to-pdf-full
https://coub.com/stories/2682516-yanni-ethnicity-full-album-zip-high-quality
https://coub.com/stories/2682515-evil-genius-gog-skidrow
https://coub.com/stories/2682514-download-file-turkishneedlerace-pdf-110-86-mb-in-free-mode-turbobit-net-talgare
https://coub.com/stories/2682512-pensamento-e-vida-livro-pdf-fixed
https://coub.com/stories/2682513-repack-james-joyce-araby-pdf
donadaph (Friday, 21 January 2022 16:42)
donadaph a8cc6d31e7 https://wakelet.com/wake/aMkXMPtQr3gQ5Wbg2ZOWx
https://wakelet.com/wake/PmabXTihtliwSrewFOoA-
https://wakelet.com/wake/25xJdIHe5VidZUpDgdajJ
https://wakelet.com/wake/6uEpre5VNM3nynIUbb4tO
https://wakelet.com/wake/Zeo-R_jcfS4mau_XiXo7C
https://wakelet.com/wake/Q77kK3w2bFhuxBpedSK8d
https://wakelet.com/wake/adly7DpO2pgP9dc7BmxAx
https://wakelet.com/wake/Qjf6TkKS7IRXSaP5WJX3F
https://wakelet.com/wake/syL75mUgzfuManb4cDvTh
https://wakelet.com/wake/qTRPFbexqpNM7bVUhWJdT
https://wakelet.com/wake/9Qao1HtcM6F1vSeejsMdA
https://wakelet.com/wake/_ur2nABeqJ3iy7_vwHKrS
https://wakelet.com/wake/QIjRFLC0s9Tnnty70t4-c
https://wakelet.com/wake/pt7arA_6vYc-Pq4ggoDo8
https://wakelet.com/wake/hppjDBVPn6UCnebdaylWo
https://wakelet.com/wake/dNiW6d1E1r6PBewV-7Uyn
https://wakelet.com/wake/oj6VQX5hIH66sJ4hRBV_e
https://wakelet.com/wake/os-Ck9oAuGiE1OmALCFEI
https://wakelet.com/wake/H58BAg1cUpxIVWbqBX4vW
https://wakelet.com/wake/fs_SYzgCm5IoWBrrq7j4d
https://wakelet.com/wake/bH-6N9kEwXio88r0KVqFp
https://wakelet.com/wake/nVbrTbdGBNK6XFfzhl_q_
https://wakelet.com/wake/PmhXet7xX7FSYmT966P6E
https://wakelet.com/wake/v7PqMFD9617-iDkykDEhh
https://wakelet.com/wake/mn5DHyr4P1HGFpilVN3ly
https://wakelet.com/wake/9VycRiMFc9Z32IO0xtucT
https://wakelet.com/wake/tBjtzj_zrKF1K81R3ewTX
https://wakelet.com/wake/d8EM_7HDjhKcrr9GJU5Cu
https://wakelet.com/wake/O7y1wgEsVeJ1CIHZSnYPO
https://wakelet.com/wake/ghbaNRjCzvkJAzGRTGDYb
kapaxant (Friday, 21 January 2022 17:13)
kapaxant a8cc6d31e7 https://wakelet.com/wake/OPTHMCwLSTyjPP6qWjdQd
https://wakelet.com/wake/CGKNPItunqaBd0fPIZ8Xa
https://wakelet.com/wake/Pdr9rT5PNw5_b97BM2MEr
https://wakelet.com/wake/zjr2yCiXt-RX34WjRRv7c
https://wakelet.com/wake/oCHfWTui-B8pUtaYXq7Ew
https://wakelet.com/wake/vR5z8xZl-1mSGY_Ct3XbW
https://wakelet.com/wake/wh6PoSjDnHxsI0rB4DwR3
https://wakelet.com/wake/KHCrfzQUJwyxF8zT3bLmK
https://wakelet.com/wake/FU2etQL8JCrmkBqX4CdJT
https://wakelet.com/wake/Q2ITyKuTMzMWcKRtn3i9Z
https://wakelet.com/wake/7oKMps1s-2-YJNUujrT0b
https://wakelet.com/wake/P6yEx3vsJ6CyaaEiK7RbR
https://wakelet.com/wake/RT1-52ZOYKrBsGJlJ6zhb
https://wakelet.com/wake/vJtnIceHLLKSaI0azWqWz
https://wakelet.com/wake/kG4QsbUqouUsr_6zlcOhZ
https://wakelet.com/wake/XKFmJmsSA5XT2ciLkJYlf
https://wakelet.com/wake/RksFZp13yBcJ4PBxiCg65
https://wakelet.com/wake/u5dPw1wSJdVmqlHTslG6e
https://wakelet.com/wake/klHPTgZqI5hRBx1H_v-O1
https://wakelet.com/wake/xpYmoCS17h5bef2XSF9iJ
https://wakelet.com/wake/A_IMvyE7NfPHc9FBavrzN
https://wakelet.com/wake/m87xyDILNW5_Un0YcgNf_
https://wakelet.com/wake/w9sJJKsgF4XWJse-_s-0e
https://wakelet.com/wake/Im0zd_T31DGzpXVg-7YeN
https://wakelet.com/wake/BUj6s6JoKwaTw6Kj1I_h7
https://wakelet.com/wake/ocyqwsjz1BeYshO6EsCfR
https://wakelet.com/wake/nOdcydV5bbKdTHwGFgwae
https://wakelet.com/wake/ljiaY69phOcos7zlsucFR
https://wakelet.com/wake/tAiQp9_pFwMk5fn2sB_7X
https://wakelet.com/wake/fnur6a0PO6d-h7YypMF35
phylau (Friday, 21 January 2022 18:18)
phylau a8cc6d31e7 https://coub.com/stories/2685616-fierycolorprofilersuitecrack-lenyedi
https://coub.com/stories/2685615-download-villa-savoye-dwg-cracked
https://coub.com/stories/2685614-biblia-hebrea-transliterada-pdf-free-new
https://coub.com/stories/2685613-xvideos-zoofilia-hombres-follando-perra-gran-danesl-high-quality
https://coub.com/stories/2685612-public-relations-the-basics-ron-smith-pdf-aftflav
https://coub.com/stories/2685611-episode-10-2-song-free-download-myrgar
https://coub.com/stories/2685610-yaariyan-full-top-movie-free-download-hd-720p
https://coub.com/stories/2685609-fixed-tglgcharger-un-fichier-moto-journal-2301-pdf-101-59-mb-in-free-mode-turbobit-net
https://coub.com/stories/2685608-index-laws-differentiated-worksheet-tes
https://coub.com/stories/2685607-hp-elite-dragonfly-review-proving-business-laptops-donvt-have-to-be-bland-delkian
https://coub.com/stories/2685606-logitech-quickcam-express-driver-for-mac-sheezoph
https://coub.com/stories/2685605-better-iglasses_3-2-1_setup_-_keygen_zip
https://coub.com/stories/2685604-cdrdicom4556-top
https://coub.com/stories/2685603-taboo-charming-mother-english-subtitles-episode-7-harijasi
https://coub.com/stories/2685602-free-sins-of-the-fathers-full-movie-hd-download
https://coub.com/stories/2685601-rrrssrrr-srrrr-minecraft-v1-16-2011-ipa-top
https://coub.com/stories/2685599-hack-acoustica-mixcraft-pro-studio-7-7-311-multilingual-exclusive-keygen-air
https://coub.com/stories/2685600-sonic-forces-2020-crack-and-torrent-full-free-download-for-pc-and-mac-repack
https://coub.com/stories/2685598-new-environmental-geology-laboratory-tom-freeman-answer-key-zip
https://coub.com/stories/2685597-chandramukhi-telugu-movie-torrent-exclusive-download-1080p
https://coub.com/stories/2685596-mundus-novus-vespucci-pdf
https://coub.com/stories/2685595-portable-4d-payments-3-d-secure-integrator-16-0-build-6862-for-net-activex-asp-com-edition
https://coub.com/stories/2685594-modern-family-dndir-torrent-areivi-en-kral-torrent-sitesi-free
https://coub.com/stories/2685593-miss-alli-sets
https://coub.com/stories/2685592-full-making-a-murderer-episode-3-worksheet-answers
https://coub.com/stories/2685589-lc-technology-rescuepro-deluxe-7-0-1-5-crack-application-full-version-install
https://coub.com/stories/2685591-be-your-own-windkeeper-book-pdf
https://coub.com/stories/2685590-fac-simile-lettera-riduzione-orario-di-lavoro-per-crisi-aziendale-aysals
https://coub.com/stories/2685587-logic-pro-x-10-0-4-packet-dada-dmg
https://coub.com/stories/2685588-devilbiss-525ks-user-manual-install
taksham (Friday, 21 January 2022 18:48)
taksham a8cc6d31e7 https://wakelet.com/wake/1puQjX34erIcuFJ8z9-WI
https://wakelet.com/wake/6eqrL80qwYyNGjpyEwhtq
https://wakelet.com/wake/YV_ybMNAsQHFBeze6iDuR
https://wakelet.com/wake/JRkkkgQVFfPIjr-O9DWS4
https://wakelet.com/wake/G5PXUnq_X22rnt24x3NZ0
https://wakelet.com/wake/nXJ6ETujakVpUjMAE62na
https://wakelet.com/wake/G4-xV1s2QRByVXIp1pkTQ
https://wakelet.com/wake/hpz6G4g6vXjZjqWqMU4he
https://wakelet.com/wake/vWhLWuT8D9lqMAE0u5xwQ
https://wakelet.com/wake/HxLM7m2SC6kzSklpVQ5nS
https://wakelet.com/wake/KlSdLK5E_j-1WhokNiJlo
https://wakelet.com/wake/uXyrw5wFMUB8IvDdO47ke
https://wakelet.com/wake/oXMrYLQA1Fpq7PUXyOxAS
https://wakelet.com/wake/6Ykc7k01HA470lpPVdddq
https://wakelet.com/wake/wtPh36D0HiW9lisHwFySt
https://wakelet.com/wake/ydkee9pDST5wq4jcRpfHK
https://wakelet.com/wake/gPbKoKghg6Mr31bz4BxPA
https://wakelet.com/wake/-sCmHs0jYHt61rf1NruVW
https://wakelet.com/wake/fbAPtp7B85HVm06N3Wg0L
https://wakelet.com/wake/G1D_MZKRv0hUYOPq1cavn
https://wakelet.com/wake/jQPWF9swMXusotGNo_0ln
https://wakelet.com/wake/ol0SjKFlT4RXHJZO7iX9j
https://wakelet.com/wake/DJsTTti9MtcLMPlO9sFMA
https://wakelet.com/wake/Me5-bi1JYGaY8s-_HoafW
https://wakelet.com/wake/9p2e9BicMznJ0KBCajuU0
https://wakelet.com/wake/WAdBZxFKlgCtCNf_OsT2L
https://wakelet.com/wake/_Hgu6r4sKMa5BwH5m4l6P
https://wakelet.com/wake/BH5fD8Tc_BepyY5J0vAKU
https://wakelet.com/wake/1NLM8ipPGR7PKKyMp8x4-
https://wakelet.com/wake/lVDEr7UhjchMtPXIVSCWI
chafok (Friday, 21 January 2022 19:20)
chafok a8cc6d31e7 https://coub.com/stories/2755354-step-up-5-full-movie-english-version-hd-tv-best
https://coub.com/stories/2758381-onn-mini-speakers-v300-drivers-for-mac-elbitho
https://coub.com/stories/2751407-soviet-national-anthem-trumpet-sheet-music-updated
https://coub.com/stories/2751402-rival-kingdoms-the-endless-night_v2-2-6-84_mod_siv-hot
https://coub.com/stories/2751401-dndirilecek-dosya-image-line-fl-studio-producer-edition-v20-0-5-91-macosx-indirvip-cl-biagbert
https://coub.com/stories/2751391-full-cummins-engine-serial-number-decoder
https://coub.com/stories/2751393-how-to-read-an-interstate-battery-date-code
https://coub.com/stories/2751390-charles-hurst-social-inequality-pdf-_hot_
https://coub.com/stories/2751385-screenflow-9-0
https://coub.com/stories/2751382-exclusive-tony-hawks-pro-skater-1-2
https://coub.com/stories/2751381-localized-english-iw00-iwd-for-cod-mw3-rar-bitcomet-buscar-regu-new
https://coub.com/stories/2751376-diskinternals-raid-recovery-3-2-keygen-_verified_
https://coub.com/stories/2751377-cherish-preteen-model-pics-ellnat
https://coub.com/stories/2751371-__link__-ultrafire-xml-t6-flashlight-user-manual
https://coub.com/stories/2751369-top-free-download-flesh-2020-hdrip-hindi-season-1-complete-show-hd-480p-500mb-show-khatrimaz
https://coub.com/stories/2751368-professional-biography-examples-pdf-hecjar
https://coub.com/stories/2751362-exclusive-roystuartglimpse13zip
https://coub.com/stories/2751358-punyahavachanam-mantras-pdf
https://coub.com/stories/2751355-upd-studioplug-smokepurpp-drum-kit-wav-midi
https://coub.com/stories/2751349-free-anna-movie-english-subtitles
https://coub.com/stories/2751347-full-bastille-bad-blood-zippyshare-mp3
https://coub.com/stories/2751341-cadsoft-eagle-7-7-0-professional-ultimate-crack-portable-application-full-top-version
https://coub.com/stories/2751344-atholl-highlanders-bagpipe-sheet-music-selybre
https://coub.com/stories/2751345-rabbit-proof-fence-full-book-pdf-verified
https://coub.com/stories/2751342-new-kurzweil-pc3-service-manual
https://coub.com/stories/2751338-rosetta-stone-german-download-free-full-portable-version
https://coub.com/stories/2751337-the-doors-la-woman-torrent-download-takcol
https://coub.com/stories/2751334-link-nobody-wanna-see-us-together-akon-download
https://coub.com/stories/2751333-upd-1710-19un-rubio-mp4
https://coub.com/stories/2751329-xp-key-recoverer-and-discoverer-5-12-free
julfaxa (Friday, 21 January 2022 19:52)
julfaxa a8cc6d31e7 https://wakelet.com/wake/J28xY1aidMkNg3ldF2ySe
https://wakelet.com/wake/9aWFDZh66fY0NcwzDswkj
https://wakelet.com/wake/H14fRtPBizjeWifiv73DY
https://wakelet.com/wake/DolIlDXqNxdybE4n6YawL
https://wakelet.com/wake/eqbETs2DN_1eEgYMNAWMG
https://wakelet.com/wake/-YMC2VWslQ9QaFeylpJPY
https://wakelet.com/wake/RMh2_FibdiNOZpJDAgooq
https://wakelet.com/wake/LpiZlWXnuEbCoCJW3tA1N
https://wakelet.com/wake/10LChyhyNJIBvmXsC4Isn
https://wakelet.com/wake/QmgsaoWT85ZQW8EAY6us6
https://wakelet.com/wake/Br5_cYPyorx7W800_1JhE
https://wakelet.com/wake/Kx5g7ywSD6oUPIOBScH6z
https://wakelet.com/wake/5JMfPg2zDsAHK_YX6zv1Y
https://wakelet.com/wake/nNUjpAK2sXB0wjx_N52wp
https://wakelet.com/wake/YF8A2jTCFMRZj4yNVWk_u
https://wakelet.com/wake/vhoYxaBhWMl58UP3jsJ5i
https://wakelet.com/wake/5jZGvfZu6Ej-jCHCwQ1Z2
https://wakelet.com/wake/o6qsBeWYRZZRYtk2Uccof
https://wakelet.com/wake/DdzdVe6zky9S1qTtnSI5f
https://wakelet.com/wake/-Wh5N4clvv4fj31QWtc7n
https://wakelet.com/wake/FlkPFCZ78pThENbxJhlho
https://wakelet.com/wake/8zY8fP-AukmS4x8Cbg5b9
https://wakelet.com/wake/pBGLFF3rjprj92eD3rjXu
https://wakelet.com/wake/ylPkE8Z13H7MgZQneu9fv
https://wakelet.com/wake/syZFv6k0qRIfYJv8RE8n1
https://wakelet.com/wake/eDddCZG2g6EF_zpsYGUL8
https://wakelet.com/wake/8HmvRQGzYv_YUH7e074b0
https://wakelet.com/wake/3ARGU4pSt3bIav97_EfmY
https://wakelet.com/wake/aDVbGWr4_HJZGhNpPTBEJ
https://wakelet.com/wake/EMyq9WgJBjcSAo2eBOUO9
vinsalar (Friday, 21 January 2022 21:32)
vinsalar a8cc6d31e7 https://coub.com/stories/2824361-the-freezing-of-time-ignzyk
https://coub.com/stories/2824360-dragon-city-hack-no-human-verification-repack
https://coub.com/stories/2824359-new-trap-boom-vst-plugin-free-download-crack
https://coub.com/stories/2824355-free-ecrire-les-chiffre-en-lettre-pdf
https://coub.com/stories/2824358-winrunner-testing-tool-full-version-free-download-exclusive
https://coub.com/stories/2824357-audi-a1-navi-freischalten-vcds-crack-link
https://coub.com/stories/2824356-wysiwyg-cast-software-crack-website-__exclusive__
https://coub.com/stories/2824354-gabriel-weiss-font-free-top
https://coub.com/stories/2824353-saint-seiya-lost-canvas-bdrip-1080p-full-hd-leschr
https://coub.com/stories/2824352-winthruster-license-key-rk0-rsv4znvcb1p1w0slefir3cv827l
https://coub.com/stories/2824350-technical-analysis-of-stocks-and-commodities-magazine-pdf-45-work
https://coub.com/stories/2824351-link-management-consultancy-book-pdf-by-cabrera
https://coub.com/stories/2824349-sherlock-plus-6-6-heidelberg-better
https://coub.com/stories/2824348-req-pro-tools-12-8-1-dmg-for-mac-uliell
https://coub.com/stories/2824347-george-washington-horatio-greenough-ap-art-history
https://coub.com/stories/2824346-link-mindvalley-learn-evolve-and-transform-your-life-v5-12-3
https://coub.com/stories/2824345-full-katya-y111-topless-cstm-2007-06-13-102-pics
https://coub.com/stories/2824344-upd-rowdy-rathore-2-in-hindi-720p-torrent
https://coub.com/stories/2824343-wood-mizer-parts-manual-link
https://coub.com/stories/2824342-download-firefox-lite-v-fast-web-browser-free-games-news-v2-1-10-18757-mod-quafil
https://coub.com/stories/2824341-rrrsrss-beat-maker-telefonbuchios14ok-ipa-link
https://coub.com/stories/2824340-happy-house-1-teacher-s-book-pdf-free-top-download
https://coub.com/stories/2824339-central-angle-and-inscribed-angle-challenge-answers-exclusive
https://coub.com/stories/2824338-mummyeditfantasiarubyrialickinbathroomavi
https://coub.com/stories/2824337-pdf2dtp-for-indesign-cs6-mac-rar-treaisam
https://coub.com/stories/2824336-d-angelo-dinero-smile-original-video-mp4-google-drive-hot
https://coub.com/stories/2824335-tglgcharger-the-witness-v1-unk-64bit-os120-ok13-user-hidden-bfi-ipa
https://coub.com/stories/2824334-tglgcharger-toca-life-vacation-toca-boca-ab-v1-v32334-phone4-univ-os80-ghay-rc336-102-ipa
https://coub.com/stories/2824333-best-us-passport-psd-template-rar
https://coub.com/stories/2824332-rocky-the-rebel-2-tamil-dubbed-movie-free-download-neumich
rawverl (Friday, 21 January 2022 22:04)
rawverl a8cc6d31e7 https://coub.com/stories/2718816-nj-transit-bus-schedule-126-pdf
https://coub.com/stories/2718815-ch37-album-on-imgur-rhierr
https://coub.com/stories/2718814-link-download-rk3328-6255-1228-androidpc-zip
https://coub.com/stories/2718813-husqvarna-61-chainsaw-price
https://coub.com/stories/2718811-stearic-acid-cooling-curve-worksheet-andgio
https://coub.com/stories/2718812-waisi-waali-khushi-2-movie-download-work
https://coub.com/stories/2718810-portable-thermodynamic-gaskell-4th-chapter-13-solutions-zip
https://coub.com/stories/2718809-klimaks-muncrat-3gp-exclusive
https://coub.com/stories/2718808-artcam-2010-sp4-dvd-iso-new-10-09-torrent-sakuphyl
https://coub.com/stories/2718807-jake-heggie-sheet-music-fixed-download
https://coub.com/stories/2718806-ireal-pro-apk-full-version-gotvan
https://coub.com/stories/2718805-download-ebook-free-english-intelligence-link
https://coub.com/stories/2718804-download-new-ets-2-crack-1-4-1
https://coub.com/stories/2718803-warriors-omen-of-the-stars-series-in-order-wontedw
https://coub.com/stories/2718801-lexmark-x5100-windows-xp-driver-download-breemar
https://coub.com/stories/2718802-spotify-music-for-android-tv-v1-9-0-mod-kaijam
https://coub.com/stories/2718800-free-bluford-high-series-pdf
https://coub.com/stories/2718799-free-download-spheroid-icon-2-6-2-patched-dlpure-com
https://coub.com/stories/2718798-guided-train-tours-of-scotland
https://coub.com/stories/2718797-better-eric-bellinger-the-rebirth-2014-full-album
https://coub.com/stories/2718796-north-24-kaatham-malayalam-movie-free-torrent-download-exclusive
https://coub.com/stories/2718795-ib-history-apartheid-notes
https://coub.com/stories/2718794-patched-watch-the-great-ephemeral-skin-online-putlocker
https://coub.com/stories/2718793-avatar-movie-in-1080p
https://coub.com/stories/2718790-shkarko-libra-shqip-falas-pdf
https://coub.com/stories/2718792-vectric-aspire-4-5-crack-top
https://coub.com/stories/2718791-jl-snc-720lat-mkv-ositnar
https://coub.com/stories/2718789-bachche-kachche-sachche-marathi-movie-full-hd-1080-moviles-catalan-marc-slaswah
https://coub.com/stories/2718788-bernina-embroidery-software-7-crack-exclusive-11
https://coub.com/stories/2718787-dumbbell-workout-pdf-jazmas
safigodd (Friday, 21 January 2022 22:35)
safigodd a8cc6d31e7 https://coub.com/stories/2662694-office-365-cracked-for-mac-tempnoel
https://coub.com/stories/2662693-datei-herunterladen-spk_voshod-connexxion-1-100-rar-22-08-mb-in-free-mode-turbobit-ne-_best_
https://coub.com/stories/2662690-devil-girl-2021-s01ep02-nuefliks-original-hindi-web-series-www-9kmovies-photos-720p-hdrip-best
https://coub.com/stories/2662689-exclusive-_pink_floyd_the_final_cut_album_free
https://coub.com/stories/2662688-hot-native-instruments-guitar-rig-v5-1-0-rammfire-reflektor-traktors-keygen
https://coub.com/stories/2662686-portable-reading-comprehension-grade-5-answer-key
https://coub.com/stories/2662685-kelly-rowland-talk-a-good-game-deluxe-edition-2013-zip-mantreni
https://coub.com/stories/2662684-tba-lolita-cheng-set-07
https://coub.com/stories/2662682-hot-dancehall-sound-effects-zip
https://coub.com/stories/2662681-portable-ritchie_blackmore_story_dvd_
https://coub.com/stories/2662680-link-perman-s-large-decision-full-movie-in-italian-free-download-hd-720p
https://coub.com/stories/2662678-n-track-studio-suite-9-x64-v-x86-full-espagol-mega-best
https://coub.com/stories/2662676-fortify-ssc-18-10-user-guide-damyjam
https://coub.com/stories/2662677-pre-algebra-with-pizzazz-career-information-answers-__top__
https://coub.com/stories/2662675-lg-3d-demo-global-1080p-hd-indirl
https://coub.com/stories/2662674-comentario-biblico-mundo-hispano-1-juan-pdf-install
https://coub.com/stories/2662672-trueman-s-elementary-biology-vol-1-pdf-free-download-otthgonz
https://coub.com/stories/2662671-2021-torrent-wondershare-dr-fone-toolkit-for-android-mac-os
https://coub.com/stories/2662669-fsecure_freedome_vpn_2-40-6717-zip-link
https://coub.com/stories/2662663-hot-download-dune-the-duke-caladan-brian-herbert-epub
https://coub.com/stories/2662666-n-track-studio-link-crack
https://coub.com/stories/2662665-free-download-ebook-biokimia-kedokteran-dasar-harysib
https://coub.com/stories/2662664-the-host-2013-dual-audio-hindi-torrent-godpars
https://coub.com/stories/2662662-microeconomics-2nd-edition-goolsbee-pdf-cornlegr
https://coub.com/stories/2662660-half-girlfriend-movie-download-utorrent-new-free
https://coub.com/stories/2662659-polycom-realpresence-desktop-license-crack-epubl-top
https://coub.com/stories/2662658-free-kmsauto_lite_1-3-1
https://coub.com/stories/2662656-food-microbiology-objective-questions-pdf
https://coub.com/stories/2662657-upd-el-amor-en-tiempos-de-colera-espanol
https://coub.com/stories/2662655-new-apush-study-guide
derouldr (Friday, 21 January 2022 23:09)
derouldr a8cc6d31e7 https://wakelet.com/wake/eSPLUBpLBxi9Ab3PWsFs0
https://wakelet.com/wake/m0QykIjkbT0gv2Z4ZsjIK
https://wakelet.com/wake/EOHIWjL7FaWiqvfgSP1kq
https://wakelet.com/wake/XcCH1EdPiQ_UY94Mfhwec
https://wakelet.com/wake/ehd8PcIOu5ABGxoJ1WYLI
https://wakelet.com/wake/7xde-YaIGgpKLQQkI-hX_
https://wakelet.com/wake/nvU5wdzsKSdiLlcGqvN2A
https://wakelet.com/wake/Wsp9MtehQQJFf65a9u9Rp
https://wakelet.com/wake/C8o6wadG0IuoEwmTIWOhe
https://wakelet.com/wake/Cy3SOGB8WM1698Ueeaob7
https://wakelet.com/wake/sq1__zEdOJeYFZolPjLl4
https://wakelet.com/wake/dGYUMDEjdNcaWUyqUeR_X
https://wakelet.com/wake/d8Voq6AslFSfF7Vuav8qh
https://wakelet.com/wake/_u-2UVxQPi1zO20Y6da_q
https://wakelet.com/wake/-8XXHEAwEbjcHsJRwFjdo
https://wakelet.com/wake/fS1odgymbB-9TVtpqIbV-
https://wakelet.com/wake/ISDpDp_Pp2jfEVrfbOkGp
https://wakelet.com/wake/-uRRU4NG4NHV3l20M3KMR
https://wakelet.com/wake/gDcOjvG5qBIzbq1Wrog10
https://wakelet.com/wake/9SFuaOEfhFb-1hWju9rGY
https://wakelet.com/wake/80FvMy6w-YKhV5eIMkhb-
https://wakelet.com/wake/L4Ie5ZYqRj7eXE0o1V_DJ
https://wakelet.com/wake/CrA6D6HkpAXKA9my4LOgN
https://wakelet.com/wake/hFGlM_PfMvsYAc4xGvIlE
https://wakelet.com/wake/DjFmu1aZEwhpz8oWaNZrX
https://wakelet.com/wake/xFk-C98_lK8-M85cvuR-k
https://wakelet.com/wake/Tvehw3ms6xpTn_p5zeaa0
https://wakelet.com/wake/31X-GenU1jk_yzT06Y-92
https://wakelet.com/wake/Wt-roOd6vga2JGzUu1K-r
https://wakelet.com/wake/MViSRPWzE9vUHxo2ZQ0uO
hawlkand (Friday, 21 January 2022 23:41)
hawlkand a8cc6d31e7 https://wakelet.com/wake/xQjyHSy2cLBL7b5vVyGrZ
https://wakelet.com/wake/WIij5V7CKvbbEVvHPsxMb
https://wakelet.com/wake/REz9mtKgyGJdrBC2dsYgI
https://wakelet.com/wake/yIe6ZK2pPqB63eMh6NJq3
https://wakelet.com/wake/yaqoB3D-7G_0ivs5E7Kgv
https://wakelet.com/wake/F7MiMi_30LWrHAq19fXf7
https://wakelet.com/wake/5pC5JMwcUU8vT7sy4WaJM
https://wakelet.com/wake/wlEwat7kwlvMl9PNz6RY1
https://wakelet.com/wake/C3DhfFLRxSMhbPzRC0TXK
https://wakelet.com/wake/IwjT83nxiwoNhFcUuPEVF
https://wakelet.com/wake/cWseCY4evxTw2LFpK1D60
https://wakelet.com/wake/qq4LihhrcRB0KMUjpcm-D
https://wakelet.com/wake/8s86wiLP1X4F_Jcek0lhs
https://wakelet.com/wake/FzqQkReHtki2lYB3KH5xT
https://wakelet.com/wake/q7CxwKkWnXuaddKZzZE07
https://wakelet.com/wake/VZPooxrkyVlD0FLyCFI7O
https://wakelet.com/wake/4vUnbLBUqLB2CpHQixVxq
https://wakelet.com/wake/I2HI4cuHPq1JTXWQjvbXS
https://wakelet.com/wake/eCksc-7ZMspfP7fFanvHO
https://wakelet.com/wake/-tYgfM-3gbD9FFOlFAkU5
https://wakelet.com/wake/VO3nJG2Sriml-f1XD8iiO
https://wakelet.com/wake/o9U2jUhPLxGsOwAFyE2gV
https://wakelet.com/wake/b2yT81tFekvYSu2IYksOx
https://wakelet.com/wake/M6MYs-JFUQU1YapU_r2VI
https://wakelet.com/wake/sqwp-xpnGpIiw62kKA7M9
https://wakelet.com/wake/RVndQp8ZZph_LklUTP8L-
https://wakelet.com/wake/bPsRJUn8fDqG0aZy5wL5X
https://wakelet.com/wake/B95Y_B2jnlvLsm5K6p0bn
https://wakelet.com/wake/m0B_2u0a2JMJ174IkO3-G
https://wakelet.com/wake/9EPYyDqLrFhnNPCGv27s5
kammlati (Saturday, 22 January 2022 01:20)
kammlati a8cc6d31e7 https://coub.com/stories/2752556-howl-s-moving-castle-theme-guitar-tab-pdf-13-abrainno
https://coub.com/stories/2752555-top-which-malm-dressers-are-recalled
https://coub.com/stories/2752554-cracked-stata13freedownloadcrackforwindows
https://coub.com/stories/2752552-work-rus-2017-1
https://coub.com/stories/2752542-apple-has-another-new-cord-updated
https://coub.com/stories/2752537-free-vyzor-g-major-2-editor-for-mac-site-forum-tcelectronic-com
https://coub.com/stories/2752536-broken-sky-pdf
https://coub.com/stories/2752530-yamudu-telugu-full-movie-1080p-hot
https://coub.com/stories/2752527-icd-10-coding-exercises-with-answers-helwend
https://coub.com/stories/2752526-aegisubkaraokeeffectcollection
https://coub.com/stories/2752525-answers-to-aleks-algebra-2
https://coub.com/stories/2752524-ticker-tape-timer-simulation-whytwilv
https://coub.com/stories/2752519-speed-learning-english-torrent-extra-quality
https://coub.com/stories/2752516-updated-figurative-language-worksheets-middle-school-pdf
https://coub.com/stories/2752514-updated-roger-waters-the-wall-dvd-2012-torrent
https://coub.com/stories/2752513-format-date-django-template
https://coub.com/stories/2752509-new-panasonic-sd-jukebox-software
https://coub.com/stories/2752506-missale-romanum-editio-typica-tertia-emendata-pdf-free-updated
https://coub.com/stories/2752487-shaun-of-the-dead-download-bittorrent-updated
https://coub.com/stories/2752496-quite-imposing-plus-3-0-serial-numberkl-bridvas
https://coub.com/stories/2752493-libro-el-color-de-mis-palabras-pdf-dararea
https://coub.com/stories/2752492-_verified_-one-tree-hill-s09e03-direct-download
https://coub.com/stories/2752488-download-lagu-mp3-songs-free-upd-download-for-mobile-website-6-04-mb-mp3-free-upd-download
https://coub.com/stories/2752485-avatar-english-subtitles-1080p-or-1080il
https://coub.com/stories/2752483-repack-new-utility-that-displays-the-files-you-previously-opened-with-the-standard-open-save-dial
https://coub.com/stories/2752476-3d-gamestudio-pro-a7-7-05-with-crack-serial-key-sammar
https://coub.com/stories/2752472-convergent-divergent-and-parallel-evolution-worksheet-work
https://coub.com/stories/2752469-top-usa-today-free-crossword-puzzles
https://coub.com/stories/2752467-gunnjan-paid-pics-google-drive
https://coub.com/stories/2752468-ea-koetting-wikipedia-hot
kammlati (Saturday, 22 January 2022 01:21)
kammlati a8cc6d31e7 https://coub.com/stories/2752556-howl-s-moving-castle-theme-guitar-tab-pdf-13-abrainno
https://coub.com/stories/2752555-top-which-malm-dressers-are-recalled
https://coub.com/stories/2752554-cracked-stata13freedownloadcrackforwindows
https://coub.com/stories/2752552-work-rus-2017-1
https://coub.com/stories/2752542-apple-has-another-new-cord-updated
https://coub.com/stories/2752537-free-vyzor-g-major-2-editor-for-mac-site-forum-tcelectronic-com
https://coub.com/stories/2752536-broken-sky-pdf
https://coub.com/stories/2752530-yamudu-telugu-full-movie-1080p-hot
https://coub.com/stories/2752527-icd-10-coding-exercises-with-answers-helwend
https://coub.com/stories/2752526-aegisubkaraokeeffectcollection
https://coub.com/stories/2752525-answers-to-aleks-algebra-2
https://coub.com/stories/2752524-ticker-tape-timer-simulation-whytwilv
https://coub.com/stories/2752519-speed-learning-english-torrent-extra-quality
https://coub.com/stories/2752516-updated-figurative-language-worksheets-middle-school-pdf
https://coub.com/stories/2752514-updated-roger-waters-the-wall-dvd-2012-torrent
https://coub.com/stories/2752513-format-date-django-template
https://coub.com/stories/2752509-new-panasonic-sd-jukebox-software
https://coub.com/stories/2752506-missale-romanum-editio-typica-tertia-emendata-pdf-free-updated
https://coub.com/stories/2752487-shaun-of-the-dead-download-bittorrent-updated
https://coub.com/stories/2752496-quite-imposing-plus-3-0-serial-numberkl-bridvas
https://coub.com/stories/2752493-libro-el-color-de-mis-palabras-pdf-dararea
https://coub.com/stories/2752492-_verified_-one-tree-hill-s09e03-direct-download
https://coub.com/stories/2752488-download-lagu-mp3-songs-free-upd-download-for-mobile-website-6-04-mb-mp3-free-upd-download
https://coub.com/stories/2752485-avatar-english-subtitles-1080p-or-1080il
https://coub.com/stories/2752483-repack-new-utility-that-displays-the-files-you-previously-opened-with-the-standard-open-save-dial
https://coub.com/stories/2752476-3d-gamestudio-pro-a7-7-05-with-crack-serial-key-sammar
https://coub.com/stories/2752472-convergent-divergent-and-parallel-evolution-worksheet-work
https://coub.com/stories/2752469-top-usa-today-free-crossword-puzzles
https://coub.com/stories/2752467-gunnjan-paid-pics-google-drive
https://coub.com/stories/2752468-ea-koetting-wikipedia-hot
elfneth (Saturday, 22 January 2022 01:53)
elfneth a8cc6d31e7 https://coub.com/stories/2633779-5-online-webm-to-gif-converter-websites-free-free
https://coub.com/stories/2632615-better-pink-full-movie-download-in-hindi-hd-1080p
https://coub.com/stories/2632614-ps3-emulator-bios-download-new-zip
https://coub.com/stories/2632612-young-life-campaigner-outlines
https://coub.com/stories/2632613-mario-kart-tour-cheats-characters-new
https://coub.com/stories/2632611-datei-herunterladen-cdkada-rar-37-62-mb-in-free-mode-turbobit-net-kalgauv
https://coub.com/stories/2632608-types-of-respiratory-hot-crackles
https://coub.com/stories/2632610-augusta-national-course-map-pdf-portable
https://coub.com/stories/2632609-technical-drawing-with-engineering-graphics-14th-edition-pdf-download-disfei
https://coub.com/stories/2632607-verified-coordinate-plane-picture-worksheet-pdf
https://coub.com/stories/2632606-__top__-modern-physics-2nd-randy-harris-solutions
https://coub.com/stories/2632605-terraform-aws_iam_policy-resource-extra-quality
https://coub.com/stories/2632598-buena-vista-social-club-torrent-kickass-genres-exclusive
https://coub.com/stories/2632604-minecraft-windows-10-free-work-download-cracked
https://coub.com/stories/2632603-rus-cyberduck-6-8
https://coub.com/stories/2632602-whmis-test-answers-2021
https://coub.com/stories/2632601-work-d2_the_mighty_ducks_mp4
https://coub.com/stories/2632600-_snooker_game_free-better-_for_mac
https://coub.com/stories/2632599-link-crack-icopybot-7-5-19
https://coub.com/stories/2632597-list-of-turkish-verbs-pdf-12
https://coub.com/stories/2632595-northman-snow-plow-manual
https://coub.com/stories/2632596-parodie-paradise-v2-naruto-xxx-3-eldlav
https://coub.com/stories/2632594-the-sims-2-nightlife-serial-key-updated
https://coub.com/stories/2632593-clarir12345-rar-google-drive-weswell
https://coub.com/stories/2632590-work-deezer-premium-mod-apk-unlocked-latest-2021
https://coub.com/stories/2632592-dlupload-rangerunner-apk-winilean
https://coub.com/stories/2632591-minecraft-beta-house-download-natimmo
https://coub.com/stories/2632589-exclusive-avira-phantom-vpn-pro-2-29-2-24183-crack
https://coub.com/stories/2632588-download-nvivo-10-for-mac-latafynn
https://coub.com/stories/2632586-air-brake-test-questions-answers-ontario
adeesb (Saturday, 22 January 2022 02:26)
adeesb a8cc6d31e7 https://wakelet.com/wake/XaEhGSqlFv2dlX0cJujib
https://wakelet.com/wake/H5h6wgMw5rIr8laZ2ni8m
https://wakelet.com/wake/p1qf9eUF8BeujJuc0mrA_
https://wakelet.com/wake/Y0B2qaSD0q_8cp0AyfZmS
https://wakelet.com/wake/nFPT1vvYQJg4qmkhy8Nzo
https://wakelet.com/wake/N508xrTZHsOmkQTSF3G91
https://wakelet.com/wake/ZNx03KiVrESU38jWZGiSk
https://wakelet.com/wake/UfLW_b35LVPeocLi9WRHk
https://wakelet.com/wake/pkF3CyGlivlKEqwFyTcb0
https://wakelet.com/wake/Wuymwj7H5RYsmHfYLa816
https://wakelet.com/wake/CiemzDp011Q46ldLD2r-W
https://wakelet.com/wake/DXQGHP2Vbz6VnA4aajPRc
https://wakelet.com/wake/byZyZpkIPNLh53V-k2xiN
https://wakelet.com/wake/kTb5QdFicnkZ-M2Nqvn-P
https://wakelet.com/wake/_eAdITrvoh2qLDgzPJTHc
https://wakelet.com/wake/QR_0u6_4ySwcDjXBORieg
https://wakelet.com/wake/tu2HVcK2sPozI3n0Io5p7
https://wakelet.com/wake/5_x0GuwkCyqzgQx4rM5lK
https://wakelet.com/wake/xztLMQPxAwt7uLu9qFWAP
https://wakelet.com/wake/u9IyTcZ_cAIs5y3Tydcdb
https://wakelet.com/wake/FLmRk5EuTQoiw2W3-UOqC
https://wakelet.com/wake/DUAsDpVIhZc8hwQrlkudB
https://wakelet.com/wake/EF4D5fgoMmM4BtTb50QPq
https://wakelet.com/wake/BkiS3FCYnT0nyAZYhunNm
https://wakelet.com/wake/2ELDY3OSMD_LIWcZ7bRSB
https://wakelet.com/wake/7NaQ2UmwDFVC2a_x_B0it
https://wakelet.com/wake/pDpVXa5okumC6zcEsu-pZ
https://wakelet.com/wake/CvYe7L8XMU9rR8PLl_cii
https://wakelet.com/wake/eTy4zjH9xvvmgctJSUVKM
https://wakelet.com/wake/9A2ESetlabsve6CTCdDF9
sweneo (Saturday, 22 January 2022 12:18)
sweneo a8cc6d31e7 https://wakelet.com/wake/C7I6g1Qob1q6mwpU2-lJA
https://wakelet.com/wake/AHSnpd5Mw6hmuFDxopSeJ
https://wakelet.com/wake/6LB8JeWVyRgcHbWryHd_F
https://wakelet.com/wake/GoQEZyHNU3xI_CjQFiSck
https://wakelet.com/wake/KojxI572uURNmiSD3Bx5r
https://wakelet.com/wake/qkaXEWU8FUZS8fmLHw7u8
https://wakelet.com/wake/wyWCNMQnLeogC8Gx98tDf
https://wakelet.com/wake/xvoB2X89-06Zxk7r6_FeI
https://wakelet.com/wake/pTzL-dAl58GpNJCbhh930
https://wakelet.com/wake/1AO7N0nPpraoQveQHU8aw
https://wakelet.com/wake/oBSd2WIFlHi_kRUy39tGt
https://wakelet.com/wake/JsLUM6aBsoVyNHHSDI0O6
https://wakelet.com/wake/fRP81fvTdZiHX2WoENur6
https://wakelet.com/wake/qcARAXQyqGH96RmqnifVU
https://wakelet.com/wake/u8FhKqGIuKqpSuIXHt9Go
https://wakelet.com/wake/1p1ejL5xS-Z8r9WsEkVY8
https://wakelet.com/wake/xHFbjN0OzTUD1JnnJIT5A
https://wakelet.com/wake/4QenEjhbexCNGgf2pkGKw
https://wakelet.com/wake/DEhryDs7YcV7zgkBcYVGq
https://wakelet.com/wake/Aa7fNPyIhUxDKYMca9ns3
https://wakelet.com/wake/cFU1xcHqyLfP9bCVHhn1f
https://wakelet.com/wake/gDCeup-AbVi_9RXtn69el
https://wakelet.com/wake/uO-aqcE-tyQ0CsZlKs3jw
https://wakelet.com/wake/k3-8Id_ARMYQytxPWK1hi
https://wakelet.com/wake/dHSwhIFQ-0ABnekGavR_r
https://wakelet.com/wake/tGmBrgi_-SbUw-kSB-FmH
https://wakelet.com/wake/lroXbiJwXeZoRsAHlS_Gr
https://wakelet.com/wake/juk_uq4ljg9QwOJ5VOsZf
https://wakelet.com/wake/rLGm_ZYUku59EQmfHTabg
https://wakelet.com/wake/vAAOqHWMWvlZMmfISBKnW
pasbain (Sunday, 23 January 2022 14:54)
pasbain 7383628160 https://wakelet.com/wake/FuS-tQDQlfTAWUEFA01La
https://wakelet.com/wake/l1VJNiBOWgUPR2ZD-NQRe
https://wakelet.com/wake/z3B2XAjHmUocrCQ18_YBH
https://wakelet.com/wake/jkzFYIsNwnIkVO-QsXE5D
https://wakelet.com/wake/DRzSTY_HFLSJWyGQkrI_1
https://wakelet.com/wake/Nvgxf5gpCLe9IVisvVjji
https://wakelet.com/wake/2tVTMFrduD5375ZklArXC
https://wakelet.com/wake/J-dKulBBPyHUrggrWCqUY
https://wakelet.com/wake/0Mi-f1Xg0Atqv-yI76f87
https://wakelet.com/wake/XppZ09L1PgFzwlbD6L6iU
https://wakelet.com/wake/nXXMzs1xIFn_a5I5vsrfm
https://wakelet.com/wake/PUjYvXcuf4rZ8WejSZYQH
https://wakelet.com/wake/a9pEsX0ndXc5G0ECFOtAy
https://wakelet.com/wake/H2_nwnfb4QEPAqMbwUh6Y
https://wakelet.com/wake/bgDBGHh62TUynZCYLfQIz
https://wakelet.com/wake/7v22xxNS8Lxa7312GiN2W
https://wakelet.com/wake/P7ko-saZr2Z-vYqmv6Rvh
https://wakelet.com/wake/bicj_XMx_Qo0gglqj2Hqg
https://wakelet.com/wake/pU9hR87ygLt-3sUufV4CA
https://wakelet.com/wake/RTbludXNz12lV9g3Co-PL
https://wakelet.com/wake/8AJGpmOB4QAIZ9yCAVU_I
https://wakelet.com/wake/eP93z-x1SqUublGC5hUeR
https://wakelet.com/wake/AMEXCvHzLBQn-p3j6ZKAa
https://wakelet.com/wake/YRyP0u-Dp4O53CC8NyIPS
https://wakelet.com/wake/erPcKKdlMMVFAgSF7YGvq
https://wakelet.com/wake/KmD8ZR_NqBl7ECmqChQkv
https://wakelet.com/wake/k9wv9-lqNN3m8zVpig2DQ
https://wakelet.com/wake/7F744ogy2JnlrZ7pYtgsf
https://wakelet.com/wake/1Gj-KU8fLNtv4byIa2bu0
https://wakelet.com/wake/j4y8LsSwPYdfGAFYnxsei
nadyhid (Sunday, 23 January 2022 15:21)
nadyhid 7383628160 https://wakelet.com/wake/JyxnfXOUs9Yfzewh8Nmn2
https://wakelet.com/wake/KQG_WrkhtFgCEXd5h71gQ
https://wakelet.com/wake/kSjAAHx0EuMOTUURx6JuK
https://wakelet.com/wake/KmIUh6LayVMtbe8jf_8ay
https://wakelet.com/wake/HAgdntAPgy8cnNDU-ZsH5
https://wakelet.com/wake/IcV55-dI-VKVg5lbSPl0v
https://wakelet.com/wake/2lMchFTyfJyu4mEOZUZhU
https://wakelet.com/wake/VgFBCcCXj9Wa6P7FIxuta
https://wakelet.com/wake/KXwWS2DWXgS4qemsRnqkj
https://wakelet.com/wake/SLGmABP5ZDm6y0Vpjeh1m
https://wakelet.com/wake/e8w9LfX4Udq0E_FaInOci
https://wakelet.com/wake/EoJP28IrxeXEWJYNMytvm
https://wakelet.com/wake/xW5ZC8gZGF6lL4sH0CM3n
https://wakelet.com/wake/HmHtjOBl7tO13ZxVRYwXn
https://wakelet.com/wake/2PuA9xIL4qxLd3zbZ4InG
https://wakelet.com/wake/fgE6HCZjcWbWpOXoVRO8S
https://wakelet.com/wake/Oe_-KPtLJuEUOR_01Olia
https://wakelet.com/wake/POblT7JwoclFzQ2ovyUtH
https://wakelet.com/wake/GcCwIC3UsnWJ-GXoVvc2P
https://wakelet.com/wake/h1IHw82zwUqgpcyYYxOBt
https://wakelet.com/wake/OGhKf_zPXMG-F_CQJqFiQ
https://wakelet.com/wake/lTUQU27545t9gNWe06BWX
https://wakelet.com/wake/Y0xAEz7ntFadSA-kPkw89
https://wakelet.com/wake/ovg_F-AVl44_swunHPNKG
https://wakelet.com/wake/Fot9JohAQ7n9veMMUtFsi
https://wakelet.com/wake/WazSj3wHQq1wOKTimotFe
https://wakelet.com/wake/2H4ms9FAarjV5BwX8CiIn
https://wakelet.com/wake/IVdO_h9aZfaDFnJtJ4zbU
https://wakelet.com/wake/BZ_hfBALCaDNADZhxylzQ
https://wakelet.com/wake/I0v6HmMk_Ab9Qxfs9WkXY
tarcberi (Sunday, 23 January 2022 15:48)
tarcberi 7383628160 https://trello.com/c/eFswlqgb/37-wondershare-allmytube-4805-key-4realtorrentz-rar-mygnbro
https://trello.com/c/WSB5tdRl/32-cracked-acte-necesare-eliberare-certificat-fiscal-sector-6
https://trello.com/c/mKHmVzNT/33-photo-stamp-remover-110-crack-with-key-full-version-birpat
https://trello.com/c/jaNgM33I/33-project-nightmares-case-36-henrietta-kedward-cheat-code-for-pc-top
https://trello.com/c/X1v08XU1/32-exclusive-crack-sex-simulator-2018-hot-ggg
https://trello.com/c/QJAJaOkF/28-cod4-crack-1-7-iw3mp-exe-free
https://trello.com/c/YBzYAa4j/58-guide-des-metiers-de-l-electrotechnique-v219-best
https://trello.com/c/6fyLlq87/27-cringer-990-artwork-updated
https://trello.com/c/LO281JE6/11-lollipop-chainsaw-pc-download-exclusive-crack-software
https://trello.com/c/sRRqnGCA/38-dance-dance-revolution-3rd-mix-iso-torrent
https://trello.com/c/cBLbDjAk/45-top-chivalry-deadliest-warrior-key-serial-number
https://trello.com/c/zugXfxtC/40-sketchuppro20171722555cracksadeempcfreedownload-adones
https://trello.com/c/ESGfaMMB/44-install-command-and-conquer-3-tiberium-wars-no-cd-crack-v10
https://trello.com/c/sgBM6blx/31-fixed-ogc-aimbot-download-19
https://trello.com/c/P1CLqJGo/9-devils-hunt-torrent-download-extra-quality-key
https://trello.com/c/kdEYWdWt/25-nba-2k15-pc-download-verified-crack
https://trello.com/c/jwTEHCrM/23-beatport-exclusive-downloader-boot-ver-13rar
https://trello.com/c/3253rsTH/26-install-asoka-hindi-720p-dvdrip-torrent
https://trello.com/c/Gi0uCEEh/11-quickmastro-crack-cracked
https://trello.com/c/lB5InWrh/71-hot-obs-studio-240-crack-download-here
https://trello.com/c/1hGrnR2w/37-hot-imagenomics-photoshop-plugins-keygen
https://trello.com/c/SnPk2NJL/28-the-pinball-arcade-v1438-dx9-dx11-viper666-hack-torrent-upd
https://trello.com/c/jpuOrXwv/41-exclusive-download-modelsim-full-crack-internet
https://trello.com/c/ILgCMDMl/40-company-of-heroes-new-steam-version-v27000-antdavo
https://trello.com/c/WOyZwpQb/34-colaj-muzica-de-petrecere-download-zippy-share-vorschau-spaywar-opp-link
https://trello.com/c/PnAabkCC/60-free-microsoft-windows-xp-tablet-pc-edition-2005-20-quygine
https://trello.com/c/nARcwhCe/28-auto-tune-7-ilok-portable-crackexe-download-musictrmdsf
https://trello.com/c/NOtjTTYC/81-nero-7012-ita-crack-exclusive
https://trello.com/c/WL8QnXPW/26-exclusive-free-download-wbs-chart-pro-47-full-version
https://trello.com/c/ipjStlxD/18-upd-full-active-file-recovery-904-crack-ec
vasnys (Sunday, 23 January 2022 16:08)
vasnys 7383628160 https://trello.com/c/YmhdFUgx/27-keygen-adobe-photoshop-cs2-paradox-verbnen
https://trello.com/c/L2o0fSzU/60-king-kong-2005-blu-ray-torrent-better
https://trello.com/c/A9GIMpzb/60-assassins-creed-origins-fitgirl-repack-top
https://trello.com/c/MDtD9w2B/39-3d-lut-creator-pro-crack-full-zip
https://trello.com/c/SkEFHm20/29-office-2010-toolkit-223-free-11-saftanu
https://trello.com/c/ImuMHQQk/42-ps3eye-camera-setup-v3000901exe-best
https://trello.com/c/cU4469Bw/44-omnisphere-2-crack-r2r-49-jammkaf
https://trello.com/c/OOPrXqE0/69-zywall-ipsec-vpn-client-serial-number-fix
https://trello.com/c/P6yidzXh/88-top-cabri-3d-v2-212-keygen
https://trello.com/c/fpNrz5Vc/41-best-ringkasan-materi-ipa-kelas-1-sd-semester-1
https://trello.com/c/U4kmn4nN/22-descargar-aritmetica-de-repetto-tomo-1zip-better
https://trello.com/c/oZI9vhGQ/41-teracopy-pro-v308-lakshannv-serial-key-keygen-ruslach
https://trello.com/c/61lIhnhJ/48-top-download-desain-sampul-buku-cdr-17
https://trello.com/c/8Hb1f4k1/87-better-driver-webcam-tsinghua-tongfangrar
https://trello.com/c/dYYQo7YN/22-pro-atc-x-torrent-fatijar
https://trello.com/c/UhKhdewH/22-supply-chain-management-chopra-test-15-dartat
https://trello.com/c/9arYYM2T/74-gta-namaste-america-game-link-free-676
https://trello.com/c/MBx2YN34/37-paul-simon-graceland-full-new-album-zip
https://trello.com/c/uqJRd82X/44-race-07-the-official-wtcc-game-crack-files-estpal
https://trello.com/c/34PRhO1A/53-link-download-buku-atlas-wali-songo-487
https://trello.com/c/v9ipcks1/33-shadow-fight-2-v1926-android-para-hile-mod-apk-top
https://trello.com/c/3hECYUq2/46-link-the-gun-pe-done-hindi-dubbed-movie-hd-download-torrent
https://trello.com/c/3RTYgyfV/26-magic-inlay-game-download-free-full-version-portable
https://trello.com/c/jRRBMwd9/60-top-hd-online-player-prince-of-egypt-1080p-tpb-torrent
https://trello.com/c/2cDUGqRG/30-xforce-exclusive-keygen-autocad-map-3d-2013-exclusive-keygen
https://trello.com/c/WzHxgV8A/32-tamil-typing-practice-book-free-download-work
https://trello.com/c/FZDwY4rT/83-patch-crysis-3-traduzione-in-italiano
https://trello.com/c/ODfP5uR9/25-airbusa320cbtrar-lennar
https://trello.com/c/4zcyP4pM/39-hitachi-hl-dt-st-dvdram-gt30n-firmware-update
https://trello.com/c/MotFzPaj/20-webreccab-download-install-wonncai
nerbry (Sunday, 23 January 2022 16:25)
nerbry 7383628160 https://coub.com/stories/2961352-38-special-handgun-serial-number-091285-16
https://coub.com/stories/2961351-radiohead-ok-computer-full-album-zip-top
https://coub.com/stories/2961350-symphony-r30-flash-file-mt6580-hw1-hw2-customer-care-file-da-fix-makgol
https://coub.com/stories/2961347-yodot-file-recovery-full-version-crack-hot
https://coub.com/stories/2961348-puthiya-thalaimurai-kalvi-book-free-download-new
https://coub.com/stories/2961349-tmpgenc-authoring-works-5-japanese-keygen-exclusive-214
https://coub.com/stories/2961345-ruby-sparks-libro-pdf-26-exclusive
https://coub.com/stories/2961344-fix-crack-one-click-privacy-v2-2-5-winall-cracked-czw
https://coub.com/stories/2961342-scf-power-toolbar-sketchup-download-crackl-hot
https://coub.com/stories/2961341-hacker-para-curtidas-em-fotos-no-facebook-hot
https://coub.com/stories/2961340-__hot__-house-flipper-beta-license-key
https://coub.com/stories/2961339-robert-lowie-historia-de-la-etnologia-pdf-download-hot
https://coub.com/stories/2961338-portable-cadmas-11-torrent-full-version-added-by-users
https://coub.com/stories/2961336-selteco-alligator-flash-designer-8-0-24-serial-ellahan
https://coub.com/stories/2961323-samsung-daseull-kamger
https://coub.com/stories/2961333-link-abcd-any-body-can-dance-2-in-hindi-full-movie-download-hd
https://coub.com/stories/2961335-3d-organon-anatomy-torrent-download-_hot_-hacked
https://coub.com/stories/2961330-folder-lock-7-serial-key-full-version-karegee
https://coub.com/stories/2961331-idm-crack-6-33-build-3-new
https://coub.com/stories/2961329-best-headus-uv-layout-v2-keygen-torrent
https://coub.com/stories/2961328-download-simplecast-v3-1-0-full-patch-link
https://coub.com/stories/2961327-bosch-esi-tronic-codice-abilitazione-crack-serial-leofmar
https://coub.com/stories/2961325-wintopo-pro-license-keygen-torrent-helels
https://coub.com/stories/2961326-directtaxlawstnmanoharanpdfdownload-verified
https://coub.com/stories/2961322-corel-paintshop-pro-2019-ultimate-21-2-0-22-keygen-rar-exclusive
https://coub.com/stories/2961321-facegen-model-ler-3-1-upd-keygen-torrentl
https://coub.com/stories/2961320-full-ontrack-disk-manager-957-boot-isozip
https://coub.com/stories/2961315-new-ncstudiov5453englishsetup
https://coub.com/stories/2961317-mirai-stage-1-coursebook-japanese-edition-books-pdf-file
https://coub.com/stories/2961316-shape-collage-2-1-download-work-free
nilavygn (Sunday, 23 January 2022 16:41)
nilavygn 7383628160 https://coub.com/stories/3052119-cutting-optimization-pro-5-7-8-11-crack-top
https://coub.com/stories/3052118-ekonomi-pembangunan-todaro-pdf-download-alaflo
https://coub.com/stories/3052117-repack-soulset-free-download-pack
https://coub.com/stories/3052116-battlefield-2142-v1-5-no-cd-crack-amamar
https://coub.com/stories/3052114-_best_-cadence-allegro-16-6-crack-licence
https://coub.com/stories/3052112-miracle-cell-no-7-tagalog-version-full-20-deroana
https://coub.com/stories/3052113-play-along-downloads-torrent-better
https://coub.com/stories/3052111-nfs-underground-2-nfs-most-wanted-rip-pc-fitgirl-repack
https://coub.com/stories/3052109-better-365frasesdeamorpdfdownload
https://coub.com/stories/3052110-brideforrentfullmoviedownloadmp4-2021
https://coub.com/stories/3052105-hot-musafir-movie-1080p-download
https://coub.com/stories/3052108-free-ezdrummer-2-win-crack-free-download
https://coub.com/stories/3052107-updated-pir-naseer-ud-din-naseer-bayan-mp3-free-download
https://coub.com/stories/3052106-jcpds-card-software-free-download-__hot__
https://coub.com/stories/3052103-link-lounge-lizard-ep4-keygen-macinstmank42
https://coub.com/stories/3052104-copilotlivepremiumeuropeupd-cracked23
https://coub.com/stories/3052101-flippednormals-mouths-40-zbrush-vdms-5-bonus-variations
https://coub.com/stories/3052100-netcad-5-2-full-indir-gezginler-birtwar
https://coub.com/stories/3052099-tumhari-sulu-movie-1080p-free-portable-download
https://coub.com/stories/3052098-va-classic-mellow-mastercuts-vol-1-3-1991-1994-nelslayd
https://coub.com/stories/3052096-wondershare-win-suite-2012-121-javpypi
https://coub.com/stories/3052095-hd-online-player-13b-movie-download-top-in-mp4-videos
https://coub.com/stories/3052091-universal-gb-root-v25-zip
https://coub.com/stories/3052093-hiren-boot-cd-15-3-iso-free-link-download
https://coub.com/stories/3052092-tamil-hd-video-songs-top-download-1080p-movie
https://coub.com/stories/3052089-age-of-empires-ii-hd-the-forgotten-reloaded-game-hack-password-top
https://coub.com/stories/3052087-verified-crack-no-cd-les-sims-3-ile-de-reve
https://coub.com/stories/3052085-rescue-dawn-dual-audio-hindi-free-downloaddcinst-better
https://coub.com/stories/3052086-windows-7-pt-pt-free-download-exclusive
https://coub.com/stories/3052084-fix-infraworks-2013-x64-torrent
kafper (Sunday, 23 January 2022 17:32)
kafper 7383628160 https://wakelet.com/wake/H2BesWjZWd29DE2XofCYr
https://wakelet.com/wake/Qnw7dqoq7MP3iOcKozTDa
https://wakelet.com/wake/_W3b2ai0L8jJnGpXJ0LGY
https://wakelet.com/wake/-zB-4xsFysTNNmKTIGwAp
https://wakelet.com/wake/UW1FdmBhbyVC4B4pgaM9m
https://wakelet.com/wake/kE--rlONmwjTJln44yPti
https://wakelet.com/wake/pgnw5LvVr_3RBcYHHYmJd
https://wakelet.com/wake/LlBe4_YHz1o1jIgYL3t6q
https://wakelet.com/wake/3tuoNqMHyHAVwLcwp54yp
https://wakelet.com/wake/fD3qdfLFz57zlPwMmtYPN
https://wakelet.com/wake/3rPcaEtdECa8jqMnAEH7u
https://wakelet.com/wake/ntEnpOSpR5oosQmaUc6EC
https://wakelet.com/wake/fqjPgR5HFNrPS5ExiSJRi
https://wakelet.com/wake/9X21xEGhcxZXo9pjJmVYI
https://wakelet.com/wake/U29_AQ76uQjcH4XdN-MFJ
https://wakelet.com/wake/OVxPYMp5Lf2Z8hNyxxvnq
https://wakelet.com/wake/7PV0hxeQ6DH8-8svQpc6U
https://wakelet.com/wake/UQhLazhEVafux57j9-2b3
https://wakelet.com/wake/662D44FTsiM-qVtj7-qcW
https://wakelet.com/wake/syOTE5WjR6AcFjI3p2o_V
https://wakelet.com/wake/iRIRQjbRMUyaXkVoLdKvn
https://wakelet.com/wake/bvpWeAm1L3O3OqvL7yWPh
https://wakelet.com/wake/e2anMXizCnI7T_hcWgIwT
https://wakelet.com/wake/aXzLb01YxtFIXDnA6biBk
https://wakelet.com/wake/qoqoY9DUq7bvBC_VbDdX1
https://wakelet.com/wake/4HNlhmygIPxpK2DDRsD18
https://wakelet.com/wake/hxD_7TiPsRelm_bHrBYWR
https://wakelet.com/wake/Y4YP_letd-hwZ9UhBu1Iw
https://wakelet.com/wake/1_dcIR0XvQyJdfKrnHgS_
https://wakelet.com/wake/nhkP2E_vejyPy_3hwXczX
propgavr (Sunday, 23 January 2022 17:49)
propgavr 7383628160 https://trello.com/c/JIhUtLxy/28-700-flash-games-in-one-filerar-download-link
https://trello.com/c/ucKsIkHg/24-cem-due-mig-welder-manual
https://trello.com/c/T4GSpwpx/37-sketchup-3skengrar
https://trello.com/c/sy7xxFPj/17-top-comfort-keys-pro-910-crack-full
https://trello.com/c/A3tETemI/12-repack-gearexpert-51-full-version
https://trello.com/c/JAetgu85/80-hot-telechargerjeuxpspgratuitresidentevil4pspiso
https://trello.com/c/KtjMTObR/42-trendyflash-site-builder-licensed-by-gncooldudrar-serial-key-keygen-growdeb
https://trello.com/c/6DxDx9rh/85-how-to-activate-microsoft-office-2013-professional-plus-crack-exclusive
https://trello.com/c/TvIxHRoN/39-upd-longtion-autorun-pro-enterprise-keygen-crack-free-download
https://trello.com/c/NDkPzdGJ/28-eric-prydz-opus-2016-crack-best
https://trello.com/c/2Mus8l2Q/75-filemaker-pro-12-advanced-crack-28-verified
https://trello.com/c/YfYCn3oe/27-top-codigo-producto-sims-4-origin-1245
https://trello.com/c/vcUSjqin/23-updated-dgs-ramsete-iii-v905-lndrar31
https://trello.com/c/ckKuIvHw/49-fix-rolling-line-free-download-key-serial-number
https://trello.com/c/cqQspKK5/79-verified-patched-ccleaner-professional-6436326-slim-keygen-crack
https://trello.com/c/jd6zJqVm/43-discovery-channel-guia-de-supervivencia-8-pandemia-new
https://trello.com/c/PtL4ChY2/58-insidious-chapter-3-full-patched-movie-in-hindi-dubbed-download-ituness
https://trello.com/c/8nGD9wst/27-portal-2-cracked-download-better-pc
https://trello.com/c/lmuU2bWe/23-clip-studio-paint-ex-193-crack-with-activation-code-free-download-2019-2021
https://trello.com/c/ib3ErEcD/42-pdf-the-estill-voice-model-theory-and-translation-install
https://trello.com/c/Y0tepWjO/49-better-videocad-8-professional
https://trello.com/c/an4181Sk/33-mercedes-benz-vito-w638-wiring-diagram
https://trello.com/c/nvt3WoNg/67-free-screen-video-recorder-3048703-premium-serial-key-keygen-best
https://trello.com/c/aH7RRmbE/23-tec-it-barcode-studio-top-cracked
https://trello.com/c/jNiOkxkX/34-link-rc415t-am-manual
https://trello.com/c/6kR3ODEB/37-navionicscaribbeanandroidverified-crackedapk
https://trello.com/c/zQmcSTJs/32-underworld-awakening-dual-audio-1080p-hdtv
https://trello.com/c/8OY7pzKA/29-hot-cycorefx-hd-171-crack-cs4
https://trello.com/c/maViKThO/35-words-their-way-letter-name-alphabetic-sorts-pdf-fixed-download
https://trello.com/c/0UCYHWeP/25-best-gezginler-solidworks-2008-full-indir
javogard (Sunday, 23 January 2022 18:06)
javogard 7383628160 https://coub.com/stories/3008337-lost-treasure-of-el-dorado-game-for-pc-extra-quality-full-version
https://coub.com/stories/3008336-top-sonic-unleashed-free-download-for-android
https://coub.com/stories/3008324-krypton-suite-license-key-missjami
https://coub.com/stories/3008333-triptofanito-en-la-celula-libro-completo-pdf-27-scobre
https://coub.com/stories/3008331-how-activate-1001bit-pro-crack-install
https://coub.com/stories/3008330-on1-photo-raw-2020-v14-0-1-8289-crack-top-free-download
https://coub.com/stories/3008327-portable-poto-bugil-andrea-dian
https://coub.com/stories/3008325-download-_best_-virtually-jenna-v25-mod-latest-version
https://coub.com/stories/3008323-_hot_-red-alert-3-english-language-pack-rar
https://coub.com/stories/3008322-hd-online-player-yashwant-full-movie-hd-1080p-downloa-work
https://coub.com/stories/3008320-download-ebook-gajah-mada-madakaripura-hamukti-moksa-darcopp
https://coub.com/stories/3008319-chic-discography-1977-2013-256-320-kbps-disco-dance-funk-r-__exclusive__
https://coub.com/stories/3008318-verified-after-effects-projects-big-pack-no-3
https://coub.com/stories/3008312-__top__-dum-laga-ke-haisha-1-movie-download-utorrent
https://coub.com/stories/3008309-materi-ekonomi-bisnis-kelas-10-smk-k13
https://coub.com/stories/3008304-behen-hogi-teri-1080p-movie-torrent-exclusive
https://coub.com/stories/3008310-refox-xii-12-1-exe-crack-keygen-zip-shareaza-librerie-ri-phybri
https://coub.com/stories/3008307-new-marykkundoru-kunjadu-malayalam-movie-bittorrent-download-sites
https://coub.com/stories/3008308-updated-warren-g-i-want-it-all-full-album-rar
https://coub.com/stories/3008306-varusa-nattu-zameen-kathai-in-pdf
https://coub.com/stories/3008303-link-prog-rock-magazine-pdf-44
https://coub.com/stories/3008302-sans-10108-the-classification-of-hazardous-locations-and-the-pdf-jamgirr
https://coub.com/stories/3008301-easy-recovery-essentials-easyre-pro-windows-xp-vista-10-full-version-work
https://coub.com/stories/3008299-hd-online-player-ungli-full-movie-in-hd-1080p-downloa-kafgab
https://coub.com/stories/3008298-2021-downloadmidigratiskoplosagita
https://coub.com/stories/3008296-revit-2009-keygen-xforce-rar-free-download-magearv
https://coub.com/stories/3008289-best-full-adobe-photoshop-lightroom-cc-6-10-1-portable-cracked
https://coub.com/stories/3008291-princess-srirasmi-nude-pictures-ziptrmdsf-ulanmarq
https://coub.com/stories/3008288-fable-3-crack-high-quality-no-dvd-drive-detected
https://coub.com/stories/3008285-throne-of-glass-book-1-pdf-download-2021
delmtail (Sunday, 23 January 2022 18:40)
delmtail 7383628160 https://wakelet.com/wake/KxvaLHSWYKleHF2D-U1zS
https://wakelet.com/wake/aJjZR1hsJAWC0NXXy5fTj
https://wakelet.com/wake/5SaAcYEqox4rM9d2oP4jq
https://wakelet.com/wake/CGV6HDMduh-9eUnfeQnes
https://wakelet.com/wake/B47LjPPD7ZwWcRCFp_tGt
https://wakelet.com/wake/TEex4QGMq5q7bfjo6rKFD
https://wakelet.com/wake/vnt7BDJxv2xHQz0A5vEa3
https://wakelet.com/wake/BPN-bQ150NM_TyHLbDwW-
https://wakelet.com/wake/8cJpYyXX0EIkTIcP7uYtE
https://wakelet.com/wake/k43sX_j6n_wzBSHLDXZ1x
https://wakelet.com/wake/ai1gnSgV9sniGovkQMzR2
https://wakelet.com/wake/zqjnK0_pOFYrNnHGl_hZv
https://wakelet.com/wake/cYJd38EIMtR592JBm8JBH
https://wakelet.com/wake/bEy8tcJfzN9jx7bvjpoTh
https://wakelet.com/wake/6YaCEhhBAOhDBTHBhiKz6
https://wakelet.com/wake/1K9NNsshoPdmOrmJt2yK_
https://wakelet.com/wake/hJ6fAMBGGAZqQrk6frt5P
https://wakelet.com/wake/-9P9GGbk-27o5JpjCFKXq
https://wakelet.com/wake/qY2fK9ZR2gKBze38ianeT
https://wakelet.com/wake/fmHkoJQMx8-R-79ZP_74F
https://wakelet.com/wake/i-PUnZc-S0MlpiiN6Xlei
https://wakelet.com/wake/L2JNKq4JVvm4fTUxR_viD
https://wakelet.com/wake/z1HvlNilD5IPG9ohG9nq-
https://wakelet.com/wake/fxndwatab-qnlu_E3Ngj6
https://wakelet.com/wake/IH9deOg9i_7GbPw5cEUNL
https://wakelet.com/wake/Hw-mZDM1JmTfo7RrDEB_L
https://wakelet.com/wake/NYylwJsEXP0fdLxeOVECz
https://wakelet.com/wake/oK8OHaC4NJquSvOoWgQFZ
https://wakelet.com/wake/FUyHDf-fWuYiQge6MIit9
https://wakelet.com/wake/ChWMuLQ183Li5VtECGnux
yitswe (Sunday, 23 January 2022 18:57)
yitswe 7383628160 https://trello.com/c/4MAhtP3T/34-top-list-of-cartoon-movies-dubbed-in-hindi
https://trello.com/c/AhF8KyQB/31-top-euro-truck-simulator-2-v1121-gold-crack-only-skidrow-reloaded
https://trello.com/c/rn9VgQM5/42-refxplasticzvstiv102-64-bit
https://trello.com/c/vziRhkYc/13-hot-bajrangibhaijaanenglishmoviefreedownload
https://trello.com/c/OvE6SaK0/41-download-hd-movie-kutumb-the-family-in-hindi-work
https://trello.com/c/VjM5a3Dp/31-upd-hotspot-shield-vpn-elite-82537-multilingual-patch-rar
https://trello.com/c/8XD0appS/37-o-kadhal-kanmani-full-movie-free-download-hd-margian
https://trello.com/c/0OaMgS5J/21-download-buku-semantik-pdf-20-work
https://trello.com/c/44At2pXK/37-bharatha-rajyangam-in-telugu-pdf-free-download-nankana
https://trello.com/c/iwz5UMqu/17-premiumsoft-navicat-premium-12021-keygen-download-pc-high-quality
https://trello.com/c/agPhhkgA/36-best-xbox-360-xplorer-extreme-2-15
https://trello.com/c/FsMkfgjs/15-downloadfilmworldwarzfullmoviesubtitleindonesialucy-paeglyv
https://trello.com/c/fLR0htBp/30-bsplayer-pro-v2621068-serials-chattchitto-rg-crack-free
https://trello.com/c/HxKMYLWQ/44-adobe-muse-cc-2018-v201810266-x64-crack-crack-laqack
https://trello.com/c/mHfAnfoB/47-crack-archicad-17-french-reiljan
https://trello.com/c/W6xbhv2b/44-norton-internet-security-199114-product-key-geojan
https://trello.com/c/NqBAAyoh/37-better-bhopal-a-prayer-for-rain-full-movie-720p-hd
https://trello.com/c/eVnglin6/29-lego-rock-band-download-do-jogo-gratis-emogar
https://trello.com/c/v4jY2y5B/27-zapatlela-2-full-movie-in-hd-dvd-torrent-download-exclusive
https://trello.com/c/dv1Y5z0h/61-nh10-movie-download-torrent-sadvytt
https://trello.com/c/yKXyb1aF/19-jose-rafael-pocaterra-cuentos-grotescos-pdf-49-link
https://trello.com/c/x2SVCLLj/27-high-quality-nepali-novel-free-download-pdf
https://trello.com/c/vNuHytgK/43-nierautomata-day-one-edition-cracked-generator-online-ottmexi
https://trello.com/c/MagtpDcb/37-fratmentv-mario-busts-a-nut
https://trello.com/c/k03Q31v0/36-abrapalabra-la-magia-de-aprender-a-leer-v20-dvd
https://trello.com/c/WLgCjLZm/52-download-norton-ghost-115-corporate-dos-boot-cd-iso-verified
https://trello.com/c/jWdC7YbA/32-descargar-el-maestro-del-disfraz-comedia-espanol-latino-dvdrip
https://trello.com/c/EYVI7IqL/40-tl-rambabu-telugu-word-2-0-software-free-downloadrarlkjh-link
https://trello.com/c/NpgIfaYd/41-movavi-slideshow-maker-610-multilingual
https://trello.com/c/9REpoZja/70-trenchless-technology-in-india-pdf-download-top
eldrans (Sunday, 23 January 2022 19:15)
eldrans 7383628160 https://coub.com/stories/2944766-free-wallpaper-download-windows-7-themes-computer-full-glass-theme-pack-fixed
https://coub.com/stories/2944768-adobe-type-manager-for-win-7-64-lativa
https://coub.com/stories/2944769-_top_-empire-total-war-rip-by-synergy-without-human-verification
https://coub.com/stories/2944767-diary-of-a-wimpy-kid-doityourself-book-book-pdf
https://coub.com/stories/2944770-if-i-fall-by-shirlengtearjerky-soft-copy-weroger
https://coub.com/stories/2944771-mahasweta-sudha-murthy-pdf-free-download-new
https://coub.com/stories/2944772-nec-display-wall-calibrator-serial-number-hot
https://coub.com/stories/2944773-better-patched-vray-4-4-04-max-2018
https://coub.com/stories/2944776-easeus-partition-master-crack-better-13-8-with-serial-key-2020-updated
https://trello.com/c/gVqGefU7/50-adobe-dreamweaver-cs6-cpu-leak-fix-update-workingdp-high-quality
https://trello.com/c/libgA9aG/58-top-downloaddriverjinka721
https://trello.com/c/3r2zG7mf/38-instalaciones-electricas-residenciales-javier-oropeza-pdf-53
https://trello.com/c/c5eKFmYC/35-gymmasterlite423crack-hot
https://trello.com/c/b5CrbG7e/49-wondershare-drfone-toolkit-for-ios-85036-crack-full-version-hot
https://trello.com/c/JJTKo4c5/41-inside-out-english-hindi-dubbed-movie-download-hdl-queyar
https://trello.com/c/1Ps1zPh5/17-patched-abbyy-finereader-corporate-152101497-incl-crack-portable-deidav
https://trello.com/c/pwKr3hac/43-verified-pornhub-premium-accounts-8-october-2019
https://trello.com/c/CRz3ag9i/39-ivan-eguez-la-linares-pdf-download-latnia
https://trello.com/c/MGcSC92q/32-solucionario-de-fisica-fundamental-1-uno-michel-valero-6-purirequ
https://trello.com/c/5QLI54SU/42-gabbar-singh-hindi-dubbed-720p-moviesl
https://trello.com/c/hcjXFSLs/29-the-film-developing-cookbook-pdf-verified
https://trello.com/c/QAX9j4mP/51-ativador-do-windows-8-rar-hot
https://trello.com/c/8MHlV7Pt/35-dsls-licgen-ssqexe-furigau
https://trello.com/c/MTl1xoNw/25-download-keygen-xforce-for-navisworks-freedom-2011-isahas
https://trello.com/c/Mg7dsJbC/31-windows-embedded-81-industry-pro-x64-pt-br-original-msdn-download-verified
https://trello.com/c/7SrRIdYA/22-repack-wscrack-32-download
https://trello.com/c/ggvkqw13/46-top-bojhena-shey-bojhena-full-movie-720p-111
https://trello.com/c/x28rVDIV/44-heroinelegendsreturnoftheblackqueen-elanswe
https://trello.com/c/4K8BnpUO/71-assassins-creed-4-black-flag-access-fleet-cracked-morfay
https://trello.com/c/hv6HIyYe/26-full-adobe-premiere-pro-cc-20153-1030-202-repack-by-dakov-en-yoshrei
werith (Sunday, 23 January 2022 19:33)
werith 7383628160 https://coub.com/stories/3109463-download-medal-of-honor-2010-crack-onlyinstmank-install
https://coub.com/stories/3109462-reaper-4-32-license-key
https://coub.com/stories/3109461-walaoke-pro-3-6-full-upd-36
https://coub.com/stories/3109460-bs-en-50363-pdf-download-fremric
https://coub.com/stories/3109459-alama-za-barabarani-na-maana-zake-pdf-download-exclusive
https://coub.com/stories/3109458-link-mechanics-of-fluids-4th-edition-solutions-manual-by-potter-wiggert-ramadan-pdf
https://coub.com/stories/3109457-wifi-2020-hacker-plus-wifi-password-hacking-software-free-download-qadikani
https://coub.com/stories/3109456-free-intercourse-for-dumbos-pdf-free-19
https://coub.com/stories/3109454-kick-2009-hindi-dubbed-movie-free-163-vickimb
https://coub.com/stories/3109455-baby-mikey-vol2-xxx-comics
https://coub.com/stories/3109453-next-stop-3-download-for-pc-better-keygen
https://coub.com/stories/3109452-serial-key-of-nod32-antivirus-9
https://coub.com/stories/3109451-fasttrack-schedule-10-for-windows-cracked-full
https://coub.com/stories/3109450-work-hack-autodesk-autocad-2018-6-2-final-x86-x64-x32-keygen
https://coub.com/stories/3109447-egy-dll-pes-2013-rar-renitai
https://coub.com/stories/3109449-crack-aact-windows-and-office-activator-v3-6-multi-crackzsoft-new
https://coub.com/stories/3109448-video-copilot-metropolitan-pack-free-top-download-mega
https://coub.com/stories/3109446-tekken-5-for-pc-highly-compressed-just-30-mb-latyida
https://coub.com/stories/3109445-deer-avenger-4-no-cd-crack-link
https://coub.com/stories/3109444-extra-quality-download-xforce-keygen-fabrication-estmep-2013-free-download
https://coub.com/stories/3109443-free-download-call-of-juarez-bound-in-blood-zip-faraust
https://coub.com/stories/3109442-microsoft-toolkit-2-6-beta-2-4realtorrentz-serial-key
https://coub.com/stories/3109441-fsx-overland-seoul-incheon-international-airport-rksi
https://coub.com/stories/3109440-spc-international-creative-album-vol-13-20-__full__
https://coub.com/stories/3109439-the-chachi-420-man-720p-download-movies-jaynlat
https://coub.com/stories/3109438-vcds-full-version-download-12-new
https://coub.com/stories/3109437-__top__-solid-edge-v20-free-download-for-windows-7-32-bit-os
https://coub.com/stories/3109436-mb-carsoft-7-4-software-68-gayber
https://coub.com/stories/3109435-codigo-de-activacion-para-deezer
https://coub.com/stories/3109434-repack-wild-things-unrated-1998-720p-bluray-x264-dtswiki
chacha (Sunday, 23 January 2022 20:08)
chacha 7383628160 https://wakelet.com/wake/_C1cVMPUTRS7WAaWnWilt
https://wakelet.com/wake/meomKzVuu7glIdJYp5jxL
https://wakelet.com/wake/n3TvQHbWKOvv_uZGptUf0
https://wakelet.com/wake/TJL98tkk2PXCSNKmieFtf
https://wakelet.com/wake/V97kUDN412FSFT76UR0WC
https://wakelet.com/wake/ibk58qZXaUlIgpB4AqwNr
https://wakelet.com/wake/gGGTYRjbVsSb2pPFxrIVc
https://wakelet.com/wake/JXm1ErlIZg5_cC014Q2LB
https://wakelet.com/wake/ys_jmsQwAU0v8bEZxCrMK
https://wakelet.com/wake/zxywethlpgh07v3ZdUQX2
https://wakelet.com/wake/g1Yk09RWuYQ6prGN_v-93
https://wakelet.com/wake/hvjeoTkQWhdegauKy64U3
https://wakelet.com/wake/Rwtw12EnPs6vuN_ZET_pP
https://wakelet.com/wake/nwskiRVMH8gISrVldjLTr
https://wakelet.com/wake/SaVcn8MrvH4UeHORcu2uf
https://wakelet.com/wake/h3RVh9EiSXLGBxNJ3z08M
https://wakelet.com/wake/gzN0yd8Oz2D82ylUFj9G6
https://wakelet.com/wake/mH5DGHOcETi8Rtr-5hSWQ
https://wakelet.com/wake/ijqrbmZuB5fHugY_7MNzp
https://wakelet.com/wake/sbB0cG1t4dzRdQGbqdN6j
https://wakelet.com/wake/2ALdpHvQjS3rEkADXEKvX
https://wakelet.com/wake/3Qmk8HhOvaAqoeHK9igd_
https://wakelet.com/wake/3-DtIJs8u5xyKgX7Psckj
https://wakelet.com/wake/EUtkaiFD89r_U3K7owizR
https://wakelet.com/wake/7KvhGle-25zO5xy66KJTP
https://wakelet.com/wake/JbJhBOYcas1tRI9MLraDv
https://wakelet.com/wake/e3tEoRV7jX_Dfu-K-IUOL
https://wakelet.com/wake/THjQlKiGgewdxpoZKwRLv
https://wakelet.com/wake/mIhqDn3ZLo2mrcwxVnni4
https://wakelet.com/wake/3a_humnLlAt6CVjc-WuTW
haynwalc (Sunday, 23 January 2022 20:26)
haynwalc 7383628160 https://trello.com/c/wvVSuZFQ/30-full-descarga-universal-adobe-patcher-painter-activador-de-los-productos-adobe
https://trello.com/c/s1gtHJBe/12-cutmaster-2d-pro-1331-crack-hot-34
https://trello.com/c/iAAr27LD/32-demul056arcaderomspackepub-luderain
https://trello.com/c/qJo2t6cE/35-gardenscapes-mansion-makeover-ce-full-precracked-foxy-game-money-hack-portable
https://trello.com/c/ZWMO0PSu/50-ms-office-2007-enterprise-activated-and-tested-download-cracked
https://trello.com/c/65cHLJeP/42-best-xforce-keygen-autocad-mobile-2019-64bit-free-download
https://trello.com/c/32Pccehd/73-a-little-agency-little-melissa-pictures-pealeon
https://trello.com/c/aMotZu8X/24-the-longbow-converter-v4-13-link
https://trello.com/c/EVyOlIV0/65-hot-pirates-tides-of-fortune-hack-tool-version-37
https://trello.com/c/fzY1chnW/41-driver-sl1000-usb-dmxl-opakafe
https://trello.com/c/B23VZJFz/36-pendidikan-kaum-tertindas-pdf-downloadl-abiseyw
https://trello.com/c/HSV3eRr2/18-scp-containment-breach-ntf-hot
https://trello.com/c/TQZTjaOz/69-step-3-enter-your-confirmation-code-here-office-2007-top
https://trello.com/c/mNMJW1uU/34-sap-gui-740-download-for-windows-10-686-gituelv
https://trello.com/c/98HhTxnC/18-gta-iv-multiplayer-nosteam-part2-top
https://trello.com/c/GZCm9bw5/25-hitman-absolution-keygen-passwordfull20-vickyes
https://trello.com/c/q7R8J9oS/19-new-archicad-14-crack-windows-7-32-bit
https://trello.com/c/C9KVVwqj/27-luv-ka-the-end-full-movie-download-in-hindi-720p-fabiquy
https://trello.com/c/lvkgmfYB/62-free-resident-evil-6-steamapi-issteamrunning
https://trello.com/c/PAVEkyB5/36-hot-detective-byomkesh-bakshy-full-movie-hd-720p
https://trello.com/c/wzX31ipJ/54-link-hd-online-player-fly-girls-720p
https://trello.com/c/OHd0F4rQ/24-hot-2012-october-movie-hindi-dubbed-free-download
https://trello.com/c/P7dgBpkK/51-better-abb-switchgear-manual-12-ed-36
https://trello.com/c/xYIKit9O/19-download-long-tail-pro-platinum-315-free-palbhen
https://trello.com/c/6V6KAxIb/42-verified-audio-transcoder-v1-7-6-1058-cracked-devils-den-release-download
https://trello.com/c/up16xZwf/57-descargar-keygen-corel-x6-gratisl-holiwale
https://trello.com/c/Dog9fZzI/35-adobe-after-effects-cc-2020-crack-full-version-is-here-updated
https://trello.com/c/8MzTRkib/30-iar-stm8-exclusive-crack
https://trello.com/c/dfBMSHq2/62-bewafa-sanam-full-movie-download-utorrent-better
https://trello.com/c/qhKE8Nl8/45-best-worldwarz720pdualaudiofreedownload
bandori (Sunday, 23 January 2022 20:44)
bandori 7383628160 https://coub.com/stories/3028192-__exclusive__-crack-kmspico-20-2-9-final-portable-office-and-windows-10-activator
https://coub.com/stories/3028191-adobe-photoshop-cc-2014-v15-2-team-rjaa-exclusive
https://coub.com/stories/3028190-download-keygen-xforce-link-for-revit-lt-2013-download
https://coub.com/stories/3028189-ittefaq-download-720p-in-hindi-better
https://coub.com/stories/3028188-aashiqui-2-full-movie-hd-1080p-free-download-utorrent-movies-laveroz
https://coub.com/stories/3028184-neat-video-4-1-crack-mac-repack
https://coub.com/stories/3028186-hot-cyberlink-powerdvd-pro-v17-0-1523-60-final-crack-keygen-full-version
https://coub.com/stories/3028187-download-willett-460-ink-jet-printer-service-and-maintenance-manuel-rar-vyncgret
https://coub.com/stories/3028185-magix-movie-edit-pro-15-plus-8-0-5-8-crack-__link__
https://coub.com/stories/3028183-lets-fish-v72-hackrar-lauelm
https://coub.com/stories/3028180-install-summon-night-swordcraft-story-3-english-patch-35
https://coub.com/stories/3028182-upd-investiguemos-10-fisica-pdf
https://coub.com/stories/3028181-_verified_-conners-adult-adhd-rating-scales-self-report-short-version-pdf
https://coub.com/stories/3028178-redgate-sql-prompt-6-keygen-14-top
https://coub.com/stories/3028179-national-theatre-live-hamlet-download-pdfl-granarc
https://coub.com/stories/3028177-purab-aur-paschim-movie-720p-download-utorrent-movies-hot
https://coub.com/stories/3028176-artioscad-12-crack-product-50-nineisi
https://coub.com/stories/3028175-eacricket07playereditorfreedownload-patched
https://coub.com/stories/3028174-svr2011wwe12modps2-arcdor
https://coub.com/stories/3028172-3d-sex-villa-2-full-free-for-android-apk
https://coub.com/stories/3028173-libro-crypta-care-santos-pdf-21-evgejer
https://coub.com/stories/3028170-the-gangs-of-wasseypur-2-free-download-nehegran
https://coub.com/stories/3028171-cracked-dr-sugimotos-lecherous-treatment
https://coub.com/stories/3028169-copyscape-free-new-download-crack-for-windows
https://coub.com/stories/3028168-new-magnet-simulator-hackscript-auto-farm-auto-berlaur
https://coub.com/stories/3028167-reikan-focal-download-crack-internetkl-free
https://coub.com/stories/3028166-sunny-2011-korean-movie-english-subtitles-download-torrent-darsal
https://coub.com/stories/3028165-iobit-uninstaller-pro-8-6-0-6-crack-product-key-download-2019-valfilb
https://coub.com/stories/3028160-adobe-photoshop-cc-2015-v1612-x64-patches-pansbes
https://coub.com/stories/2979125-link-revealer-keylogger-pro-edition-keygen
balbala (Sunday, 23 January 2022 21:18)
balbala 7383628160 https://wakelet.com/wake/kZrL62R9KN0Lh_eE29vnV
https://wakelet.com/wake/uB-RCy3WEWMXA7k-CeDzG
https://wakelet.com/wake/SKdz6nxC2gbtl8PY94Irc
https://wakelet.com/wake/giPzZeDLWuSxX2cdSMV6-
https://wakelet.com/wake/Hl0-_p-gMZJqlLPAv5fyy
https://wakelet.com/wake/GEDAeNCiugZ5eBVPnpoD-
https://wakelet.com/wake/ckcwZVvUtpXic7RT1uB5o
https://wakelet.com/wake/Fg9HmkOc9iMJ8TbBVD-2l
https://wakelet.com/wake/_tT2Jal0gD1CNhsoJVb5c
https://wakelet.com/wake/R1y8VaasVxVGK5sFenZq3
https://wakelet.com/wake/hv8DT3878qDAWZphTiP3B
https://wakelet.com/wake/ktibIh9KJc1nsw7dcxkdF
https://wakelet.com/wake/i8sbS1qTtxkEucdh9Ccx0
https://wakelet.com/wake/yUKZfl77KGlfLYGwp7Hfp
https://wakelet.com/wake/sxYNjqBtoj5mMKk30Vlx_
https://wakelet.com/wake/Ns-4FKUGRXs8nHgEVjh5g
https://wakelet.com/wake/QyVhnRYvZT4kUHj_QxTzf
https://wakelet.com/wake/87UBs6GEMj11e3UN3vKFV
https://wakelet.com/wake/gfK8_u1IxRySBTwJtPugB
https://wakelet.com/wake/vT4spSb4BeNCVMjiJuOSj
https://wakelet.com/wake/w_XYW0IDV7E5qEsmJ2efk
https://wakelet.com/wake/NvrwDrjJ6Dm43fxZvbpex
https://wakelet.com/wake/j_cgUYoFienzxvBgU82OZ
https://wakelet.com/wake/zTGKtAKGPU3ujiB5Ps3F3
https://wakelet.com/wake/-gRjZNn19YWk9C2Q-NrJC
https://wakelet.com/wake/ivz3VdAaS0gM6AETKndEH
https://wakelet.com/wake/SOqez8QSiBliFyrjTMY6v
https://wakelet.com/wake/OpKEnKt7nVNP_k11hPbg0
https://wakelet.com/wake/ja1faBe0bDAzHSX-AvER9
https://wakelet.com/wake/7EMgCZ83lNyHh3tjcm21q
kasscaro (Sunday, 23 January 2022 21:36)
kasscaro 7383628160 https://trello.com/c/OLbIsW4L/29-metalcad-designcad-pro6000-logiciel-de-dessin-zymphei
https://trello.com/c/BfYABFWx/49-mere-baap-pehle-aap-hd-1080p-in-hindi-download-work
https://trello.com/c/1wqWelL0/38-new-vandykesecurecrtv504inclcrack-tbe-serial-key
https://trello.com/c/hsKFehJH/23-work-h2o-syncrosoft-truemu-v41-64-bit
https://trello.com/c/oTVZNpfv/42-full-vas-pc-v190101-english-torrent
https://trello.com/c/QSxW6sWH/27-upd-cnckad-v10-crack-basso-condivisi-part
https://trello.com/c/TwJ2BKep/46-mahesh-khaleja-movie-download-dvdrip-torrent-adlecha
https://trello.com/c/AH3TSPYk/19-libroreinventarsemarioalonsopuigpdf30-brilatr
https://trello.com/c/FR8S4xzy/40-http-uploadsnackcom-mgkrju-nanweke
https://trello.com/c/AiE4n11e/81-hd-online-player-jai-santoshi-maa-720p-torrent-downlo-keiljale
https://trello.com/c/4vLtVMH6/65-free-download-new-insight-into-ielts-student-book-with-answers-fralata
https://trello.com/c/fYOBjqOU/41-geosoft-oasis-montaj-75-crack-exclusiverar
https://trello.com/c/b3NQsOoa/29-la-celestina-clasicos-adaptados-vicens-vives-epub-2021
https://trello.com/c/Qxn6CpgY/13-universal-xforce-keygen-autocad-lt-2010-patched
https://trello.com/c/JQLBWFLF/53-teracopy-free-download-free
https://trello.com/c/fpAGdkw9/27-hkcee-chemistry-marking-scheme-2006-meckap
https://trello.com/c/9veaVTmV/15-lego-city-undercover-pc-crack-download-hot
https://trello.com/c/BcIXRNP2/15-codigo-de-activacion-para-brainsbreaker-5-176-romgold
https://trello.com/c/RLZdfLiP/97-best-descargar-photoscore-ultimate-7-crack-full
https://trello.com/c/v4HVShBb/21-download-kbuilder-5-full-crack-software-santysab
https://trello.com/c/7zXp04WZ/40-windows-8-release-preview-build-8400-activator-crack-free
https://trello.com/c/XGFZ9fkt/52-manual-polyboard-4-castellano-3-new
https://trello.com/c/joYVALRn/74-vigil-the-longest-night-free-download-pc-game-hot
https://trello.com/c/EP4odav6/42-link-la-5082p-schematic
https://trello.com/c/h09q1f3U/14-sprut-ddos-download-best
https://trello.com/c/NYyWfGt2/30-mailing-master-bulk-emails-sender-rar
https://trello.com/c/cgUBZ5cr/24-regclean-pro-621651986-com-crack-download-hot
https://trello.com/c/jyjmidWR/31-epson-adjustment-program-rx59516
https://trello.com/c/EbUjI7uI/27-cracked-the-witcher-3-wild-hunt-v104-update-gog
https://trello.com/c/ltTlWqpk/29-bunifu-ui-winforms-v1900-work
chapfinb (Sunday, 23 January 2022 21:54)
chapfinb 7383628160 https://trello.com/c/qmauuvEY/46-link-fryturama-luz-12yiso
https://trello.com/c/1ne4f6UT/39-bangalore-days-1080p-movie-download-top
https://trello.com/c/WYHV6OIX/13-hd-online-player-dvdvideosoft-free-studio-503-seria-work
https://trello.com/c/X5pSocPA/34-la-noire-license-corrupt-fix-gerimalo
https://trello.com/c/fqfwQJ9g/29-playerexe-dv4-download-better
https://trello.com/c/LG8Aooza/18-swt-win64-dll-download-nekeasht
https://trello.com/c/YjQToPvw/32-torrent-guardians-of-the-galaxy-1080p-patched
https://trello.com/c/ihexYSLu/65-better-milorad-ulemek-legija-knjiga-legionar-pdf-download
https://trello.com/c/s38SiqVC/30-mere-yaar-ki-shaadi-hai-movie-with-english-subtitles-download-torrent-upd
https://trello.com/c/lPgGdZFH/34-jazler-show-2-crack-top
https://trello.com/c/3KuxUw5i/56-ourives-das-palavras-pdf-download-link
https://trello.com/c/XGl0rKZX/33-autotune-evo-v609-crackdimi-vst-latrhole
https://trello.com/c/BLAhb7t0/36-high-quality-downloadtrainermafia21001epub
https://trello.com/c/NN5evgiM/39-all-star-strip-poker-hard-version-by-alma69-generator-online
https://trello.com/c/samkWERi/33-victoria-2-napoleon-legacy-ielhede
https://trello.com/c/Dtys4iCI/23-family-and-friends-2-teachers-book-free-download-pdf-beltdaro
https://trello.com/c/oqhIw5xN/27-dsm-v-italiano-pdf-download-new
https://trello.com/c/zIpcqQs8/26-top-limit-konu-anlatimi-pdf-download
https://trello.com/c/gqgIdUCY/43-better-word-magic-professional-63-codigo-de-activacion
https://trello.com/c/gB71mrNm/23-resident-evil-hd-remaster-fitgirl-repack-latest-version
https://trello.com/c/vXpsqHZs/40-diana-krall-glad-rag-doll-deluxe-edition-2012-mp3-320kbps
https://trello.com/c/WQONaObR/26-tratadodecirugiabucalkruger
https://trello.com/c/yUdPMI5v/17-hizashi-no-naka-no-riaru-uncensored-20
https://trello.com/c/UHNkN8IC/43-witcher-2-en0-w2speech
https://trello.com/c/qnOQgFgr/76-revit-2013-64bit-keygen-xforce-uraijan
https://trello.com/c/gEgHs2U7/65-link-captain-sim-l-1011-cracked
https://trello.com/c/1kuK6ZbG/36-2021-crack-nemotec-dental-studio-nx-windows-7-18
https://trello.com/c/fBEHkbYe/15-best-alice-and-simone-swallow-live-fish-and-micerar
https://trello.com/c/qro29t8m/41-toyotastarletep91servicemanualrar
https://trello.com/c/H5zD5qJe/63-best-auto-keyboard-murgee-full-crack-kid
melajan (Sunday, 23 January 2022 22:12)
melajan 7383628160 https://coub.com/stories/3097026-adobe-illustrator-cc-2019-23-1-0-670-crack-top-activator-for-mac-windows
https://coub.com/stories/3097024-tweakbit-fixmypc-serial-key-2016-download-leadwac
https://coub.com/stories/3097023-crackmaxpayne12-talilang
https://coub.com/stories/3097022-patched-serial-solidworks-electrical
https://coub.com/stories/3097021-burnout-3-takedown-para-pc-1-21-makque
https://coub.com/stories/3097019-download-emupgrade-v2-26-137-alodolea
https://coub.com/stories/3097020-50-odtenkov-sive-download-free-z-reedkia
https://coub.com/stories/3097018-gm-bagi-bagi-char-cf-85-upd
https://coub.com/stories/3097017-portable-wondershare-mobile-go-crack-torrent
https://coub.com/stories/3097016-cd-panda-vai-a-escola-3-download-gratis-torrent-sargphi
https://coub.com/stories/3097015-upd-hd-online-player-governor-poker-2-free-download-crack
https://coub.com/stories/3097014-bandicam-4-0-1-1339-pre-cracked-for-windows-crackzsoft-serial-key-keygen-updated
https://coub.com/stories/3097013-hd-online-player-wrong-turn-2-in-hindi-720p-torrent-install
https://coub.com/stories/3097012-verified-meshmixer-2015-x86-x64-keygen-serial-key
https://coub.com/stories/3097011-download-film-una-canaglia-a-tutto-gas-ellnin
https://coub.com/stories/3097010-hd-online-player-stargate-sg1-season-8-720p-torrent-ekecare
https://coub.com/stories/3097009-the-rock-spy-hunter-nowhere-to-run-multi5-pc-game-no-survey-no-password-2019
https://coub.com/stories/3097008-dss-dj-56-unlock-code-bethbir
https://coub.com/stories/3097006-real-kanojo-mod-manrei
https://coub.com/stories/3097007-eamcet-physics-formulas-pdf-download-new
https://coub.com/stories/3097005-brawl-stars-privet-server-download-__full__
https://coub.com/stories/3097004-adobe-photoshop-cs6-trial-to-full-crack-best
https://coub.com/stories/3097003-volvo-rti-mmm-plus-europe-hdd-2015-multilanguage-navigon-updated
https://coub.com/stories/3097002-sims-3-patch-1-0-615-to-1-0-631-125
https://coub.com/stories/3097000-gigatribe-premium-crack-serial-keys-alinrowy
https://coub.com/stories/3097001-vspace-software-for-windows-7-32-bit-46-yemikai
https://coub.com/stories/3096998-verified-piccolo-nemo-avventure-nel-mondo-dei-sogni-2-full-movie-mp4-free-download
https://coub.com/stories/3096999-rpc-plugin-for-3ds-max-2015-crack-__full__
https://coub.com/stories/3096997-3dpageflipprofessional162keygengenerator-upd
https://coub.com/stories/3096996-scientific-workplace-5-5-build-2953-portable-cracked-file-spartito-broken-mane
talbert (Sunday, 23 January 2022 22:46)
talbert 7383628160 https://wakelet.com/wake/cgn9VIGIrw9z34_M-SYJe
https://wakelet.com/wake/U5DwO9K6j4Y_lqxIcbLxU
https://wakelet.com/wake/HJWS-WNdh3zH-f5R-I-HO
https://wakelet.com/wake/bF8jrfYTb1QMnVDgLqFtC
https://wakelet.com/wake/ecO4RF2uH36HO5cVMfKV5
https://wakelet.com/wake/ync-fDxDKIDhuiUjUbdtu
https://wakelet.com/wake/YmXgkxPsqsRRk7qx8ohQr
https://wakelet.com/wake/4s-K08iBbvcnJj-sH2DK4
https://wakelet.com/wake/GsyiI82kaIG9wpWfCxxru
https://wakelet.com/wake/ANHdJ16V3cKiJWNuBl8Vc
https://wakelet.com/wake/5zfGsQbaZb2kF33FLSL_S
https://wakelet.com/wake/BGreJCeeKQF5VHa0CCqpu
https://wakelet.com/wake/AHWmYPDZKtDHHaKH4Nroz
https://wakelet.com/wake/wt7EHXk9szE14ZrZ-9Eks
https://wakelet.com/wake/0hgZR5tnQk85CiLvOX6F7
https://wakelet.com/wake/4KxUiKE5JQtRkbEiBWpiL
https://wakelet.com/wake/hGxUAQFKLwSsD44p6MxNg
https://wakelet.com/wake/SdCA5_zc6tlV4EFbP0ZJ0
https://wakelet.com/wake/l23cgq8QAoA65MoK4Y_Lb
https://wakelet.com/wake/mnOWA97MwOxrfT85y9Pl0
https://wakelet.com/wake/GgiOy9r4kZiVKw3wr_TrE
https://wakelet.com/wake/GDVBLOFCq7efZhD9kwo41
https://wakelet.com/wake/YwzPl1PyFPIHByrGSvG1k
https://wakelet.com/wake/edrEQHAhDOnOgdC2O7ECs
https://wakelet.com/wake/SA7qVg8DNhlpcTU7L0ukm
https://wakelet.com/wake/gLQIVMyjFVsROva3lDHaN
https://wakelet.com/wake/krRqjGiqHq2bUnuk4y9AG
https://wakelet.com/wake/R5BDmrcKX8sFfg2_gayiN
https://wakelet.com/wake/c6UEDUbTUZdaH83__3aml
https://wakelet.com/wake/rt4BgGMrStxDD0Bp_tp6R
nenphy (Sunday, 23 January 2022 23:05)
nenphy 7383628160 https://trello.com/c/aSqYpntY/46-hot-tinker-tailor-soldier-spy-720p-download-links
https://trello.com/c/esIpAxxL/19-hmm-lea-set-14-part-1-top
https://trello.com/c/6Fhrq21C/12-cut-rite-modular-v82rar-walsvaug
https://trello.com/c/ftvWjedq/23-cinemaware-anthology-1986-1991-download-for-pc-crack-serial-key-top
https://trello.com/c/BmMRst69/22-descargar-telenovela-destilando-amor-completa-gratis
https://trello.com/c/lFqR2ueB/27-singham-movie-full-in-tamil-hd-1080p-ginequan
https://trello.com/c/zPN7XHn2/54-top-x-force-x32-exe-character-generator-2017-activation
https://trello.com/c/EA3q608N/82-diva-mizuki-4-ekoruzip-new
https://trello.com/c/zzjHLG6e/42-mixmeister-fusion-video-crack-pro-holagra
https://trello.com/c/vuGlTYYE/67-remshutdownv270cracked-mesmerize-free-download-verified
https://trello.com/c/zxpS0vN7/38-adobe-acrobat-xi-pro-11022-patch-cracksnow-serial-key-keygen-patched
https://trello.com/c/MdQUPV3u/40-xf-max2k9-32bit-kg-rar-free-download-rafberk
https://trello.com/c/5DB7ZZXK/30-unlock-qr-code-reader-google-android-for-android-phones-link
https://trello.com/c/6pEYniOk/19-windows-7-deep-blue-alienware-download-software-imbkri
https://trello.com/c/MNMrFA5G/33-new-eckhart-tolle-puterea-prezentului-ghid-practic-pdf-download
https://trello.com/c/Alwqff2Z/43-chryslervoyagerradiocodecalculator-new
https://trello.com/c/8qDQN67A/84-download-aphrodite-pro-font-free-zip-izuupal
https://trello.com/c/9zmn4zFF/68-r-studio-73-build-155233-network-edition-preactivated-repack-serial-key-keygen-upd
https://trello.com/c/Mlcd7J7C/29-bigjon-wheel-of-fortune-download-gilbgail
https://trello.com/c/fkfNabd4/39-final-fantasy-7-pc-ultimate-edition-skidrow-reloaded-harlchar
https://trello.com/c/vVywFuKN/34-msize-hentai-seiheki-dominancerar
https://trello.com/c/AjGPzgVR/29-bartender-101-keygen-link
https://trello.com/c/EhQTsLLf/28-2021-9dragons-skill-trainer-bot-download
https://trello.com/c/kKntNTZx/85-begriptoetse-in-afrikaans-graad-3-vraestelle-lesrai
https://trello.com/c/Vkr5Uz6C/21-install-full-soal-bahasa-inggris-smp-kelas-7-semester-1penerbit-bse
https://trello.com/c/yrKsgj9x/29-video-gay-om-om-bapak-bapak-free
https://trello.com/c/n5YCwa9L/50-new-autocad-plant-3d-2017-key-marcnewl
https://trello.com/c/csl5JETB/28-multiecuscan-keygen-upd
https://trello.com/c/kdmRIQqI/68-free-download-the-love-boat-second-chances-exe-makapan
https://trello.com/c/c6jrslfl/26-thief-english-language-pack-4-bennlin
yudruss (Sunday, 23 January 2022 23:22)
yudruss 7383628160 https://coub.com/stories/3061995-chemstations-chemcad-6-2-0-3348-license-key-full
https://coub.com/stories/3061992-batman-arkham-asylum-goty-crack-no-cd-heawhit
https://coub.com/stories/3061991-__full__-bandicam-crack-4-5-6-1647-latest-version-2020-full-download
https://coub.com/stories/3061988-tanner-tools-v141-64bit-crack-filmale
https://coub.com/stories/3061985-iobit-protected-folder-v4-3-0-50-final-serials-sh-rar-hot
https://coub.com/stories/3061983-g-force-movie-in-hindi-dubbed-free-download-hd-zaviindy
https://coub.com/stories/3061982-extra-quality-autocad-electrical-2017-64bit-product-key-and-xforce-keygen-rar
https://coub.com/stories/3061981-acp-interlude-download-makahaid
https://coub.com/stories/3061979-the-sims-3-crack-1-0-631-00001-rar-guibel
https://coub.com/stories/3061976-download-gx-developer-8-7-full-crack-357-work
https://coub.com/stories/3061977-zet-9-geo-crackbfdcm-clenage
https://coub.com/stories/3061974-cars-3-english-3-full-movie-download-720p-hd-raydae
https://coub.com/stories/3061975-autodesk-forge-2019-x64-64bit-product-key-and-xforce-keygen-exclusive
https://coub.com/stories/3061970-mujhe-is-duniya-me-laya-mujhe-bolna-chalna-sikhaya-song-lyricsl-chrixahr
https://coub.com/stories/3061969-verified-jalopy-v1-0-hack-tool-download
https://coub.com/stories/3061967-diablo-2-cd-key-generator-crack-nickrec
https://coub.com/stories/3061965-download-extreme-pbr-2-0-addon-for-blender-2-8-get-into-pc-link
https://coub.com/stories/3061964-work-sony-handycam-dcr-hc23e-software-download
https://coub.com/stories/3061962-downloadpokemonprismromfullversion-2-naddesh
https://coub.com/stories/3061961-mumbai-gram-panchayat-act-1958-in-marathi-pdf-repack-free-237
https://coub.com/stories/3061959-movavi-video-editor-plus-16-7-1-crack-serial-key-jaeber
https://coub.com/stories/3061957-genx-usb-scanner-driver-__top__-download-rcfa4601eu-for-windows-7-3271
https://coub.com/stories/3061941-repack-solucionariointroduccionalanalisisdecircuitosboylestad10
https://coub.com/stories/3061950-activation-file-delphi-2010-slip-checked-casanth
https://coub.com/stories/3061953-audaces-digiflash-download-crack-upd
https://coub.com/stories/3061951-free-download-license-key-portraiture-plugin-for-photoshop-cs5-annfeli
https://coub.com/stories/3061952-business-information-system-muneesh-kumar-pdf-download-top
https://coub.com/stories/3061949-antenna-and-wave-propagation-by-amsaveni-pdf-free-top-14
https://coub.com/stories/3061948-remo-tamil-telugu-movie-english-subtitles-download-for-movies-_hot_
https://coub.com/stories/3061947-verified-prezi-torrent
quaelod (Sunday, 23 January 2022 23:57)
quaelod 7383628160 https://wakelet.com/wake/db6vAA5b2agzBtxziPnoN
https://wakelet.com/wake/dLSuE-OEq3ypjkp2uJQ9t
https://wakelet.com/wake/bPu0US1EHHXMuHZFWI1kv
https://wakelet.com/wake/mit5jjiqAqQe-o0w2iW89
https://wakelet.com/wake/n0I4IBwrt0z18CkvhqBr3
https://wakelet.com/wake/IKlQm9c0fEX8hs29nDnyw
https://wakelet.com/wake/cVJ_pO7aB9_3sIMkovB3s
https://wakelet.com/wake/myeTgs7cNo_nvIE5vh-Ma
https://wakelet.com/wake/g9N8c1hQng2m1ttN8hhYq
https://wakelet.com/wake/bpYzhsYGpq4snR14jxufr
https://wakelet.com/wake/OXKLhPPWcKTpJGLFjoS10
https://wakelet.com/wake/ypluMFyO2LjYCNE88J0i_
https://wakelet.com/wake/93_8oRqg2TzUN91jZ-QCS
https://wakelet.com/wake/G4IRtGp7gA49i6E3jYVXb
https://wakelet.com/wake/Yx8lC3yloS9gtafpiE3LV
https://wakelet.com/wake/K505gsZSsf4BW-deiZUx6
https://wakelet.com/wake/ZLx_sEUQGnsQ0cdL0I2lS
https://wakelet.com/wake/O25IEShtT0WTg8lOHjvtr
https://wakelet.com/wake/L2Q1nhlVWu7FpYt30j9bZ
https://wakelet.com/wake/HEtN_5Mt17nD80Pu1Jyc_
https://wakelet.com/wake/_j364r4lOFebmWWse6pxz
https://wakelet.com/wake/wd-5nrSLZwhexkh7iYXMF
https://wakelet.com/wake/k8F_IGBeL9C_T7muhoz2N
https://wakelet.com/wake/OvynZusqxB6lURzgzSe5A
https://wakelet.com/wake/-ejwjWR-VmkbZurJDPJrJ
https://wakelet.com/wake/5C-B1OLNcerNq9coowGP8
https://wakelet.com/wake/aFj_OWF8-Xul-hgDXb3U5
https://wakelet.com/wake/G-5f5BzZJAPjkR6XE-k-G
https://wakelet.com/wake/l7GOHf2Q3bGa00i4SukvQ
https://wakelet.com/wake/TY4ErWVVK6ETOvh-FZS_j
seelgit (Monday, 24 January 2022 00:16)
seelgit 7383628160 https://trello.com/c/GJzChuT1/41-adobe-premiere-pro-cc-2019-v130238-repack-multilang-x64-rar-landfai
https://trello.com/c/U7LYeDFW/33-serum-vst-2020-crack-torrent-version-updated-free-download-for-win-mac-hot
https://trello.com/c/fDYczl0p/28-economia-y-contabilidad-angrisani-lopez-pdf-11-lorwat
https://trello.com/c/zMx7M434/26-madarij-al-salikeen-urdupdf-rapyfarr
https://trello.com/c/PQxJKsp4/15-the-time-that-remains-720p-torrent-lyvilyz
https://trello.com/c/J0GyHOdg/31-cobra-11-nitro-no-cd-crack-olieos
https://trello.com/c/HnZycrq1/33-lifestyle-news-mixture-images-wallpapers-part-274
https://trello.com/c/LF2QsnW0/33-best-creed-weathered-full-album-zip
https://trello.com/c/OJUAY4hG/22-portable-cadvent-61-keygen
https://trello.com/c/6suz2l8K/95-top-sage-50-premium-with-payroll-torrent
https://trello.com/c/4a2w2yO4/27-best-musiclab-realguitar-502-crack
https://trello.com/c/TlLVY7AO/39-2021-buku-psikologi-kepribadian-pdf-to-word
https://trello.com/c/4OhYq7mE/240-lords-of-football-united-states-full-crack-patchl-lachil
https://trello.com/c/7sJOmlSJ/18-vag-com-12103-cracked-28-exclusive
https://trello.com/c/j4GMYGO9/69-ecm-titanium-161-top-crack-12
https://trello.com/c/WjufmXgK/42-3d-object-converter-440-crack-top
https://trello.com/c/9Wn8MnWk/28-aui-converter-48x44-pro-crack-new
https://trello.com/c/2E0R87CB/25-qda-miner-crack-gertaju
https://trello.com/c/5JYMCGOE/26-kaththifullmovieintelugudubbeddownload-top
https://trello.com/c/aoKsUsk1/44-best-vlc-media-player-309-crack-2020
https://trello.com/c/bbPTGj4b/21-bandicam-crack-44-with-keygen-free-olwvyn
https://trello.com/c/shJuZd6H/40-unity3d-modern-ruins-packzip-purgar
https://trello.com/c/cB39I1oE/29-microangelo-on-display-703-cracked-full
https://trello.com/c/A0Em46yT/40-the-revenant-english-full-movie-in-hd-free-best-download
https://trello.com/c/vFsoekPN/36-tropical-liquor-download-exclusive-for-pc-pack
https://trello.com/c/gTO3H5TF/39-cardlife-cardboard-survival-game-vlasxili
https://trello.com/c/huds9I7p/74-top-belkasoft-evidence-center-keygen-free
https://trello.com/c/yYbh9E1F/17-revo-uninstaller-pro-400-repack-latest-serial-key
https://trello.com/c/KEVv8yb7/45-abletonlivesuitev971-serial-key-keygen-taijcher
https://trello.com/c/MEDAS989/25-mehuna-hindi-top-full-movie-online
margxell (Monday, 24 January 2022 00:34)
margxell 7383628160 https://coub.com/stories/2974428-virtual-girls-hd-free-full-shows-cracked
https://coub.com/stories/2974426-jdpaint-5-55-gilcal
https://coub.com/stories/2974427-link-ebp-crack-etools-dll
https://coub.com/stories/2974423-hd-online-player-rio-movie-download-in-hindi-720p-reikal
https://coub.com/stories/2974422-castlevania-lords-of-shadow-mirror-of-fate-hd-reloaded-fitgirl-repack-install
https://coub.com/stories/2974420-download-directx-10-for-windows-7-exclusive
https://coub.com/stories/2974419-free-adobe-photoshop-cs4-tutorial-pdf-12-chrireig
https://coub.com/stories/2974418-link-patched-recovery-toolbox-for-rar-v1-1-16-39-crack-chattchitto-rg
https://coub.com/stories/2974417-obs-studio-22-0-2-full-installer-x64-serial-key-keygen-jahmtiba
https://coub.com/stories/2974416-best-adobe-dreamweaver-cc-2019-v19-2-0-11274-x64-patch-944-mb
https://coub.com/stories/2974414-top-gangs-of-wasseypur-download-movie-1080p-torrent
https://coub.com/stories/2974413-interstellar-movie-in-hindi-2021-download-300mb
https://coub.com/stories/2974411-super-mario-64-120-stars-cheat
https://coub.com/stories/2974412-khan-absolute-power-crack-download-skidrow-geofyama
https://coub.com/stories/2974410-hot-flightradar24-crack-download-for-iphone
https://coub.com/stories/2974408-work-activation-revit-2006-keygen
https://coub.com/stories/2974409-high-quality-realplayer-plus-16-full-version-free-download-1-407
https://coub.com/stories/2974406-drawful2crackgameupdated-download
https://coub.com/stories/2974405-hot-xforce-keygen-32bits-navisworks-freedom-2017
https://coub.com/stories/2974404-planet-nomads-v1-0-3-2-update-razordox-yuleruli
https://coub.com/stories/2974403-artcampro2012cracktorrent-new
https://coub.com/stories/2974401-def-jam-fight-for-ny-xbox-iso-carlwil
https://coub.com/stories/2974402-__exclusive__-gods-pharmacy-book-pdf-download
https://coub.com/stories/2974400-software-untuk-mengubah-jpg-ke-word-kailiret
https://coub.com/stories/2974398-top-catarina-e-os-outros-filme-completo-129311
https://coub.com/stories/2974396-how-to-install-rover-t4-software-verified
https://coub.com/stories/2974397-webstorm-2019-2-3-crack-with-registration-key-free-download-_hot_
https://coub.com/stories/2974395-exitlagouwtfastcrack-free
https://coub.com/stories/2974392-rnd-portico-5043-compressor-crack-updated
https://coub.com/stories/2974390-outlines-of-chemical-technology-dryden-pdf-better
felmadd (Monday, 24 January 2022 01:12)
felmadd 7383628160 https://wakelet.com/wake/xBLCrmOswpiqTeal2ocpb
https://wakelet.com/wake/XPL11vcssAC1SAbCFgnFU
https://wakelet.com/wake/47wXZL_onZoE16sRugxUo
https://wakelet.com/wake/HOs-RiMkYcDiY9q1AareR
https://wakelet.com/wake/JIeFfGgO3_uHEA-mZ3hYM
https://wakelet.com/wake/ORaNyDf8PeHKiMwYnOqgI
https://wakelet.com/wake/-U9-rkEmNQeAvdppNaIZj
https://wakelet.com/wake/1KRQyRuaTsndchZs-7mLT
https://wakelet.com/wake/32rAYPPFzr_pl72ChoNZC
https://wakelet.com/wake/i5ClvC3W33RcrQCqSi4V0
https://wakelet.com/wake/HnEKWLGp3_YvoNz5WWLPB
https://wakelet.com/wake/Klxa2PbF0orlZaob1-rAV
https://wakelet.com/wake/RlLkgZOeFvt6XVbdURY7U
https://wakelet.com/wake/eLIplzlXjY_k9Ze7ltky3
https://wakelet.com/wake/UmfsJciskOHB9fHyL4bYo
https://wakelet.com/wake/UZo0FU8n39hh8dX4djjj2
https://wakelet.com/wake/knm1QTk8mfEQgp_Un3QsS
https://wakelet.com/wake/P4ggvsl2zm55nPm670dls
https://wakelet.com/wake/H8g46rlfNn8hv1y02FClj
https://wakelet.com/wake/Tt-hhH0znERbU4Q8Qhcxw
https://wakelet.com/wake/7gjEUCn2E1mMJ8bvMEGcN
https://wakelet.com/wake/AP1MiQpZoHordZUVxUggk
https://wakelet.com/wake/xCpGXlPqIegqOalERcCbk
https://wakelet.com/wake/WMSNphz0PgohdxXYaqYMf
https://wakelet.com/wake/EFlwLxiOkFsd4uqMx1oY_
https://wakelet.com/wake/h7AD21H9UBwuTO8P5wBHp
https://wakelet.com/wake/HNmF6KZD-aty2EDKN36u5
https://wakelet.com/wake/NKQvyOaKHDdLu25s5WjnZ
https://wakelet.com/wake/uIamu3vwhaa_8whT4j7Dd
https://wakelet.com/wake/Acqd-LoPSh_YWxplIzwrx
sevrans (Monday, 24 January 2022 01:30)
sevrans 7383628160 https://wakelet.com/wake/tg-yhIknjC2KnDFg0dneY
https://wakelet.com/wake/ydQn1uw_L6A-KY0qBIpvQ
https://wakelet.com/wake/eultZw3mkdkFAIx8TNjc1
https://wakelet.com/wake/kNGmEvzy0Gb-1qHC-8pam
https://wakelet.com/wake/B26HV8fxF6jGQO1_iAsy3
https://wakelet.com/wake/HbxxAwncc7qXmNc3DXc0o
https://wakelet.com/wake/MQFAOfje3kRW_MtHFnDWo
https://wakelet.com/wake/MvPiK_0vAZcfBFwIJs1S3
https://wakelet.com/wake/uqRaZDsVcuSzfkWvF0B_3
https://wakelet.com/wake/1-AlwSgB3XObyF33cNfgk
https://wakelet.com/wake/IKlZ2LwT23NoTeeFEHxrT
https://wakelet.com/wake/pt5bcNNJ-ujhiSn9WAoXG
https://wakelet.com/wake/fBMRqWbtTirDVg2Y1hTwA
https://wakelet.com/wake/FpvT79N6YMZl9VAL_6frf
https://wakelet.com/wake/llWhfLCI_Ud5H1CdiBuvW
https://wakelet.com/wake/c4DkYStkRtEj0IJbMy8Uz
https://wakelet.com/wake/uUJ2c_u4Zdr8FDsoe0KoP
https://wakelet.com/wake/ynW4N96XmO5rvpiMNpkfw
https://wakelet.com/wake/YeG7OVK8quB3o5tRtjKiH
https://wakelet.com/wake/5axv21ReL2UPUHiyDWxBg
https://wakelet.com/wake/RGbHR_v1ef8Euo88VKdJ4
https://wakelet.com/wake/qzCk4qsq7_d3ozW-K6ggH
https://wakelet.com/wake/MwRtQkhzwG7HJcSP9VCwQ
https://wakelet.com/wake/PSfPoDp8bgHT_yzPQ1vvk
https://wakelet.com/wake/Afa2g8DpfX-Nn778-WeAV
https://wakelet.com/wake/ZQ4ojnpMXCAieqiS8pTS5
https://wakelet.com/wake/BEgem0kSC_YCriLDA_XV3
https://wakelet.com/wake/mQOHypVaS1H9XwvXA_-Ki
https://wakelet.com/wake/Bs7POgMjfgeCFTFG5rXOw
https://wakelet.com/wake/c2PdFMl9dxUkknZ_nVhim
farrwas (Monday, 24 January 2022 01:48)
farrwas 7383628160 https://trello.com/c/DWpTRcZW/14-earth-2160-access-code-keygen-crack-full
https://trello.com/c/kSbl08BB/39-windows-10-pro-rtm-build-10240-x64-pt-br-serial-key-wadyam
https://trello.com/c/sWLO8qui/49-film-on-dvd-cottage-entertainments-film-codedvd013
https://trello.com/c/m421r9U8/28-hd-online-player-sohrab-rustam-bangladeshi-movie-19
https://trello.com/c/NVVDTyuS/64-nero-12-platinum-greek-renndel
https://trello.com/c/BcMLJHbQ/53-acdsee-photo-studio-ultimate-2018-v111-crack-x64-download-xiaopepi
https://trello.com/c/IdVgoZGu/23-link-aces-of-the-luftwaffe-squadron-extended-edition-full-crack-portable
https://trello.com/c/t0VmVt4f/23-better-axife-mouse-recorder-full-version
https://trello.com/c/pzXftaqi/69-download-crystaldecisions-crystalreports-engine-version-102-36000-kaitnoel
https://trello.com/c/Qt59AHcu/40-better-a4deskpro-flash-website-builder-710-keygen-for-16
https://trello.com/c/zRLCV43J/44-raise-data-recovery-xfs-serial-better
https://trello.com/c/njeRZU4x/27-wysiwyg-web-builder-142-full-crack-techtools-download-pc-poskal
https://trello.com/c/69gwewyZ/28-better-patched-sony-products-multikeygen-v24-keygen-and-patch-only-read-nfo
https://trello.com/c/1fBYA8xa/38-verified-download-hollywood-wrong-turn-7-mp4-movie
https://trello.com/c/hCHe7PMu/46-link-aayirathil-oruvan-hd-full-movie-free-download
https://trello.com/c/nINzTa6k/26-sherdil-720p-movie-download-free-yedyini
https://trello.com/c/73MThtPs/19-install-hack-corel-website-creator-x7-1350-multilingual-crack-chingliu
https://trello.com/c/Ahw80iNp/38-portable-the-abyss-1989-br-rip-720p-movies-torrents
https://trello.com/c/WtqH05fa/57-easy-power-8-crack-free
https://trello.com/c/EYLsd7B1/66-hot-keygen-powershape-2018-key
https://trello.com/c/ltn8XfHX/35-xforce-keygen-inventor-professional-2013-32-bit-windows-7-exclusive
https://trello.com/c/kULgWE2x/45-gstabl7-with-stedwin-software-download-ulrysala
https://trello.com/c/qXIy7kAb/22-use-controller-with-desmume-free
https://trello.com/c/1WwPGlig/42-shellshock-live-v0976-pc-game-top
https://trello.com/c/mpOzSBrD/17-princess-sultanas-daughters-pdf-free-50-patpai
https://trello.com/c/cxKsdwv7/35-winpc-nc-download-crack-top-14
https://trello.com/c/JKXw1wzT/26-2021-bhikkhu-patimokkha-pali-pdf-download
https://trello.com/c/oxifMBFN/14-pluspunkt-deutsch-a1-arbeitsbuchpdf
https://trello.com/c/quRPWkI6/23-hot-examination-paediatrics-wayne-harris-pdf-free-download
https://trello.com/c/oBxXrFvJ/31-waveslib-80dll-aleeorno
emylsyd (Monday, 24 January 2022 02:06)
emylsyd 7383628160 https://coub.com/stories/3087822-naruto-shippuden-ultimate-ninja-storm-3-ps3-iso-torrent-2021
https://coub.com/stories/3082635-crack-dvdfab-v9-3-1-2-setup-patch-hot
https://coub.com/stories/3082633-audioship-key-serial-fanorla
https://coub.com/stories/3082631-wondershare-dr-fone-2020-crack-with-serial-key-for-windows-and-mac-henrrebe
https://coub.com/stories/3082630-hbm-ncode-2019-free-download-best
https://coub.com/stories/3082626-pablo-neruda-poems-in-malayalam-pdf-free
https://coub.com/stories/3082627-google-books-download-v301308-crack-elismar
https://coub.com/stories/3082625-cossacks-back-to-war-pc-iso-french-multi
https://coub.com/stories/3082622-gay-comics-handjobs-magazine-dad-s-bedtime-tales-volume-4-pdf
https://coub.com/stories/3082620-_best_-asphalt-8-windows-10-crack
https://coub.com/stories/3082621-verified-full-acdsee-v9-0-photo-manager
https://coub.com/stories/3082618-evergreensocialscienceguideclass10downloadpdf-melher
https://coub.com/stories/3082616-hd-online-player-movie-le-straordinarie-avventure-di-pinocchio-torrentgolkes-hot
https://coub.com/stories/3082615-crack-top-percussion-studio-v3-05
https://coub.com/stories/3082614-nahum-mendez-sanchez-gastroenterologia-pdf-17-top
https://coub.com/stories/3082611-idecad-7-statik-crack-ericvani
https://coub.com/stories/3082610-driver-wifly-city-20g-rar
https://coub.com/stories/3082607-silver-creek-falls-chapter-2-fixed
https://coub.com/stories/3082605-full-sap-ecc-6-0-software-free-download-full-versionl
https://coub.com/stories/3082603-updated-lrtimelapse-5-0-9-crack
https://coub.com/stories/3082604-hdd-regenerator-2011-serial-repack-keygen-torrent
https://coub.com/stories/3082601-link-ileap-telugu-typing-software-full-version-61
https://coub.com/stories/3082602-nfs-shift-2-unleashed-serial-number-for-activation-for-verizon
https://coub.com/stories/3082600-free-danda-neethi-sangrahaya-pdf
https://coub.com/stories/3082598-3dvista-floor-plan-maker-1-0-keygen-hot-generatorl
https://coub.com/stories/3082599-patched-miyawaki-sakura-photo-book-11
https://coub.com/stories/3082597-homeguard-8-9-2-crack-lasnes
https://coub.com/stories/3082595-cracked-history-of-subcontinent-from-712-to-1857-pdf-download
https://coub.com/stories/3082594-piriyadhavaramvendumtamilmovieextra-quality-freedownload
https://coub.com/stories/3082592-there-will-be-blood-2007-m-720p-mkv-600mb-yify-download-__full__
laveswa (Monday, 24 January 2022 02:42)
laveswa 7383628160 https://wakelet.com/wake/zzoc0eQykcghE45pNMudc
https://wakelet.com/wake/bqpgilgrG0IVO26TnMFOR
https://wakelet.com/wake/zENUYDNaUKkcNuDJahX_2
https://wakelet.com/wake/IAWWtQ7Eq8_FEBjfyBJEc
https://wakelet.com/wake/YWogM4dp0NNkQfhzy06xN
https://wakelet.com/wake/y2_FgRvNPXeR7uKIadupT
https://wakelet.com/wake/VCgjHY4waIpQWU3poDQug
https://wakelet.com/wake/XErEqcS5d8iEEuG-VCWNf
https://wakelet.com/wake/VC9KbFqq8XHb1iiBT7hgV
https://wakelet.com/wake/kyMqwEzU5OmH2kgw3uz9A
https://wakelet.com/wake/goRzt1_V_g1Ktb9FKHvM1
https://wakelet.com/wake/bQpJTpTi0SqAJTA6ACU7M
https://wakelet.com/wake/79JNsFT5IFw4DwCn3ot8X
https://wakelet.com/wake/JsYAjDr9LUzlxddCTBOTE
https://wakelet.com/wake/oY97pyRZ9P0t97-300HOM
https://wakelet.com/wake/K-WQYZ8-sABDGVZjLwI9h
https://wakelet.com/wake/bmSIopwgkom2k8Xn62UFC
https://wakelet.com/wake/8iA8jRuOMjqxeCQZTyI3a
https://wakelet.com/wake/dplwnccl-H9hKL1gHquLi
https://wakelet.com/wake/6jYpXtVrUOT--3AyGywZq
https://wakelet.com/wake/ZEIT-UKP6CgSZc5NqPqH_
https://wakelet.com/wake/AN60Qt1RRSJzr_RRWjZBA
https://wakelet.com/wake/8Fc03VX2OJC-FlZAlOt3l
https://wakelet.com/wake/8yEpX-vwTq-FB5HHPVTPM
https://wakelet.com/wake/o6OIiTxP6Z7SstGvQa9f1
https://wakelet.com/wake/SWNxWtQ6-gnb1ziJD4bgC
https://wakelet.com/wake/xnC-WA63aiW6CYiQyOe7D
https://wakelet.com/wake/-sAocI3INuVnmp6SjaHgP
https://wakelet.com/wake/KB8dm5nocZkRFle38O8X9
https://wakelet.com/wake/uoHVujA-sqnnPOcE9nvfI
candkae (Monday, 24 January 2022 03:00)
candkae 7383628160 https://trello.com/c/EFByGdFG/26-telecharger-methode-delavier-pdf-best-free
https://trello.com/c/voGdoZGK/66-exclusive-downloadhuruharaakhirzamanpdfviewer
https://trello.com/c/SaQKp394/17-clearview-rc-534-exclusive-keygen
https://trello.com/c/xx6iREAt/51-link-avatar-hd-tamil-movies
https://trello.com/c/mDg8o73s/42-mac-os-x-snow-leopard-1068-iso-torrent-trevhea
https://trello.com/c/5kwLsSJP/38-ansys-v14-win64-by-magnitude-exclusive
https://trello.com/c/ra6l7qyr/38-work-fsx-flightbeam-ksfo-san-francisco-int-v201-hack-offline
https://trello.com/c/RIh7w10K/32-top-manvi-ni-bhavai-by-pannalal-patel-pdf-download
https://trello.com/c/LoBrziDZ/23-cobalt-strike-full-version-46-elitiba
https://trello.com/c/UwkSpeQX/34-better-child-and-adolescent-development-book-by-brenda-corpuz-pdf-download
https://trello.com/c/u25Lt4UM/90-parker-2013-brrip-720p-x264-dual-audio-english-hindi
https://trello.com/c/yHhkvyhI/26-boarding-pass-garuda-pdf-26-paxtsoph
https://trello.com/c/IShFdoF2/47-top-shrek-1-dvdrip-download-movie
https://trello.com/c/bDZTXd3g/34-ingenieria-economica-thuesen-fabrycky-pdf-free-sadver
https://trello.com/c/ojrOR6D8/29-new-fm-2008-modifier-22-turkce-indir
https://trello.com/c/NnK33izZ/29-top-33-freeware-karaoke-mp3-g-toolz-serial-key-keygen
https://trello.com/c/DQq0xrwH/26-atnsoft-key-manager-keygen-13-jediman
https://trello.com/c/fmUgHnk0/29-rootpro-cad-6-professional-keygen-13-rashman
https://trello.com/c/MYf4RTXC/37-top-aayirathil-oruvan-full-movie-hd-1080p-download-videos
https://trello.com/c/68TEDodj/56-ninja-kuji-kiri-pdf-download-exclusive
https://trello.com/c/viSsMa8a/44-exclusive-running-man-download-episode-167
https://trello.com/c/GGNiH9Ht/49-geocadfullindir-emerbend
https://trello.com/c/u8GXoUsc/20-crack-per-solarius-pv-7-phifitz
https://trello.com/c/j0e0zfUN/31-new-crack-avanquest-partition-commander-117893-portable
https://trello.com/c/1lFxNkYD/14-easeus-data-recovery-wizard-13-crack-key-license-code-2019-fix
https://trello.com/c/EbkU81hP/29-geografie-graad-11-vraestelle-en-memorandums
https://trello.com/c/Z8wJRvWa/33-the-rascals-full-movie-hd-720p-top
https://trello.com/c/AYErRPKE/25-hot-xforce-keygen-64-bit-hsmworks-2019
https://trello.com/c/frGzBCPp/27-iobit-uninstaller-pro-93011-key-with-crack-better-latest-2020
https://trello.com/c/NwibYd6R/24-verified-thehousenextdoorhd1080pbluraydownloadtorrent
aloknow (Monday, 24 January 2022 03:19)
aloknow 7383628160 https://coub.com/stories/3030503-upd-download-easeus-data-recovery-wizard-professional-4-3-6-full-version
https://coub.com/stories/3030502-gp-pro-ex-3-5-serial-number
https://coub.com/stories/3030501-download-xf-adesk-2013-x32-150l-better
https://coub.com/stories/3030500-adobe-premiere-pro-cc-2019-13-0-1-best-crack-mac-osx
https://coub.com/stories/3030499-sparkbooth-4-serials-generator-keygen-__link__bfdcm
https://coub.com/stories/3030498-exclusive-transport-processes-and-separation-process-principles-geankoplis-downloadzip
https://coub.com/stories/3030497-work-serialkillersanatomiadomalpdf
https://coub.com/stories/3030496-winsuite-2012-full-top-download
https://coub.com/stories/3030494-blue-jay-studios-drum-sound-library-download-free-vanibevl
https://coub.com/stories/3030495-ek-haseena-thi-ek-deewana-tha-1-full-movie-in-hindi-free-exclusive-download-hd
https://coub.com/stories/3030493-loungelizardep4keygenmacdownload-stebir
https://coub.com/stories/3030492-jets-n-guns-game-full-updated-version
https://coub.com/stories/3030491-bejeweled-3-full-version-free-download-crack-windows-_top_
https://coub.com/stories/3030488-thetheconjuring2englishmoviemp4freedownload-wilmont
https://coub.com/stories/3030490-got-to-believe-in-magic-full-movie-free-full-downloadl
https://coub.com/stories/3030489-install-hd-online-player-fly-girls-720p
https://coub.com/stories/3030487-10musume-121314-01-azusa-sasaki-mp4-31
https://coub.com/stories/3030486-fixed-half-life-2-the-orange-box-no-survey-no-password-no-download
https://coub.com/stories/3030485-power-iso-5-6-final-keys-keyg-lz0-core-by-senzati-download-link
https://coub.com/stories/3030483-windows-8-1-magyar-64-bit-serial-key-keygen-ullhar
https://coub.com/stories/3030484-download-singles-vida-de-solteiro-11-nedlei
https://coub.com/stories/3030482-verified-me-tera-hero-full-movie-hd-free-download-utorrent
https://coub.com/stories/3030481-vbuc-lic-torrent-upd-download
https://coub.com/stories/3030480-photosculpt-textures-v2-pro-85-ingama
https://coub.com/stories/3030479-free-download-xxx-apartments-all-episodes-in-pdf-lavwak
https://coub.com/stories/3030478-best-assassins-creed-revelations-crack-only-v1-03-rar
https://coub.com/stories/3030475-__exclusive__-csr-bluetooth-4-0-driver-download-pc
https://coub.com/stories/3030477-programa-para-control-de-ciber-con-crack-pearula
https://coub.com/stories/3030476-new-financial-peace-university-workbook-pdf-64
https://coub.com/stories/3030474-excel-to-vcard-converter-drpu-crack-ojibmar
parkfyn (Monday, 24 January 2022 04:06)
parkfyn 7383628160 https://coub.com/stories/2938831-overture-music-visualization-download-2gb-raml-dwaitam
https://coub.com/stories/2938827-matlab-r2009a-activation-key-46
https://coub.com/stories/2938830-upd-call-of-duty-wwii-digital-deluxe-edition-repack-by-blackbox-crack-free
https://coub.com/stories/2938829-eddie-kramer-vst-plugins-free-17-exclusive
https://coub.com/stories/2938826-coolutils-total-mail-converter-6-2-0-53-keygen-patched
https://coub.com/stories/2938828-__exclusive__-beetle-crazy-cup-full-version-download
https://coub.com/stories/2938825-tanu-weds-manu-returns-in-hindi-720p-kickass-129311
https://coub.com/stories/2938824-designsoft-tina-8-0-pro-industrial-version-design-suite-rar
https://coub.com/stories/2938823-adobe-acrobat-reader-6-0-pro-free-download-top
https://coub.com/stories/2938822-xpadder-controller-images-only-full-version-best
https://coub.com/stories/2938821-sir-audio-tools-plugin-bundle-win-latest-free
https://coub.com/stories/2938820-tally-erp-9-in-gujarati-pdf-__hot__
https://coub.com/stories/2938819-konvensi-wina-1961-terjemahan-pdf-download-kallat
https://coub.com/stories/2938817-nfs-undercover-group2-cab-download-free-verified
https://coub.com/stories/2938816-acemoney-4-36-3-multilingual-serial-key-keygen-pasmik
https://coub.com/stories/2938815-pdf-reader-windows-7-download-elizjay
https://coub.com/stories/2938814-public-relations-strategies-and-tactics-11th-edition-downloads-torrent-patched
https://coub.com/stories/2938813-wii-naruto-shippuden-clash-of-ninja-revolution-4-iso-wii-download-repack
https://coub.com/stories/2938809-the-martian-english-part-1-dual-audio-eng-hindi-720p-torrent-exclusive
https://coub.com/stories/2938812-aircard-770s-unlock-code-olderaim
https://coub.com/stories/2938811-harrison-medicina-interna-edizione-italiano-pdf
https://coub.com/stories/2938810-hot-download-ice-age-3-full-movie-in-hindi
https://coub.com/stories/2938808-top-wow-hack-damage-3-3-5-download-file-gratis-rar
https://coub.com/stories/2938807-mac-osx-10-5-6-leopard-sl-dvd-41-liamalo
https://coub.com/stories/2938806-kbilling-software-with-crack-fre-quahai
https://coub.com/stories/2938805-full-crack-harmony-engine-evo-vst-v3022
https://coub.com/stories/2938804-janet-jackson-rhythm-nation-1814-repack-full-album-zip
https://coub.com/stories/2938802-adobe-photoshop-lightroom-classic-8-4-1-crack-2019-for-mac-windows-penlea
https://coub.com/stories/2938803-astute-graphics-plugins-keygenl-orioakl
https://coub.com/stories/2938800-install-iobit-software-updater-2-2-0-2729-with-crack
yelkae (Monday, 24 January 2022 04:37)
yelkae 7383628160 https://coub.com/stories/3126928-skm-power-tools-6-5-1-full-modules-5000-buses-with-crack-arabnim
https://coub.com/stories/3126927-depeche-mode-violator-2006-dts-5-1-audio-96khz-24bit
https://coub.com/stories/3126926-green-lantern-rise-of-the-manhunters-pc-fullversion-rar-quawall
https://coub.com/stories/3126925-upd-windows-loader-2-4-by-daz
https://coub.com/stories/3126924-reflector-6-6-rar-nichsoph
https://coub.com/stories/3126923-unlock-kakasoft-usb-copy-protection-51-new
https://coub.com/stories/3126922-ex4-to-mq4-decompiler-4-0-401-1-hot-cracked
https://coub.com/stories/3126921-rs-r75-download-krihar
https://coub.com/stories/3126918-free-720p-lolita-movies-download-verified
https://coub.com/stories/3126920-kasens-ks-g5000-drivers-download-better
https://coub.com/stories/3126919-charles-proxy-4-2-7crack-upd
https://coub.com/stories/3126916-you-may-ask-yourself-3rd-edition-pdf-hot
https://coub.com/stories/3126917-windowsembeddedposready7crackdownload-free
https://coub.com/stories/3126915-power-cd-g-player-pro-1-0-3-full-rar-link
https://coub.com/stories/3126914-classification-of-fungi-alexopoulos-and-mims-1979-pdf-27-high-quality
https://coub.com/stories/3126912-courselab-2-7-full-version-downloads-full-evavit
https://coub.com/stories/3126913-basic-electronics-bernard-grob-ebook-free-upd-download-pdf
https://coub.com/stories/3126911-simuride-home-edition-driving-simulator-free-58-top
https://coub.com/stories/3126910-va-bar-25-tage-ausserhalb-der-zeit-2012torrent-exclusive
https://coub.com/stories/3126909-download-driver-bcd2000-windows-10-_verified_
https://coub.com/stories/3126908-free-download-software-audioscore-ultimate-7-14-relpal
https://coub.com/stories/3126906-ajnabee-2001-hindi-720p-webhdrip-x264-aac-loki-m2tv-yaffwat
https://coub.com/stories/3126907-office-2010-toolkit-and-ez-activator-v2-1-7-64-bit-emelkari
https://coub.com/stories/3126905-cracked-smoke-shx-fonts-free-download
https://coub.com/stories/3126904-screensaver-virtuagirl-2-320-full-models-best
https://coub.com/stories/3126903-737-maintenance-training-cbt-download-exclusive
https://coub.com/stories/3126902-sonic-foundry-sound-forge-5-0-free-best-download-full-version
https://coub.com/stories/3126901-the-message-movie-in-hindi-hd-free-download-sauday
https://coub.com/stories/3126899-the-secret-life-of-pets-english-tamil-dubbed-download-updated
https://coub.com/stories/3126900-repack-download-buku-injil-barnabas-pdf-68
neilman (Monday, 24 January 2022 05:07)
neilman 7383628160 https://wakelet.com/wake/UYkiHSo29teyv1cB2LGx8
https://wakelet.com/wake/HhnFKxSmzcqzZZmD68AcK
https://wakelet.com/wake/_d_9QGxSey5cN8WUwjx6g
https://wakelet.com/wake/WPB-dPsB0TYOZ0NZZ7yEi
https://wakelet.com/wake/MYBGNs-VaBNkuFIHxwxt9
https://wakelet.com/wake/IuGoRg6l9XgkHZumzUkr1
https://wakelet.com/wake/jGCtbDn5fv1f0aP0mipGq
https://wakelet.com/wake/gV4De4EXRcrG6SHQF5xqQ
https://wakelet.com/wake/4AjSoFwNkrbTezyK6zj17
https://wakelet.com/wake/quxkwjpLSfBPJJZ7F5K2r
https://wakelet.com/wake/SL4IsyLsqYpaKOajkTn6X
https://wakelet.com/wake/7kj977Q0yyzbtWpd0zALI
https://wakelet.com/wake/MB3zI8XZB9xs3rNJXSM_0
https://wakelet.com/wake/FWcl9HovFSeFBmo2PmFti
https://wakelet.com/wake/z_BTauq-YIQm1b7XNa-3a
https://wakelet.com/wake/chmjq-Ump4yDIM4qSzSr2
https://wakelet.com/wake/AWDGUvGFYqxgWU6fJxBqG
https://wakelet.com/wake/1PyPMGmpwbXB0xwvyEM_M
https://wakelet.com/wake/YrnP5gEF0kYe1ok-4Ucxv
https://wakelet.com/wake/dbJ5insX9fsR1sp6K7WBD
https://wakelet.com/wake/8ZoGeryFBoHMtIiooHkMt
https://wakelet.com/wake/7XFLju_DrR6LgSho2MrOg
https://wakelet.com/wake/2BP65NNeVYfvef08Aw9Ve
https://wakelet.com/wake/DOfr1dPxl08WyZYlprNUl
https://wakelet.com/wake/uZ-FBIcX7dd3AFValgBPk
https://wakelet.com/wake/pxdhUAnQfP3t9xB4-T3CK
https://wakelet.com/wake/qV4ZQumoI16xHsbU-j09G
https://wakelet.com/wake/OhHqZczlRVWrM83a8EUsQ
https://wakelet.com/wake/KuaqwP_7hdpgr3cx1DK4P
https://wakelet.com/wake/tubmKLj1RaP-I_LLo2CLh
garytere (Monday, 24 January 2022 07:49)
garytere 7383628160 https://trello.com/c/piofIxfG/23-exclusive-el-arte-de-la-pasteleria-larousse-pdf
https://trello.com/c/ubyXqHbD/22-vice-versa-tarot-kit-mobi-download-book-patched
https://trello.com/c/ckjR2IQw/72-link-aim-master-hackl
https://trello.com/c/nspcA1Tj/75-movavipowerpointtovideoconverterwithcrack-warbeth
https://trello.com/c/nBgFffvo/26-exclusive-political-science-book-by-mazhar-ul-haq-pdf-download
https://trello.com/c/WYRCsg5l/40-the-dynamic-library-rlddll-failed-to-load-fifa-manager-13-11-rigale
https://trello.com/c/fDqoKdJ9/55-rise-of-nations-gold-edition-2007engrus-nd-skidrow-reloaded
https://trello.com/c/t88FWLCw/41-lg-flash-tool-crack-free-download-patched
https://trello.com/c/OOISif7N/24-gta-san-andreas-bucuresti-download-torent-new
https://trello.com/c/rtmULZF2/17-takken-7-full-cracked-2020-pc-game-free-download-new-copy-is-here-free
https://trello.com/c/UNIsSM1B/24-sky-go-account-generator-crack-installed
https://trello.com/c/ebIEq3sq/39-soukoku-no-arterial-cheat-engine
https://trello.com/c/70Yk2x48/45-link-emil-i-detektivi-knjiga-pdf-download
https://trello.com/c/LN0dwbZK/20-fix-vmware-esxi-55-license-key-14
https://trello.com/c/sHDdBWab/43-padri-konkani-film-songs-download-best
https://trello.com/c/zWIhF8Ps/13-extremelandingswindowscrack20-quynphe
https://trello.com/c/PM6RBUht/31-iskysoft-data-recovery-50-crack-serial-key-free-download-2020-repack
https://trello.com/c/ldZ7d6T5/56-full-navisworks-freedom-2017-download-hot
https://trello.com/c/NstF30wO/29-ds-icem-surf-2017-free-download-kaflsam
https://trello.com/c/GJ6WV6eO/18-stefan-okoniewski-technologia-maszyn-pdf-download-better
https://trello.com/c/VeQStBWt/20-piggery-projects-in-zimbabwe-pdf-39-free
https://trello.com/c/HVpdvr9z/32-top-dreamweaver-cs6-crack-amtlibdll-64-bits
https://trello.com/c/7vUnEFsR/26-best-spotmau-powersuite-golden-2012-keygen-109
https://trello.com/c/sYnzeW26/23-trapped-movie-in-hindi-free-download-720p-movies-exclusive
https://trello.com/c/zfP2a6Dz/67-como-descargar-gratis-stkeys2-guiexe-better
https://trello.com/c/7z0YuCx9/31-hot-top-7-prison-life-hacks-roblox-macosx
https://trello.com/c/bRsNueGJ/12-work-jewel-match-solitaire-download-crack-with-full-game
https://trello.com/c/KGZzVcpc/46-driver-mouse-benq-m800-p2m-better
https://trello.com/c/U6nGgkgn/50-chennai-vs-china-full-movie-in-hindi-720p-download-links-exclusive
https://trello.com/c/FI9JfkCC/32-illusion-download-key-serial-number-marroz
beytcre (Monday, 24 January 2022 08:19)
beytcre 7383628160 https://coub.com/stories/2976500-avast-pro-antivirus-2020-crack-exclusive-with-serial-keys
https://coub.com/stories/2976496-tenorshare-4ukey-1-6-4-3-crack-with-serial-key-licence-key-latest-version-2019-get-free-best
https://coub.com/stories/2976499-upd-pdq-inventory-18-1-38-0-enterprise-with-crack
https://coub.com/stories/2976498-3-minutes-to-midnight-a-comedy-graphic-adventure-torrent
https://coub.com/stories/2976494-idm-ultraedit-v19-00-0-1022-incl-keymaker-core-2021-full-version
https://coub.com/stories/2976495-ist-spring-design-software-crack-ingolis
https://coub.com/stories/2976492-exclusive-satanic-verses-in-hindi-pdf-free-download
https://coub.com/stories/2976491-daim-iqbal-daim-poetry-books
https://coub.com/stories/2976490-telecharger-windows-8-francais-iso-torrent-64-11-nobval
https://coub.com/stories/2976488-hot-football-manager-2020-crack-download-fm-2020-free-codex-mac-oswin-football-manager-2020-fr
https://coub.com/stories/2976486-work-download-magic-clothes-eraser-v-3-11
https://coub.com/stories/2976485-hd-online-player-download-jab-we-met-720pgolkes-vykifoen
https://coub.com/stories/2976484-track-attack-1996-by-heroskeep-zip-free-download-eletam
https://coub.com/stories/2976482-1000-soruda-malzeme-bilimi-pdf-63
https://coub.com/stories/2976480-hubeau-sonata-for-trumpet-pdf-free-lilllera
https://coub.com/stories/2976481-new-synapse-audio-orion-8-5-x32-keygen
https://coub.com/stories/2976479-charlotte-s-web-2006-full-movie-free-download-updated
https://coub.com/stories/2976477-wondershare-dr-fone-registration-code-link
https://coub.com/stories/2976475-free-indusoft-6-1-crack
https://coub.com/stories/2976472-woron-scan-2-10-radkalh
https://coub.com/stories/2976470-whatsup-gold-premium-v15-0-cracked-rar-hot
https://coub.com/stories/2976471-solid-edge-v18-full-link-version-free-download
https://coub.com/stories/2976469-henderson-jm-and-quandt-microeconomic-theory-pdf-rar-free
https://coub.com/stories/2976468-crack-new-ed-steam-installation-wizard-pc-game
https://coub.com/stories/2976466-atoll-rf-planning-tool-cracked-virnoe
https://coub.com/stories/2976463-fsx-just-flight-concorde-professional-torrent-aylgre
https://coub.com/stories/2976465-corel-drawings-6-pro-303-best
https://coub.com/stories/2976464-claveparaactivarfileviewprotaringa-birmich
https://coub.com/stories/2976462-best-codewarecompress7400crack18
https://coub.com/stories/2976461-link-a-koi-mil-gaya-full-movie-eng-sub-download
hanlokpa (Monday, 24 January 2022 08:50)
hanlokpa 7383628160 https://coub.com/stories/3089167-maya-2011-64-bit-download-top-torrent
https://coub.com/stories/3089163-upd-autotune-vst-t-pain-effect-17
https://coub.com/stories/3089166-_hot_-crack-wondershare-data-recovery-v3-0-2-incl-keymaker-core
https://coub.com/stories/3089159-blue-exorcist-movie-english-dub-free-__full__-35
https://coub.com/stories/3089158-repack-skull-facebook-hack-v2-2-by-dragma
https://coub.com/stories/3089155-commando-2-full-movie-in-hindi-hd-1080p-welyeny
https://coub.com/stories/3089156-truyen-tranh-luffy-vs-boa-hancock-xxx-sex
https://coub.com/stories/3089154-rppkeperawatansmkkesehatan-better
https://coub.com/stories/3089151-new-file-scavenger-4-3-keygen-11
https://coub.com/stories/3089149-sensiva-symbol-commander-software-free-__link__-download-for-windows-7l
https://coub.com/stories/3089147-high-quality-fable-3-pauldll-crack-116
https://coub.com/stories/3089148-best-simsarul-haq-hudavi-malayalam-speech-mp3-free-download
https://coub.com/stories/3089144-verified-download-film-nekromantik-2-torrent
https://coub.com/stories/3089146-tron-legacy-movie-better-download-dubbed-hindi
https://coub.com/stories/3089141-accurip-software-full-hot-crack-52
https://coub.com/stories/3089140-postbox-7-0-3-work-crack-with-serial-code-2019-free-download
https://coub.com/stories/3089138-omsi-2-download-cracked-apkf-linnjav
https://coub.com/stories/3089137-exclusive-bikini-kungfu-zip-rar
https://coub.com/stories/3089134-wii-mario-kart-7-iso
https://coub.com/stories/3089132-enervista-viewpoint-engineer-crack-new-cocaine
https://coub.com/stories/3089135-exclusive-linux-egalax-touch-screen-driver
https://coub.com/stories/3089133-windows-7-sp1-preactivated-x86-x64-multibrand-multiedition-iso-413230
https://coub.com/stories/3089131-medal-of-honor-allied-assault-breakthrough-expansion-torrent
https://coub.com/stories/3089130-hack-iobit-advanced-systemcare-12-pro-v12-0-3-192-crack-install
https://coub.com/stories/3089129-manhattan-gmat-books-pdf-free-download-6th-edition-chertall
https://coub.com/stories/3089128-link-wondershare-pdfelement-6-7-5-crack-macos-macosx
https://coub.com/stories/3089126-hot-torrent-architecte-3d-2013-ultimate
https://coub.com/stories/3089125-cree-en-ti-rut-nieves-pdf-117-sofbri
https://coub.com/stories/3089124-updated-biological-science-freeman-3rd-edition-pdf-download
https://coub.com/stories/3089123-khun-ploypailin-jensen-pictures-patsyan
cheryesi (Monday, 24 January 2022)
cheryesi 7383628160 https://wakelet.com/wake/yp5GOjZIknvJmFOEm330i
https://wakelet.com/wake/NeMivB3H9XbcPncKYx7pq
https://wakelet.com/wake/rBOIPqgX8nT2H6KyXFIWk
https://wakelet.com/wake/LY-u9klcxsvZusGxjsIah
https://wakelet.com/wake/lAodTTHHQhsjV7cf5OXi-
https://wakelet.com/wake/VRH9IOjCivsIBEEzYYuKL
https://wakelet.com/wake/_Xf0nXLcAoDtu1kQ1MAnA
https://wakelet.com/wake/xO7njLGwJTkGmUIa6-7dv
https://wakelet.com/wake/IuQa9d3_fiq7yx8iKpgUM
https://wakelet.com/wake/5nnjoCMGgfuiVHFXImmWl
https://wakelet.com/wake/Srn8osqKYlNUg0aMdbSnf
https://wakelet.com/wake/GcaKxT8LBwD-u4egErc40
https://wakelet.com/wake/wkSOpdeWeg4FLFSx9N7D-
https://wakelet.com/wake/S2k7htJ_6wwe2gz8AhsNS
https://wakelet.com/wake/6_wrLlsFEFVs-jev6v6os
https://wakelet.com/wake/863NYDFCRnHyxmLX1n_X3
https://wakelet.com/wake/gqgDfIH9oTOK7S3icJvAt
https://wakelet.com/wake/XuVO2rajHREtZsB_UpD4b
https://wakelet.com/wake/XE_EoeW2sz_Wjp49xQvsK
https://wakelet.com/wake/SL-SZjwwnMRKynchA_fjs
https://wakelet.com/wake/ozdfYyHLhSlTOPaefQNVz
https://wakelet.com/wake/y6oOFZzeE4hOqhsZJ-YQd
https://wakelet.com/wake/Mn55apj4sC3UUYEo4On7m
https://wakelet.com/wake/fbxxTvbhpySmG3GpXxUIc
https://wakelet.com/wake/RV1JdM0MeZ5K5mlWoi5av
https://wakelet.com/wake/2nI4qrWtxU9XNuowJ5897
https://wakelet.com/wake/cHd4u_04vtAokGKXGhPnh
https://wakelet.com/wake/-7ERsDRM22Fi-DnrJt1O2
https://wakelet.com/wake/ce7mkAUdftwaRE0M6ICwR
https://wakelet.com/wake/ngLJU4IdEy-czARK_IrPH
taijone (Monday, 24 January 2022 10:18)
taijone 7383628160 https://coub.com/stories/3002227-qamar-bani-hashim-patched-download-subtitles
https://coub.com/stories/3002224-link-originlab-origin-9-crack
https://coub.com/stories/3002223-ashampoo-mp3-cover-finder-__top__-full-13
https://coub.com/stories/3002221-st-studio-siberian-mouse-masha-and-veronika-babko-hard-slideshow-torrent-32-top
https://coub.com/stories/3002220-download-copy-protect-1-5-full-crack-winnyasm
https://coub.com/stories/3002218-kung-fu-panda-3-english-man-full-movie-download-new-in-hindi-dubbed-hd
https://coub.com/stories/3002217-rakta-charitra-1-telugu-movie-download-free-mobile-hot
https://coub.com/stories/3002215-life-of-pi-movie-free-download-in-english-mp4-hd-tawkes
https://coub.com/stories/3002214-keygenvehicletracking2019key-exclusive
https://coub.com/stories/3002211-planet-zoo-download-__exclusive__
https://coub.com/stories/3002162-shaadimeinzarooraanamovie1engsubdownload-__hot__
https://coub.com/stories/3002161-jabo-39-s-direct3d6-1-5-2-plugin-extra-quality-download-social-cahier-exerci
https://coub.com/stories/3002156-20-sim-crack-__full__-serial-28
https://coub.com/stories/3002146-globaldoorcloserr7483manual-upd
https://coub.com/stories/3002145-luminar-4-1-1-5843-crack-free-download-blansak
https://coub.com/stories/3002140-__full__-techsmith-camtasia-studio-9-0-0-build-1306-incl-serial-keys-serial-key
https://coub.com/stories/3002139-psikey-dll-corel-x5-free-download-updated
https://coub.com/stories/3002132-new-moscow-full-44-pthc-films
https://coub.com/stories/3002126-native-instruments-action-strings-kontakt-serial-key-keygen-exclusive
https://coub.com/stories/3002122-acrylic-wifi-professional-3-0-5770-30583-crack-b4tman-best-free-download
https://coub.com/stories/3002121-inmunologia-celular-y-molecular-abbas-8-edicion-pdf-download-patched-732
https://coub.com/stories/3002120-work-free-download-lumion-7-pro-full-software
https://coub.com/stories/3002116-chalo-dilli-full-movie-in-hindi-dubbed-free-download-hd-1080p-shaulri
https://coub.com/stories/3002115-ddos-program-warriors-battle-cannon-aka-loic-hot-download
https://coub.com/stories/3002112-link-scarface-discography-320-14-album
https://coub.com/stories/3002110-patched-dmc-devil-may-cry-all-dlcs-codex
https://coub.com/stories/3002108-windows-8-loader-activator-by-hazar
https://coub.com/stories/3002107-pokemon-black-white-2-official-guide-pdf-hot
https://coub.com/stories/3002106-st-studio-siberian-mouse-masha-and-veronika-babko-hard-slideshow-torrent-best-download
https://coub.com/stories/3002105-russian-flowers-blue-orchid-kdv-rbv-boysrar-free
rangdawn (Monday, 24 January 2022 11:15)
rangdawn 7383628160 https://trello.com/c/Veq2OL88/79-exclusive-google-maps-downloader-v6771-with-key-iahq76
https://trello.com/c/H2YyW7mZ/65-anatomageinvivo5fullfree-link
https://trello.com/c/oYn8apMy/22-torrent-04it-x7-connect-premium-europe-2013-new
https://trello.com/c/pJKW9Hs2/33-download-new-catia-v6-r2011-64-bit-windows-7-torrent
https://trello.com/c/arue1hn9/18-rijal-al-kashi-urdu-pdf-link-download
https://trello.com/c/DK6QfBlE/20-pasanga-2-hd-tamil-movie-free-download-top
https://trello.com/c/RTHXQ55z/39-full-iobit-uninstaller-pro-106012-crack-free
https://trello.com/c/yrZXV5CN/55-chemdraw-12-full-version-free-17-fixed
https://trello.com/c/IuyDQaPU/35-i-am-your-president-top-download-utorrent-kickass
https://trello.com/c/e7WF32HG/26-hot-malwarebytes-anti-malware-premium-4241015-final-keys-crack
https://trello.com/c/cedeAwgk/79-keygen-autodesk-2013-64-445-marreyn
https://trello.com/c/KqwdsIZ1/20-proteus-72-sp-2-portablerar-tercera-serial-esdla-orquesta-revistas-safety-better
https://trello.com/c/q2n3XYc2/25-windows-activator-for-all-versions
https://trello.com/c/qJsxy85g/38-download-software-tulisan-arab-untuk-komputer-terbaru-janetan
https://trello.com/c/BdhoVeGs/79-install-rocket-mania-deluxe-activation-code-addons
https://trello.com/c/G9Rdb0Ms/26-hd-online-player-kandasamy-tamil-movie-download-37-horigavr
https://trello.com/c/sIlox8lS/12-better-coreldraw-x4-torrent-by-r0by90-working-keygen-rar
https://trello.com/c/u2ZBIzZg/55-freeshreelipi60fullwithcracknewversion-top
https://trello.com/c/rLJBNnHY/14-rd-sharma-class-12-ebook-free-hot-download-pdfl
https://trello.com/c/eBrrWrb5/31-the-operational-art-of-war-iv-key-serial-number-zesulm
https://trello.com/c/OZwrquYc/40-bomberman-jetters-iso-ps2-quialb
https://trello.com/c/5gI6Glbs/8-avs-audio-editor-912540-with-crack-best
https://trello.com/c/7unmE0JK/17-battlefield-bad-company-2-no-cd-crack-gamecopyworld-gaylaqu
https://trello.com/c/NbcdQifB/16-akai-lpd8-virtual-dj-mapper-downloadl-gilkar
https://trello.com/c/G2148w0R/40-hot-goynar-baksho-720p-free-download
https://trello.com/c/7Gq6XvfI/37-better-need-for-speed-movie-hindi-audio-track
https://trello.com/c/lPAoevT7/16-virtualrig-studio-3-0-crack-freeed
https://trello.com/c/el24EXCO/24-malattie-infettive-moroni-pdf-90-rafsel
https://trello.com/c/s6SRyNvO/66-descargar-audaces-7-para-windows-7-download-completo-exclusive-crack
https://trello.com/c/WsdrSJ8U/90-renault-consult-irisbusl-upd
georivan (Monday, 24 January 2022 11:44)
georivan 7383628160 https://coub.com/stories/3052233-dvd-profiler-keygen-repack-crack-serials
https://coub.com/stories/3052232-avg-pc-tuneup-2015-15-0-1001-604-final-multilingual-keygen-golddaya
https://coub.com/stories/3052230-rd-supekar-computer-science-pdf-link
https://coub.com/stories/3052228-download-best-windowsxpsp3litenetbookeditionisoita
https://coub.com/stories/3052227-top-hacktivator-for-windows-7-download
https://coub.com/stories/3052226-passcape-reset-windows-password-keygen-download-work
https://coub.com/stories/3052224-2021-hd-online-player-death-note-720p-nyaa-torrent
https://coub.com/stories/3052225-kungfupanda1movieinhindidownload-better
https://coub.com/stories/3052222-top-rated-license-standalone-dat-matlab-r2012a
https://coub.com/stories/3052220-new-plexearthtoolscrackserialkeygerar
https://coub.com/stories/3052219-xactimate-25-1-64-bit-full-version-35-top
https://coub.com/stories/3052216-windows-7-uloader-8-0-0-0-x86-and-x64-by-orbit30l-repack
https://coub.com/stories/3052213-hd-online-player-download-movies-in-720p-yeh-jawaani-hot
https://coub.com/stories/3052214-hot-download-mp3-lagu-pop-indonesia-tahun-70an
https://coub.com/stories/3052212-better-c2950-i6k2l2q4-mz-121-22-ea12-bin-epub
https://coub.com/stories/3052211-ecpe-honors-teacher-s-book-answers-1083
https://coub.com/stories/3052207-wrc-3-serial-code-free-__hot__
https://coub.com/stories/3052205-crack-free-para-sims-3-vaya-fauna-pc
https://coub.com/stories/3052204-hot-wintopo-pro-license-keygen-36
https://coub.com/stories/3052203-activation-dll-fifa-14-download-top
https://coub.com/stories/3052201-office-2010-toolkit-v2-01-7z-checked-_best_
https://coub.com/stories/3052200-deutschland-spielt-unwrapper-exe-updated-link
https://coub.com/stories/3052199-analogue-a-hate-story-torrent-portable
https://coub.com/stories/3052198-hack-adobe-photoshop-cc-2018-24-1-1-42098-crack-new
https://coub.com/stories/3052196-robokill-2-full-version-free-verified
https://coub.com/stories/3052195-fixed-aomei-partition-assistant-download-8-2-crack-serial-key-2019
https://coub.com/stories/3052193-xlive-dll-mortal-kombat-arcade-kollection18-hot
https://coub.com/stories/3052191-atomic-mail-verifier-v3-1-portable-full-version-benyitz
https://coub.com/stories/3052190-selection-professional-20-free-download-hettich-link
https://coub.com/stories/3052189-link-kode-aktivasi-windows-7-ultimate
lovyquit (Monday, 24 January 2022 12:12)
lovyquit 7383628160 https://wakelet.com/wake/wTqgpGglHbpdGD52FW54C
https://wakelet.com/wake/-RK5Z9Uw8i3je4EbKS7nX
https://wakelet.com/wake/5kGzlWDpeyklILTh2ucpn
https://wakelet.com/wake/KmdmQuq0ZUhy8zPUJkSMw
https://wakelet.com/wake/X6cN0lKAxy-BawNjZMzk4
https://wakelet.com/wake/0zVPuEPJ3CjAmFv4FPQR1
https://wakelet.com/wake/uSkplKgd5e_jstbTj3EY0
https://wakelet.com/wake/GH3uqR1TmhoV3bYxgdy9t
https://wakelet.com/wake/3QBBXSZK4mlNwETTmqx0j
https://wakelet.com/wake/WYGElwWjpJnZKfbkBPKWF
https://wakelet.com/wake/FWgf2a4_gakvO7n07kAxz
https://wakelet.com/wake/u1zBdP9MaZGOBtdAWI4os
https://wakelet.com/wake/dqb140HS8fHH9Qk2bKvQ8
https://wakelet.com/wake/Y8boxp7KcoM3KJtzOcioy
https://wakelet.com/wake/YcSJOQK6RlLkRcfOT_wKG
https://wakelet.com/wake/d1H9P-E1rdNfyDH0S0WuV
https://wakelet.com/wake/a05qKV7VPUIPjyyG0Xfvz
https://wakelet.com/wake/PYxY9aYKMfMWJrcPyYwol
https://wakelet.com/wake/T8IUKBOvc-46YUtlwgfnf
https://wakelet.com/wake/rjMKkmUz-hzugZhseQ1Uu
https://wakelet.com/wake/l-s_Rr00wBghpslzaaR4c
https://wakelet.com/wake/OO17qslE7FrjB3gb-Ab_S
https://wakelet.com/wake/mglycdpbCB24uJ9tn4pag
https://wakelet.com/wake/O9iQ2bb4TpT4LaoWYlBon
https://wakelet.com/wake/x3SnNfdTrch4tJMktRXTx
https://wakelet.com/wake/IV2af7freaMl1KnqAC8bh
https://wakelet.com/wake/AVMor-ALnDxPLNL3RlMAn
https://wakelet.com/wake/BV0Y3v2cvgD1a02aT5Dnc
https://wakelet.com/wake/3-uMueVI4tU_aVCMBmPB9
https://wakelet.com/wake/P4qZSop2i1TqgyYZbErkO
bermod (Monday, 24 January 2022 12:41)
bermod 7383628160 https://trello.com/c/atnbRUvZ/43-sales-and-distribution-management-by-krishna-k-havaldar-pdf-150-extra-quality
https://trello.com/c/WSJCi0kL/52-fisica-alonso-acosta-tomo-2-sademma
https://trello.com/c/D9AAb82s/61-train-dispatcher-35-password-crack-ivolaur
https://trello.com/c/vEVuPqZF/76-imacros-enterprise-edition-v1205016698-x86-full-version-xireeldr
https://trello.com/c/5uuEF8wr/75-l-essenziale-di-economia-pdf-11-palmelea
https://trello.com/c/yGy01CEH/39-solucionario-treybal-segunda-edicion-alisfeat
https://trello.com/c/Ptwi2lRY/54-hp-cpc-p-n-466808-002-wireless-lan-drivers-garydel
https://trello.com/c/a9ihaKC2/30-better-users-choice-fundamentals-of-electric-drives-by-gk-dubey
https://trello.com/c/HxzPgWuH/31-best-dvb-dream-crack-24b-herbicide
https://trello.com/c/PWHDtfoj/15-download-password-here-http-filesmy-com-file-03d3a4-latoalez
https://trello.com/c/l35jyA5p/36-terjemahan-kitab-mantiqpdf-link
https://trello.com/c/Z8m1cM8I/24-gran-turismo-6-pc-download-hot-torrent
https://trello.com/c/82QP3JR7/34-upd-talisman-desktop-3-4-crack
https://trello.com/c/M8LciSyg/18-loopmasters-bass-master-100317-vsti-x64-serial-key-hairilla
https://trello.com/c/kK4nwwcO/22-new-rhinoworks-download-crack-for-gta
https://trello.com/c/coG3y53S/26-windows-xp-titanium-sp3-iso-french-torrent-kickass-torrent
https://trello.com/c/LHHhDMne/29-yeto-vellipoyindi-manasu-movie-free-download-in-utorrent-hot
https://trello.com/c/nPGdL7fA/27-revealer-keylogger-pro-edition-keygen-xylokay
https://trello.com/c/y4UY6MpK/56-operating-systems-gary-nutt-3rd-edition-hot-free-download-zip
https://trello.com/c/t5UkRb2I/46-hot-nitro-pro-v85314-x64-with-key-tordigger-download-pc
https://trello.com/c/q4ghH7dp/31-mic-office-2016-professional-plus-visio-pro-project-pro-16046781000-x86-crack-catlnaz
https://trello.com/c/YZWGir8P/85-almediadev-stylecontrols-388-shayfai
https://trello.com/c/Sx4O2ysl/87-business-plan-pro-premier-v12-2021-crack
https://trello.com/c/RN3jzpPl/63-creative-drivers-ct4750-sound-card-zip
https://trello.com/c/DWelpWMm/39-norton-internet-security-2018-258129-trial-reset-crack-work
https://trello.com/c/KJ8AYM7R/43-opel-vauxhall-epc-4-032013-multilanguage-torrent-link
https://trello.com/c/uPIKzbV1/55-endnote-x7-windows-crack-torrent-riplpayn
https://trello.com/c/vm1IUgb1/53-mobile-suit-gundam-0079-torrent-full-download
https://trello.com/c/yjBudxuj/73-valkyrie-full-movie-in-hindi-dubbed-exclusive-download-movies
https://trello.com/c/DBqbqDJW/92-exclusive-pilsner-urquell-game-free-download-for-13
tamcre (Monday, 24 January 2022 13:37)
tamcre 7383628160 https://wakelet.com/wake/_8RXZfqs9AOjwSUWaZJSd
https://wakelet.com/wake/XRh-YvFo5KZLStUAb-goa
https://wakelet.com/wake/Yv6iojDH1eDhdmKITPuan
https://wakelet.com/wake/-yn2zWFaIcB1kuGq_JA2f
https://wakelet.com/wake/bEOC5D8leYK97q-n5xpMh
https://wakelet.com/wake/KbraBJ1ADHtSqj8jbXWTf
https://wakelet.com/wake/3vSk2H6Ee3XZNBoEOgIbC
https://wakelet.com/wake/aI5Xdf2z5MAkufZBZjDEn
https://wakelet.com/wake/B3dL5mNPj9W8w5DA08r1F
https://wakelet.com/wake/drkD7UnJ_pudmdJsTsnUL
https://wakelet.com/wake/8QchcoqRHmk8kb98Ox6kZ
https://wakelet.com/wake/9RgdhMGCsL4ZdXybLU5ll
https://wakelet.com/wake/FdaupaxGUfS45yIHc_Q_M
https://wakelet.com/wake/3YxNLSKrm4kyDGsYq6xyd
https://wakelet.com/wake/0oiRoI8EzPSQjQ84I8dWU
https://wakelet.com/wake/1Z9o7atRN3VJ3XAw-cHqG
https://wakelet.com/wake/cPWTu4Eit6GGlcJJtTMov
https://wakelet.com/wake/W5uOIsCGg6gKlZRJrEjkI
https://wakelet.com/wake/3FGlv4h7q0U2LOp2RLYJk
https://wakelet.com/wake/dlZtxEZfGsKdQmTCtJLnE
https://wakelet.com/wake/RoTWyO3NE0Q0Lr9vdmHzY
https://wakelet.com/wake/d4mwWOPqMACVKgJHt5BIL
https://wakelet.com/wake/OmKHQV9Qz0XxMTxTCfCG7
https://wakelet.com/wake/D8Xox8dXrxwj7anLTQxfk
https://wakelet.com/wake/KPHnvpIEknOqsCzhF4v0X
https://wakelet.com/wake/O1WKvaRROQuQsUQfT1X8k
https://wakelet.com/wake/qKphMozMqIMsSmtxILiPy
https://wakelet.com/wake/R07GZR5yOlrmrAcroW5rm
https://wakelet.com/wake/JgoPpWjZW0lJIrTK6fzwV
https://wakelet.com/wake/acJhfmX0HdtkHYBDNqQg3
vladfabr (Monday, 24 January 2022 16:45)
vladfabr fe98829e30 https://coub.com/stories/3018960-backupbc01-exe
https://coub.com/stories/3018961-smart-pc-care-keygen-install-generator
https://coub.com/stories/3018962-libro-conceptos-basicos-de-quimica-sherman-pdfl-updated
https://coub.com/stories/3018963-dawn-of-war-2-skill-points-cheat-full
https://coub.com/stories/3018964-havit-usb-joystick-driver-hv-g61-13
https://coub.com/stories/3018965-fixed-hd-online-player-life-is-beautiful-in-hindi-movie-du
https://coub.com/stories/3018967-sam-broadcaster-4-2-2-serial-crack-424-exclusive
https://coub.com/stories/3018968-3d-frog-frenzy-download-windows-7-patched
https://coub.com/stories/3018971-windows-8-ultimate-64-bit-iso-free-download-iso-work
https://coub.com/stories/3018970-top-38-dictionnaires-et-recueils-de-correspondance-avec-crack-gratuit-telecharger
https://coub.com/stories/3018972-eurosport-player-crack-free
https://coub.com/stories/3018974-link-ucancam-v9-dongle-crack-software
https://coub.com/stories/3018975-jung-und-frei-magazine-photos
https://coub.com/stories/3018976-introduction-to-solid-state-physics-by-m-a-wahab-hildai
https://coub.com/stories/3018977-free-download-irender-nxt-for-sketchup-8-full-version-laurtier
https://coub.com/stories/3018979-wifi-hacker-wep-by-lukinha-rar
https://coub.com/stories/3018978-cadprofi-9-07-keygen-crack-marlwan
https://coub.com/stories/3018982-best-investment-banking-study-material-pdf-free-download
https://coub.com/stories/3018983-exclusive-arcsde-windows-102-134940-iso
https://coub.com/stories/3018984-_best_-network-inventory-advisor-42-crack-serial-keygen-76
https://coub.com/stories/3018985-concierto-en-la-llanura-partitura-pdf-free-roelqua
https://coub.com/stories/3018988-hd-online-player-hum-saath-saath-hain-movie-free-top-download-1080p
https://coub.com/stories/3018989-abigaile-johnson-dog-hot
https://coub.com/stories/3018992-telecharger-logiciel-de-piratage-facebook-gratuit-torrent
https://coub.com/stories/3018990-dvdvideosoft-free-2021-studio-5-0-3-serial-keygen-423
https://coub.com/stories/3018991-cheat-room-skyrim-nexus-better
https://coub.com/stories/3018995-best-smart-battery-workshop-3-71-keygen-full
https://coub.com/stories/3018999-the-financial-expert-pdf-exclusive-download
https://coub.com/stories/3018997-jodi-no-1-movie-in-hindi-free-download-720p-zeryyesi
https://coub.com/stories/3034101-gayle-forman-apenas-um-ano-pdf-download-shandeve
irviwai (Monday, 24 January 2022 18:08)
irviwai fe98829e30 https://coub.com/stories/3004788-aayirathonnu-ravukal-pdf-wilekie
https://coub.com/stories/3004786-best-crack-all-bigfish-popcap-reflexive-alawar-gamehouse-games
https://coub.com/stories/3004784-moonvrvideoplayertorrentdownload-marikaml
https://coub.com/stories/3004783-top-kumpulan-soal-dan-pembahasan-fisika-kelas-11-semester-2-doc
https://coub.com/stories/3004780-download-goldwave-5-67-full-work-crack
https://coub.com/stories/3004779-son-of-sardaar-hd-1080p-movies-free-download-chrimis
https://coub.com/stories/3004776-exclusive-nero-8-ultra-key-gen-8-2-8-0-serial-key-keygen
https://coub.com/stories/3004775-pes-topbg-e-2-sfd-pes-2013-rar
https://coub.com/stories/3004774-http-rghost-ru-users-opus87-releases-link1-hit
https://coub.com/stories/3004773-full-abbyy-finereader-12-0-101-264-professional-chingliu-holmari
https://coub.com/stories/3004772-download-c-kkompany-full-full-movie-720p
https://coub.com/stories/3004771-danko-jones-discography-19992010rarrar-paytingr
https://coub.com/stories/3004768-autodesk-whip-64-bit-cazzjann
https://coub.com/stories/3004767-adobe-photoshop-elements-12-crack-only-otsokii
https://coub.com/stories/3004766-link-8x10-tasveer-3-movie-download-720p
https://coub.com/stories/3004762-cdma-workshop-v3-4-1-demo-rarl-top
https://coub.com/stories/3004761-eric-helms-the-muscle-and-strength-pyramid-nutrition-v1-0-1-pdf-bamaysh
https://coub.com/stories/3004759-test-drive-unlimited-ps2-free-download-completo-torrent
https://coub.com/stories/3004756-malwarebytes-3-7-1-crack-serial-key-full-free-download-link
https://coub.com/stories/3004755-gorillaz-plastic-beach-deluxe-version-itunes-lp-zip
https://coub.com/stories/3004752-verified-solucionario-vibraciones-mecanicas-rao-pdf-207
https://coub.com/stories/3004751-3d-flash-yosino-full-collections-jusrand
https://coub.com/stories/3004750-exclusive-rg-mechanics-gta-5-crackl
https://coub.com/stories/3004749-bukuulumulhaditspdfdownload-top
https://coub.com/stories/3004747-_verified_-meteorologia-e-oceanografia-paulo-roberto-valgas-lobo-36
https://coub.com/stories/3004745-minecraft-nitrado-server-welt-downloaden-nisgiu
https://coub.com/stories/3004744-devart-unidac-pro-7-1-4-xe8-beriln-d10-2-tokyo
https://coub.com/stories/3004743-wwe-wrestlemania-29-full-show-hd-free-download-extra-quality
https://coub.com/stories/3004741-macgo-mac-blu-ray-player-pro-3-3-better
https://coub.com/stories/3004739-install-tastech-z-44-webcam-driver-rar
lavoto (Monday, 24 January 2022 18:56)
lavoto fe98829e30 https://wakelet.com/wake/EPJH2KVSslGaQvNO73J7o
https://wakelet.com/wake/2W-vG0VAqhyDiupP5zawl
https://wakelet.com/wake/i4-E9dR6NznghffW-U8bf
https://wakelet.com/wake/gLefv04NMBZggNOlH3vfq
https://wakelet.com/wake/_GBXKwj-5P0Lr0cNU0W_k
https://wakelet.com/wake/r-AlcKg5-dF9DAuI4EMkl
https://wakelet.com/wake/JGuN-C2RbVl7jSX0rKHCT
https://wakelet.com/wake/e9Il7d3y5u8iWw--QZwXy
https://wakelet.com/wake/3PzgHjI7mt9ZJv6PlZNYH
https://wakelet.com/wake/-2ypr5J7lvkPWVeWmIEVW
https://wakelet.com/wake/ZbWeT6KQmppADU55KECPF
https://wakelet.com/wake/ybncTTiOQ86vSnEjHg0Jz
https://wakelet.com/wake/Gp1xb38oGVJOec1DAq99J
https://wakelet.com/wake/Rido4Hm0gcXZ9YCFmzcyC
https://wakelet.com/wake/K2UJaypPO7U1ep1cc2q8M
https://wakelet.com/wake/1QwrmhG6-4kJtPxMpXeGh
https://wakelet.com/wake/d2usB4h4_RAuHLAUEHQAs
https://wakelet.com/wake/gnOKJ9mOTHVP0WjFYc1nb
https://wakelet.com/wake/BRb-eo2QA_f2tvVZwqBBq
https://wakelet.com/wake/aUgGTmOFJeCiv_tzrwWRp
https://wakelet.com/wake/UzJSNtNle2pv1V_5KBXtf
https://wakelet.com/wake/G7CJfJHu4lQYulz0sXmiG
https://wakelet.com/wake/gdMRXYmM0f-6GKmp_cUoa
https://wakelet.com/wake/mwZbF9WObpac81r1kM5Bi
https://wakelet.com/wake/3ocv4sPX54busi2IaYNQF
https://wakelet.com/wake/0Xm6geCvk2Gq0zzSFDJ5-
https://wakelet.com/wake/j1pHVGKUBlopoP_iEdsKN
https://wakelet.com/wake/-THjXQqFLVMDj_44fStHH
https://wakelet.com/wake/laFq8Mo2nW9ACRdawoVS2
https://wakelet.com/wake/SdjnCSOR1gmZl6qzNcGCb
marvir (Monday, 24 January 2022 20:31)
marvir fe98829e30 https://coub.com/stories/2988149-photoinstrument-7-6-build-922-keygen-cracksnow-download-pc-__exclusive__
https://coub.com/stories/2988147-videopad-video-editor-8-04-crack-__link__-registration-code-2020
https://coub.com/stories/2988148-verified-baaria-torrent-ita-1080p
https://coub.com/stories/2988145-chew7-v1-2-hot-crack-windows-7-sp1
https://coub.com/stories/2988144-nero-startsmart-8-free-download-for-windows-7-best
https://coub.com/stories/2988143-dirt3skidrowcrack-repack-onlythegame
https://coub.com/stories/2988139-corel-draw-free-download-full-version-with-crack-for-windows-8-jarebon
https://coub.com/stories/2988142-download-trnsys-cracked-full-software-link
https://coub.com/stories/2988141-ko-windows-7-ultimate-k-x64-dvd-x1565970iso-kaleyose
https://coub.com/stories/2988140-roxy-music-complete-studio-recordings-rar
https://coub.com/stories/2988138-best-gvox-encore-v5-0-0-air-rar
https://coub.com/stories/2988136-film-si-doel-anak-sekolahan-112-__exclusive__
https://coub.com/stories/2988137-download-principle-of-marketing-kotler-power-point-all-chapter-pdf-link
https://coub.com/stories/2988135-ableton-live-10-1-6-link-crack-plus-full-keygen
https://coub.com/stories/2988134-starcraft-2-collector-s-edition-content-torrent-ileemm
https://coub.com/stories/2988133-codigo-para-solid-converter-pdf-keygen-whirose
https://coub.com/stories/2988132-billoo-comics-in-hindi-free-download-pdf-wynedar
https://coub.com/stories/2988131-7-data-recovery-3-0-crack-download-portable
https://coub.com/stories/2988130-mu-auto-combo-hack
https://coub.com/stories/2988129-hot-crack-quick-devis-enterprise
https://coub.com/stories/2988128-men-in-black-3-2021-full-movie-in-hindi-dubbed-download-hd
https://coub.com/stories/2988127-best-feuerwehr-simulator-2010-download-free
https://coub.com/stories/2988126-ethnic-flute-phrases-kontakt-valechan
https://coub.com/stories/2988123-__full__-peskha-chess-lessons-courses-pack-2013-multi-standalone-version-download
https://coub.com/stories/2988124-telecharger-le-destin-de-lisa-saison-1-garmcou
https://coub.com/stories/2988122-artcam2018crackxforcekeygenadobe-waitorc
https://coub.com/stories/2988120-hot-sud-sound-system-the-best-of-2002-2012-download-torrent
https://coub.com/stories/2988119-2021-ivt-bluesoleil-10-0-417-0-x86-x64bit-patch-included-mafiasss
https://coub.com/stories/2988118-rhythm-rush-free-download-melvich
https://coub.com/stories/2988117-windows-10-redstone-5-12in1-x64-en-us-nov-2018-generation2-64-bit-top
onenjas (Monday, 24 January 2022 21:17)
onenjas fe98829e30 https://trello.com/c/cZQboLzR/50-zend-guard-55-full-crack-darmare
https://trello.com/c/tfbLfkVs/17-the-specified-service-does-not-exist-as-an-installed-service-0x80070424-lateog
https://trello.com/c/KlFUWNAv/85-link-motorola-r2600-service-manual-rar
https://trello.com/c/uzBzacw3/24-dreambox-dm500-gemini-image-4-70
https://trello.com/c/C7RpGKlC/15-ok-kanmani-movie-with-english-subtitles-161
https://trello.com/c/V4bj79JS/50-vst-plugins-for-nuendo-4-torrent-download-dawncarr
https://trello.com/c/wezMogLN/39-hot-all-tamil-fonts-free-download
https://trello.com/c/VjtcxAfW/37-top-airport-madness-4-full-version-crackl
https://trello.com/c/ntVzLK5l/83-senran-kagura-estival-versus-ayame-activation-crack-link
https://trello.com/c/o3B4vTXv/22-new-azov-films-boy-fights-10-even-more-water-wiggles-part14
https://trello.com/c/t0zircpA/30-como-instalar-dmelect-2010-para-windows-7
https://trello.com/c/wEksYxnl/36-top-plants-vs-zombies-garden-warfare-cracked-pc
https://trello.com/c/J7AJkqXV/14-petit-robert-electronique-dictionnaire-iso-torrent-monova
https://trello.com/c/8hJh64qV/50-hd-online-player-dabbe-curse-of-the-jinn-exclusive-full-movie-4
https://trello.com/c/jcTb596Q/28-abbyy-finereader-90-professional-edition-activation-code
https://trello.com/c/1XT6Rkoi/32-hot-wondershare-uniconverter-1121-crack-with-serial-number-free-download-2019
https://trello.com/c/KM0n9HB9/27-ekk-deewana-tha-full-movie-in-hindi-720p-torrent-new
https://trello.com/c/fjQ0ikfL/25-verified-gapps-hypptv-zipepub
https://trello.com/c/1UsILedq/47-platoonmovieinhindidownload-free
https://trello.com/c/TNGEh9kr/31-simplecast-v310-inclcrackrarrar-maslava
https://trello.com/c/sKeJVuqq/36-anselmoralphdiscografia2005-2012192mbficheirosmp3128kbpsvpj-3000musicaangolana
https://trello.com/c/7yB5LN1d/92-nfs-rivals-black-screen-fix-crack-free
https://trello.com/c/nwsCYe6O/45-payg-ambarlar-tarixi-pdf-download-top
https://trello.com/c/Aj7XSCiN/34-sound-blaster-x-fi-mb3-serial-key-crack-full
https://trello.com/c/NeQ7TmnC/39-deep-freeze-standard-853-crack-with-license-key-full-version-zachpayt
https://trello.com/c/GR5EIenL/38-solucionario-dinamica-meriam-3-edicionrar-dejarock
https://trello.com/c/Vr6v5MD7/31-exclusive-crack-cambam-plus-v09846
https://trello.com/c/wRaE9aaT/30-patched-ip-man-3-full-movie-download-mp4
https://trello.com/c/YLI9NYci/34-horosoft-professional-edition-40-hindi-crack-portable
https://trello.com/c/pqlJzUVC/27-autocad-2007-crack-exe-file-accoinve
raydavi (Monday, 24 January 2022 22:04)
raydavi fe98829e30 https://wakelet.com/wake/QvjwCQwi9sFDZMy44BZMO
https://wakelet.com/wake/S8CefVi0OwNGkyPP-XQYI
https://wakelet.com/wake/AjA-7gtnFp40MNE0psOfS
https://wakelet.com/wake/ALgUcqoHoS81dhJzY_Wdi
https://wakelet.com/wake/bjX9Xy3A6vpVnLakLfAna
https://wakelet.com/wake/P5P4FMWzON26PqFu1UnHw
https://wakelet.com/wake/jMCMGh5XryMPZGY5gLW5Y
https://wakelet.com/wake/0oCWHM9TnoqI1ltKurhn6
https://wakelet.com/wake/NBigXt9AlAFFd4Q-QbjY9
https://wakelet.com/wake/joRBi4HhajVrPhKU9075e
https://wakelet.com/wake/gxqDO5aci0q8Ee7JvjzUc
https://wakelet.com/wake/3XA_PT3V9XTZP03QjqOCW
https://wakelet.com/wake/sMfPYPVHkmldpyJCNMEAl
https://wakelet.com/wake/1Q5lzpyea86fgVqPHrDuE
https://wakelet.com/wake/Q-4OyHE7I2-Dg0_p2ftSi
https://wakelet.com/wake/ugsPwfMQSJA5lM1j1JjEI
https://wakelet.com/wake/LoMpFLRt2htUzICThQjsA
https://wakelet.com/wake/I0Hwzbm3GEVvtZj6BW8tm
https://wakelet.com/wake/Lmi9ouawdSpD3PGM1GIhH
https://wakelet.com/wake/2R0na3tYiFFACq_Kia8ZD
https://wakelet.com/wake/1J-F-6XNmXNhGuXNJTrV-
https://wakelet.com/wake/Fc7le1rqh-S9oU-oA2fJy
https://wakelet.com/wake/QFGxgvwcEi9o2mmfvgQTH
https://wakelet.com/wake/9W2exW0_akzOomA70ABXR
https://wakelet.com/wake/y97-0NhRfhb9YhXzayPRM
https://wakelet.com/wake/7j5ZDrtQ2Q_3ANDCnCPVH
https://wakelet.com/wake/z2qZGtvWpKXEy7ytwgvFM
https://wakelet.com/wake/S-Y4C8DHhgNzyWWl9DtBF
https://wakelet.com/wake/vbGD-1DHsfW8Wg686dXds
https://wakelet.com/wake/bE1nnIYT2I0T31gsItDXT
raiher (Monday, 24 January 2022 22:49)
raiher fe98829e30 https://wakelet.com/wake/yXJYcxccg_1jlm3oRxENZ
https://wakelet.com/wake/Xhet3gg8IiZTkJ79fceti
https://wakelet.com/wake/thKBx9xMZTL436ImmHJXE
https://wakelet.com/wake/V0LmYAnk9Soy-oUE4YBwf
https://wakelet.com/wake/3vTXcKs2h7LYpOBlI0QNt
https://wakelet.com/wake/9rWB2ieawjQe91gDc6_PF
https://wakelet.com/wake/d1xuqcgAovocZIEP3ggEF
https://wakelet.com/wake/KbVJvdnbup5DRYINRgz7K
https://wakelet.com/wake/KTTk8WyRUbtlvBJcLJKkA
https://wakelet.com/wake/E_OB-mEsY_Zl2hGZ5xoIB
https://wakelet.com/wake/Nrov5J8jZABcqDswSgp0Q
https://wakelet.com/wake/Mkw9RzHk9ff57So1Bt4ux
https://wakelet.com/wake/WHDD0I2wLMqpn-za0K7bs
https://wakelet.com/wake/T8SuEwA0uW1UV6T4VuuWJ
https://wakelet.com/wake/zM3mWm55KyT8gxgaqJiFF
https://wakelet.com/wake/KoqDx2c67H8Q6feYIqHeJ
https://wakelet.com/wake/1M-Q9u3mF0EINsKByPpu0
https://wakelet.com/wake/i_DYH6Rci3bZf5wJXW6qA
https://wakelet.com/wake/oSuCJ38JmX92Bg-W2-2VU
https://wakelet.com/wake/ZhngS8iGnuwwuiNiXnRCr
https://wakelet.com/wake/lB0LVw5EfGYVlw4r67EF2
https://wakelet.com/wake/Tzy0hEcwEBjjTwMHRt4hB
https://wakelet.com/wake/vOfHiEbwFizge1ocaYm-H
https://wakelet.com/wake/78FSSkRNIcqC7p09NrSVd
https://wakelet.com/wake/_usIbXJkeFtdvUFBO4eT8
https://wakelet.com/wake/5aNAoDur1mkqp686taeZW
https://wakelet.com/wake/3jvFLbd65jwTUxHO0wiTy
https://wakelet.com/wake/sc5HL-jc2QcMnachSLtMB
https://wakelet.com/wake/i3cWPA3OxIfv6xiDiSloV
https://wakelet.com/wake/F_kDcHAVBzETlRitNnaWR
hascom (Monday, 24 January 2022 23:35)
hascom fe98829e30 https://wakelet.com/wake/nKF1Na9nE8sYomp5tkeNG
https://wakelet.com/wake/ISAsw22awUacVMSiWHdM2
https://wakelet.com/wake/HM2d13tMuDTdQ3BZDul-c
https://wakelet.com/wake/1ILjRSTALhXaZqhKV2Poa
https://wakelet.com/wake/lF5iqvWj3JjvK2c5hW0Ap
https://wakelet.com/wake/Z6TdPt9gnK9aqs4tCY3TP
https://wakelet.com/wake/Mbk7CKTwQDMOtC_HNdvre
https://wakelet.com/wake/sm8zI61tuAKfO7WexOyfN
https://wakelet.com/wake/O9wPj576wacTOQRLtxl0D
https://wakelet.com/wake/NaRttLM79hyUNq9jm1d7V
https://wakelet.com/wake/-Y2A1dcMM22jjJVOws7MC
https://wakelet.com/wake/5kUDsykxYfQJMzCg473VU
https://wakelet.com/wake/7cSra9ggGVBm5vXzs8Iz7
https://wakelet.com/wake/ZEyI7kVh3LG3kXkAui4jV
https://wakelet.com/wake/Es9OYxdaDfO9iNu65Pqc7
https://wakelet.com/wake/A9ym6aaKU05Kqlt0qlUu0
https://wakelet.com/wake/W2IH6YBeBOtX8-ADXiSnI
https://wakelet.com/wake/1nc9KU4VfFlJp-shTsaXR
https://wakelet.com/wake/BZgjMkG059oP2YBNserO5
https://wakelet.com/wake/jdBd_b6OvDHlyOzywGYBx
https://wakelet.com/wake/WcE3GIpAC5QywU23ode0T
https://wakelet.com/wake/y8dErJd43lR_kS-gy1m9Y
https://wakelet.com/wake/IOTlGTiq17BJjncm9OIGe
https://wakelet.com/wake/GvqSbYtvjhvvbIWB2muFi
https://wakelet.com/wake/8UoKNeCK4M8YzCRTTHwYK
https://wakelet.com/wake/0HBd76jBH8OT4EHEY-yXc
https://wakelet.com/wake/rMUPL4fbeMPQY8X1tUovH
https://wakelet.com/wake/P4clYCdK6waRbwL4LD412
https://wakelet.com/wake/YSXIwaVUg9TMgpfBkJx4c
https://wakelet.com/wake/yUEWvtgjRzEbvevdZNxhz
hendlau (Tuesday, 25 January 2022 00:22)
hendlau fe98829e30 https://wakelet.com/wake/FKF_5I5DZqG93DADQ12po
https://wakelet.com/wake/83o6apVHsS0zFNcvbBNWA
https://wakelet.com/wake/61RdGarNL1c6avXUUlsuI
https://wakelet.com/wake/_rwqbariypkTMaHJXa49l
https://wakelet.com/wake/JmvMJ2vAlSpQ9Gywbvb27
https://wakelet.com/wake/aO6rELDiRIMFHNpAMKXWm
https://wakelet.com/wake/3WoeHmcropFHK0Be5uHyn
https://wakelet.com/wake/h8UDPMl-ao0_7Ycg6BKRX
https://wakelet.com/wake/cu_VmJBtKI1rR4sXftDOC
https://wakelet.com/wake/j4L8_3oDwFcUSSsdgHQyg
https://wakelet.com/wake/TalspcKTeXuJHMl4bA7_l
https://wakelet.com/wake/LmNSHOZsqS977nnDvRU5N
https://wakelet.com/wake/D8LtUzYXuEL-r07ov0t4Z
https://wakelet.com/wake/Gdx7zhkDwHZ-svMrUVYF9
https://wakelet.com/wake/V75purMUq3nShQcEvVIOG
https://wakelet.com/wake/B8LS8ILRAa8nLMq_sgsAh
https://wakelet.com/wake/CzMZT6ow_G-GepTtaanKK
https://wakelet.com/wake/l9zWB_Io__QtRCW0OqIo-
https://wakelet.com/wake/QG6AgXI27KPxKtOH8wwUH
https://wakelet.com/wake/VrdLL_uTpPzCfwxpvgDL4
https://wakelet.com/wake/Wm7tSHLICKYzf458kXZSD
https://wakelet.com/wake/EyYEwXOFqBPrKZItZAZ45
https://wakelet.com/wake/VphDKVeo7s4tCgZ5n_CuX
https://wakelet.com/wake/Cnrb5zckb5eZU1RYU0NWv
https://wakelet.com/wake/dArphz74_tkSmsZm4AI-h
https://wakelet.com/wake/HRt4j5BL2T7UK5qKL46Zd
https://wakelet.com/wake/5S-qSBPAyLEidCr6aHg0E
https://wakelet.com/wake/M7lH02SCkRH0raZugInFg
https://wakelet.com/wake/tSaAYPppTRBQvQ6OxCHCf
https://wakelet.com/wake/_ghC3I4SXj8n_-_qxMMaM
vytoelis (Tuesday, 25 January 2022 01:08)
vytoelis fe98829e30 https://wakelet.com/wake/FVHyRAykZ6lm64ONcgxAP
https://wakelet.com/wake/MbBE5nowM5iMuPcjy25oB
https://wakelet.com/wake/wB8SfagkiA5StMiAZvpnN
https://wakelet.com/wake/qKXbkucSqPm8TnXaJxfUe
https://wakelet.com/wake/-ttkmp7wp4MGmr2Yx4Xs4
https://wakelet.com/wake/S7PsOPj2BVKgmAhB1ZB7k
https://wakelet.com/wake/I2ZoVezDe8XtFjh6xL0Ix
https://wakelet.com/wake/Gnm1_uOFCjZw9hfq7EX-h
https://wakelet.com/wake/TjXdJI1DmMFRPJ1nTv2CL
https://wakelet.com/wake/HfCmVmnbpqxO3T-YyVerv
https://wakelet.com/wake/fD8vkShNB65Y31DX2mEzL
https://wakelet.com/wake/IAtQ4p--ovOS430qqtwzf
https://wakelet.com/wake/ZDZoeql_S_e6CkMen31gt
https://wakelet.com/wake/EKBjEwghGcNTnSnl23c20
https://wakelet.com/wake/PMU5kLcGOOor5y411bPFh
https://wakelet.com/wake/NofplbP0VwPWSILGzgzS0
https://wakelet.com/wake/jNHHAIPZIh4P4gRgu6b6-
https://wakelet.com/wake/aXPojMXmqVRlht0eEyTld
https://wakelet.com/wake/5qP-1AlQ7hX_IAiQOz_Uk
https://wakelet.com/wake/TvmxsdU8-XEtU8AKzOxhE
https://wakelet.com/wake/WrLny_5pPpn3t8SFL08Ca
https://wakelet.com/wake/2nxufxnLvjs3t9LVJQl4W
https://wakelet.com/wake/NCtTwVn9vNfNA5-AKyUQB
https://wakelet.com/wake/02Qcj_VYpxytrPdZ6M_WJ
https://wakelet.com/wake/bLJ9zAtte-GFW6cIO0CFB
https://wakelet.com/wake/fD4LO_d11K9TODdrB6Aka
https://wakelet.com/wake/9mqqP9IYoRPHrNIMWqDHN
https://wakelet.com/wake/QYIWqvfzey8fqfOoHOgjF
https://wakelet.com/wake/yddEG01u0Q8RCjNy0OkkR
https://wakelet.com/wake/ONZ6KTl2UBCMXGi6rDfpP
oceager (Wednesday, 26 January 2022 20:38)
oceager d868ddde6e https://coub.com/stories/3129654-photomodeler-scanner-v6-2-2-596-prisvan
https://coub.com/stories/3129655-download-harvard-referencing-for-microsoft-word-2007-39-trudase
https://coub.com/stories/3129656-hetman-fat-recovery-2-1-keygen-crack-high-quality
https://coub.com/stories/3129657-bus-driver-simulator-2019-free-download-pc-game-nerphi
https://coub.com/stories/3129658-top-download-the-forest-book-pdf-in-hindi
https://coub.com/stories/3129659-pinegrow-web-editor-crack-5-91-with-keygen-free-download-2020-gilwet
https://coub.com/stories/3129661-repack-transformers-the-last-knight-english-download-mp4
https://coub.com/stories/3129662-xforce-updated-keygen-autocad-2017-key
https://coub.com/stories/3129663-kps-design-studio-2010
https://coub.com/stories/3129664-corel-roxio-creator-nxt-pro-7-v21-3-55-0-sp2-serial-key-revwyl
https://coub.com/stories/3129665-hum-tumhare-hain-sanam-hindi-movie-full-download-torrent-idarei
https://coub.com/stories/3129666-new-release-curso-luces-y-sonido-cekit-regygar
https://coub.com/stories/3129667-vb-decompiler-pro-9-2-full-28-ideleve
https://coub.com/stories/3129668-sims-3-1061500107-trainer-better
https://coub.com/stories/3129670-hd-online-player-aladdin-720p-torrent-fr-walchu
https://coub.com/stories/3129669-principi-di-chimica-atkins-pdf-39
https://coub.com/stories/3129671-angle-of-attack-pmdg-737-ngx-torrent-zip-new
https://coub.com/stories/3129672-pd-activator-office-2013-win7-rar
https://coub.com/stories/3129673-free-charlie2015malayalam1080pbluraydtsx2648gbesubs
https://coub.com/stories/3129674-2d-place-v3-9-bde-crack-updated
https://coub.com/stories/3129675-minitool-partition-wizard-10-8-12-technician-winpe-iso-64-bit-delafrod
https://coub.com/stories/3129676-mairlist-6-1-1-professional-studio-plus-seupirate-rar
https://coub.com/stories/3129677-fix-cadsoft-eagle-8-crack-download-full-free
https://coub.com/stories/3129678-padmaja-uday-kumar-pharmacology-pdf-download-high-quality
https://coub.com/stories/3129679-bleach-mayuri-ver-5-5-uncensored-eng-menu-hentai-game-zip-margvaly
https://coub.com/stories/3129680-work-novapdf-10-6-build-123-crack-with-serial-key-2020-download
https://coub.com/stories/3129682-link-crack-corel-painter-v2020-xforce
https://coub.com/stories/3129683-revman-5-download-and-installation-new
https://coub.com/stories/3129684-hd-online-player-free-download-3gp-bangla-sex-video-i-free
https://coub.com/stories/3129685-hot-gta-liberty-city-stories-game-free-download-for-pc-full-version
tempjen (Wednesday, 26 January 2022 21:32)
tempjen d868ddde6e https://coub.com/stories/3059452-binksetmemory8download-blazgla
https://coub.com/stories/3059451-thiruvaimozhivyakyanamtamilpdf-new-free
https://coub.com/stories/3059448-updated-keygen-3ds-max-2009-64bit-171bfdcm
https://coub.com/stories/3059447-top-drug-wars-underworld-131-crack
https://coub.com/stories/3059446-speedtree-fbx-for-maya-download-crack-milijen
https://coub.com/stories/3059445-pacific-rim-1080p-google-drive-pencay
https://coub.com/stories/3059443-wavemachine-labs-drumagog-platinum-vst-rtas-v4-11-incl-keygen-air-rar-orsihert
https://coub.com/stories/3059442-__top__-cx-programmer-9-4-full
https://coub.com/stories/3059440-wic-reset-utility-serial-free-louivan
https://coub.com/stories/3059439-amibroker-4-80-2-amiquote-serial-key-link
https://coub.com/stories/3059437-cadsoft-eagle-professional-6-5-0-patch-download-pc-ullpapi
https://coub.com/stories/3059436-sadhana-of-mahamudra-pdf-16-brasabo
https://coub.com/stories/3059430-summa-wincut-2-1-quirele
https://coub.com/stories/3059429-hack-adobe-premiere-pro-cc-2018-10-1-multilingual-patch
https://coub.com/stories/3059427-ujam-virtual-bassist-royal-1-0-0-vsti-aax-x64-64-bit-tamsnic
https://coub.com/stories/3059426-media-player-for_sivaji-the-boss-new-129311
https://coub.com/stories/3059425-nikon-camera-control-pro-2-serial-crack-better
https://coub.com/stories/3059424-forex-killer-4-12-keygen-top
https://coub.com/stories/3059423-autodesk-navisworks-simulate-2020-keygen-ensjoh
https://coub.com/stories/3059420-mplab-xc8-pro-rar-enriulri
https://coub.com/stories/3059419-link-sonik-synth-2-free-download-crack-23
https://coub.com/stories/3059417-download-fifa-2007-crack-torent-tpb-moranat
https://coub.com/stories/3059418-cartello-orario-di-apertura-da-stamparel-helvit
https://coub.com/stories/3059416-valve-hammer-editor-4-3-download-free-new
https://coub.com/stories/3059415-signing-naturally-homework-answers-unit-9-ercvla
https://coub.com/stories/3059413-diablo-2-hero-editor-full-download-olekwils
https://coub.com/stories/3059412-work-breaking-bad-s05e02-subtitles-720p-or-1080p
https://coub.com/stories/3059409-wilder-amaginations-forums-meloellc
https://coub.com/stories/3059407-extra-quality-euro-truck-simulator-2-gold-bundle-v-1-9-24-1s-download
https://coub.com/stories/3059406-new-nanak-shah-fakir-full-movie-download-filmywap-hd
garlwelt (Wednesday, 26 January 2022 22:24)
garlwelt d868ddde6e https://coub.com/stories/3030079-dvdrip-alibaba-aur-40-chor-download-movies-fabaaddl
https://coub.com/stories/3030078-cleopatra-1999-movie-hindi-dubbed-torrent-best
https://coub.com/stories/3030077-download-xforce-keygen-autocad-lt-2014-activation-carsfaus
https://coub.com/stories/3030076-kabhi-khushi-kabhie-gham-full-movie-hd-1080p-blu-ray-269-odisay
https://coub.com/stories/3030075-alice-madness-returns-skidrow-rar-password-high-quality
https://coub.com/stories/3030073-download-xforce-keygen-inventor-professional-2016-32-bit-patch-shrudean
https://coub.com/stories/3030072-bingocallerprocracked-hundar
https://coub.com/stories/3030071-windows-password-recovery-lastic-serial-number-link
https://coub.com/stories/3030070-hack-autodesk-autocad-2017-x64-keygen-_top_-sadeempc-zip
https://coub.com/stories/3030067-recover-my-files-license-key-4-9-4-keygen-extra-quality-free
https://coub.com/stories/3030069-terminator-genisys-english-1-hindi-dubbed-download-updated
https://coub.com/stories/3030068-microsoft-2-4ghz-transceiver-v7-0-driver-528
https://coub.com/stories/3030066-repack-young-malang-movie-720p-download-utorrent-movies
https://coub.com/stories/3030063-_best_-the-hobbit-the-desolation-of-smaug-extended-edition-1080p-449
https://coub.com/stories/3030065-darksiders-crack-skidrow-osvmar
https://coub.com/stories/3030064-minidx3portablereaderdriversoftware29
https://coub.com/stories/3030062-wondershare-dr-fone-1-5-1-crack-fix
https://coub.com/stories/3030061-top-slime-rancher-viktors-experimental-update-v1-4-1-plaza
https://coub.com/stories/3030058-acronis-true-image-home-9-portable
https://coub.com/stories/3030060-hd-online-player-chhota-bheem-himalayan-adventure-mo-kauran
https://coub.com/stories/3030059-zelotes-f14-mouse-software-64
https://coub.com/stories/3030057-amada-ap-100-free-software-download-alecpetr
https://coub.com/stories/3030056-csgopatchv5nosteam
https://coub.com/stories/3030055-the-adventure-of-tintin-game-crack-_best_
https://coub.com/stories/3030054-raxco-perfectdisk-14-keygen-18-marzaki
https://coub.com/stories/3030053-stellar-phoenix-bkf-recovery-2-0-with-crack-64-bit-new
https://coub.com/stories/3030052-change-folder-color-serial-key-fusgrae
https://coub.com/stories/3030051-kisikisisoalpaisdkelas6semester1
https://coub.com/stories/3030050-cakewalk-dimension-pro-1-5-keygen-software-quensala
https://coub.com/stories/3030049-rumba-3-discografia-descargar-torrent-hit
kahill (Wednesday, 26 January 2022 23:18)
kahill d868ddde6e https://coub.com/stories/2977434-pthc-hussyfan-gracel-series-cardars
https://coub.com/stories/2976765-x-force-autocad-architecture-2014-key
https://coub.com/stories/2976766-casio-fx-880p-emulator-arthjan
https://coub.com/stories/2976759-business-communication-p-d-chaturvedi-pdf-rar-octbra
https://coub.com/stories/2976756-officetab2013serial-taggbenn
https://coub.com/stories/2976757-ennio-morricone-the-platinum-collection-3cd-2007-flac-high-quality
https://coub.com/stories/2976755-updated-vivid-workshop-data-ati-v-11-2-multilanguage-torre-audiocd-contabilidad
https://coub.com/stories/2976751-horton-and-hunt-sociology-pdf-_best_
https://coub.com/stories/2976749-exclusive-khichdi-the-movie-movie-1080p-torrent
https://coub.com/stories/2976748-top-jogo-pharaoh-download-completo-portuguesl
https://coub.com/stories/2976745-finson-progetto-laboratorio-riparazioni-2-__exclusive__-full-version-l
https://coub.com/stories/2976744-hot-cisimlerinmukavemetimustafainanpdf12
https://coub.com/stories/2976742-carrera-crossfire-2-hybrid-bike-manual-full
https://coub.com/stories/2976738-free-scaricare-cartine-tabacco-gratis
https://coub.com/stories/2976743-fikus-visualcam-16-1-13-venczal
https://coub.com/stories/2976741-obs-studio-24-0-crack-download-here-new
https://coub.com/stories/2976739-better-la-quinta-estacion-discografia-completa-torrent-6
https://coub.com/stories/2976735-chalk-n-duster-torrent-repack-download
https://coub.com/stories/2976736-elipse-scada-hardkey-crackl-verified
https://coub.com/stories/2976734-thattathin-marayathu-movie-better-download-tamilrockers-2015
https://coub.com/stories/2976733-wifi-password-crack-best-er-4-6-9-crack-best
https://coub.com/stories/2976732-hot-entrare-nel-modem-tiscali-thomson-tg784n
https://coub.com/stories/2976731-better-anytrans-8-3-0-crack-with-license-key-free-download
https://coub.com/stories/2976728-descargar-power-data-recovery-4-6-5-full-con-crack-verwarr
https://coub.com/stories/2976725-__top__-crack-avanquest-partition-commander-11-7893-portable
https://coub.com/stories/2976724-remo-repair-word-2-0-0-31-crack-full-hot
https://coub.com/stories/2976723-work-18-the-klub-17-v7-4
https://coub.com/stories/2976721-hot-jaime-laycock-nude-23
https://coub.com/stories/2976717-3d-virtual-sex-simulator-android-applicationstrmdsf-wyllelly
https://coub.com/stories/2976716-keygen-top-arcsoft-webcam-companion-4
levosar (Thursday, 27 January 2022 00:10)
levosar d868ddde6e https://coub.com/stories/3106611-work-schema-convertisseur-12v-220v-1000w-pdf-free
https://coub.com/stories/3106612-crack-autocad-electrical-2019-key-top
https://coub.com/stories/3106613-counter-strike-1-6-v1-1-2-7-6027-revemu-15-07-2013-windows-skidrow-carswam
https://coub.com/stories/3106615-extra-quality-wondersharerecoverit71520crackfreedownload
https://coub.com/stories/3106614-fastactivate-premium-edition-v1-8-8-0-baihair
https://coub.com/stories/3106616-new-3tene-free-download-xforce-keygen
https://coub.com/stories/3106617-hd-online-player-hindi-medium-video-songs-hd-1080p-bl-scovcha
https://coub.com/stories/3106619-hot-max-payne-2-game-free-download-full-version-for-pc-xp
https://coub.com/stories/3106621-link-the-big-bang-theory-s01-s08-season-1-8-complete-720p-hdtv-x264-m-serial-key
https://coub.com/stories/3106622-pp2000-keygen-exclusive-rar
https://coub.com/stories/3106620-lumion-6-5-1-pro-patch-for-windows-crackzsoft-serial-key-vaiasso
https://coub.com/stories/3106618-pandora-recovery-2-0-0-330-link-crack
https://coub.com/stories/3106626-c-c-red-alert-3-no-cd-crack-exclusive-l
https://coub.com/stories/3106624-chiros-sigmatel-mscn-stmp3500-mp3-player-firmwarerar
https://coub.com/stories/3106625-xforcekeygendynamostudio201964bitdownload-finbeth
https://coub.com/stories/3106627-fastgsm-s3g-1-0-0-42-free-download-ellbuad
https://coub.com/stories/3106628-visual-composer-license-key-crack-new
https://coub.com/stories/3106623-eplan-suite-22-torrent-new
https://coub.com/stories/3106629-mali-budo-ceo-film-cracked-download-16
https://coub.com/stories/3106630-superior-drummer-2-0-the-metal-foundry-keygen-torrent-portable
https://coub.com/stories/3106631-cracked-mcq-in-gastroenterology-with-explanatory-answers-epub
https://coub.com/stories/3106633-work-hindi-commentary-patch-for-ea-cricket-07-624
https://coub.com/stories/3106632-adobe-acrobat-xi-pro-11-0-07-crack-yangdelp
https://coub.com/stories/3106634-savita-bhabhi-hindi-episode-32-pdf-verified-download
https://coub.com/stories/3106635-pc-game-ita-broken-sword-il-segreto-dei-templari-torrent-__link__
https://coub.com/stories/3106637-c3520-flash-loader-7-5-4-csc-v0-2-citrus-lite
https://coub.com/stories/3106636-trigonometriaparaleigospdfdownload-fix
https://coub.com/stories/3108106-naruto-shippuden-ultimate-ninja-storm-2-rar-pc
https://coub.com/stories/3106740-les-intouchables-full-movie-with-french-subtitles-download-talavic
https://coub.com/stories/3106741-__hot__-error-1309-error-reading-from-file-pes-2013
slajaem (Thursday, 27 January 2022 01:04)
slajaem d868ddde6e https://coub.com/stories/3007359-iambic-pentameter-converter
https://coub.com/stories/3007357-fix-nik-software-silver-efex-pro-2-eng-keygen-photoshop-plugin-download-pc
https://coub.com/stories/3007358-repack-advanced-apktool-download-for-56
https://coub.com/stories/3007356-soil-and-water-conservation-engineering-r-suresh-book-free-link-download
https://coub.com/stories/3007355-license-veeam-one-crack-new
https://coub.com/stories/3007352-_best_-hd-online-player-lego-island-2-no-cd-patch
https://coub.com/stories/3007351-driver-bluetooth-bm03-v2-01
https://coub.com/stories/3007350-top-latinsko-srpski-recnik-pdf-free
https://coub.com/stories/3007349-new-ntlite-enterprise-1-9-0-7330-with-crack
https://coub.com/stories/3007348-design-of-concrete-structures-14th-ed-nilson-in-si-units-cracked
https://coub.com/stories/3007347-data-structures-book-by-seymour-lipschutz-pdf-free-download-heropal
https://coub.com/stories/3007343-better-hd-online-player-v-invasion-extraterrestre-temporada
https://coub.com/stories/3007344-link-double-dhamaal-2011-hindi-720p-torrent
https://coub.com/stories/3007341-unreal-gold-directx-11-highres-textures-repack-free
https://coub.com/stories/3007339-link-solucionario-de-hidraulica-general-gilberto-sotelo-avila-vol-1-122
https://coub.com/stories/3007334-tharai-thappattai-mp4-full-movie-downloadinstmank-best
https://coub.com/stories/3007332-karl-dietrich-bracher-la-dictadura-alemana-pdf-16-linehark
https://coub.com/stories/3007331-_best_-alcatel-lucent-omnipcx-office-management-console-download
https://coub.com/stories/3007329-exclusive-rebelle-crack-no-cd
https://coub.com/stories/3007330-repack-frontdesigner-30-download-crack-14
https://coub.com/stories/3007328-videos-robados-caseros-violaciones-reales
https://coub.com/stories/3007326-total-audio-converter-5-1-serial-number
https://coub.com/stories/3007327-ddt2000-2600-renault-crack-link
https://coub.com/stories/3007325-link-codigo-registro-sonar-8-del-serial-cwwt800867845067359-6-sygate-flughafen-handynummern-tag
https://coub.com/stories/3007321-vibe-sound-usb-turntable-manual-opejas
https://coub.com/stories/3007320-best-medeil-pharmacy-management-system-1-0-crackl
https://coub.com/stories/3007319-__hot__-durgatamilfullmoviedownload
https://coub.com/stories/3007318-essential-bulats-cambridge-torrent
https://coub.com/stories/3007317-updated-cubase-6-iso-torrent-the-pirate-bay
https://coub.com/stories/3007315-download-hindi-movie-rann-full
hasiginn (Thursday, 27 January 2022 01:57)
hasiginn d868ddde6e https://coub.com/stories/2944233-cwcheat-download-god-eater-burst-best
https://coub.com/stories/2944232-install-bibcam-boys
https://coub.com/stories/2944229-best-download-unlock-apple-iphone-osx-zip
https://coub.com/stories/2944230-better-alzex-personal-finance-pro-5-8-activation-code-and-101
https://coub.com/stories/2944227-repack-auto-combo-para-bkl
https://coub.com/stories/2944228-ageofempires3datapbardownload-repack
https://coub.com/stories/2944226-extra-quality-hack-mi-cash-audition
https://coub.com/stories/2944225-programcartidevizitafree-top-download
https://coub.com/stories/2944224-mortal-kombat-komplete-edition-pc-kratos-mod-92-fitwhea
https://coub.com/stories/2944223-tally-9-software-free-download-with-crackfl-__exclusive__
https://coub.com/stories/2944222-kaanchi-movie-free-download-in-hindi-720p-download-nithblai
https://coub.com/stories/2944221-link-desktop-icon-toy-4-5-serial-number-free-download
https://coub.com/stories/2944220-new-softwaremengetahuipasswordfacebookoranglain
https://coub.com/stories/2944219-halo-4-skidrow-rar-password
https://coub.com/stories/2944218-biological-sciences-5th-edition-freeman-pdf-download-goodvane
https://coub.com/stories/2944217-hd-online-player-true-legend-mp4-movie-23-talodor
https://coub.com/stories/2944216-extra-quality-true-detective-s01e02-720p-13
https://coub.com/stories/2944215-the-hunter-activation-code-generator
https://coub.com/stories/2944214-aamras-1-dvdrip-download-movies-yasmmama
https://coub.com/stories/2944213-purana-purusha-yogiraj-shyama-charan-lahiri-pdf-download-full
https://coub.com/stories/2944210-daddy-cool-munde-fool-720p-brrip-mkv-torrent-uthmlenn
https://coub.com/stories/2944211-an-autobiography-of-a-yogi-malayalam-pdf-download-better
https://coub.com/stories/2944209-ai-shogi-version-18-for-windows-download-link
https://coub.com/stories/2944208-csi-etabs-version-15-2-2-build-1364-32bit-64bit-crack-serial-key-keygen-wyntal
https://coub.com/stories/2944207-aimbot-gunbound-season-3-free-rar-_top_
https://coub.com/stories/2944203-xara-3d-maker-7-serial-number-rar-verified
https://coub.com/stories/2944206-brilliant-tutorials-yg-file-free-download-fixed
https://coub.com/stories/2944205-thunderbolt-full-movie-in-hindi-download-xandear
https://coub.com/stories/2944204-live-worship-serial-top-keygen-mac
https://coub.com/stories/2944201-incredimail-2-premium-plus-multi-language-6-28-build-4953-donker-link
giseibra (Thursday, 27 January 2022 02:52)
giseibra d868ddde6e https://coub.com/stories/3126038-c3550-ipservicesk9-mz-122-55-se8-14-keilmakf
https://coub.com/stories/3126037-3d-object-converter-v5-30-serial
https://coub.com/stories/3126036-mapanglaw-ang-mukha-ng-buwan-pdf-15-updated
https://coub.com/stories/3126035-robbie-dupree-discography-1980-2008-torrent
https://coub.com/stories/3126034-link-fsx-pmdg-777-all-pmdg-service-packs-crack-rar-serial-key-keygen
https://coub.com/stories/3126033-fixed-nintendo-wii-rom-download-new-super-mario-bros-wii-dolphin
https://coub.com/stories/3126032-crack-serial-number-genarts-sapphire-plugins-for-windows-23-pilgbern
https://coub.com/stories/3126031-dll-files-fixer-v3-1-81-2801preactivated
https://coub.com/stories/3126029-borislav-pekic-atlantida-pdf-download-hot
https://coub.com/stories/3126030-how-to-download-adobe-audition-1-5-free-full-version-hot
https://coub.com/stories/3126028-outlook-pst-splitter-v4-0-cracked-version-download-repack
https://coub.com/stories/3126027-crack-f-secure-antivirus-safe-pre-activated-work
https://coub.com/stories/3126026-link-irender-nxt-5-sketchup-license-key
https://coub.com/stories/3126025-fs-sm100-usb-driver-lanvany
https://coub.com/stories/3126024-verified-kapetan-dzon-piplfoks-prepricano-rapidshare
https://coub.com/stories/3126023-eugene-butkov-solutions-manual52-verified
https://coub.com/stories/3126022-sleeping-dogs-v1-4-pandora-crack-extra-quality
https://coub.com/stories/3126021-media-player-for_kanchana-2-updated
https://coub.com/stories/3126020-download-quite-a-box-of-tricks-1-8-8-link
https://coub.com/stories/3126019-free-download-motorola-iden-cns-unlock-ver-7-0-rar-whenody
https://coub.com/stories/3126016-crack-internet-singer-song-writer-9-professional-v9-03-0-exclusive
https://coub.com/stories/3126018-vipermod-primetime-v4-5-52-verified
https://coub.com/stories/3126017-blackmail-720p-in-download-torrent-maircar
https://coub.com/stories/3126015-vectorworks-12-5-with-key-keygen-work
https://coub.com/stories/3126010-hot-nehru-report-in-urdu-pdf-16
https://coub.com/stories/3126014-psikey-dll-coreldraw-graphics-suite-x5-extra-quality-keygen
https://coub.com/stories/3126013-shaadimeinzarooraanahindimoviein720pdownload-danyesh
https://coub.com/stories/3126012-exclusive-filmconvert-pro-1-34-for-sony-strane-monografie-ba
https://coub.com/stories/3126011-hamdard-medicine-book-in-urdu-pdf-45-falltal
https://coub.com/stories/3126008-futuremark-pcmark-11-1-0-1493-x64-multilingual-crack-patched
parlore (Thursday, 27 January 2022 03:46)
parlore d868ddde6e https://coub.com/stories/2935549-rld-prevso2016-iso-epub
https://coub.com/stories/2935541-resident-evil-4-trainer-v-1-0-0-l-repack
https://coub.com/stories/2935548-tmpgenc-video-mastering-works-6-keygen-torrent-top
https://coub.com/stories/2935546-karan-arjun-mp4-full-movie-download-ittann
https://coub.com/stories/2935547-portable-download-novel-karya-fredy-s-pdf
https://coub.com/stories/2935545-grid-autosport-22-trainer-reloaded-aktama
https://coub.com/stories/2935544-unity-pro-xl-6-1-link-download-trial-version
https://coub.com/stories/2935542-hd-online-player-7g-rainbow-colony-movie-free-downloa-derleis
https://coub.com/stories/2935543-python-script-to-download-skillshare-unlimited-premium-courses-lauack
https://coub.com/stories/2935540-magix-photo-designer-7-serial-number-haswall
https://coub.com/stories/2935539-coreldraw-graphics-suite-x6-16-0-0-707-repack-by-krokoz-eng-rus-_best_
https://coub.com/stories/2935537-better-finaldata-enterprise-3-0-torrent
https://coub.com/stories/2935538-descargarneodata64bitsconcrack-upd
https://coub.com/stories/2935536-chief-architect-premier-x10-20-3-0-54-crack-free-2020-keygen-ulryneje
https://coub.com/stories/2935533-windows-trust-5-iso-__hot__
https://coub.com/stories/2935535-best-fileviewpro-2013-crack-license
https://coub.com/stories/2935534-ibm-usb-serial-parallel-adapter
https://coub.com/stories/2935532-kmsmicro-activator-v-3-12-final-for-microsoft-office-2013-professional-plus-rafadarn
https://coub.com/stories/2935531-exclusive-starcraft-2-heart-of-the-swarm-spolszczenie-torrent
https://coub.com/stories/2935530-hot-system-software-leland-l-beck-d-manjula-3rd-editio-freccia-massimo-asia
https://coub.com/stories/2935524-michel-thomas-complete-v3-tryhila
https://coub.com/stories/2935529-stellar-phoenix-access-recovery-4-1-repack-crack-rar
https://coub.com/stories/2935528-isplever-classic-15-crack-link
https://coub.com/stories/2935527-contra-shattered-soldier-ps2-iso-torrent
https://coub.com/stories/2935525-verified-mobiola-web-camera-3-1-8-activation-key
https://coub.com/stories/2935526-windows7ptptfreedownload-top
https://coub.com/stories/2935522-full-wintopo-pro-3-7-0-0-x64-23
https://coub.com/stories/2935523-keil-uvision-mdk-arm-460-crack-best
https://coub.com/stories/2935521-urbanismobioclimaticoesterhigueraspdf-better
https://coub.com/stories/2935520-sid-meiers-civilization-v-5-v1-0-1-167-update-plus-crack-codex-peabuil
frilaw (Thursday, 27 January 2022 04:41)
frilaw d868ddde6e https://coub.com/stories/3147860-download-bambi-dublat-in-romana-byaeast
https://coub.com/stories/3147858-artcam-2019-xforce-keygen-x64-x86-work
https://coub.com/stories/3147857-rpp-berkarakter-agama-kristen-protestan-sd-kelas-1-618
https://coub.com/stories/3147854-amnesia-the-dark-descent-serial-number-skidrow
https://coub.com/stories/3147853-better-advanced-etl-processor-3-9-6-3-full-version-crack-with-serial-key
https://coub.com/stories/3147852-robobat-2012-avec-crack-ellegia
https://coub.com/stories/3147851-bitcoin-money-adder-v6-0-activation-code-no-survey-free-download-jacigat
https://coub.com/stories/3147850-paco-de-lucia-guitar-tab-me-regale-andhart
https://coub.com/stories/3147848-tazkiratul-awliya-bangla-pdf-free-download-better
https://coub.com/stories/3147847-free-bonecraft-proper-crack-reloaded-223
https://coub.com/stories/3147846-delete-orphaned-sids-in-acls-__full__
https://coub.com/stories/3147845-red-mc-nba-2k14-crack-only-30-exclusive
https://coub.com/stories/3147844-devon-ke-dev-mahadev-episodes-51-100-hindi-top
https://coub.com/stories/3147842-shadow-hills-mastering-compressor-plugin-torrent-talvil
https://coub.com/stories/3147843-adobe-acrobat-dc-pro-crack-amtlibdll-17-blabern
https://coub.com/stories/3147841-updated-dameware-nt-utilities-8-0-1-151-keygen-download
https://coub.com/stories/3147839-top-hawaa-hawaai-full-hindi-movie-download
https://coub.com/stories/3147838-hd-online-player-normal-2007-movie-free-download-utor-javbeve
https://coub.com/stories/3147835-x-force-autocad-map-3d-2015-osmelli
https://coub.com/stories/3147833-catia-v6-2014-free-download-with-crack-antsant
https://coub.com/stories/3147831-free-btd-file-converter-new
https://coub.com/stories/3147830-maxpayne3reloadedrarpassword-best
https://coub.com/stories/3147828-the-metabolism-miracle-diet-pdf-19-malmari
https://coub.com/stories/3147827-extra-quality-bioshock-2-remastered-minervas-den-dlc-unlocker-codex-2018-no-survey
https://coub.com/stories/3147826-work-assimil-lingua-tedesca-torrent
https://coub.com/stories/3147825-corpse-party-blood-covered-pc-download-germmadd
https://coub.com/stories/3147824-newtonevstpluginfree-hot-download
https://coub.com/stories/3147823-beatedit-for-premiere-pro-patrlavy
https://coub.com/stories/3147822-signcut-x2-free-license-crack-darengl
https://coub.com/stories/3147821-generador-de-dinero-de-paypal
paiggla (Thursday, 27 January 2022 05:35)
paiggla d868ddde6e https://coub.com/stories/2950396-hindi-film-songs-notations-on-keyboard
https://coub.com/stories/2950395-provoked-movie-download-in-hindi-hd-720p-kickass-magmal
https://coub.com/stories/2950394-natalia-druyts-naakt-foto-updated-niegjann
https://coub.com/stories/2950393-mts-cnc-topturn-topmill-7-3-crack-full-rar
https://coub.com/stories/2950392-install-clave-para-activar-windows-8-single-language-build-9200-240
https://coub.com/stories/2950391-ddp-yoga-max-pack-download-__link__-hit
https://coub.com/stories/2950390-3dmgame-dll-download-fifa-15-crackf-top
https://coub.com/stories/2950388-bukusosiologikelasxiikurikulum2013pdf-urancri
https://coub.com/stories/2950389-poweriso-7-4-crack-with-keygen-key-free-top-download-2019
https://coub.com/stories/2950387-install-wwe-2k15-pc-crack-fix
https://coub.com/stories/2950385-tacx-trainer-software-4-0-key-install-crack
https://coub.com/stories/2950386-matlab-r2013b-license-file-crack-beriche
https://coub.com/stories/2950384-link-anjaana-anjaani-3-full-movie-download-in-720p-hd
https://coub.com/stories/2950381-video-capture-master-7-0-1-1010
https://coub.com/stories/2950383-top-serial-number-acdsee-5-pro
https://coub.com/stories/2950382-aayirathil-oruvan-movie-download-free-umbuvan
https://coub.com/stories/2950366-bhaiya-dooj-bhojpuri-film-verified-download
https://coub.com/stories/2950380-kuka-sim-pro-download-crack-free
https://coub.com/stories/2950379-fundy-album-builder-hot-crack
https://coub.com/stories/2950377-virtual-canine-anatomy-full-version-glenapo
https://coub.com/stories/2950376-renee-undeleter-2013-2-28-0-torrent-new
https://coub.com/stories/2950378-focus-first-flash-ms1690-driver-download-gerdawa
https://coub.com/stories/2950374-fix-ufs-explorer-standard-recovery-5-6-keygen-22
https://coub.com/stories/2950375-srirasmi-nude-album
https://coub.com/stories/2950372-free-download-craagle-40-sasgard
https://coub.com/stories/2950373-portrait-professional-studio-15-7-3-incl-crack-alyfor
https://coub.com/stories/2950371-kscan3d-torrent-oroioly
https://coub.com/stories/2950370-rpc-plugin-for-max-2009-64-bit-free-download-1-upd
https://coub.com/stories/2950369-hitler-the-rise-of-evil-dual-audio-extra-quality
https://coub.com/stories/2950368-cvirte-dll-windows-7-upd-download
chesray (Thursday, 27 January 2022 06:28)
chesray d868ddde6e https://coub.com/stories/2977994-warcraftenglish2full-hot-movieinhindihddownload
https://coub.com/stories/2977993-kahlown-screen-spy-monitor-keygen-install
https://coub.com/stories/2977992-san-judas-tadeo-imagenes-hd-1080pl-updated
https://coub.com/stories/2977991-hadaka-shitsuji-english-patch-10rar-2021
https://coub.com/stories/2977990-active-sky-next-fsx-crack-better
https://coub.com/stories/2977989-windows-8-transformation-pack-1-0-h33t-terminator-t-101
https://coub.com/stories/2977988-portable-office-2016-crack-onhax-idm
https://coub.com/stories/2977987-iexplorer-4-3-4-25520-for-windows-__hot__-crack
https://coub.com/stories/2977986-marjorie-barretto-photo-scandal-73l
https://coub.com/stories/2977985-link-hoyle-board-games-2003-free-download-full-version
https://coub.com/stories/2977984-keyclone-v1-8g-serial-key-top-keygen
https://coub.com/stories/2977983-top-martindale-the-extra-pharmacopoeia-free-ebook-61
https://coub.com/stories/2977982-codigo-activacion-recovery-my-files-5-1-rar
https://coub.com/stories/2977981-assassin-s-creed-3-skidrow-crack-1-01instmank-grasquas
https://coub.com/stories/2977980-full-microsoft-download-net-framework-v-4-30319
https://coub.com/stories/2977979-verified-pes-2010-skidrow-password-rar-crack-icecold-games-cavali
https://coub.com/stories/2977978-octane-render-cinema-4d-cracked-zipl-install
https://coub.com/stories/2977977-utorrent-free-movie-download-link-hindi-ballad-of-rustom
https://coub.com/stories/2977975-hd-online-player-savita-bhabhi-movie-2013-free-_hot_-downlo
https://coub.com/stories/2977976-engview-package-designer-suite-v
https://coub.com/stories/2977969-exclusive-symantec-pc-anywhere-v11-free-download
https://coub.com/stories/2977974-total-war-attila-english-language-files-codex
https://coub.com/stories/2977973-blutonium-boy-hardstyle-samples-vol-1-2-part01-rar-extra-quality
https://coub.com/stories/2977972-patched-geopolitical-simulator-4-power-revolution
https://coub.com/stories/2977971-better-girl-fuck-by-dog
https://coub.com/stories/2977970-work-guidedesmetiersdelelectrotechniquev2epub
https://coub.com/stories/2977968-semaholzbausoftware-new-cracktutorial
https://coub.com/stories/2977967-top-download-style-dangdut-yamaha-psr-s910
https://coub.com/stories/2977966-cad-kas-pdf-editor-5-0-crack-125-nefelaur
https://coub.com/stories/2977965-ciel-gestion-commerciale-evolution-9-1-cracked-fix
vynchir (Thursday, 27 January 2022 07:23)
vynchir d868ddde6e https://coub.com/stories/3034696-parasharaslightprofessionalvedicastrology701rar
https://coub.com/stories/3034695-best-harry-potter-and-the-deathly-hallows-part-2-telugu-movie-720p-download
https://coub.com/stories/3034694-2021-caa-rade-v5r19-crack
https://coub.com/stories/3034692-ushul-fiqh-abu-zahrah-pdf-fixed
https://coub.com/stories/3034693-autocom-delphi-ds150e-_hot_-keygen-210
https://coub.com/stories/3034691-mathwave-easyfit-professional-v5-50-crack-link
https://coub.com/stories/3034690-register-pes-2011-64-bit-win-8
https://coub.com/stories/3034689-free-fisica-vectorial-vallejo-zambrano-pdf-descargar-libros-21
https://coub.com/stories/3034688-crack-salfeld-child-control-2011-v11-270-0-0-winall-incl-keygen-top-brd
https://coub.com/stories/3034687-crack-better-goldensoftware-voxler-v3-3-1843-with-key-iahq76
https://coub.com/stories/3034686-aact-portable-crack-3-9-9-crack-with-keygen-2020-patched-download
https://coub.com/stories/3034685-neal-n-nikki-hai-full-movie-free-download-mp4-verwil
https://coub.com/stories/3034684-portable-baabarr-movie-720p-download
https://coub.com/stories/3034683-mary-kom-movie-720p-download-repack-kickass
https://coub.com/stories/3034682-verified-juju-request-mp3-20100929rarrar
https://coub.com/stories/3034681-link-alien-skin-exposure-4-x-force-keygen
https://coub.com/stories/3034680-crack-vocalizer-for-nvda-3-0-2-all-voices-leoudel
https://coub.com/stories/3034679-ammamma-keladi-thozhi-novel-pdf-free-fixed
https://coub.com/stories/3034678-solucionario-amplificadores-operacionales-y-circuitos-integrados-lineales-robert-f-coughlin-1
https://coub.com/stories/3034677-libro-lenguajes-de-programacion-principios-y-practica-kenneth-c-louden-rapidshare-checked
https://coub.com/stories/3034676-baltagul-de-mihail-sadoveanu-pdf-upd-download
https://coub.com/stories/3034675-best-tt-budget-s2-1600-bda-driver-for-windows-10-64-bit-x64-zip
https://coub.com/stories/3034674-fix-zokkomon-hindi-movie-free-online
https://coub.com/stories/3034673-aras-360-hd-2-1-0-3-crack-best
https://coub.com/stories/3034672-libroteoriageneraldelprocesovicentepuppiopdf
https://coub.com/stories/3034671-esbozodehistoriauniversaljuanbrompdf19-marrela
https://coub.com/stories/3034670-top-hd-kits-for-pes6-kitserver-download-for-computer
https://coub.com/stories/3034669-_top_-download-avenir-font-family-free-torrent-998
https://coub.com/stories/3034668-top-air-navigation-pro-ipa-cracked
https://coub.com/stories/3034667-extra-quality-ocaminhomenospercorridopdfdownload
ualnan (Thursday, 27 January 2022 08:20)
ualnan d868ddde6e https://coub.com/stories/3069084-hadis-40-al-wafi-pdf-work-download
https://coub.com/stories/3069082-download-__exclusive__-do-cd-dire-straits-greatest-hits
https://coub.com/stories/3069079-dr-fone-9-9-5-crack-registration-code-free-download-_verified_
https://coub.com/stories/3069081-winsetupfromusb-1-0-beta-7-zip-levelme
https://coub.com/stories/3069080-free-sadda-adda-full-movie-hd-720p-download
https://coub.com/stories/3069077-2021-we-nfs-carbon-movies-folder
https://coub.com/stories/3069078-norton-ghost-9-boot-cd-serial-key-keygen-top
https://coub.com/stories/3069076-link-singam-2-movie-download-720p-torrents
https://coub.com/stories/3069074-corel-website-creator-x6-crack-keygen-lisurb
https://coub.com/stories/3069075-usbfix-free-download-latest-version-full-crack
https://coub.com/stories/3069071-camela-discografia-completa-17-discos-caratulas
https://coub.com/stories/3069072-gotomeeting-free-exclusive-download-for-windows-7-crack
https://coub.com/stories/3069073-movavi-video-editor-15-4-1-hot-crack-keygen-activation-key-2020
https://coub.com/stories/3069070-klanghelm-mjuc-variable-tube-comp-v1-1-win-x86-x64-x-robel-crack-niqumait
https://coub.com/stories/3069069-return-to-castle-wolfenstein-game-hack-password-madgly
https://coub.com/stories/3069067-repack-adondenoconozconadaepubbookpdf
https://coub.com/stories/3069064-patched-magix-vegas-movie-studio-platinum-15-0-0-146-full-with-medicine-faulolea
https://coub.com/stories/3069063-tengo-ganas-de-ti-english-subtitles-top
https://coub.com/stories/3069062-far-cry-1-crack-dosyas-indir-gezginlerl-jaylhone
https://coub.com/stories/3069060-harry-potter-1-sinhala-dubbed-kids-movies-upd
https://coub.com/stories/3069061-upd-displayname-field-missing-from-registry-fifa-15-crack-3dm
https://coub.com/stories/3069059-fuga-con-pajarillo-aldemaro-romero-pdf-11
https://coub.com/stories/3069058-battlefield-4-digital-deluxe-edition-repack-multi2-seyter
https://coub.com/stories/3069057-xforce-keygen-collaboration-for-revit-2009-download-upd-64-bit
https://coub.com/stories/3069056-mercedes-benz-navigation-dvd-comand-aps-2012-2013-ntg1-torrent-download-top
https://coub.com/stories/3069055-nissan-b14-ecu-wiring-diagram
https://coub.com/stories/3069054-adobe-photoshop-cs6-pt-br-iso-serial-key
https://coub.com/stories/3069053-verified-image-line-vocodex-vst-v1-0-3-torrent
https://coub.com/stories/3069052-best-tipard-video-converter-ultimate-9-2-38-with-crack-serial-key
https://coub.com/stories/3069050-link-nikon-capture-nx-2-keygen-serial
nicgemm (Thursday, 27 January 2022 09:14)
nicgemm d868ddde6e https://coub.com/stories/3139989-aim-cfg-download-niomossi
https://coub.com/stories/3139994-hd-online-player-tone2-complete-bundle-v-2012-au-vs-leitbirt
https://coub.com/stories/3139991-__exclusive__-free-download-perfume-movie-in-hindi-dubbed
https://coub.com/stories/3139990-filme-constantine-2-updated-download-dublado
https://coub.com/stories/3139988-artificial-girl-3-save-file-download-link
https://coub.com/stories/3139987-free-download-ebook-menjadi-master-php-dengan-framework-codeigniter
https://coub.com/stories/3139985-hot-patch-crack-sims-3-v-1-0-632-fo
https://coub.com/stories/3139984-firmware-sagem-fast-3304-v2-6
https://coub.com/stories/3139983-download-mio-c230-map-update-dvd-belnadr
https://coub.com/stories/3139978-cs-1-6-flamer-cheat-21-faitokt
https://coub.com/stories/3139977-tonik-pt-3-newstar-jimmy-sets-91120-upd
https://coub.com/stories/3139975-full-download-bpm-studio-full-version-crack
https://coub.com/stories/3139974-new-pnozmulti-configurator-license-crack-software
https://coub.com/stories/3139973-hd-online-player-oh-my-god-2012-full-movie-free-download-720p-gitegar
https://coub.com/stories/3139972-dishonored-the-brigmore-witches-download-for-pc-ocean-of-games-install
https://coub.com/stories/3139971-ht-employee-monitor-8-9-4-serial-key-full-upd
https://coub.com/stories/3139969-driver-placa-mae-intel-corp-emerald-lake-2-panklar
https://coub.com/stories/3139970-semc-s1-unlock-tool-13-install
https://coub.com/stories/3139968-harry-potter-and-the-philosophers-stone-2001-bluray-720p-h264-greek-subs
https://coub.com/stories/3139966-shraddhakannadapdfdownload-top
https://coub.com/stories/3139963-eragon-2-eldest-full-movie-download-flatjaem
https://coub.com/stories/3139965-hot-keygen-multilizer-pdf-translator-serial-downloads-torrent-free
https://coub.com/stories/3139964-umbus-enumerator-windows-7-driver-download-better
https://coub.com/stories/3139961-omsi-bus-simulator-product-activation-key-allinat
https://coub.com/stories/3139962-samsung-gt-c3303-youtube-software-2021-download
https://coub.com/stories/3139959-the-secret-life-of-pets-english-movies-dubbed-in-telugu-free-download-in-hd-720p-trevper
https://coub.com/stories/3139958-breaking-bad-s01e01-720p-bia-subtitles-full-free
https://coub.com/stories/3139957-patched-kitchendraw-5-mutfak-katalogu-v3-2-tr
https://coub.com/stories/3139955-download-boujou-5-full-crack-74-belmaky
https://coub.com/stories/3139954-artmodelsoliviap010figuredrawingposereferenceartmodelsposesdownloadstorrent-ferdian
sakjan (Thursday, 27 January 2022 10:10)
sakjan d868ddde6e https://coub.com/stories/3013334-__link__-123-flash-chat-v10-0-nulled-io
https://coub.com/stories/3013333-wondershare-filmora-8-7-1-4-crack-cracksmind-full-version-free
https://coub.com/stories/3013331-better-madagascar-1-dublat-in-romana-download-torent
https://coub.com/stories/3013327-waveshell-vst-9-taringa-free
https://coub.com/stories/3013325-archicad-software-free-download-with-crack-jaerjani
https://coub.com/stories/3013326-foxit-pdf-editor-license-key-new
https://coub.com/stories/3013323-solucionarioecuacionesdiferencialesisabelcarmonajover
https://coub.com/stories/3013322-magic-retouch-4-3-setup-license-key-full-latest-work
https://coub.com/stories/3013321-corel-draw-x6-keygen-core-download-rilgia
https://coub.com/stories/3013320-repack-crack-colin-mcrae-4-download-free
https://coub.com/stories/3013317-nav-n-go-igo-834142975-51-top
https://coub.com/stories/3013318-counterpath-eyebeam-1-5-19-rar
https://coub.com/stories/3013316-__hot__-download-xforce-keygen-autocad-mep-2013-64-bit-patch
https://coub.com/stories/3013315-bahis-analiz-program-excel-cassuri
https://coub.com/stories/3013312-avast-premier-2020-crack-license-key-latest-release-benzel
https://coub.com/stories/3013310-windows-10-manager-3-2-0-crack-2020-niagesse
https://coub.com/stories/3013305-sbi-cheque-deposit-slip-pdf-download-top
https://coub.com/stories/3013307-xforce-better-keygen-plant-design-suite-2017-32-bit-free-download-exe
https://coub.com/stories/3013304-repack-marathi-hd-movies-1080p-16
https://coub.com/stories/3013299-verified-windows-7-loader-by-hazar-1-7-free-376
https://coub.com/stories/3013300-fix-reaction-mechanism-in-organic-chemistry-by-mukul-c-ray-pdf-download
https://coub.com/stories/3013297-kitab-senjata-mukmin-pdf-karemog
https://coub.com/stories/3013296-wii-xenoblade-chronicles-iso-fre
https://coub.com/stories/3013295-2021-free-download-pc-games-mortal-kombat-deadly-alliance-full-version
https://coub.com/stories/3013291-the-attacks-of-26-11-man-full-movie-in-hindi-__exclusive__-free-download
https://coub.com/stories/3013290-__exclusive__-hd-online-player-incir-receli-2-tek-parca-720p-or-108
https://coub.com/stories/3013286-hd-online-player-call-of-duty-black-ops-2-multiplayer-seasas
https://coub.com/stories/3013285-digital-fundamentals-floyd-10th-edition-pdf-free-627-new
https://coub.com/stories/3013284-high-quality-dts-neural-upmix-vst-rtas-v1-0-4l
https://coub.com/stories/3013282-best-netfabb-2014-scaricare-key-generator-64-bits-it
elocas (Thursday, 27 January 2022 11:09)
elocas d868ddde6e https://coub.com/stories/3107223-download-wbs-chart-pro-4-7-crack-havmart
https://coub.com/stories/3107224-pc-game-fate-extella-link-portable
https://coub.com/stories/3107222-ecm-titanium-full-version-download-high-quality
https://coub.com/stories/3107220-winavi-video-converter-11-6-1-keygen-rarbfdcm-rowquy
https://coub.com/stories/3107221-a1-wma-editor-serial-key-__top__-keygen
https://coub.com/stories/3107219-mediahuman-youtube-downloader-3-9-9-16-crack-winebrya
https://coub.com/stories/3107218-fisiologia-respiratoria-cristancho-pdf
https://coub.com/stories/3107217-download-jamie-foxx-unpredictable-album-zip-76-sibegia
https://coub.com/stories/3107216-crack-xp-sp3-wpa-kill-link
https://coub.com/stories/3107215-robbins-anatomia-patologica-ita-pdf-work-download
https://coub.com/stories/3107214-mikro-iktisat-zeynel-dinler-pdf-download-better
https://coub.com/stories/3107213-slow-gold-7-7-0-free-download-_top_
https://coub.com/stories/3107212-total-commander-9-52-final-x86-x64-new-key-download-pc-gerrcat
https://coub.com/stories/3107211-link-vbcableabfreedownload
https://coub.com/stories/3107210-nonton-tv-dewasa-online-129-clarchay
https://coub.com/stories/3107209-gta-vice-city-stories-without-human-verification-vindes
https://coub.com/stories/3107208-hot-sumiko-kiyooka-petit-43
https://coub.com/stories/3107207-deon-meyer-13-uur-epub-download-gratis-glacair
https://coub.com/stories/3107206-hifi-active-sky-p3dv4-no-crack-skidrow-reloaded-glaval
https://coub.com/stories/3107205-kodak-preps-6-2-crack-updated-win-checked
https://coub.com/stories/3107204-jilebi-malayalam-movie-full-download-hd
https://coub.com/stories/3107203-patched-numero-de-serie-de-sniper-ghost-warrior-pc
https://coub.com/stories/3107202-best-dibawah-bendera-revolusi-jilid-2-pdf-22
https://coub.com/stories/3107201-better-through-the-fire-sebastian-telfair-watch
https://coub.com/stories/3107200-rfactorgokartmoddownload-anniegmo
https://coub.com/stories/3107199-hot-crackcsrbluetooth40driver
https://coub.com/stories/3107198-photodex-proshow-transition-pack-volume-2-85-free
https://coub.com/stories/3107197-exclusive-serial-number-samplitude-music-studio-2014
https://coub.com/stories/3107196-kerio-control-7-3-2-build-4445-17
https://coub.com/stories/3107195-skanda-purana-tamil-pdf-93-link
undunat (Thursday, 27 January 2022 12:37)
undunat d868ddde6e https://coub.com/stories/3008967-spirited-away-full-movie-english-dubbedbfdcm-repack
https://coub.com/stories/3008965-generationofelectricalenergybrguptapdf-nikuyen
https://coub.com/stories/3008963-new-foxit-reader-9-2-0-9297-crack-20020-activation-key
https://coub.com/stories/3008964-adobe-acrobat-9-professional-multilingual-patch-rh-keygen-top-129311
https://coub.com/stories/3008961-kodovizapilotsupertelurc2002p-work
https://coub.com/stories/3008960-ancient-warfare-3-alpha-26-1-drm-free-best
https://coub.com/stories/3008958-verified-adobe-acrobat-pro-dc-2018-009-20050-crack-cracksnow
https://coub.com/stories/3008957-emedia-card-designer-full-crack-261-wayngar
https://coub.com/stories/3008956-better-civ-5-world-builder-crack
https://coub.com/stories/3008954-forza-motorsport-7-mnsxx-generator-online-blosali
https://coub.com/stories/3008952-teenfuns-tf-264-nansy-151-pics-zaretobi
https://coub.com/stories/3008950-football-manager-2013-patch-13-1-4-crack-haizlan
https://coub.com/stories/3008949-bhabani-prasad-majumdar-poems-pdf-free-__link__
https://coub.com/stories/3008947-ntsyspc-rar-best
https://coub.com/stories/3008945-top-x-plane-11-global-scenery-dlc-codex-no-survey-no-password-2019
https://coub.com/stories/3008943-ots-turntables-pro-rar-schnbonn
https://coub.com/stories/3008942-__top__-rslogix-500-software-crack-11
https://coub.com/stories/3008939-new-altium-file-type-not-recognized
https://coub.com/stories/3008937-updated-autosplitter-full-version-with-crack
https://coub.com/stories/3008938-exclusive-jazz-guitar-voicings-randy-vincent-pdf-35
https://coub.com/stories/3008924-keygen-fatek-plc-password-break-rar-work
https://coub.com/stories/3008934-adobe-after-effects-cc-2017-v14-1-0-x64-incl-crack-portable-utorrent-weldjen
https://coub.com/stories/3008932-coreldraw-graphics-suite-x8-18-0-0-448-keygen-pennwal
https://coub.com/stories/3008933-ganamrutha-bodhini-tamil-pdf-free-18-better
https://coub.com/stories/3008931-wifree-connect-crack-verified
https://coub.com/stories/3008930-hot-the-last-airbender-3-movie-in-mp4-tamil-free-download
https://coub.com/stories/3008927-exclusive-codigo-registro-elifoot-2011rar
https://coub.com/stories/3008925-best-fe-review-manual-3rd-edition-pdf-zip
https://coub.com/stories/3008923-full-hd-video-songs-1080p-hindi-ishq-junoon-onitobb
https://coub.com/stories/3008920-__top__-make-drones-teach-an-arduino-to-fly-downloads-torrent
kahcou (Thursday, 27 January 2022 17:13)
kahcou d868ddde6e https://coub.com/stories/2985571-link-sonnenfreunde-magazine
https://coub.com/stories/2985570-solucionario-meriam-estatica-3-edicion-lavemald
https://coub.com/stories/2985567-install-trackmania-2-canyon-crack-only-download-couples
https://coub.com/stories/2985569-subdivide-and-smooth-plugin-sketchup-rar-upd
https://coub.com/stories/2985565-all-alone-full-movie-download-in-hd-720p-install
https://coub.com/stories/2985563-comport-for-android-usb-2-6-xe6-d10-2-hot
https://coub.com/stories/2985561-descargar-radar-10-homeopatia-gratis-upd
https://coub.com/stories/2985559-princess-lover-game-patch-english-rar-updated
https://coub.com/stories/2985558-link-esail-sailing-simulator-crack-gamehackstudios
https://coub.com/stories/2985551-natural-reader-full-version-crack-free-513-hanzur
https://coub.com/stories/2985550-cinci-eroi-de-legenda-dublat-in-romana-_top_
https://coub.com/stories/2985549-network-topology-mapper-solarwinds-crack-full-verified
https://coub.com/stories/2985552-governor-of-poker-2-premium-edition-crack-mac-evaisa
https://coub.com/stories/2985548-2021-luxonix-purity-vst-64-bits99
https://coub.com/stories/2985545-godhi-banna-sadharana-mykattu-2016-kannada-320kbps-sri-ninjan
https://coub.com/stories/2985546-daag-the-fire-movie-link-download-in-hindi-720p-hd-kickass
https://coub.com/stories/2985547-eze-bootable-usb-v0-0-0-2-by-orbit30-download-tasphee
https://coub.com/stories/2985539-d-guard-anti-ddos-firewall-full-verified-crack-5-23-for-windows
https://coub.com/stories/2985541-investigacion-de-operaciones-wayne-l-winston-solucionario-__link__
https://coub.com/stories/2985542-remington-788-serial-number-lookup-better
https://coub.com/stories/2985540-autocad-2015-english-win-64bit-dlmsfx22
https://coub.com/stories/2985536-business-in-a-box-crack-top-serial-keygen-90golkes
https://coub.com/stories/2985535-microsoft-toolkit-2-6-4-for-windows-and-office-activation-download-pc-tamfenn
https://coub.com/stories/2985534-lesson-7-homework-practice-subtract-linear-expressions-jymmver
https://coub.com/stories/2985533-repack-keygen-objectdock-plus-serial-number
https://coub.com/stories/2985532-heroglyph-4-licence-mtkey
https://coub.com/stories/2985530-18-the-klub-17-v7-4l
https://coub.com/stories/2985528-if-i-were-a-boy-duet-beyonce-and-r-kelly-mp3-best-download
https://coub.com/stories/2985527-cbt-nuggets-microsoft-system-center-configuration-manager-sccm-2012-70-243-plato-__hot__
https://coub.com/stories/2985525-torrent-ciel-compta-2013-crack-better-musketier-happy-vidi
fallphyl (Thursday, 27 January 2022)
fallphyl d868ddde6e https://coub.com/stories/2967494-crack-windows-7-sp1-aio-x86x64-11in1-en-us-may2016-incl-activator-t-chahau
https://coub.com/stories/2967495-repack-revealerkeyloggerproeditioncracked
https://coub.com/stories/2967496-project-igi-1-cheat-codes-full-version-deatrys
https://coub.com/stories/2967493-avalon-direct-english-book-2-teacher-handbook-pdf-link
https://coub.com/stories/2967492-ulead-photoimpact-x3-full-hot-addons-rar
https://coub.com/stories/2967491-pictocolor-icorrect-editlab-pro-6-0-eng-photoshop-plugin-full-version-work
https://coub.com/stories/2967487-visual-paradigm-free-license-hot
https://coub.com/stories/2967486-new-simplify3d-4-1-2-crack-download-here
https://coub.com/stories/2967484-ramayana-the-epic-hindi-movie-3gp-download-halayar
https://coub.com/stories/2967483-__hot__-flexisign-pro-6-5-free-download
https://coub.com/stories/2967482-pb-downforce-0-3-3-1-anti-ban-sxe-11-6-113l-top
https://coub.com/stories/2967480-the-great-escape-1963-720p-hdtv-x264-vice-mkv-flodagw-129311
https://coub.com/stories/2967478-new-full-nero-2017-platinum-18-0-06100-incl-serial-key-content-pack
https://coub.com/stories/2967477-adeko-x-full-indir-fix
https://coub.com/stories/2967474-xforce-keygen-64-bits-autocad-electrical-2019-descargar-natelle
https://coub.com/stories/2967475-top-spandrio-biochimica-clinica-pdf
https://coub.com/stories/2967471-sims4_hot_-cracknoorigin
https://coub.com/stories/2967470-clave-de-licencia-smart-driver-updater
https://coub.com/stories/2967472-alexandra-ledermann-6-no-dvd-epub-ursuwyan
https://coub.com/stories/2967466-shaurya-movie-download-hd-1080p-kickass-torrent-bremart
https://coub.com/stories/2967469-boris-fx-sapphire-2019-04-adobe-ofx-crack-372-mb-dagwatte
https://coub.com/stories/2967468-superior-drummer-sdx-__top__-keygen-crack
https://coub.com/stories/2967464-link-microsoft-photodraw-2000-v2-serial-key
https://coub.com/stories/2967463-devil-may-cry-4-dx9-dx10-no-dvd-crack-full-7z
https://coub.com/stories/2967462-exclusive-hajra-choudhary-workshop-technology-vol-2-pdf-free-download
https://coub.com/stories/2967460-new-chef-de-partie-cv-pdf-download
https://coub.com/stories/2967456-mount-and-blade-warband-serial-key-generator-talvari
https://coub.com/stories/2967455-hd-online-player-download-ulead-video-studio-12-full-frigia
https://coub.com/stories/2967454-kingsoft-office-2012-pro-12-better
https://coub.com/stories/2967452-verified-download-do-livro-tratado-de-anatomia-veterinaria-dyce-sack-rar
guasar (Thursday, 27 January 2022 19:22)
guasar d868ddde6e https://coub.com/stories/3006937-free-download-template-undangan-corel-draw-x4-verified
https://coub.com/stories/3006934-descargar-cyber-admin-control-con-crack-__link__
https://coub.com/stories/3006933-patched-articulate-storyline-2-8-1605-515-crack-sadeempc-weltere
https://coub.com/stories/3006932-fix-bigben-interactive-ps3pad-drivers
https://coub.com/stories/3006931-best-layers-in-revit-2013-crack
https://coub.com/stories/3006927-free-krantiveer-full-movie-hd-download-720p
https://coub.com/stories/3006925-__exclusive__-revo-uninstaller-pro-4-2-0-patch
https://coub.com/stories/3006924-best-download-windows-7-alienware-32-bit-iso-torrent-best-download
https://coub.com/stories/3006923-uplay-skidrow-account-password
https://coub.com/stories/3006921-simplo-automotivo-2012-crackeado-new
https://coub.com/stories/3006920-foto-kontol-orang-indonesia-olachri
https://coub.com/stories/3006918-madras-cafe-movie-hot-full-download-in-hindi
https://coub.com/stories/3006916-link-download-filme-com-merito-dublado
https://coub.com/stories/3006915-libro-trabajo-y-ciudadania-editorial-maipue-pdf-371-brankame
https://coub.com/stories/3006914-vorwerk-libretto-di-istruzione-bimby-modello-tm-21
https://coub.com/stories/3006909-eca-vrt-dvd-2009-crack-rar-repack
https://coub.com/stories/3006908-kannada-nudi-typing-master-software-free-download-nanhar
https://coub.com/stories/3006906-vrigger-8-0-keygen-crack-wisfin
https://coub.com/stories/3006904-kannada-tunne-tullu-kathegalu-pdf-janlawl
https://coub.com/stories/3006900-2021-outlook-lan-messenger-5-0-2-for-windows
https://coub.com/stories/3006901-analog-devices-1981b-l-intel-82801eb-ich5-ac-97-audio-controller-a-2-a-3-pci-rapidshare-repack
https://coub.com/stories/3006899-bloody2-ultra-core3-activate-code
https://coub.com/stories/3006898-install-download-abb-robotstudio-v5-07-01-by-mjk-rar-5
https://coub.com/stories/3006897-srs-audio-sandbox-1-10-2-0-patch
https://coub.com/stories/3006896-win8woh-zip
https://coub.com/stories/3006895-gonit-ebong-aro-gonit-pdf-download-erorewa
https://coub.com/stories/3006893-maps-for-navigation-rns-315-free-download-bellosen
https://coub.com/stories/3006892-ism-3-0-keyboard-driver-for-windows-7-free-download-rar-patched
https://coub.com/stories/3006891-aadukalam-full-movie-hd-1080p-blu-ray-hot
https://coub.com/stories/3006890-download-__top__-msxml-version-6-10-11-29-0-microsoft-grat-abenteuerspiele-kauf
heidatt (Thursday, 27 January 2022 20:18)
heidatt d868ddde6e https://coub.com/stories/2945818-x-force-civil-3d-2010-crack-new
https://coub.com/stories/2945815-bernina-embroidery-software-7-crack-11-rhyflo
https://coub.com/stories/2945814-upd-vray-19-64-bit-for-c4d-r15-keygen-xforce-chingliu
https://coub.com/stories/2945813-hd-online-player-charlie-2015-malayalam-1080p-blu-ray-dts-x264-8gb-esubs-extra-quality
https://coub.com/stories/2945812-memturbo-4-1-0331-portable-cracked-download-ellgill
https://coub.com/stories/2945811-gamemaker-studio-2-desktop-download-by-utorrent-top
https://coub.com/stories/2945809-psihologia-copilului-pantelimon-golu-pdf-14-badcher
https://coub.com/stories/2945810-official-leagoo-t10-mediatek-mt6797-stock-rom-exclusive
https://coub.com/stories/2945807-hd-online-player-shootout-at-wadala-full-movie-torren-orsell
https://coub.com/stories/2945806-cara-pro-v1-4-homeopathic-software-best-crack-12
https://coub.com/stories/2945805-paragon-extfs-for-windows-hot-keygen
https://coub.com/stories/2945804-bossgt100patchespinkfloyd
https://coub.com/stories/2945803-shaiya-viper-next-generation-download-new
https://coub.com/stories/2945802-apowersoft-video-converter-studio-8-11-4-crackl-chazac
https://coub.com/stories/2945801-kreith-principios-de-transferencia-de-calor-pdf-63-new
https://coub.com/stories/2945800-ixl-stereo-analyzer-free-__hot__
https://coub.com/stories/2945799-thrausi-1-36-cinema-4d-plugin-download-quedmant
https://coub.com/stories/2945798-total-av-antivirus-2020-crack-serial-key-lifetime-here-new
https://coub.com/stories/2945797-hoi4-save-game-editor-install
https://coub.com/stories/2945796-pagani-salsa-analisi-matematica-2-pdf-2021-download
https://coub.com/stories/2945795-link-net-monitor-for-employees-professional-5-5-7-crack-keygen-download
https://coub.com/stories/2945794-epson-me-office-620f-adustment-program-rar
https://coub.com/stories/2945793-humantechnik-infralight-lr-operating-instructions-manual-upd
https://coub.com/stories/2945792-autodesk-inventor-professional-2020-1-1-win-x64-wangra
https://coub.com/stories/2945790-batman-bajo-la-capucha-roja-1080p
https://coub.com/stories/2945789-top-mtk-reader-v1-0-0-169
https://coub.com/stories/2945787-zokkomon-full-free-movies-720p-torrent
https://coub.com/stories/2945788-crack-gear-generator-3-14-wattan
https://coub.com/stories/2945784-2021-crazytalk-animator-training-dvd-download-torrent
https://coub.com/stories/2945786-defraggler-pro-2018-latest-key-crack-keygen-free-download-movievon
kaylnik (Thursday, 27 January 2022 21:18)
kaylnik d868ddde6e https://coub.com/stories/2976682-barbie-princess-charm-school-high-quality-full-movie-dubbed-in-hindi-19
https://coub.com/stories/2976681-compaq-presario-cq57-recovery-disk-zip-verified
https://coub.com/stories/2976678-free-dhoom-2-telugu-full-movie-free-download-19
https://coub.com/stories/2976677-powermill-2013-crack-top-xforce-64
https://coub.com/stories/2976675-hetman-file-repair-keygen-download-brikei
https://coub.com/stories/2976673-express-vpn-2020-crack-with-license-key-free-download-2019-googfaye
https://coub.com/stories/2976671-verified-robot-vision-berthold-horn-pdf-download
https://coub.com/stories/2976669-securom-failed-to-initialize-fifa-manager-13-keygen-winhart
https://coub.com/stories/2976668-adobe-acrobat-pro-dc-2015-020-20042-incl-crack-sadeempc-full-version-top
https://coub.com/stories/2976666-sony-vegas-pro-14-78-build-298-patch-crack-bertdory
https://coub.com/stories/2976665-peretti-metodo-per-tromba-pdf-download-install
https://coub.com/stories/2976662-interstellar-full-movie-in-hindi-download-720p-sarider
https://coub.com/stories/2976661-war-thunder-v-1-43-7-49-eng-rus-l-corepack-gaurena
https://coub.com/stories/2976659-visualizer-3d-okm-keygen-generatorl-hot
https://coub.com/stories/2976658-como-sobrevivir-a-un-apocalipsis-zombie-libro-pdf-11-carjenn
https://coub.com/stories/2976654-ratiborus-kms-tools-01-04-2018
https://coub.com/stories/2976655-extra-quality-chris-pc-lock-v2-60-yag
https://coub.com/stories/2976650-hd-online-player-sanam-teri-kasam-telugu-movie-english-subtitles-download-free-torrentgolkes
https://coub.com/stories/2976649-__hot__-comic-life-3-5-12-full-version-crack-download-win
https://coub.com/stories/2976648-autod-2-eesti-keeles-film-21-brecas
https://coub.com/stories/2976646-repack-intuit-turbotax-2018-deluxe-serial-key-keygen
https://coub.com/stories/2976644-frontschweine-vollversion-kostenlos-casober
https://coub.com/stories/2976643-repack-jazler-radiostar-2-7-crack-14
https://coub.com/stories/2976642-new-vvvvvv-v2-2-pc-full-fas-pc-game
https://coub.com/stories/2976641-portable-crack-ableton-live-8-v8-0-1
https://coub.com/stories/2976640-engineering-mechanics-basudeb-bhattacharyya-pdf-download-marekaf
https://coub.com/stories/2976638-rally-trophy-download-full-version-19-gartran
https://coub.com/stories/2976625-allegro-free-top-viewer-16-6-download
https://coub.com/stories/2976635-free-caddproj-s8-eletrica-crack-653
https://coub.com/stories/2976634-fixed-s5s7forwindowsv7downloadcracksoftware
darhani (Thursday, 27 January 2022 23:15)
darhani d868ddde6e https://coub.com/stories/3070083-contingency-ff-mw2-dir-file-extra-quality-download
https://coub.com/stories/3070081-fixed-atris-technik-1q-2015-68
https://coub.com/stories/3070080-hot-bana-masal-anlatma-720p-51
https://coub.com/stories/3070079-full-recap-pro-2019-free-download-best
https://coub.com/stories/3070078-2021-how-to-make-your-own-megalovania
https://coub.com/stories/3070077-how-to-undo-on-grammarly-fixed
https://coub.com/stories/3070076-embarcadero-rad-studio-xe5-architect-crack-28-tibemar
https://coub.com/stories/3070075-akuntansi-perpajakan-sukrisno-agoes-pdf-57-verified
https://coub.com/stories/3070074-free-download-video-cutter-and-joiner-with-crackinstmank
https://coub.com/stories/3070073-muhsin-demirci-tefsir-tarihi-pdf-11
https://coub.com/stories/3070072-top-production-editing-toolbar-arcgis-download
https://coub.com/stories/3070071-updated-fsx-gsx-crack-rar
https://coub.com/stories/3070069-babado-forte-erika-palomino-pdf-19
https://coub.com/stories/3070067-t-spline-solidworks-crack-23-best
https://coub.com/stories/3070068-solucionario-de-fisica-alonso-acosta-tomo-1-high-quality
https://coub.com/stories/3070066-command-and-conquer-renegade-no-cd-crack-better-4-0-scripts-skidrow
https://coub.com/stories/3070065-como-quitar-la-censura-a-3d-sexvilla-2golkes-portable
https://coub.com/stories/3070064-ironmanthegamecrackiso-petrimo
https://coub.com/stories/3070063-keygen-magix-music-maker-15-activation-codel-_best_
https://coub.com/stories/3070061-shin-kanzen-master-n3-pdf-downloadgolkes-repack
https://coub.com/stories/3070059-hd-online-player-anniyan-full-movie-hd-1080p-bluray-t-new
https://coub.com/stories/3070060-debajyoti-das-biochemistry-pdf-147
https://coub.com/stories/3070057-hot-movavi-video-suite-key
https://coub.com/stories/3070058-toyota-tns310-traffic-plus-dvdrar-fulfbets
https://coub.com/stories/3070056-verified-s5s7forwindowscrackkey
https://coub.com/stories/3070055-nuendo-6-with-activation-key-wandemal
https://coub.com/stories/3070054-city-car-driving-mod-installer-__hot__
https://coub.com/stories/3070053-worknc-v21-free-crack-verified
https://coub.com/stories/3070052-better-the-sims-medieval-2-0-113-crack-tpb
https://coub.com/stories/3070051-adobe-acrobat-xi-pro-serial-number-generator
cathela (Friday, 28 January 2022 00:13)
cathela d868ddde6e https://coub.com/stories/3118995-magix-movie-edit-pro-2019-plus-18-0-1-207-with-crack-serial-key-janile
https://coub.com/stories/3116542-delphi-auto-diagnostic-software-torrent-116-link
https://coub.com/stories/3116541-edius-6-02-serial-number-halleof
https://coub.com/stories/3116540-a360-2018-64bit-product-key-and-xforce-keygen-rar-patched
https://coub.com/stories/3116539-my-system-aron-nimzowitsch-free-pdf-upd-download
https://coub.com/stories/3116537-kernel-for-ost-to-pst-full-crack-better
https://coub.com/stories/3116538-install-gramatica-teoria-e-exercicios-paschoalin-e-spadoto-pdf-34
https://coub.com/stories/3116535-cfosspeed-10-50-2338-crack-serial-key-keygen-softwtare-for-mac-windows-valyov
https://coub.com/stories/3116536-reaper-v2-58-echo-rar-updated
https://coub.com/stories/3116534-geet-gata-chal-hindi-movie-free-12-extra-quality
https://coub.com/stories/3116533-_top_-scorpion-king-2-movie-in-hindi-free-19
https://coub.com/stories/3116532-hd-online-player-slumdog-millionaire-full-movie-in-hi-eidalli
https://coub.com/stories/3116531-x-particles-c4d-torrent
https://coub.com/stories/3116530-follow-liker-free-cracked-40-wartcin
https://coub.com/stories/3116529-appgini-professional-edition-zip-_verified_
https://coub.com/stories/3116527-pc-life-is-feudal-your-own-eng-0-2-4-2-corepack-thekgord
https://coub.com/stories/3116528-free-gerber-accumark-82-crack-83
https://coub.com/stories/3116526-k53-leerlinglisensie-vraestelle-pdf-42-better
https://coub.com/stories/3116525-exclusive-captainsim737200fsxtorrent
https://coub.com/stories/3116524-wintrack-v110-3d-full-top-505
https://coub.com/stories/3116522-kitab-terjemahan-fiqh-manhaji-pdf
https://coub.com/stories/3116523-il-pirata-barbanera-gioco-pc-dow
https://coub.com/stories/3116521-new-gujarat-earthquake-essay
https://coub.com/stories/3116520-guerrini-superior-2-accordion-for-ni-kontakt-crack-free
https://coub.com/stories/3116519-cracked-celemony-melodyne-studio-3-2-2-2-keygen-generator
https://coub.com/stories/3116518-empires-of-the-undergrowth-full-crack-license-link
https://coub.com/stories/3116517-bluesoleil-10-crack-keygen-download-free
https://coub.com/stories/3116516-__full__-corel-gallery-magic-1-000-000
https://coub.com/stories/3116515-auto-tune-8-ilok-crack-mac-bihjrose
https://coub.com/stories/3116514-700-flash-games-in-one-file-rar-generator-online
fairwan (Friday, 28 January 2022 01:12)
fairwan d868ddde6e https://coub.com/stories/2933035-2021-residentevil5re5dx9exedownloadhit
https://coub.com/stories/2933036-_top_-patched-easeus-partition-master-5-8-1-server-edition-portable
https://coub.com/stories/2933034-fixed-manualul-apicultorului-incepator-pdf-download
https://coub.com/stories/2933033-final-fantasy-xiv-online-pc-crack-sadida
https://coub.com/stories/2933032-unitek-usb-to-serial-driver-windows-7-43-fix
https://coub.com/stories/2933031-hd-online-player-casino-royale-__exclusive__-full-movie-hindi-dubbe
https://coub.com/stories/2933030-boris-godunov-libretto-russian-edition-modest-petrovich-mussorgsky-2021
https://coub.com/stories/2933029-netframework-v4-0-303-19-rar-2021
https://coub.com/stories/2933028-verified-the-klub-17-7-4
https://coub.com/stories/2933027-link-keygen-autocom-delphi-2012-3
https://coub.com/stories/2933026-link-edgar-baqueiro-rojas-derecho-civil-introduccion-personas-pdf-download
https://coub.com/stories/2933025-blackpantherenglishmp3songsfreedownload-gennkam
https://coub.com/stories/2933024-wondershare-dr-fone-for-android-9-8-1-final-serials-rar-willdawa
https://coub.com/stories/2933023-crack-keygen-autocad-plant-3d-2019-portable
https://coub.com/stories/2933022-crack-adobe-muse-cc-2014-8-0-multilanguage-64-bit-patch-best
https://coub.com/stories/2933021-exclusive-download-windows-7-ultimate-boot-loader-torrent
https://coub.com/stories/2933020-trials-in-tainted-space-cheats-debeerl
https://coub.com/stories/2933019-data-doctor-recovery-sim-card-5-3-1-2-crack-exclusive
https://coub.com/stories/2933018-put-mirnog-ratnika-pdf-new-download
https://coub.com/stories/2933017-napro-pc-scan-3000-__full__-crack-61
https://coub.com/stories/2933016-portable-teknogods-codmw3-update-2-7-0-9-re-pack-zomb413-edition-with-lucky-patcher
https://coub.com/stories/2933015-true-philippine-ghost-stories-pdf-download-exclusive
https://coub.com/stories/2933014-aarteeacienciadememorizartudo
https://coub.com/stories/2933013-link-courage-the-cowardly-dog-full-episodes-torrent
https://coub.com/stories/2933012-teamspeak3privilegekeygenerator-blamak
https://coub.com/stories/2933011-127-hours-hd-tamil-movie-free-download-free
https://coub.com/stories/2933010-eurovision-2013-320kbps-torrent
https://coub.com/stories/2933009-fifa-15-ultimate-team-edition-repack-by-corepack
https://coub.com/stories/2933008-stradacard-v2-better
https://coub.com/stories/2933007-best-kasthuri-nivasa-movie-songs-download
glagiov (Friday, 28 January 2022 02:10)
glagiov d868ddde6e https://coub.com/stories/3035537-crack-rosetta-stone-french-1-2-language-disc-iso-s0ilw0rk-hot
https://coub.com/stories/3035535-hum-dil-de-chuke-sanam-the-movie-720p-download-exclusive
https://coub.com/stories/3035536-crackautocadlt2007activation-gerenav
https://coub.com/stories/3035532-aiyingyong-pc-v4-6-4-epub
https://coub.com/stories/3035534-portraitpro-19-0-5-crack-with-serial-key-2020-neiurba
https://coub.com/stories/3035533-mg-mu-client-tools-download-install
https://coub.com/stories/3035531-upd-coreldraw-graphics-suite-x6-v-16-1-0-843-x86-ita-serial-key
https://coub.com/stories/3035530-bitshare-crysis-3-highly-compressed-10mb-free-download-full-for-pc-6-free
https://coub.com/stories/3035529-link-hd-online-player-khiladi-kolkata-bangla-full-movie-do
https://coub.com/stories/3035528-vcds-lite-1-1-crack-rar-better
https://coub.com/stories/3035527-exclusive-naruto-the-last-movie-download-english-sub-kickassl
https://coub.com/stories/3035526-exclusive-lockdir-registration-key-full-rar
https://coub.com/stories/3035525-descargar-zooskool-de-jovencitas-con-perros-gratis-mega
https://coub.com/stories/3035523-mentor-pads-9-5-torrent-top
https://coub.com/stories/3035524-extra-quality-tmpgenc-authoring-works-5-jp-keygen-best
https://coub.com/stories/3035518-sap-ecc-v6-0-sr3-ides-oracle-10-2-0-2-64-bit
https://coub.com/stories/3035521-family-tree-maker-2006-iso-setup-free-chammar
https://coub.com/stories/3035519-proshow-producer-templates-free-download-for-wedding-install
https://coub.com/stories/3035517-rtl-racing-team-manager-no-cd-crack-marcshan
https://coub.com/stories/3035516-omsi-2-add-on-urbino-stadtbusfamilie-download-portable-edition-otthnik
https://coub.com/stories/3035515-sonyacidpro40keygendownloadcrack-tabufayg
https://coub.com/stories/3035514-hablemos-de-amor-walter-riso-pdf
https://coub.com/stories/3035513-disney-fairies-tinker-bell-s-adventure
https://coub.com/stories/3035512-best-xforce-keygen-alias-speedform-2017-64-bit-windows-10
https://coub.com/stories/3035509-leica-geo-office-tools-64-bit-free-download-l-vivijaq
https://coub.com/stories/3035508-download-keygen-xforce-for-autocad-electrical-2012-keygen-weljens
https://coub.com/stories/3035507-artcam-2017-keygen-only-xforce-gondisl
https://coub.com/stories/3035506-compegps-land-7-0-1-crack-top
https://coub.com/stories/3035505-3d-pageflip-professional-1-6-2-crack-repack-ed
https://coub.com/stories/3035504-family-tree-maker-v2012-iso-lz0
tulegeer (Friday, 28 January 2022 03:07)
tulegeer d868ddde6e https://coub.com/stories/2935481-dragon-essence-color-my-world-free-download-patched-pc
https://coub.com/stories/2935479-advanced-office-password-recovery-full-version-free-portable
https://coub.com/stories/2935478-__exclusive__-download-origin-8-0-full-crack
https://coub.com/stories/2935477-grassington-north-yorkshire-lxk-link
https://coub.com/stories/2935476-imgsrc-ru-kids-1
https://coub.com/stories/2935475-downloadmastercamx9fullcracksoftware-hasameli
https://coub.com/stories/2935474-sidefxhoudinifx17windowscrackdownload-isidal
https://coub.com/stories/2935473-cheeni-kum-hindi-dubbed-720p-__link__
https://coub.com/stories/2935472-link-xforce-keygen-maya-2015-key
https://coub.com/stories/2935471-saathiya-2-free-download-top-in-hindi
https://coub.com/stories/2935470-adobe-premiere-pro-cc-crack-german-vukmleve
https://coub.com/stories/2935469-gearhead-garage-windows-7-full-download-eiribai
https://coub.com/stories/2935468-super-fast-shutdown-1-0-setup-free-top
https://coub.com/stories/2935467-_verified_-transoft-solutions-autoturn-pro-3d-8-1-1-200-13
https://coub.com/stories/2935466-updated-daf-kompakt-a1-b1-arbeitsbuch-pdf-18
https://coub.com/stories/2935465-solucionario-levine-quimica-cuantica
https://coub.com/stories/2935464-microsoft-office-2010-activator-iorrt-3-5-torrent
https://coub.com/stories/2935463-new-iobit-driver-booster-pro-2-3-1-1-2015-serial-key
https://coub.com/stories/2935462-world-constitutions-by-kaeley-pdf-19-exclusive
https://coub.com/stories/2935461-re-loader-activator-3-3-windows-office-full-version-clarwal
https://coub.com/stories/2935460-free-code-akses-maksi-pro-epub
https://coub.com/stories/2935458-__full__-armedia-plugin-for-autodesk-3ds-max-crack-downloadl
https://coub.com/stories/2935459-jazler-radiostar-2-6-4-full-_verified_-crack-download-portable
https://coub.com/stories/2935457-telecharger-patch-diagbox-v701-hot
https://coub.com/stories/2935455-autos-bauen-mit-willy-werkel-rar
https://coub.com/stories/2935456-psychology-from-inquiry-to-understanding-4th-edition-books-pdf
https://coub.com/stories/2935454-adele-live-at-the-royal-albert-hall-2011-mkv-1080p-dts-hd-bd-rip-mw68-new
https://coub.com/stories/2935453-diagnoza-psychopedagogiczna-jarosz-wysocka-pdf-free-link
https://coub.com/stories/2935452-patched-adobe-indesign-cc-2018-v24-0-1-215-crack-garryua
https://coub.com/stories/2935450-download-portable-ebook-100-tokoh-yang-mewarnai-jakarta-dki
eravla (Friday, 28 January 2022 04:04)
eravla d868ddde6e https://coub.com/stories/3144219-we-the-skythians-pdf-kalayia
https://coub.com/stories/3144217-bootloader-error-id-1-miracle-box-56
https://coub.com/stories/3144218-solucionario-paula-yurkanis-fundamentos-de-la-quimica-organicarar-best
https://coub.com/stories/3144216-fixed-cerita-sex-ngentot-ummahat
https://coub.com/stories/3144215-better-activation-id-for-srs-hd-audio-lab
https://coub.com/stories/3144214-better-photoprint-server-pro-5-0v2-12
https://coub.com/stories/3144213-portrait-wizard-crack-by-razor1911-download-top
https://coub.com/stories/3144212-top-cryengine-3-sdk-3-4-5-crack-offline
https://coub.com/stories/3144211-hd-online-player-jack-the-giant-slayer-hindi-dubbed-m-hansdar
https://coub.com/stories/3144209-mims-medical-microbiology-5th-edition-pdf-free-download-__top__
https://coub.com/stories/3144206-waves-one-knob-series-au-vst-vst3-rtas-tdm-mac-osx-intel-rar-lavrmau
https://coub.com/stories/3144204-better-bus-simulator-2012-english-patch-1-2-4
https://coub.com/stories/3144203-full-dump-original-vision-x215-series-ali-c-zip
https://coub.com/stories/3144201-gijom-muso-pdf-knjige-download-ningmea
https://coub.com/stories/3144200-full-vray-mac-4-0-crack-keygen-next-for-sketchup-2019-download
https://coub.com/stories/3144199-download-film-secretary-2002-soundtrack-install
https://coub.com/stories/3144196-japan-dating-raynico
https://coub.com/stories/3144197-downloadsap2000advancedv12patchcrack-top
https://coub.com/stories/3144194-kmspico-12-2-9-final-portable-office-and-windows-10-activator-rexsim
https://coub.com/stories/3144192-hd-online-player-no-problem-full-movie-hd-1080p-hindi-repack
https://coub.com/stories/3144190-autocad-2015-crack-xforce-better-32
https://coub.com/stories/3144191-high-quality-riptide-gp-renegade-download-for-pc-key
https://coub.com/stories/3144189-vishram-singh-anatomy-head-and-neck-pdf-download-install
https://coub.com/stories/3144186-bpm-studio-pro-5-01-multilanguage-pack-26-anofae
https://coub.com/stories/3144185-jagged-alliance-back-in-action-trainer-113g-download-upd
https://coub.com/stories/3144183-verified-sims-4-puberty-mod
https://coub.com/stories/3144178-unigraphics-nx-nx-8-torrent
https://coub.com/stories/3144181-2021-hum-dono-full-movie-download-hd-720p
https://coub.com/stories/3144179-netsupport-manager-v12-keygen-24-delkaf
https://coub.com/stories/3144180-extra-quality-deewaar-movie-download-in-hindi-hd-720p
shangar (Friday, 28 January 2022 05:00)
shangar d868ddde6e https://coub.com/stories/3143267-hyip-lister-pro-nulled-script-poinalb
https://coub.com/stories/3143265-link-jang-e-badar-ka-waqia-urdu-pdf-22
https://coub.com/stories/3143258-roxio-creator-2012-pro-keygen-rar-top
https://coub.com/stories/3143263-baixar-contagem-regressiva-dublado-720p-octmak
https://coub.com/stories/3143261-_best_-download-video-bugil-cewek-usia-8-tahun-indonesia-3gp
https://coub.com/stories/3143262-analog-electronics-jb-gupta-pdf-free-download-sharbrad
https://coub.com/stories/3143255-sadqay-tumhare-novel-pdf-free-download-upd
https://coub.com/stories/3143259-top-moorman-s-book-of-poker-free-download
https://coub.com/stories/3143254-verified-handy-backup-professional-7-crack-full
https://coub.com/stories/3143251-r4i3d-multi-com-v2-1-58
https://coub.com/stories/3143250-__top__-nch-wavepad-sound-editor-masters-edition-v7-05-crack-free-download
https://coub.com/stories/3143248-command-and-conquer-red-alert-3-uprising-english-l-fiorello-cavallo-dif-hectwin
https://coub.com/stories/3143249-easyusetool-frontend-0514-rar-top
https://coub.com/stories/3143243-download-patched-burnin-rubber-4-pc
https://coub.com/stories/3143242-pilgrim-treasure-island-sample-library-wav-link
https://coub.com/stories/3143240-benq-siemens-e61-driver-download-link
https://coub.com/stories/3143241-top-advance-steel-2017-x64-key-download-pc
https://coub.com/stories/3143239-patched-crack-zktime-lite-eu-tested
https://coub.com/stories/3143237-new-the-sims-3-le-cirque-celebration-set-download
https://coub.com/stories/3143236-heli-x-flight-simulator-crack-upd
https://coub.com/stories/3143235-nekojishi-full-crack-garchas
https://coub.com/stories/3143234-2021-hero-tamil-movie-720p-download
https://coub.com/stories/3143232-frm-part-2-schweser-pdf-download-new
https://coub.com/stories/3143233-best-service-era-medieval-legends-engine-2-utorrent-repack
https://coub.com/stories/3143231-archicad-14-crack-patch-francais-gratuit-kaslau
https://coub.com/stories/3143228-repack-ferrari-virtual-academy-v1-3-hack-tool-free-download
https://coub.com/stories/3143227-yamicsoft-windows-10-manager-v2-2-0-final-keygen-verified-sh
https://coub.com/stories/3143226-weekly-math-homework-q1-2-answer-key
https://coub.com/stories/3143225-better-abhiram-ranade-c-pdf
https://coub.com/stories/3143222-hd-online-player-download-shaadi-mein-zaroor-aana-movie-torrent-1080p-better
eneund (Friday, 28 January 2022 05:57)
eneund d868ddde6e https://coub.com/stories/2947046-autocad-2015-et-covadis-2015-zip-exclusive
https://coub.com/stories/2947044-link-yanni-live-1080p-torrent
https://coub.com/stories/2947040-free-download-ebook-for-mobile-computing-shanfol
https://coub.com/stories/2947043-ip-man-3-subtitles-english-download-fix
https://coub.com/stories/2947042-topaz-denoise-5-full-hot-crack-internet
https://coub.com/stories/2947041-hack-bittorrent-pro-7-9-9-build-42924-stable-incl-link-crack-portable
https://coub.com/stories/2947039-arcview-3-2-para-windows-7-64-bits-descargar
https://coub.com/stories/2947038-ultraiso-premium-v9-5-3-2901-incl-keygen-mesmerize-exclusive
https://coub.com/stories/2947037-download-3d-sexvilla-2-everlust-full-crack-torrentl-verified
https://coub.com/stories/2947036-best-full-hirens-boot-dvd-15-2-restored-edition-1-1-january-2013
https://coub.com/stories/2947035-repack-crucc-2-4-car-radio-universal-code-calculator-zip-psychologie-beamer-b
https://coub.com/stories/2947034-whiplashmoviedownloadinhindi-markflem
https://coub.com/stories/2947033-pixedit-7-updated-crack
https://coub.com/stories/2947032-new-hasan-bin-sabbah-in-urdu-pdf-free
https://coub.com/stories/2947026-download-novela-zorro-a-espada-e-a-rosa-dublado-portugues-40-16-__full__
https://coub.com/stories/2947030-recover-my-files-v4-6-8-1012-license-key-free-download-zip-full
https://coub.com/stories/2947029-psa-diagbox-crack-new
https://coub.com/stories/2947028-avatar-the-last-airbender-all-episodes-tamil-dubbed-torrent-ladwhe
https://coub.com/stories/2947027-download-chicken-invaders-6-myegy-best
https://coub.com/stories/2947025-pc-command-and-conquer-tiberian-sun-no-cd-patch-from-skafa-crack-top
https://coub.com/stories/2947023-xforce-keygen-32-bit-autocad-lt-2019-new
https://coub.com/stories/2947024-wps-office-10-premium-business-edition-crack-serial-key-patched
https://coub.com/stories/2947022-updated-download-bellas-lullaby-in-twilight
https://coub.com/stories/2947021-dishkiyaoon-full-hindi-movie-download-free-in-hd-3gp-mp4-jandar
https://coub.com/stories/2947020-haan-maine-bhi-pyaar-kiya-full-movie-in-hindi-1080p-hd-exclusive
https://coub.com/stories/2947019-phpstorm-license-server-crack-fixed-games
https://coub.com/stories/2947018-fifa-14-crack-only-v5-final-3dm-yelladri
https://coub.com/stories/2947017-the-polar-express-full-mp4-movie-in-hindi-downloadl-free
https://coub.com/stories/2947016-getdata-recover-my-files-pro-v5-2-1-58
https://coub.com/stories/2947015-link-hd-online-player-everest-2015-720p-bluray-x264-dua
arylat (Friday, 28 January 2022 06:54)
arylat d868ddde6e https://coub.com/stories/2952761-crack-exclusive-autocad-2008-windows-7-32-bit
https://coub.com/stories/2952760-verified-revit-lt-2010-32bit-product-key-and-xforce-keygen-rar
https://coub.com/stories/2952758-first-year-engineering-drawing-by-ac-parkinson-pdf-free-download-berttiti
https://coub.com/stories/2952756-csc-show-control-serial-number-verified
https://coub.com/stories/2952755-katyar-kaljat-ghusli-movie-downl-__full__
https://coub.com/stories/2952754-optimizador-de-corte-lineal-3-5-crack-best
https://coub.com/stories/2952753-techsmith-snagit-v12-2-1-1968-en-espanol-exclusive
https://coub.com/stories/2952751-updated-fsx-beech-b200-king-air-torrent
https://coub.com/stories/2952752-downloadaudiocatalyst21crack-laugpan
https://coub.com/stories/2952750-nfpa70epdftorrentbetter-download
https://coub.com/stories/2952747-marlax-mx100-flash-file-2nd-update-lcd-dead-recovery-firmware-link
https://coub.com/stories/2952749-cautivante-john-eldredge-pdf-descargar-12-__hot__
https://coub.com/stories/2952748-trendpoker-3d-texas-hold-em-poker-crack-serial-key-vitowend
https://coub.com/stories/2952745-exclusive-a-serbian-film-2010-480p-brrip
https://coub.com/stories/2952746-steve-biko-i-write-what-i-like-pdf-hot-free-download
https://coub.com/stories/2952743-lilypad3gamingedition-work-download
https://coub.com/stories/2952744-latex-software-free-download-for-windows-7-32-bit-25-greterr
https://coub.com/stories/2952742-__full__-the-brain-by-edgar-thorpe-pdf
https://coub.com/stories/2952741-tajima-dgml-by-pulse-14-crack-free-32-tyaeud
https://coub.com/stories/2952740-epsxe-1-9-0-for-pc-bios-plugins-complete-rar-full-link-version
https://coub.com/stories/2952738-updated-alctron-um900-driver-13
https://coub.com/stories/2952737-amcc-pci-matchmaker-s5935qf-driver
https://coub.com/stories/2952736-high-quality-ford-fiesta-mk6-sam-naprawiam
https://coub.com/stories/2952735-windows-xp-sp3-pt-br-drivers-office-iso-rar-hot
https://coub.com/stories/2952733-hot-ghost32-7z-download-best
https://coub.com/stories/2952734-pinnacle-pixie-activation-500-exe-12-new
https://coub.com/stories/2952732-__top__-quikseps-professional-v4-for-adobe-photoshop-internal-fosi-rar
https://coub.com/stories/2952730-practically-cheating-statistics-handbook-pdf-free-download-hot
https://coub.com/stories/2952731-premalekhanam-malayalam-novel-pdf-17-anaerra
https://coub.com/stories/2952728-yugioh-rulebook-version-1-0-pdf-download-ingeyes
baicat (Friday, 28 January 2022 07:54)
baicat d868ddde6e https://coub.com/stories/3088814-ab-bulk-mailer-with-keyl
https://coub.com/stories/3088818-ram-advanse-9-5-crack-best-rar
https://coub.com/stories/3088817-top-grammatik-aktiv-a1b1-cornelsen-pdf-184
https://coub.com/stories/3088812-office-2010-32-bit-product-key
https://coub.com/stories/3088810-extra-quality-lavasoft-file-shredder-7-7-0-2-serial-number-never-winap-ipodwiza
https://coub.com/stories/3088809-exclusive-crack-fifa-08-download-torent-kickass
https://coub.com/stories/3088807-hot-spotlight-on-oracle-keygen-21
https://coub.com/stories/3088806-norton-internet-security-19-9-1-14-serial-key-ottfab
https://coub.com/stories/3088804-ra-one-exclusive-full-movie-download-in-720p
https://coub.com/stories/3088802-__link__-vxworks-tornado-2-2-torrent-6
https://coub.com/stories/3088801-boso-2006-pinoy-dvdrip-xvid-softengsubs-tagalog-wingtip-darizal
https://coub.com/stories/3088800-teorija-knjizevnosti-ivo-tartalja-pdf-download-girgeno
https://coub.com/stories/3088798-daisy-s-destruction-video-completo-zip-yilyhedd
https://coub.com/stories/3088797-new-startek-fm220-driver-free-downloadtrmds
https://coub.com/stories/3088796-patched-bhaag-milkha-bhaag-movie-in-hindi-download-720p-hd
https://coub.com/stories/3088791-descargar-gratis-wellflo-extra-quality
https://coub.com/stories/3088789-iron-speed-designer-12-2-crack-link
https://coub.com/stories/3088787-topsurv-8-keygen-exclusive-rar
https://coub.com/stories/3088785-roxio-toast-titanium-17-4-multilingual-macos-free-download-hot
https://coub.com/stories/3088781-descargardiablo2pc1linksupercomprimidorar
https://coub.com/stories/3088780-ample-sound-agm-library-r2r-keygen-64-bitl-neljaen
https://coub.com/stories/3088778-pulp-fiction-english-subtitles-1080p-torrent-gavrram
https://coub.com/stories/3088777-chemsketch-12-full-top-32
https://coub.com/stories/3088763-keplerth-game
https://coub.com/stories/3088775-calculus-by-howard-anton-8th-edition-ebook-free-download-new-pdf-rar
https://coub.com/stories/3088773-upd-hauppauge-wintv-v8-crack-101
https://coub.com/stories/3088771-editplus-4-3-2543-keygen-full-crackingpatching-download
https://coub.com/stories/3088772-margalef-ecologia-libro-pdf-26-better
https://coub.com/stories/3088770-hot-adobe-photoshop-lightroom-cc-6-12-portable-cracked-cracksnow-full-version
https://coub.com/stories/3088765-repack-kaspersky-total-security-crack-2021-21-0-42-1482-license-key-free-download
nazajann (Friday, 28 January 2022 08:50)
nazajann d868ddde6e https://coub.com/stories/3097978-dvdfab-9-0-2-5-final-free-best-download
https://coub.com/stories/3097977-hot-boilsoft-video-joiner-7-02-2-portable
https://coub.com/stories/3097976-wurth-wow-5-03-generator-keygen-zip-link
https://coub.com/stories/3097975-top-steinberg-mymp3pro-v5-bit-byte-download
https://coub.com/stories/3097974-2021-teracopy-2-3-beta-2
https://coub.com/stories/3097973-crack-new-yo-presidente-objetivo-la-moncloa
https://coub.com/stories/3097972-vogone-vocal-remover-crack-free-__hot__
https://coub.com/stories/3097971-train-to-busan-in-hindi-720p-giowals
https://coub.com/stories/3097970-stahl-key-to-steel-free-download-22-_hot_
https://coub.com/stories/3097969-vikramadithyan-malayalam-movie-link-download-mp4-11
https://coub.com/stories/3097968-the-anarchist-cookbook-epubl-lerypev
https://coub.com/stories/3097967-verified-driver-joystick-k-one-mit-800a
https://coub.com/stories/3097966-gauss-view-5-linuxtorrent
https://coub.com/stories/3097965-antonio-da-silva-films-limanakia-mp4-epub-isaoto
https://coub.com/stories/3097964-heroes-stagione-1-tutti-i-torrent-dvdrip-ita-tnt-village-70-nadapelh
https://coub.com/stories/3097962-boy-agraxxx-millidal
https://coub.com/stories/3097963-return-to-mecca-free-download-full
https://coub.com/stories/3097961-portable-kaspersky-reset-trial-v5-1-0-35-final-softhound-crack
https://coub.com/stories/3097960-duniyadari-gujarati-man-1080p-download-better-movies
https://coub.com/stories/3097959-pdf2id-professional-v35-downloadgolkes-jayyary
https://coub.com/stories/3097958-best-crack-of-idm-6-23-build-18v
https://coub.com/stories/3097957-downloadfilmpyaarimpossiblelovefullmovie-creapacy
https://coub.com/stories/3097956-censor-3-verified-free-movie-download-in-hd
https://coub.com/stories/3097955-rpp-bahasa-lampung-berkarakter-sd-kelas-1-6-portable
https://coub.com/stories/3097954-extra-quality-nazrul-geeti-swaralipi-pdf-download101
https://coub.com/stories/3097953-cadsoft-eagle-professional-eagle-6-4-0-crack-sabhett
https://coub.com/stories/3097952-free-download-na-ghar-ke-na-ghaat-ke-2-in-hindi-in-mp4-tanecely
https://coub.com/stories/3097951-transformice-cheese-hack-no-survey-no-download-extra-quality
https://coub.com/stories/3097950-garmin-city-navigator-india-download-repack
https://coub.com/stories/3097949-empereur-l-empire-du-milieu-verified
amerxer (Friday, 28 January 2022 09:46)
amerxer d868ddde6e https://coub.com/stories/3058122-bibleworks-8-activation-keygen-repack-26
https://coub.com/stories/3058121-elango-tamil-font-typing-software-free-19-install
https://coub.com/stories/3058120-hd-online-player-rebel-2012-telugu-movie-dubbed-in-hindi-free-download-f-golkes-madreit
https://coub.com/stories/3058118-install-the-revenant-english-movie-download-dubbed-hindi
https://coub.com/stories/3058117-red-hat-enterprise-linux-5-7-x64-dvd-iso-torrent-extra-quality
https://coub.com/stories/3058116-spider-man-edge-of-time-pc-full-download-exclusive
https://coub.com/stories/3058112-sql-navigator-67-serial-key-vancher
https://coub.com/stories/3058111-housefull-2-2-full-movie-download-in-720p-ngarmel
https://coub.com/stories/3058110-motorola-wimax-cpei-23825-hack-22-vyrautu
https://coub.com/stories/3058107-class-7-math-book-bangla-version-pdf-download-2021
https://coub.com/stories/3058109-serious-sam-4-planet-badass-zip-free-download-emmneva
https://coub.com/stories/3058106-gta-iv-serial-key-and-unlock-code-genarator
https://coub.com/stories/3058108-multiviewer-2-0-easycap-software-32-hot
https://coub.com/stories/3058105-billa-2-full-movie-hd-1080p-bluray-tamil-54-exclusive
https://coub.com/stories/3058104-mireo-viagps-3-1-black-edition-update-2012-download-merder
https://coub.com/stories/3058102-realtek-rtl8187-wireless-lan-utility-windows-7-downloadl-lionulri
https://coub.com/stories/3058101-__link__-pk-de-sarkar-english-grammar-book-pdf-440
https://coub.com/stories/3058100-s-artificial-girl-3-trainer
https://coub.com/stories/3058099-native-instruments-west-africa-serial-number
https://coub.com/stories/3058098-native-instruments-b4-ii-2-0-4-vsti-dxi-rtas-rar-work
https://coub.com/stories/3058096-edraw-max-7-2-crack-free-download-tanmala
https://coub.com/stories/3058092-patched-dastek-unichip-software-free-36
https://coub.com/stories/3058093-xforce-keygen-32-bits-buzzsaw-2018-descargar-bevham
https://coub.com/stories/3058094-top-dt04-img-pes-2013-rar
https://coub.com/stories/3058087-ummy-video-download-link-er-1-10-7-0-crack-final-keygen-2020
https://coub.com/stories/3058086-avast-cleanup-premium-activation-code-19-1-7734-incl-full-version-crack-andped
https://coub.com/stories/3058085-best-skalp-for-sketchup-2016-crack
https://coub.com/stories/3058084-simulator-for-arduino-pro-crack-felare
https://coub.com/stories/3058083-mcafee-unlock-user-interface-password-crack-yamoliv
https://coub.com/stories/3058079-portable-imo-im-messenger-1-2-10-for-windows-desktop-download-balotay
divmar (Friday, 28 January 2022 10:41)
divmar d868ddde6e https://coub.com/stories/3097802-jazz-jackrabbit-2-1-23-full-fixed-version
https://coub.com/stories/3097801-hot-hi-tech-c-compiler-v9-83-crack
https://coub.com/stories/3097800-supergirl-season-1-complete-720p-webdl-ensub-x264mulvacoded-elmfry
https://coub.com/stories/3097799-vray-texture-pack-v2-c4d-torrent-hot-free
https://coub.com/stories/3097797-canl-mac-izle-trabzon-alanya-work
https://coub.com/stories/3097798-repack-autodata-3-40-2012-full-crack-download
https://coub.com/stories/3097796-tscm50-tscm52-pdf-fix
https://coub.com/stories/3097795-software-gv250-windows-7-download-zenofanc
https://coub.com/stories/3097794-macmillan-hot-spot-3-teachers-book
https://coub.com/stories/3097793-kmspico-v4-2-by-heldigard-64-bit-best
https://coub.com/stories/3097792-x-force-autocad-lt-2017-crack-new
https://coub.com/stories/3097791-acrorip-8-2-6l
https://coub.com/stories/3097790-shadowrun-crack-only-razor1911-india-birhali
https://coub.com/stories/3097789-xxx-indian-heroin-without-clothes-imagesl-otslayd
https://coub.com/stories/3097788-gta-vice-city-full-game-mediafire-epub-jaedciar
https://coub.com/stories/3097787-link-kunci-jawaban-auditing-dan-jasa-assurance-jilid-1-arens-full-rar
https://coub.com/stories/3097786-visual-parsic-4-49-top
https://coub.com/stories/3097785-link-getdata-recover-my-files-pro-v5-1-0-1824-including-crack-mediafire
https://coub.com/stories/3097784-better-age-of-empires-definitive-edition-codex-latest-versionl
https://coub.com/stories/3097783-banglacprogrammingbookbynitonpdf-free
https://coub.com/stories/3097782-need-for-speed-underground-2-please-insert-disc-2-crack-patched
https://coub.com/stories/3097781-xbox-360-emulator-bios-v3-2-4-rar-51-73-kb-salakac
https://coub.com/stories/3097780-intelr-awrdacpi-drivers-for-windows-7-32bit-download-cracked
https://coub.com/stories/3097779-new-nativeinstrumentsmaschine20fullversiontorrent
https://coub.com/stories/3097778-lie-with-me-dubbed-in-hindi-full-movie-download-in-mp4-link
https://coub.com/stories/3097777-flexsim-simulation-software-crack-keygens-exclusive
https://coub.com/stories/3097775-crack-acoustica-mixcraft-6-rar-better
https://coub.com/stories/3097773-just-friends-by-sumrit-shahi-pdf-ebook-free-download-makcare
https://coub.com/stories/3097776-link-class-12-ip-book-free-download-pdf
https://coub.com/stories/3097774-updated-la-celestina-adaptacion-eduardo-alonso-pdf
preswil (Friday, 28 January 2022 11:38)
preswil d868ddde6e https://coub.com/stories/3136730-infotech-english-for-computer-users-teacher-s-book-pdf-download-uriafreb
https://coub.com/stories/3136726-top-moondance-1995-download-hd-quality
https://coub.com/stories/3136729-extra-quality-download-terjemahan-kitab-irsyadul-ibad-pdf-to-excel
https://coub.com/stories/3136727-the-ultimate-country-fake-book-pdf-updated-download
https://coub.com/stories/3136724-full-top-activator-cmd-windows-10-1809-and-office-2019-new-updete
https://coub.com/stories/3136723-link-dark-orbit-dark-hack-generator-rar-download
https://coub.com/stories/3136722-kumpulan-soal-bhs-madura-dan-jawaban
https://coub.com/stories/3136720-pl7prov45sp5fixed-crack
https://coub.com/stories/3136718-farming-simulator-2011-multiplayer-lan-crack-pedxyl
https://coub.com/stories/3136719-stardock-start8-1-40-1-final-pre-activated-painter-best-full-version
https://coub.com/stories/3136717-alien-shooter-2-conscription-rip-unleashed-vip-hack
https://coub.com/stories/3136715-download-best-film-faith-like-potatoes-subtitle-indonesia-running
https://coub.com/stories/3136714-extra-quality-dirotta-su-cuba-discografia
https://coub.com/stories/3136713-xforce-keygen-autocad-2016-64-bit-windows-1016-top
https://coub.com/stories/3136712-extra-quality-bosch-esitronic-archive-cds-c-k-w-megaupload-serial
https://coub.com/stories/3136708-velai-illa-pattathari-full-movie-download-tamilrockers-hd-desrei
https://coub.com/stories/3136711-shema-elektro-instalacije-za-imt-539-top
https://coub.com/stories/3136710-new-release-zoran-pa500-set-telecharger-rythme-rai-chawi-chaabi-kabyle
https://coub.com/stories/3136707-link-silhouette-studio-designer-edition-serial
https://coub.com/stories/3136706-alien-shooter-3-full-version-free-download-peadpaga
https://coub.com/stories/3136705-omsi2addonberlinx10downloadbittorrentpc-2-halreb
https://coub.com/stories/3136704-repack-sama-tamil-full-movie-download
https://coub.com/stories/3136702-better-camp-buddy-full-game-download
https://coub.com/stories/3136701-free-key-for-winthruster
https://coub.com/stories/3136700-fixed-crack-assassin-creed-revelations-skidrow-1-03
https://coub.com/stories/3136698-portable-nfpa-13-handbook-pdf-57
https://coub.com/stories/3136697-latest-dj-software-free-download-full-version-for-pc-2012-new
https://coub.com/stories/3136695-link-ceja-pinknightyon4-pv-fantasia-models-wmv
https://coub.com/stories/3136694-prodad-mercalli-v5-sal-6-2-459-4-multilingual-cracked-work-full-version
https://coub.com/stories/3136693-cx-programmer-9-1-free-download-full-grehay
preswil (Friday, 28 January 2022 11:38)
preswil d868ddde6e https://coub.com/stories/3136730-infotech-english-for-computer-users-teacher-s-book-pdf-download-uriafreb
https://coub.com/stories/3136726-top-moondance-1995-download-hd-quality
https://coub.com/stories/3136729-extra-quality-download-terjemahan-kitab-irsyadul-ibad-pdf-to-excel
https://coub.com/stories/3136727-the-ultimate-country-fake-book-pdf-updated-download
https://coub.com/stories/3136724-full-top-activator-cmd-windows-10-1809-and-office-2019-new-updete
https://coub.com/stories/3136723-link-dark-orbit-dark-hack-generator-rar-download
https://coub.com/stories/3136722-kumpulan-soal-bhs-madura-dan-jawaban
https://coub.com/stories/3136720-pl7prov45sp5fixed-crack
https://coub.com/stories/3136718-farming-simulator-2011-multiplayer-lan-crack-pedxyl
https://coub.com/stories/3136719-stardock-start8-1-40-1-final-pre-activated-painter-best-full-version
https://coub.com/stories/3136717-alien-shooter-2-conscription-rip-unleashed-vip-hack
https://coub.com/stories/3136715-download-best-film-faith-like-potatoes-subtitle-indonesia-running
https://coub.com/stories/3136714-extra-quality-dirotta-su-cuba-discografia
https://coub.com/stories/3136713-xforce-keygen-autocad-2016-64-bit-windows-1016-top
https://coub.com/stories/3136712-extra-quality-bosch-esitronic-archive-cds-c-k-w-megaupload-serial
https://coub.com/stories/3136708-velai-illa-pattathari-full-movie-download-tamilrockers-hd-desrei
https://coub.com/stories/3136711-shema-elektro-instalacije-za-imt-539-top
https://coub.com/stories/3136710-new-release-zoran-pa500-set-telecharger-rythme-rai-chawi-chaabi-kabyle
https://coub.com/stories/3136707-link-silhouette-studio-designer-edition-serial
https://coub.com/stories/3136706-alien-shooter-3-full-version-free-download-peadpaga
https://coub.com/stories/3136705-omsi2addonberlinx10downloadbittorrentpc-2-halreb
https://coub.com/stories/3136704-repack-sama-tamil-full-movie-download
https://coub.com/stories/3136702-better-camp-buddy-full-game-download
https://coub.com/stories/3136701-free-key-for-winthruster
https://coub.com/stories/3136700-fixed-crack-assassin-creed-revelations-skidrow-1-03
https://coub.com/stories/3136698-portable-nfpa-13-handbook-pdf-57
https://coub.com/stories/3136697-latest-dj-software-free-download-full-version-for-pc-2012-new
https://coub.com/stories/3136695-link-ceja-pinknightyon4-pv-fantasia-models-wmv
https://coub.com/stories/3136694-prodad-mercalli-v5-sal-6-2-459-4-multilingual-cracked-work-full-version
https://coub.com/stories/3136693-cx-programmer-9-1-free-download-full-grehay
preswil (Friday, 28 January 2022 11:39)
preswil d868ddde6e https://coub.com/stories/3136730-infotech-english-for-computer-users-teacher-s-book-pdf-download-uriafreb
https://coub.com/stories/3136726-top-moondance-1995-download-hd-quality
https://coub.com/stories/3136729-extra-quality-download-terjemahan-kitab-irsyadul-ibad-pdf-to-excel
https://coub.com/stories/3136727-the-ultimate-country-fake-book-pdf-updated-download
https://coub.com/stories/3136724-full-top-activator-cmd-windows-10-1809-and-office-2019-new-updete
https://coub.com/stories/3136723-link-dark-orbit-dark-hack-generator-rar-download
https://coub.com/stories/3136722-kumpulan-soal-bhs-madura-dan-jawaban
https://coub.com/stories/3136720-pl7prov45sp5fixed-crack
https://coub.com/stories/3136718-farming-simulator-2011-multiplayer-lan-crack-pedxyl
https://coub.com/stories/3136719-stardock-start8-1-40-1-final-pre-activated-painter-best-full-version
https://coub.com/stories/3136717-alien-shooter-2-conscription-rip-unleashed-vip-hack
https://coub.com/stories/3136715-download-best-film-faith-like-potatoes-subtitle-indonesia-running
https://coub.com/stories/3136714-extra-quality-dirotta-su-cuba-discografia
https://coub.com/stories/3136713-xforce-keygen-autocad-2016-64-bit-windows-1016-top
https://coub.com/stories/3136712-extra-quality-bosch-esitronic-archive-cds-c-k-w-megaupload-serial
https://coub.com/stories/3136708-velai-illa-pattathari-full-movie-download-tamilrockers-hd-desrei
https://coub.com/stories/3136711-shema-elektro-instalacije-za-imt-539-top
https://coub.com/stories/3136710-new-release-zoran-pa500-set-telecharger-rythme-rai-chawi-chaabi-kabyle
https://coub.com/stories/3136707-link-silhouette-studio-designer-edition-serial
https://coub.com/stories/3136706-alien-shooter-3-full-version-free-download-peadpaga
https://coub.com/stories/3136705-omsi2addonberlinx10downloadbittorrentpc-2-halreb
https://coub.com/stories/3136704-repack-sama-tamil-full-movie-download
https://coub.com/stories/3136702-better-camp-buddy-full-game-download
https://coub.com/stories/3136701-free-key-for-winthruster
https://coub.com/stories/3136700-fixed-crack-assassin-creed-revelations-skidrow-1-03
https://coub.com/stories/3136698-portable-nfpa-13-handbook-pdf-57
https://coub.com/stories/3136697-latest-dj-software-free-download-full-version-for-pc-2012-new
https://coub.com/stories/3136695-link-ceja-pinknightyon4-pv-fantasia-models-wmv
https://coub.com/stories/3136694-prodad-mercalli-v5-sal-6-2-459-4-multilingual-cracked-work-full-version
https://coub.com/stories/3136693-cx-programmer-9-1-free-download-full-grehay
preswil (Friday, 28 January 2022 11:39)
preswil d868ddde6e https://coub.com/stories/3136730-infotech-english-for-computer-users-teacher-s-book-pdf-download-uriafreb
https://coub.com/stories/3136726-top-moondance-1995-download-hd-quality
https://coub.com/stories/3136729-extra-quality-download-terjemahan-kitab-irsyadul-ibad-pdf-to-excel
https://coub.com/stories/3136727-the-ultimate-country-fake-book-pdf-updated-download
https://coub.com/stories/3136724-full-top-activator-cmd-windows-10-1809-and-office-2019-new-updete
https://coub.com/stories/3136723-link-dark-orbit-dark-hack-generator-rar-download
https://coub.com/stories/3136722-kumpulan-soal-bhs-madura-dan-jawaban
https://coub.com/stories/3136720-pl7prov45sp5fixed-crack
https://coub.com/stories/3136718-farming-simulator-2011-multiplayer-lan-crack-pedxyl
https://coub.com/stories/3136719-stardock-start8-1-40-1-final-pre-activated-painter-best-full-version
https://coub.com/stories/3136717-alien-shooter-2-conscription-rip-unleashed-vip-hack
https://coub.com/stories/3136715-download-best-film-faith-like-potatoes-subtitle-indonesia-running
https://coub.com/stories/3136714-extra-quality-dirotta-su-cuba-discografia
https://coub.com/stories/3136713-xforce-keygen-autocad-2016-64-bit-windows-1016-top
https://coub.com/stories/3136712-extra-quality-bosch-esitronic-archive-cds-c-k-w-megaupload-serial
https://coub.com/stories/3136708-velai-illa-pattathari-full-movie-download-tamilrockers-hd-desrei
https://coub.com/stories/3136711-shema-elektro-instalacije-za-imt-539-top
https://coub.com/stories/3136710-new-release-zoran-pa500-set-telecharger-rythme-rai-chawi-chaabi-kabyle
https://coub.com/stories/3136707-link-silhouette-studio-designer-edition-serial
https://coub.com/stories/3136706-alien-shooter-3-full-version-free-download-peadpaga
https://coub.com/stories/3136705-omsi2addonberlinx10downloadbittorrentpc-2-halreb
https://coub.com/stories/3136704-repack-sama-tamil-full-movie-download
https://coub.com/stories/3136702-better-camp-buddy-full-game-download
https://coub.com/stories/3136701-free-key-for-winthruster
https://coub.com/stories/3136700-fixed-crack-assassin-creed-revelations-skidrow-1-03
https://coub.com/stories/3136698-portable-nfpa-13-handbook-pdf-57
https://coub.com/stories/3136697-latest-dj-software-free-download-full-version-for-pc-2012-new
https://coub.com/stories/3136695-link-ceja-pinknightyon4-pv-fantasia-models-wmv
https://coub.com/stories/3136694-prodad-mercalli-v5-sal-6-2-459-4-multilingual-cracked-work-full-version
https://coub.com/stories/3136693-cx-programmer-9-1-free-download-full-grehay
jaciden (Friday, 28 January 2022 12:31)
jaciden d868ddde6e https://coub.com/stories/3061200-laubwerk-plants-kit-4-win-mac-weyzab
https://coub.com/stories/3061199-link-handycafe-3-4-14-cracked-sn-per-x
https://coub.com/stories/3061196-top-diskinternals-ntfs-recovery-full-crack
https://coub.com/stories/3061195-upd-secret-files-3-gog-classic-i-know
https://coub.com/stories/3061197-transformers-2007-brrip-720p-subtitles-34
https://coub.com/stories/3061194-splayer-4-9-1-crack-2021-free-download
https://coub.com/stories/3061192-siemensnx1201win64ssqsetupfree-exclusive
https://coub.com/stories/3061190-samsung-2g-tool-v3-5-0033-setup-www-mobile-rdx-com-__link__
https://coub.com/stories/3061189-gy-521-datasheet-pdf-work
https://coub.com/stories/3061185-windows-7-sp1-x86-x64-aio-11in1-iso-ita-vinnrei
https://coub.com/stories/3061186-top-nitro-pdf-pro-v6-2-3-6-keygen-guide-32bit-64bit-serial-key-keygen
https://coub.com/stories/3061183-repack-adobe-photoshop-cc-2019-v20-0-0-multilingual-crack-techtools-downloadl
https://coub.com/stories/3061181-bios-dll-3ds-dilireg
https://coub.com/stories/3061178-work-dido-greatest-hits-2013-320kbps-cbr-mp3-tugazx-dido-greatest-hits-2013-320kbps-cb
https://coub.com/stories/3061179-aspen-plus-11-1-crack-rar-top
https://coub.com/stories/3061180-verified-wtm-copy-protection-2-6-crack
https://coub.com/stories/3061176-shaderlight-for-sketchup-download-portable-crack
https://coub.com/stories/3061173-let-me-make-you-a-martyr-scaricare-film
https://coub.com/stories/3061175-gotham-season-2-720p-hdtv-x265-hevc-shaanig-new
https://coub.com/stories/3061174-dhan-dhana-dhan-goal-exclusive-full-movie-in-hindi-torrent-720p
https://coub.com/stories/3061171-avira-antivirus-serial-key-karedar
https://coub.com/stories/3061169-devart-dbforge-sql-complete-crack-16-webfit
https://coub.com/stories/3061167-mydac-for-rad-studio-xe3-crack-exclusive
https://coub.com/stories/3061166-heat-treatment-by-rajan-and-sharma-pdf-free-161-exclusive
https://coub.com/stories/3061162-shirley-ooi-emergency-medicine-pdf-free-download-exclusive
https://coub.com/stories/3061163-descargar-tekken-6-para-ps2-iso-torrent
https://coub.com/stories/3061161-monster-university-1080p-download-14-sabger
https://coub.com/stories/3061160-exclusive-gangs-of-wasseypur-2-2-720p-download-movie
https://coub.com/stories/3061157-portable-jv16-powertools-5-0-0-484-multilingual
https://coub.com/stories/3061159-full-libro-de-estadistica-y-probabilidad-1-santillana-pdf
qwynwave (Friday, 28 January 2022 13:26)
qwynwave d868ddde6e https://coub.com/stories/3117446-exclusive-clarion-8-ee-crack
https://coub.com/stories/3117445-bewerbungsmaster-2013-crack-download-link
https://coub.com/stories/3117443-extra-quality-buku-statistika-untuk-penelitian-sugiyono-pdf
https://coub.com/stories/3117444-sony-sound-forge-7-free-repack-download-with-crackl
https://coub.com/stories/3117442-hot-monografi-ekstrak-tumbuhan-obat-indonesia-pdf-download
https://coub.com/stories/3117441-verified-aventura-en-tierradentro-pdf-free
https://coub.com/stories/3117440-flame-assist-2006-x64-64bit-product-key-download-high-quality
https://coub.com/stories/3117439-free-let-s-explore-the-farm-junior-field-trips-torrent-full
https://coub.com/stories/3117438-rocket-league-rocket-pass-3-update-v1-63-plaza-top
https://coub.com/stories/3117437-hot-adobe-white-rabbit-photoshop-cs5
https://coub.com/stories/3117435-virtual-assistant-denise-1-0-free-software-download-best
https://coub.com/stories/3117434-cuteftp-pro-v8-utorrent-cracked
https://coub.com/stories/3117436-free-dope-vst-beat-machine-download-freel
https://coub.com/stories/3117433-wave-function-spartan-keygen-download-upd
https://coub.com/stories/3117432-ta-ra-rum-pum-full-movie-download-_best_-300-mb
https://coub.com/stories/3117431-counter-strike-xtreme-v7-map-download-haljam
https://coub.com/stories/3117430-fs9-fsx-aerosoft-mega-airport-paris-orly-v1-01-game-fixed
https://coub.com/stories/3117429-3d-album-commercial-suite-332-keygen-mornsas
https://coub.com/stories/3117428-business-mathematics-by-vk-kapoor-pdf-free-1080-maudart
https://coub.com/stories/3117427-minipe-usb-bootable-download-14-phigia
https://coub.com/stories/3117426-geovision-gv-650-800-s-v3-52-drivers-zip-40
https://coub.com/stories/3117425-adobe-photoshop-cs2-crack-torrent-portable
https://coub.com/stories/3117424-molly-groove-2000-pics-warwdar
https://coub.com/stories/3117423-software-solid-works-2008-sp4-0-64bit-crack-12-patched
https://coub.com/stories/3117420-new-richardson-editrocket-4-5-3-keygen-full
https://coub.com/stories/3117422-7-data-recovery-v4-4-keygen-with-registration-code-latest-peacigna
https://coub.com/stories/3117421-mastercam-x8-full-crack-19https-scoutmails-com-index301-php-k-mastercam-x8-full-crack-19-top
https://coub.com/stories/3117419-verified-age-of-empires-iii-complete-collection-eng-rus-repack-r-g-download
https://coub.com/stories/3117418-the-curious-expedition-v1-3-8-8-simplex-cheat-engine
https://coub.com/stories/3117417-hd-online-player-dammu-telugu-movie-download-dvdrip-2-salerayn
feakaf (Friday, 28 January 2022 14:19)
feakaf d868ddde6e https://coub.com/stories/2953798-making-history-book-christopher-culpin-pdf-link-download
https://coub.com/stories/2953797-kidnap-full-movie-download-in-720p-1080p-kirver
https://coub.com/stories/2953796-fix-urc-complete-control-program-ccp-rar
https://coub.com/stories/2953795-download-buku-cheat-ps2-lengkap-antochry
https://coub.com/stories/2953794-vocabolario-latino-castiglioni-mariotti-by-gigacrew-64-bit-pander
https://coub.com/stories/2953793-_best_-clip-studio-paint-ex-crack-1-9-5-full-keygen-latest-2019
https://coub.com/stories/2953791-exclusive-descargar-solucionario-de-wangsness
https://coub.com/stories/2953792-full-verified-microsoft-office-2010-professional-plus-pt-pt
https://coub.com/stories/2953789-kingsoft-internet-security-9-plus-serial-number-download-11-gidgnad
https://coub.com/stories/2953790-globaltis-key-generator
https://coub.com/stories/2953786-xmind-8-pro-v3-7-6-with-crack-free
https://coub.com/stories/2953788-windows-8-super-lite-torrent-download-repack
https://coub.com/stories/2953787-__hot__-navicat-premium-free-download-full-version
https://coub.com/stories/2953785-jannat-hd-1080p-bluray-download-movie-cellau
https://coub.com/stories/2953783-cubase-7-64bit-activation-code-2
https://coub.com/stories/2953784-free-setup-2a-bin-call-of-duty-black-ops
https://coub.com/stories/2953782-agisoft-photoscan-professional-1-3-0-crack-ambelle
https://coub.com/stories/2953781-fixed-cara-download-ebook-di-goodreads-app
https://coub.com/stories/2953780-therapeutic-choices-7th-edition-torrent
https://coub.com/stories/2953779-fast-and-furious-8-english-1080p-tamil-dubbed-movie
https://coub.com/stories/2953778-_best_-contoh-kwitansi-kosong-113
https://coub.com/stories/2953777-download-better-film-akb48-majisuka-gakuen-sub-indo
https://coub.com/stories/2953776-titan-quest-immortal-throne-crack-no-cd-130-__full__
https://coub.com/stories/2953775-3d-native-cad-converter-crack-extra-quality
https://coub.com/stories/2953774-new-magix-samplitude-music-studio-16-crack
https://coub.com/stories/2953773-internet-download-manager-6-35-build-10-crack-better
https://coub.com/stories/2953772-vietcong-2-game-free-download-endwony
https://coub.com/stories/2953771-compaq-visual-fortran-windows-7-64-bit-verified-free-download
https://coub.com/stories/2953770-enter-serial-key-battlefield-bad-company-2
https://coub.com/stories/2953769-everest-ultimate-edition-4-20-with-serial-jermac
bambkapi (Friday, 28 January 2022 15:14)
bambkapi d868ddde6e https://coub.com/stories/3018140-crack-magic-utilities-5-20-for-windowsl-top
https://coub.com/stories/3018139-bbmultiunlockerkeyv150descargar-hot
https://coub.com/stories/3018138-crack-emulator-lectra-modaris-v7-64-valgiu
https://coub.com/stories/3018137-download-film-the-raid-2-berandal-bluray-26-ferwhal
https://coub.com/stories/3018136-extra-quality-download-map-indonesia-lajur-kiri-haulin
https://coub.com/stories/3018135-audio-record-wizard-720-serial-key-plus-16
https://coub.com/stories/3018133-ezee-front-desk-hotel-software-crack-download-exclusive
https://coub.com/stories/3018132-tropico-5-the-supercomputer-password-xandelis
https://coub.com/stories/3018127-crack-artcam-2015-free-download-best
https://coub.com/stories/3018126-free-answers-to-escience-lab-11-mitosis-rar
https://coub.com/stories/3018125-battlefield-4-cd-key-generator-54
https://coub.com/stories/3018123-va-erotic-lounge-vol-1-9-2003-2010-mp3
https://coub.com/stories/3018122-filmul-eragon-2-online-subtitrat-gratis-updated
https://coub.com/stories/3018121-crack-change-folder-icons-8-7-xyrona
https://coub.com/stories/3018119-__hot__-the-princess-mononoke-1080p-torrent
https://coub.com/stories/3018118-flow-3d-v10-crack-12-ansmacc
https://coub.com/stories/3018114-2011baixarfilmealendadopianistadomardublado
https://coub.com/stories/3018117-link-silenthunter4cracknocd14
https://coub.com/stories/3018116-conwep-software-clausof
https://coub.com/stories/3018113-pensonic-midi-karaoke-song-download-verified-2
https://coub.com/stories/3018111-install-firmware-tablet-titan-7009
https://coub.com/stories/3018110-torrent-igo-primo-24-for-windowsce-fixed
https://coub.com/stories/3018109-kinderspellen-dvd-1-pc-nl-nlt-release-hack-torrent
https://coub.com/stories/3018108-poultry-farming-in-tamil-nadu-pdf-download-janijawd
https://coub.com/stories/3018106-enttec-d-pro-8u-with-licence-dongle-crack-marevel
https://coub.com/stories/3018105-verified-online-pmd-to-pdf-converter-free-download
https://coub.com/stories/3018102-200-clasicas-de-la-musica-tropical-y-bailable-mega
https://coub.com/stories/3018103-windows-7-ultimate-activation-key-2014
https://coub.com/stories/3018100-top-hard-truck-18-wheels-of-steel-crack-no-cd-player-in-computer
https://coub.com/stories/3018099-verified-windows-7-ultimate-32bit-removewatt-iso-poweriso-v4-7-serial-free-download
emmavos (Friday, 28 January 2022 16:05)
emmavos d868ddde6e https://coub.com/stories/3150342-madmapper-1-4-2-crack-for-mac-torrent-19-slavwal
https://coub.com/stories/3150341-manual-book-kijang-krista-pdf-wendwel
https://coub.com/stories/3150339-ansys-products-v1507-3264-bitmagni-patched
https://coub.com/stories/3150340-macro-recorder-5-0-3-6-with-crack-for-pc-leakala
https://coub.com/stories/3150337-new-convertxtodvd-v5-3-0-9-installer-nelly-serial-key
https://coub.com/stories/3150338-caietespecialeclasapregatitoarepdfdownload-verified
https://coub.com/stories/3150336-windows-vista-extreme-edition-iso-pdr-64-bit
https://coub.com/stories/3150334-z3x-smart-card-rockey-200-driver-free-download-gilfid
https://coub.com/stories/3150335-new-super-simple-songs-6album-collection-torrent
https://coub.com/stories/3150333-avira-antivirus-pro-2015-v15-0-8-624-key
https://coub.com/stories/3150331-kolambasanniyasinhalamoviefree-work-download
https://coub.com/stories/3150332-machfive-3-cracked-tavall
https://coub.com/stories/3150330-matlab-2013-free-torrent-download-wi-repack
https://coub.com/stories/3150329-the-black-prince-hd-1080p-bluray-download-torrent-papbib
https://coub.com/stories/3150328-patched-bibleworks-10-better
https://coub.com/stories/3150327-walaoke-pro-3-6-full-crack-__hot__-11
https://coub.com/stories/3150324-cadware-9-5-for-autocad-2005-crack-link
https://coub.com/stories/3150326-link-sybase-pc-client-15-7-download102-12
https://coub.com/stories/3150325-programming-in-c-by-ashok-kamthane-pdf
https://coub.com/stories/3150323-work-dreamweaver-cs6-portable-fr
https://coub.com/stories/3150321-mahjong-pretty-girls-battle-school-girls-edition-torrent-2021-download-portable-edition
https://coub.com/stories/3150316-__exclusive__-star-wars-jedi-fallen-order-codex-fitgirl
https://coub.com/stories/3150318-skytest-crack-epub-zoffxyre
https://coub.com/stories/3150315-call-of-duty-black-ops-iii-mp-zombie-addon-kaos-fitgirl-repack
https://coub.com/stories/3150314-patched-descargar-srt23dass
https://coub.com/stories/3150313-hex-workshop-6-7-full-crackgolkes-quyxavi
https://coub.com/stories/3150312-artcampro2010sp4downloadfullversion-install
https://coub.com/stories/3150311-collezione-di-basi-musicali-in-mp3-per-k
https://coub.com/stories/3150310-deep-freeze-software-for-windows-7-crack-download-link
https://coub.com/stories/3150307-xforce-keygen-32bits-or-64bits-version-vred-presenter-2016-keygen-jankah
yelvin (Sunday, 30 January 2022 12:37)
yelvin b7f02f1a74 https://sivilthighcrinphym.wixsite.com/framerolxa/post/materialise-magics-18-0-3-16-x-windows-cracked-full-version-activation-utorrent-64-zip
https://mormispsorgverrach.wixsite.com/nessnozztollde/post/hd-online-player-raghu-romeo-marathi-movie-free-downl
https://arlenajustason108e.wixsite.com/phowhilasma/post/tsunamis-99-dongle-crack-torrent-9
https://withers1838bd7.wixsite.com/percahighru/post/book-grammatik-aktiv-a1-b1-cornelsen-download-rar-epub-full
https://abexpredesti.wixsite.com/teraltoyhe/post/folder-colorizer
https://layjuasilocattback.wixsite.com/giawindebest/post/manual-do-operador-valtra-bm-125i
https://slavunrewello.wixsite.com/maxaserci/post/serial-citroen-service-box-e-download-latest-64bit-full-version-windows
https://birgitperez88.wixsite.com/thariderla/post/vault-basic-2006-x64-xforce-keygen-download
https://nuctifisourdeotinc.wixsite.com/netcioterga/post/full-version-url-helper-3-44-pc-utorrent-ultimate
https://wingipipodecal.wixsite.com/ufobmenty/post/research-methods-for-business-students-7th-edition-pdf-free-download
https://layfisemblygaparga.wixsite.com/jazignaman/post/calcgen-by-isa-2010-free-downloads-1
https://kecaltiomenjobthmo.wixsite.com/arimlure/post/highti-ultimate-windows-32-download
https://geivirenegpoly.wixsite.com/pleginremi/post/utorrent-p-tch-summit-1-teachers-12-rar-book-pdf-free
https://charisseruell804d9.wixsite.com/lbitabentio/post/free-metin2-switchbot-v3-by-padmak-ultimate-zip-download
https://pysballbackpersuri.wixsite.com/analines/post/utorrent-bel-sekolah-o-pc-license-patch
https://funzarislav.wixsite.com/cornfecalsai/post/build-java-1-4-2-15-patch-activator-windows-zip-download
https://pingnersternlaptir.wixsite.com/pardistfaso/post/kutty-tamil-movie-free-torrent-download-2009
https://ferrerebrona.wixsite.com/goestaralow/post/screencast-2018-scaricare-64-full-rar-key-torrent-serial
https://proberbronorkeysta.wixsite.com/vorssobrore/post/srs-remote-unlock-code-client-v1-0-15-15
https://cacobertthero.wixsite.com/heartpostomo/post/como-activar-windows-server-2012-release-candidate-datacenter-build-8400-41-97
https://rierihoja.wixsite.com/propryscaytar/post/malwarebytes-anti-malware-premium-2-1-4-1018-keys-piplarsson-swe-serial-key-keygen
https://whittbotisilocar.wixsite.com/renseipetge/post/full-sejarah-dunia-ku-download-ebook-zip-pdf
https://haggar633.wixsite.com/fotirihead/post/bus-simulator-2008-crack-deutsch
https://tekvesamsdream1979.wixsite.com/nessbalata/post/te-rshare-4u-for-2-0-1-1-torrent-activator-x32-full-zip-professional-android
https://nadiami62stultz.wixsite.com/starconsjouma/post/soundforge-10-keygen-64-bit
https://pheotradenilbini.wixsite.com/taitaiblocmay/post/webstorm-2019-1-crack-with-activation-code
https://rowitow.wixsite.com/woprholete/post/sql-server-database-32-pc-free-key
https://descnesspawonle.wixsite.com/collkarrieti/post/insanity-plyometric-cardio-circuit-full-video
https://biacalbesaseg.wixsite.com/kripamgasec/post/kodi-addon-repository-download-zip
https://etondinraser.wixsite.com/stylagmare/post/hd-online-player-v-per-vendetta-full-movie-online-fre
lanolan (Sunday, 30 January 2022 15:16)
lanolan b7f02f1a74 https://amnalacallperti.wixsite.com/scupophealsa/post/supermariosunshinewbfs
https://lisettdenqueduva.wixsite.com/taavateli/post/autocad-2013-english-win-64bit-exe
https://ashleighbendle1280.wixsite.com/mortcycsoftdop/post/simfatic-forms-4-0-torrent-download
https://marcelmorrisett.wixsite.com/seorecnoecir/post/download-buku-ulumul-hadits-pdf-writer
https://abunrigpetug.wixsite.com/erzanapi/post/social-build-windows-registration-full-version-rar-64bit
https://olegkostin350.wixsite.com/moiliotersu/post/activation-gear-template-genera-windows-torrent-rar-pro
https://netupekana.wixsite.com/tarwilldicsi/post/32bit-archicad-14-zip-activation-full-final-patch
https://barcdifgeder.wixsite.com/beismarhostgang/post/administracion-10-edicion-robbins-coulter-pdf-download
https://ifmabeatimerbamedu.wixsite.com/footmenenfue/post/plaga-perros-libro-full-pdf-zip-book-utorrent
https://liamachaphynutria.wixsite.com/soaliredi/post/key-lotus-simula-rar-full-version-download
https://nilmisargertfusy.wixsite.com/propapintruc/post/where-to-play-sex-games
https://flexinsleevul1975.wixsite.com/frozmeosmokag/post/microsoft-office-professional-plus-2018-pt-br-ativador-keygen
https://rinmapepthocenot.wixsite.com/watchgarpeba/post/descargar-voda-shit-exe-18
https://ineximpharti.wixsite.com/planfundchitou/post/64-loa-r-2-0-9-utorrent-full-pc-rar
https://tipeddsica1975.wixsite.com/franbitasy/post/windows-10-pro-x64-rs5-incl-office-2019-en-us-nov-2018-gen2-serial-key
https://vandenboo.wixsite.com/vetonserog/post/ssspsx-pad-plugin-pressure-mod-160-download
https://widsentzamhenslapa.wixsite.com/eruphiner/post/rar-vanchipattu-lyrics-222-utorrent-book-free-mobi
https://incotanmerugle.wixsite.com/lanithearwho/post/sap-business-one-8-8-license-crack
https://rail914ny.wixsite.com/samacita/post/ed-bibleworks-10-activation-torrent-crack-exe-full-version
https://flexentusystchobu.wixsite.com/prommodowla/post/netscan-full-version-activation-nulled-torrent-iso-x32
https://inwanesperale.wixsite.com/lisounamra/post/ccboot-game-menu-crack-21
https://hunderda.wixsite.com/sititinog/post/keygen-for-smscaster-e-marketer-gsm-standard-v3-7-montagegratuit-parti
https://nodonarviportre.wixsite.com/risbicori/post/winstep-xtreme-18-12-1373-multilingual-medicinebabu-free-cracked-utorrent-zip
https://knapicralansbi.wixsite.com/sembthatmechen/post/pc-cubaseelementsv706x86x-iso-64bit-activation-free-file
https://comptheverdaconve.wixsite.com/dieherasep/post/film-oui-french-kickass-full-dubbed-full
https://acilmigdersberpare.wixsite.com/throshalanne/post/gsdeditorv51-10-zip
https://distlycirater.wixsite.com/statigconri/post/alfaobd-crack
https://bomlitibidijo.wixsite.com/siobatfipunk/post/uvi-darklight-iix-torrent
https://evelynfineberg115q.wixsite.com/centdisttiperp/post/pedro-el-pollo-la-pelicula-dvdrip-espa-ol-latino-2-19
https://scottiewhitehorn59.wixsite.com/alereren/post/full-compufour-aplicativos-comerciais-2011-rio2016
lanolan (Sunday, 30 January 2022 15:17)
lanolan b7f02f1a74 https://amnalacallperti.wixsite.com/scupophealsa/post/supermariosunshinewbfs
https://lisettdenqueduva.wixsite.com/taavateli/post/autocad-2013-english-win-64bit-exe
https://ashleighbendle1280.wixsite.com/mortcycsoftdop/post/simfatic-forms-4-0-torrent-download
https://marcelmorrisett.wixsite.com/seorecnoecir/post/download-buku-ulumul-hadits-pdf-writer
https://abunrigpetug.wixsite.com/erzanapi/post/social-build-windows-registration-full-version-rar-64bit
https://olegkostin350.wixsite.com/moiliotersu/post/activation-gear-template-genera-windows-torrent-rar-pro
https://netupekana.wixsite.com/tarwilldicsi/post/32bit-archicad-14-zip-activation-full-final-patch
https://barcdifgeder.wixsite.com/beismarhostgang/post/administracion-10-edicion-robbins-coulter-pdf-download
https://ifmabeatimerbamedu.wixsite.com/footmenenfue/post/plaga-perros-libro-full-pdf-zip-book-utorrent
https://liamachaphynutria.wixsite.com/soaliredi/post/key-lotus-simula-rar-full-version-download
https://nilmisargertfusy.wixsite.com/propapintruc/post/where-to-play-sex-games
https://flexinsleevul1975.wixsite.com/frozmeosmokag/post/microsoft-office-professional-plus-2018-pt-br-ativador-keygen
https://rinmapepthocenot.wixsite.com/watchgarpeba/post/descargar-voda-shit-exe-18
https://ineximpharti.wixsite.com/planfundchitou/post/64-loa-r-2-0-9-utorrent-full-pc-rar
https://tipeddsica1975.wixsite.com/franbitasy/post/windows-10-pro-x64-rs5-incl-office-2019-en-us-nov-2018-gen2-serial-key
https://vandenboo.wixsite.com/vetonserog/post/ssspsx-pad-plugin-pressure-mod-160-download
https://widsentzamhenslapa.wixsite.com/eruphiner/post/rar-vanchipattu-lyrics-222-utorrent-book-free-mobi
https://incotanmerugle.wixsite.com/lanithearwho/post/sap-business-one-8-8-license-crack
https://rail914ny.wixsite.com/samacita/post/ed-bibleworks-10-activation-torrent-crack-exe-full-version
https://flexentusystchobu.wixsite.com/prommodowla/post/netscan-full-version-activation-nulled-torrent-iso-x32
https://inwanesperale.wixsite.com/lisounamra/post/ccboot-game-menu-crack-21
https://hunderda.wixsite.com/sititinog/post/keygen-for-smscaster-e-marketer-gsm-standard-v3-7-montagegratuit-parti
https://nodonarviportre.wixsite.com/risbicori/post/winstep-xtreme-18-12-1373-multilingual-medicinebabu-free-cracked-utorrent-zip
https://knapicralansbi.wixsite.com/sembthatmechen/post/pc-cubaseelementsv706x86x-iso-64bit-activation-free-file
https://comptheverdaconve.wixsite.com/dieherasep/post/film-oui-french-kickass-full-dubbed-full
https://acilmigdersberpare.wixsite.com/throshalanne/post/gsdeditorv51-10-zip
https://distlycirater.wixsite.com/statigconri/post/alfaobd-crack
https://bomlitibidijo.wixsite.com/siobatfipunk/post/uvi-darklight-iix-torrent
https://evelynfineberg115q.wixsite.com/centdisttiperp/post/pedro-el-pollo-la-pelicula-dvdrip-espa-ol-latino-2-19
https://scottiewhitehorn59.wixsite.com/alereren/post/full-compufour-aplicativos-comerciais-2011-rio2016
vynynee (Monday, 31 January 2022 06:33)
vynynee c0c125f966 https://athoutcondexi.wixsite.com/gurddifresetz/post/copycat-5-720p-movies
https://bilcuralandcohan.wixsite.com/retrekena/post/utorrent-little-girls-on-the-beach-and-pool-37-013-imgsrc-ru-watch-online-x264-hd-download
https://juncraczibacanders.wixsite.com/tombrepleiga/post/x264-the-other-poker-girls-1293630539-imgsrc-ru-mkv-dvdrip-utorrent-4k-free-movie
https://siennafeliberty567.wixsite.com/conswiggsembri/post/tv-series-torrent-mission-impossible
https://jumpcapselec.wixsite.com/adobacsek/post/affresco-italiano-b1-pdf-31
https://maicualsicibore.wixsite.com/imtodonum/post/soal-ujian-masuk-fkg-moes-keygen-64-utorrent-pc-build
https://arafmoildedepemanc.wixsite.com/naudedenspran/post/free-girls-skirts-n-dresses-06-imgsrc-ru-activation-nulled-software
https://ballsapbestrilveba.wixsite.com/muegreatidop/post/vipbox-gloucester-vs-harlequins-streaming-online-link-2
https://saffierenkes024au3.wixsite.com/skybelatex/post/torrent-cute-girls-cutepeach008-imgsrc-ru-windows-full-x64-pro
https://passmonsyraravo.wixsite.com/awimfungu/post/trailer-park-kids-2-wt2-284-imgsrc-ru
https://juidoversodissi.wixsite.com/puzzsalcircsa/post/full-version-garage-doors-mod-minecraft-1-15-2-cracked-pro-utorrent-license
https://kenelmjure828b4c.wixsite.com/aselflanod/post/x32-dion-and-the-belmonts-greatest-hits-rar-rar-activator-utorrent-windows-build-crack
https://bosmonttabcons1988.wixsite.com/devisechowd/post/torrent-able-exe-full-x64
https://vuqile.wixsite.com/crakarasmar/post/tsuna-latest-torrent-activator-pc-rar
https://nategarnes6047mnw.wixsite.com/becyhoma/post/activator-expandrive-7-3-0-x64-nulled-download-full-version-windows
https://julianewallace.wixsite.com/viefredhumar/post/live-hapoel-be-er-sheva-fc-vs-ogc-nice-streaming-en-ligne
https://nanrimiketemp.wixsite.com/dotajobtmil/post/zynaptiq-plugin-bundle-win-macosx-ex23-serial-key-keygen
https://lizoperchickneedpe.wixsite.com/viegrounitsee/post/catalina-slow-wifi
https://raihevettali.wixsite.com/basskowscrowpo/post/ш-щѓш-щ-щ-шєщ-щ-ш-щ-щљщ-шєш-щѓщљщ-шєш-щ-щ-шєщѓщ-шєщѓщ-mp3-download
https://cobiwheelwcoroso.wixsite.com/lixanniro/post/ferdinand-the-bull-english-movie-download-in-hindi
https://peachleworfirsra.wixsite.com/neggagahu/post/girls-21-girls-209-imgsrc-ru
https://hodokov2010.wixsite.com/comstivibrist/post/neubau-bold-font-free-download
https://nabonecwitchcont.wixsite.com/uneneleb/post/exe-girls-mixed-02-mix16678-149-imgsrc-ru-pc-torrent-key-final
https://maerahapormuso.wixsite.com/preshubkulo/post/activation-big-mix-full-version-patch-64-torrent-final
https://gabriele97.wixsite.com/exretele/post/14yo-teen-girls-15yo-2e576f6c-e07a-4771-821c-86708257-imgsrc-ru-zip-torrent-full-activator
https://ruromabali.wixsite.com/anonafout/post/64-mp3-savage-love-mp3-full-version-patch-download-windows-pro-activator
https://menricksorpceme.wixsite.com/clicanpheiderc/post/hot-girls-assortment-42b4c379-9bfc-420d-9b22-e29792c8-imgsrc-ru
https://tripimhamastita.wixsite.com/bertukingba/post/thгґng-tin-miui-7-1-chг-nh-thб-c-ra-mбєїt-vг-o-ngг-y-5-1-2016
https://gisellerull814g9jh.wixsite.com/faeprevwhizztur/post/intro-pack-by-yuvi
https://kandicemackellar19.wixsite.com/bacourlydscons/post/utorrent-l-t2004_lsls-exe-activation-windows-x64-final
wannzebu (Monday, 31 January 2022 07:34)
wannzebu c0c125f966 https://nunniracpicom.wixsite.com/vineboore/post/female-anatomy-for-artist-download
https://raparhamengabur.wixsite.com/nidethinza/post/license-cara-nak-semak-nulled-full-version-64-file-download
https://mpixtorchildla1981.wixsite.com/ifracrimi/post/linear-system-thomas-kailath-solution-manual-rar
https://lconurketsevi.wixsite.com/rwebevprovwing/post/own-candids-img_8076-imgsrc-ru-pc-32bit-utorrent-full-final-crack-exe
https://myrnapratte809p269.wixsite.com/etelulla/post/draw-coordinates-on-google-maps
https://diamondrobel563n4b.wixsite.com/asatcultu/post/blanco-oven-manual-bs0632
https://tiobharenmiarea.wixsite.com/percoegregep/post/pc-recreation-and-entertainment-final-full-version-registration-torrent-32
https://wrenagandevlati.wixsite.com/neoprarpeci/post/download-full-version
https://ursulathompson84.wixsite.com/cardchambcere/post/torrent-salaam-e-ishq-dubbed-720-hd-dubbed-download
https://ldonimsisnosu.wixsite.com/texthorbovin/post/key-bnha-x-pregnant-rea-download-patch-pc-exe-32bit
https://hardthoculiden.wixsite.com/geschmisnolig/post/flexible-dancer-cocktease-b286e745-1563-4658-a3d9-99f8574a-imgsrc-ru
https://defwinngesuropu.wixsite.com/malsandtegib/post/girls-5-zobvx524dyg-1-imgsrc-ru
https://haicockmorinfoitra.wixsite.com/darmacyve/post/nice-screen-shot-2016-12-09-at-8-07-4-imgsrc-ru-pc-download-rar-32
https://tamekiabardin306sa.wixsite.com/gadsdalarti/post/32bit-ig-girls-4-376-imgsrc-ru-nulled-zip-activator-windows
https://denhett.wixsite.com/tenverssinle/post/64-bikini-mix-2-orii_martinet-11-imgsrc-ru-utorrent-file-rar-full
https://milagrossczbecki65.wixsite.com/roapunano/post/rar-2d-gateway-shopping-sites-file-windows-full-download-license
https://forenemindcha.wixsite.com/ningnawilra/post/license-young-mo-torrent-crack-64-full-version-pc-iso
https://schafitraivan1984.wixsite.com/sacrewirtbo/post/the_parent_trap_1998_movie_free
https://franseaw.wixsite.com/extrilsuacol/post/cute-kids-uj316bxiff8-imgsrc-ru
https://lornbinnsq5.wixsite.com/tiamimuvo/post/adobe-photoshop-cs6-extended-serial-number-keygen
https://evangelinabuschner.wixsite.com/drafralracer/post/windows-pic-simula-zip-x32-activator-full-version-utorrent
https://lallaraj29.wixsite.com/reukeyddoubvi/post/2k-www-8xflix-info-first-night-2020-hd-video-bluray-mkv-torrent-hd
https://niwamcaigusaczo.wixsite.com/atlyrate/post/young-hot-black-girls-with-smooth-legs-4828c272-d12d-40a8-b7cb-ded162ab-imgsrc-ru
https://unfloodpubnomodu.wixsite.com/trucagmismo/post/fabolous-street-dreams-subtitles-free-x264-english
https://nantvecourrefeewi.wixsite.com/ningnonspabpo/post/bikini-girls-eeb41ca9-678e-4562-9dfd-6d2ebd4c-imgsrc-ru
https://penphyothoto1972.wixsite.com/stoptiotatu/post/daz-studio-professional-v4-12-1-118-serials
https://pregerprepboa1971.wixsite.com/cuxilesyn/post/dvdrip-ganga-watch-online-subtitles-blu-ray-avi-watch-online
https://moddiapredunclubmi.wixsite.com/founnapega/post/fantasy-vii-advent-children-complete-full-dual-watch-online-kickass-dts
https://zyfquedeper1989.wixsite.com/amprathvengurg/post/windows-рїрѕрґсђрѕсѓс-рѕрє-img_7919-imgsrc-ru-full-utorrent-patch-zip
https://anderumbsoncmcafan.wixsite.com/centmarseate/post/beautiful-teresa-7-yo-85b3a90e-21ce-4ac3-a99f-b38d1d37-imgsrc-ru
raifri (Monday, 31 January 2022 09:50)
raifri c0c125f966 https://masbifisigsign.wixsite.com/rhenunlanet/post/download-4-zip
https://petrarca091zj.wixsite.com/tranastoro/post/english-original-audio-track-disturbia-2007-ac3-в-audio-tracks-for-movies
https://sashalkyfe.wixsite.com/guangbakasekt/post/angel-a2bff25b-7c04-4bf1-83dd-144e7375-imgsrc-ru
https://tikabohsawg1972.wixsite.com/vornalido/post/ready-to-get-all-wet-in-the-pool-aad11383984b7c92fda6f7420e06b3ee-imgsrc-ru
https://tarensi152.wixsite.com/kerwateript/post/doculivery-sign-in-registration-utorrent-free-final
https://tattpiskeyvitmiba.wixsite.com/fiseltihun/post/щ-шµш-ш-щ-шїщљщ-ш-щ-ш-шјщ-щ-щ-шјщ-шіш-щѓ-mp3-download
https://borislobanov593.wixsite.com/unpunesupp/post/21-tesla-mo-exe-crack-activator-full
https://rydibih.wixsite.com/heiratyrest/post/macos-catalina-10-15
https://savcacilupithooure.wixsite.com/cribkingbettou/post/crack-mila-tights-120202553_1242423339459079_45957-imgsrc-ru-full-pc-download-license-professional
https://piabrocexgoclicodi.wixsite.com/bucpuboco/post/karafun-studio-1-10a-download-rar-32-crack-free-registration-software
https://trigivbolnyaredi.wixsite.com/grohlightranrac/post/beautiful-14yo-ava-ava-is-daddys-favorite-27-imgsrc-ru-torrent-zip-full-pro
https://mohrmann607g.wixsite.com/leigastmati/post/girls-in-bikini-and-swimwear-1-p1190469-imgsrc-ru
https://bornemudaci.wixsite.com/wooohelciaje/post/hack-avira-antivirus-pro-2018-v22-0-8-633-key
https://veliandzcodd.wixsite.com/petscenpobal/post/lovely-lauryn-14-year-old-31-imgsrc-ru-exe-pro-full-version-patch-x64
https://creamsofttoghogema.wixsite.com/fimictipoc/post/sisters-preview-19-imgsrc-ru
https://vasiliynesterov674.wixsite.com/nediticbest/post/shell2vst-mac-download
https://ilwipsotechoo.wixsite.com/beaumidana/post/maria-vi-free-build-torrent-x32
https://feirieliri1982.wixsite.com/poutarvobell/post/dubbed-the-sims-4-s-full-dubbed-kickass-free
https://yongloranhjgs.wixsite.com/gohitchhostby/post/daughter-comments-please-tributes-also-20201219_223912-imgsrc-ru
https://promennasazan.wixsite.com/verbhanremo/post/hose-love-579a96ef-bade-48a1-8934-f1969cd0-imgsrc-ru
https://dodiekingcade865iz.wixsite.com/ansoware/post/kawasaki-mule-st-windows-ultimate-download-x32-nulled-zip
https://sacgoldcocurussi.wixsite.com/leiscufraga/post/lovely-day-bill-withers-mp3-zippy
https://tranmirockfrananto.wixsite.com/lingworkdystwreath/post/alcor_43b14
https://unicacsire.wixsite.com/biolaparbio/post/full-tг-lг-charger-un-fichier-nxmac-com_mso20191-professional-windows-torrent-exe-license
https://birgitfreeman.wixsite.com/nisleconny/post/windows-fat-boys-tr84ggzr0wu-imgsrc-ru-rar-full-version-activation-download
https://idlacdinalbint.wixsite.com/anidtanra/post/symptoms-of-a-faulty-diesel-primer-pump
https://flinnemafinfawelln.wixsite.com/morrmortdamcu/post/detection-of-di-renjie-2019-web-dl-720p-pp-mp4
https://brigittebennett2.wixsite.com/tavasnerect/post/build-ibeesoft-iphone-data-recovery-2-2-zip-free-utorrent-patch-windows-registration
https://ardonirablo.wixsite.com/ecephlihand/post/serial-otype-brooklyn-font-download-32-key-rar
https://barios669vuk.wixsite.com/taikepicol/post/file-lost-lands-mistakes-of-the-past-download-activation-windows
chedar (Monday, 31 January 2022 10:44)
chedar fb158acf10 https://marzurumoca.wixsite.com/cessringreter/post/advent-speaker-serial-numbers
https://ortizsandra7.wixsite.com/saychomanrarl/post/more-2-see-060512171421-imgsrc-ru
https://rimehgifolarmill.wixsite.com/layprunbendsa/post/windows-gala11-increг-ble-received_628693847584038-imgsrc-ru-full-serial-software-64bit-rar
https://drininunmirorock.wixsite.com/inefexiw/post/just-cause-3-pc-download-free
https://mozulocini2009.wixsite.com/cellreborntan/post/sp573-lil-blon-x64-free-iso-torrent-pro-windows
https://fresunriwate.wixsite.com/kaycrewvollso/post/ukrainian-girl-yana-k-9-16-yrs-рїрѕр-рљ9-imgsrc-ru
https://heartgaguttmarmath.wixsite.com/blumhasridan/post/mad-n-servers-down-twitter-full-rar-file-nulled-windows-license-torrent
https://laytingftetas1975.wixsite.com/riamunfeefic/post/windows-8-crack-all-version
https://forpafensmladac.wixsite.com/comgardsabta/post/model-girl-2-saphie-f7-imgsrc-ru
https://thaononrilastipor.wixsite.com/redsaggcesspac/post/zooskool-simone-first-cut
https://harriscrosier900p1.wixsite.com/rooficoza/post/older-kids-in-diaper-vidsnaps-caps-diaper-49-imgsrc-ru
https://rentcebermavefidd.wixsite.com/hydnititwijd/post/windows-games-x64-activation-full-software
https://swifesluperpie.wixsite.com/ifatreope/post/3dvista-virtual-tour-suite-2019-free-download-ms-3d-designer
https://pattersonclaudia.wixsite.com/membthylbestpi/post/i-love-it-14813353qvu-imgsrc-ru-64-download-pc-rar
https://sacnarearrelygorar.wixsite.com/trosicvaroug/post/racing-extinction-worksheet-answers
https://evemrituse.wixsite.com/paystyplipo/post/evening-fights-pw-pdvd_080-imgsrc-ru
https://ronosondakiren.wixsite.com/viosubtacom/post/themen-neu-2-kursbuch-reshebnik
https://telessalorwhiispad.wixsite.com/spicemconchea/post/windows-2-daughters-pool-imgsrc-ru-utorrent-exe-key
https://hzharris1985.wixsite.com/slinabacblan/post/samsung-spp-2040-digital-photo-printer-driver-for-mac
https://harmonydewick557ag.wixsite.com/berpaybemar/post/rebecca-11yo-girls-summer-2013-lake-photos-140210994844-imgsrc-ru
https://kaja8906.wixsite.com/beaubremenen/post/the-prototype-2013-dvdrip-xvid-rar-password
https://vragakexgetel.wixsite.com/peduckpuso/post/nautanki-saala-man-full-movie-dubbed-in-hindi-free-download
https://vasiliy19vk.wixsite.com/esutsenday/post/patch-hadidja-hadidja-8-imgsrc-ru-pro-64bit-pc-zip
https://davissabrina83.wixsite.com/thandkasasse/post/fluid-mechanics-for-chemical-engineers-noel-de-nevers-solution-manual-torrent-rar
https://letzmactonaterrext.wixsite.com/biatriborjour/post/arizona-state-vs-grand-canyon-online-live-stream
https://spantincloonisbe.wixsite.com/lijiggfulfe/post/final-my-princesses-51-imgsrc-ru-zip-activation-x32
https://bersreblidif1978.wixsite.com/rucmegera/post/whatsapp-background-wallpapers-posted-by-samantha-walker
https://chunn5867ot.wixsite.com/kicomlongtor/post/pc-just-boys-things-jbt2-7-imgsrc-ru-file-zip-utorrent
https://zilanmelinel.wixsite.com/midniapenkto/post/reign-of-darkness-ariana-nash-epub
https://attumescado.wixsite.com/regrastsewest/post/orb-crack-brush-zbrush-trial
ullzimr (Monday, 31 January 2022 11:25)
ullzimr fb158acf10 https://tarcareleja.wixsite.com/walgropilis/post/my-girl-30-my-girl-30-14-imgsrc-ru
https://satoprourosladest.wixsite.com/flatmenhapy/post/school-girl-camp-5-candid-ass-img_9687-imgsrc-ru
https://kindlinewsprocjets.wixsite.com/blogtipsperju/post/рїрѕр-рёрѕр-i-37-imgsrc-ru-full-pc-latest-download-keygen-x64-registration
https://onunkaicen1971.wixsite.com/platatalib/post/malwarebytes-winpe-v20-12-zip
https://ronetzcaparda.wixsite.com/northkilibo/post/boys-a-imgsrc-ru
https://guetufilasarosc.wixsite.com/holkeponu/post/webkinz-login
https://lighgiretrake.wixsite.com/tribanpaavers/post/nissan-battery-drain-problem
https://hawkins.wixsite.com/moghuabila/post/quikquak-pitchwheel-5-0-64bit-activator-final-pc-utorrent
https://hartprotroncanorle.wixsite.com/meerbesicut/post/live-boise-state-vs-san-jose-state-streaming-online-link-3
https://fraceromundayde.wixsite.com/tercapicard/post/preteenbook-2-bpbp35-imgsrc-ru
https://gauchirwollhem1977.wixsite.com/peuplasenac/post/shared-secrets41024-rar
https://dagakacihead.wixsite.com/redundiolatt/post/nn-teen-beach-bc-nn-57-imgsrc-ru-utorrent-registration-pc-professional-full-version-64bit-iso
https://prescorrogelo.wixsite.com/grumunocrac/post/look-up-charleston-3-walking-tours-in-the-holy-city-look-up-america-ebook-rar
https://hlystovka.wixsite.com/stattitogwa/post/registration-abandoned-homes-for-sale-in-mississippi-windows-rar-64bit-ultimate-download
https://dojb1980.wixsite.com/byojudgzabthe/post/windows-pastel-backgrounds-posted-by-sa-x32-zip-software-key-torrent
https://huntwinssubgoorate.wixsite.com/wancahossi/post/sleep-talking-spiritual-meaning
https://flourudcephigh.wixsite.com/exriraho/post/sacred-evil-a-true-s-dts-mkv-video-720p
https://defiddkatsgudoughl.wixsite.com/ndicelarprop/post/fav-boys-11272477fqt-imgsrc-ru-build-free-32bit-key-nulled-pc
https://baketsspecjeomero.wixsite.com/tenwheemuma/post/subtitles-kids-in-my-family-dvdrip-kickass-watch-online-dual-x264
https://dekeberna1983.wixsite.com/tangedete/post/imobie-anytrans-v7-1-1-2018-12-22-activated-license-zip-nulled-torrent-full-version
https://annamaejethro701bn.wixsite.com/faclidemo/post/windows-beautiful-alesya-gymnast-ales25-imgsrc-ru-rar-full-version-32bit-build-keygen-activation
https://orobtasitmo.wixsite.com/concadurchron/post/torrent-pasiely-img_5248~pho-pc-license-pro
https://dustdaxdiscmogeabc.wixsite.com/meovemaman/post/registration-phetsarath-ot-nulled-full-version-zip-64bit-software
https://blogkampnergtricso.wixsite.com/russhovicell/post/sane-new-world-epub-to-pdf
https://lucas94.wixsite.com/tiocintmicle/post/evil-dubbed-free-dual-watch-online-2k-dubbed-watch-online
https://downbiztorowalme.wixsite.com/viatifboove/post/diana-und-lisa-dsc01988-imgsrc-ru
https://skyjidtemenmo.wixsite.com/ybpienore/post/dil-dhadakne-do-2k-mp4-dubbed-dvdrip-hd
https://thopavarecom.wixsite.com/giboovecon/post/lor-pure-heroine-crack-windows-32-professional-full-version
https://derpitoutexchhokar.wixsite.com/disccessohu/post/rar-cute-dara-21151565_773367116175734_8831946-imgsrc-ru-keygen-x64-professional-windows-free
https://raucannerolipu.wixsite.com/isidrolna/post/4-ovslkxtvcqk-imgsrc-ru-zip-x32-nulled-utorrent
urielby (Monday, 31 January 2022 12:02)
urielby fb158acf10 https://larphedetrecil.wixsite.com/presgensmortli/post/inazuma-eleven-pc-game-english-version-free-download-torrents
https://avisnoakes394oe3c.wixsite.com/tricchiloti/post/the-hunger-games-kickass-video-mkv-watch-online-4k-blu-ray
https://nuebuzzhicendiecia.wixsite.com/neoriethylerw/post/download-911-vpn-setup
https://leiphybadelre.wixsite.com/taxcredisme/post/omni-step-patch-full-software-activation-32bit
https://lucahughes9.wixsite.com/ropidiffsys/post/beatriz-47acbbaa-107c-4ee0-b577-3dd85b83-imgsrc-ru
https://stanoxviloti.wixsite.com/chofadunlie/post/emerald-ecu-maps-download
https://gtipexeanitho.wixsite.com/tsongarrichi/post/download-mahu-1080p-mp4
https://vilytaninneuprot.wixsite.com/rerekuco/post/omar-series-episo-x32-build-torrent-exe-patch
https://katheygrauman966oa.wixsite.com/hastlindlenlu/post/leggings-20160507_110923671_ios-imgsrc-ru
https://nigelialangdale118.wixsite.com/laycosulgo/post/heiгџe-hг-schen-und-andere-sachen-965-imgsrc-ru
https://borisisaev141.wixsite.com/lanspitswindme/post/build-р-рµс-рѕ-рі-р-р-рірµсђрµ-p9145422-imgsrc-ru-windows-cracked-download-free-exe
https://marmentmentighka.wixsite.com/inunquegai/post/torrent-propellerhead-reason-602-for-mac-osx-and-win
https://netmentcosdeza.wixsite.com/tilmuderi/post/green-screen-news-room-posted-by-john-johnson
https://phyofqualundiestar.wixsite.com/copdescfacti/post/full-version-svetlananagornya-treiding-slivkursa-cky-windows-build-x32-utorrent
https://imitbinityvin.wixsite.com/lenbergkano/post/la-lingua-italiana-per-stranieri-katerinov-chiavi-pdf-30
https://averyhillers048o2w.wixsite.com/adesasgu/post/preteen-feet-574ccace2089c41cb3e6cc5927df01e1-imgsrc-ru
https://tamiecui9440rg.wixsite.com/mortprefchemo/post/oculus-rift-stutter-fix-64-crack-free-windows-activator-ultimate
https://zoetessudenboperwh.wixsite.com/tentsacmifu/post/admau5-able-professional-exe-64-windows
https://meputbecushamell.wixsite.com/frechysthonet/post/keygen-st-louis-w-x32-professional-exe-license-pc-full
https://soratwit.wixsite.com/nalichurti/post/vanessa-and-others-p1050446-2-imgsrc-ru-keygen-download-activation-full-version-32bit-rar-pc
https://obvandidocon.wixsite.com/zahmenslepde/post/torrent-my-niece-nn-13-activation-file-crack
https://jeanette0.wixsite.com/essessaha/post/free-buried-truth-of-the-maya-2019-yts-pc-rar-patch
https://loakenlignbarsto.wixsite.com/chieltinrarac/post/serial-lagu-key-torrent-64-build-rar
https://lepasacadyssia.wixsite.com/gopadenpkon/post/pho-shop-cc-2015-for-iso-x32-utorrent-ultimate-full-macos
https://swigunloonone.wixsite.com/inryutiquaf/post/epson-xp-440-fac-keygen-software-key-utorrent-pc
https://teestanedeemtuca.wixsite.com/bestsanewbi/post/candid-tight-ass-51-capture20201011003703167-imgsrc-ru
https://varelenquidrogin.wixsite.com/pardeeapina/post/vidblaster-studio-pro-2-27-keygen-11
https://delottycandi.wixsite.com/liralelo/post/mix-fb_img_1608896851380-imgsrc-ru-pc-download-key-crack-x64-free
https://heibult892.wixsite.com/abblasciva/post/ksenia-v-w_db9c8e23-imgsrc-ru
https://dorward958ujx4.wixsite.com/eronlyimang/post/gorilas-en-la-niebla-dvdrip-spanis-ingl
shatapa (Monday, 31 January 2022 12:40)
shatapa fb158acf10 https://penratechtdergcons.wixsite.com/vicvepusun/post/please-enjoy-30-imgsrc-ru
https://myrnapratte809p269.wixsite.com/etelulla/post/summer-series-wlyybj_0060-2-imgsrc-ru-torrent-zip-32bit-pc
https://nemriocontculope.wixsite.com/compjanecor/post/alcorn-state-live-stream-online-x32-patch-torrent-activator-windows
https://jonghamostgovbank.wixsite.com/neineguscou/post/b-et-boy-1-c73f7154-effc-4dc0-8265-d622c7b7-imgsrc-ru-serial-windows-latest-torrent-registration
https://kozhevnica.wixsite.com/racostpulnie/post/sholay-subtitles-watch-online-movies-free-4k-utorrent-mp4
https://chlorsocapti1972.wixsite.com/tattpeerfjustconf/post/western-civilization-spielvogel-textbook-pdf
https://junarmenah.wixsite.com/psoreldiagas/post/metaphors-for-sadness
https://rietartincting1975.wixsite.com/ciaconbetu/post/diaper-boys-mix-diaper25-imgsrc-ru-zip-pc-utorrent-x64-nulled
https://shardanate259xs6.wixsite.com/dimpvirafme/post/crack-starseed-lineage-activation-pc-x32-free
https://oslalobenchcelldis.wixsite.com/onverritil/post/scp-999-w-activation-64-windows-exe-keygen-torrent-file
https://adpl2001.wixsite.com/sisadende/post/cute-random-boys-30-image-39-imgsrc-ru
https://magdawebb.wixsite.com/eqexelnar/post/thais-souto-friends-family-pqaaahxoxb-yerlemlregrjt-ugbetbb-imgsrc-ru
https://cenwhafomemila.wixsite.com/quechiciles/post/12yo-stepdaughter-panties-i-imgsrc-ru_69063790umv-imgsrc-ru
https://belenxye8ca.wixsite.com/heyquesige/post/easeus-data-recovery-wizard-8-5-unlimited-multi-patch-ultimate-registration-64-utorrent-free
https://longbemitertio.wixsite.com/betrateso/post/test-boys-imgsrc-ru-windows-cracked-torrent-full-version
https://myogirodep1989.wixsite.com/paegnosamin/post/gabbar-is-back-2-in-avi-full-torrents-subtitles-movie-dubbed
https://flower86nlindau.wixsite.com/louikathera/post/fall-in-love-with-little-layla-layla-73-imgsrc-ru
https://tacalremathi.wixsite.com/neningtranin/post/league-table-generator
https://unwengarbgi1974.wixsite.com/mostsferivhi/post/qasas-ul-ambia-in-bangla-pdf-free
https://itliadohandmes.wixsite.com/fectpsycharim/post/laila-3-laila-461-imgsrc-ru-latest-windows-nulled-utorrent-free-64bit-rar
https://stadtherntranmomea.wixsite.com/bremeqacac/post/lil-cutie-amari-imgsrc-ru-patch-build-x64-pc-activator-download
https://roafranfurlycont.wixsite.com/ovemreelu/post/exe-ewp-hanging-eileen-eileen-schulz-mpg-cracked-windows-full-x32
https://hilmapfirsch267lxh.wixsite.com/rerestrinfai/post/brian-boy-bx583jk2-imgsrc-ru
https://beatrisromera114v0.wixsite.com/reattaupergeo/post/full-cute-budding-black-teens-2-mari-13-imgsrc-ru-nulled-64-pc
https://earewql.wixsite.com/spiremdigo/post/cracked-two-sisters-age-10-and-14yo-ez-10-5-imgsrc-ru-full-license-file-pc-zip
https://finnegbabi.wixsite.com/ogpenhoter/post/live-arizona-state-vs-california-online-arizona-state-vs-california-stream-link-3
https://hunnaponrarati.wixsite.com/vietelstiris/post/mo-poly-here-and-pc-serial-registration-64bit-full-version-zip-download
https://contvecenttesmo.wixsite.com/palebocria/post/latest-letter-of-intent-template-for-graduate-school-64-pc-exe-activation
https://altringer365v7.wixsite.com/nanthmitpietio/post/coins-unlimited-windows-full-version-nulled-32-professional-download-key
https://andreyvvlukin.wixsite.com/destdisgebit/post/pioneer-avic-d1-install-manual
shatapa (Monday, 31 January 2022 12:40)
shatapa fb158acf10 https://penratechtdergcons.wixsite.com/vicvepusun/post/please-enjoy-30-imgsrc-ru
https://myrnapratte809p269.wixsite.com/etelulla/post/summer-series-wlyybj_0060-2-imgsrc-ru-torrent-zip-32bit-pc
https://nemriocontculope.wixsite.com/compjanecor/post/alcorn-state-live-stream-online-x32-patch-torrent-activator-windows
https://jonghamostgovbank.wixsite.com/neineguscou/post/b-et-boy-1-c73f7154-effc-4dc0-8265-d622c7b7-imgsrc-ru-serial-windows-latest-torrent-registration
https://kozhevnica.wixsite.com/racostpulnie/post/sholay-subtitles-watch-online-movies-free-4k-utorrent-mp4
https://chlorsocapti1972.wixsite.com/tattpeerfjustconf/post/western-civilization-spielvogel-textbook-pdf
https://junarmenah.wixsite.com/psoreldiagas/post/metaphors-for-sadness
https://rietartincting1975.wixsite.com/ciaconbetu/post/diaper-boys-mix-diaper25-imgsrc-ru-zip-pc-utorrent-x64-nulled
https://shardanate259xs6.wixsite.com/dimpvirafme/post/crack-starseed-lineage-activation-pc-x32-free
https://oslalobenchcelldis.wixsite.com/onverritil/post/scp-999-w-activation-64-windows-exe-keygen-torrent-file
https://adpl2001.wixsite.com/sisadende/post/cute-random-boys-30-image-39-imgsrc-ru
https://magdawebb.wixsite.com/eqexelnar/post/thais-souto-friends-family-pqaaahxoxb-yerlemlregrjt-ugbetbb-imgsrc-ru
https://cenwhafomemila.wixsite.com/quechiciles/post/12yo-stepdaughter-panties-i-imgsrc-ru_69063790umv-imgsrc-ru
https://belenxye8ca.wixsite.com/heyquesige/post/easeus-data-recovery-wizard-8-5-unlimited-multi-patch-ultimate-registration-64-utorrent-free
https://longbemitertio.wixsite.com/betrateso/post/test-boys-imgsrc-ru-windows-cracked-torrent-full-version
https://myogirodep1989.wixsite.com/paegnosamin/post/gabbar-is-back-2-in-avi-full-torrents-subtitles-movie-dubbed
https://flower86nlindau.wixsite.com/louikathera/post/fall-in-love-with-little-layla-layla-73-imgsrc-ru
https://tacalremathi.wixsite.com/neningtranin/post/league-table-generator
https://unwengarbgi1974.wixsite.com/mostsferivhi/post/qasas-ul-ambia-in-bangla-pdf-free
https://itliadohandmes.wixsite.com/fectpsycharim/post/laila-3-laila-461-imgsrc-ru-latest-windows-nulled-utorrent-free-64bit-rar
https://stadtherntranmomea.wixsite.com/bremeqacac/post/lil-cutie-amari-imgsrc-ru-patch-build-x64-pc-activator-download
https://roafranfurlycont.wixsite.com/ovemreelu/post/exe-ewp-hanging-eileen-eileen-schulz-mpg-cracked-windows-full-x32
https://hilmapfirsch267lxh.wixsite.com/rerestrinfai/post/brian-boy-bx583jk2-imgsrc-ru
https://beatrisromera114v0.wixsite.com/reattaupergeo/post/full-cute-budding-black-teens-2-mari-13-imgsrc-ru-nulled-64-pc
https://earewql.wixsite.com/spiremdigo/post/cracked-two-sisters-age-10-and-14yo-ez-10-5-imgsrc-ru-full-license-file-pc-zip
https://finnegbabi.wixsite.com/ogpenhoter/post/live-arizona-state-vs-california-online-arizona-state-vs-california-stream-link-3
https://hunnaponrarati.wixsite.com/vietelstiris/post/mo-poly-here-and-pc-serial-registration-64bit-full-version-zip-download
https://contvecenttesmo.wixsite.com/palebocria/post/latest-letter-of-intent-template-for-graduate-school-64-pc-exe-activation
https://altringer365v7.wixsite.com/nanthmitpietio/post/coins-unlimited-windows-full-version-nulled-32-professional-download-key
https://andreyvvlukin.wixsite.com/destdisgebit/post/pioneer-avic-d1-install-manual
sobeell (Monday, 31 January 2022 16:55)
sobeell f4bc01c98b https://coub.com/stories/3385470-ps2-usb-util-v2-1-full-english-free-download-rar-ferrvict
https://coub.com/stories/3385469-reactor-6-2-0-full-crack-gilken
https://coub.com/stories/3385468-agustincamposarenaspensamientocriticopdf-patched
https://coub.com/stories/3385467-perfecto-garcia-chornet-metodo-de-13-top-129311
https://coub.com/stories/3385466-link-fabulous-angelas-sweet-revenge-pe-final-2015-foxy-games-license-key
https://coub.com/stories/3385465-htc-pda-rom-upgrade-utility-3-27-4-3-mobims-15-wiaing
https://coub.com/stories/3385464-hd-online-player-download-free-movie-ishaqzaade-in-hi-fridree
https://coub.com/stories/3385462-24-season-2-download-exclusive-utorrentgolkes
https://coub.com/stories/3385463-persamaan-mosfet-sm-630-n
https://coub.com/stories/3385461-hot-dabbe-3-torrent-indir
https://coub.com/stories/3385457-best-call-of-duty-black-ops-update-4-read-nfo-skidrow-hack-tool-download
https://coub.com/stories/3385460-fixed-cossacks-3-download-ita
https://coub.com/stories/3385459-manjula-aunty-kannada-sex-kathegalu-samuthr
https://coub.com/stories/3385458-better-star-command-galaxies-alpha-6-skidrow-reloaded
https://coub.com/stories/3385456-total-network-inventory-4-3-1-build-4212-with-full-crack-license-key-update-olwyokii
https://coub.com/stories/3385455-ambulimama-stories-in-tamil-pdf-free-pedrwyl
https://coub.com/stories/3385454-monopolyplussteampunkskeygenerator-new
https://coub.com/stories/3385453-ancient-aliens-the-game-mod-unlock-all
https://coub.com/stories/3385452-exclusive-tharai-thappattai-mp4-full-movie-download
https://coub.com/stories/3385451-vray-studio-tools-v1-3-5-pro-rar-top
https://coub.com/stories/3385449-clara-ravens-dcv-download-repack
https://coub.com/stories/3385450-soodhu-kavvum-2013-lotus-dvdrip-xvid-1cd-700mb-tamil-23-free
https://coub.com/stories/3385448-gundam-00-movie-sub-indo-720p-film
https://coub.com/stories/3385447-portable-sony-vaio-pcg-3b2l-drivers
https://coub.com/stories/3385446-nudist-miss-junior-beauty-pageant-contest-11-117golkes-takbla
https://coub.com/stories/3385445-download-repack-carry-on-pandu-marathi-movie-kickass-torrent
https://coub.com/stories/3385444-introduction-to-embedded-systems-by-shibu-k-v-pdf-files-ransrash
https://coub.com/stories/3385443-hot-ginecologiadenovak15edicionpdfdownload
https://coub.com/stories/3385442-fixed-integraltransformsbygoyalandguptapdffreedownloadzip
https://coub.com/stories/3385441-_verified_-teknosam-2-0-serious-sam-20
zopger (Monday, 31 January 2022 18:24)
zopger f4bc01c98b https://coub.com/stories/3299757-top-tgt-three-kings-2013
https://coub.com/stories/3299758-wpfront-user-role-editor-pro-nulled-15-eladari
https://coub.com/stories/3299756-__exclusive__-private-video-magazine-3
https://coub.com/stories/3299755-my-sims-itwins-link-crack
https://coub.com/stories/3299753-buffy-season-1-720p-torrent
https://coub.com/stories/3299751-she-s-the-man-1080p-torrent-opeyan
https://coub.com/stories/3299749-terjemah-kitab-qurrotul-uyun-pdf-geowilm
https://coub.com/stories/3299748-bookworm-deluxe-nl-2lions-team-lucky-patcher-hot
https://coub.com/stories/3299747-crack-dmitrirender-v4-beta-uncracked-l-exclusive
https://coub.com/stories/3299745-hd-online-player-radmin-server-3-5-crack-keygen-softw-denall
https://coub.com/stories/3299742-xf-a2011-64bits-87-best
https://coub.com/stories/3299740-verified-xforce-keygen-autocad-2012-x86-x64go
https://coub.com/stories/3299739-portable-microsoft-word-2007-free-download-full-version-brothersoft-games
https://coub.com/stories/3299736-wirelesscommunicationbymulletpdfdownload-yamhung
https://coub.com/stories/3299735-link-doutrina-e-teologia-de-umbanda-sagrada-rubens-saraceni-pdf-files
https://coub.com/stories/3299731-contoh-surat-rujukan-puskesmas-ke-rumah-sakit-attody
https://coub.com/stories/3299729-filmesonlinerambo5dublado-link
https://coub.com/stories/3299728-sleeping-dogs-crack-update-17-15-sadver
https://coub.com/stories/3299726-moyea-ppt-to-video-converter-registration-code-keygen-hot-torrent
https://coub.com/stories/3299727-seed-of-chucky-full-movie-in-hindi-dubbed-846-railnen
https://coub.com/stories/3299725-super-contra-8-free-__full__-download
https://coub.com/stories/3299722-virtual-dj-mapper-for-pioneer-ddj-sx-top
https://coub.com/stories/3299721-shajahan-full-movie-hd-download-verified
https://coub.com/stories/3299719-p3d-just-flight-c152-crack-extra-quality
https://coub.com/stories/3299718-swiss-kraft-sk-8500w-manual-epub-work
https://coub.com/stories/3299717-ddx-software-easy-wood-amosla
https://coub.com/stories/3299716-disaster-management-book-class-9-ncert-in-english-layunit
https://coub.com/stories/3299715-goodsync-10-9-29-crack-hartgile
https://coub.com/stories/3299713-midas-gen-2015-crack-download-jaelgeor
https://coub.com/stories/3299711-flipalbum-vista-pro-7-serial-number
benezad (Monday, 31 January 2022 19:02)
benezad f4bc01c98b https://coub.com/stories/3341739-believe-in-forever-jett-series-book-3-books-pdf-file-top
https://coub.com/stories/3341741-joshua-goodman-vs-brooklyn-bodywrecker-dasjan
https://coub.com/stories/3341740-new-ror-cards-bhandarkar-publications-pdf-34
https://coub.com/stories/3341743-suicidesquadenglishhindimoviedvdripdownload-upd
https://coub.com/stories/3341736-download-updated-musicasanos70e80
https://coub.com/stories/3341745-mujahid-balussery-speech-mp3-dow
https://coub.com/stories/3341749-grand-ages-rome-gold-edition-serial-key-free
https://coub.com/stories/3341750-hikmat-ki-kitab-urdu-pdf-download-cracked-arabic-navigator-lag
https://coub.com/stories/3341752-better-3-angoori-bani-angaara-mp4-full-movie-free-download
https://coub.com/stories/3341755-link-aao-pyar-karen-full-movie-downloadl
https://coub.com/stories/3341758-nascar-simracing-rar-download-deiaansl
https://coub.com/stories/3341760-battle-cards-savage-heroes-tcg-ccg-decks-v1-4-15-mod-apk-geshar
https://coub.com/stories/3341762-beauty-and-the-beast-english-1-telugu-movie-free-download-3gp-rayabapt
https://coub.com/stories/3341766-schneider-electric-pl7-pro-v4-5-rar-peaksyr
https://coub.com/stories/3341765-introduction-to-mythology-contemporary-approaches-to-classical-and-world-myths-books-pdf-krihug
https://coub.com/stories/3341767-hot-bravely-default-flying-fairy-soundtrack-by-revo-rar
https://coub.com/stories/3341764-mallelatheegalasirimallepuvvumoviedownloadutorrent-hasyans
https://coub.com/stories/3355584-playful-kiss-full-episodes-free-download-hot-with-english-subtitles
https://coub.com/stories/3337444-hum-aapke-hain-koun-full-movie-hd-1080p-free-16-henjarv
https://coub.com/stories/3337440-work-descarga-el-mejor-antimalware-portable-para-usb-2020
https://coub.com/stories/3337442-fixed-dragonageorigins105trainer
https://coub.com/stories/3337438-halimbawa-ng-mga-anekdota-ng-mga-bayani-favoally
https://coub.com/stories/3337437-toni-braxton-ft-trey-songz-free-mp3-download-best
https://coub.com/stories/3337435-link-research-methodology-pdf-books-free-download
https://coub.com/stories/3337434-the-pool-download-movie-1080p-torrent-link
https://coub.com/stories/3337433-skech-bluetooth-headphones-bth561-user-manual-pdf-taiwel
https://coub.com/stories/3337432-plantasia-cracked-download-full-version-72
https://coub.com/stories/3337431-3-idiots-full-movie-hd-1080p-free-download-kickasstorrent-link
https://coub.com/stories/3337428-spc-international-creative-album-vol-13-20-better
https://coub.com/stories/3337427-ayurved-sar-sangrah-book-200
hugoimog (Monday, 31 January 2022 19:39)
hugoimog f4bc01c98b https://coub.com/stories/3474539-total-quality-management-book-by-jayakumar-pdf-22-naygal
https://coub.com/stories/3474538-less-and-more-the-design-ethos-of-dieter-rams-pdf-pdf-pdf
https://coub.com/stories/3474537-etka-7-3-updates-vw-audi-906-to-915-64-bit-ellarah
https://coub.com/stories/3474535-verified-tutorial-sap2000-indonesia-pdf-download
https://coub.com/stories/3474536-audio-guide-download-john-legend-all-of-me-free-musicpleer-repack
https://coub.com/stories/3474534-cb-sachdeva-class-12-macroeconomics-pdf-download-_verified_
https://coub.com/stories/3474533-pdf-xchange-viewer-pro-serial-keygen-15-illauma
https://coub.com/stories/3474531-la-troia-nel-cortile-full-watyil
https://coub.com/stories/3474532-extra-quality-humming-korean-movie-eng-sub
https://coub.com/stories/3474530-descargar-gratis-bb-multi-unlocker-key-v-19-0-patched
https://coub.com/stories/3474529-new-sailor-moon-movie-720p-kickass-torrent
https://coub.com/stories/3474528-new-the-social-network-movie-with-english-subtitle-free-download
https://coub.com/stories/3474527-upload-photo-see-hairstyles-suit-you-free-fabyvasi
https://coub.com/stories/3474526-root-tool-case-v1-15-0-premium-aosp-latest
https://coub.com/stories/3474525-jeeyo-shaan-se-full-movie-download-in-720p-hd-link
https://coub.com/stories/3474524-free-download-huawei-modem-unlocker-v10-by-micro-box-teamrar-garnfinn
https://coub.com/stories/3474523-pagalworld-chota-bheem-video-portable
https://coub.com/stories/3474522-download-__link__-sweet-possession-maya-banks-epub
https://coub.com/stories/3474520-microsoft-office-standard-2013-product-key-generator-vermele
https://coub.com/stories/3474521-toyota-techstream-keygen-activation-crack-trisren
https://coub.com/stories/3474519-hot-danielle-wolfe-nude-pics
https://coub.com/stories/3474518-rldea-dll-crysis-3-fix-17
https://coub.com/stories/3474517-sylenth1-3-064-best-crack-download-here
https://coub.com/stories/3474516-tom-and-jerry-cartoon-dvdrip-22
https://coub.com/stories/3474514-hot-angel-summers-tyna-enquetes-tres-privees-le-client-timide-rar
https://coub.com/stories/3474515-propellerhead-the-salazar-brothers-reggaeton-refill-1-laurfig
https://coub.com/stories/3474513-portable-boyka-undisputed-4-french-torrentgolkes
https://coub.com/stories/3474512-captain-tsubasa-ps2-ntsc-jap-iso
https://coub.com/stories/3474510-railway-empire-the-great-lakes-codex-crack-free-hot
https://coub.com/stories/3474511-argentino-luna-discografia-completa-mediafire-hot
julbir (Monday, 31 January 2022 20:20)
julbir f4bc01c98b https://coub.com/stories/3380119-free-download-mdi-jade-5-0-ranglaw
https://coub.com/stories/3380118-full-femme-sexe-image-sans-gras
https://coub.com/stories/3380117-hot-wish-upon-english-hd-720p-download
https://coub.com/stories/3380116-top-barbie-swan-lake-movie-download
https://coub.com/stories/3380115-__exclusive__-sambhaji-kadambari-by-vishwas-patil-20
https://coub.com/stories/3380113-updated-bluestacks-for-windows-7-32-bit-1gb-ram-download
https://coub.com/stories/3380114-hindi-hd-guardians-of-the-galaxy-vol-2-movies-1080p-torrent-_hot_
https://coub.com/stories/3380112-mamanarum-marumagal-thamil-sex-stories
https://coub.com/stories/3380111-marcel-m-rod-paragonmen-download-charans
https://coub.com/stories/3380110-300-rise-of-an-empire-online-subtitrat-hd-720p
https://coub.com/stories/3380109-updated-thebookofchanchaldownloadinhindi
https://coub.com/stories/3380108-epson-r280-adjustment-program-annaros
https://coub.com/stories/3380107-work-manfred-mann-do-wah-diddy-diddy-mp3
https://coub.com/stories/3380106-microsoft-office-professional-plus-2010-product-key-version-14-0-4734-1000-furnimm
https://coub.com/stories/3380105-keygen-for-melodyne-31-20-15-hendia
https://coub.com/stories/3380104-crack-verified-paradigmgocadskuav20092build2rar
https://coub.com/stories/3380103-hd-online-player-ram-lakhan-full-movie-free-download-hot
https://coub.com/stories/3380102-fix-mali-budo-ceo-film-download-torrent-filme
https://coub.com/stories/3380101-jumanji-2-full-movie-in-hindi-download-work-hd
https://coub.com/stories/3380100-verified-velamma-episode-4-hindi-pdf-download
https://coub.com/stories/3380098-top-povarabunatatiinoastredeiondrutapdfdownload
https://coub.com/stories/3380097-motu-patlu-king-of-kings-movie-with-english-subtitles-download-top-for-movie
https://coub.com/stories/3380095-3-words-8-letters-say-it-and-i-m-yours-ebook-download-__link__
https://coub.com/stories/3380096-exclusive-alfu-laila-wa-laila-pdf-download
https://coub.com/stories/3380094-xmp-panels-4-0-sti-download-gorway
https://coub.com/stories/3380093-top-ibm-imm-activation-key-743
https://coub.com/stories/3380092-3dsemulatorbiosfilerar
https://coub.com/stories/3380091-bsplayer-pro-2-0-937-keygen-rar-download-pc-berode
https://coub.com/stories/3380090-nicelabel-designer-pro-6-crack-exclusive
https://coub.com/stories/3380089-portable-power-cd-g-player-pro-1-0-3-full-rar
xinari (Monday, 31 January 2022 20:58)
xinari f4bc01c98b https://coub.com/stories/3362115-differential-and-integral-calculus-by-feliciano-and-uygolkes-2021
https://coub.com/stories/3362111-accusonus-era-bundle-pro-4-1-10
https://coub.com/stories/3362110-fix-kartodromo-ciudad-evita-rfactor-13
https://coub.com/stories/3362109-better-the-data-warehouse-lifecycle-toolkit-2nd-edition-pdf-free-download
https://coub.com/stories/3362108-free-luxonixpurityserialnumbermactorrent
https://coub.com/stories/3362105-fratmensucks-cole-and-neil-gay-zip-beryzenp
https://coub.com/stories/3362104-hindi-language-learning-through-tamil-pdf-download-latepear
https://coub.com/stories/3362103-fifa-16-crack-3dm-v1-free-best-download
https://coub.com/stories/3362099-hindi-movies-kuch-kuch-locha-hai-free-download-winfmar
https://coub.com/stories/3362097-full-akame-ga-kill-complete-series-episode-1-24-english-subbed-360p-46
https://coub.com/stories/3362096-student-of-the-year-movie-english-subtitle-__hot__-free-download
https://coub.com/stories/3362095-veluthu-kattu-movie-mp4-download-exclusive-k
https://coub.com/stories/3362092-full-pluraleyes-3-5-serial-keygen-and-crack
https://coub.com/stories/3362090-cece-winans-throne-room-full-patched-album-zip
https://coub.com/stories/3362084-program-do-projektowania-szaf-komandor-chomikuj-software-engineer-walway
https://coub.com/stories/3362085-smart-mzd-player-full-v10-0-patched-apk-leshhest
https://coub.com/stories/3362083-adobe-dreamweaver-cc-13-2-serial-number-nanvyv
https://coub.com/stories/3362082-alpha-and-omega-2-a-howl-iday-adventure-torrent-malvvand
https://coub.com/stories/3362080-atnsoft-key-remapper-crack-seria-work
https://coub.com/stories/3362079-refog-employee-monitor-7-6-full-crack-davden
https://coub.com/stories/3362078-kedara-gowri-vratam-book-in-tamil-pdf-90-rawsyury
https://coub.com/stories/3362077-crack-extra-quality-fsxpmdg737ngx
https://coub.com/stories/3362075-red-giant-trapcode-suite-16-2-7-key-for-windows-crack-top-rar
https://coub.com/stories/3362074-brazilian-naturist-festival-tour-movies-heerglo
https://coub.com/stories/3362072-cracksqlways60-verified
https://coub.com/stories/3362068-jasc-paint-shop-pro-9-keygen-portable-crack
https://coub.com/stories/3362065-exclusive-simulator-cnc-heidenhain-itnc-530-simulator-cnc-machines-sinutrain-603
https://coub.com/stories/3362061-maa-pasalapudi-kathalu-stories-pdf-free-download-new
https://coub.com/stories/3362062-zero-hour-a-royal-massacre-hai-full-movie-free-install-download
https://coub.com/stories/3362058-kelley-blue-book-for-5th-wheel-campers-zip-repack
kaeedou (Monday, 31 January 2022 21:35)
kaeedou f4bc01c98b https://coub.com/stories/3353910-free-grimm-saison-2-complete-french-torrent
https://coub.com/stories/3359889-timeshift-cd-key-code-serial-install
https://coub.com/stories/3359890-dragons-witches-and-other-fantasy-creatures-in-origamirar-verified
https://coub.com/stories/3359892-download-crack-pes-2006-torent-tpb-portable
https://coub.com/stories/3359893-trainz-route-mojave-sub-division-free-download-portable-hot
https://coub.com/stories/3359894-download-terjemahan-kitab-tanbihul-ghafilin-pdf-readerl-top
https://coub.com/stories/3359898-distance-ochiru-tenshi-vol-03-c20-23-rar-pipihors
https://coub.com/stories/3359901-immo-universal-decoding-3-2-keygen-download-mediafire-exclusive
https://coub.com/stories/3359903-fs2004-alphasim-su-33-naval-flanker-admiral-kuznetsov-rar-janibir
https://coub.com/stories/3359906-verified-code-visual-to-flowchart-v30-crack
https://coub.com/stories/3359907-download-steam-api-dll-for-call-of-duty-black-ops-arial-todos-recreati-algkend
https://coub.com/stories/3359913-upd-meigs-financial-accounting-11th-edition-solutions
https://coub.com/stories/3359912-jai-dakshineshwar-kali-maa-2-720p-blu-ray-movies-herflo
https://coub.com/stories/3359916-valya-sister-final-version-part-0321
https://coub.com/stories/3359917-ram-leela-full-movie-download-hd-1080pl-best
https://coub.com/stories/3359918-patched-quest-hindi-movie-download-720p-hd
https://coub.com/stories/3359919-gta-vice-city-java-games-128-160-caicar
https://coub.com/stories/3359921-fsx-captain-sim-757-200-captain-block-b-v1-3-keygen-free
https://coub.com/stories/3359923-cadence-allegro-extracta-exe-best-download
https://coub.com/stories/3359925-realspeak-daniel-22khz-british-english-voice-sapi-5-serial-key-exclusive
https://coub.com/stories/3359920-repack-oracle-11g-dba-cbt-training-videos-download
https://coub.com/stories/3359928-download-easeus-data-recovery-wizard-professional-4-3-6-full-version-carfro
https://coub.com/stories/3359932-link-the-white-land-5-full-movie-in-hindi-free-download-hd
https://coub.com/stories/3359933-dhoom-3-full-movie-480p-download-brinal
https://coub.com/stories/3359935-fast-amp-furious-7-english-movie-download-kickass-720p-torrent-wanijasd
https://coub.com/stories/3359936-link-crack-keygen-3ds-max-2016-crack
https://coub.com/stories/3359937-exclusive-downloadworldwarzmoviesubtitleindonesiamomentum
https://coub.com/stories/3359938-shootout-at-wadala-hd-movies-download-720p-anjewan
https://coub.com/stories/3359943-new-download-subtitle-indonesia-kehta-hai-dil-baar-baar
https://coub.com/stories/3359944-windows-8-free-_verified_-torrent-download-full-version
ulalell (Monday, 31 January 2022 22:12)
ulalell f4bc01c98b https://coub.com/stories/3411578-__link__-l-orologiaio-riparatore-pdf-download
https://coub.com/stories/3411573-driving-zone-2-ver-0-68-unlimited-money-mod-apk-helfeli
https://coub.com/stories/3411569-mathtype-7-9-crack-with-activation-code-free-download-2019-patched
https://coub.com/stories/3411566-download-super-phisher-1-0-freedcinst-better
https://coub.com/stories/3411561-crack-adobe-photoshop-cc-2018-v19-1-5-x86-x64-multilingual-update-sahdar
https://coub.com/stories/3411560-cg-lolita-channel-cg-158-cg-epub-betdel
https://coub.com/stories/3411559-aboboy-s-small-adventure-ingwal
https://coub.com/stories/3411558-agentvinoddubbedmoviesinhindi720p
https://coub.com/stories/3411557-raees-4-full-movie-free-download-in-hindi-hd-mp4-fayrmac
https://coub.com/stories/3411556-kitab-qawaid-fiqhiyyah-pdf-187
https://coub.com/stories/3411530-free-scrum-the-art-of-doing-twice-the-work-in-half-the-time-epub
https://coub.com/stories/3411528-__top__-office2010vlactivationtool
https://coub.com/stories/3411525-verified-scaricare-autocad-mobile-2014-crack-64-bits
https://coub.com/stories/3411524-kilgray-memoq-translator-pro-9-2-5-crack-exclusive-full-review
https://coub.com/stories/3411517-dhoom-3-bollywood-3gp-movie-download-verified
https://coub.com/stories/3411511-fubu-rap-collection-vol-1-better
https://coub.com/stories/3411506-upd-kamasutra-3d-3-film-download-3gp-moviegolkes
https://coub.com/stories/3411504-midi-guitar-2-crack-3-frebota
https://coub.com/stories/3411501-omkara-full-movie-new-free-download-720p
https://coub.com/stories/3411475-ace-ventura-pet-detective-hindi-dubbedl-link
https://coub.com/stories/3411493-bujjigadu-telugu-dvdrip-rajmahal-infiltrados-casados-gangs-tortura-criminal-progamas-work
https://coub.com/stories/3411490-link-ways-to-have-sweet-sex-with-a-childhood-friend-psp-rar-hit
https://coub.com/stories/3411485-gestmag-2011-crack-best
https://coub.com/stories/3411487-sniper-elite-3-mods
https://coub.com/stories/3411484-portable-free-download-inventor-2012-crack-keygen-129311
https://coub.com/stories/3411481-_verified_-ganter-philippe-les-gammes-de-la-guitare-pdf-mp3rar
https://coub.com/stories/3411480-extra-quality-sporbust-content-free-download
https://coub.com/stories/3411479-new-el-diario-de-ana-frank-mobi
https://coub.com/stories/3411478-v-for-vendetta-screenplay-pdf-14
https://coub.com/stories/3411476-free-batman-arkham-city-skidrow-password-rar
ingfay (Monday, 31 January 2022 22:47)
ingfay f4bc01c98b https://coub.com/stories/3511578-billa-telugu-movie-bluray-torrent
https://coub.com/stories/3511579-coldplay-a-rush-of-blood-to-the-head-entire-album-320kbps-mp3-tamscai
https://coub.com/stories/3511580-download-gx-developer-8-7-full-exclusive-crackl
https://coub.com/stories/3511585-armedia-plugin-for-autodesk-3ds-max-crack-downloadl-winnkeil
https://coub.com/stories/3511582-rhinoceros-6-19-free-crack-macos
https://coub.com/stories/3511583-best-rc-plane-3-f-53b-crack-by-razor1911-download
https://coub.com/stories/3511584-link-vampire-the-masquerade-bloodlines-torrent-download
https://coub.com/stories/3511581-vectorworks-12-5-with-key-keygen-upd
https://coub.com/stories/3511586-hot-toontrack-metal-machine-ezx-win-expansion-audiop2p-torrent
https://coub.com/stories/3511588-hq-video-songs-1080p-hindi-movies-new
https://coub.com/stories/3511589-exclusive-age-of-magic-apk-mod-unlock-all
https://coub.com/stories/3511587-hamara-dil-aapke-paas-hai-kannada-movie-mp3-repack-download
https://coub.com/stories/3511590-ponnumani-1993-fix-download-tamil-movie-wwwuyirvanicommcet-mse-rockzmkv
https://coub.com/stories/3511591-best-daily-wisdom-abdur-raheem-kidwai-pdf-download
https://coub.com/stories/3511594-nanak-shah-fakir-full-movie-download-720p-movies-515-chatar
https://coub.com/stories/3511593-a-lolita-full-movie-eng-sub-download-amalang
https://coub.com/stories/3511595-top-tyldesleys-oral-medicine-5th-edition-pdf-free-download
https://coub.com/stories/3511596-new-download-file-iso-game-ps2-ukuran-kecil
https://coub.com/stories/3510220-industrial-microbiology-by-a-h-patel-pdf-download-gilbemel
https://coub.com/stories/3510219-hach-maza-marg-marathi-book-84-churmar
https://coub.com/stories/3510217-exclusive-video-bokep-gadis-india
https://coub.com/stories/3510216-2021-danza-kuduro-video-hd-1080p
https://coub.com/stories/3510215-link-autocom-delphi-2013-3-keygen-v1-download
https://coub.com/stories/3510214-battle-for-middle-earth-2-1-06-trainer-36-reeoves
https://coub.com/stories/3510213-hack-tuneskit-spotify-music-converter-v1-2-3-118-final-serial-hinenata
https://coub.com/stories/3510209-link-free-download-moldflow-insight-2015-crack-keygen
https://coub.com/stories/3510212-bootlust-free-download-exclusive
https://coub.com/stories/3510211-retail-man-2-5-4-90-crack-link
https://coub.com/stories/3510208-wondershare-mobiletrans-licensed-email-and-registration-code
https://coub.com/stories/3510207-exclusive-bigfish-games-trial-reseter-exe
jezfur (Tuesday, 01 February 2022 16:07)
jezfur f4bc01c98b https://coub.com/stories/3502038-download-fix-lloyds-tsb-paying-in-slipl
https://coub.com/stories/3502037-pinnacle-pctv-tvcenter-pro-serial-number-new
https://coub.com/stories/3502032-adobe-after-effects-cc-12-0-0-404-ls20-multilingual-serial-keyl-verified
https://coub.com/stories/3502034-behen-hogi-teri-part-1-full-movie-download-in-hindi-mp4-top
https://coub.com/stories/3502035-top-kitab-rohmatul-ummah-pdf-download
https://coub.com/stories/3502036-teddi-barrett-nympho-nurse-rm-jakkhers
https://coub.com/stories/3502033-crack-covadis-11-rar-verified
https://coub.com/stories/3502031-download-verified-phoenix-firstbios-pro-extract-tools
https://coub.com/stories/3502030-keyner-ramirez-mojica-libros-pdf-downloadl-beneoli
https://coub.com/stories/3502029-wordly-wise-3000-book-7-answers-online-geovis
https://coub.com/stories/3502028-anak-umur-10-tahun-ngentot
https://coub.com/stories/3502027-calendar-girls-movie-with-eng-subtitles-download-janwhyt
https://coub.com/stories/3502026-navicat-premium-12-crack-serial-key-full-free-download-exclusive
https://coub.com/stories/3502025-motu-patlu-comics-pdf-free-free
https://coub.com/stories/3502024-alarm-for-cobra-11-crash-time-reloaded-fitgirl-repack-peltjil
https://coub.com/stories/3502023-native-instruments-fm8-vsti-dxi-rtas-v1-0-3-utorrent-halijal
https://coub.com/stories/3502022-land-rover-microcat-parts-catalog-download-hot-pdf
https://coub.com/stories/3502021-jocul-seductiei-johanna-lindsey-pdf-27
https://coub.com/stories/3502020-sims-4-boob-mod-tanwarw
https://coub.com/stories/3502019-fix-kevin-miranda-consentement-streaming
https://coub.com/stories/3502018-verified-soaldescriptivetextpilihangandabesertakuncijawaban
https://coub.com/stories/3502017-delicious-9-emily-s-honeymoon-cruise-foxy-games-full-crack-extra-quality-hack-torrent
https://coub.com/stories/3502016-hd-online-player-freemake-video-converter-gold-pack-f-exclusive
https://coub.com/stories/3502015-miss-lovely-full-movie-free-download-best
https://coub.com/stories/3502014-players-in-hindi-720p-torrent-download-panctawn
https://coub.com/stories/3502013-project-sam-orchestral-brass-classic-1-2-kontakt-torrent
https://coub.com/stories/3502012-thirukural-with-tamil-explanation-pdf-free-download-__top__
https://coub.com/stories/3502011-hd-online-player-the-chronicles-of-narnia-4-the-silve
https://coub.com/stories/3502010-pd-5500-63-pdf-patched
https://coub.com/stories/3502008-better-nanak-shah-fakir-movie-mp4-download
phytthur (Thursday, 03 February 2022 13:37)
259bd65dd4 . https://coub.com/stories/2467636-the-adventures-of-tintin-720p-kickass https://coub.com/stories/2529592-antares-auto-tune-efx-keygen-free-generator https://coub.com/stories/2472493-repack-easeus-data-recovery-wizard-9-5-crack-keygen https://coub.com/stories/2534279-__full__-download-getting-over-it-mac-free https://coub.com/stories/3672201-clipwrap-2-6-serial-number-cracked https://coub.com/stories/2540232-__link__-httpsystem53-com https://coub.com/stories/2522777-the-office-uk-season-1-torrent-tpb https://coub.com/stories/2533709-free-download-new-headway-academic-skills-level-3-rar-dawnuriq https://coub.com/stories/3674253-verified-honda-spacy-ch125-service-manual https://coub.com/stories/2478059-turn-handwriting-into-a-font-free-pekelno https://coub.com/stories/2519554-gardner-27s-art-through-the-ages-a-concise-western-history-4th-edition-ebook https://coub.com/stories/3663837-compusoft-winner-v9-0a2-multilanguage-iso-absokt https://coub.com/stories/3675569-instructional-strategies-for-pre-emergent-ell-students https://coub.com/stories/2533782-__hot__-unreal-engine-marketplace-bundle-2-feb-2020 https://coub.com/stories/3678735-navigon-7-7-5-build-447-for-wince-5-0-free https://coub.com/stories/2524464-grand-cimbalom-kontakt-orseeleit https://coub.com/stories/2476831-verified-ewp-ewprod-hanging-asphyxia-olivia-simon-now-hiring-rapidsharel https://coub.com/stories/2475095-download-aact-portable-rar-top https://coub.com/stories/2523519-clipart-3d-free-download-portable https://coub.com/stories/2460481-enriching-our-worship-4-pdf-new https://coub.com/stories/2557131-downloaddivortiareikanatassapdf__full__-free https://coub.com/stories/2542003-top-american-civil-war-casualties-statistics https://coub.com/stories/2473155-exclusive-black-s-law-dictionary-tenth-edition-pdf https://coub.com/stories/2525637-wp-mlm-pro-nulled-wordpress-hot https://coub.com/stories/2535307-download-file-studrfd320-rar-528-87-mb-in-free-new-mode-turbobit-net https://coub.com/stories/2525832-amadeus-1984-directors-cut-720p-brrip-x264-yify-subtitles https://coub.com/stories/3671340-top-libros-de-teologia-pdf https://coub.com/stories/2546858-blood-typing-activity-worksheet-answers https://coub.com/stories/2545854-total-war-three-kingdoms-1-0-10 https://coub.com/stories/2537620-dwell-best-homes-in-america-pdf-zanzand
dorpans (Saturday, 05 February 2022 08:23)
dorpans 1ba3a6282b https://wakelet.com/wake/T-cHKBWK0Cb3vMhHrbxB-
https://wakelet.com/wake/sbIyHvH898Fn_yeJ9-eMU
https://wakelet.com/wake/CR5jEIuDfmlU4d3Ii4OVO
https://wakelet.com/wake/ls90Y3W6K3oewhvyZ9EVU
https://wakelet.com/wake/F5Mceoc65UpbqRJTVkXX0
https://wakelet.com/wake/OeKufoPiuzva7HxPkDoYA
https://wakelet.com/wake/nmgUzgr9XIbbd8Sr4APLg
https://wakelet.com/wake/zJFuCdbCQ-fu61gA5OG4Z
https://wakelet.com/wake/FW8W5HUpUfrEU4I9PueRE
https://wakelet.com/wake/pyJezmsHxcbdxC8gwkYow
https://wakelet.com/wake/lDRgIWZ_xBxpWPbAsuMYo
https://wakelet.com/wake/tizkCmp8xw6nPqMPLYT1o
https://wakelet.com/wake/fBgBAVFh7q5s6gYxCp0Ry
https://wakelet.com/wake/Hnd0W1pWCJJdj10mUrMxx
https://wakelet.com/wake/anofv2AqJRAWceJZjiqwu
https://wakelet.com/wake/MkQyzzdgsgsF8VjJU-OXH
https://wakelet.com/wake/nLgW3oZoGH6I0eKq4IDN7
https://wakelet.com/wake/7FoSCyv36xGuAa7EZ5UDg
https://wakelet.com/wake/Z0a7VnSkoaLMoMIMASWOw
https://wakelet.com/wake/-0Rf2xU_N3bKNjrAZI08s
https://wakelet.com/wake/ueymqyNo6LPao0Xb4yoFl
https://wakelet.com/wake/gz5YeZFBzMYXMemi5LHLp
https://wakelet.com/wake/WvadG5bJLs2bnlZ_PiCPz
https://wakelet.com/wake/9VZPwSqPmtiNY4foPvNvH
https://wakelet.com/wake/E9hvceBajreJMkhFRQ5iE
https://wakelet.com/wake/Kc2D8KDJnVbuE7Gj2DtXC
https://wakelet.com/wake/lJmojrAWu6iZeio6V8Y0h
https://wakelet.com/wake/g80e32IZ7yxY0sZpGw6kx
https://wakelet.com/wake/8yO4vEpxZhM8qcfhsi2oy
https://wakelet.com/wake/PJU0fEp7JGb46ZvP1dHtx
http://dynamicmedonline.com/en/smartblog/4_pellentesque-sollicitudin-iaculis-gravida.html
yeldeid (Saturday, 05 February 2022 09:04)
yeldeid 1ba3a6282b https://wakelet.com/wake/C_7VT3ULyKG7ogH1vRfeZ
https://wakelet.com/wake/r-AHjiMiMkHB0kgpidWwU
https://wakelet.com/wake/ORBNvxT2MVk5yoTS-HfYu
https://wakelet.com/wake/aLs7lJCzmlgJxQea8A27O
https://wakelet.com/wake/y1ZtCSCP02Sj0J1_I1fBT
https://wakelet.com/wake/cSwG896Ggat3EbDTkyFFa
https://wakelet.com/wake/pT7EO0CcEA0i2VOFiw9Y4
https://wakelet.com/wake/OdbM1GvlJCV_OxtGZR-qX
https://wakelet.com/wake/e2mqro4UwVZeslxPVlye7
https://wakelet.com/wake/LHTT3XMPf3G-1GjxJ8GBO
https://wakelet.com/wake/4k07tydh-CcFTmglDeN2O
https://wakelet.com/wake/jL7C6subvlnl3oD83S97c
https://wakelet.com/wake/9ghVc6UBsEZ21nSWzc05m
https://wakelet.com/wake/_L5PfcFB71rYCchXBpe00
https://wakelet.com/wake/y_-cXkdN6j8QY3qcbGgcy
https://wakelet.com/wake/eyD63hqZh2n7ay83XnDoN
https://wakelet.com/wake/VXzPhu0rlWdak5zc0xBU1
https://wakelet.com/wake/QFvlpI3t9mCU62Ouasg4z
https://wakelet.com/wake/V5SOYK7ZKUErxDdlqktTV
https://wakelet.com/wake/L9BQGV1R0hHDAG0LCWy4Y
https://wakelet.com/wake/Nq81vx-oc1bwIXqLTGnbn
https://wakelet.com/wake/NiKXtj84FpzecUao4AXFk
https://wakelet.com/wake/teqguSDZLKx08BEkkEzum
https://wakelet.com/wake/5hnro4RGkFn9D6I8j8akV
https://wakelet.com/wake/D--i1b1Lra3eMI_tGXheL
https://wakelet.com/wake/zMRqf09368z5wZJgTuc-0
https://wakelet.com/wake/znS63_Tb71hNEzLDWk1y_
https://wakelet.com/wake/f2h3uOrmiN85-K44F58Fu
https://wakelet.com/wake/fhmqzsDI3Qlk65KihmjgB
https://wakelet.com/wake/qk4nFOE4dlZUojK0C7jpV
https://akusewa.com/product/meja-kotak-ibm/
yeldeid (Saturday, 05 February 2022 09:04)
yeldeid 1ba3a6282b https://wakelet.com/wake/C_7VT3ULyKG7ogH1vRfeZ
https://wakelet.com/wake/r-AHjiMiMkHB0kgpidWwU
https://wakelet.com/wake/ORBNvxT2MVk5yoTS-HfYu
https://wakelet.com/wake/aLs7lJCzmlgJxQea8A27O
https://wakelet.com/wake/y1ZtCSCP02Sj0J1_I1fBT
https://wakelet.com/wake/cSwG896Ggat3EbDTkyFFa
https://wakelet.com/wake/pT7EO0CcEA0i2VOFiw9Y4
https://wakelet.com/wake/OdbM1GvlJCV_OxtGZR-qX
https://wakelet.com/wake/e2mqro4UwVZeslxPVlye7
https://wakelet.com/wake/LHTT3XMPf3G-1GjxJ8GBO
https://wakelet.com/wake/4k07tydh-CcFTmglDeN2O
https://wakelet.com/wake/jL7C6subvlnl3oD83S97c
https://wakelet.com/wake/9ghVc6UBsEZ21nSWzc05m
https://wakelet.com/wake/_L5PfcFB71rYCchXBpe00
https://wakelet.com/wake/y_-cXkdN6j8QY3qcbGgcy
https://wakelet.com/wake/eyD63hqZh2n7ay83XnDoN
https://wakelet.com/wake/VXzPhu0rlWdak5zc0xBU1
https://wakelet.com/wake/QFvlpI3t9mCU62Ouasg4z
https://wakelet.com/wake/V5SOYK7ZKUErxDdlqktTV
https://wakelet.com/wake/L9BQGV1R0hHDAG0LCWy4Y
https://wakelet.com/wake/Nq81vx-oc1bwIXqLTGnbn
https://wakelet.com/wake/NiKXtj84FpzecUao4AXFk
https://wakelet.com/wake/teqguSDZLKx08BEkkEzum
https://wakelet.com/wake/5hnro4RGkFn9D6I8j8akV
https://wakelet.com/wake/D--i1b1Lra3eMI_tGXheL
https://wakelet.com/wake/zMRqf09368z5wZJgTuc-0
https://wakelet.com/wake/znS63_Tb71hNEzLDWk1y_
https://wakelet.com/wake/f2h3uOrmiN85-K44F58Fu
https://wakelet.com/wake/fhmqzsDI3Qlk65KihmjgB
https://wakelet.com/wake/qk4nFOE4dlZUojK0C7jpV
https://akusewa.com/product/meja-kotak-ibm/
yeldeid (Saturday, 05 February 2022 09:05)
yeldeid 1ba3a6282b https://wakelet.com/wake/C_7VT3ULyKG7ogH1vRfeZ
https://wakelet.com/wake/r-AHjiMiMkHB0kgpidWwU
https://wakelet.com/wake/ORBNvxT2MVk5yoTS-HfYu
https://wakelet.com/wake/aLs7lJCzmlgJxQea8A27O
https://wakelet.com/wake/y1ZtCSCP02Sj0J1_I1fBT
https://wakelet.com/wake/cSwG896Ggat3EbDTkyFFa
https://wakelet.com/wake/pT7EO0CcEA0i2VOFiw9Y4
https://wakelet.com/wake/OdbM1GvlJCV_OxtGZR-qX
https://wakelet.com/wake/e2mqro4UwVZeslxPVlye7
https://wakelet.com/wake/LHTT3XMPf3G-1GjxJ8GBO
https://wakelet.com/wake/4k07tydh-CcFTmglDeN2O
https://wakelet.com/wake/jL7C6subvlnl3oD83S97c
https://wakelet.com/wake/9ghVc6UBsEZ21nSWzc05m
https://wakelet.com/wake/_L5PfcFB71rYCchXBpe00
https://wakelet.com/wake/y_-cXkdN6j8QY3qcbGgcy
https://wakelet.com/wake/eyD63hqZh2n7ay83XnDoN
https://wakelet.com/wake/VXzPhu0rlWdak5zc0xBU1
https://wakelet.com/wake/QFvlpI3t9mCU62Ouasg4z
https://wakelet.com/wake/V5SOYK7ZKUErxDdlqktTV
https://wakelet.com/wake/L9BQGV1R0hHDAG0LCWy4Y
https://wakelet.com/wake/Nq81vx-oc1bwIXqLTGnbn
https://wakelet.com/wake/NiKXtj84FpzecUao4AXFk
https://wakelet.com/wake/teqguSDZLKx08BEkkEzum
https://wakelet.com/wake/5hnro4RGkFn9D6I8j8akV
https://wakelet.com/wake/D--i1b1Lra3eMI_tGXheL
https://wakelet.com/wake/zMRqf09368z5wZJgTuc-0
https://wakelet.com/wake/znS63_Tb71hNEzLDWk1y_
https://wakelet.com/wake/f2h3uOrmiN85-K44F58Fu
https://wakelet.com/wake/fhmqzsDI3Qlk65KihmjgB
https://wakelet.com/wake/qk4nFOE4dlZUojK0C7jpV
https://akusewa.com/product/meja-kotak-ibm/
yeldeid (Saturday, 05 February 2022 09:05)
yeldeid 1ba3a6282b https://wakelet.com/wake/C_7VT3ULyKG7ogH1vRfeZ
https://wakelet.com/wake/r-AHjiMiMkHB0kgpidWwU
https://wakelet.com/wake/ORBNvxT2MVk5yoTS-HfYu
https://wakelet.com/wake/aLs7lJCzmlgJxQea8A27O
https://wakelet.com/wake/y1ZtCSCP02Sj0J1_I1fBT
https://wakelet.com/wake/cSwG896Ggat3EbDTkyFFa
https://wakelet.com/wake/pT7EO0CcEA0i2VOFiw9Y4
https://wakelet.com/wake/OdbM1GvlJCV_OxtGZR-qX
https://wakelet.com/wake/e2mqro4UwVZeslxPVlye7
https://wakelet.com/wake/LHTT3XMPf3G-1GjxJ8GBO
https://wakelet.com/wake/4k07tydh-CcFTmglDeN2O
https://wakelet.com/wake/jL7C6subvlnl3oD83S97c
https://wakelet.com/wake/9ghVc6UBsEZ21nSWzc05m
https://wakelet.com/wake/_L5PfcFB71rYCchXBpe00
https://wakelet.com/wake/y_-cXkdN6j8QY3qcbGgcy
https://wakelet.com/wake/eyD63hqZh2n7ay83XnDoN
https://wakelet.com/wake/VXzPhu0rlWdak5zc0xBU1
https://wakelet.com/wake/QFvlpI3t9mCU62Ouasg4z
https://wakelet.com/wake/V5SOYK7ZKUErxDdlqktTV
https://wakelet.com/wake/L9BQGV1R0hHDAG0LCWy4Y
https://wakelet.com/wake/Nq81vx-oc1bwIXqLTGnbn
https://wakelet.com/wake/NiKXtj84FpzecUao4AXFk
https://wakelet.com/wake/teqguSDZLKx08BEkkEzum
https://wakelet.com/wake/5hnro4RGkFn9D6I8j8akV
https://wakelet.com/wake/D--i1b1Lra3eMI_tGXheL
https://wakelet.com/wake/zMRqf09368z5wZJgTuc-0
https://wakelet.com/wake/znS63_Tb71hNEzLDWk1y_
https://wakelet.com/wake/f2h3uOrmiN85-K44F58Fu
https://wakelet.com/wake/fhmqzsDI3Qlk65KihmjgB
https://wakelet.com/wake/qk4nFOE4dlZUojK0C7jpV
https://akusewa.com/product/meja-kotak-ibm/
pearschm (Saturday, 05 February 2022 09:42)
pearschm 1ba3a6282b https://wakelet.com/wake/mpbVywLQvpzl0IGFNwarm
https://wakelet.com/wake/nVxhd8l9J1ZETP8mYHTYx
https://wakelet.com/wake/PU_Smvm0TVt1p-AOMSsig
https://wakelet.com/wake/XzoompS1gXcWbKHeHEkuB
https://wakelet.com/wake/AuX669hd2z9DAxfk3WWOR
https://wakelet.com/wake/Bn9GiSK7iyLlEh3aSK7Kg
https://wakelet.com/wake/D9Yo3-COl_myibKFzdKDI
https://wakelet.com/wake/FFMGcAed4BEzaqGzRVAh-
https://wakelet.com/wake/_1NLyuaa8mHPkE1QY_119
https://wakelet.com/wake/XLaegxJZaKeJgxKpINX80
https://wakelet.com/wake/h6zSaE7P_jC6nqEP7R58k
https://wakelet.com/wake/hh-CPihfn4kx1DajGkAtA
https://wakelet.com/wake/oxboGkyhshnY53Mwd49qN
https://wakelet.com/wake/MZbrLm79RQIBP5GZ2DEtj
https://wakelet.com/wake/043rEJbze9RcB1tUAJ8px
https://wakelet.com/wake/CCcmhTNyTxJS7rtmD8ggW
https://wakelet.com/wake/CUdFJ5BTRnuT_ZSUXyPAW
https://wakelet.com/wake/8pQ5lRU2Kh6Do9wicr6lx
https://wakelet.com/wake/q91x8718WDpkG9KsecDjz
https://wakelet.com/wake/S4Lxmrhpvgo0vyOTCt4Pj
https://wakelet.com/wake/eIcDOQGL7pwK0sO2Fif2M
https://wakelet.com/wake/2YhNtPx-EicRK8h0cM6G_
https://wakelet.com/wake/SU94eyZ5wGj0Z0VbAhYoo
https://wakelet.com/wake/DCG0PJM6-EL3oAUXYebPX
https://wakelet.com/wake/T5xsfQeFVInFJS2JYPzz4
https://wakelet.com/wake/LrFxs7qcD3h6RuemA7aVz
https://wakelet.com/wake/7yFr_T9MhbkAO-NoPgdQ2
https://wakelet.com/wake/g_pmP3KYRg7n_jsAKBOPV
https://wakelet.com/wake/fOIB7b0nDUqYFpRELAw6n
https://wakelet.com/wake/QSjF7rEqTxWmAVTrEJTTV
http://thecarltoncenter.com/virtual-offices-the-5-benefits-of-having-one/
giamon (Sunday, 06 February 2022 02:00)
giamon 1ba3a6282b https://wakelet.com/wake/3BgS1YyD-ZVB5BQSBWUc3
https://wakelet.com/wake/QWeOzw7fQtXSEvC2EPsi5
https://wakelet.com/wake/MrFysyfjV08fpxHalG2s5
https://wakelet.com/wake/LH_Uva15w9I_ynSi0QDcq
https://wakelet.com/wake/D2cvuNJG19V9MlQtoVXQw
https://wakelet.com/wake/0Lr2eEHMrx2Vqz75d_3rZ
https://wakelet.com/wake/VBsQsuGypMoTf_WYSHV3Q
https://wakelet.com/wake/Oth27aBobsUvlo9lqDUna
https://wakelet.com/wake/ddFlxyAlv5i1ZdL4pDfVf
https://wakelet.com/wake/dJ4xug3VNoMVhzQihmDhy
https://wakelet.com/wake/Gbesh2KmNYQfp8W5zNQjC
https://wakelet.com/wake/LopDgXGXMOqY3PteCLLjK
https://wakelet.com/wake/Mi20fE7oSeYHFOXfZbYhX
https://wakelet.com/wake/a5UbQQRzBHZxHPkjK2Jb6
https://wakelet.com/wake/_guN9noPH0YREoRW5B015
https://wakelet.com/wake/FRhcpdsA21g_4mopp9zF0
https://wakelet.com/wake/yEWndGGBFzOiCu8VAIpeZ
https://wakelet.com/wake/IiA7GwHh_IEm_qQPfrPJ9
https://wakelet.com/wake/qolER1nUo-OTNRR4zDiFz
https://wakelet.com/wake/0EaoHQVRa7-RhXaSkiw9B
https://wakelet.com/wake/2UDsjRanFxkweXxnLZ23N
https://wakelet.com/wake/T1Uc3TKV7Xms_0CgQ6F9Y
https://wakelet.com/wake/qvlNSEcHfq3-idthi187z
https://wakelet.com/wake/e3syRJRiYjh-cKwZAewoH
https://wakelet.com/wake/KXRAtz-6NBXC77LgJHPGF
https://wakelet.com/wake/YPOzxZDTIloA0GOwfLgVf
https://wakelet.com/wake/_xWOkKOz69yqOz-14_anF
https://wakelet.com/wake/tmm7umBb9WWtjv0rijJP-
https://wakelet.com/wake/i-K0xio_9KdGoDqqLMIgn
https://wakelet.com/wake/C9MJsZnzwAiv8Fg72hd4L
https://soc.cungcap.net/rantihanbea
watfene (Sunday, 06 February 2022 07:10)
watfene cceab18d79 https://coub.com/stories/3490464-cv-maker-resume-builder-pdf-template-format-editor-v9-1-16-pro-b3000246-pro-crack-best-ed-lates
https://coub.com/stories/3490463-ben-10-skin-pack-for-windows-7-free-download-_top_
https://coub.com/stories/3490461-canon-ir1022-scanner-driver-download-for-windows-7-17-lorgil
https://coub.com/stories/3490460-blaupunkt-travelpilot-e-ex-v9-cd-rns-300-torrent-gorinc
https://coub.com/stories/3490462-adobe-photoshop-activation-key-creihal
https://coub.com/stories/3490459-gandhi-to-hitler-marathi-movie-mp3-songs-download-link
https://coub.com/stories/3490458-vitettateoriadeisegnalipdf21
https://coub.com/stories/3490457-_best_-5-34-crack-para-maxikiosco-epub
https://coub.com/stories/3490456-windows-7-diamond-gold-ultimate-final-x86-x64-new-download-now
https://coub.com/stories/3490455-krrish-2006-tamil-dubbed-movie-dvdrip-1cd-700mb-download-holiwale
https://coub.com/stories/3490454-golmaal31fullmovieinhindi720pdownload-vyrmac
https://coub.com/stories/3490453-snsd-gee-dance-version-1080i-vs-1080p-hot
https://coub.com/stories/3490452-magixmovieeditpro15plus-link-downloadversionserialnumber
https://coub.com/stories/3490449-rundll32-exe-windows-7-64-bits-download-darmahl
https://coub.com/stories/3490451-new-download-simba-cartoon-sahara-one-hindi-episodes
https://coub.com/stories/3490450-patch-commentaire-arabe-pour-pes-2013-pc-startimes-install
https://coub.com/stories/3490447-celine-dion-falling-into-you-full-album-zip-kengre
https://coub.com/stories/3490448-digital-anarchy-backdrop-designer-15-crack-repack
https://coub.com/stories/3490446-diabloiiireaperofsoulspc2013fullgame2013iso-kalstep
https://coub.com/stories/3490445-top-jungle-adventures-apk-mod-unlock-all
https://coub.com/stories/3490444-full-ford-vcm-ids-v86-crack
https://coub.com/stories/3490443-exclusive-crack-adobe-acrobat-xi-pro-working-100
https://coub.com/stories/3490442-xilinx-ise-14-5-crack-only-torrent-free
https://coub.com/stories/3490440-upd-hd-online-player-video-porno-anak-ngentot-ibu-kandu
https://coub.com/stories/3490441-tamilrockers-maan-karate-movie-free-upd-download
https://coub.com/stories/3490439-portable-fs9-fsx-p3d-x-plane-navigraph-airac-cycle-1803-game-hack-password
https://coub.com/stories/3490438-stufa-pirolisi-progetto-pdf-flowmar
https://coub.com/stories/3490436-64mb-video-card-with-directx-9-compatible-drivers-download-walsail
https://coub.com/stories/3490437-need-for-speed-shift-2-no-cd-crack-download-eletal
https://coub.com/stories/3490435-link-baadshaho-1080p-hindi-movies
http://allamericanleakdetection.net/guestbook/
watfene (Sunday, 06 February 2022 07:11)
watfene cceab18d79 https://coub.com/stories/3490464-cv-maker-resume-builder-pdf-template-format-editor-v9-1-16-pro-b3000246-pro-crack-best-ed-lates
https://coub.com/stories/3490463-ben-10-skin-pack-for-windows-7-free-download-_top_
https://coub.com/stories/3490461-canon-ir1022-scanner-driver-download-for-windows-7-17-lorgil
https://coub.com/stories/3490460-blaupunkt-travelpilot-e-ex-v9-cd-rns-300-torrent-gorinc
https://coub.com/stories/3490462-adobe-photoshop-activation-key-creihal
https://coub.com/stories/3490459-gandhi-to-hitler-marathi-movie-mp3-songs-download-link
https://coub.com/stories/3490458-vitettateoriadeisegnalipdf21
https://coub.com/stories/3490457-_best_-5-34-crack-para-maxikiosco-epub
https://coub.com/stories/3490456-windows-7-diamond-gold-ultimate-final-x86-x64-new-download-now
https://coub.com/stories/3490455-krrish-2006-tamil-dubbed-movie-dvdrip-1cd-700mb-download-holiwale
https://coub.com/stories/3490454-golmaal31fullmovieinhindi720pdownload-vyrmac
https://coub.com/stories/3490453-snsd-gee-dance-version-1080i-vs-1080p-hot
https://coub.com/stories/3490452-magixmovieeditpro15plus-link-downloadversionserialnumber
https://coub.com/stories/3490449-rundll32-exe-windows-7-64-bits-download-darmahl
https://coub.com/stories/3490451-new-download-simba-cartoon-sahara-one-hindi-episodes
https://coub.com/stories/3490450-patch-commentaire-arabe-pour-pes-2013-pc-startimes-install
https://coub.com/stories/3490447-celine-dion-falling-into-you-full-album-zip-kengre
https://coub.com/stories/3490448-digital-anarchy-backdrop-designer-15-crack-repack
https://coub.com/stories/3490446-diabloiiireaperofsoulspc2013fullgame2013iso-kalstep
https://coub.com/stories/3490445-top-jungle-adventures-apk-mod-unlock-all
https://coub.com/stories/3490444-full-ford-vcm-ids-v86-crack
https://coub.com/stories/3490443-exclusive-crack-adobe-acrobat-xi-pro-working-100
https://coub.com/stories/3490442-xilinx-ise-14-5-crack-only-torrent-free
https://coub.com/stories/3490440-upd-hd-online-player-video-porno-anak-ngentot-ibu-kandu
https://coub.com/stories/3490441-tamilrockers-maan-karate-movie-free-upd-download
https://coub.com/stories/3490439-portable-fs9-fsx-p3d-x-plane-navigraph-airac-cycle-1803-game-hack-password
https://coub.com/stories/3490438-stufa-pirolisi-progetto-pdf-flowmar
https://coub.com/stories/3490436-64mb-video-card-with-directx-9-compatible-drivers-download-walsail
https://coub.com/stories/3490437-need-for-speed-shift-2-no-cd-crack-download-eletal
https://coub.com/stories/3490435-link-baadshaho-1080p-hindi-movies
http://allamericanleakdetection.net/guestbook/
watfene (Sunday, 06 February 2022 07:11)
watfene cceab18d79 https://coub.com/stories/3490464-cv-maker-resume-builder-pdf-template-format-editor-v9-1-16-pro-b3000246-pro-crack-best-ed-lates
https://coub.com/stories/3490463-ben-10-skin-pack-for-windows-7-free-download-_top_
https://coub.com/stories/3490461-canon-ir1022-scanner-driver-download-for-windows-7-17-lorgil
https://coub.com/stories/3490460-blaupunkt-travelpilot-e-ex-v9-cd-rns-300-torrent-gorinc
https://coub.com/stories/3490462-adobe-photoshop-activation-key-creihal
https://coub.com/stories/3490459-gandhi-to-hitler-marathi-movie-mp3-songs-download-link
https://coub.com/stories/3490458-vitettateoriadeisegnalipdf21
https://coub.com/stories/3490457-_best_-5-34-crack-para-maxikiosco-epub
https://coub.com/stories/3490456-windows-7-diamond-gold-ultimate-final-x86-x64-new-download-now
https://coub.com/stories/3490455-krrish-2006-tamil-dubbed-movie-dvdrip-1cd-700mb-download-holiwale
https://coub.com/stories/3490454-golmaal31fullmovieinhindi720pdownload-vyrmac
https://coub.com/stories/3490453-snsd-gee-dance-version-1080i-vs-1080p-hot
https://coub.com/stories/3490452-magixmovieeditpro15plus-link-downloadversionserialnumber
https://coub.com/stories/3490449-rundll32-exe-windows-7-64-bits-download-darmahl
https://coub.com/stories/3490451-new-download-simba-cartoon-sahara-one-hindi-episodes
https://coub.com/stories/3490450-patch-commentaire-arabe-pour-pes-2013-pc-startimes-install
https://coub.com/stories/3490447-celine-dion-falling-into-you-full-album-zip-kengre
https://coub.com/stories/3490448-digital-anarchy-backdrop-designer-15-crack-repack
https://coub.com/stories/3490446-diabloiiireaperofsoulspc2013fullgame2013iso-kalstep
https://coub.com/stories/3490445-top-jungle-adventures-apk-mod-unlock-all
https://coub.com/stories/3490444-full-ford-vcm-ids-v86-crack
https://coub.com/stories/3490443-exclusive-crack-adobe-acrobat-xi-pro-working-100
https://coub.com/stories/3490442-xilinx-ise-14-5-crack-only-torrent-free
https://coub.com/stories/3490440-upd-hd-online-player-video-porno-anak-ngentot-ibu-kandu
https://coub.com/stories/3490441-tamilrockers-maan-karate-movie-free-upd-download
https://coub.com/stories/3490439-portable-fs9-fsx-p3d-x-plane-navigraph-airac-cycle-1803-game-hack-password
https://coub.com/stories/3490438-stufa-pirolisi-progetto-pdf-flowmar
https://coub.com/stories/3490436-64mb-video-card-with-directx-9-compatible-drivers-download-walsail
https://coub.com/stories/3490437-need-for-speed-shift-2-no-cd-crack-download-eletal
https://coub.com/stories/3490435-link-baadshaho-1080p-hindi-movies
http://allamericanleakdetection.net/guestbook/
reenlaug (Sunday, 06 February 2022 08:18)
reenlaug cceab18d79 https://coub.com/stories/3391342-altova-xmlspy-crack-keygen-serial-yoshrayb
https://coub.com/stories/3391341-teenage-mutant-ninja-turtles-theme-song-download-mp3-free-link
https://coub.com/stories/3391340-joe-budden-padded-room-full-album-zipl-_best_
https://coub.com/stories/3391339-photoshop-cs6-on-mac-install-with-crack-macosx-repack
https://coub.com/stories/3391338-afoxgeforceg210driver-goddea
https://coub.com/stories/3391337-a-melody-in-the-haunted-2-dvdrip-download-movie-kathar
https://coub.com/stories/3391336-badrinath-ki-dulhania-movie-2015-download-better-in-hindi
https://coub.com/stories/3391335-work-baahubali-2-the-conclusion-movie-download-full-hd-torrent
https://coub.com/stories/3391334-pictures-of-vaginas-from-ugandan-ladies
https://coub.com/stories/3391333-mehmet-omurtag-dinamik-pdf-12
https://coub.com/stories/3391332-adobe-acrobat-pro-dc-2015-v-12-acrobat-dc-web-wwmui-exe-portable
https://coub.com/stories/3391330-iap-textbook-of-pediatrics-5th-edition-pdf-free-download-barjan
https://coub.com/stories/3391331-pushbullet-pro-sms-on-pc-v18-2-31-crack-bested-latest
https://coub.com/stories/3391329-digimonmasterofflinepcgamedownload-leroleil
https://coub.com/stories/3391328-hd-video-songs-1080p-blu-hate-story-3-movies-link
https://coub.com/stories/3391327-extra-quality-mardaani-movie-dual-audio-720p
https://coub.com/stories/3391326-microsoft-research-autocollage-2008-10-serial-keygen-upd-torrent
https://coub.com/stories/3391325-jewelcad-5-1-software-free-download-kalheart
https://coub.com/stories/3391324-w300v100a-zrd-eg-firmware-full
https://coub.com/stories/3391322-presence-of-oxalate-ion-in-guava-fruit-pdf-freel-__hot__
https://coub.com/stories/3391323-tamil-actress-jyothika-blue-film-video
https://coub.com/stories/3391321-top-flash-loader-7-4-7-ssg-v0-1-lite-rar
https://coub.com/stories/3391320-dcs-a-10c-warthog-1-2-4-crack-naniwel
https://coub.com/stories/3391319-chanakya-niti-book-in-bengali-pdf-free-downloadgolkes-nichari
https://coub.com/stories/3391317-assassins-creed-ii-updated-repack-mr-dj-money-hack
https://coub.com/stories/3391318-novel-terjemahan-bahasa-indonesia-karya-johanna-lindsey-added-by-users
https://coub.com/stories/3391316-dum-laga-ke-haisha-2015-movie-download-kickass-hot
https://coub.com/stories/3391314-solidworks-2010-2013-activator-by-team-ssq-windows-8-tanmacm
https://coub.com/stories/3391315-official-upgrade-firmware-alcatel-onetouch-hero-2-8030b-8030y
https://coub.com/stories/3391313-namak-download-top-720p-in-hindi
https://xiangyue.homemom.ca/en/forum/601?page=245#comment-107949
reenlaug (Sunday, 06 February 2022 08:18)
reenlaug cceab18d79 https://coub.com/stories/3391342-altova-xmlspy-crack-keygen-serial-yoshrayb
https://coub.com/stories/3391341-teenage-mutant-ninja-turtles-theme-song-download-mp3-free-link
https://coub.com/stories/3391340-joe-budden-padded-room-full-album-zipl-_best_
https://coub.com/stories/3391339-photoshop-cs6-on-mac-install-with-crack-macosx-repack
https://coub.com/stories/3391338-afoxgeforceg210driver-goddea
https://coub.com/stories/3391337-a-melody-in-the-haunted-2-dvdrip-download-movie-kathar
https://coub.com/stories/3391336-badrinath-ki-dulhania-movie-2015-download-better-in-hindi
https://coub.com/stories/3391335-work-baahubali-2-the-conclusion-movie-download-full-hd-torrent
https://coub.com/stories/3391334-pictures-of-vaginas-from-ugandan-ladies
https://coub.com/stories/3391333-mehmet-omurtag-dinamik-pdf-12
https://coub.com/stories/3391332-adobe-acrobat-pro-dc-2015-v-12-acrobat-dc-web-wwmui-exe-portable
https://coub.com/stories/3391330-iap-textbook-of-pediatrics-5th-edition-pdf-free-download-barjan
https://coub.com/stories/3391331-pushbullet-pro-sms-on-pc-v18-2-31-crack-bested-latest
https://coub.com/stories/3391329-digimonmasterofflinepcgamedownload-leroleil
https://coub.com/stories/3391328-hd-video-songs-1080p-blu-hate-story-3-movies-link
https://coub.com/stories/3391327-extra-quality-mardaani-movie-dual-audio-720p
https://coub.com/stories/3391326-microsoft-research-autocollage-2008-10-serial-keygen-upd-torrent
https://coub.com/stories/3391325-jewelcad-5-1-software-free-download-kalheart
https://coub.com/stories/3391324-w300v100a-zrd-eg-firmware-full
https://coub.com/stories/3391322-presence-of-oxalate-ion-in-guava-fruit-pdf-freel-__hot__
https://coub.com/stories/3391323-tamil-actress-jyothika-blue-film-video
https://coub.com/stories/3391321-top-flash-loader-7-4-7-ssg-v0-1-lite-rar
https://coub.com/stories/3391320-dcs-a-10c-warthog-1-2-4-crack-naniwel
https://coub.com/stories/3391319-chanakya-niti-book-in-bengali-pdf-free-downloadgolkes-nichari
https://coub.com/stories/3391317-assassins-creed-ii-updated-repack-mr-dj-money-hack
https://coub.com/stories/3391318-novel-terjemahan-bahasa-indonesia-karya-johanna-lindsey-added-by-users
https://coub.com/stories/3391316-dum-laga-ke-haisha-2015-movie-download-kickass-hot
https://coub.com/stories/3391314-solidworks-2010-2013-activator-by-team-ssq-windows-8-tanmacm
https://coub.com/stories/3391315-official-upgrade-firmware-alcatel-onetouch-hero-2-8030b-8030y
https://coub.com/stories/3391313-namak-download-top-720p-in-hindi
https://xiangyue.homemom.ca/en/forum/601?page=245#comment-107949
reenlaug (Sunday, 06 February 2022 08:19)
reenlaug cceab18d79 https://coub.com/stories/3391342-altova-xmlspy-crack-keygen-serial-yoshrayb
https://coub.com/stories/3391341-teenage-mutant-ninja-turtles-theme-song-download-mp3-free-link
https://coub.com/stories/3391340-joe-budden-padded-room-full-album-zipl-_best_
https://coub.com/stories/3391339-photoshop-cs6-on-mac-install-with-crack-macosx-repack
https://coub.com/stories/3391338-afoxgeforceg210driver-goddea
https://coub.com/stories/3391337-a-melody-in-the-haunted-2-dvdrip-download-movie-kathar
https://coub.com/stories/3391336-badrinath-ki-dulhania-movie-2015-download-better-in-hindi
https://coub.com/stories/3391335-work-baahubali-2-the-conclusion-movie-download-full-hd-torrent
https://coub.com/stories/3391334-pictures-of-vaginas-from-ugandan-ladies
https://coub.com/stories/3391333-mehmet-omurtag-dinamik-pdf-12
https://coub.com/stories/3391332-adobe-acrobat-pro-dc-2015-v-12-acrobat-dc-web-wwmui-exe-portable
https://coub.com/stories/3391330-iap-textbook-of-pediatrics-5th-edition-pdf-free-download-barjan
https://coub.com/stories/3391331-pushbullet-pro-sms-on-pc-v18-2-31-crack-bested-latest
https://coub.com/stories/3391329-digimonmasterofflinepcgamedownload-leroleil
https://coub.com/stories/3391328-hd-video-songs-1080p-blu-hate-story-3-movies-link
https://coub.com/stories/3391327-extra-quality-mardaani-movie-dual-audio-720p
https://coub.com/stories/3391326-microsoft-research-autocollage-2008-10-serial-keygen-upd-torrent
https://coub.com/stories/3391325-jewelcad-5-1-software-free-download-kalheart
https://coub.com/stories/3391324-w300v100a-zrd-eg-firmware-full
https://coub.com/stories/3391322-presence-of-oxalate-ion-in-guava-fruit-pdf-freel-__hot__
https://coub.com/stories/3391323-tamil-actress-jyothika-blue-film-video
https://coub.com/stories/3391321-top-flash-loader-7-4-7-ssg-v0-1-lite-rar
https://coub.com/stories/3391320-dcs-a-10c-warthog-1-2-4-crack-naniwel
https://coub.com/stories/3391319-chanakya-niti-book-in-bengali-pdf-free-downloadgolkes-nichari
https://coub.com/stories/3391317-assassins-creed-ii-updated-repack-mr-dj-money-hack
https://coub.com/stories/3391318-novel-terjemahan-bahasa-indonesia-karya-johanna-lindsey-added-by-users
https://coub.com/stories/3391316-dum-laga-ke-haisha-2015-movie-download-kickass-hot
https://coub.com/stories/3391314-solidworks-2010-2013-activator-by-team-ssq-windows-8-tanmacm
https://coub.com/stories/3391315-official-upgrade-firmware-alcatel-onetouch-hero-2-8030b-8030y
https://coub.com/stories/3391313-namak-download-top-720p-in-hindi
https://xiangyue.homemom.ca/en/forum/601?page=245#comment-107949
zanald (Sunday, 06 February 2022 09:19)
zanald cceab18d79 https://coub.com/stories/3287793-audioease-altiverb-6-for-windows-portable-download
https://coub.com/stories/3287792-morgan-heritage-another-rockaz-moment-rar-better
https://coub.com/stories/3287791-hd-online-player-cevio-creative-studio-crack-22-naislava
https://coub.com/stories/3287790-link-vip-2-lalkar-movie-with-eng-subtitles-download
https://coub.com/stories/3287789-battlefield-3-game-files-part35-rar-18-398l-new
https://coub.com/stories/3287788-the-hunter-2012-wallhack-nirerugg
https://coub.com/stories/3287787-phoenix-crisis-disk-usb-top-download
https://coub.com/stories/3287786-hetman-partition-recovery-2-6-portable-keygen-crackingpatc-free-download-fryigna
https://coub.com/stories/3287785-error-missing-ilok-authorization-for-pro-tools-10-crack-install-ed
https://coub.com/stories/3287783-313a-exam-direct-download-extra-quality
https://coub.com/stories/3287770-full-ls-land-issue-06-little-pirates-top
https://coub.com/stories/3287782-windows-10-altum-pro-axeswy-tomecar-teamos-free-download-chefre
https://coub.com/stories/3287780-zenne-filmi-izle-720p-mkv-wylyarr
https://coub.com/stories/3287779-estrarre-dati-da-pagine-gialle-gratis-verified
https://coub.com/stories/3287778-st-thumbnails-explorer-15-beta-5-crack-harlburn
https://coub.com/stories/3287774-cyberlink-media-suite-10-ultra-keygen-crack-free
https://coub.com/stories/3287773-better-pacific-rim-uprising-english-the-movie-english-sub-1080p-hd
https://coub.com/stories/3287772-jumanji-welcome-to-the-jungle-english-hindi-dubbed-720p
https://coub.com/stories/3287769-namaz-e-nabvi-dr-shafiq-ur-rehmann-pdf-download-hot
https://coub.com/stories/3287768-amma-magana-sex-stories-kannada-20
https://coub.com/stories/3287764-a-x-l-2018-720p-nf-web-dl-dd5-1-h264-cmrg-ethd-download-new-pc
https://coub.com/stories/3287762-jannat-2-hindi-movie-download-laykail
https://coub.com/stories/3287761-revit-architecture-2016-full-version-download-ogyfra
https://coub.com/stories/3287760-work-ism-310-marathi-typing-softwarerar
https://coub.com/stories/3287759-ogden-nash-s-zoo-mobi-exclusive-download-book
https://coub.com/stories/3287758-javidic-2010-final-better-full-crack-idm
https://coub.com/stories/3287757-autocom-delphi-2013-2-keygen-verified-39
https://coub.com/stories/3287756-drivers-numark-dj-io-windows-8-zip-top
https://coub.com/stories/3287754-lma-manager-2002-psx-iso-_best_
https://coub.com/stories/3287753-verified-dog-training-books-in-malayalam
http://tachihara-ayumi-info.sblo.jp/article/184521253.html
quynwero (Sunday, 06 February 2022 10:17)
quynwero cceab18d79 https://coub.com/stories/3505633-jasoosi-digest-may-2018-free-download-hot
https://coub.com/stories/3505632-commando-hindi-movie-2013-torrent-download-mkv-file-cracked
https://coub.com/stories/3505631-command-and-conquer-red-alert-2-full-game-apk-_top_
https://coub.com/stories/3505630-pdf2id-professional-v3-5-download-full-hot
https://coub.com/stories/3505629-7ci-sinif-fizika-test-cavablari-rapidshare-nimawaly
https://coub.com/stories/3505628-new-sinister-2012-brrip-720p-greek-subs-for-movies
https://coub.com/stories/3505627-shreya-saran-ishtam-telugu-movie-free-full-download
https://coub.com/stories/3505623-poor-sakura-vol-4-edihar
https://coub.com/stories/3505626-install-pather-panchali-movie-in-hindi-free-downloads
https://coub.com/stories/3505625-new-serial-number-for-pinnacle-tv-center-pro-70
https://coub.com/stories/3505624-new-warcraft-iii-reign-of-chaos-the-frozen-throne-1-27b-cheat-engine
https://coub.com/stories/3505622-starsector-activation-code-generator-work
https://coub.com/stories/3505621-strength-of-materials-by-bc-punmia-pdf-elissim
https://coub.com/stories/3505620-download-hd-movie-black-sheep-in-hindi-upd
https://coub.com/stories/3505619-elf-bowling-hawaiian-vacation-free-download-crack-bevlloy
https://coub.com/stories/3505618-residentevil4isopspgame-top-downloadtorrent
https://coub.com/stories/3505616-thebigbangtheoryseason2torrentdownloadkickass-maeemi
https://coub.com/stories/3505615-exclusive-tamil-movie-tron-legacy
https://coub.com/stories/3505614-1-nenokkadine-movie-download-blu-ray-rip-moviesinstmank-__full__
https://coub.com/stories/3505613-exclusive-biologia-celular-y-molecular-de-robertis-15-edicion-pdf-free
https://coub.com/stories/3505611-download-facebook-ultimate-hacking-software-351-hot
https://coub.com/stories/3505610-new-sea-men-sex-videos-free
https://coub.com/stories/3505609-sobotta-edisi-23-pdf-download-reanhaiz
https://coub.com/stories/3505608-better-sarkarmoviewithenglishsubtitlefreedownload
https://coub.com/stories/3505607-best-t-l-charger-hacker-mot-de-passe-facebook-gratuit-2013
https://coub.com/stories/3505606-exclusive-audio-hijack-license-key-crack
https://coub.com/stories/3505605-dil-kabaddi-720p-movie-download-kickass-hot
https://coub.com/stories/3505604-jack-the-giant-slayer-patched-full-movie-direct-download
https://coub.com/stories/3505603-99nepalifontsdownload-install
https://coub.com/stories/3505602-zvuk-toki-voki-motorola-policija-exclusive
https://bajopalabra.com.mx/muere-don-diego-el-papa-de-maradona
quarnin (Sunday, 06 February 2022 11:16)
quarnin cceab18d79 https://coub.com/stories/3412786-download-ps3-emulator-v1-9-6-with-bios-and-plugin-torrent-download-hitl-top
https://coub.com/stories/3412784-download-4ch-usb-dvr-driver-windows-7-64-bit-5-kevmar
https://coub.com/stories/3412783-iserson-getting-into-a-residency-pdf-verified
https://coub.com/stories/3412782-link-subtitle-indonesia-human-vs-zombies
https://coub.com/stories/3412781-link-delcam-crispin-engineer-pro-2012-r1-sp4-ssq
https://coub.com/stories/3412778-walkman-chanakya-901-hindi-fonts-brikama
https://coub.com/stories/3412779-ladies-vs-ricky-bahl-download-better-1080p-movie
https://coub.com/stories/3412780-link-court-movie-free-download-in-hindi-in-mp4
https://coub.com/stories/3412777-discografia-litfiba-19822012-top
https://coub.com/stories/3412776-abcd-__link__-full-movie-online-in-hindi-hd
https://coub.com/stories/3412774-2011-savarkhed-ek-gaon-full-marathi-movie-link
https://coub.com/stories/3412769-cyberflix-vip-4-1-4-working-firestick-mod-jarrgro
https://coub.com/stories/3412766-__top__-all-in-one-toolbox-cleaner-tools-pro-v5-3-7-premium-unlocked
https://coub.com/stories/3412765-top-dragon-ball-z-battle-of-gods-english-subtitles-download-srt-free-28
https://coub.com/stories/3412767-updated-max-for-live-essentials-pack-download
https://coub.com/stories/3412762-install-mutools-mulab-ul-v4-5-1-r2r-rar
https://coub.com/stories/3412761-pes-6-kits-map-manager-helgarm
https://coub.com/stories/3412760-advanced-apktool-download-for-56-link
https://coub.com/stories/3412759-aaru-tamil-movie-download-extra-quality-dvdrip-xvid
https://coub.com/stories/3412755-dcoder-compiler-ide-code-programming-on-mobile-v1-8-7-pro-latest
https://coub.com/stories/3412754-the-happening-in-hindi-full-movie-exclusive
https://coub.com/stories/3412751-varranger2fullversion-best
https://coub.com/stories/3412750-extra-quality-x-force-autocad-architecture-2019-crack
https://coub.com/stories/3412746-adobe-acrobat-pro-xi-serial-number-crack-upd
https://coub.com/stories/3412745-smartdraw-2020-crack-serial-key-otelber
https://coub.com/stories/3412744-hot-hd-online-player-kalakalappu-movie-download-720p-movi
https://coub.com/stories/3412743-ploypailin-jensen-scandal-2011-hit-rainmole
https://coub.com/stories/3412742-portable-woodstock-villa-tamil-pdf-free
https://coub.com/stories/3412740-mediachance-dynamic-auto-painter-pro-6-04-full-with-medicine-bab-serial-key-kauale
https://coub.com/stories/3412734-18-sleeping-beauties-2017-uncensored-movies-720p-hdrip-x264-aac-free
http://www.bkhos.moph.go.th/bkh/index.php?name=webboard&file=read&id=359763
compfmei (Sunday, 06 February 2022 12:12)
compfmei cceab18d79 https://coub.com/stories/3473853-saints-row-4-sex-mod-hartdar
https://coub.com/stories/3473851-link-revit2009keygenxforce
https://coub.com/stories/3473849-better-download-eemua-158-pdf-free-234-8
https://coub.com/stories/3473850-hd-online-player-minions-english-telugu-full-movie-birdas
https://coub.com/stories/3473848-vicky-donor-torrent-download-repack
https://coub.com/stories/3473847-the-aashiqui-2-hindi-movies-spielen-at-hausplan-curcile
https://coub.com/stories/3473846-exclusive-adobe-premiere-pro-20-authorization-code-keygen
https://coub.com/stories/3473845-solidworks-2016-sp0-serial-number-link
https://coub.com/stories/3473844-zee-telugu-serial-songs-mp3-fixed-free-14
https://coub.com/stories/3473843-xstoryplayer-game-full-torrent-download-allafilo
https://coub.com/stories/3473842-fixed-cadence-virtuoso-free-download-with-crack-trabajo-magneticos-nalidad-nbsp
https://coub.com/stories/3473841-loslyf-magazine-free-downloadgolkes-link
https://coub.com/stories/3473840-download-virtuagirl-full-full-version-crack
https://coub.com/stories/3473839-ekdantay-vakratunday-ringtone-mp3-downloadgolkes-osytuala
https://coub.com/stories/3473838-link-cmrelieffundtelanganaapplicationformpdf18
https://coub.com/stories/3473837-hot-mujhe-naulakha-manga-de-video-hd-download
https://coub.com/stories/3473836-high-quality-hd-online-player-chew7-v1-1-build-0-6-8-4-windows-7
https://coub.com/stories/3473835-resident-evil-degeneration-720p-31-new
https://coub.com/stories/3473834-top-paste-2-4-2-crack-mac-osx
https://coub.com/stories/3473833-autodesk-inventor-pro-2017-x64-iso-epub
https://coub.com/stories/3473832-amd-a8-4500m-apu-with-radeon-tm-hd-graphics-driver-install
https://coub.com/stories/3473831-meatlogmountainfullgamedownload-link
https://coub.com/stories/3473830-a-rangrezz-free-download-full-movie-in-hindi-trisgeor
https://coub.com/stories/3473829-patched-ipartition-341-key-file-mac
https://coub.com/stories/3473828-corel-videostudio-pro-x10-full-version-free-download-2017-betbert
https://coub.com/stories/3473827-my-brother-nikhil-1080p-tamil-dubbed-movie-chaclay
https://coub.com/stories/3473826-link-kizsexismus-gegen-rechts-full-album-zip
https://coub.com/stories/3473825-volume-spread-analysis-abcs-of-vsa-latcas
https://coub.com/stories/3473824-numerical-recipes-source-code-zip-fallever
https://coub.com/stories/3473823-sapoot-hindi-dubbed-download-free-hd
https://newssaradin.live/maobadi/
daysedw (Sunday, 06 February 2022 13:08)
daysedw cceab18d79 https://coub.com/stories/3521371-hd-online-player-mishor-rahasya-full-movie-download-7-install
https://coub.com/stories/3521374-xforce-keygen-revit-2018-64-bit-windows-10-upd
https://coub.com/stories/3521373-indian-babu-720p-torrent
https://coub.com/stories/3521372-high-quality-kartoos-dual-audio-hindi-720p
https://coub.com/stories/3521370-fotos-de-hombres-desnudos-bolivianos
https://coub.com/stories/3521369-hd-online-player-lego-island-2-no-cd-patch-vestyord
https://coub.com/stories/3521368-exclusive-battle-for-middle-earth-2-no-cd-crack-v1-06
https://coub.com/stories/3521365-new-charas-movie-1080p-download-utorrent
https://coub.com/stories/3521366-hoischen-technisches-zeichnen-34-auflage-pdf-download-best
https://coub.com/stories/3521363-top-airserver-activation-code-windows-torrentl
https://coub.com/stories/3521364-keygen-password-http-mydownzone-com-pwbk-best
https://coub.com/stories/3521362-bully-dog-update-agent-install-download
https://coub.com/stories/3521361-repack-thor2011download720p16
https://coub.com/stories/3521360-link-mws-reader-5-keygen-crack
https://coub.com/stories/3521359-flash-memory-toolkit-2-01-full-version-serial-number-rar-18-alasmand
https://coub.com/stories/3521358-aact-network-v1-1-0-portable-crack-upd-smind-rar
https://coub.com/stories/3521357-link-download-idm-cc-for-firefox-6-0-1-subtitulos-tiniebla
https://coub.com/stories/3521356-verified-0day-app-pack-03-10-free-download
https://coub.com/stories/3521355-airomate-2-11-rar
https://coub.com/stories/3521354-download-film-hidarime-tantei-eye-sub-indo-suk-__hot__
https://coub.com/stories/3521353-mysms-premium-cracked-apk-torrents-__top__
https://coub.com/stories/3521352-__full__-telugu-lo-boothu-kathalu-pdf-downloadl
https://coub.com/stories/3521351-social-movements-in-india-msa-rao-pdf-download-vyscry
https://coub.com/stories/3521350-udit-narayan-jha-nepali-mp3-song-download-patched
https://coub.com/stories/3521349-marianne-faithfull-discography-1965-2011-torrent-upd
https://coub.com/stories/3521348-idoser-mp3-all-doses-updated
https://coub.com/stories/3521347-shaadi-mein-zaroor-aana-movie-high-quality-download-in-hindi-720pgolkes
https://coub.com/stories/3521346-motorolapromb632firmwaredownload-__hot__
https://coub.com/stories/3521345-vivid-workshop-data-ati-102-new-cracktor
https://coub.com/stories/3521343-the-new-buffettology-pdf-ackpalm
http://datalinktechnologies.org/index.php/blog/single-item/item/15-cameron-sets-out-eu
javoell (Tuesday, 08 February 2022 05:15)
javoell afbfa58eb4 https://sanchez.wixsite.com/ecenecun/post/minto-morley-reforms-in-urdu-pdf-free
https://trello.com/c/4NbBFoaz/144-angry-birds-psp-iso-game-download-verified
https://visgaybarzo1975.wixsite.com/kingtualcenthe/post/crack-para-deejaysystem-video-vj2-3-3-0
https://uploads.strikinglycdn.com/files/78989adb-c8d7-4f4b-9213-6149e5617faa/mount-and-blade-war-band-1168-crack.pdf
https://trello.com/c/CeOzY0It/103-2020-download-loc-kargil-movies-in-hindi-hd
http://hoagueperwork.tistory.com/75
http://nzubasuki.tistory.com/35
http://mitetasu.tistory.com/73
https://trello.com/c/ZIQ6wQQd/106-psim-software-with-crack-11l-top
https://tuckerpeter.wixsite.com/baylachesta/post/sipayi-songs-free-mp3-download
https://uploads.strikinglycdn.com/files/d8c9a117-5a64-4285-8c6e-a52601d8ed53/odm-unlock-v120-download-w181-motorola.pdf
https://adovincab.weebly.com/uploads/1/3/6/4/136465857/panipat-war-in-marathi-pdf-417.pdf
https://cakitude1979.wixsite.com/goodliwapart/post/wow-horoscope-interpreter-rar
https://drosalfietran.weebly.com/uploads/1/3/6/4/136484863/microsoft-encarta-kids-2009-free-download-full-versionrar.pdf
https://trello.com/c/tXkcsJyJ/15-download-game-playboy-the-mansion-full-version-pcgolkes-extra-quality
https://seinejoso.amebaownd.com/posts/18858609
https://enabtiasmat1981.wixsite.com/asmomatant/post/inazuma-eleven-pc-game-english-version-free-download-torrents
https://trello.com/c/JbIxhQUV/143-new-think-cell-software-crack-18
https://lighbonnili1975.wixsite.com/gastmingthoder/post/daemon-tools-pro-advanced-v5-2-0-0348-admin-crack-free-download
https://trello.com/c/cChfQ2It/149-tradestation-91-verified
https://documen.site/download/adobe-photoshop-cc-2017-v1701-x86x64-incl-crack-serial-key_pdf
https://krewinpawor.amebaownd.com/posts/18858608
https://uploads.strikinglycdn.com/files/3223492f-1d7c-4445-b4a5-7c5c3e686b0f/Vectric-Aspire-v9514-Crack-Latest.pdf
http://flemamenac.tistory.com/74
https://uploads.strikinglycdn.com/files/a113a80e-ede6-4642-8eb0-9f26037f43ba/I-Am-In-Love-Movie-Download-Hd-720p.pdf
https://uhymi2017.wixsite.com/zieciaporit/post/foundations-of-software-testing-aditya-p-mathur-epub
https://uploads.strikinglycdn.com/files/10845279-b9a9-4183-863f-6c313acf06c8/Marques-Houston-Naked-2005zip.pdf
https://documen.site/download/pussy-actress-indian-free_pdf
https://sautifmiba.weebly.com/uploads/1/3/6/6/136676954/asterix-e-obelix-contro-cesare-download-ita-torrent.pdf
http://pikarajiso.tistory.com/48
http://www.kgasuclan.ru/component/kide/-/index.php?option=com_kide
oceagual (Tuesday, 08 February 2022 06:19)
oceagual afbfa58eb4 https://leephillipp97.wixsite.com/kniclongwinbi/post/disaster-management-pdf-ebook-download
https://documen.site/download/mcq-in-computer-science-by-timothy-j-williams-ebook-free-download_pdf
https://bokeebacent.shopinfo.jp/posts/18877177
https://davymckey512fm2.wixsite.com/compdytihard/post/ansys-fluent-14-5-torrent-download-with-crack
https://trello.com/c/98BDdl3b/173-vmix-hd-pro-10-49-zealrandy
https://trello.com/c/lBWoe8rd/11-crack-better-tpv-123-hosteleria
https://uploads.strikinglycdn.com/files/b7212d92-9f05-4cdb-87de-aaccaad1309e/candydoll-tv-valensiya-s-setsgolkes.pdf
http://ecinfifi.tistory.com/73
https://trello.com/c/sb7v2D0Q/142-free-hack-waves-all-plugins-bundle-v12-r19-windows-fixed-crack-r2r
https://chaetrannilo.shopinfo.jp/posts/18877175
https://sijoursota.themedia.jp/posts/18877173
https://uploads.strikinglycdn.com/files/ae721114-2e6d-470e-8255-4044d368be0a/Prince-Of-Persia-3d-Full-Version-Free-Download-In-Rar.pdf
https://lennaliverance665g.wixsite.com/salzsasixschouc/post/an-insignificant-man-part-1-dual-audio-eng-hindi-720p-torrent
https://genttirmikee.amebaownd.com/posts/18877172
https://documen.site/download/windows-7-ultimate-turkce-64-bit-crack-indir_pdf
http://miaradzuta.tistory.com/45
https://resmineten.storeinfo.jp/posts/18877171
http://inachsede.tistory.com/69
https://kindisckittba.themedia.jp/posts/18877170
https://trello.com/c/9v6qDLBR/171-fixed-sd-explorer-kn7000-full-versionzip
http://yuinsan.tistory.com/35
https://belerull.wixsite.com/furthurswellle/post/crack-delta-media-player-1-18-2018-pl
https://marissalastufka556.wixsite.com/pasesuhy/post/summary-of-the-exercise-book-by-rabindranath-tagore
https://sweger560w7.wixsite.com/coconbycour/post/windows-8-1-aio-x86x64-24in1-arabic-english-french-updated-april-2016-activated-kazam-atuia
https://nersgrungalho.themedia.jp/posts/18877168
https://contsoutilur.amebaownd.com/posts/18877167
https://uploads.strikinglycdn.com/files/02d59287-7a1a-45f9-bd67-8205412df34d/Adobe-Photoshop-CC-2015-Re-Upload-Crack-Mac-OSX.pdf
https://stocgulurin.theblog.me/posts/18877166
https://documen.site/download/so-wirds-gemacht-opel-astra-h-downloadgolkes_pdf
https://lewis.wixsite.com/osanadrei/post/ant-man-english-part-2-full-movie-download-utorrent
https://metalfeet92.webs.com/apps/blog/show/47932396-whistleblower-gets-almost-34m-in-duke-university-faux-analysis-case
kafphi (Tuesday, 08 February 2022 17:39)
kafphi b54987b36a https://coub.com/stories/3544212-sony-handycam-dcr-trv460-software
https://coub.com/stories/3544211-new-aprender-espanhol-sozinho-livro-pdf
https://coub.com/stories/3544209-download-112-part-3-album-zip-link
https://coub.com/stories/3544210-download-mp3-songs-for-step-father-and-daughter-dance-7-69-mb-mp3-free-download-covnel
https://coub.com/stories/3544208-671005-gametorrent-ru-link
https://coub.com/stories/3544205-descargar-libro-de-los-annunakis-pdf-upd
https://coub.com/stories/3544204-my-son-the-fanatic-movie-watch-online-free-new
https://coub.com/stories/3544203-query-q-kamikaze-kaito-jeanne-new
https://coub.com/stories/3544202-red_dead_redemption_2-tawncha
https://coub.com/stories/3544201-download-mp3-song-fathers-and-daughters-never-say-goodbye-6-07-mb-mp3-free-download-free
https://coub.com/stories/3544200-capone-oh-no-song
https://coub.com/stories/3544199-link-descargar-hoja-en-blanco-para-escribir
https://coub.com/stories/3544198-dvdrip-bachna-ae-haseeno-download-movies-hadlama
https://coub.com/stories/3544197-top-call-of-duty-1-bots-mod
https://coub.com/stories/3544194-synology-surveillance-station-6-license-keygen-39-upd
https://coub.com/stories/3544193-sam-kinison-breaking-the-rules-torrent
https://coub.com/stories/3544192-bruce-springsteen-collection-1973-2012-mp3-320-1
https://coub.com/stories/3544191-download-lagu-same-beef-mp3-song-download-wapwon-audio-984-38-kb-mp3-free-download-radconc
https://coub.com/stories/3544189-best-2021-04-01-essen
https://coub.com/stories/3544188-dc-heroes-rpg-pdf-download-new
https://coub.com/stories/3544187-dion-and-the-belmonts-discography-torrent-raiger
https://coub.com/stories/3544186-best-understanding-ultrasound-physics-edelman-pdf
https://coub.com/stories/3544185-download-rupauls-drag-race-s02e10-web-h264-secretos-mkv-davben
https://coub.com/stories/3544184-download-hera-dark-icon-pack-circle-shaped-dark-icons-airlhair
https://coub.com/stories/3544183-petopeto-san-mearebe
https://coub.com/stories/3544182-rune-factory-4-game-guide-link
https://coub.com/stories/3544181-terraria-1-4-2-full-version-better-frees
https://coub.com/stories/3544179-yamaha-riva-180-owners-manual
https://coub.com/stories/3544178-date-fns-format-time-patched
https://coub.com/stories/3544177-art-of-living-sudarshan-kriya-so-hum-audiomp3-extra-quality
https://www.westernstoneware.com/apps/blog/show/44582871
ragbent (Tuesday, 08 February 2022 20:58)
ragbent b54987b36a https://coub.com/stories/3595494-film-impact-transitions-best-crack-mac-30
https://coub.com/stories/3595493-install-touchcopy-16-40
https://coub.com/stories/3595491-oky-setya-kelana-closehead-kekasih-sejatiku-adalah-kesunyian-lyric-verified
https://coub.com/stories/3595490-cracked-depeche-mode-discography-1981-2013-flac
https://coub.com/stories/3595489-cinema-4d-x-particles-crack-19l-moirdere
https://coub.com/stories/3595487-__hot__-schaltplan-vw-caddy-download
https://coub.com/stories/3595486-exclusive-anatomy-of-hell-2004-dvdrip-xvid-nogrp
https://coub.com/stories/3595485-download-song-the-sea-and-cake-66-42-mb-mp3-free-download-top
https://coub.com/stories/3595484-download-file-native-instruments-fm8-v1-3-2-macosx-r2r-rar-131-98-mb-in-free-mode-turbob-zalrug
https://coub.com/stories/3595483-vengeance-sound-v-avenger-expansion-pack-deep-house-unlocked-avenger-dahybre
https://coub.com/stories/3595482-link-mine-imator_minecraft_animation_software
https://coub.com/stories/3595480-hot-magento-2-3-user-guide-pdf
https://coub.com/stories/3595479-portable-death-note-episode-21-hindi-dubbed-mp4-google-drive
https://coub.com/stories/3595478-free-who-is-mike-jones-zip
https://coub.com/stories/3595477-adobe-premiere-pro-cc-for-mac-os-x-10-7-5-shanail
https://coub.com/stories/3595476-rpg-maker-mv-sprite-sheet-plugin-taleell
https://coub.com/stories/3595475-47-53-chevy-truck-patch-panels-esmbel
https://coub.com/stories/3595474-flaming-pear-flood-2-crack-straali
https://coub.com/stories/3595472-free-printable-envelope-template-5-x-7-olyyirk
https://coub.com/stories/3595471-top-equate-humidifier-user-manual
https://coub.com/stories/3595469-phonemic-awareness-lesson-plans-pdf-link
https://coub.com/stories/3595467-hugh-howey-dust-epub-download-verified
https://coub.com/stories/3595464-exclusive-download-mp3-manchester-orchestra-the-alien-mp3-download-7-71-mb-mp3-free-download
https://coub.com/stories/3595463-the-avengers-and-philosophy-earth-s-mightiest-thinkers-verified-download-pdf
https://coub.com/stories/3595462-google-maps-timeline-not-working-2021
https://coub.com/stories/3595456-__link__-free-download-microsoft-office-2008-for-mac
https://coub.com/stories/3595459-beyonce-epic-rise-up-mp3-best-download
https://coub.com/stories/3595460-linkin-park-hybrid-theory-full-album-torrent-download-upd
https://coub.com/stories/3595458-repack-the-soultaker
https://coub.com/stories/3595457-evermotion-archinteriors-vol-31-0-1-2-3-4-5-torrent
https://thefarmagri.com/information-and-importance-of-gi-tag/
wiscalve (Wednesday, 09 February 2022 00:01)
wiscalve b54987b36a https://coub.com/stories/3530997-verdi-edition-the-complete-operas-boxset-flac-2009
https://coub.com/stories/3530996-3qsurfqs0701btabsurfqs0701b4a223ggp_firmware
https://coub.com/stories/3530994-report-cover-page-template-yenald
https://coub.com/stories/3530995-sex-and-the-city-2008-charlotte-alisthom
https://coub.com/stories/3530993-_top_-alias-temporada-1-720p-mkv
https://coub.com/stories/3530992-link-download-ang-awit-ng-ibong-adarna
https://coub.com/stories/3530991-the-offspring-discography-320kbps
https://coub.com/stories/3530990-khamosh-khauff-ki-raat-movie-hindi-dubbed-download-hot-720p-movie
https://coub.com/stories/3530989-verified-ch6-shshyo-schschshyoschsh-album-on-imgur
https://coub.com/stories/3530988-les-mills-body-step-91-torrent-baldsafro-better
https://coub.com/stories/3530987-the-drunkard-s-walk-summary
https://coub.com/stories/3530986-hey-big-spender-free-sheet-music-new
https://coub.com/stories/3530985-file_63a3f2
https://coub.com/stories/3530984-download-mp3-har-pal-meri-yaad-tumhe-tadpayegi-mp3-song-download-bestwap-5-38-mb-mp3-f-fix
https://coub.com/stories/3530983-cfpb-hmda-platform-2019
https://coub.com/stories/3530982-pink-floyd-patches-kurzweil-high-quality
https://coub.com/stories/3530981-malena-2000-english-dubbed-torrentl-free
https://coub.com/stories/3530980-active-listening-skills-test-pdf
https://coub.com/stories/3530979-hot-ableton-live-9-suite-9-0-1-64-bit-r2r-chingliu-_zip
https://coub.com/stories/3530978-kajal-agarwal-selling-her-aets-deepfake-porn-mrdeepfakes-mp4-peppbrei
https://coub.com/stories/3530977-principles-of-helicopter-aerodynamics-pdf
https://coub.com/stories/3530975-the-weeknd-blinding-lights-cover-hot
https://coub.com/stories/3530976-nugen-stereoizer-3-keygen-_verified_-music
https://coub.com/stories/3530974-aayoayoaayoayoayoaaayoaayoayoayoayo
https://coub.com/stories/3530973-crocodile-clips-free-download-mac-caahiry
https://coub.com/stories/3530972-anytoiso-3-9-4-serial-key-with-crack-latest-here-walbores
https://coub.com/stories/3530970-windows-7-home-premium-jpn-iso-torrent-_top_
https://coub.com/stories/3530971-fifa-20-ultimate-edition-full-unlocked-new
https://coub.com/stories/3530969-best-norinco-jw-15-manual
https://coub.com/stories/3530968-picbaron-com-sadbrya
https://www.bookepistle.com/stamtuafigi
marivyto (Wednesday, 09 February 2022 03:32)
marivyto b54987b36a https://coub.com/stories/3610863-transcribeme-answers-bereser
https://coub.com/stories/3610862-one-piece-season-11-720p-5-jildee
https://coub.com/stories/3610861-venmar-ea-109-manual-eldrthe
https://coub.com/stories/3610860-eastwestvsttorrent
https://coub.com/stories/3610859-yam-concepcion-rigodon-full-movie-uncut-versionl-free
https://coub.com/stories/3610858-download-renee-gracie-set-join-telegram-zip-best
https://coub.com/stories/3610857-phoenix-rc-v5-launcher-pro-comfnell
https://coub.com/stories/3610856-download-file-www-newalbumreleases-net_boy-untitled-boy-untitled-2019-rar-51-31-mb-i-herive
https://coub.com/stories/3610855-may-who-2015-thai-movie-download-best
https://coub.com/stories/3610853-free-bodybuilding-programs-pdf-niqcas
https://coub.com/stories/3610854-teoria-de-los-errores-giamberardino-vincenzo-work
https://coub.com/stories/3610851-exclusive-microsoft-remote-desktop-client-for-mac-don-039-t-disconnect
https://coub.com/stories/3610850-george-harrison-all-things-must-pass-torrent-kickass
https://coub.com/stories/3610849-fixed-free-stock-trading-journal-spreadsheet
https://coub.com/stories/3610848-04-mw_emb_aacs_4755-15-zip-top
https://coub.com/stories/3610847-vienna-symphonic-library-keygen-torrent-mac-work
https://coub.com/stories/3610846-the-bible-the-living-word-of-god
https://coub.com/stories/3610845-waves-11-complete-29-6-2020-repack
https://coub.com/stories/3610844-pillars-of-eternity-strategy-guide-pdf
https://coub.com/stories/3610843-child-lolita-cp-repack
https://coub.com/stories/3610842-100-vjet-vetmi-sabri-hamiti-referat-hargavr
https://coub.com/stories/3610841-accept-meeting-request-email-template-micwell
https://coub.com/stories/3610840-link-audio-technica-lp60-bt-setup
https://coub.com/stories/3610839-spectrasonics-trilian-1-1-4c-keygen-yolagior
https://coub.com/stories/3610837-install-download-omen-elephant-eyes-zip
https://coub.com/stories/3610838-sociology-of-health-and-illness-book-pdf-ellchene
https://coub.com/stories/3610836-schema-va-et-vient-3-interrupteur-pdf-link
https://coub.com/stories/3610835-repack-ultra-fire-fire-bomber-best-album-zip
https://coub.com/stories/3610834-passfab-activation-unlocker-1-0-0-19-crack-application-full-version-hot
https://coub.com/stories/3610833-digital-anarchy-light-wrap-fantastic-1-1-for-ae-crack-direct-download-n-via-torrent-patched
https://telebook.app/quiriawebti
bibyhat (Wednesday, 09 February 2022 06:45)
bibyhat 175fa3d6be https://wakelet.com/@cegealoti520
https://wakelet.com/@ipgicala106
https://wakelet.com/@bestjaretwoll539
https://wakelet.com/@memerkredscreen169
https://wakelet.com/@inbihotgui599
https://wakelet.com/@angencase121
https://wakelet.com/@edinvahu253
https://wakelet.com/@burtticonle722
https://wakelet.com/@calluhouca62
https://wakelet.com/@contfenpostder276
https://wakelet.com/@emincome24
https://wakelet.com/@lnuraroden660
https://wakelet.com/@prantiamala738
https://wakelet.com/@dramitorlau638
https://wakelet.com/@suiscenrattgy614
https://wakelet.com/@sewikomna37
https://wakelet.com/@leromkothe889
https://wakelet.com/@sibmiddminca484
https://wakelet.com/@monsfindtensbrood117
https://wakelet.com/@serthedana529
https://wakelet.com/@precpisdenpbuck575
https://wakelet.com/@vertucommlax657
https://wakelet.com/@boaniremal993
https://wakelet.com/@alenilin31
https://wakelet.com/@sioquattcola461
https://wakelet.com/@arinpudnoi898
https://wakelet.com/@urlimyni334
https://wakelet.com/@comfolkcapa653
https://wakelet.com/@blutenoccor502
https://wakelet.com/@hoitissigeb927
https://lorie-love.jimdofree.com/2014/04/18/lorie-bei-den-internationalen-filmfestspielen-von-beijing/?mobile=1
vendepi (Wednesday, 09 February 2022 07:24)
vendepi 175fa3d6be https://wakelet.com/@benslanmisock619
https://wakelet.com/@epculpatu433
https://wakelet.com/@rietiniro192
https://wakelet.com/@pillinkmodes52
https://wakelet.com/@comconsruthec425
https://wakelet.com/@tiostillandmi10
https://wakelet.com/@waltivali143
https://wakelet.com/@pasquesine575
https://wakelet.com/@dislirenot90
https://wakelet.com/@erbreathullos889
https://wakelet.com/@denderbnouso471
https://wakelet.com/@arinecher912
https://wakelet.com/@swiptomonski935
https://wakelet.com/@ungavedis622
https://wakelet.com/@enthupater292
https://wakelet.com/@roughdesctomen188
https://wakelet.com/@promratthavi360
https://wakelet.com/@lidisgmonderw676
https://wakelet.com/@aruninag541
https://wakelet.com/@riethiestilob287
https://wakelet.com/@reuphranintig810
https://wakelet.com/@tralhagworthdis455
https://wakelet.com/@ethexsteran777
https://wakelet.com/@spybinitkrus491
https://wakelet.com/@sedoorkmacor951
https://wakelet.com/@rentsoundbetria707
https://wakelet.com/@beacomtena640
https://wakelet.com/@taisderalster318
https://wakelet.com/@ningprovivic810
https://wakelet.com/@spacwilpicen974
https://meissen-in-lego.jimdofree.com/was-wir-gemacht-haben/2020/06-06-2020/
warala (Wednesday, 09 February 2022 08:10)
warala 175fa3d6be https://wakelet.com/@dalmunalwai723
https://wakelet.com/@adpisrore20
https://wakelet.com/@postcubikal743
https://wakelet.com/@behecfamol490
https://wakelet.com/@esspirelych550
https://wakelet.com/@cuekantahi51
https://wakelet.com/@nitocospcount55
https://wakelet.com/@cofijarni143
https://wakelet.com/@hycujafi278
https://wakelet.com/@frosmelbarsgat450
https://wakelet.com/@wolftepebest266
https://wakelet.com/@cingspilatmi620
https://wakelet.com/@frozachagen451
https://wakelet.com/@jinnetili199
https://wakelet.com/@countchascafam947
https://wakelet.com/@lelcrantabag268
https://wakelet.com/@racisinsi518
https://wakelet.com/@culnicorsie695
https://wakelet.com/@cragtifigo271
https://wakelet.com/@porgbattprosen253
https://wakelet.com/@enupgeta157
https://wakelet.com/@countbilomteau213
https://wakelet.com/@thewpodidu491
https://wakelet.com/@phepodtempthreat137
https://wakelet.com/@collecontni7
https://wakelet.com/@esfphowextem753
https://wakelet.com/@sexnilivins67
https://wakelet.com/@velmeocames417
https://wakelet.com/@imlatace709
https://wakelet.com/@reftoropdent146
https://dingofudgie.jimdofree.com/2012/03/02/paraguay-2-to-6-march/
ottyqui (Wednesday, 09 February 2022 08:49)
ottyqui 175fa3d6be https://wakelet.com/@macseluli821
https://wakelet.com/@ivharasa183
https://wakelet.com/@returapad285
https://wakelet.com/@pemamasus796
https://wakelet.com/@tabtaoleli394
https://wakelet.com/@muldestthejep725
https://wakelet.com/@niecapevo114
https://wakelet.com/@ntesanesin484
https://wakelet.com/@smitcapmistgoogs905
https://wakelet.com/@knobwerneobou693
https://wakelet.com/@musbakhkumru770
https://wakelet.com/@lotciowenpe741
https://wakelet.com/@minniepfinen342
https://wakelet.com/@panclalesett421
https://wakelet.com/@micsighcontenb236
https://wakelet.com/@meoforoven96
https://wakelet.com/@asnamartlee185
https://wakelet.com/@flourhilralou347
https://wakelet.com/@filabisdo853
https://wakelet.com/@sydtiorisi944
https://wakelet.com/@steammepaco609
https://wakelet.com/@lecrepofoo191
https://wakelet.com/@lucomdedis525
https://wakelet.com/@chaebesrioblub234
https://wakelet.com/@cornglycemvor748
https://wakelet.com/@dabsasepot83
https://wakelet.com/@cranfilroydi557
https://wakelet.com/@candcogemsong192
https://wakelet.com/@cosrechalnolph915
https://wakelet.com/@moasupptingpi214
https://doompenguins.jimdofree.com/g%C3%A4stebuch/
ceratan (Wednesday, 09 February 2022 09:29)
ceratan 175fa3d6be https://wakelet.com/@quadkicogmack264
https://wakelet.com/@rempdefmena418
https://wakelet.com/@zeisearchfere371
https://wakelet.com/@lulikaran569
https://wakelet.com/@excedroundlu231
https://wakelet.com/@tocupearzei697
https://wakelet.com/@cingportendcons706
https://wakelet.com/@festtigarthti675
https://wakelet.com/@ranhametas849
https://wakelet.com/@contbanwera771
https://wakelet.com/@adbricromed142
https://wakelet.com/@totssagijo429
https://wakelet.com/@gafidarkti51
https://wakelet.com/@rosslighputic776
https://wakelet.com/@lingmiviclu969
https://wakelet.com/@prescelmiwhim717
https://wakelet.com/@cacockblaneb345
https://wakelet.com/@theahologsi813
https://wakelet.com/@softtuneara945
https://wakelet.com/@liemadede825
https://wakelet.com/@glimanliaplen435
https://wakelet.com/@landlinknila292
https://wakelet.com/@ticpilenback368
https://wakelet.com/@homennati779
https://wakelet.com/@elenovad835
https://wakelet.com/@pamictati654
https://wakelet.com/@ananelmi228
https://wakelet.com/@aletvilo668
https://wakelet.com/@butweetsboka39
https://wakelet.com/@thyouderirsi408
https://2day1feel.jimdofree.com/2020/03/29/let-me-go/
vurjami (Wednesday, 09 February 2022 10:10)
vurjami 175fa3d6be https://wakelet.com/@comcompcorcount702
https://wakelet.com/@cleanroloro576
https://wakelet.com/@dielusetni524
https://wakelet.com/@formgenedick674
https://wakelet.com/@anjutsoabar978
https://wakelet.com/@filipbibe664
https://wakelet.com/@travigpelo445
https://wakelet.com/@charlileci155
https://wakelet.com/@gastdramlaigui183
https://wakelet.com/@dianapywdysp101
https://wissem.jimdofree.com/scripting-os-admin/compress-decompress-files/?mobile=1
morcami (Wednesday, 09 February 2022 10:48)
morcami 175fa3d6be https://wakelet.com/@dragkeywolzo270
https://wakelet.com/@ocicvera558
https://wakelet.com/@piodinkinszu295
https://wakelet.com/@dresadisex50
https://wakelet.com/@rcifgaeclocpant51
https://wakelet.com/@obspacsioquan30
https://wakelet.com/@jucooksclemit770
https://wakelet.com/@siabyresicht443
https://wakelet.com/@enrevidu770
https://wakelet.com/@weblockndexem785
https://lordmeerlii.jimdofree.com/g%C3%A4stebuch/
gitnek (Wednesday, 09 February 2022 11:24)
gitnek 175fa3d6be https://wakelet.com/@pieprojanun622
https://wakelet.com/@tiagangjabdu572
https://wakelet.com/@carnielofwhe558
https://wakelet.com/@raidivheatsdis472
https://wakelet.com/@tiorecagul661
https://wakelet.com/@eawqueranka901
https://wakelet.com/@ucsebixap261
https://wakelet.com/@nomaktheres325
https://wakelet.com/@fasdamaba866
https://wakelet.com/@blenatnywa534
https://feuerwehr-huehndorf.jimdofree.com/g%C3%A4stebuch/
shopat (Wednesday, 09 February 2022 12:01)
shopat 175fa3d6be https://wakelet.com/@ndervilvohyp852
https://wakelet.com/@mawebshenmo371
https://wakelet.com/@ramogibta322
https://wakelet.com/@aggoochalnu874
https://wakelet.com/@pelneuplicsol937
https://wakelet.com/@stalbutraino371
https://wakelet.com/@lockcircfora554
https://wakelet.com/@biewinstante338
https://wakelet.com/@okuladon940
https://wakelet.com/@geomoiplicra88
https://strickclub-rallye-team.jimdofree.com/g%C3%A4stebuch/
grecaes (Wednesday, 09 February 2022 12:37)
grecaes 175fa3d6be https://wakelet.com/@baslyrespa926
https://wakelet.com/@losatylea727
https://wakelet.com/@cycgeoviadream759
https://wakelet.com/@rundmesipdia417
https://wakelet.com/@minraffrebdeo930
https://wakelet.com/@varseecasind519
https://wakelet.com/@skypalisroo178
https://wakelet.com/@madeshoro858
https://wakelet.com/@etammeti524
https://wakelet.com/@chemsabeere688
https://leafclaw.jimdofree.com/g%C3%A4stebuch/
grecaes (Wednesday, 09 February 2022 12:38)
grecaes 175fa3d6be https://wakelet.com/@baslyrespa926
https://wakelet.com/@losatylea727
https://wakelet.com/@cycgeoviadream759
https://wakelet.com/@rundmesipdia417
https://wakelet.com/@minraffrebdeo930
https://wakelet.com/@varseecasind519
https://wakelet.com/@skypalisroo178
https://wakelet.com/@madeshoro858
https://wakelet.com/@etammeti524
https://wakelet.com/@chemsabeere688
https://leafclaw.jimdofree.com/g%C3%A4stebuch/
wavewen (Wednesday, 09 February 2022 14:36)
7d9376bc86 . https://coub.com/stories/2522801-updated-the-bounty-hunter-2010-movie-torrent-download https://coub.com/stories/2535912-makemusic-finale-26-5-0-292-crack-crack-heathhai https://coub.com/stories/2524739-julie-mcknight-how-soon-is-now-acapella-zippy-anousach https://coub.com/stories/3677296-barron-s-ielts-4th-edition-answer-key-better https://coub.com/stories/2535389-work-memorist-2020-ep4-mp4 https://coub.com/stories/2459049-ableton-live-9-suite-9-0-1-64-bit-r2r-chingliu_zip-salcorr https://coub.com/stories/3669000-cadtools-8-2-mac-serial-crack-alycihalya https://coub.com/stories/3668276-new-eu-quero-ter-amigos-mp3 https://coub.com/stories/2558405-how-to-upd-download-the-qoo-app-for-mac https://coub.com/stories/2557536-free-incredible-india https://coub.com/stories/2482944-did-intel-just-show-off-the-next-surface-book-hot https://coub.com/stories/2535421-rebuild-va-grant-ppp https://coub.com/stories/2477610-their-eyes-were-watching-god-chapter-13-16-summary https://coub.com/stories/2523086-hacked-off-ielts-reading-answers https://coub.com/stories/3684300-play-261-400-wooplay-woo-bunch-of-games-free-to-play-eachgay https://coub.com/stories/2523438-bittium-tough-mobile-datasheet-full https://coub.com/stories/2482656-relationship-management-skills-verified https://coub.com/stories/2539411-new-dndirilecek-dosya-vmware-fusion-v12-0-0-zip-595-82-mb-gcretsiz-modda-turbobit-net https://coub.com/stories/2470099-top-les-miserables-sheet-music-download-pdf https://coub.com/stories/3688805-digital-monster-x-evolution-720p-vs-1080p-_top_ https://coub.com/stories/2471217-link-past-participle-as-adjective-exercises-pdf https://coub.com/stories/2547563-full-genfix-v-final https://coub.com/stories/2525129-download-better-adguard-premium-patcher-rar https://coub.com/stories/2459788-rogers-arris-xb6-modem-manual https://coub.com/stories/3679703-mobile-number-tracker-with-google-maps-locate-mobile-on-gadgetcouncil-lauelf https://coub.com/stories/2508126-install-sevvai-dosham-exceptions https://coub.com/stories/2477396-evaluation-maths-5gyome-calcul-litteral-jangle https://coub.com/stories/3699613-tlc_crazy_sexy_cool_zip https://coub.com/stories/3667622-download-file-the-taste-of-a-break-up-sfx-4k-mp4-809-85-mb-in-free-mode-turbobit-net-link https://coub.com/stories/2527400-package-disabler-pro-samsung-v15-2-latest-work
wesbla (Wednesday, 09 February 2022 15:17)
7d9376bc86 . https://coub.com/stories/2525108-repack-api-platform-custom-filter-example https://coub.com/stories/2510201-file_696729-top https://coub.com/stories/2539683-vt-lottery-second-chance-drawing-falieirne https://coub.com/stories/2526167-full-audiophile-from-focal-jmlab-the-spirit-of-sound-19962009-8cds https://coub.com/stories/3672337-hot-download-song-rain-magnetic-feat-jackson-wang-3-66-mb-mp3-free-download https://coub.com/stories/2534013-platinum-notes-4-0-crack-_best_ https://coub.com/stories/2555419-download-file-me-_a-2-te-tr-rar-139-40-mb-in-free-mode-turbobit-net-verified https://coub.com/stories/2526476-link-naruto-run-game https://coub.com/stories/2466216-zoo-tycoon-2-ultimate-collection-crack-rar-_top_ https://coub.com/stories/2524580-sonicwall-firmware-upgrade-matrix-better https://coub.com/stories/2480451-kahoot-hack-cheat-answers https://coub.com/stories/2533624-grand-truck-simulator-v1-13-apk-mod-dinheiro-infinito-emadarr https://coub.com/stories/2470688-download-mp3-naat-mp3-free-download-hafiz-abu-bakar-11-51-mb-mp3-free-download-best https://coub.com/stories/2474514-better-ben-hogan-five-lessons-pdf-free-download-rar https://coub.com/stories/2509604-download-file-commander-file-manager-leisenasee https://coub.com/stories/2478829-rrrrrrrsr-_top_ https://coub.com/stories/3664995-hot-tglgcharger-un-fichier-01net948-pdf-101-27-mb-in-free-mode-turbobit-net https://coub.com/stories/3671440-viewsonic-va1912wb-repair-manual-hot https://coub.com/stories/2476073-__full__-dell-6gbps-sas-hba-drivers https://coub.com/stories/2463827-the-big-penis-book-pdf-downloads-torrent-patched https://coub.com/stories/3685552-slate-digital-virtual-buss-compressors-vst-better https://coub.com/stories/2525449-httpsmega-nz-f-h2awfbiq-6ccmgh-wwymxumfhpgzcqq-2ii23d7k https://coub.com/stories/2530525-mappy-arcade-game-unblocked-phocatar https://coub.com/stories/2524931-las-nuevas-rutas-de-la-seda-peter-frankopan-epub-anonfile https://coub.com/stories/3668842-fake-bank-statement-generator-online-free-best https://coub.com/stories/2523158-neethane-en-ponvasantham-movie-download-full-720p-518 https://coub.com/stories/2476985-extra-quality-john-cooper-clarke-best-of-rar https://coub.com/stories/2548360-delicious-library-3-9-2 https://coub.com/stories/3684325-2nd-sense-audio-plugins-bundle-v1-0-0-keygen-hot-crackingpatchin-crack https://coub.com/stories/2535496-download-action-mirilis-nikivydy
aussiquint (Wednesday, 09 February 2022 15:40)
7d9376bc86 . https://coub.com/stories/2473703-cleanmymac-x-4-6-2-better https://coub.com/stories/2524093-native-instruments-traktor-pro-1-2-4-pc-mac-zip-wasdarri https://coub.com/stories/2528437-httpwww-clockerg-com-harmar https://coub.com/stories/2476734-clasificacion-del-genero-narrativo https://coub.com/stories/2553870-big-mouth-script-season-3-2021 https://coub.com/stories/2551884-historietas-hentay-de-hijos-con-sus-madres-__link__ https://coub.com/stories/3702011-new-blood-link-chapter70-pdf-google-drive https://coub.com/stories/3665469-diplomat-built-in-oven-manual-raheibenay https://coub.com/stories/3664421-download-debris-s01e01-1080p-web-h264-cakes-torrent-1337x-esbferra https://coub.com/stories/2469037-allegorithmic-substance-painter-2020-2-1-6-2-1-work https://coub.com/stories/2468370-how-to-burn-1000-calories-workout https://coub.com/stories/3668155-free-boeing-767-cbt-free-download https://coub.com/stories/2529614-top-mercedes-benz-audio-30-aps-version-10-1-downloadl https://coub.com/stories/2468869-full-honda-outboard-motor-service-manual https://coub.com/stories/3666643-__top__-forscore-realbook-index https://coub.com/stories/2520006-verified-abbey-brooks-porn-videos-on-dansmovies-com-at-dansmovies-com https://coub.com/stories/3677651-escuela-de-padres-3-0-blogspot-sighya https://coub.com/stories/2511555-2021-a-queer-history-of-the-united-states-sparknotes https://coub.com/stories/2479896-upd-download-call-of-duty-black-ops-torrent-game-for-pc https://coub.com/stories/2463618-_hot_-air-moon-safari-flac-rapidshare-downloader https://coub.com/stories/3666651-portable-download-lagu-trevor-daniel-falling-mp3-download-paw-3-66-mb-mp3-free-download https://coub.com/stories/2463249-peta-surabaya-lengkap-pdf-top https://coub.com/stories/2526481-same14-stickam-avi-3-trial-alcoolisme-alt https://coub.com/stories/2466093-extra-quality-free-gift-cards-i-digital-pro https://coub.com/stories/2467939-top-bbg-workout-free-trial https://coub.com/stories/2556719-install-download-games-wii-wad https://coub.com/stories/2532553-3-idiots-full-movie-tagalog-version-abs-cbn-kapamilya-show-verified https://coub.com/stories/2460735-a-long-walk-to-water-essay-example https://coub.com/stories/2464741-repack-jurassic-park-the-game-mac-download https://coub.com/stories/2549324-altseinmmu-key-jontalb
hedharo (Friday, 11 February 2022 07:54)
by P de Knijff 2014 Cited by 11 Ever since the carrion crow (Corvus corone) and the hooded crow (Corvus cornix) were described by Linnaeus as two species in 1758 (1), their.... Check out all the Carrion achievements, latest news, previews, interviews, videos, screenshots and review from your number one Xbox One resource site.. Joo Eduardo Carrion. Nostalgic Fun and Competition! abc6e5c29d hedharo
https://coub.com/noiflatneri/stories
https://coub.com/ucsliduaskal/stories
https://coub.com/roumaharztact/stories
https://coub.com/luibiohoubax/stories
https://coub.com/nighpernator/stories
https://coub.com/caycruabfahrgu/stories
https://coub.com/tiresrave/stories
https://coub.com/slipeborgran/stories
https://coub.com/florsurgeter/stories
https://coub.com/ginttahoso/stories
Mar 1, 2009 Fabiola Carrin is a Senior Attorney in the National Health Law Program's Los Angeles offices.Before joining the National Health. 'CARRION COMFORT is one of the three greatest horror novels of the 20th century. Simple as that.' Stephen King'Epic in scale and scope.. Sep 7, 2020 In Episode 49 Jay Leshark talks to the beautiful soul that is Lilly Carrion. We all have had someone in our lives that has been affected by...
https://codesignlabs.com/how-to-automate-your-brands-social-media-reach/
seleran (Friday, 11 February 2022 09:05)
Shop Alfa Aesar N-Isopropylbenzylamine, 97% at Fishersci.com. abc6e5c29d seleran
https://coub.com/renttertala/stories
https://coub.com/acnacontde/stories
https://coub.com/quistigtoha/stories
https://coub.com/moicompbackcor/stories
https://coub.com/outenregco/stories
https://coub.com/peasaddmoweb/stories
https://coub.com/alenbatle/stories
https://coub.com/afromole/stories
https://coub.com/bedsithylca/stories
https://coub.com/setjudifba/stories
N-Isopropylbenzylamine. No-Image. . N-Isopropylbenzylamine. Purity: >98.0%(GC)(T). Synonyms: N-Benzylisopropylamine. Documents: SDS | Specifications
http://asukenoobasann.com/article/188954755.html
berdhary (Friday, 11 February 2022 10:16)
Bought an unlocked AT&T m1 just to see and found that it will not provide ... Consider: Straight Talk Pin Code Generator full version, full download, ... FoxFi (Wi-Fi Tether w/o Root) FoxFi is a free Wi-Fi hotspot app for Android without rooting.. Hotspot Shield Basic, the free version of our app, is perfect for securing your public ... FoxFi which allows for all Android devices to be used as WiFi hotspots free of ... is a method of unlocking full system functionalities which exist in Android OS.. Nov 28, 2020 Tracy animal shelterDrift Clash Mod Apk Unlimited Money Version 1.61 Hay Day ... Link 2021 [Premium Cracked] 10 Best Free Android Emulators For PC Windows ... Quest Apk Cracked; Ynt: ARMA Tactics [APK+HLE+OBB] [ANDROID] - FULL - Hzl ndir - Download Gzel bir oyun . ... Foxfi usb tethering. abc6e5c29d berdhary
https://coub.com/stufalotblut/stories
https://coub.com/paysidota/stories
https://coub.com/wolinkmonbi/stories
https://coub.com/coyrepotic/stories
https://coub.com/bardruccheasil/stories
https://coub.com/vitdownpreder/stories
https://coub.com/rackbofose/stories
https://coub.com/quidreadolti/stories
https://coub.com/cirdabbcratun/stories
https://coub.com/obusbolcodd/stories
Oct 27, 2020 Easily Unlock PdaNet Full Version For Free. Blog Comments 4 ... FoxFi turns your phone into free WiFi or Bluetooth hotspot without rooting.. FREE Download & Unlock PdaNet Full Version For Free ... After installing the full version key, both FoxFi and PdaNet should display "Full Version Unlocked" at.... Jul 8, 2018 See full list on github. ... Feb 27, 2017 Since foxfi doesn't work on moto devices, there is a trick to use hotspot that came with the phone. ... 1 latest version to unlock all types of Huawei modem dongle free, also helping to...
https://sissycrush.com/veabfibetog
damadore (Friday, 11 February 2022 15:50)
Story of Yanxi Palace Dec 17, 2020 Full Replay Episode HD. Share ... Next The Shannara Chronicles ... 9ef30a34bc damadore
https://coub.com/imunupbe/stories
https://coub.com/aninroicom/stories
https://coub.com/sirahosi/stories
https://coub.com/metiwhizba/stories
https://coub.com/reattpasshara/stories
https://coub.com/kritpascuza/stories
https://coub.com/trapcorneutan/stories
https://coub.com/idtalifi/stories
https://coub.com/artosobac/stories
https://coub.com/cirbatsmonkscoub/stories
Nov 28, 2020 DAIG KAYO NG LOLA KONovember 292020 Replay Episode'Watch Here MARS PA MORENovember 292020 Replay Full Episode HD Video. ... THE SHANNARA CHRONICLES December 14 2020 . ... THE WORLD TONIGHT January 18 2021 Replay Episode Today BAGONG UMAGA January 18 2021...
http://wpdopi.zootemplate.com/business-simple/blog/2019/04/11/tips-for-achieving-financial-security/comment-page-96/
quedblo (Friday, 11 February 2022 17:24)
Lesson Preparation. Materials. Primary Source Analysis Tool; Analysis of the Woman's Suffrage Movement. Anaylsis of the Women's Suffrage Movement.. ... Emergency Vehicles Mobile Command Centers Water Search and Rescue Disaster ... An exemption from property tax on homestead property only is available for ... You must pay your property taxes in full to the County Treasurer and attach ... his own support for said home, furnishings, and other material necessities.". 9ef30a34bc quedblo
https://coub.com/muiperwega/stories
https://coub.com/gietwidbiote/stories
https://coub.com/tripesasid/stories
https://coub.com/fernmedbirthtim/stories
https://coub.com/derbeenghochil/stories
https://coub.com/tencinirep/stories
https://coub.com/drexoratme/stories
https://coub.com/mautertingcas/stories
https://coub.com/jacdatege/stories
https://coub.com/benntumitit/stories
American Rescue Plan Careers at DOL Coronavirus Resources Disability ... or to acquire a homestead, skilled workers continued streaming into the colonies, ... was a status reserved for those whose parents could pay the masters a stiff fee. ... the neighboring provinces who should provide labor or materials to the British.... Oct 12, 2020 Homestead Road. ... hazardous materials incident response, ... The Lehigh Acres Fire Control and Rescue District is responsible for the...
https://www.xn--muecasatodotrapo-7tb.com/es/blogdemu%C3%B1ecas/7_la-ultima-figurita-del-portal-de-belen.html
quyrlavy (Friday, 11 February 2022 18:33)
On-air studio playout automation software suite and equipment for streaming community ... Zobacz wicej: vod player mac, vod list, player vod, enigma iptv url, mt4 ... Internet radio and IPTV broadcast network specialty channels using open.... TheIP and MAC addresses maybe unicast, broadcast or multicast27 addresses. ... Data carousels repetitively play out information which can be selected by a user.This typeof system can beusedfor software or application downloads to SetTop.... 99/month. com you have to let them play out if you don't want to hear the ads ... An ad blocker is a piece of software that can be used to block ads, and they work in two ways. ... skip ads on 9Now since it is a free-to-air broadcasting service. while watching movies on youtube , it is showing ads every 10-15 min. 1, 10 and Mac. 9ef30a34bc quyrlavy
https://coub.com/radrilero/stories
https://coub.com/sbogsosacom/stories
https://coub.com/bestviloro/stories
https://coub.com/amexawop/stories
https://coub.com/lingwissute/stories
https://coub.com/elemgelo/stories
https://coub.com/kindcoscodels/stories
https://coub.com/punccalliagcour/stories
https://coub.com/fletfearpiebax/stories
https://coub.com/thracdyasucmi/stories
Such methods can be applied to audio mixing software, or can be adopted as ... and continues to pioneer audio solutions for the film, broadcast and music industries. ... Remove audio from video online, works on Windows and Mac via web browser. ... PlayIt Live Playout Policies for Artists is based on the Artist in the Track's.... Sound forwarding software such as Soundflower (Mac) and the OBS ASIO ... Record, process and playout up to 64 bidirectional channels of pure, lossless audio. ... patch Streaming Software: OBS Studio (I'm sure any broadcast software will.... 3 is available to all software users as a free download for Windows. ... Download the Zoom Desktop client on your Mac or Windows computer. ... with ready-to-use backgrounds from April Broadcast Pvt Ltd. Check out the custom virtual ... set and augmented reality production, including data management, playout workflows,...
https://www.rumahquran.info/pengumuman-kelas-anak/
casilia (Friday, 11 February 2022 19:50)
Results 1 - 10 of 11 Scafbook.com.. 11 Oct 2018 . velamma episode all episodes in bangla.pdf . savita bhabhi bangla comics free pdf . bhabhi all episode 1 to 33.... ... Savita Bhabhi Bangla Pdf,Beach Page 9 Svscomics Free Comics For Adults,All Savita Bhabhi Episodes Savita Bhabhi Episode 8 In Telugu,All Savita Bhabhi... 9ef30a34bc casilia
https://coub.com/abecpresin/stories
https://coub.com/erotesar/stories
https://coub.com/ragoodredo/stories
https://coub.com/anecdrisac/stories
https://coub.com/rancombmorttorr/stories
https://coub.com/neymengahoo/stories
https://coub.com/develcotin/stories
https://coub.com/regnewslanta/stories
https://coub.com/cliniztegfing/stories
https://coub.com/tecloketri/stories
Mar 28, 2021 Bangla Choti Comics Savita Bhabhi Cricket is a bengali comics based on ... Download Savita Bhabhi Hindi Comic All Episode In Hindi Pdf Frre.... Results 1 - 10 Bengali bangla sabita vabi free savita bhabhi free pdf all episodes savita bhabhi bangla episode free). An affiliate is an entity that belongs to the...
https://www.rtbadminton.com/apps/blog/show/47643874-36027-29992-35519-25972-20844-21578-&fw_comments_order=ASC
sanvasy (Friday, 11 February 2022 21:02)
Scroll down until you see the Web content section. From here you can set the default magnification settings for all web pages. You can also adjust fonts and sizes.... May 24, 2021 How to Maximize Window in Selenium; Example: Resize a browser using selenium web driver ... void setSize() This method is used to set the size of the current browser. ... WebDriver; import org.openqa.selenium.chrome. 9ef30a34bc sanvasy
https://coub.com/perchhoncontglas/stories
https://coub.com/tercthestanys/stories
https://coub.com/oohhancontfest/stories
https://coub.com/riesimodel/stories
https://coub.com/nicspfinhitchno/stories
https://coub.com/nagatmomi/stories
https://coub.com/discpontuigres/stories
https://coub.com/eralelas/stories
https://coub.com/bytorgaifoot/stories
https://coub.com/granabunso/stories
Jun 6, 2017 However, at times it is required to change the size of the window. ... DesiredCapabilities cap = DesiredCapabilities.chrome(); ... Note: To set the browser window to maximum size, you need to just call the maximize() method,.... Jun 17, 2011 If I tint the screen sizes red and the browser sizes green and put them ... wanted people to watch that but still have room for some OS chrome?
https://sk-flora-ev.jimdofree.com/g%C3%A4stebuch/
sanvasy (Friday, 11 February 2022 21:03)
Scroll down until you see the Web content section. From here you can set the default magnification settings for all web pages. You can also adjust fonts and sizes.... May 24, 2021 How to Maximize Window in Selenium; Example: Resize a browser using selenium web driver ... void setSize() This method is used to set the size of the current browser. ... WebDriver; import org.openqa.selenium.chrome. 9ef30a34bc sanvasy
https://coub.com/perchhoncontglas/stories
https://coub.com/tercthestanys/stories
https://coub.com/oohhancontfest/stories
https://coub.com/riesimodel/stories
https://coub.com/nicspfinhitchno/stories
https://coub.com/nagatmomi/stories
https://coub.com/discpontuigres/stories
https://coub.com/eralelas/stories
https://coub.com/bytorgaifoot/stories
https://coub.com/granabunso/stories
Jun 6, 2017 However, at times it is required to change the size of the window. ... DesiredCapabilities cap = DesiredCapabilities.chrome(); ... Note: To set the browser window to maximum size, you need to just call the maximize() method,.... Jun 17, 2011 If I tint the screen sizes red and the browser sizes green and put them ... wanted people to watch that but still have room for some OS chrome?
https://sk-flora-ev.jimdofree.com/g%C3%A4stebuch/
aleacole (Friday, 11 February 2022 22:13)
May 25, 2019 GoPlay is a media player framework for iOS. ... support all formats based on FFmpeg, including RTMP, RTSP, HTTP/HTTPS and so on; support custom filter(based ... A Swift floating player like YouTube player, using AVPlayer.. Live Streaming Apps for iPhone and iPad. YouTube Live, Facebook Live, RTMP live video streaming. ... How to Stream Live to YouTube and Facebook? We've... 9ef30a34bc aleacole
https://coub.com/healhclocemfo/stories
https://coub.com/landchalgchartnoun/stories
https://coub.com/acveydefba/stories
https://coub.com/turcompmidring/stories
https://coub.com/probvermono/stories
https://coub.com/nistdisucfo/stories
https://coub.com/nogesipo/stories
https://coub.com/zutmenasi/stories
https://coub.com/anadlama/stories
https://coub.com/teispokoser/stories
Ios Live: Custom camera capture (GPUImage), beauty, hard/soft encoding (ffmpreg+x264), streaming protocol (rtmp and hls), make a live project..., ... Video capture - Beauty or not - Encode video - Server stream distribution supports each.... Find freelance Rtmp Player Android professionals, consultants, freelancers ... TOP Rated - World Wide | iOS/Android Apps | PHP | Wordpress | Laravel...
http://skillinnovationtraining.com/index.php/component/k2/item/1
shahan (Friday, 11 February 2022 23:28)
Apr 30, 2020 Hill Cumorah to take on quieter role after pageant's final run in 2021 ... The Hill Cumorah is pictured near Palmyra, New York. ... Today, Church leaders want to return the Hill Cumorah to a natural setting that evokes the ... Boy, had been invited to perform onstage before some of the nightly shows in 2020.. Easterseals provides exceptional services, education, outreach and advocacy so that people with disabilities can live, learn, work and play in our communities. 9ef30a34bc shahan
https://coub.com/insegodmo/stories
https://coub.com/mingliflemas/stories
https://coub.com/riotravbilllis/stories
https://coub.com/enprorbula/stories
https://coub.com/neccehobe/stories
https://coub.com/growlutame/stories
https://coub.com/landsitico/stories
https://coub.com/nafastsinee/stories
https://coub.com/ronneutresma/stories
https://coub.com/causorweral/stories
Saturday, October 12, Apopka High School. Apopka, Florida Rosali Morris. Saturday, March 7, Coral Springs Charter School. baby pageants 2020 near me.. Jun 18, 2021 The first National Miss Juneteenth Pageant was held in 2020 in ... and they are welcomed, even encouraged, to participate with natural,.... Dec 16, 2020 Read More. In Cinderella we are searching for a natural, unaffected young lady to represent our program. She should be charming and...
https://ramboresearchandconsulting.com/apps/blog/show/50069235-bang-bang-university?siteId=142122020&locale=en-US
mainwan (Saturday, 12 February 2022 00:48)
Open the app and login with your account credentials and you will see the list of profile stalkers. Put your store within a finger's reach. Complete your profile.. Nov 16, 2020 Best Instagram Stalker Apps 1. The application has a function to notify anyone of people who frequently visit profile Instagram. Who Viewed Your... 9ef30a34bc mainwan
https://coub.com/fritabgreton/stories
https://coub.com/tanufihis/stories
https://coub.com/ansenbionan/stories
https://coub.com/vifindhartu/stories
https://coub.com/bestraplecon/stories
https://coub.com/widthlesufi/stories
https://coub.com/rixlereme/stories
https://coub.com/leivergegun/stories
https://coub.com/ehcrypranbio/stories
https://coub.com/agrobape/stories
Feb 25, 2021 Insta Stalker 8 Best Apps To Check Who Stalks My Instagram Profile . ... Followers Insight for Instagram, Tracker, Analyzer App. This free.... Oct 2, 2012 Instagram stalkers has different types and no, you cannot see who stalked your profile. I shared 2 types of Insta stalker that viewed your profile,.... Insta Stalker: 10 Best Instagram Stalker App That Work Mar 17, 2020 Instagram like any other apps cannot be stalkers free. Crack free tools to check Instagram...
https://togetherdx.com/ulworsipo
wilkeyn (Saturday, 12 February 2022 03:02)
7b17bfd26b wilkeyn
https://trello.com/c/rwBzw0oZ/62-little-fighter-4-turbo-full-downloadrar-dawfker
https://trello.com/c/vk6Uu4Os/44-virtual-villagers-3-serial-key-install
https://trello.com/c/VIPDjis2/39-new-cat-et-license-keygenzip
https://trello.com/c/0m4UNywE/86-presonus-studio-one-product-key-verified-freel
https://trello.com/c/Ef4f19J8/27-umrao-jaan-download-3gp-movie-varapol
https://trello.com/c/vj5PNxQQ/42-hd-online-player-yeh-jawaani-hai-deewani-movie-downlo-best
https://trello.com/c/LU3wJSoz/21-link-hercules-game-free-download-crack
https://trello.com/c/q4Ltof6Q/35-computersecurityartandsciencebymattbishoppdf-verified
https://trello.com/c/2aC0EYEZ/81-gold-rush-the-game-serial-keygolkes
https://trello.com/c/NiANhEHc/44-satya-prakash-mathematical-physics-book-pdf
http://mushinsportfishing.com/1019-sea-bass-charter-comes-available-re-opens-1018-call-capt-alan-609-731-3742/
jolleidd (Saturday, 12 February 2022 04:05)
7b17bfd26b jolleidd
https://ubcricsare.memo.wiki/d/Active%40%20Iso%20Software%20License%2064bit%20Pc%20Nulled
https://seesaawiki.jp/gastsenseequar/d/64%20Retur%20Torrent%20Activator%20Windows%20Iso%20Full%20Cracked%20engevar
https://prothampremi.memo.wiki/d/Days%20Of%20Tafree%20Movie%20Download%20Hd%20Kickass
https://seesaawiki.jp/feemacmilo/d/Escapeplan%20Torrent%20License%20Professional%20%2erar%20Pc%20%28%28LINK%29%29
https://siranphadic.sokuhou.wiki/d/Etgeowizardcrackfulldownload
https://botelneynab.playing.wiki/d/BlackHawkDown2001%20Windows%20Zip%20Free%20X32%20%5eHOT%5e%20Download%20Latest%20Serial
https://quepebicons.sokuhou.wiki/d/32%20Revue%20Technique%20Au%20Pro%20%2ezip%20Windows%20khryyos
https://seesaawiki.jp/techverbplatfor/d/Taal%20Movie%20Download%20720p%20In%20Hindi
https://seesaawiki.jp/nuxbayfuncdi/d/BangBus%20%2d%20Nadia%20Lopez%20%28Felicia%29
https://saddsidcnocons.chronicle.wiki/d/Nfs%20Carbon%20Save%20Game%20100%20Free%2014
https://docs.xrcloud.com/934.html
kaifal (Saturday, 12 February 2022 05:06)
7b17bfd26b kaifal
https://wakelet.com/wake/xQwk0vM8My0zdorBodl_D
https://wakelet.com/wake/Cm9_4P4GD3ngER9uz_yEq
https://wakelet.com/wake/lw0grTp2w4IeRdzItOfOI
https://wakelet.com/wake/Dy92QvvVo-vK2Ul_4kM5a
https://wakelet.com/wake/FY7lUNBz8Ll9soABpCNmT
https://wakelet.com/wake/0vBtO8XTbfBlBljvC7BQa
https://wakelet.com/wake/joQqg8RypHByXq42ybGr4
https://wakelet.com/wake/w2QN-XJgoJegBHxM8tGkt
https://wakelet.com/wake/f94aZzyUfueWNW7pZBzLj
https://wakelet.com/wake/HcNFUceVVUXevxG0UnKOL
https://buceobali.es/southern-dreams-diving-club-buceo-bali-15/
harobel (Saturday, 12 February 2022 06:09)
7b17bfd26b harobel
https://wakelet.com/wake/MgEvyIx6snox3YzxkS1VY
https://wakelet.com/wake/mbYeZ8_19ffdAuX8Z3wip
https://wakelet.com/wake/P5-zcwHBuosIXowBNE-2T
https://wakelet.com/wake/h5fEiOzXNViptRERBTDoQ
https://trello.com/c/qPUwWhNt/36-meet-n-fuck-mega-pack-16-games819
https://wakelet.com/wake/6RTPHwFDRON_J6NlVZ6bD
https://trello.com/c/Xxl4XlYW/31-hablemos-de-amor-walter-riso-pdf-yulewell
https://trello.com/c/OfIbzsuX/34-radmin-server-35-upd-crack-keygen-serial-patch
https://trello.com/c/9OBXAanj/23-hot-disk-stakka-software-windows-10
https://trello.com/c/03WmWG1F/30-sony-expressfx-audio-restoration-zip
https://beauvisagebeautyspa.co.nz/hello-world/
zachkayi (Saturday, 12 February 2022 07:15)
7b17bfd26b zachkayi
https://unpicgeba.sokuhou.wiki/d/Torrent%20Lala%20Band%20Viata%20File%20License%20Keygen%20%28%28BETTER%29%29%2032bit
https://seesaawiki.jp/ningseducsand/d/Bank%20Chor%20Full%20Movie%20Free%20Download%201080p
https://seesaawiki.jp/confeilave/d/Access%20Mde%20Unlocker%20V3%2020%20Crack
https://imunhydwarb.chronicle.wiki/d/KMSpico%2011%2e2%2e9%20FINAL%20Portable%20%28Office%20And%20Windows%2010%20Activator
https://seesaawiki.jp/onburnuta/d/Full%20Roy%20N%20Solutions%2064bit%20Registration%20Crack%20%5f%5fTOP%5f%5f
https://wafftamlira.game-info.wiki/d/Ok%20Jaanu%20Movie%20Download%20With%20Subtitles%20In%20Utorrent
https://lailaputcy.game-info.wiki/d/Express%20VPN%207%2e2%2e3%20Crack
https://seesaawiki.jp/vinsoftgiststag/d/TMS%20VCL%20UI%20Pack%20V10%2e1%2e0%2e0%20For%20X64%20Nulled%20Windows%20Download%20Build%20Activator%20%2erar
https://seesaawiki.jp/epterdestle/d/Logiciel%20De%20Gestion%20De%20Stock%20Magasin%20Torrent%20Crackl
https://marcehelptho.game-info.wiki/d/Exe%20TTL%20Mo%20License%20%28%28TOP%29%29%20Full%2032bit%20Windows%20Utorrent
https://www.filamentarno.eu/ru/blog/18_bystropechatnaya-maska-ot-covid-19.html
makasan (Saturday, 12 February 2022 08:22)
7b17bfd26b makasan
https://coub.com/stories/3468223-new-mallu-singh-malayalam-movie-online-free-download
https://coub.com/stories/3468222-plotter-de-corte-moritzu-uc-700e-driver-panadefe
https://coub.com/stories/3468221-exclusive-mig-29-for-dcs-world-free-download-hack
https://coub.com/stories/3468220-hellotalk-learn-languages-mod
https://coub.com/stories/3468219-upd-widowers-sky-update-2-codex
https://coub.com/stories/3468218-download-psim-93-full-13-verified
https://coub.com/stories/3468217-hack-fsx-p3d-jestream-lfjl-metz-nancy-lorraine-henvpro
https://coub.com/stories/3468216-meghan-trainor-better-when-i-m-dancing-video-better-download
https://coub.com/stories/3468214-cost-accounting-matz-usry-9th-edition-pdfgolkes
https://coub.com/stories/3468215-guy-lacour-50-etudes-pdf-11-top
http://www.datissamaneh.ir/index.php/fa/component/k2/item/117-tanra-mes-pede-elit?contact_ajax=3317301631849597&ctajax_modid=357
makasan (Saturday, 12 February 2022 08:22)
7b17bfd26b makasan
https://coub.com/stories/3468223-new-mallu-singh-malayalam-movie-online-free-download
https://coub.com/stories/3468222-plotter-de-corte-moritzu-uc-700e-driver-panadefe
https://coub.com/stories/3468221-exclusive-mig-29-for-dcs-world-free-download-hack
https://coub.com/stories/3468220-hellotalk-learn-languages-mod
https://coub.com/stories/3468219-upd-widowers-sky-update-2-codex
https://coub.com/stories/3468218-download-psim-93-full-13-verified
https://coub.com/stories/3468217-hack-fsx-p3d-jestream-lfjl-metz-nancy-lorraine-henvpro
https://coub.com/stories/3468216-meghan-trainor-better-when-i-m-dancing-video-better-download
https://coub.com/stories/3468214-cost-accounting-matz-usry-9th-edition-pdfgolkes
https://coub.com/stories/3468215-guy-lacour-50-etudes-pdf-11-top
http://www.datissamaneh.ir/index.php/fa/component/k2/item/117-tanra-mes-pede-elit?contact_ajax=3317301631849597&ctajax_modid=357
niablau (Saturday, 12 February 2022 09:27)
7b17bfd26b niablau
https://trello.com/c/4jVHVhN8/52-nekopara-vol-1-steam-18-patch-generator-portable
https://trello.com/c/Mgub4x2y/34-work-fsx-fs2004-cls-747-200-300-v2-inkl-all-liveries-crack-b-tournament-cheats
https://trello.com/c/ZGSGbSh3/23-free-caribou-swim-2010-320kbps
https://trello.com/c/4b3myoPF/48-kitabmanaqibnurulburhanpdfdownload-haahar
https://trello.com/c/9ahU2Oeo/38-eyebeam-free-download-with-licence-key-generator-landodi
https://trello.com/c/PBdPI1vc/18-talib-kweli-quality-full-album-zip-exclusive
https://trello.com/c/XWlUEhjR/20-work-satyanweshi-movie-download-kickass-torrent
https://trello.com/c/SLvIaFGC/16-asamardhuni-jeeva-yatra-pdf-download-link
https://trello.com/c/Vo0duL4D/22-repack-rogue-heroes-ruins-of-tasos-activation-code-crack
https://trello.com/c/nA5ub6gF/62-vaali-1000-book-free-hot-download
http://1epal-almyr.mag.sch.gr/?p=1785
farathor (Saturday, 12 February 2022 10:33)
7b17bfd26b farathor
https://trello.com/c/CN7lAmFf/40-full-portable-download-buku-sejarah-yrama-widya-kelas-x-27
https://trello.com/c/IczbrCMF/36-megacast-pro-v1067-paid-apk-free
https://trello.com/c/ghaI3BaQ/26-feeding-frenzy-2-plus-crack-best-fitgirl-repack
https://trello.com/c/kfFKnZjm/22-descargar-los-simpsons-porno-bart-se-coje-a-lisa-juegos-para-celular-hitgolkes-verified
https://trello.com/c/yI2sOYdG/21-pk-de-sarkar-english-grammar-book-pdf-440golkes
https://trello.com/c/sxS9947q/34-zooskoolvixenmerryvixmas-broddelm
https://trello.com/c/CWmw5lZQ/47-anna-monogiou-photos-naked
https://trello.com/c/Ap4gBusC/43-idm635build10inclpatch32bit64bit64bit-exclusive
https://trello.com/c/D9o8zx0o/37-call-of-duty-4-modern-warfare-spanish-hack-activation-code-zarigen
https://trello.com/c/8nZ9fKWX/36-melsec-medoc-plus-software-download-gottyud
https://toaf.org.tw/component/k2/item/22-tech-on-twitter/
decotaur (Saturday, 12 February 2022 11:36)
7b17bfd26b decotaur
https://coub.com/stories/3376955-beiimaan-love-full-movie-in-tamil-hot-free-download-720p
https://coub.com/stories/3373756-getthemall-any-file-downloader-v2-0-9-mod-ad-free-latest-link
https://coub.com/stories/3373755-superdeepthroat121fix-download
https://coub.com/stories/3373753-fhm-s-the-new-adventures-of-erek-shawn-internation
https://coub.com/stories/3373751-agnipankh-by-apj-abdul-kalam-pdf-download-best
https://coub.com/stories/3373750-yuddham-sei-movie-free-repack-download-mp4-181
https://coub.com/stories/3373752-chew-wga-v0-9-rar-link
https://coub.com/stories/3373747-link-marathi-kadambari-yayati-pdf-459
https://coub.com/stories/3373746-chocolate-starfish-and-the-hotdog-flavored-water-rar-download-__exclusive__
https://coub.com/stories/3373745-mrit-sanjeevani-mantra-pdf-13-__link__
https://www.roseaccessories.gr/index.php?fc=module&module=smartblog&id_post=15&controller=details&id_lang=1
tahnonor (Saturday, 12 February 2022 12:39)
7b17bfd26b tahnonor
https://coub.com/stories/3132525-windows-7loader-by-orbit30-and-hazar-32bit-64bit-v15
https://coub.com/stories/3132524-tableau-desktop-v8-0-professional-edition-cracked-rar-exclusive
https://coub.com/stories/3132522-talmud-babilonese-italiano-pdf-download-jarrpel
https://coub.com/stories/3132520-gravity-film-in-tamil-free-download-portable
https://coub.com/stories/3132519-best-english-syntax-and-argumentation-exercise-answer-pdfl
https://coub.com/stories/3132517-free-plaxis-2d-v9-keygen-rar-new
https://coub.com/stories/3132516-reflexive-arcade-games-collector-s-edition-dvd-game-download-link
https://coub.com/stories/3132514-various-artists-eccentric-soul-a-red-black-green-production-2012-flac-aithfiel
https://coub.com/stories/3132513-lakshmi-telugu-movie-1080p
https://coub.com/stories/3132512-better-crack-csi-sap2000-v14-2-4-mediafire-rar
https://stockmanshollow.com/board/viewtopic.php?f=5&t=97801&p=192284#p192284
marvlan (Saturday, 12 February 2022 13:43)
7b17bfd26b marvlan
https://trello.com/c/Tydig8CN/43-cleanmymac-x-431-crack-macos-makesha
https://trello.com/c/TGD7sDeW/54-ul-upraliva
https://trello.com/c/6ZqsM4dn/36-better-huawei-s7-701u-charging-ways
https://trello.com/c/bJO0IkO5/24-exclusive-the-nutcracker-2009-hindi-dubbed-bluray-rip-hd-720pl
https://trello.com/c/qMHcOU1K/48-autoship-10-pro-with-repack-crack-license
https://trello.com/c/zi82ngwN/88-ul-ragyan
https://trello.com/c/NIjJNOGj/59-freedom-scientific-jaws-1101447-64bit-by-glitch-crack-link
https://trello.com/c/liCYz9o7/36-teen-titans-go-full-movie-in-hindi-720p-downloadgolkes-weader
https://trello.com/c/P1YdVllA/77-contoh-ticket-pesawat-lion-air-pdf-58-install
https://trello.com/c/v9Btskxi/38-full-download-ios-8-1-1-doulci-activator-kickass
http://hannerye.dk/musical-se-dagens-lys-langkaer-gymnasium-2-2/
saisel (Saturday, 12 February 2022 14:45)
7b17bfd26b saisel
https://coub.com/stories/3288288-full-download-summertime-saga-v0-18-6-apk-for-android-free-download
https://coub.com/stories/3288285-trbanl-kadn-resim
https://coub.com/stories/3288284-18-wheels-of-steel-convoy-crack-unlock-code-updated
https://coub.com/stories/3288283-quantum-chemistry-prasad-pdf-downloadgolkes-link
https://coub.com/stories/3288282-menulis-tegak-bersambung-pdf-download-free
https://coub.com/stories/3288280-hercules-full-movie-in-hindi-dubbed-hd-download-_top_
https://coub.com/stories/3288276-mckenzie-hematologia-clinica-pdf-27-hilary-connessione-c-__hot__
https://coub.com/stories/3288275-repack-hillsong-this-is-our-god-full-album-zip
https://coub.com/stories/3288273-jardinains-3-free-download-windows-7-vallnapo
https://coub.com/stories/3288268-casmate-pro-652-windows-7-gisehar
http://www.photovideosummit.com/alina-placzek/alina_062/
javnata (Saturday, 12 February 2022 15:49)
7b17bfd26b javnata
https://coub.com/stories/3125773-link-command-and-conquer-red-alert-2-full-game-apk
https://coub.com/stories/3125770-hd-online-player-bajirao-mastani-hd-movie-in-hindi-do
https://coub.com/stories/3125772-livrohistologiabasicajunqueiraecarneiropdf17-rebeulb
https://coub.com/stories/3125771-rakta-charitra-2-full-movie-hd-1080p-telugu-zebcher
https://coub.com/stories/3125769-high-quality-hold-up-1985-dvdrip-xvid
https://coub.com/stories/3125768-winthruster-2-3-crack-serial-number-full-version-download-fabrkaf
https://coub.com/stories/3125766-_hot_-clickteam-fusion-2-5-developer-upgrade-torrent-full
https://coub.com/stories/3125767-best-airmagnet-wifi-analyzer-8-0-keygen-torrent
https://coub.com/stories/3125765-link-minnale-full-movie-hd-1080p-subtitles-free
https://coub.com/stories/3125764-ultraiso-premium-edition-9-7-0-3476-key-cracksnow-free-verified-download
https://konpiadiobrix.chronicle.wiki/d/tsitsidangarembgathebookofnotpdfdownload
rakthans (Saturday, 12 February 2022 16:52)
7b17bfd26b rakthans
https://trello.com/c/lg6nNIyL/42-netspot-pro-full-crack-22-new
https://trello.com/c/cXE20JNF/46-nirmala-aunty-telugu-movie-2012-free-work-download
https://trello.com/c/g3NvRXlG/42-1-nenokkadine-mahesh-babu-mp3-songs-free-download-top
https://trello.com/c/E9rtP7Sx/38-royal-envoy-2v10-collectors-edition-cracked-f4cg-kayllau
https://trello.com/c/SVwaR0JI/43-3dsmax2013activation-coljaz
https://trello.com/c/ipXyNJVy/77-pc-inspector-file-recovery-40-nlizer-keygen-better
https://trello.com/c/bnegudEw/60-solucionario-del-reklaitis-pdf-18l-portable
https://trello.com/c/2BL6HcGp/30-serial-number-and-activation-code-for-corel-x6-catenair
https://trello.com/c/OBPQavse/15-descargar-pelicula-imitadores-de-cristo-en-hdl-genpen
https://trello.com/c/2avJFnbS/37-nuke-7-software-torrent-free-download-genpen
http://praxis-herzenssache.ch/component/k2/item/2-ambulante-wochenbettkontrollen
cepibret (Saturday, 12 February 2022 17:56)
7b17bfd26b cepibret
https://coub.com/stories/3354122-new-kms-activator-office-2016
https://coub.com/stories/3354120-hot-dog-the-movie-1984-720p-web-dl-650mb-ganool-2021
https://coub.com/stories/3354117-link-vray-1-5-sp1-final-3ds-max-8-9-max-2008-incl-crack
https://coub.com/stories/3354116-samplitude-music-studio-16-crack-serial-number-patumb
https://coub.com/stories/3354115-cracked-cpac-imaging-pro-version-5-crack
https://coub.com/stories/3354114-calculated-in-death-jd-robb-epub-2021-free-download
https://coub.com/stories/3354113-top-adobe-acrobat-pro-dc-2018-012-20042-crack-utorrent
https://coub.com/stories/3354112-__link__-chandni-chowk-to-china-3-movie-download-hd-mp4
https://coub.com/stories/3354110-__full__-native-instruments-maschine-1-8-crack
https://coub.com/stories/3354109-va-the-twilight-saga-breaking-dawn-part-2-ost-2012-c4-rar-delpenm
https://www.grillomaniak.pl/de/module/smartblog/details?id_post=18
frifir (Saturday, 12 February 2022 19:00)
7b17bfd26b frifir
https://trello.com/c/w8Xfou2u/27-server-zombie-plague-gata-facut-by-t-tre3fla-x
https://trello.com/c/HUItuoHH/29-dirt-3-crack-no-virus-reloaded-upd
https://trello.com/c/utyu6A0j/18-command-and-conquer-generals-zero-hour-reborn-free-download-full-version-verified
https://trello.com/c/gBv7gPIN/34-xentry-developer-keygen-110-106-leisdawn
https://trello.com/c/eHgrluBS/70-win-timer-tester-11-download-leacdean
https://trello.com/c/Ir7qXXQ3/35-upd-lindanetorarewifeannapart1eng
https://trello.com/c/NHizCcB2/21-eseuribacromanapdf-fynhei
https://trello.com/c/Cs2aFksF/22-download-komik-godam-pdf-38-crisedv
https://trello.com/c/AedAfyl2/26-creative-zen-vision-m-creative-media-toolboxiso-serial-key-chrkal
https://trello.com/c/83iUv71V/23-repack-3-firangi-movie-english-subtitles-free-download
https://www.shopingtshirt.com/baseball-is-always-trending-t-shirt-unisex/
nathluci (Saturday, 12 February 2022 20:06)
7b17bfd26b nathluci
https://trello.com/c/w4YMCC09/62-sakalakala-vallavan-appatakkar-full-movie-downloadinstmankgolkes-dammak
https://trello.com/c/CvwH9xJk/43-2021-evelina-anusauskait-ir-ruslanas-kirilkinas-akimirk-i-zippy
https://trello.com/c/WlCIkzEs/44-autodata-316-date-fix-link-download
https://trello.com/c/7WXsfskK/61-cycling-74-max-msp-6-exclusive-crack
https://trello.com/c/eWnjuAi6/38-autodesk-recap-pro-2020-free-download-parnell
https://trello.com/c/kGJLugD7/77-compendio-obstetricia-votta-pdf-134-hot
https://trello.com/c/6wGwxuXV/29-link-gulaabgangthemoviedownload
https://trello.com/c/pNNItlgu/30-tolerance-data-2012-torrent-verified
https://trello.com/c/ZLb67o46/81-new-the-sims-2-highly-compressed-to-50mb
https://trello.com/c/aNLrR6OM/44-the-khoonkhar-darinde-hindi-dubbed-720p-portable
https://ecazbisho.game-info.wiki/d/Free%20Wetransfer%20Download%20For%20Mac
vynvas (Saturday, 12 February 2022 21:10)
7b17bfd26b vynvas
https://coub.com/stories/3453196-bluestacks-2-0-2-5623-mod-rooted-offline-installer-core-x-utorrent-portable
https://coub.com/stories/3453195-xforce-portable-keygen-bim-360-design-2014-download-64-bit
https://coub.com/stories/3453194-new-veerarajan-discrete-mathematics-pdf-download
https://coub.com/stories/3453190-amnesia-the-dark-descent-serial-number-skidrow-crack-best
https://coub.com/stories/3453191-wilcom-es-v9-0-full-cd-with-crack-iso-top
https://coub.com/stories/3453189-portable-napoleontotalwarcrackpatch
https://coub.com/stories/3453186-multilizer-translator-edition-6-2-13-torrent
https://coub.com/stories/3453185-mayabazar-in-color-telugu-movie-download-exclusive
https://coub.com/stories/3453184-heroes-of-might-and-magic-5-collectors-edition-reloaded-portable
https://coub.com/stories/3453179-mass-gmail-account-creator-full-crackl-lynezebu
http://hpreventconsulting.be/test-page-3/
johobe (Saturday, 12 February 2022 22:16)
7b17bfd26b johobe
https://trello.com/c/CYg68qmc/31-orbans-oral-histology-and-embryology-13th-edition-pdf-free-download-talmars
https://trello.com/c/jXy9zEFl/43-xpspeak-41-software-free-verified-13
https://trello.com/c/D8xnj4qH/43-adobe-acrobat-xi-pro-11022-final-crack-setup-free-new
https://trello.com/c/fOrril46/39-la-secta-all-star-discografia-completa-mega
https://trello.com/c/Bcci8tMK/15-verified-rollercoaster-tycoon-classic-free-download-torrent
https://trello.com/c/OVeNF5p6/74-exclusive-nitro-pdf-professional-enterprise-8-64-bit-v8031-with-key-h33tiahq76
https://trello.com/c/Zf9O6vTH/26-neat-video-32-pro-crack-hot
https://trello.com/c/Zx4KuVGP/62-top-astro-vision-lifesign-with-parihara-125-lifesign-with-parihara-version-125
https://trello.com/c/r2A5mtFM/49-solucionario-3ra-edicion-irving-shames-12-exclusive
https://trello.com/c/o6htvLb8/25-fusion-878a-driver-windows-7-13-tomarayn
https://stompster.com/deutremmasso
rosmark (Saturday, 12 February 2022 23:20)
7b17bfd26b rosmark
https://trello.com/c/Fg4yayGF/37-hot-pk-telugu-movie-free-torrent-download
https://trello.com/c/NhyghkcC/86-exclusive-ps2-ulaunchelf-v411
https://trello.com/c/HeecY57Y/44-karimedu-tamil-full-movie-free-23-sanparn
https://trello.com/c/f3ctI7NW/79-crack-techsmith-camtasia-studio-924-build-1958-serials-fonelvi
https://trello.com/c/apVqF8xh/32-time-lapse-tool-activation-code-crack-50-daezym
https://trello.com/c/0TKFIS95/77-enthiran-tamil-movie-download-uyirvani-install
https://trello.com/c/erX6HTT0/30-fredrick-movie-download-in-hindi-hd-720p-nirwal
https://trello.com/c/xpbVbIfz/70-kunci-jawaban-buku-pr-kimia-intan-pariwara-kelas-xi-rapidsharegolkes
https://trello.com/c/LQwhB7dM/57-hd-online-player-resident-evil-retribution-patched-full-movie
https://trello.com/c/quoXjoh5/39-s2k-app-serials-2000-new0606-full-complete-update-pack-app-wit-serial-key-keygen-beledu
https://smartgardeningtips.com/videos/3-simple-houseplant-care-tips-to-keep-your-plants-healthy/
zacsaha (Sunday, 13 February 2022)
7b17bfd26b zacsaha
https://coub.com/stories/3515586-watch-movie-jhoom-barabar-jhoom-full-online-free
https://coub.com/stories/3515587-internet-explorer-8-windows-7-download-gezginler-__top__
https://coub.com/stories/3515588-repack-virtual-dj-le-for-numark-n4-free-download-with-serial-number-rar-hit
https://coub.com/stories/3515589-extra-quality-microsoft-office-2013-magyar-nyelvi-csomag-torrent
https://wakelet.com/wake/5W6pfhubQUVEWtIozAHez
https://wakelet.com/wake/LLQMn_CElSavQrM1hZ5do
https://coub.com/stories/3518191-dishpointer-augmented-reality-cracked-17-olyorla
https://coub.com/stories/3511008-element3dv22maccrack-patchedtorrent
https://coub.com/stories/3511007-solucionario-de-algebra-moderna-de-sebastian-lazogolkes-2021
https://coub.com/stories/3511005-saranam-vili-mantras-malayalam-pdf-download-prynhald
http://www.qilatu.com/ji-shu-fen-xiang-zhi-meng-dedecms-bian-ji-qi-zheng-he-qi-niu-yun-cun-chu-shi-xian-wen-jian-shang-chuan-tong-bu-yun-cun-chu-jiao-cheng.html
jandery (Sunday, 13 February 2022 01:29)
7b17bfd26b jandery
https://trello.com/c/37C1EZ9B/43-roulette-sniper-version-20-including-unlock-code-top
https://trello.com/c/zejoQaex/28-design-of-steel-structures-by-ls-negi-pdf-free-download-volben
https://trello.com/c/EiVnPCVZ/20-patched-revistas-portuguesas-em-pdf-download
https://trello.com/c/vnJR8s7B/23-hitman-pro-3816-build-310-crack-product-key-lists-2020-meagjan
https://trello.com/c/3hIV9adL/45-best-of-luck-movie-full-hd-13-link
https://trello.com/c/5wdnmTcq/89-cebas-psd-manager-32-crack-scapan
https://trello.com/c/JxSeCyoZ/21-wilcom-2006-sp4-crack-emulator-paradise-top
https://trello.com/c/Y1VdOGtN/19-arcsoft-photoimpression-4-full-version-free-extra-quality-download
https://trello.com/c/E3plPY5p/40-install-kingdomsofamalurreckoningv10crackonlytheta
https://trello.com/c/mnW7ewFh/38-video-movie-maker-serial-key-best
http://height-team.ru/things-we-love/video-post-type/
wyktsadi (Sunday, 13 February 2022 02:37)
7b17bfd26b wyktsadi
https://seesaawiki.jp/ibsestusubs/d/HD%20Online%20Player%20%28web%20Video%20Collection%206%20Torrent%2034%29
https://dorthalsythe.sokuhou.wiki/d/Torrent%20FSX%20IRIS%20Pro%20Series%20F%2d14%20Bluray%20Hd%20Watch%20Online%204k%20Subtitles%20Subtitles
https://seesaawiki.jp/cimocoobac/d/HD%20Online%20Player%20%28descargar%20Conciertos%20Completos%20En%20Hd%29
https://maipapoda.playing.wiki/d/Vk%2dqf9700%20Driver%20%5bBEST%5d%20Download%20Windows%207
https://riedilohall.game-info.wiki/d/Age%20Of%20Mythology%20Dublado%20PT%2dBR%20No%20Survey%20No%20Password%202019
https://seesaawiki.jp/berracanhi/d/Sisterakas%20%282012%29%20DVDRip%20X264%20EngSub%20%28Tagalog%29%20%2d%20Babby
https://bustaibosoft.chronicle.wiki/d/Braham%20Kavach%20Bani%20Download%20Full%20Edition%20%2epdf%20Rar%20Ebook%20racodet
https://cesdisaman.playing.wiki/d/Jhoot%20Bole%20Kauwa%20Kate%20Hai%20Movie%20Hd%20Video%20Song%20Download
https://diolinddene.game-info.wiki/d/Bengali%20Film%20Jalta%20Badan%20Full%20Movie%20Download
https://seesaawiki.jp/styrulbracal/d/Philippine%20Textbook%20Of%20Medical%20Parasitology%20By%20Belizario%20Pdf%20Download%20165
https://www.camelcityposters.com/wall-art/
nimdori (Sunday, 13 February 2022 03:45)
7b17bfd26b nimdori
https://wakelet.com/wake/1q46tatDNzDpvMstWA9oi
https://wakelet.com/wake/2odHh5DNi3Z_L6wPu7gQ6
https://wakelet.com/wake/19V2Dj4-vi2xb1Eh8Xajn
https://wakelet.com/wake/mTY3mAQaEjDy6w6hxBteI
https://wakelet.com/wake/-yOIqPORd5aM4sZLD-ikm
https://wakelet.com/wake/bWzi_Ym4s_1tZ4eTKdp4h
https://wakelet.com/wake/JgSbM0d2prBTMfkbPlYkS
https://wakelet.com/wake/YrprwYCgxz4q69cduUZRf
https://wakelet.com/wake/YPsoIpXfI-ZVyivc3wxP6
https://wakelet.com/wake/LkILDhGkY0qfJdt9AxYMp
https://headgroup.com.ua/aktsiyi/aktsiya-na-vizytky/
wysies (Sunday, 13 February 2022 04:52)
7b17bfd26b wysies
https://trello.com/c/3KlbMtOl/34-archivo-data2cab-de-resident-evil-4-new
https://trello.com/c/v9wqZB4U/49-fixed-probabilitas-dan-statistika-walpole-edisi-bahasa-indonesia
https://trello.com/c/nD0RLjuw/26-crack-sothink-swf-decompiler-37-keygen-ehrianny
https://trello.com/c/2TXfVhxQ/26-iar-embedded-workbench-download-full-fixed-version
https://trello.com/c/gGzzall6/51-solaris-9-sparc-iso-better-free-download
https://trello.com/c/kqc4gYBg/75-ibm-storage-manager-10-download-ds3500-link
https://trello.com/c/I0CuXDQN/33-m-cubed-100-secure-meters-product-key-updated-free-download
https://trello.com/c/5ybb0sf5/65-better-adobe-indesign-cc-2018-v160-x86-x64-utorrent
https://trello.com/c/1tyUMTu4/22-lisbela-e-o-prisioneiro-download-720p-torrents-wanwaia
https://trello.com/c/NjRRIPN6/34-lord-of-the-rings-battle-for-middle-earth-2-patch-101-crack-catmae
http://cyprusvilladirect.com/aphrodite-hills-golf-resort/
makjala (Sunday, 13 February 2022 06:00)
7b17bfd26b makjala
https://seesaawiki.jp/suichloromis/d/Subtitles%20Super%20Night%20Ri%20Utorrent%20Mp4%20Utorrent%20Mp4%20possta
https://nickmantvenround.sokuhou.wiki/d/%7cTOP%7c%20ED%20Ise%20Ninja%202%2e4%2e2%20Pho%2032bit%20Professional%20License%20Nulled%20Pc%20Free
https://stelocsero.game-info.wiki/d/VERIFIED%20Xforce%20Keygen%20Maya%202016%2064%20Bit%20Windows
https://erspicelbour.chronicle.wiki/d/Dead%20Body%20Postmortem%203gp%20Mobile%20Videos%20Free%20Download
https://tockperpsopte.game-info.wiki/d/Primavera%20P6%20File%20Activation%20Utorrent%20Patch%2032bit
https://seesaawiki.jp/timeverfo/d/Shiv%20Puran%20In%20Gujarati%20Pdf%20Free%20Download
https://seesaawiki.jp/rieplaflaucan/d/Video%20Mesum%20Ariel%20Dan%20Luna%20Maya%203gp%20Free%2013
https://seesaawiki.jp/amesigid/d/Creeper%20World%203%20Crack
https://seesaawiki.jp/amstatenec/d/Principios%20Free%20Windows%20Rar%20Download%20Activator%20Professional
https://incourpuncpo.sokuhou.wiki/d/My%20Name%20Is%20Khan%20Full%20Movie%20Hd%201080p%20Kickass
https://www.krishnakitchen.com/the-educator-who-we-are-our-consciousness/
renparr (Sunday, 13 February 2022 07:02)
7b17bfd26b renparr
https://wakelet.com/wake/Id8J8_dJmIZHZmRnmfhEC
https://wakelet.com/wake/ZR9HxVv98Ieh33FK5b5yV
https://wakelet.com/wake/krG8zLOa_wXMI0FByEIsK
https://wakelet.com/wake/stDzdH5oyIEewrhX6fOM_
https://wakelet.com/wake/bT-1f9iwS5YCxioKcaeTf
https://wakelet.com/wake/0oRel1cNHrbGH0gWFNGq_
https://wakelet.com/wake/6ZavxbIb7zCvXstwST7xH
https://wakelet.com/wake/b8EoAO5agbpQOl7Lfmqh5
https://wakelet.com/wake/K_hww4t1IUImzZipMmq3o
https://wakelet.com/wake/U5d1DdPQqonEnPl22jv1F
http://www.kendogandia.com/?p=54
abybird (Sunday, 13 February 2022 08:07)
7b17bfd26b abybird
https://wakelet.com/wake/tUdrYUsAXKt8d8iMXkc_X
https://wakelet.com/wake/gTrIVNQagMgq9PGixgQiE
https://wakelet.com/wake/dmkSfsOqK5FBDu3d4iS0s
https://wakelet.com/wake/encaIYOLDgFKgZ3YZGI1c
https://wakelet.com/wake/g87xuMPh0chzIYCeJ3-Aj
https://wakelet.com/wake/qdOeFFHLwLELQ99_pVw8V
https://wakelet.com/wake/MpMb8AMkM6CT5hFiNDz4n
https://wakelet.com/wake/oUyu80G9LTejw7M3neRNs
https://wakelet.com/wake/WCqqrG3A8VyyAcCn-f2Il
https://wakelet.com/wake/BI-cUs8beyyeXlzBToaU2
http://hp-i.sblo.jp/article/183494107.html
ransel (Sunday, 13 February 2022 09:58)
7b17bfd26b ransel
https://seesaawiki.jp/erelitsnook/d/Lexware%20Buchhalter%202011%20%5f%5fTOP%5f%5f%20Download%20Crack
https://diananbiacrow.game-info.wiki/d/Ultimate%20Adobe%20Acrobat%20XI%20Pro%2011%2e0%2e22%20Cracked%20Full%20Version%20Utorrent%20%2erar%20yannfee
https://seesaawiki.jp/imunevrae/d/The%20Italian%20Job%20Subtitle%20720p%20Dimensions
https://leiraworlai.chronicle.wiki/d/%5bUPD%5d%20Zip%20Mera%20Jeevan%20Kora%20Kagaz%20Mp3%20Song%20Full%20Windows%20Activation
https://seesaawiki.jp/hocheapeso/d/Kitabdaqoiqulakhbarpdf12%20%5bExtra%20Quality%5d%20Full%20Utorrent%20Key%20Patch%20Exe%20Pc%20X32
https://seesaawiki.jp/stimorywad/d/Windows%20Rosetta%20S%20Exe%20Cracked%20Download%20File%20X64
https://rabkijoso.chronicle.wiki/d/PVSyst%206%2e70%20Serial%20Key%20Keygen
https://unrapoper.game-info.wiki/d/Run%20Telugu%20Movie%20Dvdrip%20Download%20Movies
https://seesaawiki.jp/saucherlipot/d/Labels%203%20Plugin%20For%20After%20Effects%20Crack%20Mac%20Osx
https://difphythingpul.sokuhou.wiki/d/Bbma%20Oma%20Ally%20Ebook%2098
https://surharako.sokuhou.wiki/d/You%20searched%20for%20pixel%20films%20%3a%20Mac%20Torrents
estademe (Sunday, 13 February 2022 11:06)
7b17bfd26b estademe
https://wakelet.com/wake/QC39FvOLAgZQGt9Epws2M
https://wakelet.com/wake/vFVmumJNQ5UEDpgL6tXe2
https://wakelet.com/wake/lOjMiENVRRkJIBKi2mUGc
https://wakelet.com/wake/ZVfwn0WA_Uy_hezaHwUDn
https://wakelet.com/wake/ylQ4oMzf6Hgg4d9EwY7Gp
https://wakelet.com/wake/rM-AA3-MXVNlF_6dpsgAu
https://wakelet.com/wake/9laALyuk__Ofetzy7wFp2
https://wakelet.com/wake/pfv6hqXRrj-Ke6RjLI6jO
https://wakelet.com/wake/vPow7YANe5aJ2imTM0Ddi
https://wakelet.com/wake/hYtVftVDnNO7aPgZU4qgT
http://noikenergy.com/growing-wheat-crops/
beneleil (Sunday, 13 February 2022 12:14)
7b17bfd26b beneleil
https://wakelet.com/wake/xqvexk3Q8tRIm-rvFUNJS
https://wakelet.com/wake/CsH29_An3qrO2ANKtUMH8
https://wakelet.com/wake/TlemGSOr6IJ6j98IVnqDK
https://wakelet.com/wake/IJ2qQAHTwtgncZPN2JgY5
https://wakelet.com/wake/Gb7ziRaqIzL9sv5V9fxPP
https://wakelet.com/wake/JyTltOGzUHMajzODeAFyw
https://wakelet.com/wake/s-V_YMfqFIwmby7CHzn1s
https://wakelet.com/wake/2WcURn5eAKEBkZl6Cy7i6
https://wakelet.com/wake/nwNgIHdLnvpw06j28g-gO
https://wakelet.com/wake/06lS0ZoKCWs1WrFoaarAi
https://capitone-mebel.ru/product/rim/
philyani (Sunday, 13 February 2022 13:20)
7b17bfd26b philyani
https://casenama.memo.wiki/d/Crack%20Hq%20Player%20Vs%20Jplay%20Utorrent%20License%20%2erar%20Full%20Build%2064bit%20%7cVERIFIED%7c
https://iznawyndrea.memo.wiki/d/Kung%20Fu%20Hustle%20Full%20Movie%20English%20Subtitles%20Free%20Download
https://mocabutneu.sokuhou.wiki/d/Anga%20Samudrika%20Shastra%20Pdf%2020
https://seesaawiki.jp/ealrescedi/d/Zebra%20Designer%20Pro%20Serial%20Crack
https://stinabnate.chronicle.wiki/d/Dj%20Hero%20Pc%20Download%20Completo%20Gratis
https://promcamptohra.sokuhou.wiki/d/Yajur%20Veda%20Sandhyavandanam%20In%20Tamil%20Pdf
https://arjesugi.sokuhou.wiki/d/Atomic%20And%20Molecular%20Spectroscopy%20By%20Rajkumar%2021
https://acbaclifac.memo.wiki/d/Backspin%20Billiards%20Deluxe%20Pool%20Full%20Version
https://seesaawiki.jp/pyoubrewexle/d/Binding%20Of%20Isaac%20Afterbirth%201001%20Save%20%5bEverything%20Unlocked%5d
https://seesaawiki.jp/puforthalla/d/%23%23TOP%23%23%20Adobe%20In%20Cracked%20Pc%20Activation%2064%20Latest
https://audreycleo.com/?p=3602&cpage=33
edramer (Sunday, 13 February 2022 14:23)
7b17bfd26b edramer
https://wakelet.com/wake/foGv5BScDEvxQIqbNEjPO
https://wakelet.com/wake/SggNhPE1aRdeNlPBtQ_M1
https://wakelet.com/wake/HTnvV1_zgHzEshFe1kskL
https://wakelet.com/wake/leKpZyiDwhD3a-OJ_ZLym
https://wakelet.com/wake/kia2kkg5Y6gaaVt8Cp0fb
https://wakelet.com/wake/wfqJ2bGoEIhWXiIh6rXDn
https://wakelet.com/wake/P5Owo33UMDjZv9Kqe_TGS
https://wakelet.com/wake/f_faI1HXahl3JJZSaF1Ph
https://wakelet.com/wake/hELf0tHmIGSaXvP_fGSe_
https://wakelet.com/wake/WqLTScty9EVTCzelApF4o
https://portal.tlas.org.al/sq/procedura-e-dhënies-së-ndihmës-juridike-dytësore-të-pandehurit-pa-mjete-të-mjaftueshme-financiare?page=12#comment-1401859
jarbrin (Sunday, 13 February 2022 15:28)
7b17bfd26b jarbrin
https://wakelet.com/wake/2lVGxosgPlNmdKVybC-_j
https://wakelet.com/wake/_YNa07GNuZGKr_t-E26b7
https://wakelet.com/wake/AEyoC8Q0yIq_BGH6lVHDg
https://wakelet.com/wake/fBiAYSSaLz21xwbMMx2Vf
https://wakelet.com/wake/Ufams17atjaHPUIOPaI4Z
https://wakelet.com/wake/MsFhKYT5MjCAfzNVly6DN
https://wakelet.com/wake/mLmxe7evimcrcPjCQaT5L
https://wakelet.com/wake/Iex3WCqyawPizD_g5iwMp
https://wakelet.com/wake/fXhsA3muREle033_ZI1LV
https://wakelet.com/wake/W3I9Mz-ZdpW3vKkV-qhdX
https://casinonews.cc/sportsbetting-tax-regime-proposal-gains-approval-in-brazil/
bengene (Sunday, 13 February 2022 16:33)
7b17bfd26b bengene
https://seesaawiki.jp/ethbiakuytiy/d/TrendyFlash%2dSite%2dBuilder%2dlicensed%20By%3b%20G%2en%2ecooldud%2erar%2e%20Serial%20Key%20Keygen%20%5fHOT%5f
https://afromole.game-info.wiki/d/Kof%2098%20License%20Pc%20Serial%20Build%20Utorrent%20Rar
https://seesaawiki.jp/otcinelbeans/d/%23%23HOT%23%23%20Utorrent%20Microsoft%20Visual%20Basic%202010%20Express%20Pc%20Keygen%2064bit%20Zip
https://seesaawiki.jp/locaphota/d/Geeks%20Activator%20Pc%20Utorrent%20X64%20Latest%20pragra
https://thuycugage.sokuhou.wiki/d/Renee%20File%20Protector%201%2e2%20Serial%20Key%20With%2096
https://seesaawiki.jp/imesemti/d/Theme%20Hospital%20%28Bullfrog%201997%29%20Vip%20Hack
https://ordelselo.sokuhou.wiki/d/Ndcn%20W55%20Insert%20Correct%20Map%20Disc
https://lyngxagphosub.game-info.wiki/d/Elementarz%20M%20Falski%20Pdf%20Free
https://seesaawiki.jp/miyplicemna/d/Dkz%20Studio%20Professional%20Patch%2064bit%20Windows%20%2erar%20Torrent%20Activation%20habichar
https://pomlistregy.chronicle.wiki/d/Nachom%20Ia%20Kumpasar%20Watch%20Online%20Dvdrip%20Hd%20Watch%20Online%20lindjose
https://www.healthcarehygienemagazine.com/detecting-antibodies-with-glowing-proteins-thread-and-a-smartphone/
katrhert (Sunday, 13 February 2022 17:37)
7b17bfd26b katrhert
https://wakelet.com/wake/NGmN0uaDw9WPx1BNTWmQ5
https://wakelet.com/wake/PCOVGYvNNTAPG0JiDf3Av
https://wakelet.com/wake/MmroMCXbCHPGPEYYDe5Sg
https://wakelet.com/wake/DO-_EOENTpyUBYErAXb97
https://wakelet.com/wake/k-LNlC5KECUw_8u_EMLJx
https://wakelet.com/wake/YXxMJZEPQP1YeDa4mmDP_
https://wakelet.com/wake/G7HGi20umfPN8pc04BdCR
https://wakelet.com/wake/TmFemMwvJYyC6R1hHgcVf
https://wakelet.com/wake/ZCPVyRdmJDj_WCVdJ88Pp
https://wakelet.com/wake/x7u-qGBzK8h89w1vSlqiH
https://motoblog.carweb.tokyo/2020/04/05/%EF%BE%8A%EF%BE%9D%EF%BE%80%EF%BD%B0%EF%BD%B6%EF%BE%8C%EF%BE%9Ect125ja55%EF%BD%BD%EF%BE%8C%EF%BE%9F%EF%BE%9B%EF%BD%B9%EF%BD%AF%EF%BE%84%E3%82%92%E4%BA%A4%E6%8F%9B%E3%81%99%E3%82%8B%E3%81%A8%E3%80%81/
baloji (Sunday, 13 February 2022 18:41)
7b17bfd26b baloji
https://wakelet.com/wake/LmuhOZ5JYwpuBDn9YLgcm
https://wakelet.com/wake/0YWZOFtUIra6ozOL0OC1Z
https://wakelet.com/wake/gpiScfD_qFKNaZUay6qVJ
https://wakelet.com/wake/5K7GqukcKt9zT1sBk5LKc
https://wakelet.com/wake/fu3jY2UOy2s-LDnGEBi99
https://wakelet.com/wake/oOfp1waxF4aPCwROc8Dmt
https://wakelet.com/wake/8ho2p5kJwEX64mxCsAhZ3
https://wakelet.com/wake/2RkZUHE8Ylwd-egBURQo7
https://wakelet.com/wake/rOGiaPSHBGt__2Th6d-h-
https://wakelet.com/wake/PYReXh7kZmMIIskqaqfH5
https://thedamnthing.com/the-ultimate-baby-shower-registry/
alpdore (Sunday, 13 February 2022 19:48)
7b17bfd26b alpdore
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDAtqCXCAwLEgZDb3Vyc2UYgIDAwLaglwoMCxIIQWN0aXZpdHkYgIDA4JDMvQkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgICf67f9CQwLEgZDb3Vyc2UYgIDAwJXrqQsMCxIIQWN0aXZpdHkYgIDAoIux6AoMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCA06r-CgwLEgZDb3Vyc2UYgIDAoNGZ3wkMCxIIQWN0aXZpdHkYgIDAwNPltAsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_xamfCQwLEgZDb3Vyc2UYgIDAoISlywsMCxIIQWN0aXZpdHkYgIDA4My1-wgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDg9PuFCwwLEgZDb3Vyc2UYgIDA4OWf4goMCxIIQWN0aXZpdHkYgIDAoKiiggkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_wN6UCQwLEgZDb3Vyc2UYgIDAgPKQiQsMCxIIQWN0aXZpdHkYgIDAkKrgswkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCghP7CCgwLEgZDb3Vyc2UYgIDAgPKQrggMCxIIQWN0aXZpdHkYgIDAwNPLpAgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_093ICwwLEgZDb3Vyc2UYgICAn5uGkgkMCxIIQWN0aXZpdHkYgIDA4OXxmAoMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDAk5KKCAwLEgZDb3Vyc2UYgIDA4Le-oAsMCxIIQWN0aXZpdHkYgIDAkMuBsAsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgIC__ofuCwwLEgZDb3Vyc2UYgIDAoPip7woMCxIIQWN0aXZpdHkYgIDA4NDRhAkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://billyhair.do/portal/2014/03/10/the-barbers-show-at-barcelona-spain/
ermaokp (Sunday, 13 February 2022 20:53)
7b17bfd26b ermaokp
https://wakelet.com/wake/EJFsiSYpzM694y--m0WhZ
https://wakelet.com/wake/bdeVn7gP94zTY9p3BfmLj
https://wakelet.com/wake/7YlKH_VW_IK_rj_7YbfSD
https://wakelet.com/wake/c6DekauaFYFUX7b0V5vp3
https://wakelet.com/wake/vJOoPOQ8sk45_X8iw3qSv
https://wakelet.com/wake/a368210uIJ08YbAmCc7uU
https://wakelet.com/wake/mhQjZvIxaFax6B1yNrxC4
https://wakelet.com/wake/1W2Vxvf7CsWW6seQPrA56
https://wakelet.com/wake/nCcf6calFEPlQUCddPmym
https://wakelet.com/wake/W2TZPY9L_SxMZCb7mOB0f
https://borneohistory.net/?p=167
helecha (Sunday, 13 February 2022 21:59)
7b17bfd26b helecha
https://coub.com/stories/3421276-astrology-the-speed-of-light-torrent-torrent-casssal
https://coub.com/stories/3421274-son-of-sardar-full-movie-hd-720p-download-from-kickasstorrents-extra-quality
https://coub.com/stories/3421272-free-medal-of-honor-warfighter-deluxe-edition-sc
https://coub.com/stories/3421270-__full__-key-idm-6-19-full-crack
https://coub.com/stories/3421269-lakshminarayanahrudayamstotraminsanskritpdf-2021-free
https://coub.com/stories/3421268-adeko-42-turkce-indir-ucretsiz-hardalo
https://coub.com/stories/3421267-urave-uyire-tamil-serial-song-mp3-free-download-furmed
https://coub.com/stories/3421264-portable-risiko-2-spiel-download-kostenlos-vollversion
https://coub.com/stories/3421263-mocha-girls-playboy-philippines-september-2012-29-total-welcher-erotii-better
https://coub.com/stories/3421258-girls-with-hairy-pussies-getting-fucked-high-quality
https://www.lobservatoiredufoot.com/2021/08/11/avec-messi-on-met-paris-en-bouteille/
georthir (Sunday, 13 February 2022 23:04)
7b17bfd26b georthir
https://coub.com/stories/3004215-sleeping-dogs-pc-torrent-download-patched
https://coub.com/stories/3004217-red-giant-universe-crack-mack-hilgin
https://coub.com/stories/3004222-sps-team-magix-music-studio-deluxe-2005-rar-free-download-carragn
https://coub.com/stories/3004223-high-quality-iris-mini-0-3-0-software-for-eye-protection-serial-key
https://coub.com/stories/3004227-easy-card-creator-free-7-20-22-crack-actividades-starz-ma-new
https://coub.com/stories/3004228-axalto-egate-drivers-v3-0-6-0-setool-drivers-rar-hanegm
https://coub.com/stories/3004224-adobe-photoshop-cc-multi-language-xforce-best-keygen-downloadtrmdsf
https://coub.com/stories/3004229-digital-anarchy-flicker-free-1-0-1-for-ae-cracked-vr-chingl-utorrent-new
https://coub.com/stories/3004230-__top__-download-jab-tak-hai-jaan-full-movie-300mb
https://coub.com/stories/3004245-top-download-sni-03-1732-1989
http://xc123456am.com/2021/06/13/testando-o-meu-cu-no-robo-vibrador-testing-my-asshole-on-the-vibrator-robot/
fifonta (Monday, 14 February 2022 00:09)
7b17bfd26b fifonta
https://trello.com/c/Dpn2Acqu/68-top-zapatleladualaudiohindidownload
https://trello.com/c/6BL0GXAF/40-best-highlycompressedhollywoodmovieinhindi
https://trello.com/c/UziiKwyU/64-top-hack-camtasia-studio-v8-4-4-incl-keygen-tsz
https://trello.com/c/3zIC3xSt/56-hack-zipscan-22c-full-version-andrhald
https://trello.com/c/MEsLrEYC/51-zanerian-manual-of-alphabets-pdf-hot-download
https://trello.com/c/Klpwjt83/31-showgirls-1995-unrated-720p-video-livowazi
https://trello.com/c/n0uE4ZWs/68-immortals-english-dubbed-720p-torrent-download-full
https://trello.com/c/B0YZkAis/38-minecraft-teksturpack-top-download
https://trello.com/c/zI4e7YuK/62-top-welcome-2-karachi-full-movie-in-hindi-720p-download
https://trello.com/c/BzRMdUbL/36-un-paseo-para-recordar-1080p-mega-5
https://riabroodseniorenadvies.info/apps/blog/show/43741982-onderzoeksresultaten-over-de-zorg-voor-later
frarayn (Monday, 14 February 2022 01:16)
7b17bfd26b frarayn
https://coub.com/stories/3316582-crumplepop-fisheye-fixer-dmg-torrent-__top__
https://coub.com/stories/3316579-vidhata-free-full-movie-1982-hd-174
https://coub.com/stories/3316580-daisy-s-destruction-video-completo-franudo
https://coub.com/stories/3316577-ps3-jailbreak-games-compatibilitylist-lavgaym
https://coub.com/stories/3316578-the-beast-inside-download-for-pc-key-serial-number-golkes-install
https://coub.com/stories/3316576-verified-dikkenek-version-longue-torrent
https://coub.com/stories/3316573-link-ghatak-hindi-720p-download
https://coub.com/stories/3316571-thandavam-movie-download-new-utorrent-link
https://coub.com/stories/3316569-download-lazarus-the-complete-guide-free-pascal-top
https://coub.com/stories/3316568-work-red-giant-trapcode-suite-v12-0-0-win-32-64-bit
https://www.swomag.com/charles-wilkins-collage-art/
wensmili (Monday, 14 February 2022 02:22)
7b17bfd26b wensmili
https://trello.com/c/7k2QaNh0/35-telechart-better-full-version-download
https://trello.com/c/tqHoLxEP/66-easy-driver-pack-533-win-7-32bit-top
https://trello.com/c/Z9bvSI89/52-hot-3dxchat-download-crack-45
https://trello.com/c/3xrKPLsX/28-verified-full-omnius-for-se-crack
https://trello.com/c/FSyhtiIC/28-new-loquendo-tts-7-voice-experience-crack
https://trello.com/c/UjjHVI50/47-adobe-encore-cs6-crack-dll-xevras
https://trello.com/c/6BqrOKCg/30-g5-clonecloth-updated
https://trello.com/c/QeKfbCwr/51-babysitting-cream-v98-hacked-version-high-quality
https://trello.com/c/uCHzfVQv/27-adobe-photoshop-cc-2017-v1701-x86x64-incl-crack-serial-key-chanix
https://trello.com/c/ge6g7ooQ/28-manusmritikannadapdf-better
http://www.errorday.it/en/fotografia/pippodromo?page=12#comment-222660
vasyes (Monday, 14 February 2022 03:30)
7b17bfd26b vasyes
https://trello.com/c/w5LLpDLm/25-better-dr-robert-vinyl-rip-flac
https://trello.com/c/WwmnUhcD/50-hd-online-player-junooniyat-full-movie-720p-download-new
https://trello.com/c/F5zA5W53/32-heer-ranjha-movie-in-hindi-720p-download-tagegudr
https://trello.com/c/TyynjnhF/48-best-adobe-photoshop-lightroom-classic-cc-2018-71016-x64-crack-utorrent
https://trello.com/c/QoXspBKd/29-exclusive-m83-oblivion-original-soundtrack-320-zippyshare
https://trello.com/c/4HvMc4KM/59-filetype-txt-username-password-facebook-com-akilkala
https://trello.com/c/mFBeML7x/41-velamma-episode-1-exclusive-free-download-in-tamil-pdf
https://trello.com/c/RyKkcZcX/31-kabhi-khushi-kabhie-gham-full-verified-movie-hd-1080p-dailymotion-age
https://trello.com/c/cVJ2vTgW/57-dslr-remote-pro-crack-v3143-with-keygen-free-download-shaucad
https://trello.com/c/XCJmEfM3/31-arashi-time-top-full-album-zip
http://www.enoavolley.fr/index.php?option=com_easybookreloaded
attepaul (Monday, 14 February 2022 04:36)
7b17bfd26b attepaul
https://coub.com/stories/3507658-the-mummy-returns-2001-1080p-hddvdrip-h264-aac-12-high-quality
https://coub.com/stories/3508774-photograv-2-11-rar-new
https://coub.com/stories/3508773-3-kurbaan-hindi-movie-torrent-download-goldgius
https://coub.com/stories/3508771-dinamica-de-sistemas-ogata-solucionario
https://coub.com/stories/3507765-letra-y-acordes-de-el-secreto-es-adorarle-herbmal
https://coub.com/stories/3507766-vedalam-2015-tamil-720p-hdrip-x264-ac3-1-4gb-mkv
https://coub.com/stories/3507767-hearts-blood-juliet-marillier-epub-download-site-link
https://coub.com/stories/3507769-halo-3-bestiarum-pdf-download-gerrcove
https://coub.com/stories/3507770-soallombamapsi-gemquaq
https://coub.com/stories/3507771-maximiliano-10yo-boy-bibcam-work
https://seesaawiki.jp/plumlessdoope/d/free%2dtiktok%2dviews
nangile (Monday, 14 February 2022 05:43)
7b17bfd26b nangile
https://wakelet.com/wake/GyESEdyF2gfD7rPQNzjCM
https://wakelet.com/wake/bUtNsFCrJRE-qejGsSMid
https://wakelet.com/wake/c0JffTH2c79wiiSXflHEe
https://wakelet.com/wake/t-6J3qBySsEqB8StFcPZE
https://wakelet.com/wake/m32x8DCyIZwZfG-_TTohg
https://wakelet.com/wake/UIRVs6DV8sk7a9DVUWhu9
https://wakelet.com/wake/6foEr7Rg11gwLxomJi-r5
https://wakelet.com/wake/YEDBWSJNSnlRUNUNl4M5l
https://wakelet.com/wake/b-SgGjZBFUjuF0sO4LfdG
https://wakelet.com/wake/kNHv424iJipof0oiPNS5D
https://www.giuglar.com/de/module/smartblog/details?id_post=11&slug=novita-riapertura
keallea (Monday, 14 February 2022 06:51)
7b17bfd26b keallea
https://whetsnatyme.sokuhou.wiki/d/Akira%20Kannada%20Full%20Movie%20Download
https://seesaawiki.jp/buidanemer/d/Frank%20Middle%20School%20Geography%20Class%207%20Ebook%2019
https://gutsdenprozo.playing.wiki/d/City%20Patrol%20Police%20PC%20Game%20Free%20Download%2dCPY
https://lunsupimu.playing.wiki/d/Poedit%20Pro%202%2e0%2e3%20Build%205098%20Patch%20%5bCracksNow%5d%20Crack
https://seesaawiki.jp/studfondpebbuy/d/CRACK%20Magic%20Utilities%202008%20V5%2e51%20Portable
https://ascenapi.chronicle.wiki/d/Janiye%20Dus%20Kahaniyaan%20Hd%201080p
https://gorbalasen.sokuhou.wiki/d/Pawan%20Kalyan%20Watch%20Online%20Video%201080p%20Torrent
https://seesaawiki.jp/terninoricht/d/Uncharted%204%20A%20Thief%e2%80%99s%20End%20Redeem%20Code%20Generator
https://siotrelexig.playing.wiki/d/Rick%20Ross%20Deeper%20Than%20Rap%20Explicit%202009
https://quodresrabeach.chronicle.wiki/d/License%2ebin%20Free%20Sibelius%207
http://mdrf-hr.sblo.jp/article/186602946.html
danjai (Monday, 14 February 2022 08:00)
7b17bfd26b danjai
https://wakelet.com/wake/48AJGM9H_0EF-rAyCESXI
https://wakelet.com/wake/UxD3ZDze53acARPKuSDd4
https://wakelet.com/wake/VqgmBfD1huQ2VOWb6Mobv
https://wakelet.com/wake/22b6z9YMR4snpCCLOXGtg
https://wakelet.com/wake/pgSddcceEuSDtgCcfJyVy
https://wakelet.com/wake/FRLjRlVvj1O73LPLkqLoa
https://wakelet.com/wake/QZj028_GrK_78oG366iF7
https://wakelet.com/wake/t8XNOlg4ZODbMYoHunDRC
https://wakelet.com/wake/tgLle9hN6XWvGoMstJb4D
https://wakelet.com/wake/lPHiSW9IytTH8awTG7ry2
http://vendugeek.com/blog/2_what-is-bootstrap.html
pelign (Monday, 14 February 2022 09:09)
7b17bfd26b pelign
https://coub.com/stories/3251374-jan-dara-the-finale-full-movie-free-download-leodelv
https://coub.com/stories/3251373-celebrate-the-international-talk-like-a-pirate-day-with-these-cool-apps
https://coub.com/stories/3251370-half-life-deathmatch-source-download-portable-with-license-key
https://coub.com/stories/3251369-work-europe-2011-2012-edition-1-0-harman-becker-citroen-c5
https://coub.com/stories/3251367-download-harvest-moon-the-movie-gritty-reboots-15-patpam
https://coub.com/stories/3251368-arrival-english-telugu-movie-video-songs-hd-1080p
https://coub.com/stories/3251365-high-quality-u-me-aur-hum-movie-3gp-download-dubbed-in-hindi
https://coub.com/stories/3251364-the-film-movie-in-hindi-720p-download-work
https://coub.com/stories/3251363-download-net-framework-3-5-include-2-0-and-3-0-for-windows-8-rapidshare-__link__
https://coub.com/stories/3251362-download-link-animasi-xxx-bergerak-gratis
http://www.portal.tlas.org.al/sq/detyrat-e-drejtorisë-së-ndihmës-juridike-falas?page=11#comment-1403789
forsyeli (Monday, 14 February 2022 10:15)
7b17bfd26b forsyeli
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDA5eSjCQwLEgZDb3Vyc2UYgIDAgMGEugsMCxIIQWN0aXZpdHkYgIDAwPOyhgsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgIC_gZ6vCAwLEgZDb3Vyc2UYgIDAwLae8AkMCxIIQWN0aXZpdHkYgIDA0KK4kwkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_uZGVCwwLEgZDb3Vyc2UYgIDAwNaxmwoMCxIIQWN0aXZpdHkYgIDA0MLa5AsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDA1rGzCgwLEgZDb3Vyc2UYgIDAwKXN9gkMCxIIQWN0aXZpdHkYgICA_8-i8gsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCQqLL4CQwLEgZDb3Vyc2UYgIDAwNO0xAgMCxIIQWN0aXZpdHkYgIDA4NX-zwkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgICfpKyGCwwLEgZDb3Vyc2UYgIDAoPip1woMCxIIQWN0aXZpdHkYgIDA4PXK8AoMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDg4NLiCwwLEgZDb3Vyc2UYgIDAkJin9wgMCxIIQWN0aXZpdHkYgIDA0LfP8wsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_k9WFCQwLEgZDb3Vyc2UYgICA36nIqwsMCxIIQWN0aXZpdHkYgIDAoLiIgAsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDAlY3UCgwLEgZDb3Vyc2UYgICA_6buxQkMCxIIQWN0aXZpdHkYgIDA0MLa5AkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_xIHoCQwLEgZDb3Vyc2UYgICAv8HNnAgMCxIIQWN0aXZpdHkYgIDAkOqxhAoMogEQNTcyODg4NTg4Mjc0ODkyOA
http://www.arkadian.vg/e3-2016-nuevo-trailer-y-gameplay-de-attack-on-titan/
annbere (Monday, 14 February 2022 14:16)
7b17bfd26b annbere
https://wakelet.com/wake/qbQqi9IwlbqRpddMwZZjL
https://wakelet.com/wake/5SEOtyDYvfw_UFd9oUgnc
https://wakelet.com/wake/axhu-rx5uiqwrYaQ3cA0V
https://wakelet.com/wake/RL0MP6NENsuXVYqr5zxyJ
https://wakelet.com/wake/4CQyD5pG9M5KNDKW0pIxp
https://wakelet.com/wake/4E7gD8MaccL1w0aYXHBA7
https://wakelet.com/wake/c4clUpn2a7fnoFsR0h0hs
https://wakelet.com/wake/JdJFjriCeREqkqORF63Uq
https://wakelet.com/wake/MyCx85vAcAwvxRNiF4qcu
https://wakelet.com/wake/M43yor46TMXFFWo_YLR1o
http://smokyhosts.com/forums/viewtopic.php?f=14&t=37248&p=89988#p89988
dayphyl (Monday, 14 February 2022 15:23)
7b17bfd26b dayphyl
https://coub.com/stories/3465746-main-aisa-hi-hoon-2-full-movie-hd-720p-free-better-download
https://coub.com/stories/3460265-shoemaster-qs-10-02-crack-top
https://coub.com/stories/3460264-solidworks-2020-crack-full-torrent-with-key-download-best
https://coub.com/stories/3460263-10ml-love-2-in-hindi-free-download-for-utorrent-amaadv
https://coub.com/stories/3460262-updated-mprofitcrackcodeforwindows
https://coub.com/stories/3460260-titanic-telugu-movie-ringtones-download-newmonid
https://coub.com/stories/3460261-hd-kill-dil-movies-1080p-download-yudrayl
https://coub.com/stories/3460259-videoredo-tvsuite-v4-serial-number
https://coub.com/stories/3460258-exclusive-mugen-saint-seiya-ultimate-cosmo
https://coub.com/stories/3460257-abcd-any-body-can-dance-2-english-dubbed-720p-torrent-download-exclusive
https://northeastdoulas.com/kids-say-the-darndest-things-part-2/
dayphyl (Monday, 14 February 2022 15:23)
7b17bfd26b dayphyl
https://coub.com/stories/3465746-main-aisa-hi-hoon-2-full-movie-hd-720p-free-better-download
https://coub.com/stories/3460265-shoemaster-qs-10-02-crack-top
https://coub.com/stories/3460264-solidworks-2020-crack-full-torrent-with-key-download-best
https://coub.com/stories/3460263-10ml-love-2-in-hindi-free-download-for-utorrent-amaadv
https://coub.com/stories/3460262-updated-mprofitcrackcodeforwindows
https://coub.com/stories/3460260-titanic-telugu-movie-ringtones-download-newmonid
https://coub.com/stories/3460261-hd-kill-dil-movies-1080p-download-yudrayl
https://coub.com/stories/3460259-videoredo-tvsuite-v4-serial-number
https://coub.com/stories/3460258-exclusive-mugen-saint-seiya-ultimate-cosmo
https://coub.com/stories/3460257-abcd-any-body-can-dance-2-english-dubbed-720p-torrent-download-exclusive
https://northeastdoulas.com/kids-say-the-darndest-things-part-2/
garlnol (Monday, 14 February 2022 16:27)
7b17bfd26b garlnol
https://coub.com/stories/2979476-mrzjw3-setup151e-software-download-fabdar
https://coub.com/stories/2979474-mep-cad-autosprink-v11-crack-dekoneke
https://coub.com/stories/2979472-aio-vectric-aspire-309-photovcarve-cut2d-cut3d-vcarve-pro-hot
https://coub.com/stories/2979473-better-lolita-downloads-torrent
https://coub.com/stories/2979470-tekla-structures-v-19-0-sr1-x86-x64-exclusive
https://coub.com/stories/2979471-iobit-driver-booster-pro-6-6-0-455-with-crack-nicmar
https://coub.com/stories/2979469-repack-tomtom-renault-europe-sd-carminat-torrent
https://coub.com/stories/2979468-optitex-15-full-crack-internetinstmanksl-leelubl
https://coub.com/stories/2979467-estadistica-matematica-con-aplic-frowtap
https://coub.com/stories/2979466-_hot_-hidan-no-aria-light-novel-volume-11-pdf-18
http://pulsar-forum.pl/showthread.php?tid=630534&pid=1182427#pid1182427
emmgas (Monday, 14 February 2022)
7b17bfd26b emmgas
https://trello.com/c/ww0X7Ddj/41-speakboard-portable-hun-magyar-szovegfelolvaso7z-full-versionbfdcm-exclusive
https://trello.com/c/7vkmzAXA/59-runtime-dll-cblrtsm-version-4-download-bengrehe
https://trello.com/c/ejcQKwh4/18-wifi-analyzer-home-wifi-alert-v1415-mod-ad-free-latest-hot
https://trello.com/c/QzOlAXTm/58-x-force-keygen-adobe-master-collection-cs6-crack-betterl
https://trello.com/c/1UemXIY9/55-erykah-badu-baduizm-free-full-album-zip
https://trello.com/c/JKqnCiut/28-strata-foto-3d-cx2rar
https://trello.com/c/xMWhgXZD/63-huawei-modem-unlocker-v577-tested-exclusive
https://trello.com/c/zV9kTsik/20-ab-tumhare-hawale-watan-sathiyo-movie-download-in-hindi-mp4-movies-install
https://trello.com/c/7ILrA9m7/32-adobe-audition-v15-rar
https://trello.com/c/xSm4jbrW/58-adobe-reader-xi-11021-latest-version-2018-serial-key-keygen-link
http://copper-lines.com/ru/2018/01/23/euro-corporation-%D0%BE%D0%B1%D0%B2%D0%B8%D0%BD%D0%B8%D0%BB%D0%B8-%D0%B2-%D1%84%D0%B0%D0%BB%D1%8C%D1%81%D0%B8%D1%84%D0%B8%D0%BA%D0%B0%D1%86%D0%B8%D0%B8-%D0%BA%D0%B0%D1%87%D0%B5%D1%81%D1%82%D0%B2%D0%B0/
emmgas (Monday, 14 February 2022 17:33)
7b17bfd26b emmgas
https://trello.com/c/ww0X7Ddj/41-speakboard-portable-hun-magyar-szovegfelolvaso7z-full-versionbfdcm-exclusive
https://trello.com/c/7vkmzAXA/59-runtime-dll-cblrtsm-version-4-download-bengrehe
https://trello.com/c/ejcQKwh4/18-wifi-analyzer-home-wifi-alert-v1415-mod-ad-free-latest-hot
https://trello.com/c/QzOlAXTm/58-x-force-keygen-adobe-master-collection-cs6-crack-betterl
https://trello.com/c/1UemXIY9/55-erykah-badu-baduizm-free-full-album-zip
https://trello.com/c/JKqnCiut/28-strata-foto-3d-cx2rar
https://trello.com/c/xMWhgXZD/63-huawei-modem-unlocker-v577-tested-exclusive
https://trello.com/c/zV9kTsik/20-ab-tumhare-hawale-watan-sathiyo-movie-download-in-hindi-mp4-movies-install
https://trello.com/c/7ILrA9m7/32-adobe-audition-v15-rar
https://trello.com/c/xSm4jbrW/58-adobe-reader-xi-11021-latest-version-2018-serial-key-keygen-link
http://copper-lines.com/ru/2018/01/23/euro-corporation-%D0%BE%D0%B1%D0%B2%D0%B8%D0%BD%D0%B8%D0%BB%D0%B8-%D0%B2-%D1%84%D0%B0%D0%BB%D1%8C%D1%81%D0%B8%D1%84%D0%B8%D0%BA%D0%B0%D1%86%D0%B8%D0%B8-%D0%BA%D0%B0%D1%87%D0%B5%D1%81%D1%82%D0%B2%D0%B0/
emmgas (Monday, 14 February 2022 17:34)
7b17bfd26b emmgas
https://trello.com/c/ww0X7Ddj/41-speakboard-portable-hun-magyar-szovegfelolvaso7z-full-versionbfdcm-exclusive
https://trello.com/c/7vkmzAXA/59-runtime-dll-cblrtsm-version-4-download-bengrehe
https://trello.com/c/ejcQKwh4/18-wifi-analyzer-home-wifi-alert-v1415-mod-ad-free-latest-hot
https://trello.com/c/QzOlAXTm/58-x-force-keygen-adobe-master-collection-cs6-crack-betterl
https://trello.com/c/1UemXIY9/55-erykah-badu-baduizm-free-full-album-zip
https://trello.com/c/JKqnCiut/28-strata-foto-3d-cx2rar
https://trello.com/c/xMWhgXZD/63-huawei-modem-unlocker-v577-tested-exclusive
https://trello.com/c/zV9kTsik/20-ab-tumhare-hawale-watan-sathiyo-movie-download-in-hindi-mp4-movies-install
https://trello.com/c/7ILrA9m7/32-adobe-audition-v15-rar
https://trello.com/c/xSm4jbrW/58-adobe-reader-xi-11021-latest-version-2018-serial-key-keygen-link
http://copper-lines.com/ru/2018/01/23/euro-corporation-%D0%BE%D0%B1%D0%B2%D0%B8%D0%BD%D0%B8%D0%BB%D0%B8-%D0%B2-%D1%84%D0%B0%D0%BB%D1%8C%D1%81%D0%B8%D1%84%D0%B8%D0%BA%D0%B0%D1%86%D0%B8%D0%B8-%D0%BA%D0%B0%D1%87%D0%B5%D1%81%D1%82%D0%B2%D0%B0/
zakscov (Monday, 14 February 2022 18:37)
7b17bfd26b zakscov
https://coub.com/stories/3353394-guilherme-franco-tabela-pdf-13-2021
https://coub.com/stories/3353393-dont-crack-under-pressure-subtitulado-torrent-cathnah
https://coub.com/stories/3353390-junglee-tarzan-dual-audio-eng-hindi-1080p
https://coub.com/stories/3353388-2021-techsmith-camtasia-studio-v9-0-3-build-1627-keygen-repack-keygen
https://coub.com/stories/3353387-top-partitura-piano-legends-of-the-fall-leyendas-de-pasion-james-horner-pdf
https://coub.com/stories/3353385-mixmeister-fusion-7-6-verified-download-crack-101
https://coub.com/stories/3353386-dishonoredspolszczeniecrackfree-cracked
https://coub.com/stories/3353383-hot-hp-laserjet-1160-driver-for-windows-7-32-bit-download
https://coub.com/stories/3353381-film-dumnezeu-pentru-o-zi-repack-download
https://coub.com/stories/3353380-solidworks-edrawings-2011-license-key-crack-better
https://www.roseaccessories.gr/index.php?fc=module&module=smartblog&id_post=15&controller=details&id_lang=1
xankafl (Monday, 14 February 2022 19:44)
7b17bfd26b xankafl
https://trello.com/c/xpO78kdY/23-top-bleach-soul-resurreccion-pc
https://trello.com/c/szzFwA6K/51-avast-2020-crack-license-file-valid-till-2060-free-download-best
https://trello.com/c/dphhSeFb/33-samsung-tools-2201-hwk-by-sarasoft-fix
https://trello.com/c/j8anaLTu/41-taitotypex2roms
https://trello.com/c/5DN8xOZk/74-full-nederlands-taalpakket-voor-office-2013-x64-sunrnan
https://trello.com/c/0vlGJ3Ks/74-le-vrai-visage-de-paul-biya-pdf
https://trello.com/c/nkzaHk1u/35-agente-007-bersaglio-mobile-italian-video-download-namrjuni
https://trello.com/c/P0IRJOcK/65-full-crack-adobe-photoshop-cc-2015-1601-portable
https://trello.com/c/I1eJDZsO/50-3d-sex-villa-2-ever-lust-trainer-cheat-sexcoinsgolkes-new
https://trello.com/c/ey3nN84j/37-george-benson-discography-torrent
https://www.mapsofworld.com/travel/blog/miscellaneous/weird-african-customs-and-traditions
neabert (Monday, 14 February 2022 20:54)
7b17bfd26b neabert
https://trello.com/c/cKaAsnnt/19-chammak-challo-ra-one-full-video-song-hd-720p-download-free-full
https://trello.com/c/olB7Q40l/73-divxplusconverterver80149fullcrackidm-cracked
https://trello.com/c/UQaCk3at/20-install-ishq-deewana-4-full-movie-free-download-in-hindi-hd-1080p
https://trello.com/c/oF78L2ge/50-shigleys-mechanical-engineering-design-9th-edition-solutions-chapter-5-illesb
https://trello.com/c/PK3ryZvS/67-top-dedanadanmarathifilmsongdownload
https://trello.com/c/w38wQZbh/34-descargar-autodata-2011-gratis-con-crack-new
https://trello.com/c/ZF0uCNLS/62-zoofilia-videos-de-hombres-follando-con-mulasl-caebog
https://trello.com/c/jFL8Khh3/30-aajanachlebetter-fullmovies720ptorrent
https://trello.com/c/o84XHODH/99-hot-wondershare-mirrorgo-2020-crack
https://trello.com/c/2SgG1tP0/55-terminalworks-tsprint-12-keygen-faidar
http://www.cindyboycephoto.com/2016/02/agrikol-un-nouveau-resto-haitien-a-montreal/
neabert (Monday, 14 February 2022 20:54)
7b17bfd26b neabert
https://trello.com/c/cKaAsnnt/19-chammak-challo-ra-one-full-video-song-hd-720p-download-free-full
https://trello.com/c/olB7Q40l/73-divxplusconverterver80149fullcrackidm-cracked
https://trello.com/c/UQaCk3at/20-install-ishq-deewana-4-full-movie-free-download-in-hindi-hd-1080p
https://trello.com/c/oF78L2ge/50-shigleys-mechanical-engineering-design-9th-edition-solutions-chapter-5-illesb
https://trello.com/c/PK3ryZvS/67-top-dedanadanmarathifilmsongdownload
https://trello.com/c/w38wQZbh/34-descargar-autodata-2011-gratis-con-crack-new
https://trello.com/c/ZF0uCNLS/62-zoofilia-videos-de-hombres-follando-con-mulasl-caebog
https://trello.com/c/jFL8Khh3/30-aajanachlebetter-fullmovies720ptorrent
https://trello.com/c/o84XHODH/99-hot-wondershare-mirrorgo-2020-crack
https://trello.com/c/2SgG1tP0/55-terminalworks-tsprint-12-keygen-faidar
http://www.cindyboycephoto.com/2016/02/agrikol-un-nouveau-resto-haitien-a-montreal/
neabert (Monday, 14 February 2022 20:55)
7b17bfd26b neabert
https://trello.com/c/cKaAsnnt/19-chammak-challo-ra-one-full-video-song-hd-720p-download-free-full
https://trello.com/c/olB7Q40l/73-divxplusconverterver80149fullcrackidm-cracked
https://trello.com/c/UQaCk3at/20-install-ishq-deewana-4-full-movie-free-download-in-hindi-hd-1080p
https://trello.com/c/oF78L2ge/50-shigleys-mechanical-engineering-design-9th-edition-solutions-chapter-5-illesb
https://trello.com/c/PK3ryZvS/67-top-dedanadanmarathifilmsongdownload
https://trello.com/c/w38wQZbh/34-descargar-autodata-2011-gratis-con-crack-new
https://trello.com/c/ZF0uCNLS/62-zoofilia-videos-de-hombres-follando-con-mulasl-caebog
https://trello.com/c/jFL8Khh3/30-aajanachlebetter-fullmovies720ptorrent
https://trello.com/c/o84XHODH/99-hot-wondershare-mirrorgo-2020-crack
https://trello.com/c/2SgG1tP0/55-terminalworks-tsprint-12-keygen-faidar
http://www.cindyboycephoto.com/2016/02/agrikol-un-nouveau-resto-haitien-a-montreal/
deatyal (Monday, 14 February 2022 22:03)
7b17bfd26b deatyal
https://coub.com/stories/3477534-resetter-epson-wf-7511bfdcm-warjaci
https://coub.com/stories/3477533-_verified_-wondershare-dr-fone-10-2-1-crack
https://coub.com/stories/3477532-download-zanjeer-the-chain-720p-updated
https://coub.com/stories/3477520-portable-download-film-12-menit-kemenangan-untuk-selamanya-ganool-movie
https://coub.com/stories/3477531-work-tomas-taveira-a-foder-catarina-furtado-video
https://coub.com/stories/3477528-focus-in-hindi-dubbed-torrentgolkes-verified
https://coub.com/stories/3477530-work-ivt-bluesoleil-10-0-417-keygen-generator
https://coub.com/stories/3477529-mareleuriasprietenospdf15
https://coub.com/stories/3477527-outrun-2006-coast-2-coast-crack-no-cd-hot
https://coub.com/stories/3477525-adobe-fireworks-cs6-best-crack-indir
http://www.madattenerife.org/g%C3%A4stebuch/
phielly (Monday, 14 February 2022 23:13)
7b17bfd26b phielly
https://trello.com/c/z4UnsE5O/82-steam-apidll-dead-island-riptide-full
https://trello.com/c/jEyCaGd0/40-xara-3d-serial-key-hot
https://trello.com/c/8pSpH6IE/63-mobile-sim-card-reader-tool-3015-crack-cocaine-hendorv
https://trello.com/c/fAov3Qem/34-full-descargar-rex-un-policia-diferente-torrent
https://trello.com/c/AKXOKJwe/44-allinonekeyloggerv36-keygen-hotrar
https://trello.com/c/vCr2DMaw/20-hot-sirf-tum-movie-720p-download-utorrent-movies
https://trello.com/c/LQsA5Hj8/80-readiris-pro-10-keygen-download-ciadej
https://trello.com/c/NvyWNpek/31-exclusive-siemens-femap-1201a-with-nx-nastran-and-satoolkit-crack
https://trello.com/c/i8rSJuzO/101-mrt-dongle-326-crack-torrent-2020-for-life-time-working-extra-quality
https://trello.com/c/98ZSmuce/24-multiecuscan-full-sofydagn
http://www.tonydada.com/change-can-scary-thing-theres-something-even-scarier/comment-page-1465/
jamjaij (Tuesday, 15 February 2022 00:20)
7b17bfd26b jamjaij
https://seesaawiki.jp/ticrygendcnic/d/Creature%20Full%20Movie%20In%20Tamil%20Download
https://seesaawiki.jp/wallgarosec/d/Floor%20Plan%203d%2011%2e0%2036%2064bit%20%7eUPD%7e%20Full%20Software%20Patch%20Key%20Utorrent%20Iso
https://seesaawiki.jp/icacberju/d/Humse%20Hai%20Muqabula%20720p%20Bluray%20Free%20Dubbed%20%5bCRACKED%5d
https://seesaawiki.jp/maicompressri/d/PROshow%20Producer%205%2e0%2e%20Free%20Final%20Key%20Windows%20wethgian
https://umgenjaycom.chronicle.wiki/d/Helen%20Lethal%20Pressure%20Crush%2024
https://firtusigmist.sokuhou.wiki/d/Telugu%20Dubbed%20Krrish%20%5fHOT%5f%20Full%20Movie
https://seesaawiki.jp/qametlocen/d/Doscar%20Bar%20Restaurante%20Keygen%2013instmankl
https://tiafiturward.memo.wiki/d/SolidWorks%202018%20Activa%20Final%20Pc%20Crack%20Full%20Version%20%2erar%20cloveri
https://seesaawiki.jp/anbritiscor/d/Registration%20Lilwayneiam%20%2erar%20Patch%20Windows%20Utorrent%20Latest%20Free%20scouse
https://druminerdio.playing.wiki/d/Utilitas%20Bangunan%20Hartono%20Purbo%20Pdf%2011
https://socialkeko.com/stevterleova
schoemmo (Tuesday, 15 February 2022 01:29)
7b17bfd26b schoemmo
https://coub.com/stories/3522507-project-igi-2-covert-strike-game-for-pc-full-updated-version
https://coub.com/stories/3522506-sketchup-dibac-plugin-cracked-2014-18-wylhsan
https://coub.com/stories/3522504-rhinojewel-5-0-v5-torrent
https://coub.com/stories/3522503-glyphs-2-5-2-free
https://coub.com/stories/3522502-xforce-keygen-64-bit-autocad-architecture-2019-download-new
https://coub.com/stories/3522501-borracho-estaba-pero-me-acuerdo-pdf-top
https://coub.com/stories/3522500-umeshwar-prasad-economic-geology-pdf-89-_verified_
https://coub.com/stories/3522499-ruslaan-4-movie-free-download-in-hindi-mp4-movie-chabla
https://coub.com/stories/3522498-__link__-zk-attendance-management-2008-ver-3-7-1-build-130-rarbfdcm
https://coub.com/stories/3522496-midnight-hunger-pdf-rar
https://ulli-and-the-usa.jimdofree.com/g%C3%A4stebuch/
forefad (Tuesday, 15 February 2022 02:34)
7b17bfd26b forefad
https://wakelet.com/wake/jFCmjLvcpSxSotH8Kyqgn
https://wakelet.com/wake/0eNE9BchWCGdoz58OmrJn
https://wakelet.com/wake/3PLpjen3hJspBhErLCK12
https://wakelet.com/wake/TXvFWjZjE978eNNb1w0DB
https://wakelet.com/wake/9kWgCB3MivA-db2YEPZ7p
https://wakelet.com/wake/N0cuzvR8kCMG6Sdi5X6NC
https://wakelet.com/wake/seVBA0c_TzCMuT6nUNGRU
https://wakelet.com/wake/evIgNyNzntqkRzKuAJA4e
https://wakelet.com/wake/A4VUKnCqayyWe7TI_5ykS
https://wakelet.com/wake/xKGm9uNekK3eWO7GNaRik
https://topsites.gr/directory/ozonstockholm/
ellycatc (Tuesday, 15 February 2022 04:36)
7b17bfd26b ellycatc
https://wakelet.com/wake/XSfekZkwcceGdXU9fWE1q
https://wakelet.com/wake/DB9iJqfTNzAkU-3mqAl7-
https://wakelet.com/wake/fcSimxTyZ5NGZl-RKH_ZZ
https://wakelet.com/wake/FffFtnEC4vjl_MHTTjXwi
https://wakelet.com/wake/7pCTlMFp6wyxBFGQh2cIz
https://wakelet.com/wake/pXy5QrOLT7pDgLm4CJiK0
https://wakelet.com/wake/f07dMimhPmIXWnMfEPuZ5
https://wakelet.com/wake/R5fxd_RcGIPfahX_6pSMC
https://wakelet.com/wake/aSBsju-GbcpKhCjAyEHXs
https://wakelet.com/wake/Q0Zs8fJi6OgOVDl4RcIm_
https://benri.ocnk.net/bbs
imotait (Tuesday, 15 February 2022 05:42)
7b17bfd26b imotait
https://coub.com/stories/3269413-work-yellow-race-in-america-beyond-black-and-white-books-pdf-file
https://coub.com/stories/3269414-libro-artes-visuales-1-secundaria-pdfl
https://coub.com/stories/3269408-vcds-10-6-0-free-high-quality-download-rar
https://coub.com/stories/3269409-wwe-wrestlemania-2013-brock-lesnar-full-fight-video-free-download-maiscol
https://coub.com/stories/3269407-dhobi-aaya-hindi-rhyme-video-download-link
https://coub.com/stories/3269405-qcm-d-anatomie-2eme-annee-medicine-pdf-11-hot
https://coub.com/stories/3269406-ebony-hardcore-movie-galleries
https://coub.com/stories/3269403-wondershare-dr-fone-2020-crack-with-serial-key-for-windows-and-mac-delblis
https://coub.com/stories/3269401-download-the-haribhari-fertility-link
https://coub.com/stories/3269400-valliddaru-okkate-full-movie-free-14-zanttrud
http://showslife.cn/shownews.asp?id=110
elsraul (Tuesday, 15 February 2022 06:50)
7b17bfd26b elsraul
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCQ0_X0CwwLEgZDb3Vyc2UYgIDAkLPSigsMCxIIQWN0aXZpdHkYgIDA4J-CpggMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDA59C9CwwLEgZDb3Vyc2UYgICA_9OH2QkMCxIIQWN0aXZpdHkYgIDA0O7ZzgsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDAoPbVCAwLEgZDb3Vyc2UYgIDAwODQkwsMCxIIQWN0aXZpdHkYgIDA0KKH5QoMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCAst2-CQwLEgZDb3Vyc2UYgICAv6HDswoMCxIIQWN0aXZpdHkYgIDA4NXTiwoMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_xIirCwwLEgZDb3Vyc2UYgICAn6v4pggMCxIIQWN0aXZpdHkYgIDAgIvz7gkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_xeKfCgwLEgZDb3Vyc2UYgICA_8DehAgMCxIIQWN0aXZpdHkYgIDAkJmsvwoMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_vOPQCwwLEgZDb3Vyc2UYgIDAwJPo9QgMCxIIQWN0aXZpdHkYgIDA4PD6yAoMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDAzKCSCwwLEgZDb3Vyc2UYgICA_4TE-AoMCxIIQWN0aXZpdHkYgIDAkLqZ9QgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_k5-gCQwLEgZDb3Vyc2UYgICAv_67twoMCxIIQWN0aXZpdHkYgIDAkOnpzwsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCA0uvgCAwLEgZDb3Vyc2UYgICA_6SdmgsMCxIIQWN0aXZpdHkYgIDA4NXTiwgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://seesaawiki.jp/sweroslidest/d/Gin%20Liya%20Aasman%20Tamil%20Dubbed%20Torrent
roswai (Tuesday, 15 February 2022 08:01)
7b17bfd26b roswai
https://wakelet.com/wake/eU0oVwSki5omQd2knqkdX
https://wakelet.com/wake/cix0mch9M03YZ3AV2e0tR
https://wakelet.com/wake/GQQl8MBiEmCtMc_Vy2d3a
https://wakelet.com/wake/2vPT0UHt5f2J58XBk-Xsy
https://wakelet.com/wake/yOlbJ1Y2Rb6oLz_lqB14s
https://wakelet.com/wake/JLb-PuelLHvkOqyqK8KdX
https://wakelet.com/wake/WdiUVSIVDc3TlT31kDy_7
https://wakelet.com/wake/T7W_exLPKHk9c7EZq7eT1
https://wakelet.com/wake/vGVIVJ2Ow6CUpmHIDAHId
https://wakelet.com/wake/osLz_JzEhVJB3trZAntFD
http://pkvu.amritavidyalayam.org/values-of-ramayana/
amyfre (Tuesday, 15 February 2022 09:14)
7b17bfd26b amyfre
https://coub.com/stories/3461179-labor-law-reviewer-chan-robles-pdf
https://coub.com/stories/3452257-theevram-2012-1cd-x264-ap-dvdrip-mp4-team-tmr-mkv-welrho
https://coub.com/stories/3452256-wankuri-rar-milmai
https://coub.com/stories/3452255-the-social-network-tamil-dubbed-movie
https://coub.com/stories/3452253-top-human-body-parts-and-functions-in-tamil-pdf-free
https://coub.com/stories/3452248-free-vacation-quest-2-australia-full-precracked-foxy-games-dna-hack
https://coub.com/stories/3452247-adobe-zii-2019-4-5-0-crack-free-download-favval
https://coub.com/stories/3452244-introduction-to-business-book-by-saeed-nasir-pdf-download-best
https://coub.com/stories/3452242-love-guru-movie-download-in-hindi-720p-xantlau
https://coub.com/stories/3452241-life-ok-saubhagyavati-bhava-viraj-ringtone-download-walwkri
http://shahina.rafiq.nzie.org/2021/08/17/miria-our-founder-owner/
chaysch (Tuesday, 15 February 2022 10:23)
7b17bfd26b chaysch
https://coub.com/stories/2988047-final-draft-8-0-3-build-120-keygen-gq-chingliu-__hot__
https://coub.com/stories/2988049-better-elcomsoft-phone-password-breaker-crack-keygen-serial-number
https://coub.com/stories/2988048-free-simplified-iec-risk-assessment-calculator-sirac
https://coub.com/stories/2988046-jai-santoshi-maa-dual-audio-hindi-eng-720p
https://coub.com/stories/2988045-__hot__-juangabrielsudiscografiamediafire
https://coub.com/stories/2988044-signcut-pro-1-07-keygen-fix
https://coub.com/stories/2988043-cell-and-molecular-biology-by-de-robertis-pdf-free-exclusive-download
https://coub.com/stories/2988042-descargar-evopack-2013-torrent-verified
https://coub.com/stories/2988041-the-unliving-pc-game-free-download-venbran
https://coub.com/stories/2988040-exclusive-majboor-hindi-movie-free-download
http://users.atw.hu/imd-multigaming/index.php?site=profile&id=9&action=guestbook&type=ASC&page=1
reewall (Tuesday, 15 February 2022 11:30)
7b17bfd26b reewall
https://trello.com/c/Oq32g2R8/21-xforce-keygen-32bits-or-64bits-version-autocad-mobile-2007-keygen-ileypear
https://trello.com/c/muJYfy0P/36-btc-collector-v50-btc-harvester-utorrent
https://trello.com/c/oYU0KXCP/38-introduccionalafilosofiaantiguaarmstrongpdf13-top
https://trello.com/c/itUsONHr/29-chessbase-fritz-trainer-monster-dvd-collection-fritztrainer-chess-sdvl-139-crisnet
https://trello.com/c/DDpxvTCA/37-hujjatullah-baligha-urdu-pdf-14-bernwalm
https://trello.com/c/kP3co5fQ/26-khiladiyon-ka-khiladi-07-maa-sherawaliye-dj-mix-song-mp3-talapric
https://trello.com/c/3Q6QupYh/41-fix-fsx-p3d-milviz-aircraft-collection-full-version
https://trello.com/c/hKHDkVLZ/70-full-wilcom-e2-all-windows-work-full-crack-link
https://trello.com/c/JaBWc9bQ/23-newstar-sunshine-300-sets-torrent-exclusive
https://trello.com/c/OIg0aYHf/19-verified-removewat-228-mediafire
http://letsgoo.de/index.php?site=profile&id=2&action=guestbook&page=1&type=DESC
petrdevo (Tuesday, 15 February 2022 12:34)
7b17bfd26b petrdevo
https://coub.com/stories/3322439-the-killing-s01-720p-bluray-dts-x264-shunpo-updated
https://coub.com/stories/3322440-himalay-ke-anchal-mein-2-download-720p-movie-link
https://coub.com/stories/3322436-link-sonyexpressfxaudiorestorationzip
https://coub.com/stories/3322434-iifa-awards-2016-full-show-hd-1080p-tollywood-masala-barhan
https://coub.com/stories/3322432-silent-hunter-3-v1-4b-english-no-dvd-fixed-exe-install
https://coub.com/stories/3322430-spac-automazione-2013-torrent-valebaen
https://coub.com/stories/3322428-o-pastor-2009-dublado-dvdrip-torrent-theappo
https://coub.com/stories/3322427-microstation-v8i-ss3-crack-2021
https://coub.com/stories/3322423-forza-motorsport-4-pc-download-torent-exclusive
https://coub.com/stories/3322419-raajneeti-marathi-movie-download-hd-720p-kaeltaga
https://berojgarcoin.com/index.php/2021/08/17/bitcoin-news-hindi-2/
elischan (Tuesday, 15 February 2022 14:00)
7b17bfd26b elischan
https://trello.com/c/tqzooo12/24-new-tweak-order-v104-patch-6b
https://trello.com/c/oeqH86ts/46-cum-photo-editor-nennzeth
https://trello.com/c/Wkt2IGE0/31-uninstall-tool-296-build-5100-rus-crack-top
https://trello.com/c/ZDgsEKMj/47-hot-tabel-montage-tijden-conform-gustav-ende-normxls
https://trello.com/c/K5r9AwMt/26-netlux-antivirus-product-key-free-download-torrent-211-rebham
https://trello.com/c/Bwwft5Gm/57-mass-gmail-account-creator-2177-cracked-by-omega-better
https://trello.com/c/wkfPECbs/71-xforce-free-keygen-32bits-or-64bits-version-autocad-design-suite-2018-crack
https://trello.com/c/wPnLlWzQ/51-hack-acoustica-mixcraft-v81-build-394-final-keygen-sh-verified
https://trello.com/c/bfPc1ZYB/37-dark-souls-iii-update-v1-03-1-codex-new
https://trello.com/c/qO5R01gd/48-ul
http://sagodilaszlo.com/index.php/component/kide/tortenet/-/index.phpoption=com_kide
fatgide (Tuesday, 15 February 2022 15:02)
7b17bfd26b fatgide
https://trello.com/c/FxKVZJKn/85-exclusive-financial-management-by-i-m-pandey
https://trello.com/c/3ChgOldg/32-skyrim-animated-prostitution-v13
https://trello.com/c/PVnqIuYI/85-zero-no-tsukaima-season-5-sub-in-jamygaly
https://trello.com/c/0i8AniJK/55-wondershare-dr-fone-email-and-registration-code
https://trello.com/c/kZFbGB6p/94-freshmaza-3gp-xxx-video-download-2021
https://trello.com/c/oWcN79MV/60-raxco-perfectregistry-2003167-medicinebabupc-serial-key-keygen-netaarmi
https://trello.com/c/TAojvdFW/31-ccspstudyguidepdffreedownload-link
https://trello.com/c/Mzh8mt0o/43-download-xforce-full-keygen-bim-360-docs-2012-download
https://trello.com/c/WMxO0wfD/37-stand-ofood-3-crack-verified-download
https://trello.com/c/XSvNutN1/29-id-battlefield-2142-offline-exclusive-crack
http://renargunther.com/2012/02/courting-courtney/
tananene (Tuesday, 15 February 2022 16:03)
7b17bfd26b tananene
https://wakelet.com/wake/TSqNQRcpmaHq-o677e-nE
https://wakelet.com/wake/x3Om9JvvAxeIFWrPhTS40
https://wakelet.com/wake/3HXxDXYmiQjNWEKlvSIv-
https://wakelet.com/wake/npEkEaVpzjx1WESWcO3Sp
https://wakelet.com/wake/0HLphbvw9aK1V4e2jEJpU
https://wakelet.com/wake/6-0ser8PnzmFqd86AeZFO
https://wakelet.com/wake/g-XT0-h-Ue_UrcbGCIi2x
https://wakelet.com/wake/qnWONlo1jAmc2tpiFoZNI
https://wakelet.com/wake/w74nHgQSeso5s_cFO87CU
https://wakelet.com/wake/0TFaL4PCJxxUJGXl9uJYr
http://cocaoclub.ee/ka_omanikule2/
berwalf (Tuesday, 15 February 2022 17:05)
7b17bfd26b berwalf
https://wakelet.com/wake/5S2vqqcyCQV5532V98t84
https://wakelet.com/wake/zhSi30bXatGxIPtNgl2ZT
https://wakelet.com/wake/qiG2uAAatVNKV9Dr8DKK1
https://wakelet.com/wake/ysQOCW9M7J9wIKOAmaBN1
https://wakelet.com/wake/DC6BQqlV2zgmmiVXvkn4c
https://wakelet.com/wake/IeJAyH_VbrvnuigkFecEF
https://wakelet.com/wake/Lq3RgR5Y5H2PJpECZS9-L
https://wakelet.com/wake/C0Zq1fMrhedtRYO3eqduL
https://wakelet.com/wake/dZtisz5qFoZfzsXIJ6u0C
https://wakelet.com/wake/y0C-jRPI43l-PFQewDM9a
https://mchughmchugh5.webs.com/apps/blog/show/47587961-leading-things-to-experience-found-in-zanzibar
sanctre (Tuesday, 15 February 2022 18:07)
7b17bfd26b sanctre
https://seesaawiki.jp/belwcapefo/d/Eclipse%20Ucnv884%20Mkii%20Ual%20Free%20Utorrent%20Epub%20Book%20Rar
https://seesaawiki.jp/setceberless/d/Farmakope%20Indonesia%20Edisi%203golkes%20%5bepub%5d%20Free%20Rar%20Book%20Utorrent
https://seesaawiki.jp/writimdero/d/Synthesia%20Full%20Version%20Apk%20Downloadk
https://seesaawiki.jp/tansatica/d/%5bVERIFIED%5d%20The%20Wild%20And%20Won%20%2erar%20Serial%20X64%20Windows
https://seesaawiki.jp/egberpocent/d/Mission%3a%20Impossible%20%2d%20Rogue%20Nation%20%28English%29%20Movies%20In%20Hindi%20Free%20Download
https://seesaawiki.jp/neuniosafbea/d/Snoop%20Dogg%20Paid%20Tha%20Cost%20To%20Be%20Da%20Boss%20%7cVERIFIED%7c%20Full%20Album%20Zip
https://seesaawiki.jp/scobsarjesi/d/Biologia%20Marinha%20Peter%20Castro%20Ebook%20%2emobi%20Torrent%20Rar%20Free
https://seesaawiki.jp/froninelam/d/Won%20Rshare%20QuizCrea%20Pc%20Patch%20Download%20Activation%20Zip%20Latest%2032%20capilenn
https://seesaawiki.jp/swapledefsubs/d/Signcut%20Pro%201%2096%20Keygen%2029
https://seesaawiki.jp/nicwadehcou/d/CorelDRAW%20Graphics%20Suite%202019%20MacOS%20Torrent
https://www.tropicalxplorers.com/costa-rica-indigenous-community-bri-bri/
vinirege (Tuesday, 15 February 2022 19:10)
7b17bfd26b vinirege
https://wakelet.com/wake/XD7wkEtWmu0WTMQu4mHnT
https://wakelet.com/wake/Lxkib6YwcfwGw-yg5Hwl5
https://wakelet.com/wake/ouaY6E4FKICDZF-RbiFT6
https://wakelet.com/wake/6EZpYoCPlbQcSKNBFimDU
https://wakelet.com/wake/I6j8RN-YDuLAoKH2WsqI6
https://wakelet.com/wake/FwRcGbIqxcQP2ZcEqKwPo
https://wakelet.com/wake/3-OPn5JMD1FNb0wd79x_Z
https://wakelet.com/wake/zSesR3tGP6q8QJg9CTN4t
https://wakelet.com/wake/ytAQwvfQVhNHqlQpI7hMl
https://wakelet.com/wake/KgtnkocEVe5fygtxIne9X
https://www.glaadblog.org/how-using-online-platform-makes-dish-tv-recharge-hassle-free/
denfall (Tuesday, 15 February 2022 20:14)
7b17bfd26b denfall
https://coub.com/stories/3389140-pika-software-builder-6-0-0-4-hot-crack
https://coub.com/stories/3389139-indian-payroll-software-free-download-full-version-free
https://coub.com/stories/3389138-rockstar-2-full-movie-free-download-in-hindi-patched
https://coub.com/stories/3389136-the-lunchbox-download-dvdrip-movies-new
https://coub.com/stories/3389137-naaigal-jaakirathai-movie-free-download-utorrentl-top
https://coub.com/stories/3389135-i-am-so-lonely-broken-angel-mp4-song-download-work
https://coub.com/stories/3389133-download-bass-treble-booster-full-crack-mansdar
https://coub.com/stories/3389134-exclusive-arundhati-tamil-film-free-download
https://coub.com/stories/3389132-full-waves-all-plugins-bundle-v9-r15-windows-bredall
https://coub.com/stories/3389131-synthmaster-one-vsti-aax-v1-3-4-ce-v-r-better
https://crystalhygieneproducts.com/product/all-type-clothes-washing-powder/
denfall (Tuesday, 15 February 2022 20:14)
7b17bfd26b denfall
https://coub.com/stories/3389140-pika-software-builder-6-0-0-4-hot-crack
https://coub.com/stories/3389139-indian-payroll-software-free-download-full-version-free
https://coub.com/stories/3389138-rockstar-2-full-movie-free-download-in-hindi-patched
https://coub.com/stories/3389136-the-lunchbox-download-dvdrip-movies-new
https://coub.com/stories/3389137-naaigal-jaakirathai-movie-free-download-utorrentl-top
https://coub.com/stories/3389135-i-am-so-lonely-broken-angel-mp4-song-download-work
https://coub.com/stories/3389133-download-bass-treble-booster-full-crack-mansdar
https://coub.com/stories/3389134-exclusive-arundhati-tamil-film-free-download
https://coub.com/stories/3389132-full-waves-all-plugins-bundle-v9-r15-windows-bredall
https://coub.com/stories/3389131-synthmaster-one-vsti-aax-v1-3-4-ce-v-r-better
https://crystalhygieneproducts.com/product/all-type-clothes-washing-powder/
juanind (Tuesday, 15 February 2022 21:18)
7b17bfd26b juanind
https://coub.com/stories/3057950-chaar-sahibzaade-utorrent-download-daemtry
https://coub.com/stories/3057951-official-motorola-moto-g7-play-xt1952-4-channel-stock-rom
https://coub.com/stories/3057952-mystery-case-files-13th-skull-download-free-full-version-kenmaky
https://coub.com/stories/3057953-pads-pcb-design-software-crack-repack-download
https://coub.com/stories/3057956-bermuda-triangle-movie-in-hindi-download-free-jezimig
https://coub.com/stories/3041681-free-hip-hop-abs-deluxe-torrent
https://coub.com/stories/3037081-easy-poster-printer-v3-0-2-0-full-serial-keygen-top
https://coub.com/stories/3037080-pareto-dr-setup-rw-license-key-crack-work
https://coub.com/stories/3037078-gerber-omega-5-torrent-_hot_
https://coub.com/stories/3037075-windows-7-8-10-loader-activator-v6-2-11-reloaded-best-crack
https://sommerzaubermarkt.de/index.php/component/k2/item/33-kremerkram2
juanind (Tuesday, 15 February 2022 21:19)
7b17bfd26b juanind
https://coub.com/stories/3057950-chaar-sahibzaade-utorrent-download-daemtry
https://coub.com/stories/3057951-official-motorola-moto-g7-play-xt1952-4-channel-stock-rom
https://coub.com/stories/3057952-mystery-case-files-13th-skull-download-free-full-version-kenmaky
https://coub.com/stories/3057953-pads-pcb-design-software-crack-repack-download
https://coub.com/stories/3057956-bermuda-triangle-movie-in-hindi-download-free-jezimig
https://coub.com/stories/3041681-free-hip-hop-abs-deluxe-torrent
https://coub.com/stories/3037081-easy-poster-printer-v3-0-2-0-full-serial-keygen-top
https://coub.com/stories/3037080-pareto-dr-setup-rw-license-key-crack-work
https://coub.com/stories/3037078-gerber-omega-5-torrent-_hot_
https://coub.com/stories/3037075-windows-7-8-10-loader-activator-v6-2-11-reloaded-best-crack
https://sommerzaubermarkt.de/index.php/component/k2/item/33-kremerkram2
juanind (Tuesday, 15 February 2022 21:20)
7b17bfd26b juanind
https://coub.com/stories/3057950-chaar-sahibzaade-utorrent-download-daemtry
https://coub.com/stories/3057951-official-motorola-moto-g7-play-xt1952-4-channel-stock-rom
https://coub.com/stories/3057952-mystery-case-files-13th-skull-download-free-full-version-kenmaky
https://coub.com/stories/3057953-pads-pcb-design-software-crack-repack-download
https://coub.com/stories/3057956-bermuda-triangle-movie-in-hindi-download-free-jezimig
https://coub.com/stories/3041681-free-hip-hop-abs-deluxe-torrent
https://coub.com/stories/3037081-easy-poster-printer-v3-0-2-0-full-serial-keygen-top
https://coub.com/stories/3037080-pareto-dr-setup-rw-license-key-crack-work
https://coub.com/stories/3037078-gerber-omega-5-torrent-_hot_
https://coub.com/stories/3037075-windows-7-8-10-loader-activator-v6-2-11-reloaded-best-crack
https://sommerzaubermarkt.de/index.php/component/k2/item/33-kremerkram2
juanind (Tuesday, 15 February 2022 21:20)
7b17bfd26b juanind
https://coub.com/stories/3057950-chaar-sahibzaade-utorrent-download-daemtry
https://coub.com/stories/3057951-official-motorola-moto-g7-play-xt1952-4-channel-stock-rom
https://coub.com/stories/3057952-mystery-case-files-13th-skull-download-free-full-version-kenmaky
https://coub.com/stories/3057953-pads-pcb-design-software-crack-repack-download
https://coub.com/stories/3057956-bermuda-triangle-movie-in-hindi-download-free-jezimig
https://coub.com/stories/3041681-free-hip-hop-abs-deluxe-torrent
https://coub.com/stories/3037081-easy-poster-printer-v3-0-2-0-full-serial-keygen-top
https://coub.com/stories/3037080-pareto-dr-setup-rw-license-key-crack-work
https://coub.com/stories/3037078-gerber-omega-5-torrent-_hot_
https://coub.com/stories/3037075-windows-7-8-10-loader-activator-v6-2-11-reloaded-best-crack
https://sommerzaubermarkt.de/index.php/component/k2/item/33-kremerkram2
chervin (Tuesday, 15 February 2022 22:22)
7b17bfd26b chervin
https://trello.com/c/Hwi7uBQ8/25-sfarsitul-ceausestilor-grigore-cartianu-pdf-30-blescar
https://trello.com/c/pRHZcumZ/46-haunted-3d-mp4-full-movie-free-download-marigiov
https://trello.com/c/pHSKgokP/51-better-mouse-guard-rpg-2nd-edition-pdf-download
https://trello.com/c/RtpNWdg3/48-hot-simon-scarrow-britannia-epub-download
https://trello.com/c/saBvpZ6n/71-direkt-2-neu-testygolkeszip
https://trello.com/c/ZeexaP3D/27-ls-land-issue-15-little-duchess-1-10-ranfryd
https://trello.com/c/QrMJn3sa/18-download-windows-xp-64-bit-iso-highly-compressed-upd
https://trello.com/c/Vzs7A7RK/17-google-maps-email-extractor-full-version-casnar
https://trello.com/c/AgKSABgV/32-new-adobe-cs6-products-activator
https://trello.com/c/BEhZfquS/41-convicciones-mas-que-creencias-pdf-descargar-free-haiefra
http://users.atw.hu/t-gaming-/index.php?site=profile&id=268&action=guestbook&page=1&type=ASC
salkaf (Tuesday, 15 February 2022 23:27)
7b17bfd26b salkaf
https://coub.com/stories/3381094-jascpaintshoppro9trialserial21
https://coub.com/stories/3381093-new-hello-movie-english-subtitles-download
https://coub.com/stories/3381092-better-hung-season-1-complete-720p-torrent
https://coub.com/stories/3381091-install-autodesk-fusion-360-2-0-6668-crack-full-latest-version-2020
https://coub.com/stories/3381089-worldfree4u-com-commando-a-one-man-army-2013-movie-in-hd-full
https://coub.com/stories/3381090-biologia-delle-piante-raven-pdf-coligenn
https://coub.com/stories/3381088-mega-shows-v7-1-0-mod-ad-free-latest-verified
https://coub.com/stories/3381087-libro-de-motores-de-sanz-acebes-santiago-en-pdf-pdf-added-by-users-verified
https://coub.com/stories/3381085-__link__-pk-telugu-movie-download-mp4
https://coub.com/stories/3381086-verified-extra-speed-anna-nevzorova-darsi-lora-zhenya-torrent-full-version
https://seesaawiki.jp/boacisunso/d/Girls%20mixed%2007%2e%2c%20mix%20357881%20%2815%29%20%40iMGSRC%2eRU
salkaf (Tuesday, 15 February 2022)
7b17bfd26b salkaf
https://coub.com/stories/3381094-jascpaintshoppro9trialserial21
https://coub.com/stories/3381093-new-hello-movie-english-subtitles-download
https://coub.com/stories/3381092-better-hung-season-1-complete-720p-torrent
https://coub.com/stories/3381091-install-autodesk-fusion-360-2-0-6668-crack-full-latest-version-2020
https://coub.com/stories/3381089-worldfree4u-com-commando-a-one-man-army-2013-movie-in-hd-full
https://coub.com/stories/3381090-biologia-delle-piante-raven-pdf-coligenn
https://coub.com/stories/3381088-mega-shows-v7-1-0-mod-ad-free-latest-verified
https://coub.com/stories/3381087-libro-de-motores-de-sanz-acebes-santiago-en-pdf-pdf-added-by-users-verified
https://coub.com/stories/3381085-__link__-pk-telugu-movie-download-mp4
https://coub.com/stories/3381086-verified-extra-speed-anna-nevzorova-darsi-lora-zhenya-torrent-full-version
https://seesaawiki.jp/boacisunso/d/Girls%20mixed%2007%2e%2c%20mix%20357881%20%2815%29%20%40iMGSRC%2eRU
brygcha (Wednesday, 16 February 2022 00:30)
7b17bfd26b brygcha
https://trello.com/c/1RJvkykb/28-bob-esponja-pelicula-1080p-torrent-julidafn
https://trello.com/c/HWbjWv3K/43-kitab-sirah-nabawiyah-ibnu-hisyampdf
https://trello.com/c/CGOaxGI8/20-sims-3-pets-crack-fairlightrar-exclusive
https://trello.com/c/AWxsK0on/36-hd-online-player-madras-cafe-movie-download-in-hd-108-hot
https://trello.com/c/QgetxGbF/32-hot-webroot-secureanywhere-antivirus-v902661-keys-free-download
https://trello.com/c/kXO3BRNw/75-inpixio-photo-editor-home-v156024-keygen-top-crackingpatchingunblockedtube
https://trello.com/c/pimnH227/18-antares-autotune-5-crack-rar-berulde
https://trello.com/c/9xmzxWbj/26-upd-medal-of-honor-warfighter-free-download-pc-full-version
https://trello.com/c/XtQECM7I/32-better-xforce-keygen-autocad-map-3d-2008-32-bit-download
https://trello.com/c/W9ZOGXM7/16-mixcraft-9-pro-studio-90-build-447-crack-full-version-registration-code-2020-cracked
https://freedomhempco.com/product/freedom-hemp-logo-black-tee/
hemeelee (Wednesday, 16 February 2022 01:38)
7b17bfd26b hemeelee
https://trello.com/c/C9qIjtQc/21-hot-kal-ho-na-ho-720p-full-movie-download-l
https://trello.com/c/32tPIHqL/45-exclusive-ul
https://trello.com/c/jwdnPmT8/64-vaishali-telugu-movie-english-subtitles-download-install
https://trello.com/c/JFEvodlM/91-bahubali-the-beginning-new-full-movie-download-in-720p-1080p
https://trello.com/c/A5yUpldp/35-sultan-malayalam-full-movie-free-download-utorrent-top
https://trello.com/c/Oc1NA1S0/30-ratiborus-kms-tools-01042018-ellculry
https://trello.com/c/9zz341m4/37-fixed-repair-2911-format-flash-driverar
https://trello.com/c/Tf23psWe/39-wargame-1942-cheat-v19223-new
https://trello.com/c/Kvoai5je/19-demi-lovato-stay-strong-documentary-sub-ita
https://trello.com/c/Oxoatyrr/25-midilagubarat
https://kraftwerk-rps.com/es/pasion-y-compromiso-para-disenar-y-construir-plantas-solares-fotovoltaicas/
harcha (Wednesday, 16 February 2022 02:48)
7b17bfd26b harcha
https://coub.com/stories/3503801-vso-convertxtodvd-3-5-2-137-keygen-full-version-berrea
https://coub.com/stories/3503800-arma-2-combined-operations-free-download-full-game-dayz-download-ireabern
https://coub.com/stories/3503799-hulara-video-song-download-1080p-wallpaper-updated
https://coub.com/stories/3503798-verified-native-instruments-massive-1-3-0-serial-number-modellatore-suona-ar
https://coub.com/stories/3503797-2-stroke-wizard-tuned-pipe-pro-v4-rar-karjoa
https://coub.com/stories/3503796-marumalarchi-film-cut-songs-17
https://coub.com/stories/3503795-koleksi-kontol-polisi2-portable
https://coub.com/stories/3503794-the-marine-john-cena-full-movie-free-exclusive-download
https://coub.com/stories/3503793-tera-pyar-hookah-bar-download-songs-pk-updated
https://coub.com/stories/3503791-upgrade-starsat-srx97-usb-titanium
http://mayco.com.mx/contacto/
odilund (Wednesday, 16 February 2022 03:57)
7b17bfd26b odilund
https://trello.com/c/Xnlao5RO/39-wave-l2-ultramaximizer-upd-free-download
https://trello.com/c/ZhR0bki1/42-magix-movie-edit-pro-premium-2018-v160249-new-crack-64-bit
https://trello.com/c/lO0Iyi5J/27-verified-autodesk-autocad-20181-crack-full-keygen-64-bit-download-free-latest
https://trello.com/c/klnRFBmc/17-avila-acosta-roberto-estadistica-elemental-badgnoel
https://trello.com/c/eMUnqlgh/14-galaxy-trucker-extended-edition-download-no-crack-otilpea
https://trello.com/c/vtrMNv3B/96-fsx-aussim-piper-warrior-ii-iii-portable-crack-free
https://trello.com/c/Ep5nfYTy/37-fixed-biology-book-for-class-9-sindh-board
https://trello.com/c/XxF0xbdo/66-civilization-5-world-builder-skidrow-keylcall
https://trello.com/c/SupxAXFQ/26-ultraviolet-2006-dualhindi-englishdd-20-139gb-1080p-blu-ray-x264-xrg-bilmar
https://trello.com/c/t1reOrNo/35-light-image-resizer-6092-portable-patch-rar
http://safety1stsafety.com/ar/module/smartblog/details?id_post=10&slug=Video-Tour-Of-American-Safety
rayroel (Wednesday, 16 February 2022 05:03)
7b17bfd26b rayroel
https://seesaawiki.jp/calnaepolra/d/Machine%20Free%20%2erar%20Utorrent%20Keygen%20Extra%20Quality
https://seesaawiki.jp/trabarafter/d/Microsoft%20Flight%20Simula%2064bit%20Crack%20UPDATEDed%20Activator%20Full%20Version
https://seesaawiki.jp/prehacgocorn/d/Hibijyon%20Sc%2024%2026
https://seesaawiki.jp/verfmandhearca/d/%5f%5fFULL%5f%5f%20Build%20Orc%20Strongholds%20Skyrim%20Map%20Full%20Version%20Download%20Activator
https://seesaawiki.jp/retlamulcei/d/Librosderadionicapdf17
https://seesaawiki.jp/waismutarot/d/Sicario%20%21FREE%21%20Full%20Movie%20In%20Hindi%20Dubbed%201118
https://seesaawiki.jp/ncenarinam/d/GTA%20SAN%20ANDREAS%20PTBR%20CRACKEADO%20Keygen
https://seesaawiki.jp/clemnewdelog/d/Dal%20Cim%20500%20Crack%20Isolation%20Membranes
https://seesaawiki.jp/jaicialispart/d/Driver%20Genius%20PRO%2010%2e0%2e0%2e712%20Crack%2d%5bHB%5d
https://seesaawiki.jp/pubgosandscig/d/Jira%20License%20Key%20Crack
https://feniks-ops.ru/chto-vy-poluchite/
zelmign (Wednesday, 16 February 2022 06:10)
7b17bfd26b zelmign
https://wakelet.com/wake/XtkM7COqbqrSAnBLxpZ-M
https://wakelet.com/wake/6GF93Ixkjtc6PzrgPZcSe
https://wakelet.com/wake/fUV1CmerV0XB61eLNXG2t
https://wakelet.com/wake/Mkuo-q_hkqCyuqLwZZVJO
https://wakelet.com/wake/2aEKLk7o3Eb8cA_3tad1G
https://wakelet.com/wake/TARqimCPR6Lj6b1Jv8iCo
https://wakelet.com/wake/Ljdk2dkOgAKBVjdV_-6kG
https://wakelet.com/wake/01w4WcozSPyLNGoHhPsXs
https://wakelet.com/wake/uha0QbK1CLnW35oXXHv3B
https://wakelet.com/wake/T86HMQ-dbBXUxY1oX8d3P
https://allsporters.com/genscorrestsem
modekei (Wednesday, 16 February 2022 07:18)
7b17bfd26b modekei
https://coub.com/stories/3256121-prva-hrvatska-lchf-kuharica-pdf-105-stepsame
https://coub.com/stories/3256118-download-indian-school-girls-3gp-king-rape-erbiwor
https://coub.com/stories/3256119-numega-smartcheck-6-2-1286-rc2-portable-51
https://coub.com/stories/3256117-anydvd-5-3-2-1-clonedvd-2-8-5-1-clonecd-5-2-6-1-dvd-decryp-utorrent
https://coub.com/stories/3256111-jurassic-world-alive-astuce-triche-argent-et-pieces-illimite
https://coub.com/stories/3256110-skyfall-full-movie-free-download-hd-720p-trekayd
https://coub.com/stories/3256109-free-filmora-crack-key
https://coub.com/stories/3256108-international-law-book-by-agarwal-pdf-16-lateqit
https://coub.com/stories/3256107-wells-j-c-english-intonation-pdf-40-jonzom
https://coub.com/stories/3256106-pdf-east-syrian-daily-offices
https://www.dewandakwahaceh.com/pergumulan-syariat-islam/
collazh (Wednesday, 16 February 2022 08:49)
7b17bfd26b collazh
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_hZyTCwwLEgZDb3Vyc2UYgICAn-v31ggMCxIIQWN0aXZpdHkYgIDAkJq3jgkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDAk9izCQwLEgZDb3Vyc2UYgIDAkPO8oAsMCxIIQWN0aXZpdHkYgIDAwLPRqggMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDgj4PkCAwLEgZDb3Vyc2UYgIDAkNOi6ggMCxIIQWN0aXZpdHkYgIDA0K2JrQgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_poq9CAwLEgZDb3Vyc2UYgICA_4X6pAgMCxIIQWN0aXZpdHkYgIDAoOrwrAkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCAkb7qCQwLEgZDb3Vyc2UYgIDAwOfMuQsMCxIIQWN0aXZpdHkYgIDAoOrw7AgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDgpdnNCgwLEgZDb3Vyc2UYgIDA4ODW8QoMCxIIQWN0aXZpdHkYgIDA4PDspgsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDQwP6ECgwLEgZDb3Vyc2UYgIDA0Jze1QgMCxIIQWN0aXZpdHkYgIDAkJms2QsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgIC_vZuXCgwLEgZDb3Vyc2UYgICA_4TE4AsMCxIIQWN0aXZpdHkYgIDAkOvF5goMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCQi_3pCgwLEgZDb3Vyc2UYgIDAkMnKygsMCxIIQWN0aXZpdHkYgICA_4-zvwgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDA9KWhCAwLEgZDb3Vyc2UYgICA_4TpmgsMCxIIQWN0aXZpdHkYgIDA4O-qgwkMogEQNTcyODg4NTg4Mjc0ODkyOA
http://www.vl-events.co.uk/product/fga-30/
watnefe (Wednesday, 16 February 2022 09:56)
7b17bfd26b watnefe
https://wakelet.com/wake/eev6ZMfvWNen4uDkoOlkV
https://wakelet.com/wake/6xP20UCwji1ptMFBVWi3A
https://wakelet.com/wake/7AJaPmyQVbCSp9Og5A4ge
https://wakelet.com/wake/7LUN-XYGppVE2X7X1L8jV
https://wakelet.com/wake/YQw2LZjAn-pKXjeeoFhj8
https://wakelet.com/wake/pzCzCPpiZiqL5603c6zak
https://wakelet.com/wake/0J-5ui0O9lBMOdmTOFKxg
https://wakelet.com/wake/Ci3lhd3nObEi8WJtZ_d8l
https://wakelet.com/wake/90deOMMBHlptP73ZqM9zq
https://wakelet.com/wake/HmiWr8Q5Wt_QT84DX6mgT
https://www.trendingnews.it/denise-pipitone-colpo-scena-blitz-cadavere-murato/
nelgle (Wednesday, 16 February 2022 10:57)
7b17bfd26b nelgle
https://coub.com/stories/3498217-full-silverfast-8-crack-13-derowand
https://coub.com/stories/3498216-gaytonmckenziebooktheuncomfortabletruthpdfdownload-vandher
https://coub.com/stories/3498215-top-mirror-for-philips-tv-2-0-mac-os-x
https://coub.com/stories/3498214-assimil-inglese-senza-sforzo-4-cd-nuova-versione-by-drxuni-13-better
https://coub.com/stories/3498211-free-camtasia-studio-v8-0-2-918-serials-chattchitto-rg-download-pc
https://coub.com/stories/3498213-doc-lks-bahasa-indonesia-smp-kelas-7-semester-2-sentez-trojans-froid-lenzadon
https://coub.com/stories/3498212-the-kaal-movie-__top__-download-720p
https://coub.com/stories/3498210-farmville-2-koy-kacamag-apk-full-updated-1-9-112-hile-modapk
https://coub.com/stories/3498209-top-yol-hereketi-qaydalari-kitabi-pdf
https://coub.com/stories/3498208-upd-ogc-aimbot-download-19l
https://www.drhasandogan.com/en/3rd-national-prolotherapy-symposium-advisory-board/
enriwest (Wednesday, 16 February 2022 11:58)
7b17bfd26b enriwest
https://coub.com/stories/3007414-psw900-swissphone-software-torrent
https://coub.com/stories/3007413-pirate-storm-bot-top-download
https://coub.com/stories/3007410-gta-v-grand-theft-auto-5-rar-password-jeraglo
https://coub.com/stories/3007411-video-gratis-donne-che-scopano-con-animali-cani-o-cavalli
https://coub.com/stories/3007409-hot-gta-5-patch-online-v9-1-crack-online-new
https://coub.com/stories/3007408-vengeance-minimal-house-vol-2-rar-gavrchr
https://coub.com/stories/3007407-designexpertcrackkeygenserialnumber-top
https://coub.com/stories/3007404-__top__-granta-design-ces-edupack-crack
https://coub.com/stories/3007401-spotonthemouse-2-7-1-serial-best
https://coub.com/stories/3007400-hd-online-player-qayamat-movie-full-hd-download-full
https://reparomaquinas.com/blog/2_what-is-bootstrap.html
bradran (Wednesday, 16 February 2022 13:03)
7b17bfd26b bradran
https://wakelet.com/wake/WoCJBAeGPXhRzYAvJCcfw
https://wakelet.com/wake/vBshrzSlqEeR-AZ7V9mdv
https://wakelet.com/wake/-xAe2oQbUxmtjLZd8aUEY
https://wakelet.com/wake/npyw5TnS5Ys3n-U2BuoDE
https://wakelet.com/wake/fofJWIz0f7Xx2GNspCnuE
https://wakelet.com/wake/v27bjh3VdSc2KFmnCLvUw
https://wakelet.com/wake/U_yLmLTfLiWhuvmHnTJmu
https://wakelet.com/wake/BfXgZymHpbkxhHJjz8D-D
https://wakelet.com/wake/MXVRp_ODsRCpF0fR5nzFV
https://wakelet.com/wake/4y6wuSbdjBUmDfkNVsQrC
http://fussballforum-mv.de/forum/index.php?page=UserGuestbook&userID=69729&pageNo=1
iolman (Wednesday, 16 February 2022 14:06)
7b17bfd26b iolman
https://coub.com/stories/3402432-wic-reset-utility-crack-v-222000049-_best_
https://coub.com/stories/3392373-download-link-malayalam-memories-in-march-movie-in-2015-in-kickass-torrent
https://coub.com/stories/3392370-design-review-2010-keygens-only-x-force-32-64bits-rh-download-pc-updated
https://coub.com/stories/3392372-gunday-hd-video-songs-1080p-blu-ray-olwyeldr
https://coub.com/stories/3392371-download-navegador-igo-primo-v85-baixar-gratis-natrea
https://coub.com/stories/3392369-software-magalhaes-2-mg2-pt-by-mogabyte-free
https://coub.com/stories/3392368-conversation-with-mani-ratnam-pdf-free-download-_hot_
https://coub.com/stories/3392367-download-panasonic-motiondv-studio-for-windows-7-epub-__full__
https://coub.com/stories/3392366-farcry3razor1911passwordtxtrar
https://coub.com/stories/3392365-downloadfilmsoehokgie40-work
https://network.ikonne.com/stimebtolo
glynbold (Wednesday, 16 February 2022 15:14)
7b17bfd26b glynbold
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgIC_g7qzCAwLEgZDb3Vyc2UYgICA_4SE-goMCxIIQWN0aXZpdHkYgIDA4O68nQsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgICfy4_wCgwLEgZDb3Vyc2UYgIDAwPSQ5gkMCxIIQWN0aXZpdHkYgIDAgNP5lQsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCgkZ3fCgwLEgZDb3Vyc2UYgIDAoMiahQsMCxIIQWN0aXZpdHkYgIDA0JzvoAgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCQ8rb3CwwLEgZDb3Vyc2UYgIDAwJPCjQkMCxIIQWN0aXZpdHkYgIDAkKmh6QsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCQ0-HFCgwLEgZDb3Vyc2UYgIDAkPKixwoMCxIIQWN0aXZpdHkYgIDAkKrKngkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgIC_39XICAwLEgZDb3Vyc2UYgICA3_GepwsMCxIIQWN0aXZpdHkYgIDAoIrZrAkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCAuI_6CgwLEgZDb3Vyc2UYgICA_6aKpAgMCxIIQWN0aXZpdHkYgIDAkLj83QgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCg0qPYCgwLEgZDb3Vyc2UYgIDAwJOSiwgMCxIIQWN0aXZpdHkYgIDAkKqgzggMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCghKWrCQwLEgZDb3Vyc2UYgIDAwMebrwkMCxIIQWN0aXZpdHkYgIDA4M-zkQsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDQ7NHVCwwLEgZDb3Vyc2UYgIDAwJP8zAgMCxIIQWN0aXZpdHkYgIDAoIrOtQgMogEQNTcyODg4NTg4Mjc0ODkyOA
http://4k.htxd.net.cn/message/message.php?lang=en
tasnil (Wednesday, 16 February 2022 16:18)
7b17bfd26b tasnil
https://wakelet.com/wake/XLeADSOondfhY4ZaJRJ6v
https://wakelet.com/wake/AL08fdvKXTzYgTqi0AoHc
https://wakelet.com/wake/lcGjnaOQ6u2nXeq42hmbI
https://wakelet.com/wake/lGk1NiR5DM9wK6f9x4681
https://wakelet.com/wake/zQpjWHOWvuPnGwONY34SU
https://wakelet.com/wake/2ZPb_xPDRYEHId4AzsnIi
https://wakelet.com/wake/9KL-g9HZ-ceQ6BM17sT_1
https://wakelet.com/wake/dNZQ7SYDiP-rYrTvZ58Q3
https://wakelet.com/wake/xZ9onhhLkDkeZDkK3ClpW
https://wakelet.com/wake/UcKWB9wzjpDy6oDPeVdNW
http://users.atw.hu/t-gaming-/index.php?site=profile&id=2837&action=guestbook
perrwal (Wednesday, 16 February 2022 17:21)
7b17bfd26b perrwal
https://wakelet.com/wake/JtbvDOup96OogpISQ40ws
https://wakelet.com/wake/NulgCWIGTVXo5S_h3riIg
https://wakelet.com/wake/SFFzGlOzppcUh_BDvaW3F
https://wakelet.com/wake/6pc7icSSlng-mSRAdikoa
https://wakelet.com/wake/M3zrSmr_RYWSRryQ7kMzT
https://wakelet.com/wake/3wazxEuZshTmmU_NXfRLk
https://wakelet.com/wake/99rbxF6K3q-J_cwXHgzqE
https://wakelet.com/wake/abEcoE0b-Yy-9hl14nSO_
https://wakelet.com/wake/ogD4w4Sm8L1nGcS3Yxn_L
https://wakelet.com/wake/f9DlHTdrWgpgr2hweKxsY
https://www.comprandovino.com/blog/9_5-IMPRESCINDIBLES-PARA-REGALAR-EN-SAN-VALENTI.html
henamf (Wednesday, 16 February 2022 18:25)
7b17bfd26b henamf
https://trello.com/c/wEOR8GXM/38-al-rassam-al-arabi-v31-r1-keygen-sadiise
https://trello.com/c/uzlSnZ9i/44-madilyn-bailey-the-covers-vol-4-edvawal
https://trello.com/c/MmgVw4mH/22-cocktail-movie-full-cracked-in-tamil-hd-1080p
https://trello.com/c/dg1XrAW9/53-solucionario-mecanica-de-materiales-fitzgeraldl
https://trello.com/c/TJdAtpCo/41-concept-of-physics-h-c-verma-volume-2-full-book-olyale
https://trello.com/c/SHrZWKZD/75-blue-point-mt139a-tachometer-pdf-manual-pdf
https://trello.com/c/ILDhJCw7/68-wrong-turn-5-2021-full-movie-in-hindi-free-download-2021-full-hd
https://trello.com/c/IyvW6kpd/47-catalogo-monedas-argentinas-janson-2012-21-full
https://trello.com/c/VOZw8qkx/31-security-monitor-pro-53-serial-generator-download-better
https://trello.com/c/N9oMb7MU/57-hoodie-allen-all-american-album-download-zip-link
https://www.qcepconsulting.com/front-page/ernst-and-young-entrepreneur-of-the-year-2/comment-page-199/
ermple (Wednesday, 16 February 2022 19:31)
7b17bfd26b ermple
https://coub.com/stories/3307325-download-supreme-ruler-ultimate-verified
https://coub.com/stories/3307321-dear-boy-act-3-read-online-_top_
https://coub.com/stories/3307319-top-tamil-sex-auntes-photos
https://coub.com/stories/3307313-verified-twilight-breaking-dawn-part-1-hindi-dubbed-dvd-dailymotion
https://coub.com/stories/3307314-johnny-gaddaar-hindi-video-download-fixed
https://coub.com/stories/3307308-english-is-easy-chetanand-singh-book-pdf-extra-quality
https://coub.com/stories/3307306-feitian-rockey4-emulator-11
https://coub.com/stories/3307305-portable-kumpulan-rumus-kimia-sma-lengkap-pdf-download
https://coub.com/stories/3307303-l3dt-pro-2-8-keygen-download-yardhaa
https://coub.com/stories/3307302-2021-hotline-miami-pc-trainer-secure-downloading-11
https://streetjuicetv.com/he-snuck-him-tho/
kathabad (Wednesday, 16 February 2022 20:37)
7b17bfd26b kathabad
https://coub.com/stories/3018552-catia-v5r20-64-bit-js0group-dll-download-sakyora
https://coub.com/stories/3018553-hd-online-player-seagull-cbt-answers
https://coub.com/stories/3018550-sacred-la-leggenda-dell-arma-sacrarar-alehara
https://coub.com/stories/3018548-ls-magazine-dark-studios-present
https://coub.com/stories/3018547-l-exorciste-en-folie-dvdrip
https://coub.com/stories/3018545-windows-8-1-permanent-activator-kmspico
https://coub.com/stories/3018544-nammalvar-books-in-tamil-pdf-44
https://coub.com/stories/3018541-top-adobe-after-effects-cc-12-0-0-404-ls20-multilingual-serial-key
https://coub.com/stories/3018539-new-english-vinglish-full-movie-download-worldfree4u-23
https://coub.com/stories/3018537-download-contemporary-oral-and-maxillofacial-surgery-5th-edition-pdf-wenkar
http://virtualbarter.net/blog/exchange-setup/fees
ernnira (Wednesday, 16 February 2022 21:45)
7b17bfd26b ernnira
https://wakelet.com/wake/ugLUJaiMKXL-DBnMTOhuv
https://wakelet.com/wake/_dvtKwTKpy-gAH0_GSA6i
https://wakelet.com/wake/Q7xvX9WBS2S25TvdYV0mI
https://wakelet.com/wake/vkcUedu58TGzo62bvYJ5f
https://wakelet.com/wake/CCp4noGWJVnaH4VDw_lRI
https://wakelet.com/wake/FhoHMSEmi0l-nbLOdvI4U
https://wakelet.com/wake/6Q6J2QOVrNE6uA31Fe11g
https://wakelet.com/wake/NQHtQ21ybO9YJTNeZHLKS
https://wakelet.com/wake/9f7WZQneFugAzDbwp154r
https://wakelet.com/wake/vhvExkHPhtwMXQLdU1Ila
http://nuancebb.us/things-to-do/tlr-mirror-lake-3/
yovdaw (Wednesday, 16 February 2022 22:51)
7b17bfd26b yovdaw
https://coub.com/stories/3269906-complex-edition-v1-6-8-cracked-by-termica-md-hot
https://coub.com/stories/3269905-sibelius-6-portable-top
https://coub.com/stories/3269904-raat-ke-saudagar-full-movie-download-720p-movie-work
https://coub.com/stories/3269903-usb-pc-camera-model-dc-2120-driver-free-zip-top
https://coub.com/stories/3269902-repack-woman-having-sex-in-colored-pantyhose-videos
https://coub.com/stories/3269900-paragon-alignment-tool-4-0-professional-hot-crack
https://coub.com/stories/3269901-love-in-japan-full-movie-in-english-hd-free-download-kailcha
https://coub.com/stories/3269899-work-music-theory-for-electronic-producers-on-one-page-siberius-jackson
https://coub.com/stories/3269898-hot-the-private-club-3-js-cooper-epub-download
https://coub.com/stories/3269897-verified-quantenheilung-2-punkt-methode-anleitung-pdf-download
https://appsxad.com/850/
padgwek (Wednesday, 16 February 2022 23:56)
7b17bfd26b padgwek
https://seesaawiki.jp/tioronkingven/d/Ca%20Anele%20Iubirii%20A%20Da%20Quick%2021%20Full%20Version%20Ebook%20Rar%20%5bepub%5d%20Torrent%20%28%28TOP%29%29
https://seesaawiki.jp/klisunarit/d/Download%20//TOP%5c%5c%20Terminator%202%20Judgment%20Day%20English%202%20In%20Hindi%20Dubbed%20Mp4
https://seesaawiki.jp/misundcipos/d/Spertar%20Free%20Download%20Crack%20Pc%20X32%20Latest%20falsha
https://seesaawiki.jp/sappsirilgu/d/Vodafone%20Zte%20K3772%20Z%20Firmware%20Download
https://seesaawiki.jp/cecohatpe/d/Cracked%20Resi%2032%20Registration%20Full%20Version%20Extra%20Quality
https://seesaawiki.jp/getamatas/d/Rango%20Movie%20Hindi%20Dubbed%20Free%20UPD%20Downloadgolkes
https://seesaawiki.jp/rekeconra/d/12ammadyaratrikannadafullmovie
https://seesaawiki.jp/dawdtecaba/d/Pz445%20Sd333%200j%20Download%20Software%20%2ezip%20Full%20Pc
https://seesaawiki.jp/pinscatmether/d/PPSSPP%20Gold%20%c2%80%93%20PSP%20Emulator%20V1%2e6%2e3%20Apk
https://seesaawiki.jp/theudurchpuna/d/Elevayta%20Extra%20Boy%20Pro%20502%20Cracked
https://itoutsourced.co.za/component/k2/item/23-harvard-takes-me-to-dubai
saroeart (Thursday, 17 February 2022 01:06)
7b17bfd26b saroeart
https://wakelet.com/wake/lp71v0-jsk0OebGq6dF3J
https://wakelet.com/wake/PS2pu95o0_2k9eacKDOJG
https://wakelet.com/wake/UIzv3tZPp4u6DM59Ze1Iu
https://wakelet.com/wake/wP-DyNk-JWsQ0aHWUqmg-
https://wakelet.com/wake/KDyVHYNZOJk2iL_G8J3Ug
https://wakelet.com/wake/dxjc7zM00aRqDxg1rfQ4I
https://wakelet.com/wake/YVjfWeVY-5r_Y-dJzdKzv
https://wakelet.com/wake/DbZxprlFTYWALcozq_5bH
https://wakelet.com/wake/w9tuQZQQ8OKp6E8K_F6Hf
https://wakelet.com/wake/OJL7yyH8yF02PXM557IUY
https://megasportsarena.com/70000-tickets-sold-for-joshua-fight/
giachal (Thursday, 17 February 2022 02:13)
7b17bfd26b giachal
https://trello.com/c/I37Sjgni/39-top-transformational-grammar-exercise-answer
https://trello.com/c/dgr7hjKY/44-download-naruto-classico-dublado-720p-or-1080p-monhild
https://trello.com/c/OJMxZRSS/26-work-silver-linings-playbook-dual-audio-eng-hindi
https://trello.com/c/U0Vo8pWw/33-pharmacognosy-and-phytochemistry-vinod-d-rangari-pdf-32
https://trello.com/c/sUBuuH0I/60-nuwebe-full-movie-best-free-download
https://trello.com/c/hsRz7Ena/22-shivasutraintamilpdf224
https://trello.com/c/y8p39nO5/43-zhong-wen-zhi-xin-free-repack-downloads-software
https://trello.com/c/FV1ocQfx/34-free-babylon10licensekey
https://trello.com/c/IPSjJb2l/26-smurfs-the-lost-village-english-2-tamil-dubbed-movie-torrent-download-free
https://trello.com/c/YJYJ4mRY/34-unformat-serial-number-waiulfr
http://www.thecrewhotel.co.id/index.php/dining/item/23-cockpit5%3Ftmpl=component%26amp=
jaygarm (Thursday, 17 February 2022 03:23)
7b17bfd26b jaygarm
https://trello.com/c/xaOWeOJ6/60-os-72-nomes-de-deus-tecnologia-da-alma-pdf-download-6-cedomann
https://trello.com/c/uqNzxgEc/37-transformational-reconstruction-by-shingo-sato-pdf-217-filmal
https://trello.com/c/u6b7biRQ/23-eptarreinforcementforarchicad1618-2021
https://trello.com/c/ZN2rhjgK/68-hoadley-finance-add-in-for-excel-crack-protect-vismoni
https://trello.com/c/v5L7lvoQ/45-kasumi-rebirth-331-2223-work
https://trello.com/c/QKdq0LZV/28-spider-man-homecoming-english-hindi-dubbed-mp4-download-new
https://trello.com/c/vVn1puC9/22-hindi-1080p-hd-the-martian-english-install-downloadl
https://trello.com/c/SfH3jbC3/52-just-cause-2-serial-key-daniesbi
https://trello.com/c/bhJVcnOp/37-perfume-movie-download-in-hindi-mp4-mobile-movies-vampires-acceleratio-wankang
https://trello.com/c/5OnsYhYY/27-free-download-picha-za-uchi-za-wema-sepeturar-better
https://multiplikasi.com/ketaatan-yang-mutlak/
folkvan (Thursday, 17 February 2022 04:27)
7b17bfd26b folkvan
https://coub.com/stories/3321462-psp-audioware-xenon-au-vst-rtas-1-3-0-pc-mac-elibell
https://coub.com/stories/3321465-gang-hindi-movie-free-download-utorrent-2021
https://coub.com/stories/3321463-el-buscavidas-1961-hdrip-xvid-ac3-esp-el-buscavidas-1961-hdrip-xvid-ac3-esp-l
https://coub.com/stories/3321459-piya-o-re-piya-atif-aslam-1080p-hd-129311
https://coub.com/stories/3321460-hd-online-player-hindi-medium-full-movie-1080p-downlo-savzea
https://coub.com/stories/3321457-best-aastha-in-the-prison-of-spring-1997-hindi-movie-dvdrip-xvid
https://coub.com/stories/3321456-zend-guard-7-crack-124-exclusive
https://coub.com/stories/3321455-install-xforce-keygen-fbx-2006
https://coub.com/stories/3321454-verified-miss-teacher-4-movie-free-download-in-hindi-mp4-moviegolkes
https://coub.com/stories/3321452-tamil-pdf-elizabeth-the-golden-age-free-fixed-download
https://www.essilor-instruments.com/meuleuse-delta-2/
fradav (Thursday, 17 February 2022 05:31)
7b17bfd26b fradav
https://coub.com/stories/3069597-adobe-cs6-crack-amtlib-dll-auto-patcher-keygen-top
https://coub.com/stories/3069596-verified-download-bishop-dag-heward-mills-books-53
https://coub.com/stories/3069594-tes-3600-power-analyzer-software-__exclusive__-download
https://coub.com/stories/3069595-raw-and-bangladesh-by-zainal-abedin-pdf
https://coub.com/stories/3069593-optitex-11-crack-felkris
https://coub.com/stories/3069592-sonic-foundry-sound-forge-6-0-keygen-download-faequee
https://coub.com/stories/3069591-xforce-keygen-64-bit-vred-design-2008-keygen-odolele
https://coub.com/stories/3069590-solucionario-resnick-4ta-edicion-vol-1-zip-joshcarr
https://coub.com/stories/3069589-x-force-high-quality-keygen-inventor-cam-2017
https://coub.com/stories/3069586-apple-music-mod-apk-free-download-premium-version-free-free-download-jahkim
http://www.fahrschule-hinze.de/index.php?option=com_phocaguestbook&view=phocaguestbook&id=1
kallwind (Thursday, 17 February 2022 06:38)
7b17bfd26b kallwind
https://trello.com/c/ttoT8EBC/72-the-myth-full-movie-download-in-hindi-mp4-featali
https://trello.com/c/13FObF0e/28-verified-kitchendraw-45-crackrar
https://trello.com/c/Lepid3vp/71-textbook-of-neuroanatomy-vishram-singh-pdf-free-quilrean
https://trello.com/c/g3gMO8NL/84-link-rppaudiovideosmk
https://trello.com/c/jHu0LfQV/19-monster-woman-ranmaru-graphics-18l-tamvana
https://trello.com/c/HF1R7E0f/80-youcut-video-editor-pro-133384-full-apk-for-android-top-free-download
https://trello.com/c/vOV3W6cm/25-pengantar-ilmu-hukum-soeroso-pdf-download-link
https://trello.com/c/ILvKM5ps/78-yodot-recovery-software-30-keygen-software-wynjana
https://trello.com/c/7cYADveq/37-download-kudiyon-ka-hai-zamana-movies-1080p-torrent-imanarn
https://trello.com/c/KzwpSOTf/17-yuganiki-okkadu-full-movie-hd-1080p-09-link
https://lyucifer.tv/serii-2s-podryad
laurfri (Thursday, 17 February 2022 07:46)
7b17bfd26b laurfri
https://coub.com/stories/3440221-best-underworld-blood-wars-english-1080p-dual-audio-movie
https://coub.com/stories/3440222-upd-no-time-to-relax-activation-key-crack
https://coub.com/stories/3477151-program-de-spart-parole-de-wireless-wpa-pskl-_hot_
https://coub.com/stories/3477149-oziexplorerce-2-40-keygen-updated
https://coub.com/stories/3439403-hd-online-player-crazy-beautiful-you-2015-hdrip-720p-x264-rsg-plekad
https://coub.com/stories/3439401-mappillai-rajini-video-songs-hd-1080p
https://coub.com/stories/3439399-tecno-b1p-flash-file-mt6580-frp-dead-recovery-fix-sign-customer-care-file-waildary
https://coub.com/stories/3439398-__hot__-vanesa-maria-ordonez-garmon-follando-con-su-padre
https://coub.com/stories/3439397-lexicon-pcm-native-reverb-plug-in-bundle-vst-rtas-v1-0-4-download-pc-patched
https://coub.com/stories/3439395-patched-eklg-gujarati-fonts
https://inspiralizedali.com/monthly-challenges-august/
mankal (Thursday, 17 February 2022 08:54)
7b17bfd26b mankal
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_hISkCgwLEgZDb3Vyc2UYgICAn4T6rAgMCxIIQWN0aXZpdHkYgIDA0LD08wkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCA8v6kCQwLEgZDb3Vyc2UYgIDAwOfvoAkMCxIIQWN0aXZpdHkYgIDA0ILHwQoMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_uev2CQwLEgZDb3Vyc2UYgIDAwIeDiwsMCxIIQWN0aXZpdHkYgIDAkNrIogsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCQ8rKOCwwLEgZDb3Vyc2UYgIDA0Jzq3woMCxIIQWN0aXZpdHkYgIDA4L6XoAgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDAx5uRCQwLEgZDb3Vyc2UYgIDAgLiPrwoMCxIIQWN0aXZpdHkYgIDAsKX-swoMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDAmeOBCAwLEgZDb3Vyc2UYgIDAkPO80QoMCxIIQWN0aXZpdHkYgIDAwPnl1ggMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgICfpOXXCAwLEgZDb3Vyc2UYgIDAwMDL0QoMCxIIQWN0aXZpdHkYgIDAgIuvuAsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCAuI-MCgwLEgZDb3Vyc2UYgIDAgITk4ggMCxIIQWN0aXZpdHkYgIDA0O7ZkAoMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCQydS9CgwLEgZDb3Vyc2UYgIDA4MzYiwkMCxIIQWN0aXZpdHkYgIDA0K3t5wsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCgq42ECgwLEgZDb3Vyc2UYgICA_-aNhwsMCxIIQWN0aXZpdHkYgIDA0PetxQsMogEQNTcyODg4NTg4Mjc0ODkyOA
http://thecrewhotel.co.id/index.php/dining/item/3-metus-varius-laoreet
kaepsh (Thursday, 17 February 2022)
7b17bfd26b kaepsh
https://wakelet.com/wake/CrcLVoGrgtwaJiBwgCLML
https://wakelet.com/wake/5-KJlGXHjj1j3HjsVhEWE
https://wakelet.com/wake/4CF0ucpIzV9HgnAu5a9Oe
https://wakelet.com/wake/kZY3IyCo8jONH6XVS05g6
https://wakelet.com/wake/wS89PBXjCED38TZdsgDdv
https://wakelet.com/wake/H8z2Wfx7rQQdKvEF4cgEV
https://wakelet.com/wake/zaInE-8_Yryn8qD2a46ic
https://wakelet.com/wake/glHUr1w7FDc0tTPO8k6bx
https://wakelet.com/wake/LlN6SnbI9_2HcUeL3AujC
https://wakelet.com/wake/W9NDGmQxwUlbkXJVN2uhj
https://cracked.sx/showthread.php?tid=90878
bernwal (Thursday, 17 February 2022 11:16)
7b17bfd26b bernwal
https://wakelet.com/wake/4RtzI8talPoeWo9j5DUzg
https://wakelet.com/wake/vKfkNsgGsnjAuFc2nwMVH
https://wakelet.com/wake/bQ1BXuKevV2XCHM1FOVvo
https://wakelet.com/wake/4uo6VPG2TvQY9onZ-kzo-
https://wakelet.com/wake/pG-w51wq2vUM7b4OFV37g
https://wakelet.com/wake/qZSQXqr89mr5BFBFPAah8
https://wakelet.com/wake/e2kTGtA0hWZwzECbGm94X
https://wakelet.com/wake/EX97fIlbRXaaqJ33Kq6wU
https://wakelet.com/wake/mIJ6mUA9M1UAfK1HdVHKF
https://wakelet.com/wake/ir3MRQncfVOt7CBJ51Ga_
http://yellowpagoda.com/1426879377619/
romijar (Thursday, 17 February 2022 12:20)
7b17bfd26b romijar
https://orpallandgic.chronicle.wiki/d/Serva%20Supporter%20X64%20V2%201%204Serva%20Supporter%20X64%20V2%201%204
https://quoraviphas.memo.wiki/d/Steinberg%20Halion%203%205%20Vsti%20Dxi%20X86%20Crack%2erar%20Axelle%20Phonetools%20Sa
https://unbimrete.chronicle.wiki/d/Dasavatharamfull%20%5f%5fTOP%5f%5fmovietelugu1080pvideo
https://talibfoten.game-info.wiki/d/Design%20Of%20Machine%20Elements%20Bhandari%20Ebook%20Free%20Download
https://lohohoro.chronicle.wiki/d/Memen%202k%20Video%20Avi%20Dts%20720%20Dts
https://seesaawiki.jp/buidanemer/d/32bit%20Email%20Hacker%20V3%2e4%2e6%20Torrent%20Pc%20Key%20Keygen%20salawill
https://seesaawiki.jp/eljatibgi/d/Final%20Launch%20Easydiag%203%2e0%20Better%20Launch%20Easydiag%202%2e0%20Full%20Version%20%2erar%20Activator
https://seesaawiki.jp/terninoricht/d/Rad%20Studio%20Xe2%20Update%204%20Hotfix%201%20Crack
https://hunjaconmegh.game-info.wiki/d/Hillis%20Tree%20Of%20Life%20Pdf%20Download
https://lianounsiro.playing.wiki/d/Izotope%20T%20Pain%20Effect%2erar
https://vistasbelda.com/home/11047278-3d-plan-drawing/
wakehal (Thursday, 17 February 2022 13:20)
7b17bfd26b wakehal
https://coub.com/stories/3508870-asrar-ul-awliya-in-urdu-pdf-download-osbomah
https://coub.com/stories/3508869-simhadriya-simha-movie-video-songs-download-verified
https://coub.com/stories/3508868-new-mechanics-of-materials-5th-beer-johnston-solution-manualpdf
https://coub.com/stories/3508867-athadu-mp4-movies
https://coub.com/stories/3508866-witanlore-dreamtime-crack-and-patch-fix
https://coub.com/stories/3508865-revit-architecture-2009-xforce-keygen-rar-new
https://coub.com/stories/3508864-fixed-decompiler-ex4-to-mq4-4-0-401-1
https://coub.com/stories/3508863-patched-gta-4-all-patches-crack-hack-tool
https://coub.com/stories/3508861-nepali-kt-ko-thulo-puti
https://coub.com/stories/3508860-ufc-throwdown-pc-game-free-download-corgil
https://alumni.armtischool.com/blogerenje
iolasar (Thursday, 17 February 2022 15:54)
7b17bfd26b iolasar
https://coub.com/stories/2997341-r-sarkar-inorganic-chemistry-pdf-download-zemfia
https://coub.com/stories/2997344-ek4-steelworks-2013-win64ssq
https://coub.com/stories/2997345-b-series-internet-search-and-settings-download-merifin
https://coub.com/stories/2997347-minna-no-nihongo-lesson-2650-_hot_
https://coub.com/stories/2997346-exclusive-mafia-2-dlc-ps3-pkg
https://coub.com/stories/2997348-repairv2911reparapendrivezip1-ellakeel
https://coub.com/stories/2997349-adobe-livecycle-designer-es4-trial-serial-number-ernehaz
https://coub.com/stories/2997350-exclusive-new-libro-no-se-obsesione-con-el-amor-de-susan-forward
https://coub.com/stories/2997351-verified-supreme-host-whmcs-template-nulled-xenforo
https://coub.com/stories/2997353-atmosfearfx-zombie-invasion-dvdrip-11
https://profilespedia.com/erin-colton/
evanvys (Thursday, 17 February 2022 16:56)
7b17bfd26b evanvys
https://wakelet.com/wake/ImHJL9CvzgrUAtH1Vanux
https://wakelet.com/wake/Porl__j-oj-iQd59NZyAh
https://wakelet.com/wake/DLwrDOcNqjekHoBZJazSw
https://wakelet.com/wake/x-4JqGxvRXL4VMU1mLLb2
https://wakelet.com/wake/UN3Y75-T8r_FDFzBbD17a
https://wakelet.com/wake/847B3_4cnVx3qZkPnUKLZ
https://wakelet.com/wake/FJnDJuobmz8EMQ4h752BM
https://wakelet.com/wake/yulKt_UXowutGgJKQWBoj
https://wakelet.com/wake/yuG3QROcjbxZWE2vW3eko
https://wakelet.com/wake/fRpj69q5T-2wKY5MkYoiK
http://forums.m4fg.at/showthread.php?tid=93142&pid=306993#pid306993
darsjava (Thursday, 17 February 2022 17:55)
7b17bfd26b darsjava
https://coub.com/stories/3488144-verified-schwinn-serial-number-search
https://coub.com/stories/3488143-el-resurgir-del-rey-brujo-serial-number-vanozan
https://coub.com/stories/3488145-aroundme-apk-mod-all-unlocked
https://coub.com/stories/3488142-download-verified-film-amigos-x-siempre-subtittle-indonesiagolkes
https://coub.com/stories/3488141-pdf-pdf-playboy-brazil-julho-2014-vanessa-mesquita-mara-wittz-ordexan
https://coub.com/stories/3488140-top-icecream-slideshow-maker-pro-3-41-crack-with-serial-key
https://coub.com/stories/3488139-actress-jaya-seal-hot-scene-target
https://coub.com/stories/3488138-driver-vga-for-asus-x201e-windows-7-32bit
https://coub.com/stories/3488137-download-kaspersky-antivirus-torrent-osikravi
https://coub.com/stories/3488136-kariera-nicosia-dyzmy-720p-film-sanbcher
http://samatools.com.br/index.php/component/k2/item/1
josquea (Thursday, 17 February 2022 18:57)
7b17bfd26b josquea
https://coub.com/stories/3292901-download-dreams-worth-more-than-money-sharebeast-conyos
https://coub.com/stories/3292904-luv-ka-the-end-1-movie-in-hindi-download-fraquil
https://coub.com/stories/3292905-upd-tone2-complete-bundle-v-2012-au-vst-windows-mac-os-crack-93
https://coub.com/stories/3292906-autodata-3-45-crack-full-techtool-exclusive
https://coub.com/stories/3292907-patched-normas-agma-para-engranajes-pdf-download
https://coub.com/stories/3292908-norton-protection-center-ui-stub-serial-key-ergevano
https://coub.com/stories/3292911-new-culo-by-raphael-mazzucco-pdf
https://coub.com/stories/3292913-10-link-crack-commandments-notorious-big-download-songs
https://coub.com/stories/3312233-the-legend-of-tarzan-english-tamil-movie-download-720p-hd-xenpaul
https://coub.com/stories/3283573-fairy-tail-natsu-x-erza-fanfiction-_verified_
http://kenyaearthmovers.co.ke/component/k2/item/7-how-to-give-every-kindergarten-child-the-chance/7-how-to-give-every-kindergarten-child-the-chance
quynaki (Thursday, 17 February 2022 19:59)
7b17bfd26b quynaki
https://coub.com/stories/3130212-linear-control-system-pdf-by-b-s-manke-32
https://coub.com/stories/3130213-extra-quality-snow-white-a-graphic-novel-download
https://coub.com/stories/3130211-automationthecarcompanytycoongamefullcrackserialnumber-updated
https://coub.com/stories/3130210-batman-arkham-city-cheat-happens-trainer-download-upd
https://coub.com/stories/3130209-good-girl-gone-bad-1-2-final-game-download-full-link-version
https://coub.com/stories/3130208-best-3d-max-serial-rar
https://coub.com/stories/3130206-link-crack-adobe-photoshop-cs3-extended-full-crack
https://coub.com/stories/3130205-hack-honestech-vhs-to-dvd-v4-0-25-www-portorrent-com-por-gamolama-r-__full__
https://coub.com/stories/3130197-hot-leo-gold-astrology-software-crack-torrent
https://coub.com/stories/3130204-aspekte-neu-b1-plus-pdf-new-download
http://donezkayslada.forumex.ru/viewtopic.php?f=27&t=29&p=21687#p21687
quynaki (Thursday, 17 February 2022 20:00)
7b17bfd26b quynaki
https://coub.com/stories/3130212-linear-control-system-pdf-by-b-s-manke-32
https://coub.com/stories/3130213-extra-quality-snow-white-a-graphic-novel-download
https://coub.com/stories/3130211-automationthecarcompanytycoongamefullcrackserialnumber-updated
https://coub.com/stories/3130210-batman-arkham-city-cheat-happens-trainer-download-upd
https://coub.com/stories/3130209-good-girl-gone-bad-1-2-final-game-download-full-link-version
https://coub.com/stories/3130208-best-3d-max-serial-rar
https://coub.com/stories/3130206-link-crack-adobe-photoshop-cs3-extended-full-crack
https://coub.com/stories/3130205-hack-honestech-vhs-to-dvd-v4-0-25-www-portorrent-com-por-gamolama-r-__full__
https://coub.com/stories/3130197-hot-leo-gold-astrology-software-crack-torrent
https://coub.com/stories/3130204-aspekte-neu-b1-plus-pdf-new-download
http://donezkayslada.forumex.ru/viewtopic.php?f=27&t=29&p=21687#p21687
darsber (Thursday, 17 February 2022 21:02)
7b17bfd26b darsber
https://enogtosa.memo.wiki/d/The%20Mumbai%20Police%201080p
https://sorguachisti.game-info.wiki/d/Online%20Player%20Naseeb%20Watch%20Online%20Video%20Watch%20Online%20Bluray%20Dual%20Dubbed%20saladaug
https://taimirestio.game-info.wiki/d/Latest%20Mariana%20Mihaila%20Dulce%20Mama%2064bit%20Activation%20Exe%20Utorrent%20Keygen%20godsun
https://seesaawiki.jp/pulldistoody/d/Ebook%20Kutrala%20Kuravanji%2022%20Download%20HOT%21%20Full%20Version%20%2emobi%20Zip
https://ciecheapnocon.chronicle.wiki/d/Fifa%2015%20Lag%20Fix%20Crack%20In%2011
https://orroothohut.playing.wiki/d/Fix%20Vero%20Pc%20Free%2064%20Download%20Latest%20Crack
https://seesaawiki.jp/terndenely/d/An%20Introduction%20To%20Sociology%20By%20Abdul%20Hameed%20Taga%20Ebook%20Free%2080
https://revewikin.game-info.wiki/d/Anbu%20Sagotharan%20Arjun%20Movie%20319
https://seesaawiki.jp/leivergegun/d/Iron%20Man%202008%20Hindi%20Dubbed%20Movie%20Download
https://seesaawiki.jp/lenssaboover/d/Rar%20Opel%20Vauxh%20Windows%20Keygen%20Torrent%20Ultimate%20Activation%2032bit
https://www.lollyshoplane.com/apps/blog/show/43870976-from-lolly?&fw_comments_body=&fw_comments_commenterName=Lolly&fw_comments_commenterEmail=Lolly@lollyshoplane.com&fw_comments_validator=body&fw_comments_order=ASC&siteId=133271572&locale=en-US
otaymart (Thursday, 17 February 2022 22:07)
7b17bfd26b otaymart
https://wakelet.com/wake/1XLY2rBWeH4ZqfZtbua_K
https://wakelet.com/wake/QOrVQ8nemPogHtLDzzl8y
https://wakelet.com/wake/hSbvUkV2isjArI00E445d
https://wakelet.com/wake/Uis5ZOPoiAsQYKUAvRpQ9
https://wakelet.com/wake/7srNje3j08FMVx0OQjlab
https://wakelet.com/wake/nBfCVxypQmrq0R_skUtBo
https://wakelet.com/wake/jT5Z30jIZEh6XWATowBhf
https://wakelet.com/wake/m5OP1EyAQVc2TSIaCm1At
https://wakelet.com/wake/eRGruJRy_2ISW0A1qHLBZ
https://wakelet.com/wake/8lz2ffsm0Wy-4ZFKGujwq
http://support-247.com/mybb/showthread.php?tid=1407237&pid=1807895#pid1807895
obedkass (Thursday, 17 February 2022 23:09)
7b17bfd26b obedkass
https://wakelet.com/wake/-FynPjeImK7KjpY813w25
https://wakelet.com/wake/uDRS5BtmKBF9IoW_QD-62
https://wakelet.com/wake/nK1i5PQQ0m3LWaIllk5ts
https://wakelet.com/wake/P90z53_gQCGB6dMpHUgkG
https://wakelet.com/wake/aPitvk60Pmt3zcVDo2V2g
https://wakelet.com/wake/fHQ5Hdv16La8syPvU456r
https://wakelet.com/wake/_OgIQ7Y-iM0uPU7VcRM00
https://wakelet.com/wake/GdVLDkidnRe-s7jMg7DvE
https://wakelet.com/wake/-MbhrdUspHmG38qbMd1zr
https://wakelet.com/wake/vPdpFNxm-lIjGN0UvRS_w
https://fromsis.com/showthread.php?tid=27014&pid=63455#pid63455
eronas (Friday, 18 February 2022 00:12)
7b17bfd26b eronas
https://coub.com/stories/3401014-download-link-monster-hunter-iso-for-ppsspp-cheats
https://coub.com/stories/3401010-hot-gta-san-andreas-maroc-pc-gratuit
https://coub.com/stories/3401008-gta-licence-key
https://coub.com/stories/3401006-khwaishe-bar-bar-yar-ki-karo-mp3-songs-download-top
https://coub.com/stories/3401007-michael-jackson-history-1080p-torrent-demvyky
https://coub.com/stories/3401004-infraworks201232bitfull-best-indirteklink
https://coub.com/stories/3401005-critical-strike-cs-9-01-apk-mod-unlimited-money-for-android
https://coub.com/stories/3401003-ht-employee-monitor-893-with-keyrar
https://coub.com/stories/3401002-new-blue-fx-power-director-torrent-top
https://coub.com/stories/3401000-iso-11064-pdf-free-download-exclusive
http://jiangsusufa.com/sufa/plus/guestbook.php
criqui (Friday, 18 February 2022 01:16)
7b17bfd26b criqui
https://trello.com/c/4e0BLECN/72-kiss-kiss-spin-the-bottle-hack-coins-vip-mod-apk-16-tertev
https://trello.com/c/rND9qrGf/54-android-reverse-tethering-33-zip-do-marbirg
https://trello.com/c/Ux7jyQaf/26-gta-san-andreas-baku-free-download-yukle-navedall
https://trello.com/c/r8n8ifQW/48-mary-keepers-aching-head-answer-key-zip
https://trello.com/c/aeN81mUW/58-guitar-pro-6-sound-bankrar-upd
https://trello.com/c/6nLI5emy/20-street-legal-racing-redline-221-mwm-100-save-game-hildlat
https://trello.com/c/H3JztdTi/62-steamapi-registercallresult-1-wavepeg
https://trello.com/c/R2ZsOfX8/46-windev-17-crack-rar-better
https://trello.com/c/BFzhymkl/24-ye-jemila-enat-free-download-better
https://trello.com/c/8YAI8O0D/40-coreldraw-graphics-suite-x6-16301114-sp3-portabletorrent
http://www.tjakgl.com/plus/guestbook.php
daralys (Friday, 18 February 2022 02:21)
7b17bfd26b daralys
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDg9PuFCwwLEgZDb3Vyc2UYgIDA4OWf4goMCxIIQWN0aXZpdHkYgIDAoLOO5wgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgID_5oiNCwwLEgZDb3Vyc2UYgIDAwNXSpAgMCxIIQWN0aXZpdHkYgIDA4M6DtAgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgIC_34vyCAwLEgZDb3Vyc2UYgICAv_2XjAoMCxIIQWN0aXZpdHkYgIDAkKmIgwgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDA7OTDCQwLEgZDb3Vyc2UYgIDAwM7wxwgMCxIIQWN0aXZpdHkYgIDA4M-LkQoMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgIC_3--_CwwLEgZDb3Vyc2UYgICAn8uP3AsMCxIIQWN0aXZpdHkYgIDAoMuAxQsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgIC_39qLCwwLEgZDb3Vyc2UYgIDAwJSDoggMCxIIQWN0aXZpdHkYgIDAoLOOpwsMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDAgJe-CAwLEgZDb3Vyc2UYgIDAwNXS3AgMCxIIQWN0aXZpdHkYgIDA4I7N4AkMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMCAkarNCAwLEgZDb3Vyc2UYgICA__nU3wgMCxIIQWN0aXZpdHkYgIDA0MCc6AgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgICf6_fyCwwLEgZDb3Vyc2UYgIDAwMebtgkMCxIIQWN0aXZpdHkYgIDAkPiKoQgMogEQNTcyODg4NTg4Mjc0ODkyOA
https://www.cloudschool.org/activities/ahFzfmNsb3Vkc2Nob29sLWFwcHI5CxIEVXNlchiAgMDAjq7KCwwLEgZDb3Vyc2UYgIDAoPjHiQgMCxIIQWN0aXZpdHkYgIDA4M7HlwsMogEQNTcyODg4NTg4Mjc0ODkyOA
http://www.malchuty.org/component/kide/-/index.php?option=com_kide%22>abscesses</a>
wojcflor (Friday, 18 February 2022 03:27)
7b17bfd26b wojcflor
https://trello.com/c/LLK5afbN/67-9yo-vicky-bj-with-sound-torrents-trusted
https://trello.com/c/zjQomQ4t/33-studio-d-a2-testheft-pdf-free-free-download
https://trello.com/c/62gG8B4X/41-playboy-marilyn-monroe-1953-download-kamman
https://trello.com/c/gGKmtcHo/47-3-movie-bewakoofiyaan-download-janwes
https://trello.com/c/S6nFZpKE/23-windows-server-2012-foundation-iso-download-nikblac
https://trello.com/c/MSgZUHKM/32-extra-quality-the-water-dual-audio-hindi
https://trello.com/c/fxMMlYaz/68-free-best-download-ns-virtual-dj-60-full-version-for-window-7rar
https://trello.com/c/UHepcD8l/46-i-love-you-boss-movie-tamil-dubbed-download-free-best
https://trello.com/c/8JWYPALe/25-adobe-after-effects-2020-crack-hasysar
https://trello.com/c/Ps9nKuq1/21-isee-systems-ithink-pro-902torrent-meltnad
https://diakomile.game-info.wiki/d/North%20Carolina%20Vs%20Miami%20Live%20Stream%20Online%20Link%202
marcreil (Friday, 18 February 2022 04:34)
7b17bfd26b marcreil
https://wakelet.com/wake/ODovvwO1pugU36tmgARry
https://wakelet.com/wake/82iIy7Ij_B1ykTm3ADeGE
https://wakelet.com/wake/PTs4cgsI-iIvhFipN3PfO
https://wakelet.com/wake/_PoNHpB_VlyRxtk8xnMeb
https://wakelet.com/wake/_SdxR6EQIBVliVzYCZZ9u
https://wakelet.com/wake/ntz-W6PnPEyDLdn27RDAj
https://wakelet.com/wake/S8SeAFdGUvFDS9oDiQgux
https://wakelet.com/wake/PfOxoB9DmzI_vCgkKTcRz
https://wakelet.com/wake/Yopf-ttBstRIG3jESIQvL
https://wakelet.com/wake/Af7SIs8T5qLuA0iuldSi7
https://trident-tkd.co.uk/apps/blog/show/49794959-1st-t-uk-black-belt-grading-7th-may-2011
angdar (Friday, 18 February 2022 05:38)
7b17bfd26b angdar
https://coub.com/stories/3248270-descargar-ganar-estatura-pdf
https://coub.com/stories/3250022-new-mobilego-for-android-4-3-crack
https://coub.com/stories/3250020-shringar-software-download-for-21-bertlev
https://coub.com/stories/3250021-free-turpal-cds-1-6-shirtless-boy-gymnast-model-novelart
https://coub.com/stories/3250024-garfield-2-tamil-dubbed-movie-14-orlbitt
https://coub.com/stories/3250025-the-wolf-of-wall-street-hindi-audio-track-148golkes-top
https://coub.com/stories/3250026-sleepover-download-for-mobile-hatholea
https://coub.com/stories/3250028-duncanmultiplerangetestsoftwarefreedownload-__exclusive__
https://coub.com/stories/3250029-downloadthetransporterrefueledenglishmoviesinhindi-aleamoll
https://coub.com/stories/3250027-xforce-keygen-64-bits-autocad-2012-descargar-xymoalea
https://acaipalmito.com/apps/blog/show/44179928-our-participation-at-the-natural-products-expo-east-baltimore-usa-?siteId=134598588&locale=en-GB&fw_comments_order=ASC&siteId=134598588&locale=en-GB
reilnail (Friday, 18 February 2022 06:44)
7b17bfd26b reilnail
https://wakelet.com/wake/dn3BH5IWYVsOwUKSmdowy
https://wakelet.com/wake/XsiNe2OeD1t4CSAsVk2wj
https://wakelet.com/wake/V2iDoYe5VTWm6OI5luQei
https://wakelet.com/wake/QAsfB1c4hSnAJNf7d5eYx
https://wakelet.com/wake/XofsAS9ZfBcr1-6i8pLh2
https://wakelet.com/wake/UEJKhhs8SGNKjaAgnIoN8
https://wakelet.com/wake/U5ejF4SDFts-zvFqEjI5D
https://wakelet.com/wake/6P2DU822Z3PylLl40sisb
https://wakelet.com/wake/YovYuV6BeBHi6LkMgTx3O
https://wakelet.com/wake/h8paKYQX3XPCXpH_x2iUm
https://coleccionamos.com/smartblog/6_el-stand-de-los-recuerdos-feria-del-libro-201.html
gaslor (Friday, 18 February 2022 07:56)
7b17bfd26b gaslor
https://coub.com/stories/2939826-blade-and-soul-atomix-eu-repack-top
https://coub.com/stories/2939827-bs-8007-crack-width-examples-antaheat
https://coub.com/stories/2939825-norton-mobile-security-key-crack-lindhenr
https://coub.com/stories/2939823-freedownloadharrypotter7fullmovieinenglish-bernwhat
https://coub.com/stories/2939822-hd-online-player-pokemon-arceus-and-the-jewel-of-life-better
https://coub.com/stories/2939821-fix-i-am-number-four-part-2-movie-free-27
https://coub.com/stories/2939820-link-paduka-books-for-ca-final-free-download
https://coub.com/stories/2939819-2021-the-hunger-games-mockingjay-part-2-dual-audio-bluray
https://coub.com/stories/2939818-akbar-birbal-stories-in-kannada-pdf-repack
https://coub.com/stories/2939817-updated-hack-eggcrack-2-0-minecraft-account-hacker
http://jycdnhj.com/shownews.asp?id=180
hanndire (Friday, 18 February 2022 09:06)
7b17bfd26b hanndire
https://sicoshannflan.memo.wiki/d/JetBrains%20CLion%20Crack%202020
https://seesaawiki.jp/inelgeslung/d/Ole%20Gallis%20Riddim%20Cd%201996%20Rar
https://gibrawari.chronicle.wiki/d/Nangi%20Nahati%20Ladki%20Ki%20Chudai%20Hindi%20Sex%20Story
https://seesaawiki.jp/inunalin/d/Windows%20Type3%20Type%20Edit%202003%20V5300%20Final%20Patch%2064bit%20Full%20Torrent%20Zip
https://seesaawiki.jp/tapicfetif/d/Samsara%205%20Hindi%20Dubbed%20Movie%20Download
https://seesaawiki.jp/lenfamofi/d/Black%20Sabbath%20The%20Last%20Supper%201999%20Full%20DVDRip%20H264%20AAC%20CTShoN%20CTRC%2046
https://seesaawiki.jp/gnoslombabbvi/d/Fo%20Dan%20Komik%20Kartun%2c%20Naru%20Torrent%20License%20Rar%20File%20Full%20WORK%20Version%20Windows%2032
https://tandpacducu.game-info.wiki/d/Vettaikaran%20Video%20Songs%20Hd%201080p%20Blu%2dray%20Tamil%20Movie
https://seesaawiki.jp/giturnere/d/Ashirwad%20Mantra%20Sanskrit%20Pdf%2036
https://trello.com/c/WggCGRVH/35-wicam-pn-4000-exclusive
https://siemefo.com/etinsyba
simomel (Friday, 18 February 2022 10:28)
7b17bfd26b simomel
https://wakelet.com/wake/bj3n4mW7Yp9w8bJ6sr-qB
https://wakelet.com/wake/on_qL8aKOGN0EdiVN69hE
https://wakelet.com/wake/OO6xACF-x08gSvbZY_Fu_
https://wakelet.com/wake/q4m8iexNLb4y-7JXJRcG1
https://wakelet.com/wake/J3vO1F5XfTCOS9MZH9qeA
https://wakelet.com/wake/3iDvtBF4UGertLrAWQQfG
https://wakelet.com/wake/LsyZZAcPhj7lpvNljGBex
https://wakelet.com/wake/dBXyHiWzhr6vzD7saVE5a
https://wakelet.com/wake/1IVAjPPNXwl8JpbOfQx6V
https://wakelet.com/wake/TK0olNRMO06thqpRcdn7H
https://www.bow-bow.com/phone/bbs
kaelwak (Friday, 18 February 2022 11:50)
7b17bfd26b kaelwak
https://wakelet.com/wake/0nx3OHgvAkWI_JZQ4usNf
https://wakelet.com/wake/sNyfBhQOM_-cUtysgP0UZ
https://wakelet.com/wake/dGv183y-Ede5Dt3A6MXZX
https://wakelet.com/wake/ZCg17W5dIodWSg-vQU-Cj
https://wakelet.com/wake/waX5fZ6zmedrsZ-FMnOPC
https://wakelet.com/wake/kOgG1m7X_sM1g26yCRRzu
https://wakelet.com/wake/VUgnMB33zTcNXxCCdbUSv
https://wakelet.com/wake/OR9h8C2p2Kn6tE4wFHwM0
https://wakelet.com/wake/GZi5q1_pV5yP-T6xpUdx2
https://wakelet.com/wake/NdaNA0PgU25UPOHv7rBGX
http://evyer.ir/hp_41c_manual_pdf_/
imbailea (Friday, 18 February 2022 13:41)
7b17bfd26b imbailea
https://coub.com/stories/3444568-velamma-comics-pdf-free-download-in-15-better
https://coub.com/stories/3444566-full-igo-for-windows-ce-60
https://coub.com/stories/3444567-sri-suktam-in-tamil-pdf-40
https://coub.com/stories/3444565-bodyguard-1080p-movie-download-kickass-dorkala
https://coub.com/stories/3444564-savant-racepoint-blueprint-work
https://coub.com/stories/3444562-oasys-frew-v19-1-1-15-incl-crack-tordigger-verified-full-version
https://coub.com/stories/3444561-download-asphalt-8-apk-data-highly-compressed-victrosa
https://coub.com/stories/3444560-epic-character-generator-torrent-upd-download-pc
https://coub.com/stories/3444559-bentley-flowmaster-v8i-08-11-01-03-14-top
https://coub.com/stories/3444558-venice-deluxe-free-download-crack-serial-key-keygen-venecha
https://priroda-centr.jimdofree.com/%D0%B3%D0%BB%D0%B0%D0%B2%D0%BD%D0%B0%D1%8F-%D0%BDome/%D0%B2%D0%BE%D0%BF%D1%80%D0%BE%D1%81%D1%8B-%D0%B8-%D0%BE%D1%82%D0%B2%D0%B5%D1%82%D1%8B/
checal (Friday, 18 February 2022 15:05)
7b17bfd26b checal
https://coub.com/stories/3442550-hot-gallery-foto-chika-bugil
https://coub.com/stories/3442546-advanta-witty-turbo-crack-link
https://coub.com/stories/3442545-smadav-2020-revision-13-4-crack-better
https://coub.com/stories/3442543-download-xforce-keygen-autocad-2014-64-bit-patch-new
https://coub.com/stories/3442542-fixed-magic-dvd-ripper-720-registration-code
https://coub.com/stories/3442541-upd-dhan-dhana-dhan-goal-2-movie-download-in-hindi
https://coub.com/stories/3442540-rtsp-mpeg4-sp-control-plugin-firefox-orlxia
https://coub.com/stories/3442539-swansoft-cnc-simulator-keygen-crack-lylieif
https://coub.com/stories/3442538-ek-jaan-hain-hum-full-movie-1010-repack
https://coub.com/stories/3442535-fix-gunday-movie-video-song-mp4-free-download
http://forum.summitroleplay.com/showthread.php?tid=70947&pid=307220#pid307220
jesfall (Friday, 18 February 2022 16:23)
7b17bfd26b jesfall
https://wakelet.com/wake/2XeCgSNQXxH5lWoZ1DUFG
https://wakelet.com/wake/z9B3t_rleanuTJYaz_5k_
https://wakelet.com/wake/pajXVLix4lkyPBQNlbe2B
https://wakelet.com/wake/cx2nSTl8NJepxgLvK8TS8
https://wakelet.com/wake/R9Q8dmgdIeRCOCw5JeWKN
https://wakelet.com/wake/uD8DfxtCrT5jDlvL55ry_
https://wakelet.com/wake/gF1IHcNY4FBCz9ReOzQ5j
https://wakelet.com/wake/5REE4l5dW7zW0_WL2ksH2
https://wakelet.com/wake/nSxtgoqRGRDsqaQgEvEHQ
https://wakelet.com/wake/csOOiZPuCFo_YkciQdOXU
https://seesaawiki.jp/magnolingcen/d/Hindi%20Songs%20Raja%20Pdf%20Free%20Download
turwyl (Friday, 18 February 2022 17:41)
7b17bfd26b turwyl
https://trello.com/c/tG9XPU39/87-best-offline-game-of-dragon-city-for-pc
https://trello.com/c/6o0oiSfj/22-microsoft-toolkit-263-final-windows-and-office-activator-utorrent
https://trello.com/c/cyDSNM12/57-crack-best-do-gothic-3-175-18
https://trello.com/c/ncm5Mghd/19-ajp13-download-verified
https://trello.com/c/u5MG4v8b/17-red-giant-all-suites-x64-incl-license-keys-fix
https://trello.com/c/bXeUulNo/35-weliamuna-report-on-srilankan-airlines-pdf-download-premanf
https://trello.com/c/jygAyjMp/50-jihosoft-file-recovery-keygen-best-crack
https://trello.com/c/o2fAa3Io/49-farmacognosia-de-claudia-kuklinski-pdf-59-hot
https://trello.com/c/97GQpeg6/32-gomezpalaciomargaritalalecturaenlaescuelapdf11-valegeo
https://trello.com/c/gP5Ca5IW/53-ice-lakes-v194-game-hack-top
https://treklr.com/read-blog/13385
naiswald (Friday, 18 February 2022 19:05)
7b17bfd26b naiswald
https://coub.com/stories/2942193-repack-adobe-acrobat-7-0-professional-rar-setup-free
https://coub.com/stories/2942194-legion-de-angeles-1080p-mega-top
https://coub.com/stories/2942192-dell-inspiron-1440-1545-1750-recovery-dvd-download-pc-fiorgaet
https://coub.com/stories/2942191-vmware-workstation-8-0-4-crack-extra-quality
https://coub.com/stories/2942190-rd-sharma-class-12-ebook-free-download-pdfl-takisha
https://coub.com/stories/2942189-descarga-instala-y-activa-autocad-2020-64-bits-espanol-e-ingles-licencias-de-por-vida-updated
https://coub.com/stories/2942188-graphisoft-archicad-22-build-3006-win64-full-2021-version
https://coub.com/stories/2942187-peach-model-custom-set-rar
https://coub.com/stories/2942185-sunt-un-mic-ticalos-1-dublat-in-romana-11-better
https://coub.com/stories/2942186-facebook-hacker-v-6-2-download-verified
http://www.grgsecurity.com/plus/guestbook.php
lisejarl (Friday, 18 February 2022 20:24)
7b17bfd26b lisejarl
https://seesaawiki.jp/elanpacra/d/Adobemediaencodercccrackamtlibdllfile
https://seesaawiki.jp/zerdhasacfa/d/Ek%20Phool%20Teen%20Kante%20Movies%20Kickass%20720p%20Dts%20Mkv%20High%20Quality
https://seesaawiki.jp/leiprevnesssar/d/Sulabh%20Jyotish%20Shastra%20Pdf%20Free
https://seesaawiki.jp/tedlecubou/d/%28%28TOP%29%29%20Altium%2064bit%20Full%20Build%20Serial%20Key%20Torrent%20Pc
https://seesaawiki.jp/inbenpobal/d/Download%20Driver%20Printer%20Matrix%20Point%20Mp%207645%20Hp
https://seesaawiki.jp/cordearedi/d/Higiene%20E%20Inspeccion%20De%20Carnes%20T%2e%20Ii
https://seesaawiki.jp/baulisliega/d/Smart%20Card%204k%20Video%20Dubbed%202k%20Watch%20Online%20canite
https://seesaawiki.jp/emenavin/d/%28%28FREE%29%29%20Full%20Version%20Indianeco%20Torrent%2032%20Exe%20File%20Pc
https://seesaawiki.jp/kaitrigatran/d/Mr%2e%20Majnu%20Full%20Movie%20In%20English%20Hd%20Free%20Download
https://seesaawiki.jp/zathorefi/d/The%20Ghazi%20Attack%20Movie%20Download%20720p%20Kickassl
https://kehrhealthrabi.memo.wiki/d/FB%20Friends%203%2c%201115917%5f1404161846468679%5f2740039%20%40iMGSRC%2eRU
gloregi (Friday, 18 February 2022 21:46)
7b17bfd26b gloregi
https://trello.com/c/eJRF6nBP/29-descargar-winunisoft-44-full-es-ultwhit
https://trello.com/c/02K28Ejm/34-top-the-adventures-of-tintin-1080p-english-subtitles
https://trello.com/c/UcqOxtcX/40-portable-frumoasa-si-bestia-film-limba-ro
https://trello.com/c/vNSpjnre/37-fix-second-hand-husband-hindi-dubbed-720p-movies
https://trello.com/c/GWFjj4kL/45-high-quality-sworkit-premium-personalized-workouts-v820-apk
https://trello.com/c/KYVl2bLk/46-descargar-libro-primero-lo-primero-stephen-covey-pdf-download-verified
https://trello.com/c/6ZXiq6Fu/55-bas-gitar-metodupdfgolkes-fixed
https://trello.com/c/0WbitWJ1/33-upd-easyvcw-v1-51
https://trello.com/c/Gt3BuBbF/40-time-pass-2-full-movie-in-hindi-hd-1080p-fadimoj
https://trello.com/c/pAHFooBX/22-speed-in-hindi-pdf-download-free-top
http://62.33.234.15/viewtopic.php?f=23&t=164323&p=1887584#p1887584
wiljan (Friday, 18 February 2022 22:55)
7b17bfd26b wiljan
https://wakelet.com/wake/0h8_4S7dDR_f0vkYnR7FN
https://wakelet.com/wake/IAGK-Hkj6y34GltNAJ_xc
https://wakelet.com/wake/0zIAgHHx3omxljsG-XGeT
https://wakelet.com/wake/VYhkgTQRZKl2U3b1XMBUQ
https://wakelet.com/wake/nV4IjFTUhQZsGF0T9rlpU
https://wakelet.com/wake/rmubjJ856BPpEybaHsS-U
https://wakelet.com/wake/PBSw6MSuUTf0RhpuAqGyW
https://wakelet.com/wake/EmxDqut-tzf_DnxXuiLXR
https://wakelet.com/wake/gd4HuoRXnI8EQw4Ms4j5W
https://wakelet.com/wake/cytd5tUL4mfBrb_bTKvbW
https://leadersofevolution.com/types-of-coaching/
aurelevi (Saturday, 19 February 2022 00:02)
7b17bfd26b aurelevi
https://coub.com/stories/3329523-q-skills-for-success-listening-and-speaking-3-free-extra-quality-download
https://coub.com/stories/3326967-ee-hrudayam-video-song-hd-tamil-1080p-valfai
https://coub.com/stories/3326965-best-pathfinder-player-character-folio-pdf-download
https://coub.com/stories/3326964-inkaar-in-hindi-movie-download-verified
https://coub.com/stories/3326963-optimum-k-software-crack-16-free
https://coub.com/stories/3326962-strength-of-materials-3rd-edition-by-pytel-and-singer-solution-manual-zip-link
https://coub.com/stories/3326961-daemon-tools-lite-449-serial-number
https://coub.com/stories/3326960-bonetown-104-patch-__hot__
https://coub.com/stories/3326956-parazitii-daca-as-fi-presedinte-_hot_-download-zippy
https://coub.com/stories/3326955-driverjoystickxtechxg881s-neyjan
https://thefuturegoal.com/giuwadcero
willchap (Saturday, 19 February 2022 01:17)
7b17bfd26b willchap
https://coub.com/stories/3053167-upd-quikquak-crowd-chamber-v4-0-1-incl-keygen-win-osx-r2r
https://coub.com/stories/3053162-patch-fr-pour-afterfall-insanity-5
https://coub.com/stories/3053161-samprefs-iphone-unlocker-pc-version-free-27-perble
https://coub.com/stories/3053159-mediachance-editstudio-6-0-5-keygen-download-updated
https://coub.com/stories/3053160-flipside-studio-free-download-crack-with-full-top-game
https://coub.com/stories/3053155-usb-redirector-technician-edition-crack-upd
https://coub.com/stories/3053156-parashara-light-703-free-download-kamvan
https://coub.com/stories/3053153-mad-max-fury-road-dual-audio-eng-hindi-720p-download-in-kickass-torrent-repack
https://coub.com/stories/3053151-achyutananda-malika-oriya-pdf-download-upd
https://coub.com/stories/3053150-umt-dongle-5-4-crack-full-keygen-exclusive-setup-loader-free-download
http://www.shmq-water.com/shownews.asp?id=113
rafrans (Saturday, 19 February 2022 02:28)
7b17bfd26b rafrans
https://trello.com/c/0xjnMAgf/46-tensor-calculus-sheikhpdfl-portable
https://trello.com/c/1Ujh0YlG/57-fsx-p3d-alabeo-pa36-pawnee-brave-375-no-survey-no-password-no-download-updated
https://trello.com/c/ISD7ZMn6/58-need-for-speed-v6115-mod-apk-pc-no-limits-obb-setup-free-mycgere
https://trello.com/c/5xaMkcH9/27-adobe-acrobat-xi-pro-10022-final-patched-crack-serial-key-keygen
https://trello.com/c/Wjoh1ieV/11-free-player-manager-2000-pc-crack-game
https://trello.com/c/27qsqRVh/23-high-quality-download-ebook-farmakope-indonesia-edisi-3
https://trello.com/c/wdJiKSTr/65-e5-00-rm-632-v101-003-arrar-tulpea
https://trello.com/c/6EWOyGzl/77-link-chatrak-full-movie-download
https://trello.com/c/5QeRGn7n/52-stranger-things-season-2-s02-complete-torrent-yify-torrent
https://trello.com/c/dFVrvjWz/62-gameguardian-game-hack-alteration-tool-v780-latest-hot
https://cdldotphysical.com/apps/blog/show/48367765-commercial-drivers-and-high-blood-pressure&fw_comments_order=ASC&siteId=140700574&locale=en-US
ferhale (Saturday, 19 February 2022 03:53)
7b17bfd26b ferhale
https://wakelet.com/wake/ZO6qXkHbjXl0dsHPEPZiM
https://wakelet.com/wake/N-IKCjAB54TOjQlYMtrVn
https://wakelet.com/wake/DRWRkd_p8Gnj1kTqxR9Zw
https://wakelet.com/wake/WpZZVP0zT9sy93_4_d-bp
https://wakelet.com/wake/NRNlaIsFMK4GNgrai6zxY
https://wakelet.com/wake/KsnlenD8ZrzSisFKQlYEq
https://wakelet.com/wake/C1_553YBgYsm-4VZX5qm5
https://wakelet.com/wake/2unEUHn4aclglCm7ijc1R
https://wakelet.com/wake/GikgZ1bOsANKUJebcwCUY
https://wakelet.com/wake/YksBeUOpxtjIeEqS0WwtZ
https://seesaawiki.jp/pherpipercya/d/auto%20brew%20psp%20download
guiundu (Saturday, 19 February 2022 05:15)
7b17bfd26b guiundu
https://wakelet.com/wake/EVlv3UHpZ-YNm8x9qXzXE
https://wakelet.com/wake/tFXj8nIXUyj3HbKbmF-sx
https://wakelet.com/wake/m1YP85Iw6_iTpS0ueHdEb
https://wakelet.com/wake/ykA7XTVN9m-LWET7BaIpd
https://wakelet.com/wake/O05zuAF1g3aGzWbs87sZs
https://wakelet.com/wake/Ns0kepcfCfOPAJGT_w-qJ
https://wakelet.com/wake/8GPguxtUC9k4GcWPvWqyu
https://wakelet.com/wake/HSohIsbdLR9K8JBkld-rx
https://wakelet.com/wake/WVX7XIYKCrE7abffKs_Db
https://wakelet.com/wake/1kwb2o_7lTXyXGiOyuxah
http://reedso.com/blog/4_nec-intellegat-deseruisse-te.html
enskpier (Saturday, 19 February 2022 06:37)
7b17bfd26b enskpier
https://coub.com/stories/3487231-dua-e-tawassul-urdu-pdf-download-machine-minorenne-personalizzare-plus21-qudjaim
https://coub.com/stories/3487230-top-download-buku-ekonomi-kelas-x-pdf
https://coub.com/stories/3487229-hot-bio-rad-cfx-manager-software-download-free
https://coub.com/stories/3487228-portable-linear-system-thomas-kailath-solution-manualrar
https://coub.com/stories/3487227-xforce-verifiedkeygenvaultworkgroup2019mempatch
https://coub.com/stories/3487226-false-color-plug-in-3-for-after-effects-davinci-and-ofx-win-igrdeit
https://coub.com/stories/3487225-milkman-showerboys-vol-2-videogolkes
https://coub.com/stories/3487224-hot-data-cash-crack-sysinfotools-openoffice-calc-recovery-10
https://coub.com/stories/3487223-do-lucky-watch-online-720p
https://coub.com/stories/3487222-limba-romana-manual-pentru-studentii-straini-pdf-zlatlori
http://socialmediascript.aistechnolabs.xyz/read-blog/6133
warcat (Saturday, 19 February 2022 08:03)
7b17bfd26b warcat
https://coub.com/stories/3501439-portable-call-recorder-boldbeast-v11-9-pro-latest
https://coub.com/stories/3501438-be2works-crack-408-top
https://coub.com/stories/3501437-isafe-keylogger-pro-7-0-0-best-cracked
https://coub.com/stories/3501436-camera360-selfie-photo-editor-with-funny-sticker-v9-7-5-mod-latest-work
https://coub.com/stories/3501435-little-busters-little-busters-refrain-original-soundtrack-download-cheat-humkay
https://coub.com/stories/3501434-imspost-7-4-crack-repack
https://coub.com/stories/3501433-aplikasi-struk-spbu-full-versionl-jamabill
https://coub.com/stories/3501430-systools-dbx-converter-4-0-crack-forghis
https://coub.com/stories/3501432-link-hauptwerk-4-cracktorrent75
https://coub.com/stories/3501431-verified-download-prosim-plus-software-free
http://amphenol-apc.com/k2-categories/item/213-creative-s?zabgal.xyz/iveta-soft/0.html?contact_ajax=4575941636348621&ctajax_modid=318
aylfle (Saturday, 19 February 2022 09:23)
7b17bfd26b aylfle
https://coub.com/stories/3228205-serial-heidelberg-sherlock-plus
https://coub.com/stories/3228201-ahista-ahista-dubbed-in-hindi-hd-torrent-birkris
https://coub.com/stories/3228200-home-stay-stay-alive-full-movie-download-in-dual-audio-english-hindi-link
https://coub.com/stories/3228199-patched-kodak-prinergy-connect-5-22-serial-key-keygen
https://coub.com/stories/3228198-decrypttheufd2hashpasswordonlinerar-exclusive
https://coub.com/stories/3228182-extra-quality-douazeci-si-patru-de-ore-din-viata-unei-femei-pdf-download
https://coub.com/stories/3228195-install-gaddafisharembookfreedownloadpdf
https://coub.com/stories/3228190-download-xparanormal-detector-pro-1-7-top-full-serial-of-neeli
https://coub.com/stories/3228189-1666redemptionthroughsinpdf12
https://coub.com/stories/3228187-autodata-338-romana-17-lanphil
https://www.hiroyukiyamanoi.co.jp/bbs
edynkaf (Saturday, 19 February 2022 10:40)
7b17bfd26b edynkaf
https://wakelet.com/wake/A2X9IgoAe2U1zQIZOF3XO
https://wakelet.com/wake/1MQKY3RD6zh9upnVcJkns
https://wakelet.com/wake/ZXzPQNdM0tGSZCwikm7li
https://wakelet.com/wake/Sa8qT7xr2HPW_FyKs60fV
https://wakelet.com/wake/99TbFzt1p3DGWATmZBvic
https://wakelet.com/wake/Ev6DL_NII2GORhZM2WVDu
https://wakelet.com/wake/nTVMeDkMuvcDm93zmtdrs
https://wakelet.com/wake/XHPDD42VXenmZUsVoyZvB
https://wakelet.com/wake/WzWFwqHg-M3xAUj9Z2Z0_
https://wakelet.com/wake/TV9zPkR_Sa4xY1eLjMDa1
http://forum.sakarea2.go.th/viewtopic.php?f=9&t=6&p=161703#p161703
wynphi (Saturday, 19 February 2022 11:57)
7b17bfd26b wynphi
https://trello.com/c/iqtsWknp/35-hot-cash-register-express-101-crack
https://trello.com/c/LwJdhEBJ/27-anydvd-hd-v7180-final-multilenguaje-serial-key-install
https://trello.com/c/wPYDulNl/30-crack-winquick-kfz-agnvan
https://trello.com/c/nVLcWM6h/30-upd-crackbitche35build50
https://trello.com/c/BRDiY1p5/24-one-tree-hill-season-1-complete-free-download-kamllau
https://trello.com/c/t3mSR3Ud/24-ramaurshyamhdfullmoviedownload1080phd-new
https://trello.com/c/DePixe0P/24-introduccionalastelecomunicacionesmodernasenriqueherreraperez
https://trello.com/c/L4tazX8g/46-new-hindi-movie-mere-yaar-ki-shaadi-hai-full-movie-download
https://trello.com/c/eglvffkJ/39-patched-tuneskit-spotify-converter-170657-crack-pre-activated-2020
https://trello.com/c/l7dfSSy7/34-computeraidedthermodynamictables3catt3-ilegal
https://lorie-love.jimdofree.com/2014/03/15/bon-anniversaire-les-enfoir%C3%A9s-sehr-gute-einschaltquoten/
evaamal (Saturday, 19 February 2022 13:13)
7b17bfd26b evaamal
https://coub.com/stories/2936848-va-those-classic-golden-years-40-cd-box-2008
https://coub.com/stories/2936847-hot-como-recuperar-mi-boleta-credencial-de-la-unam
https://coub.com/stories/2936846-__exclusive__-planet-coaster-classic-rides-collection-download-winrar
https://coub.com/stories/2936845-classic-project-15-dvd-full-free
https://coub.com/stories/2936844-_best_-wonderware-intouch-scada-software-free-download-crack-fifa
https://coub.com/stories/2936843-hackhotmailpasswordhacktoolv51-lavegil
https://coub.com/stories/2936841-chhota-bheem-and-the-throne-of-bali-telugu-movie-1080p-download-torrent-upd
https://coub.com/stories/2936842-weapon-res-file-for-igi-2-covert-59-whytamat
https://coub.com/stories/2936840-gorenje-wa-583-uputstvo-za-13https-scoutmails-com-index301-php-k-gorenje-wa-583-uputstvo-za-13
https://coub.com/stories/2936839-teracopy-free-download-fix
https://goddessprom.com/apps/blog/show/prev?from_id=49712252&siteId=142130404&locale=en-US
denjem (Saturday, 19 February 2022 14:28)
7b17bfd26b denjem
https://seesaawiki.jp/bilningliper/d/Uth%20Maha%20Ganapati%20Mp3%20Download
https://seesaawiki.jp/hocheapeso/d/2%20Spark%20Blu%2dray%20Mkv%20Avi%20Torrent%20Download
https://seesaawiki.jp/chessrazutist/d/TeamViewer%2014%2e7%2e1965%2e0%20Crack%20License%20Key%20Torrent%20%7bPortable%7d
https://seesaawiki.jp/quidreadolti/d/Lista%20Completa%20Key%20Iso%20Professional%20Free%20Torrent%20%21%21INSTALL%21%21
https://seesaawiki.jp/avjerrimu/d/Pc%20Securecrt%206%207%20X%20Full%20Version%20Key%20%2ezip%20Latest
https://seesaawiki.jp/provlentwescy/d/F1%202013%20Update%207%20Reloaded%20Crack
https://seesaawiki.jp/apterpaulym/d/Solid%20Edge%20V20%20Portable
https://seesaawiki.jp/debucerny/d/Crack%2eBuzzEdit%2e3%2e3%2e4%2e60
https://seesaawiki.jp/amasvasa/d/3d%20Sex%20Villa%20Highly%20Compressed
https://seesaawiki.jp/rusfoegixa/d/Shaolin%20Soccer%20Movie%20Download%20In%20Tamil
https://vanquitelli.chronicle.wiki/d/roblox%2daction%2dfigures%2dcodes
leticar (Saturday, 19 February 2022 15:43)
7b17bfd26b leticar
https://seesaawiki.jp/tutentiobau/d/Rab%20Ne%20Bana%20Di%20Jodi%202%20Hd%20720p%20%28%28TOP%29%29%20Free%20Dubbed%20Download%20Mkv%20Dubbed
https://brentarapas.memo.wiki/d/Branko%20Milenkovic%20Ispovesti%20Iz%20Harema%20Pdf%20Free
https://sundcratrodmi.memo.wiki/d/Kambi%20Car%20Registration%20Windows%20Patch%20Pro%2032bit%20Rar%20bertgil
https://acbaclifac.memo.wiki/d/Merlin%20X2%20Ikosoft%20Full%20Version%20Activation%20Pc%20Zip%2032bit%20Cracked%20moryrai
https://neleslighti.game-info.wiki/d/Crysis%20Crack%20For%20Windows%207%2032bit
https://direbetof.memo.wiki/d/Crack%20Au%20Enterpresserv40rar%20License%20Torrent%20Windows%2064bit%20Professional%20%5bWORK%5d
https://seesaawiki.jp/birepnati/d/Windows%20Chris%20Brown%20Royalty%20License%20%5bHOT%5d%20Download%20File%2032%20Free
https://seesaawiki.jp/smelgadcaubatl/d/Gsa%20Email%20Spider%20706%20Crack
https://seesaawiki.jp/astogmontplum/d/Automailmerge%20Plugin%20For%20Adobe%20Acrobat%20Crack%2031
https://seesaawiki.jp/tepiranra/d/%21%21BETTER%21%21%2064bit%20Au%20Motive%20Expert%207%2e93%20Registration%20Windows%20%2erar
http://www.tennisteam-ortenau.de/2020/02/02/roulette-techniques-for-arranging-beginners/
vanyed (Saturday, 19 February 2022 17:00)
7b17bfd26b vanyed
https://trello.com/c/kabf3xul/34-metal-gear-solid-integral-pc-crack-top-sites
https://trello.com/c/HFQ6HQMf/47-verified-pari-full-hd-free-download
https://trello.com/c/gzb3J2To/90-best-thenalitamilmovie720pdownload
https://trello.com/c/LAyPtPHr/18-mapc2mapcregistrationkey
https://trello.com/c/a9GjDNqS/33-pandji-pragiwaksono-bhinneka-tunggal-tawa-full-patched-version
https://trello.com/c/PtfahJgz/31-filme-minha-gostosa-empregada-etelvina
https://trello.com/c/ROJgzfvR/89-avid-sibelius-crack-with-serial-keys-latest-2020-oleafra
https://trello.com/c/XdV7WjVA/45-better-dear-v-s-bear-2015-movie-songs-free-download
https://trello.com/c/6kCTBwXz/11-geet-hui-sabse-parayi-all-episodes-free-downloadgolkes-halimb
https://trello.com/c/O1bLmHrV/31-better-mizuna-rei-hbad-179-11
https://www.pickmemo.com/read-blog/2145
phylhay (Saturday, 19 February 2022 18:15)
7b17bfd26b phylhay
https://wakelet.com/wake/VcB1TKQHmZ-V6zKNFITGN
https://wakelet.com/wake/JzfZOIgiaxNpa5S0-0WCu
https://wakelet.com/wake/kHo-C4enYNDvltG6Ig7VM
https://wakelet.com/wake/gPB03pz6OxotsKGbwuU0J
https://wakelet.com/wake/QON4zKL8b_3_39l8DW_u-
https://wakelet.com/wake/DBpP5NUcXWodDcF9eiwxY
https://wakelet.com/wake/ts8LovGVt_NEjvgvuLN8T
https://wakelet.com/wake/QLLPqmBPcum3hnQdMTFnH
https://wakelet.com/wake/jxadEmooqfUZvg8-Z_R2C
https://wakelet.com/wake/ia8kJccrf_kelYkVdSaUj
http://juppheidi-geocaching.de/g%C3%A4stebuch/
keilter (Saturday, 19 February 2022 19:30)
7b17bfd26b keilter
https://wakelet.com/wake/osVDPA6nLs-GiquzG5exQ
https://wakelet.com/wake/gx8H06Oql2TIoIQ6-j3XQ
https://wakelet.com/wake/VzXuMsDbkpPbyCoJSIOgw
https://wakelet.com/wake/ItbuEKpRhtu3V7UAZqAD4
https://wakelet.com/wake/nKqquKEyMonznXgedSMPn
https://wakelet.com/wake/uwzBfLiXzzfRYGR6gSS6X
https://wakelet.com/wake/gGa8-0puIr6nI2W7PqCHx
https://wakelet.com/wake/wPhroGVRR_GOn-QkA9pTy
https://wakelet.com/wake/lP9tA_XqkNfS98qW6KKRg
https://wakelet.com/wake/wc28kaE5a1Ksrx73CzRld
https://social.mactan.com.br/read-blog/4230_videopad-video-editor-8-04-crack-registration-code-2020.html
daggsil (Saturday, 19 February 2022 20:43)
7b17bfd26b daggsil
https://coub.com/stories/3491675-xforce-keygen-64-bit-fabrication-camduct-2016-download-link
https://coub.com/stories/3491674-serat-babad-tanah-jawi-pdf-76-innredn
https://coub.com/stories/3491673-resident-evil-the-final-chapter-english-tamil-movie-torrent-free-downloadgolkes-dorepasc
https://coub.com/stories/3491672-driver-samsung-e1205t-tamzber
https://coub.com/stories/3491670-rocky-handsome-1-full-movie-subtitle-indonesia-download-ermafabr
https://coub.com/stories/3491671-nanaumi-nana-dv-1151-dvdrip-torrent-best
https://coub.com/stories/3491669-download-six-x-full-hindi-dubbed-3gp-movie-better
https://coub.com/stories/3491668-pdfcreator-4-0-3-crack-activation-key-2020-_best_
https://coub.com/stories/3491667-supreme-ruler-2020-6-6-1-trainer-updated
https://coub.com/stories/3491666-ls-magazine-dark-studios-presents-dark-robbery-rar-tymivasy
http://forum.gamerepin.com/showthread.php?tid=125577&pid=203245#pid203245
georkaiy (Saturday, 19 February 2022 21:57)
7b17bfd26b georkaiy
https://coub.com/stories/3231915-download-driver-signalking-sk-10tn-work
https://coub.com/stories/3231916-perfume-the-story-of-a-murderer-in-hindi-torrent-download-39-reetzsy
https://coub.com/stories/3231918-bug-mafia-ft-cheloo-limbaj-de-cartier-zippy-better
https://coub.com/stories/3231920-the-beach-full-movie-in-hindi-free-download-upd-hd
https://coub.com/stories/3231914-verified-dr-israr-ahmed-mp3-lectures-in-urdu-free-download-virus-satis-maschera-riparazione
https://coub.com/stories/3231921-install-mushroom-cultivation-in-nepal-pdf-20
https://coub.com/stories/3231922-kaal-hai-movie-download-mp4-high-quality
https://coub.com/stories/3231925-free-download-rhinoceros-4-0-full-version-with-high-quality-crack
https://coub.com/stories/3231926-mr-prepper-torrent-free-download-patch
https://coub.com/stories/3239415-free-bentley-sewercad-v8i-ss5-free-download
https://faithbread.com/read-blog/4461
pascarv (Sunday, 20 February 2022 13:47)
https://www.youtube.com/watch?v=F6Q2m6DtApU. bcbef96d84 pascarv
https://wakelet.com/wake/047mks4oOQiHCNdidPiGZ
https://wakelet.com/wake/6VXCB1cC4mXRH-xU9BKN4
https://wakelet.com/wake/kAEDD4SMHxI9333hG2-Fr
https://wakelet.com/wake/Nzm-k2s_E2QJaGOtH5WFa
https://wakelet.com/wake/97PyJbq3RsdMC1aeD8roY
https://wakelet.com/wake/QofDr7lSw7nyyR1Z_YgV4
https://wakelet.com/wake/SVYgfMcebko6AtBnFCmL6
https://wakelet.com/wake/MvIUTikAxzcR4goWI8BsT
https://wakelet.com/wake/Na-gX4d_3JNjL0oGKfqCm
https://wakelet.com/wake/oCEAT9WDX9_m5ojW1biql
GraphiSoft ArchiCAD 19 Crack Full is exceptionally compelling and propelled illustrations apparatus which you gave the 3D building outlining. In which this.... 6 results SAS JMP Pro Statistical . rar >> DOWNLOAD Oct 19, 2019 Toyota TIS Techstream 15. per file, your Nov 12, 2020 Look for ... ArchiCAD 14 x64+crack.. how to install and crack archicad 19 ... bonjour cette vido met en exergue l'installation complet de archicad ...
https://bonbon-journey.biz/2020/03/20/eventzoro/
samphib (Sunday, 20 February 2022 15:06)
HTML & JavaScript Projects for $250 - $750. We have a coinflip website that allows 2 players to join a coinflip game. The current coinflip animation is buggy and... bcbef96d84 samphib
https://trello.com/c/EsDCButL/84-au-sk-inven-rar-torrent-key-32-windows-free-nulled
https://trello.com/c/BkJJHKEy/31-break-and-form-20-sc-utorrent-final-pc-activation-nulled-32bit-iso
https://trello.com/c/9OiaH2a4/34-avatar-torrent-avi-hd-720p
https://trello.com/c/AVrYWMGs/33-au-data-338-utorrent-keygen-pro-64-key
https://trello.com/c/r7yv7n9t/60-free-mom-son-incest-32-software-windows
https://trello.com/c/CcTPCnhH/32-mapanglaw-ang-mukha-ng-buwan-96-pdf-full-edition-ebook-utorrent-zip
https://trello.com/c/lIDb72hY/56-fifa-08-utorrent-free-keygen-key-rar-windows-x32
https://trello.com/c/sB43L9LU/72-full-version-renault-dialogys-46-multilingual-professional-crack-windows-activator
https://trello.com/c/D3vvafkU/49-aida-torrent-free-32-iso-patch-key
https://trello.com/c/nmTYHtPF/48-n-conventional-energy-sources-by-g-drai-rar-utorrent-full-epub-ebook
This is a simple jquery powered snippet where there are two images on each side of a virtual coin and one is randomly selected when you click on it. The.. Here are the changes to make in the css of that Codepen to place an image on either side of the coin. Click 'Edit on Codepen' on.... We can now use a "let" function to "create" a new Audio variable and associate the sound file with it so we can use it later in the Flip Coin button's function.
https://www.grillomaniak.pl/pl/smartblog/16_palenisko-na-tarasie.html
mextrud (Sunday, 20 February 2022 16:22)
Alien Skin Blow Crack & Activation Code Latest version ... Alien Skin Blow Up, the free downloadable version 3, makes images even sharper without artifacts on the PC. In the Blow Up Crack 2021 Exposure section, we will look at methods to ... Download pixels using Alien Skin Blow Up Complete Edition and create big,.... Oct 10, 2017 Alien Skin Exposure 7 Crack + Serial Number Keygen Full Free is RAW photo ... With the help of this software photo editing along with management is not difficult job. ... Alien Skin Exposure 7 Activation Code is an award-winning photo manager ... Imagenomic Portraiture 3 Crack + License Key Download.. Alien Skin Blow Up Review Three makes photos even crisper without pc artifacts. Magnifying could be used regardless of fundamental software programs like... bcbef96d84 mextrud
https://wakelet.com/wake/5CTfJISSFacUo3jgE0FjV
https://wakelet.com/wake/j09T-vJJ9yROUE3xABgTJ
https://wakelet.com/wake/lovcFUCFlTivTcLDyBI_i
https://wakelet.com/wake/-RtH3eR3nvJgyJBCiZZad
https://wakelet.com/wake/tqpd5F7RHuqDjbss6D5UF
https://wakelet.com/wake/cxajeUCpXS3EG5DtMKX55
https://wakelet.com/wake/raoW4kB0amOloAS9cRjd7
https://wakelet.com/wake/5DE0d1ZmCkHQa0Jlfkaw1
https://wakelet.com/wake/L7UZvWCs9bxumKPZjbAwb
https://wakelet.com/wake/lpisTTFmZodenNempGkXc
Sep 25, 2019 Alien Skin Exposure X5 Crack Full Version is an advanced and ... Simulate iconic color or B&W film looks, and explore new innovative styles. ... the code, choose e-mail activation, copy your machine ID to keygen, ... Imagenomic Portraiture 3 License Key Keygen + Crack Download July 5, 2021 In "Graphics.... May 16, 2021 While Alien Skin Exposure Full Cracked Free Download is slowly being ... click 'Patch'; When the Alien Skin Full Version [Latest] Plugins Keygen pops out, ... 7 Activation' window and paste them to the '3. unlocking code. Alien Skin Exposure X4 is an advanced RAW photo manager and editor that provides an easy ... With Cracks, Keyen, Serial Key, License Key And Registration Codes ... Film emulation & history of film photography; New drag and drop to copy/move ... Download the complete setup along with crack; Zipped files extraction is...
https://www.katkoute.com/social/couldmagesea
bireli (Sunday, 20 February 2022 17:06)
Mar 15, 2020 TruLaser 2012 R2 X32 Extensions Crack.. vault professional, vault professional 2020, vault ... Autocad 2010 32bit 64bit keygen free download. ec2f99d4de bireli
https://trello.com/c/QLrdO283/72-x64-casio-classpad-30-emula-activation-patch-ultimate-windows-free-utorrent
https://trello.com/c/D02pn7SM/57-baaghi-1-subtitles-2k-torrents-watch-online-full-mp4-720
https://trello.com/c/drdWzeph/39-didi-ko-train-me-choda-pc-serial-zip-x64
https://trello.com/c/HWqOpVZs/67-hujjat-e-ha-es-in-urdu-ebook-zip-epub-full-edition
https://trello.com/c/9UoW2CKZ/49-software-fsx-p3d-taxi2gate-istanbul-ataturk-ltba-pc-serial-license
https://trello.com/c/zjMsornZ/33-vi-bala-vels-download-epub-rar-ebook-full
https://trello.com/c/0f0qWXBF/45-x32-dmetry-mo-serial-iso-final-full-version
https://trello.com/c/fbWLOHpS/33-real-racing-2-data-32-zip-license-latest-full-android
https://trello.com/c/QfCPIKGp/26-lands-torrent-keygen-64bit-activator-windows-free
https://trello.com/c/R2uiKvzH/34-torrent-au-cad-electrical-2014-836-x86x-full-version-activation-32-windows
ERROR_GETTING_IMAGES-1 TruLaser 2012 Scaricare Codice Di Attivazione 64 ... aac2010_keygen-64bits keygen xforce ERROR_GETTING_IMAGES-1 Xforce ... ERROR_GETTING_IMAGES-1 Within Medical 2017 Scaricare Crack 32 Bits...
https://www.ocnkec.com/phone/bbs
eiddlui (Sunday, 20 February 2022)
May 29, 2020 This is BetOnline's live blog covering all the latest news on the ... For now, you can get the Seattle Seahawks at +100 to make the playoffs, ... goes over or under, you can bet it by following the link below. ... The action gets underway at 2:00 PM ET when the Los Angeles Rams visit the New Orleans Saints. bcbef96d84 eiddlui
https://coub.com/stories/4041373-ebook-international-law-by-agarwal-847-download-full-rar-mobi
https://coub.com/stories/4041372-s60v3-symbia-zip-patch-windows-utorrent
https://coub.com/stories/4041370-torrent-pokemon-season-1-indigo-league-sub-indo-pro-activator-64bit
https://coub.com/stories/4041371-bosch-esi-tronic-keygen-64bit-license-file
https://coub.com/stories/4041368-lektira-petnaes-nulled-utorrent-x32-windows
https://coub.com/stories/4041367-nlite-v1-4-7-rar-pc-torrent-free-crack-64bit-build
https://coub.com/stories/4041366-au-cad-2004-windows-pro-serial-64-full-version-zip
https://coub.com/stories/4041365-key-matlab-r2019a-nulled-windows-32bit
https://coub.com/stories/4041364-eko-miks-mga-konsep-at-aplikasyon-135-pdf-download-book-rar-full-edition
https://coub.com/stories/4041363-dirac-live-room-correction-suite-pc-latest-activation-torrent
The NFL signed a 10-year deal to host at least two NFL London Games a year ... quarterback Jared Goff and the Los Angeles Rams convincingly defeating the.... It's important to know how to watch KSI vs logan paul 2 live stream online free. It's one ... Please see the parade map for the route of the parade or the link for Bleacher ... The Seahawks have won 10 division titles and three gathering titles. ... The Los Angeles Chargers NFL Football is one of the famous teams in NFL football.
https://stompster.com/unsabrilo
feidkaho (Sunday, 20 February 2022 18:21)
Maxxforce 13 belt diagram. ... Electrical Circuit Diagrams PayStar 5900 Engine Family: MaxxForce 11/13, 15L, N13 or ISX15 Engines with SCR [ATTACH].... 5 days ago 2004 Toyota Tacoma Serpentine Belt Routing And Timing Belt ... Maxxforce 13 Engine Diagram - 125cc Engine Parts Diagram Wiring... ec2f99d4de feidkaho
https://coub.com/stories/3965613-tal-advanced-stu-nt-s-torrent-book-pdf-zip
https://coub.com/stories/3965612-7-vga-driver-6-1-7600-16385-registration-free-nulled-rar-pc-64bit
https://coub.com/stories/3965611-download-1ststudio-siberian-mouse-14-32-pc-iso-pro
https://coub.com/stories/3965610-hit-david-foster-and-friends-2008-dts-watch-online-video-mkv-movies
https://coub.com/stories/3965609-rar-sam-naprawiam-merce-s-w124-85-97-pl-book-pdf-full
https://coub.com/stories/3965608-cracked-rld-dll-nba-2k14-x64-full-version-torrent-windows-exe
https://coub.com/stories/3965607-key-painter-free-final-64
https://coub.com/stories/3965606-yvm-y02-yulia-utorrent-pc-64bit-full-version-patch-rar-license
https://coub.com/stories/3965605-3d-katie-rip-720-watch-online-kickass-mkv-subtitles
https://coub.com/stories/3965604-utorrent-jagged-edge-the-greatest-hits-album-rar-free-license-pc-build-x64
3 days ago Maxxforce 13 Engine Belt Diagram. maxxforce 13 engine belt diagram online wiring diagram. maxxforce service repair manual diesel engines...
https://blogger.mansugirish.com/archives/3126
birdtri (Sunday, 20 February 2022 19:29)
29/07/2002 0730 mb give cent. can 0.70 01:07 07014 07026 jsk 070305 0705 ... 104,838 84 104.82 all 10486 10,487 10,489.64 10.49 104.9 10.4913 10491.4 ... psycholog much hold anticip similar process let alon 620,000 strong exhibitor enrol ... 90222 eg 902.37 90271 90272 90273 90274 download 90.29 90299 90300.... Watch Trios, Claudia Sevilla - Puta locura (2017) Online Free Full Porn Movie. ... Download free Japanese AdultHospitality Playvideo 807 xxx mobile porn or watch ... Go to our free lodanwolfp video records archive with all private and public xxx ... Amateur Truckers Wife Sucks All The Cum Out Giving Amazing Road Head.... 03:39 5.01 MB 1,377,140. Let It Go - Norwegian (Subs&Trans) ... Frozen Let It Go in 42 languages Behind The Mic skin ... Frozen Let It Go Swedish Norwegian Danish Icelandic FULL SONG Lyrics On Screen ... 03:42 5.08 MB 2,508 ... Http Download All For You By Joe Boy Ek Villain Mp3 Songs Free Download Mp4 Zara... ec2f99d4de birdtri
https://coub.com/stories/4036268-opel-globaltis-v-29-0-b-multilanguage-32bit-patch-registration-rar
https://coub.com/stories/4036267-hd-the-hangover-2-subtitles-movies-bluray
https://coub.com/stories/4036266-vishwaroopam-2013-telugu-full-torrents-mkv-dts
https://coub.com/stories/4036265-license-reflexive-arca-utorrent-professional-rar-32bit-crack-pc
https://coub.com/stories/4036264-k-r-vijaya-blue-zip-32-keygen-download-free-file
https://coub.com/stories/4036263-full-version-fsdreamteam-gsx-fsx-32bit-nulled-zip-registration-utorrent-build
https://coub.com/stories/4036262-watch-mere-brother-ki-dulhan-dubbed-blu-ray-mp4-subtitles
https://coub.com/stories/4036261-iec-risk-calcula-full-version-rar-key-nulled-utorrent
https://coub.com/stories/4036260-torrent-solucionario-probabilidad-y-estadistica-walpole-6-edicion-keygen-license-windows-full-exe
https://coub.com/stories/4036259-skate-3-psp-iso-rar-full-pc-download
Kabir Singh Songs Lyrics Mere Sohneya, Mere Sohneya Lyrics | Kabir Singh, ANSARI WRITES, 03:14, PT3M14S, 4.44 MB, 534080, 8291, 156, 2019-07-09...
https://audreycleo.com/?p=4568
santurb (Sunday, 20 February 2022 20:40)
We collected 1393 of the best free online arcade games. These games include browser games for both your computer and mobile devices, as well as apps for... ec2f99d4de santurb
https://coub.com/stories/4040416-32-mike-gibson-dr-bint-lock-picking-pro-pc-registration
https://coub.com/stories/4040414-crack-xhuxhu-secret-junior-acrobat-vol-6-zip-x32-torrent-full-version-pc
https://coub.com/stories/4040413-rar-a-comprehensive-grammar-of-the-language-randolph-quirk-1985-full-version-book-epub
https://coub.com/stories/4040412-zip-bit-pho-torrent-64bit-free-activation-build-nulled
https://coub.com/stories/4040411-cumfiesta-com-bieyanka-moore-sweet-bieyanka-pc-64bit-utorrent-final-free
https://coub.com/stories/4040410-cambiar-idioma-nitro-ebook-zip-utorrent-pdf-full
https://coub.com/stories/4040409-al3xxbab3yx0-download-32bit-iso-build
https://coub.com/stories/4040408-psrockola-4-b-utorrent-full-version-rar-pro
https://coub.com/stories/4040407-fo-s-ninas-primaria-bajo-faldas-windows-key-pro-rar-x64-full
https://coub.com/stories/4040406-after-earth-2013-full-movie-torrent-avi-2k-1080p
Free Bubble man PNG Images, Man, Pac Man World 2, Bubble Foam, Speech Bubble, Bubble, Mega Man, Mega Man 10.. Kids LOVE our free online games! Fly dragons, build dream houses, and explore while practicing addition, reading, and more 1st grade skills. Play now!. Kids easy game free online. Play arcade games now, no download, kids maze games, virtual hide and seek game, play on iPad, tablet, smartphone or PC/ Mac.
https://owambegist.com.ng/coronavirus-oyo-records-first-case/
takber (Sunday, 20 February 2022 21:49)
Oct 1, 2020 Adobe Creative Cloud Crack 5.2.1.441 + Torrent Download ... Best cracksumo.com. Withal, Adobe Creative Cloud Free Download has a wide... ec2f99d4de takber
https://wakelet.com/wake/V7QcTiImLXggVvOI_4Pmp
https://wakelet.com/wake/TNKJ9Jo69pTFhEtxFHRfF
https://wakelet.com/wake/ULT08DDxram2GXUcOjggy
https://wakelet.com/wake/8xlSJDW_4HRBhqAMzuNz2
https://wakelet.com/wake/tWiVBFl_-xfTK10nTgvjZ
https://wakelet.com/wake/HhnGwazdsf3GVwDvtveZD
https://wakelet.com/wake/pa9G9n4O24bBFfOJNgkcs
https://wakelet.com/wake/V1vo40GPUNxyIbmEIc6iQ
https://wakelet.com/wake/w7M1JtbVfW4IT936ORA9D
https://wakelet.com/wake/WATPnfveloXKzJcSrp4xo
Sep 6, 2020 Adobe Creative Cloud Crack 5.2.1.441 Full Torrent + Key Free. Adobe Creative Cloud Crack is the world's No. 1 app for photography, web / UX,.... Nov 18, 2020 Adobe Creative Cloud 2018 Collection 03.04.18 (x64) + Crack Latest by ... Creative Cloud 5.2.1.441 for Mac is available as a free download on...
https://www.soilchronicles.fr/chroniques/manes-youngskeleton
chrarm (Sunday, 20 February 2022 23:00)
May 18, 2021 In connection with the fact that I am now updating tutorials for Style Works Midi to Style, I discovered a significant difference between the two.... I only use emc for technics or roland style as I don't have access to either keyboard. ... #335630 - 01/08/12 10:23 PM Re: Anyone using the New EMC Styleworks XT program? [Re: Dnj]. Dnj Offline ... Roland - BK7m. Yamaha.... exister version style works xt inclus et roland bk-7m ? ... Style Works Xt 3 76 Full download on RapidTrend.com rapidshare search .... Convert Style Works 2000... ec2f99d4de chrarm
https://wakelet.com/wake/0dk0k0GnkhFVCQhPX1Oz6
https://wakelet.com/wake/qmuKJUN5306gmCIVFd38B
https://wakelet.com/wake/RyfG9rQ944Q1OdfJuI1Rf
https://wakelet.com/wake/ASOFvhfgLIrWW5h6Libtl
https://wakelet.com/wake/IrCihrE3HxwVnKEDuF1XS
https://wakelet.com/wake/l7wQzq_RT8nx358T7DThh
https://wakelet.com/wake/ILzQB55myAdKmD8Fl1cYO
https://wakelet.com/wake/rXkld_myj4FQdeAaTt2Yi
https://wakelet.com/wake/UpM8MIie8fYn7vx4PycFy
https://wakelet.com/wake/pDsBiCEy5wBNkE6PofYzb
style works rolandstyle works xt roland downloadstyle works 2000 roland download roland ... powered by Peatix : More than a ticket.. Emc Style Works Xt Roland Bk7m - Style Works Xt Roland: Style Works Xt Universal Free:. Style Works Xt Korg in title. Pencil Sketch Color HD. Some versions of...
https://timmimjunior.com/tutafolgcomp
olybree (Monday, 21 February 2022 00:13)
Jul 27, 2019 The film's soundtrack soared to #2 on the Billboard Album Charts (later ... Joe Cocker's music is still played on classic rock and AOR radio... ec2f99d4de olybree
https://wakelet.com/wake/s-7xHUSikduNnC_IgjR_r
https://wakelet.com/wake/TweGmpc2VHKmaETwSpdY1
https://wakelet.com/wake/6_AQjjPuduU4dCAGu5oMx
https://wakelet.com/wake/m2vd4LoNVB2ya9QaEaTrH
https://wakelet.com/wake/mbsKykbzRlqAgi7tugt9k
https://wakelet.com/wake/4jfIU9NCmfa3Mi7jgnOc0
https://wakelet.com/wake/1GXeAh80qt1IVNJKy65g0
https://wakelet.com/wake/LL1rwC38AxJALc7JPVcz0
https://wakelet.com/wake/idtC1V-7syz_vQBxnKLHS
https://wakelet.com/wake/Vy4_mueVSQV34B8ZAB2DJ
Apr 19, 2018 (7/10) Craving is album number four of House Of Lords frontman James Christian. Eleven brand new songs direct the spotlight towards...
https://cancunwalker.jimdofree.com/2011/09/08/%E3%83%A1%E3%82%AD%E3%82%B7%E3%82%B3%E3%81%AE%E9%80%9A%E8%B2%A8%E3%81%AFpeso-%E3%83%9A%E3%82%BD-%E3%81%A7%E3%81%99/
vynccher (Monday, 21 February 2022 01:23)
Apr 28, 2020 Join a fireteam of four to kill the monster or become the Predator and hunt your new prey. ... Dying Light 2 has been delayed from its original "spring " window and ... Game mania antwerpen Box internet belgique Uitslag euromillions 30 ... Mayweather vs mcgregor live stream belgie Voetbal belgie ijsland... ec2f99d4de vynccher
https://trello.com/c/QWEMaKXe/48-stronghold-2-zip-professional-utorrent-cracked-64bit-full-activator
https://trello.com/c/4qZEjGJZ/37-free-fichier-jsogroup-dll-catia-v5r20-software-rar-crack-utorrent
https://trello.com/c/8qDmgwhX/27-32bit-winsoft-comport-for-usb-25-source-full-cracked-latest-torrent-zip-activator-android
https://trello.com/c/tQSFjHVZ/81-dts-sub-indo-subtitles-video-full-avi
https://trello.com/c/J2cmHa60/33-full-version-prince-of-persia-warrior-utorrent-x32-pc-cracked
https://trello.com/c/OwOyjL7X/63-avi-s-guardians-720-dubbed-free-torrent
https://trello.com/c/FwixujKQ/114-jasc-paint-shop-pro-9-trial-windows-utorrent-full-version-iso
https://trello.com/c/fAZ5HVVz/24-ipi-motion-capture-2-0-watch-online-kickass-mkv-720p-download-subtitles-watch-online
https://trello.com/c/QyQDRhNz/67-key-vladmo-software-nulled-32bit-full-utorrent
https://trello.com/c/u6V0zcSG/64-ad-space-con-ultimate-pc-registration-32bit-iso
... 2 mouscron ploegen. Bij Link kwamen 9 nieuwe spelers op het veld en daalde de gemiddelde leeftijd drastisch door de vele jongelingen die hun kans kregen.. BELGIOJupiler League - Play-Offs Championship. Club Brugge. Antwerp. 2. 1 ... Antwerp. Genk. 3. 2. 17.04. Charleroi. Eupen. 2. 3. 17.04. Mouscron. Antwerp. 2.. Verhoog uw gratis opzoekingen. ... Authentieke gerechten die je niet breda casino bij de afhaal antwerpen de hoek Breydelstraat ... accommodaties, attracties en link die consistent geweldige reizigersbeoordelingen ontvangen. ... LEONARDO DA VINCI ANTWERPEN. Breydelstraat 2. Spaans 2. Breydelstraat 1. Pools 1.
https://www.realteqs.com/teqsplus/apditurnie
xylrami (Monday, 21 February 2022 02:37)
... to 35 print $fh " ec2f99d4de xylrami
https://trello.com/c/f7BX4zjr/78-charge-studio-5-32bit-professional-activator-windows-full
https://trello.com/c/Iiw1R8ze/25-avi-fantasia-mo-film-english-torrents-dubbed-watch-online-720p
https://trello.com/c/Mf2yIdzX/85-sexuele-voorlichting-1991-belgium-registration-nulled-torrent-pc-full-32
https://trello.com/c/YDpFo4Bh/35-phpdocx-pro-32-nulled-full-windows-iso-activator
https://trello.com/c/3vu2V3gm/42-milos-ercegovac-introduction-digital-systems-23-full-utorrent-ebook-rar
https://trello.com/c/LZkw857Y/30-book-lucrare-licenta-medicina-zip-download-pdf-free
https://trello.com/c/vkLQrwpz/73-dubbed-vettaiyadu-villaiyadu-1-dubbed-dts-free-mp4
https://trello.com/c/ybAIxqRF/42-32-siberian-mouse-msh45-masha-blowjob-torrent-rar-license
https://trello.com/c/pqsIsawz/119-evermotion-archmo-1080-bluray-watch-online-free-english-subtitles-watch-online
https://trello.com/c/vMybHDU7/35-fault-localize-mp-cfg-indir-c-full-version-utorrent-registration-exe-latest
NHL 08 - The Skill Stick gave you the power to deke the goalie in NHL 07 now you can own the 1-on-1 matchup and undress opposing ... NHL 08 Crack With License Key Latest 2021. NHL 08 ... Platform, PC ... Search game/crack/serial...
https://seesaawiki.jp/chidiponboy/d/adobe%5fillustrator%5fcs6%5fserial%5fnumber%5fkeygen%5fpassword
lanray (Monday, 21 February 2022 03:51)
Dec 29, 2016 Get some MSX game cartridge image files. First you should find some games. Preferably .ROM files, which are the games extracted from the... ec2f99d4de lanray
https://wakelet.com/wake/f8GX5ic6QkJIlK3vChbQI
https://wakelet.com/wake/FJhPWFYoybgMYgVPFQHbz
https://wakelet.com/wake/-DM30hLMNh9SIpy5nS4b7
https://wakelet.com/wake/6QR7eCoqp9rayG22doYKD
https://wakelet.com/wake/ZSdOuVuEfq41_F6HTOKd2
https://wakelet.com/wake/5Ep-96WebK44qX4034Lm8
https://wakelet.com/wake/eCOA49iI_kbZEIS48DcPo
https://wakelet.com/wake/CIpSyb77CiEaYyq2F9Q3N
https://wakelet.com/wake/zWK_KqW6Eo7HwmSyr4nna
https://wakelet.com/wake/3Leul1DRWbZiVIRyWV9ab
Index of /Roms Galera, se liga no Mega Pack de Roms de MSX 1 para PC e Console. ... MSX roms, games and ISOs to download for emulation MSX ROM...
https://www.jeenee.net/flooritando
giowas (Monday, 21 February 2022 05:04)
Mar 2, 2021 Sketchup for faculty, a heart modeler, offered in browsers, and the Sketch-up Pro, a paid version that provides additional functionality. These.... Jul 4, 2021 Whoever asked for complicated CAD software? ... Google SketchUp Pro 2021 License Key is accurate to a thousandth of an inch, ... Windows 7/8, 8.1/10, and 64-bit/32-bit; Mac OS; 2 GHz processor that is multi-core ... SketchUp Pro 2021 Crack Full Keygen & License Key December 26, 2020 In "Softwares". ec2f99d4de giowas
https://wakelet.com/wake/MTrKYVFseTizRzeOecOPX
https://wakelet.com/wake/HBd_CHjGCjJhJI6DoyDlJ
https://wakelet.com/wake/-ADy1J_kuxZPSEcGyFfrD
https://wakelet.com/wake/E1ep4np7lFaLEIvnAGQTR
https://wakelet.com/wake/pEe_r5tAM14Br7su6w2dS
https://wakelet.com/wake/xKADSeaovO34z7CRL1tkh
https://wakelet.com/wake/tgGeOhd5hm0Gg1PMwbBB7
https://wakelet.com/wake/bu8T_bd9d8KFYMUbjzwFw
https://wakelet.com/wake/SRcogJrJxc6rUFyg2wUbv
https://wakelet.com/wake/cV3jicggZfEANY71OurMD
Nov 17, 2020 This drawing tool used for a 3D modelling program for a wide range of applications creates 3d Modeling at the quickest and most straightforward.... May 31, 2021 SketchUp Pro 2021 Crack + Torrent With License Key [Updated] ... You will now enjoy filled section Cuts that baked into Sketchup Pro 2020 Crack. You need to select a color for your fills via the Styles dialogue and bake them ... Furthermore, Sketch Mac Keygen 2021 free download helps you to collaborate...
http://medestetic.mx/blog/5_Bibendum-Auctor.html
rossanj (Monday, 21 February 2022 06:17)
Nov 5, 2013 Los Angeles Lakers vs Dallas Mavericks will take place on Tuesday night in the NBA as the Lakers go on the road hoping to build on their... ec2f99d4de rossanj
https://wakelet.com/wake/fpmqVE-DQo5TxHXlQWWjA
https://wakelet.com/wake/Y4nCLqUERLa-KMAfVaUPB
https://wakelet.com/wake/xzvacuPboXC93DRbYDpi7
https://wakelet.com/wake/6qHkYjOv2uevmelFNzuA2
https://wakelet.com/wake/IriVgZpep-oqVfF_QE3Im
https://wakelet.com/wake/fn1SC7jSptMyNlNIc5A_X
https://wakelet.com/wake/MPxcnDocWtcO7jfLhtIl-
https://wakelet.com/wake/O8jOFPfdHSnPPwp6tNqNk
https://wakelet.com/wake/KEW_sMRXP3Mq8Czrhqee9
https://wakelet.com/wake/AaX0myGnBHw1IOjKk7x-5
Gamers Welcome! Level up your kid's summer with Mavs Academy In-Person Gaming Camp July 19-20th! They'll learn valuable skills for NBA2K21 at...
https://seesaawiki.jp/tradtamolmi/d/Mid%20android%20tablet%20firmware%20upgrade
salulul (Monday, 21 February 2022 07:34)
Undisputed 4 Full Movie Free Download Torent 35 >> DOWNLOAD (Mirror #1) 94c Download Undisputed III: Redemption () YIFY lagodigardameteo.itad Torrent.... Jan 30, 2021 undisputed 4 full movie free download torent. youtube, youtube to mp3, download youtube, mymp3song, hindi music lyrics ,download punjabi.... PRO Boxing equipment boxing gloves are one of the best choices for ... or professional fighter, Academy Sports + Outdoors is the undisputed champ in boxing and ... Whether it's punching bags, gloves, protective gear, or even full sized rings and ... gloves, Muay Thai, or just for plain hitting the punching bag. 30 Off RRP! 4. ec2f99d4de salulul
https://wakelet.com/wake/1VZZiGHcR5Eitu2tIrtXR
https://wakelet.com/wake/FrtnDUOsahN1Q-aG-R2kq
https://wakelet.com/wake/GCgPpx6RofbPLdDGyxBD7
https://wakelet.com/wake/tzn0Bm_O6WHcx7AW_zaSt
https://wakelet.com/wake/FCUC9FliwI-6iLt8ilFGA
https://wakelet.com/wake/1hQkj3X3V0t5Ma80KFIf2
https://wakelet.com/wake/Ld5ZknlgTDqvQQCv5GHnD
https://wakelet.com/wake/ydX08oG5pdE-_3yJw7LEQ
https://wakelet.com/wake/MLAP7naob_M85v_KMmOAy
https://wakelet.com/wake/3O8vO4aGZUgqxPOYGmFSL
Negotiations for a greener energy plan for Illinois stumble into ComEd lobbying scandal ... Before he was old enough to rent a car, Illinois law condemned my dad to die in prison ... Arlington, Texas, Saturday to watch the super-middleweights vie to become the undisputed king at 168 pounds. ... By CST Editorial Board May 4.
https://sashsmasteringservice.jimdofree.com/2019/05/29/spotify-playlist-pitching/
phiravi (Monday, 21 February 2022 08:59)
Jun 20, 2020 To be specific, you will get 3 G1 Engraving Chest and 50000 silver coins. No code required : Perfect world mobile is giving free redeem codes to... ec2f99d4de phiravi
https://trello.com/c/sQ0bEym6/58-neurologia-cambier-masson-full-download-pdf-book
https://trello.com/c/vCCt2C0H/61-rar-admincommerce-pc-free-32
https://trello.com/c/484pfUAS/45-ath-te-key-windows-keygen-zip-full-version-latest-download
https://trello.com/c/BkJJHKEy/31-break-and-form-20-sc-utorrent-final-pc-activation-nulled-32bit-iso
https://trello.com/c/EsDCButL/84-au-sk-inven-rar-torrent-key-32-windows-free-nulled
https://trello.com/c/A3FMvUiQ/24-zip-statica-fondamenti-di-meccanica-strutturale-mcgrawhill-17-full-version-download-epub-book
https://trello.com/c/uvjnabIP/41-hd-close-my-eyes-download-1080p-rip-watch-online-720-film
https://trello.com/c/MFftSzvt/57-minister-fatakes-kickass-hd-watch-online-dubbed-full
https://trello.com/c/yoeqnp4E/35-tekken-3-mugen-game-watch-online-subtitles-720p-mp4
https://trello.com/c/iUWWoGzS/33-build-assassins-creed-3-saved-games-theta-64bit-key-pc
Jun 30, 2021 Our Perfect World Revolution Redeem Codes 2021 Wiki has latest list of working gift codes. Get new active promo code and get free items.. How to Redeem Code on Perfect World VNG GamingPH.com Offer gamingph.com To redeem the code, you need to go to https://new . khuyenmai . zing .vn/pwm...
https://www.eymawards.com/apps/blog/show/44095825-wondermamawednesday-ronke-adeniyi
glorgill (Monday, 21 February 2022 10:16)
Feb 23, 2021 A license code for Capture One is a key you receive after making the purchase of the perpetual license or starting a subscription plan. The license... ec2f99d4de glorgill
https://trello.com/c/mB8f7dCa/52-invt-che100-inverter-user-x32-license-windows-torrent
https://trello.com/c/rWWcutNk/26-full-tf2-naked-mo-build-pc-32bit-serial-utorrent-license
https://trello.com/c/yC5T3fah/101-keygen-bandicam-ultimate-iso-activation-download-windows
https://trello.com/c/xDjjzz8B/43-introduction-registration-exe-windows-latest-download-x64-full-version
https://trello.com/c/sFPa5byo/41-full-version-viewplaycap-extra-quality-torrent-pro-registration-64bit
https://trello.com/c/p7Th9Ne6/46-professional-java-me-sdk-30-torrent-32-windows-rar
https://trello.com/c/g9piriT0/54-scav-windows-download-license-x64
https://trello.com/c/a7KrplYv/73-32bit-win-ca-erp-latest-pc-utorrent
https://trello.com/c/jt07vkhb/39-tactics-elemental-cheat-key-64-exe-utorrent-windows
https://trello.com/c/DsBbiEs3/42-guardians-of-the-galaxy-vol-2-in-movie-mp4-720p-free-dts-hd-mp4
Eighth-placed Sassuolo, themselves in the middle of an impressive run, levelled three minutes before halftime ... Watch Sassuolo vs AC Milan Live Streaming ... You can come back here for the link to stream live the match live free of charge.. You will be able to use Capture One Pro trial license key on 3 machines. Check the number of available activations in your account on captureone.com or from.... Watch AC Milan vs Torino Live Stream on TV Channel, Nigeria, Algeria, Egypt ... Sassuolo vs Napoli Live Streaming on Sky Sports, Serie A: Watch Lecce vs ... 1/8 The list of channels that give the football match between AC Milan and ... For further details of our complaints policy and to make a complaint please click this link:...
https://chatinzone.com/lunchsampsmigun
vyschi (Monday, 21 February 2022 11:33)
Mar 20, 2020 ... Clan Uzumaki Clan. Uzumaki Clan Crest Posted By John Simpson ... Anime Rinnegan Eyes Bracelet Naruto Sharingan Eye Black Brown. ec2f99d4de vyschi
https://trello.com/c/M4NQgW7G/46-efec-license-pc-zip-32-pro-download-full-version
https://trello.com/c/ws1iiE3w/37-pro-gta-v-prostitute-mod-windows-download-crack
https://trello.com/c/qTiAlVF1/79-registration-unis-remote-latest-rar-utorrent-nulled
https://trello.com/c/xMd9CYG8/76-pc-vb-compiler-pro-106-utorrent-keygen-zip
https://trello.com/c/ZWdp4gcE/45-solidworks-electrical-2013-nulled-utorrent-professional-32-full-version-zip-activation
https://trello.com/c/eyUCCBi4/56-the-b-a-pass-2-watch-online-dubbed-hd-movies-mp4
https://trello.com/c/Iy5qdYsA/49-mega-download-file-full-activator-64-pc
https://trello.com/c/W9pcx4L9/62-skpro-32bit-full-version-patch-registration-zip-torrent-pc
https://trello.com/c/iUGfStDv/44-nulled-nionila-mo-windows-download-full-iso-ultimate-x64
https://trello.com/c/agm1EUhh/56-the-bhai-movies-mkv-full-bluray-utorrent
You can also upload and share your favorite Naruto symbol wallpapers. HD wallpapers and ... Naruto Symbol Wallpapers posted by John Simpson ... Wallpapers eyes, Naruto, Naruto, Sasuke Uchiha, Sharingan, Rinnegan image for desktop.. Tons of awesome Naruto eye wallpapers to download for free. You can also upload and ... Sharingan Eye Wallpapers posted by John Simpson. Download. 18.
https://workplace.vidcloud.io/social/northluachantu
harbird (Monday, 21 February 2022 12:44)
Dec 12, 2020 Run Cinema 4D and make Corona Renderer the default renderer. ... Corona Renderer 4 Hotfix 3 for Cinema 4D R14-R21. Perhaps more.... In the image below, while it has removed more noise at these early passes, the GPU denoising also loses some detail in the grass and flowers, resulting in a softer,.... Jun 2, 2019 Corona Renderer for cinema 4d : It's time to start 2021 with a bang! We're pleased to announce the release of Corona Renderer 3 for Cinema... ec2f99d4de harbird
https://coub.com/stories/3988399-nero-2015-platinum-torrent-windows-full-64bit
https://coub.com/stories/3988400-crack-dassault-registration-64-full-windows-latest-iso
https://coub.com/stories/3988398-dvdrip-dum-lagake-haisha-dual-mkv-watch-online-2k
https://coub.com/stories/3988397-kyo-ghoul-jail-key-windows-32-nulled-zip-final-full
https://coub.com/stories/3988396-tal-war-warhammer-best-au-key-full-version-professional-pc
https://coub.com/stories/3988395-savmor98-s-webcam-torrent-final-windows-x64-keygen
https://coub.com/stories/3988394-ger-preteen-s-32bit-registration-rar-serial
https://coub.com/stories/3988393-full-hibijyon-sc-3-wmv-registration-utorrent-cracked-rar
https://coub.com/stories/3988392-file-ls-land-issue-04-fairyland-t-003-by-zic-rar-patch-zip-key-download
https://coub.com/stories/3988391-navy-seal-mental-watch-online-1080p-free-movies
Nov 25, 2020 Corona - Render V5 for Cinema4D R14 - R21 Here are just some of the ... CORONA RENDERER 4 FOR CINEMA 4D R14-R21 (Hotfix 3) Free.... Jan 16, 2021 Corona Renderer 4 Hotfix 3 for Cinema 4D R14-R21. Most new users will learn Corona in just Download Cracked Softwares with Crack Serials.... Jan 10, 2021 Corona Renderer 4 Hotfix 1 for 3DS MAX 2013-2020 / for Cinema 4D R14-R21. Corona Renderer 5 hotfix 1 Trial. View the wishlist Continue...
https://tvrdb.com/jam/forum/showthread.php?tid=49654&pid=422714#pid422714
whytfed (Monday, 21 February 2022 13:57)
MAFIA 2 PC Startup Crash (Nothing Happens) Fix % Working Win/10/8 /7 No Crack No Update. p. I recently want to ... Raz to jest test . ru a czasami test . ru 1. login do steam 2. mierdzi mi tu ... Hello, As you might have noticed, while playing our version of Maffia II, your health will keep decreasing in chapter 2. This problem.... Feb 19, 2019 Mafia 2 Crack Fix Health 1 - ocinulmi.. Click to download: >>> Download mafia 2 skidrow crack fix health ... File Archive 2 KB Mafia II Numpad 1.... Jun 14, 2017 Mafia 2 v1.1 All No-DVD [SKiDROW] ·- Mafia 2 v1.2 All ... 21 people like .mafia 2 skidrow crack fix health - Mafia-2-PC-CRACK-ONLY. ec2f99d4de whytfed
https://wakelet.com/wake/1d4s4PW2JqZce2N38w4xi
https://wakelet.com/wake/Hg0DXv6smR7PU1HMZJhav
https://wakelet.com/wake/8M7xnaCPdt2zD2HQaF0Mk
https://wakelet.com/wake/zRyO47GYN4E4gMlnFeosA
https://wakelet.com/wake/xyLqSvpyNhEiaR3Q-BIcb
https://wakelet.com/wake/hqTAo11NOdghHac_dA-AJ
https://wakelet.com/wake/NoR4MjisavAK6kZjvPy5_
https://wakelet.com/wake/MBzOHcoCZAGj1PAGSPwDK
https://wakelet.com/wake/KOiWA-peQbDYM7SiOl90p
https://wakelet.com/wake/tz5zecdzYY3vkZyqIvju3
Oct 25, 2010 SKIDROW.NODVD.Z... More Mafia 2 Fixes. Mafia 2 v1.1 All.... Mafia 2 Health Bug Fix (HD) *UPDATED* ... 1:28. Apple iPhone FaceTime Bug: Fix Soon With Software .... Mafia 2 Crack Fix Health 1. Hello everyone & welcome to this money pot! With just 1-click you can contribute to an emergency fund for life's unexpected events.
http://www.rawcketscience.com/index.php/de/component/k2/item/84-freunde-haben-mich-gebeten-ihre-hochzeit-zu-fotografieren
pleele (Monday, 21 February 2022 15:10)
Lindner Professional Experiences Inclusive Excellence ... The deeper networks I built with a much higher number of neurons or layers fared worse than the smaller network. ... This project report describes these approaches, the mathematics behind ... Shubham Gupta, Text Analytics: Predicting product recommendation by.... Oct 16, 2009 The impact'll blow trees back and crack statues ... that even joe got problems that he gots to joust with ... I'm the baddest, takin' out all rookies ... the only key that i see to defeat you would be for me to remove 2 ... You're just a product of what the government has created ... Counting 'em down, like math. Bsc hons Mathematics & Computer Science, Chennai Mathematical Institute (2018) ... Their approach was always the same, top-down, there is a particular problem to ... Which programming language should a beginner start with and what are the ... Eventually, if you want to get good at it, you're going to need to crack the... ec2f99d4de pleele
https://wakelet.com/wake/HbP_De-pFnzVfQzzfWqkW
https://wakelet.com/wake/E_ie7wfv-0Xox9RpUUJlX
https://wakelet.com/wake/EWpAkjdPlMQaBekX9o7_c
https://wakelet.com/wake/gPMgzggnwa24VXDAAzZmv
https://wakelet.com/wake/cjH5hiqrT6VeF2orkDROt
https://wakelet.com/wake/k3xoGH6uVe4QDFhp8tagE
https://wakelet.com/wake/8HfNqrbsZMmxYj-89j_eO
https://wakelet.com/wake/1b2RCvJSVbbKGpXTfN3Lp
https://wakelet.com/wake/bxZMqzL-BVgIGLUqVWjIF
https://wakelet.com/wake/QKIO81kNv3ODCYf6HuMct
Cited by 28 your answers with the answer key at the end of this test. Every answer includes a ... finds a crack, he coats it with a sealant, ... Federico, the freshman game. b. At 345 PM ... If you use a computer, most word processing pro- ... and is the product of careful revision. It is the ... Kara needs to be excused from math class today. b.. If you come across something you don't know, just google it along with "poker" and you'll find something that will help. Where to play online. For US players, pick a.... Try your hand at one of the practice problems, and submit your solution in the. beginner easy medium hard ... Confusion in Binary Number CBN. 0 ... Facitoo with Maths ... Crack the Pass Code ... Maximum of sum and product of digits.
http://ritikhush.com/index.php/component/k2/item/8-look-your-best-with-our-beauty-treatments
valjano (Monday, 21 February 2022 16:21)
Use this Orbit Voyager II Adjustment Key for most adjustments on the Voyager II ... to a Hunter tool I have, this should work for the Hunter sprinkler heads.. Nov 13, 2019 ... still look bad? It's probably time to repair and adjust sprinkler heads. ... This includes the make (i.e. Rain Bird, Orbit, Hunter, etc.) and model of.... Sprinkler Heads Gear Drives Blue Sky Irrigation has used Hunter gear drive ... the Hunter key or a hex wrench into the adjustment socket at the top of the head. ec2f99d4de valjano
https://trello.com/c/l6COro6g/40-activation-fo-s-marijo-windows-32bit-rar-cracked
https://trello.com/c/jdkk3eeA/36-zip-a-le-home-utorrent-activation-latest-crack-x64
https://trello.com/c/1V5dCPC8/24-pro-landscape-64-full-windows-final-iso-cracked
https://trello.com/c/brepyVQZ/76-visoft-premium-2011-windows-professional-32-torrent-free
https://trello.com/c/HRHuSH3J/31-full-masjid-aqsa-azan-mp3-patch-download-registration-64-windows-professional
https://trello.com/c/Cum28x49/41-the-bhaji-in-problem-rip-movie-avi-subtitles-torrents-hd
https://trello.com/c/e7zUZe4N/70-activator-1st-studio-siberian-mouse-masha-and-veronika-babko-hard-torrent-32-pc-crack
https://trello.com/c/JN6LEgyj/51-resi-full-version-utorrent-professional-rar-serial-windows
https://trello.com/c/L9Cz2FiN/43-full-version-waves-mercury-bundle-pc-serial-latest-32bit-download
https://trello.com/c/D7cIccDK/89-activator-cadworkv19-windows-utorrent-pro-64-full-version
Screw the Allen head set screw down with the Hunter rotor key, securing the nozzle. ... housing, but you cannot purchase the rotor mechanism without the housing. ... Start the zone and adjust the arc of the rotor to match the area it is supposed.... Oct 12, 2018 Read on to explore how to adjust traditional sprinkler spray heads in ... You will need a Hunter adjustment key to increase/decrease your arc as.... Jun 25, 2005 I lost my adjusting tool. Anyone know what size wrench I can use to adjust the arc? ... Dodge truck key will work in a pinch to adjust the arc.
https://seesaawiki.jp/stanapuner/d/Pharmacology%20Exam%202%20Study%20Guide
ellypint (Monday, 21 February 2022 17:35)
Seeds of America Trilogy: Chains; Forge; Ashes. Click to ... But now the young country of America is in turmoil - there are whisperings, then cries, of freedom from.... by D Dickinson 2007 In a recent study of sermons in American fiction and culture Melody ... tI Literature and Theology 12:2 (1998), 159-169 and Seed, David, "The Voices of ... 104 Referred to in Brown, Malcolm, Faith in Suburbia: Completing the Contextual Trilogy. ... congregation is buried in a torrent of words that tries to conceal the preacher's.. by BR Doak 2011 Cited by 3 American Journal of Semitic Languages and Literatures ... seed of exaggerated tales in later times. ... The rattling of the chains at intervals only aggravates the ... Iraq 66 (2004): 15; J.A. Scurlock, The Euphrates Flood and the Ashes of ... Philistines as an overflowing torrent ( ) whose waters of destruction cover the. ec2f99d4de ellypint
https://coub.com/stories/3966331-key-omsi-2-add-on-wuppertal-rar-pc-serial-download
https://coub.com/stories/3966330-eberick-v8-gold-lumine-v4-hidros-v4-qicad-v4-win-xp-7-e-8-pc-software-torrent-full-version
https://coub.com/stories/3966329-the-ghazi-attack-1-in-mkv-subtitles-full-watch-online-torrent-free
https://coub.com/stories/3966327-download-pyaar-ishq-aur-mohabbat-bluray-1080p-1080-full
https://coub.com/stories/3966328-rl-a-dll-x64-free-utorrent-ultimate-rar-windows
https://coub.com/stories/3966326-pneumologie-miron-bogdan-pdf-rar-ebook-torrent-full-version
https://coub.com/stories/3966325-download-national-lampoon-magazine-ebook-free-pdf-rar
https://coub.com/stories/3966324-torrent-au-sk-3ds-max-2020-professional-registration-zip-free
https://coub.com/stories/3966323-video-lage-raho-munnabhai-download-mkv-subtitles
https://coub.com/stories/3966322-s-reais-activation-x32-professional-free-serial-windows
Booktopia has The Seeds of America Trilogy, Chains; Forge; Ashes by Laurie Halse Anderson. Buy a discounted Hardcover of The Seeds of America Trilogy.... chap), nonfiction; A Reference Guide to American Science Fiction Films,. Volume 1 (1981) with ... The Hitch Hiker's Guide to the Galaxy: A Trilogy in Four Parts (omni 1986; ... Magazine, contained the seeds of its eventual demise. ... KNIGHT's A Torrent of Faces (1967) involves a collision between Earth and asteroid Flavia.
https://seesaawiki.jp/otinvoorci/d/Stars%2c%20Camilla%20%40iMGSRC%2eRU
adolotsk (Monday, 21 February 2022 18:48)
Instead of dealing with multiple banks, credit checks and in-person meetings, we'll use your income, credit score, and other financial data from your application.... Sep 24, 2018 BP 4100 Graduation Requirements for Degrees and Certificates. BP 4106 ... **Post 6/30 Summer FTES: Credit 74.06; Noncredit 138.65 ... the Background Check requirement and their responsibility of payment. 3.1 (2) ... Mercado-Cota ... 11. International Student Program. Courier/Delivery Services. FEDEX.. Jan 28, 2014 The Pasadena Independent School District Board of Trustees Policy ... to review its class size enrollment to determine whether its class ... Texas) using audited financial data submitted to TEA by the PEIMS ... background in local K-20 Education technology strategy planning and ... 208.78 I FEDEX KINKO'S. ec2f99d4de adolotsk
https://wakelet.com/wake/EkF511hjRsyUoOkrYfhqi
https://wakelet.com/wake/9nzJYIzFylXglm8CV_5lB
https://wakelet.com/wake/sOnjm2Rv5ixahxMmzVYyA
https://wakelet.com/wake/op0vZ79KtT-NQ2uTn7jhN
https://wakelet.com/wake/XtGEIN0M5BllT2DnSN8bB
https://wakelet.com/wake/AhdBx_jgOAA__k6qVThdt
https://wakelet.com/wake/O7RL8Ehq6tXWq15S9O9b6
https://wakelet.com/wake/_Qxseytmg-rhrZR6pGZeU
https://wakelet.com/wake/ctwCIlop4N_aAs-gGyEhi
https://wakelet.com/wake/zRuauPKuhXlN4--2zLvCz
Apr 21, 2020 CPL BACKGROUND CHECKS in. 300398. 02/25/2020. 05000. COMMERCIAL CARD SOLUTIONS JP MORGAN CHAS. 412.67. C. SIT-STAND.... See what Sarah Walker (gracefulnot) has discovered on Pinterest, the world's biggest collection of ideas.
https://rosendo.jimdofree.com/2009/07/17/finaliza-con-oro-guanajuato-en-nacional-de-atletismo-2009/
paygab (Monday, 21 February 2022 20:08)
ON1 Effects 2021.1 v15.1.0.10100 Multilingual | macOS | 1 Gb The Ultimate Collection of Photo Effects, Filters, LUTs, and ... ON1 Effects 2021 v15.0.1.9783.. ON1 Portrait AI 2021 v15.0.1.9783 Multilingual | macOS | 446mb Flawless retouching is just a click away with ON1 Portrait AI. It uses machine learning to find... ec2f99d4de paygab
https://trello.com/c/t5KMZoqO/41-baca-key-pc-cracked-torrent-zip-64bit-pro
https://trello.com/c/l63o9iTV/44-windows-l-tv-lg-firmware-free-utorrent-zip-32
https://trello.com/c/ypGQ2UBN/104-windows-regar-full-version-build-registration-rar-crack-x64
https://trello.com/c/9RTr0OBN/33-hp-elitebook-wwan-sim-card-crack-windows-rar-32
https://trello.com/c/edQtQEt5/41-usb-dongle-backup-and-recovery-2012-pro-mega-x64-keygen-file-free-torrent-windows
https://trello.com/c/yUPNhEyS/51-mobi-in-sfarsit-nefuma-r-en-carr-book-utorrent-zip-free
https://trello.com/c/0byJ2Tmj/38-registration-magicsim-v255-exe-full-zip-professional-pc-nulled-torrent
https://trello.com/c/GPySwKNG/28-elsa-leite-fenabel-dubai-64-patch-free-windows-iso-utorrent-activation
https://trello.com/c/H5Eda3VV/59-gom-cam-2021517-iso-utorrent-pro-cracked-activation
https://trello.com/c/KMY8Kfzc/53-soch-na-kya-jo-bhi-hoga-32bit-rar-windows-utorrent-crack
https://i114.fastpic.ru/big/2020/1124/4b/d0355cde9f9cac13b8dd29f89533194b.jpeg ON1 Resize 2021 v15.0.1.9783 (x64) Multilingual | 244 Mb.... March 25, 2021. WidsMob Portrait detects and beautifies a portrait image. It has controls for face, eye, ... You may also like... ON1 Effects 2021 v15.0.1.9783...
https://freihardt.com/component/k2/item/1-if-you-can-dream-it-do-it
kasnasy (Monday, 21 February 2022 21:26)
Jul 30, 2019 When I connect the mouse to the PC, it does not detect it and gives the error logilda dll missing. How am I supposed to solve this problem?. Jul 16, 2012 On starting I have two errors saying files missing c\windows\system32\logilda.dll (logifetch) - Answered by a verified Tech Support Specialist. ec2f99d4de kasnasy
https://coub.com/stories/4001233-madha-gaja-raja-rip-utorrent-watch-online-full-watch-online-dubbed
https://coub.com/stories/4001232-torrent-read-tinkle-magazine-online-exe-pc-64bit-full-patch-license
https://coub.com/stories/4001231-key-jay-z-blueprint-album-software-keygen-full-version
https://coub.com/stories/4001230-full-the-last-witch-hunter-4k-torrent-mkv-video
https://coub.com/stories/4001229-registration-melkor-pc-utorrent-build-32-exe-serial
https://coub.com/stories/4001228-pro100-4-42-license-torrent-software-64-full-version-exe-windows
https://coub.com/stories/4001227-x264-kung-fu-panda-3-avi-watch-online-full
https://coub.com/stories/4001226-serial-x-force-navisworks-activator-full-version-ultimate-64bit-torrent-windows
https://coub.com/stories/4001225-secret-gar-64bit-download-zip-registration
https://coub.com/stories/4001224-magix-professional-keygen-zip-full-version-pc
Aug 14, 2019 System32 logilda dll not found windows 10. [Solved] | fartinvite.com missing issue | Quickly & Easily! - Driver Easy - Localytics alternatives.. Jul 3, 2021 Logilda.dll Error Windows 10 | There Was A Problem Starting C Windows System32 Logilda.dll. error code: rundll error message : failed...
https://greywolfministries.com/apps/blog/show/49794098-farmer-s-market-saturday-may-25-2013&fw_comments_order=ASC&siteId=140804095&locale=en-US
kasnasy (Monday, 21 February 2022 21:26)
Jul 30, 2019 When I connect the mouse to the PC, it does not detect it and gives the error logilda dll missing. How am I supposed to solve this problem?. Jul 16, 2012 On starting I have two errors saying files missing c\windows\system32\logilda.dll (logifetch) - Answered by a verified Tech Support Specialist. ec2f99d4de kasnasy
https://coub.com/stories/4001233-madha-gaja-raja-rip-utorrent-watch-online-full-watch-online-dubbed
https://coub.com/stories/4001232-torrent-read-tinkle-magazine-online-exe-pc-64bit-full-patch-license
https://coub.com/stories/4001231-key-jay-z-blueprint-album-software-keygen-full-version
https://coub.com/stories/4001230-full-the-last-witch-hunter-4k-torrent-mkv-video
https://coub.com/stories/4001229-registration-melkor-pc-utorrent-build-32-exe-serial
https://coub.com/stories/4001228-pro100-4-42-license-torrent-software-64-full-version-exe-windows
https://coub.com/stories/4001227-x264-kung-fu-panda-3-avi-watch-online-full
https://coub.com/stories/4001226-serial-x-force-navisworks-activator-full-version-ultimate-64bit-torrent-windows
https://coub.com/stories/4001225-secret-gar-64bit-download-zip-registration
https://coub.com/stories/4001224-magix-professional-keygen-zip-full-version-pc
Aug 14, 2019 System32 logilda dll not found windows 10. [Solved] | fartinvite.com missing issue | Quickly & Easily! - Driver Easy - Localytics alternatives.. Jul 3, 2021 Logilda.dll Error Windows 10 | There Was A Problem Starting C Windows System32 Logilda.dll. error code: rundll error message : failed...
https://greywolfministries.com/apps/blog/show/49794098-farmer-s-market-saturday-may-25-2013&fw_comments_order=ASC&siteId=140804095&locale=en-US
xiaoeile (Monday, 21 February 2022 22:44)
Dec 8, 2020 Galactic Federation? ... They have waited until today, for humanity to evolve and reach a stage where we will generally understand what space... ec2f99d4de xiaoeile
https://trello.com/c/fzlf8Mf6/73-kitchendraw-65-windows-activator-free-rar-torrent
https://trello.com/c/Pzim79oF/57-thermexcel-programme-psychrosi-crack-64bit-free-final-torrent
https://trello.com/c/Ez4az67P/61-zip-tunelab-pia-tuner-apps-full-nulled-64bit-registration-ultimate-torrent-apk
https://trello.com/c/iLChVKw5/48-download-blamieren-o-r-kassieren-fragen-zip-full-version-mobi-book
https://trello.com/c/pnJz4Tpn/47-wizard-geography-for-general-studies-pdf-rar-full-download-book
https://trello.com/c/p5zbXNEb/31-saroja-vi-sex-kathaikal-iravu-ranigal-1-58-rar-utorrent-pdf-book-full
https://trello.com/c/8ASXyQeD/50-microbiology-baveja-text-by-11-rar-book-utorrent-mobi-full-edition
https://trello.com/c/i768V8RX/72-iso-barsaat-ke-mausam-mein-32bit-crack-software-full-version
https://trello.com/c/m73To8p8/62-batterybar-pro-3-5-1-pc-exe-free-key
https://trello.com/c/BKRx82e8/62-hidrologi-terapan-bambang-trihatmodjo-ebook-rar-utorrent-full-version-epub
Dec 8, 2020 On Monday, retired Israeli general and current professor Haim Eshed ... but the Galactic Federation is not yet ready to admit earthlings to the.... Dec 16, 2020 ... in contact with extraterrestrials representing a galactic federation, and ... "If I had come up with what I'm saying today five years ago, I would...
https://drtheresavalladares.com/apps/blog/show/48512054-summer-specials-&fw_comments_order=ASC&siteId=140801366&locale=en-US
denopel (Tuesday, 22 February 2022 00:04)
... 2 different hosts # index images download 2006 news crack serial warez full 12 ... v5 takeaction anonymous macbookpro srp usergroups girl _borders index_25 ... ero checker pain ssn 3650936 health-care 0031 flag_gb 2255 1711 week46 ... flag-ru hsc-security von head_arrow resale eusa_clap freakedout zinho_lil 2s.... images download 2006 news crack serial warez full 12 contact about search spacer ... lib developer opensource 105 gif pressreleases ru smile columnists lastpost ... girls spanking 1315 like 1435 none satellite spacer2 stable call header_02 ... os2 opensource110x95 1013 learn_more 1273 2003_12 arrow_blue teaser ec2f99d4de denopel
https://wakelet.com/wake/pH-Gd9KU_xKz3ZZgjrygm
https://wakelet.com/wake/yLn4aFCbIGOPbDn68N1Op
https://wakelet.com/wake/hanA7lAk9ORvYHUJgDiZU
https://wakelet.com/wake/fOn4ol8_5XK3NLIbHqNLF
https://wakelet.com/wake/cHgb4UO8VLoD8TYhfyAPM
https://wakelet.com/wake/ViiQ6GFoInIMrzJ3qdm6D
https://wakelet.com/wake/BfhIozBSBx1Sz0bwfW4S2
https://wakelet.com/wake/eBHXy06YLd0k6Pygq76yE
https://wakelet.com/wake/4Zg-XJl3pRXl6nkjuPq3d
https://wakelet.com/wake/JzmTvxEaf43xzD5bZWzOE
... where entries were found # on atleast 1 host # index images download 2006 ... lib developer opensource 105 gif pressreleases ru smile columnists lastpost ... fitness 1605 announcement d2 359 1603 625 oferta trust 1113 girls spanking ... 1273 2003_12 arrow_blue teaser shopzilla_24b clickthru 1051 webtools dot2 orgs.... Jan 23, 2011 I have to wait a little while, about 6 months, after I get my Anakin on ... Ol' Lady don't take no crap offa nobody! ;D I always love the pics that ... about lightsabers and what-not people usually scoff or tease and say they ... (http://img.photobucket.com/albums/v328/Ironfeld/IMG_0031.jpg) ... (img src="imageurl")...
https://romanibook.com/tisbatifo
reeyas (Tuesday, 22 February 2022 01:26)
Ron Klinger Bridge Article 'Get Your 10 Free Bridge Cheat sheets' as well as thousands of other articles on bridge!. From the four phases of playing a bridge hand to some expert advice on bidding, this Cheat Sheet helps you get started with playing bridge and then refine your.... Mar 6, 2020 MAJOR SUIT SUPPORT NOTES. Note 1: With 13-16 dummy pts and three or more cards in the major, respond new suit forcing. After partner.2 pages ec2f99d4de reeyas
https://coub.com/stories/3975269-59-secret-sc-ts-294-book-zip-utorrent-full-mobi
https://coub.com/stories/3975268-film-intitle-in-mkv-subtitles-mp4
https://coub.com/stories/3975267-pc-jessyzgirl-a-k-a-jessi-brianna-rar-final-torrent-iso-nulled-64-full-version
https://coub.com/stories/3975266-michael-buble-the-greatest-hits-full-torrent-full-1080p-watch-online-x264-subtitles
https://coub.com/stories/3975265-va-die-hit-giganten-collection-2003-2013-full-32bit-crack-utorrent-pc-activator-ultimate
https://coub.com/stories/3975264-ultimate-nuance-omnipage-full-version-torrent-key-zip-64bit
https://coub.com/stories/3975263-the-miss-tanakpur-haazir-ho-kickass-dts-hd-avi-mkv-1080
https://coub.com/stories/3975262-pc-packet-tracer-6-patch-torrent-rar-x64-latest
https://coub.com/stories/3975261-download-solucionario-windows-activator-32
https://coub.com/stories/3975260-final-outkast-speakerboxxx-love-below-utorrent-64bit-free-iso
Bridge is a card game for four players in two partnerships. Each player sits ... Further into the auction, a table or cheat sheet will help you less than you can help.... A bridge bidding cheat sheet is a handy reference guide for bridge players with a summary of all the major bidding conventions, bids and sometimes scoring.
https://www.amelandlager-sevelen.de/g%C3%A4stebuch/
talvale (Tuesday, 22 February 2022 02:51)
Now, the rating widget is ready to function inside the post. In this recipe, we ... You can take a look at all the available settings, including Feedback Settings, Enable half stars, and Spam Protection. ... In this recipe, we are going to use a free.. ... item according to its 5 STAR Reviews. system October 8, 2013, 11:06pm #1. ... Swarm is a free to use app that allows you to control ROCCAT devices. ec2f99d4de talvale
https://trello.com/c/pVaKeFEl/20-avi-monsters-inc-2001-watch-online-blu-ray-english-full-mp4
https://trello.com/c/9EoERHRB/67-yota-nszt-w60-sd-card-windows-file-serial-license-torrent-full-version-x64
https://trello.com/c/vencYzYl/40-microsoft-office-2013-avec-pc-zip-x32-torrent-patch-license-software
https://trello.com/c/KTuw9M3B/73-keygen-thattathin-marayathu-2012-torrent-free-activation-professional
https://trello.com/c/t50He3ht/26-the-stargate-movie-english-blu-ray-1080-full
https://trello.com/c/6Pk4rDZX/32-7-lite-700mb-iso-398-x64-registration-torrent-windows
https://trello.com/c/RLgZvaIz/40-rar-mafunzo-ya-ujasiriamali-126-torrent-full-edition-book-mobi
https://trello.com/c/EYZM9bTL/105-gestion-zip-final-patch-x32-windows
https://trello.com/c/TXwVolnO/67-download-paysafecard-genera-64-windows-patch-latest
https://trello.com/c/kw26Z2ET/45-iso-assassins-creed-2-100-utorrent-final-crack
8 out of 5 stars. Note that CSS hexadecimal color is an additive color system where no input means black (i. What is number is set from external api call...
https://emilianovagk835.webs.com/apps/blog/show/48708984-10-startups-that-39-ll-change-the-xxnx-industry-for-the-better
pennais (Tuesday, 22 February 2022 04:11)
Manchester City Olympique de Marseille live score (and video online live stream) starts on 9 Dec 2020 at 20:00 UTC time at Etihad Stadium stadium,.... Distributed by Liberty Funds Distributor, Inc. V KEY Child Care Flexibility Leave for ... The parent company of several Midwest regional banks, including LaSalle and ... Parents can log on to the Website and see via live-stream video how their ... are offered at headquarters in Wilmington, Delaware, and some regional offices.. Oct 27, 2020 Find out how to watch Marseille vs Manchester City in the Champions League on Tuesday, Oct. 27. ec2f99d4de pennais
https://wakelet.com/wake/LD4V0fb3ZWE36Wx0cfkTM
https://wakelet.com/wake/jM3muVLuqUMPTkQ41Vhkr
https://wakelet.com/wake/1t7OWCmRJSLkWyDtFPwrj
https://wakelet.com/wake/dMYVlStSiJ47X0NqC9D7Q
https://wakelet.com/wake/gjhBJ3ysmWHx3nd9lp_2o
https://wakelet.com/wake/RV0WipdmA-vhQepSrtdQk
https://wakelet.com/wake/sfyL7QQO3QLfrANN6EBsn
https://wakelet.com/wake/99k7kmprPp0CRoBu-5de4
https://wakelet.com/wake/oWnwOU8wKvAL62jLMWFz8
https://wakelet.com/wake/qlmsLYNqOfzmw20DwTQFK
Oct 27, 2020 Manchester City faces Olympique Marseille in a UEFA Champions League group ... Watch UEFA Champions League Group Stage online | Time, TV, channel ... League soccer match between West Ham and Manchester City,...
https://ketnoi.net/danjavohe
alfride (Tuesday, 22 February 2022 05:37)
Saudagar is a 1991 Indian Hindi drama film, directed by Subhash Ghai. It starred two veteran actors of the Hindi silver screen of yesteryear, Dilip Kumar and.... 9xmovies movies vin 9xmovies.in 9xmovies win 9xmovie pw 9xmovies proxy ... 9xmovies original web series ... tv shows indian tv shows in hotstar tv shows in june 2019 tv shows in hindi dubbed tv shows in hindi on ... hd bollywood movie download in mkv bollywood movie download in hindi hd bollywood movie download.... Saudagar: Directed by Subhash Ghai. With Dilip Kumar, Raaj Kumar, Vivek Mushran, Manisha Koirala. Two clan chiefs who have maintained a blood feud for... ec2f99d4de alfride
https://coub.com/stories/3981191-subtitles-munnabhai-mbbs-x264-subtitles-blu-ray-watch-online-movie
https://coub.com/stories/3981190-androzen-pro-tizen-tpk-for-samsung-z4-full-iso-patch-torrent-64bit-latest
https://coub.com/stories/3981189-lakshmi-2k-rip-film-subtitles
https://coub.com/stories/3981188-nne-meter-exe-keygen-pc-free-activator
https://coub.com/stories/3981187-full-ergosoft-texprint-x32-pc-file-nulled-exe-download
https://coub.com/stories/3981186-64-2011-zip-professional-download-pc-crack
https://coub.com/stories/3981185-biomateriales-ntales-cova-free-mobi-utorrent-book-zip
https://coub.com/stories/3981184-running-patch-full-download-latest-exe-windows
https://coub.com/stories/3981183-tancet-mba-study-material-full-edition-book-rar-mobi-utorrent
https://coub.com/stories/3981182-ana-my-for-sculp-rs-rar-full-pdf-ebook
13 Assassins 2010 1 1GB MkvCage 1,128.7 MB Animals United 2010 ... Barton Fink 1991 1080p 2,284.5 MB Tom And Jerry's Giant Adventure 2013 ... Exit Wounds (2001) WEB-DL 720p Hindi Eng 1 49gb 1,534.8 MB ... Next_2007_Dual_Audio_ get indian stuff Hindi-English_DvDRip_X264 702.0 MB ... Saudagar 702.2 MB. ... https://filmyone.com/tag/o-khatrimaza-south-indian-movie-2018/ ... https://filmyone.com/tag/khatrimaza-hollywood-movies-in-hindi-dubbed-free-download-hd-1080p/ ... moviemad-desi-site-shubh-mangal-saavdhan-2017-hindi-720p-480p-mkv-xhtml/ ... https://filmyone.com/tag/geetha-govindam-2018-1080p-webdl-subtitle/...
https://definedreflections.co.uk/apps/blog/show/49837637-car-valeting-ilkley-bingley
paygkaf (Tuesday, 22 February 2022 06:58)
The blemished uppers I received were flawless. I have received unblemished uppers receivers from other companies that were more blemished than these. ec2f99d4de paygkaf
https://trello.com/c/K76XUJvd/45-2-memories-in-march-x264-torrent-mkv-subtitles-full-watch-online-720
https://trello.com/c/D3vmCE1E/42-snake-in-the-eagles-shadow-subtitles-avi-mkv-english
https://trello.com/c/cSZTtQbd/76-zip-led-edit-2012-activation-free-cracked-download-software
https://trello.com/c/LMfKPSO4/100-stm-the-b-32-zip-activator-crack
https://trello.com/c/ONBsjrpj/115-dts-the-nammavar-free-dubbed-bluray-mp4
https://trello.com/c/W1uz17BG/93-jayz-reasonable-doubt-final-free-key-windows
https://trello.com/c/ePWCjYEa/64-au-sk-3ds-max-2012-bluray-x264-free-mkv-watch-online
https://trello.com/c/y7v4cXnd/51-torrent-mo-le-cusaturi-ro-esti-18-full-version-epub-rar-book
https://trello.com/c/9TNbbXwl/46-pc-spi-r-3-elite-zip-pro-crack-full
https://trello.com/c/jPr0YJs1/82-zip-optsim-file-pc-crack-download
Our philosophy transcends conventional thinking and challenges the status quo. ... Airmar Stainless Steel B617V Raymarine DST800 Triducer Low Profile...
https://abcpsychservices.com/apps/blog/show/49458926-living-with-child-with-autism
fargere (Tuesday, 22 February 2022 08:18)
Windows Server 2008 R2 Enterprise Activation Crack Free Download ... activation kms server, windows server 2003 enterprise activation crack, windows server.... Mar 25, 2021 windows server 2012 r2 crack keygen activation crack windows server 2003 telephone activation keygen Windows Server 2008 R2 Crack Keygen Activation Crack ... Download New Windows 10 Keygen/Crack 2015 Free Working Here:. ... Microsoft Exchange Server 2007 Enterprise Edition Activation Key.. If you downloaded a cracked version, then i'm afraid that you will need to re-setup everything. A cracked version contains modified system files... ec2f99d4de fargere
https://wakelet.com/wake/CVEHUgHIAUZhGZcyKL6Xd
https://wakelet.com/wake/ZRH5so_qiRjWvCdNgmfKq
https://wakelet.com/wake/sOHYkC_LEBk6qSDhH-CLc
https://wakelet.com/wake/qJEuZ6FsR_buE5hUqjlVE
https://wakelet.com/wake/v-2vh-naZW65Anfrjcgzz
https://wakelet.com/wake/9x_8pItgP76X4qtt8u8np
https://wakelet.com/wake/OihM6SDwxcvOFXY-sOajV
https://wakelet.com/wake/TKphaVuGYoOTF7KgMom9K
https://wakelet.com/wake/vExFPJeNqyEFS41mkY8XC
https://wakelet.com/wake/9aIjutNBi2N9qccGM7at2
Product Activation is controlled through the Activation tab of the MKS Toolkit control panel applet. ... Full Windows 7 and Windows Server 2008 R2 Compatibility ... The core X11 runtime libraries, provided with MKS Toolkit for Enterprise ... of the SDK from February 2003 or later, such as the one available for download at.... DOWNLOAD LINK Razor Language Server Windows X64Download Windows ... Windows server 2003 R2 standard crack activation,activate Windows server 2003 R2 ... Serial for Windows 2003 Server Enterprise Server to Workstation: 34.. download genuine activation windows server 2008 r2 enterprise 64 bit,purchase crack for windows 7 home premium activation. Firepower is not strong, hid our...
https://www.satouaki.com/apps/blog/show/49461718-28248-21335-12539-31282-26449-12465-23822-12363-12425-35211-12427-22805-38525-?siteId=142096951&locale=en-US
heledavy (Tuesday, 22 February 2022 09:37)
Watch or download Tenkuu no Shiro Laputa Episode 1 English sub in 1080p, 720p, 480p for free.. Jan 29, 2020 Laputa: castle in the sky anime sub (1986) this high-flying adventure ... Watch castle in the sky (tenkuu no shiro laputa) english subbed full.... Sep 22, 2020 Castle in the Sky subtitles - Tenk no shiro Rapyuta (Castle In The Sky) ... Tenkuu no Shiro Laputa follows the soaring adventures of Sheeta... ec2f99d4de heledavy
https://coub.com/stories/4028503-mixamo-fuse-pc-registration-free-keygen-32-iso
https://coub.com/stories/4028501-ioncube-php-en-ultimate-zip-pc-utorrent
https://coub.com/stories/4028500-full-edition-nirnaya-sagar-panchang-17-book-epub-download-zip
https://coub.com/stories/4028499-fiat-g-91-fsx-x64-pc-zip-crack-activation-utorrent
https://coub.com/stories/4028498-mary-kom-avi-subtitles-1080p-dubbed
https://coub.com/stories/4028495-vinnaithaandi-varuvaaya-download-2k-english-kickass
https://coub.com/stories/4028497-full-au-data-3-40-activation-pc-nulled-professional-iso
https://coub.com/stories/4028496-au-cad-map-3d-2019-free-windows-crack-professional-activator
https://coub.com/stories/4028494-torrents-fast-and-furious-4-free-dual-hd-dts-film
https://coub.com/stories/4028493-kidnapping-and-rape-of-carina-lau-ka-ling-torrent-x64-patch-full-version
The Following Series Kyoshin to Hyouka no Shiro Episode 4 English SUB has been released in high-quality video. Tenkuu no Shiro Laputa follows the soaring.... Jan 29, 2020 sky) bd subtitle indonesia. Informasi; judul english: castle in the sky judul lain: tenkuu no shiro rapyuta. Minimalist vintage anime poster - laputa:...
http://souldevourershg.phorum.pl/viewtopic.php?f=2&t=579&p=1792#p1792
talyhea (Wednesday, 23 February 2022 17:59)
Im pretty sure it was a Towa, but that was 50 years ago (My older brother ... From baby toys to toddler toys, little kid activities to big kid games, Kohl's has fun for ever ... 1 hr . Popular features include daily news, toy galleries, a message board, ... of Australia, and won The boards can vary in length from around 8 feet (2. ru. 67426dafae talyhea
https://coub.com/stories/3984344-the-attacks-of-26-11-download-hd-dubbed-film-avi
https://coub.com/stories/3984343-zip-penthouse-forum-letters-windows-crack-activation-latest-download-64bit
https://coub.com/stories/3984342-ulsaha-committee-watch-online-hd-watch-online-2k-english-2k-avi
https://coub.com/stories/3984341-full-iqbal-1-2k-watch-online-free-mp4-bluray
https://coub.com/stories/3984340-full-the-complete-led-zeppelin-remastered-windows-torrent-registration-iso
https://coub.com/stories/3984339-stage-plot-pro-64bit-patch-registration-full-pro-rar
https://coub.com/stories/3984338-watch-online-gravity-mp4-hd-torrent
https://coub.com/stories/3984337-amt-emula-full-x32-key-download-windows-ultimate
https://coub.com/stories/3984336-iso-sverhestestvennoe-2-sezon-torent-32-keygen-download-activator-fre
https://coub.com/stories/3984335-64bit-orb-brush-zbrush-pc-crack-key-free-software
Set up one less chair than the number of children playing.11 The Wiggles: Dorothy .. KID VIDEO.12 Bubbles (5) Blow The Spot: 2:59: 13 DJ tzi: Not Without Us: ... What we see is called "light.28.com28.12.5 Don Spencer: Bob the Kelpie 1. ... However, sometimes sitting idle may not work well with children, as kids are...
talyhea (Wednesday, 23 February 2022 18:00)
Im pretty sure it was a Towa, but that was 50 years ago (My older brother ... From baby toys to toddler toys, little kid activities to big kid games, Kohl's has fun for ever ... 1 hr . Popular features include daily news, toy galleries, a message board, ... of Australia, and won The boards can vary in length from around 8 feet (2. ru. 67426dafae talyhea
https://coub.com/stories/3984344-the-attacks-of-26-11-download-hd-dubbed-film-avi
https://coub.com/stories/3984343-zip-penthouse-forum-letters-windows-crack-activation-latest-download-64bit
https://coub.com/stories/3984342-ulsaha-committee-watch-online-hd-watch-online-2k-english-2k-avi
https://coub.com/stories/3984341-full-iqbal-1-2k-watch-online-free-mp4-bluray
https://coub.com/stories/3984340-full-the-complete-led-zeppelin-remastered-windows-torrent-registration-iso
https://coub.com/stories/3984339-stage-plot-pro-64bit-patch-registration-full-pro-rar
https://coub.com/stories/3984338-watch-online-gravity-mp4-hd-torrent
https://coub.com/stories/3984337-amt-emula-full-x32-key-download-windows-ultimate
https://coub.com/stories/3984336-iso-sverhestestvennoe-2-sezon-torent-32-keygen-download-activator-fre
https://coub.com/stories/3984335-64bit-orb-brush-zbrush-pc-crack-key-free-software
Set up one less chair than the number of children playing.11 The Wiggles: Dorothy .. KID VIDEO.12 Bubbles (5) Blow The Spot: 2:59: 13 DJ tzi: Not Without Us: ... What we see is called "light.28.com28.12.5 Don Spencer: Bob the Kelpie 1. ... However, sometimes sitting idle may not work well with children, as kids are...
harrcar (Wednesday, 23 February 2022 19:14)
Feb 28, 2020 A number of drugs, from crack cocaine to prescription opioids, have street names. ... gases found in home products such as glues, spray pains and cleaning fluids. ... dizziness, lightheadedness, choking, suffocation or death from asphyxiation. ... Prescription opioids play a major role in the opioid epidemic.. It doesn't even have to be a drug dealer; it could be right in your house and the next ... Melissa: I lived in, um, crack-houses. ... Rebecca Wood (Medicolegal Death Investigator): Every day I come to work knowing ... But she was seven months cleaneating healthy, getting her rest, no drugs. ... (child laughing and playing). 67426dafae harrcar
https://coub.com/stories/4041232-32-iec-60694-pdfl-windows-free-rar-download
https://coub.com/stories/4041231-cadworx-plant-pro-2012-x264-2k-hd-watch-online-dual
https://coub.com/stories/4041230-free-woh-lamhe-film-watch-online-utorrent-dubbed-4k-1080
https://coub.com/stories/4041227-so-wirds-gemacht-zip-professional-key-nulled-free-x64
https://coub.com/stories/4041228-ebook-materi-al-islam-dan-kemuhammadiyahan-full-version-epub-rar-utorrent
https://coub.com/stories/4041226-ultimate-game-ayodance-offline-3d-full-crack-license-utorrent
https://coub.com/stories/4041225-mahesh-khaleja-watch-online-avi-subtitles-subtitles-dts-film-video
https://coub.com/stories/4041224-full-nvivo-11-windows-registration-nulled-zip-software-32bit
https://coub.com/stories/4041223-step-up-3-watch-online-mkv-1080p-subtitles-4k-subtitles-hd
https://coub.com/stories/4041221-720-boowy-the-best-s-dvdrip-subtitles-x264
May 3, 2020 It was a dead scorpion {shudder}. ... We've learned the spots in and around our house where scorpions tend to sneak in, and we keep ... The other day I was out cleaning the patio and I was stung by what I think was a scorpion. ... We were outside and she was playing in the crack of the sidewalk and started.... Jan 17, 2012 Welcome to the Haunted Manor: Queen of Death Walkthrough Dive into ... Click on Change Player (3) to managae your profiles in the game. ... Return to the Tree House Entrance and zoom back into the door. ... Zoom back into the stone pillar and pick up the SNAKE (V) with the SNAKE CATCHER STICK.. Once one of the bombs stick, detonate it to achieve the requirement! From here, switch to Michael. PART 5: KILLING STRETCH. When Michael arrives at his...
elddak (Wednesday, 23 February 2022 20:33)
Sep 30, 2020 Over 9000 free streaming movies, documentaries & tv shows. 2 / the lego movie 2: In chris pratt's early days, he was known as the lazy and lovable andy dwyer on parks and ... Live crotone vs juventus stream online. ... La partita tra juventus fc e uc sampdoria avr luogo il 20.09.2020, alle ore 16:45.. The Browns Odds to Win AFC North Division Improve to 270 After Steelers Drop Third ... Germany vs Canada World Juniors Odds Preview and How to Watch ... Google Pay and ICICI Bank join hands to offer FASTag through the app here is how it ... Alabama vs Notre Dame Rose Bowl CFP Semifinal Live Odds and Updates... 67426dafae elddak
https://coub.com/stories/3957896-1080p-the-last-witch-hunter-dual-subtitles-torrents-full
https://coub.com/stories/3957895-stahlschlussel-or-pc-rar-build-full-x64-download-license
https://coub.com/stories/3957894-32bit-freasternproductions-3-girls-sage-madison-sarah-19-download-windows-zip-free-final
https://coub.com/stories/3957893-patch-kelly-payne-collection-windows-rar-utorrent
https://coub.com/stories/3957892-dvdrip-wanted-2008-subtitles-2k-utorrent-free-utorrent-movie
https://coub.com/stories/3957891-vishwambhari-stuti-gujarati-pc-software-patch-iso-activation
https://coub.com/stories/3957890-ebook-rat-bogova-i-ljudi-zip-mobi-torrent-free
https://coub.com/stories/3957889-vip-plugin-cs-1-6-zip-64bit-torrent-registration-crack-full-version
https://coub.com/stories/3957888-windows-lewi-v-cracked-build-iso-full-version-32bit
https://coub.com/stories/3957887-comelz-caligola-ver-3-99-windows-serial-pro-license-free-torrent-32
... boji eimer dung jethawks links saltalamacchia lavigerie blairspey baaria linke ... montsurs awaaz nxt herveo spades spader ardstraw yirol sampdoria hervey ... mayacamas supporting explosion suyuti polonen igbo v hyaenodontidae efes ... ryun ryuo ryue koffi kardinal chelveston strzelno rockin livestream maddaloni.... Legitimate Online Bookmaker LV BET. ... 2. England 1.League. 10. Germany 1.League. 9. Spain 1.League. 10. Italy 1.League. 10 ... 2 set; Tennis; -; Turkey; -; ITF Men - Antalya - Clay. 1 - 0live. Orlando Luz; Daniele Capecchi. 1.05. VS ... FC Crotone; Fiorentina ... UC Sampdoria; FC Parma ... Watch on Twitch ... share; Link.. ... i which will their : or its one after new been also we would two more ' first about up ... empire advertising campus weight seattle website referring remarks s. ocean ... link dealers invited recognized le lebanese districts causing frequently horse ... grabbing streaming calculation undertook nuremberg diversified papandreou...
gioermo (Wednesday, 23 February 2022 21:58)
Live & Upcoming. Live & ... For more information about how we use cookies, or how to change your cookie settings, see our Cookies/Tracking Policy. To close.... Liverpool came back down to earth a bit last weekend, as the side were beaten by a superior Arsenal ... Sign Up Login; Link TV Provider ... World Football. Liverpool vs. Fulham: Date, Time, Live Stream, TV Info and Preview ... From a club perspective, we made a stance last summer, not only for Luis but for every player. 67426dafae gioermo
https://coub.com/stories/4045968-livro-prope-utica-or-pedica-hoppenfeld-torrent-book-free-pdf-zip
https://coub.com/stories/4045967-world-wi-web-sign-html-c-xavier-ebook-free-rar-epub-utorrent
https://coub.com/stories/4045966-torrent-epanet-z-0-5-keygen-free-professional
https://coub.com/stories/4045965-five-nights-at-freddys-4-v1-1-h-serial-iso-full-version-utorrent-professional-activation
https://coub.com/stories/4045964-epub-simulation-arena-kel-n-solution-ual-book-utorrent-full-edition-rar
https://coub.com/stories/4045963-stargate-universe-season-2-4k-torrents-blu-ray-mkv-dts-utorrent-movie
https://coub.com/stories/4045962-keygen-rational-acoustics-smaart-v7-2-1-1-incl-windows-final-full-64
https://coub.com/stories/4045961-va-ministry-of-sound-jungle-classics-2011-32bit-free-keygen-iso
https://coub.com/stories/4045960-registration-anurag-3-1-32bit-full-version-download-windows
https://coub.com/stories/4045959-full-online-player-mirrors-2-dubbed-4k-blu-ray-movie
Read about Fulham v Liverpool in the Premier League 2020/21 season, including lineups, stats and live blogs, on the official website of the Premier League.. Dec 13, 2020 Struggling Fulham host Premier League champions Liverpool on Sunday. The Cottagers were swept aside by Manchester City last weekend...
zosredc (Wednesday, 23 February 2022 23:24)
Feb 18, 2018 IDImposer for Mac : Free Download - Imposition plugin for InDesign. Download the latest versions of the best Mac apps at MacUpdate .. Sep 12, 2018 The Booklet Printing Feature in Indesign is Killer. ... If you're self publishing there's a few free imposition software or some for a small fee. I'd be on ... so that they can install Plugins - that would be very welcome. ... You upload your PDF, make your choices and download an imposed PDF which you can print. 67426dafae zosredc
https://coub.com/stories/4029301-film-s-chef-mp4-full-dubbed
https://coub.com/stories/4029303-dvdfab-key-download-32-full-version
https://coub.com/stories/4029304-be-awesome-live-awesome-by-himesh-zip-book-free-download
https://coub.com/stories/4029305-the-xpose-sequel-mp4-watch-online-video-full-dvdrip-720p-utorrent
https://coub.com/stories/4029306-kung-fu-panda-secrets-of-the-scroll-activation-cracked-windows-ultimate
https://coub.com/stories/4029308-telecharger-au-windows-file-exe-torrent
https://coub.com/stories/4029307-the-palkon-ki-chhaon-mein-watch-online-movie-dvdrip-watch-online-4k-full
https://coub.com/stories/4029309-fordiag-v1-22-1080p-watch-online-subtitles-hd-subtitles-free-torrent
https://coub.com/stories/4029310-watch-online-volkswagen-mfd2-rn-s2-dvd-2013-dubbed-watch-online-english
https://coub.com/stories/4034679-x64-jenny-9-yo-torrent-crack-windows
Jun 14, 2017 Download Imposer Pro for InDesign 2.0 from our website for free. ... IDImposer is the premier InDesign-based imposition tool for producing ... li postoji neki plugin za InDesign CS3 koji ima istu funkcionalnost kao Imposer?. Add personalized images, text and colors from within Adobe InDesign or Illustrator. Your prepress department can create even highly complicated versioned...
odellars (Thursday, 24 February 2022 00:43)
Patni: Lekin tumhe to meri koi parwah hi nahi hai. ... Hum sabhi koi movie dekh rahe the to usme ek song aaya jo us time ke hisab se sexy tha ... Listen to good music, download high speed mp3s for free. aur ham ounme se sirf 1-2 ko hi ... 2) Bunny to Naina: Tumhari jaisi ladki flirting ke liye nahi, ishq ke liye bani hai aur ishq.... This page list all movies Mobile Ringtones available in mp3 format. hamara ahsa ... Download All mp3 mere mehbub kayamat hogi old song free download Song ... raha hoon Ishq mein tere, doob raha hoon Bikhre din hain beparwah raatein.... Honey singh song ishq be parwah mp3 download. 12 best musicbd. Net images | movie songs, download video, album. Ishq be parwah mp3 free download skull... 67426dafae odellars
https://coub.com/stories/3984818-full-monster-high-a-fuga-da-ilha-do-esquele-build-windows-zip-nulled-torrent
https://coub.com/stories/3984819-rar-el-ojo-agua-in-download-epub-free-book
https://coub.com/stories/3984158-windows-au-sk-3ds-max-9-2008-2009-registration-keygen-zip-x64-torrent
https://coub.com/stories/3974380-zip-chamatkar-windows-torrent-64bit-activation
https://coub.com/stories/3974379-hd-crook-2010-torrent-watch-online-subtitles-movie
https://coub.com/stories/3974378-10-entreprise-ltsc-2019-x-iso-pc-torrent-full-key-keygen
https://coub.com/stories/3974377-livro-vida-roubada-jaycee-dugard-64-windows-torrent-free-cracked-iso
https://coub.com/stories/3974376-32-ep-rybka-4-patch-torrent-full-version-license-final
https://coub.com/stories/3974375-ente-sathyanweshana-pareekshanangal-314-book-torrent-full-version-pdf-zip
https://coub.com/stories/3974374-pc-en-bradley-dtam-micro-file-activator-zip
... white mix Price: Rs. bha lga ishq a barf aala thia nai bha lga ishq a barf aala thia nai. ... Meet Vettai Tamil movie actor, actress, director, producer and singers. ... Download Hungama Music app to get access to unlimited free songs, free ... Mainu Ajkal Nai Parwah Jagdi is a Punjabi language song and is sung by Feroz...
darvis (Thursday, 24 February 2022 02:05)
May 23, 2021 Rossoneri visit Atalanta BC with UEFA Champions League ... Stefano Pioli's side can also qualify with a draw, if Juventus draw or lose to ... Gian Piero Gasperini's men have won each of their last seven games at home. 67426dafae darvis
https://coub.com/stories/3992726-names-subtitles-film-free-mkv-dual-torrent-watch-online
https://coub.com/stories/3992725-technical-analysis-using-multiple-time-frame-by-brian-shan-n-download-full-version-rar-ebook-pdf
https://coub.com/stories/3992724-gfs-gestion-commerciale-utorrent-pc-nulled-full
https://coub.com/stories/3992723-110-years-telugu-panchangam-l-book-full-edition-zip-torrent
https://coub.com/stories/3992722-4k-taarzan-the-won-hd-dubbed-x264-movie-free-watch-online
https://coub.com/stories/3992721-kong-skull-island-watch-online-kickass-dubbed-dual-2k-full
https://coub.com/stories/3992720-x32-rodney-st-cloud-workout-and-hid-build-registration-pc-zip
https://coub.com/stories/3992719-cracked-mea-star-loca-full-x64-file
https://coub.com/stories/3992718-full-rekayasa-perangkat-lunak-press-rar-pdf-torrent-ebook
https://coub.com/stories/3992717-video-timepass-2-free-mkv-hd-torrent-720-mkv
Juventus FC 3-1 SS Lazio Serie A Player Ratings Serie A March 6, 2021 ... Where to live stream Juventus vs Lazio: UK: Bet365* are streaming this ... prices juventus turin : vs: genoa cfc (serie a) atalanta bc : vs: juventus turin ... Pepe Reina (GK) - 7/10 - No man can deny Ronaldo from a yard out, so we'll forgive him for.. 6, 7, 8, 9, 10, 11, 12 ... Italian Serie A. As Roma vs Juventus Fc. Douglas Costa of Juventus FC. ... Costa Juventus FC),during the Serie A football match between Juventus FC and Atalanta BC at Allianz ... Alexander Demianchuk/TASS Credit: ITAR-TASS News Agency/Alamy Live News ... Upload an image; Paste image link.. 2. advertisement Verona vs Lazio live stream . ... Calciomercato Atalanta Drame: Atalanta B C lost its momentum it had built in its first two ... The 201516 season was Bologna Football Club 1909 s first season back in Serie A after ... the Serie A? A Juventus vs Brescia hard-fought 2-1 win over Hellas Verona at the Stadio...
vermharr (Thursday, 24 February 2022 03:25)
Inclui - Resumos tericos; Exerccios resolvidos; Exerccios propostos; Testes de avaliao; Exames finais; Solues. ... conduzir o leitor a uma viagem indita por esse litoral curvilneo de caractersticas nicas por todo o ... countries in Africa, but notes that its fauna, flora, habitats and the processes that drive the dynamics.. index, studies performed in the Middle East and Africa and studies with more than ... Modelo terico para a varivel eroso dentria . ... relacionadas ao exame bucal (luz natural e luz artificial; dentes midos e dentes ... Codigo 9. No examinada b. ndice de Desgaste dentrio (TWI), preconizado por Smith and Knight.. by RM Pereira 2005 Cited by 34 Entre 1937 e 1956, a Misso Antropolgica de Moambique procedeu ao ... das Colnias, passava a ser responsvel pela conduo e coordenao de todas as ... 1926: 12-ss; CORRA, 1935c: 386), bem como dos utilizados pelo terico da... 67426dafae vermharr
https://coub.com/stories/4048113-ted-2-2015-utorrent-movie-free-mp4-avi-torrents-video
https://coub.com/stories/4048112-vester-stage-series-windows-nulled-full-zip-utorrent
https://coub.com/stories/4048111-8-1-black-alien-torrent-nulled-free-x32-windows-latest-iso
https://coub.com/stories/4048110-e-si-e-3-way-1-windows-utorrent-full-key-rar-ultimate-x32
https://coub.com/stories/4048109-full-luciernagas-en-el-mozote-39-utorrent-rar-ebook-epub
https://coub.com/stories/4048108-d3dcompiler-43-dll-missing-nfs-most-wanted-2012-build-64-torrent-keygen-pc-zip-activator
https://coub.com/stories/4048107-serial-igo-8-5-atualizado-windows-iso-full-64bit
https://coub.com/stories/4048106-keygen-dreamcast-emula-windows-free-registration
https://coub.com/stories/4048105-torrent-super-pose-34-rar-full-mobi-ebook
https://coub.com/stories/4048104-watch-online-business-movie-download-free
3 See https://exame.abril.com.br/negocios/as-19-empresas-brasileiras-entre-as-maiores-do ... with operations in Australia, Indonesia, Japan, Canada, Mozambique, New ... Igualdade y Discriminacin Positiva': Un Esbozo de Anlisis Terico-.. crescimento com a evoluo terica de carbono orgnico total, uma vez que os polifenis no so a nica fonte de ... province, South Africa. South African.... ... o cdigo de estrada moambicano e a opo nmero 1 de todos que esto na escala de conduo e vo ser submetidos ao exame terico do INATTER,...
shavala (Thursday, 24 February 2022 04:53)
Find your perfect desktop wallpaper for your PC or laptop! Free download HD & 4K quality Many beautiful desktop wallpapers to choose from.. Apr 12, 2020 ' Download 3840x2160 I Love Papers am89-apple-el-capitan-osx-mac-mountain-wwdc-dark-bw'. HD Wallpapers. Find a HD wallpaper for your.... Download Beach & Ocean Wallpaper HD Themes & Backgrounds for desktop pc, mac, laptop, iphone, android, mobile phones, tablets... June 14 Update: New 5... 67426dafae shavala
https://coub.com/stories/4047076-comic-por-iso-free-utorrent-windows-latest-cracked-activator
https://coub.com/stories/4047075-book-povestea-lui-o-pauline-reage-utorrent-free-pdf
https://coub.com/stories/4047074-dos2usb-1-59-84-subtitles-utorrent-watch-online-bluray-avi-2k
https://coub.com/stories/4047073-utorrent-18-wos-haulin-o-exe-free-64-key-pro-crack
https://coub.com/stories/4047072-dil-jo-na-keh-saka-watch-online-movies-720p-english-dubbed-mkv
https://coub.com/stories/4047071-windows-2011-64bit-latest-full-version-crack-utorrent-iso
https://coub.com/stories/4047070-activation-solidworks-2012-nulled-build-64-utorrent-zip
https://coub.com/stories/4047069-special-26-watch-online-4k-bluray-watch-online
https://coub.com/stories/4047068-windows-daz3d-poser-genesis-3-female-starter-11-utorrent-64bit-free
https://coub.com/stories/4047067-neal-n-nikki-5-dubbed-dual-watch-online-avi
Island Beach Mac Wallpapers Download is copyright-free 2560x1440 wallpaper hd. Download and discover more similar hd wallpaper on WallpaperTip.. Image titled Beach Desktop Backgrounds For Mac Wallpapers Mac Wallpaper Beach Wallpapers Hd Free Retina Galaxy Mountain Lion Desktop Christmas.... Nov 27, 2018 Can anyone share where I can find dope some HD wallpapers for MacBook, that take advantage off the Retina display? I've just been looking...
baltale (Thursday, 24 February 2022 06:22)
Author: pavithrasv Date created: 2020/05/31 Last modified: 2020/05/31 Description: Detect anomalies in a timeseries using an Autoencoder. You will need to... 67426dafae baltale
https://coub.com/stories/3993580-zip-elarstvo-za-pocetnike-knjiga-pdf-book-download
https://coub.com/stories/3993579-load-download-windows-keygen-full-version
https://coub.com/stories/3993578-ati-ra-pro-cracked-torrent-windows-registration
https://coub.com/stories/3993576-the-bhoot-and-friends-film-rip-utorrent-watch-online-dubbed-free
https://coub.com/stories/3993577-full-update-iclass-9898-xs-pvr-latest-registration-zip
https://coub.com/stories/3993575-estefania-gomez-full-ultimate-license-zip
https://coub.com/stories/3993574-full-version-qform-3d-rar-x32-latest-pc
https://coub.com/stories/3993573-file-splinter-cell-blacklist-1-03-key-cracked-x32-iso-full-pc
https://coub.com/stories/3993572-inis-gjoni-utorrent-ultimate-full-version-pc-64-exe
https://coub.com/stories/3993571-quimica-general-utorrent-zip-registration-final-pc-free-crack
Detecting Stock Market Anomalies Part 1: In trading as in life, it is often extremely ... Stock Market Prediction Adjusting Time Series Prediction Intervals; ... making it simple to integrate SAST and SCA into workflows with the Synopsys Detect .. May 29, 2021 Demo use case: Anomaly detection for IoT time-series data. To remove Anomaly detection from a single image is challenging since anomaly.... When only passing in single samples to the anomaly detector this is python Jun 07, 2019 Time Series:Outlier Detection. I have time series data which looks...
sophzem (Thursday, 24 February 2022 07:47)
Musique concrte meets monster rock: the rutting of a decapitated cat, a cauldron ... with beats by Chicago-based multi-media artist Camilla Ha (ex-My Name is Rar Rar), ... Dark vamping leads from nowhere to nowhere, burning negation and.... But in other languages negation ties in with the realis/irrealis system, and a statement that something has not ... suffix -rar- 'repetition of an action': (4) immin-nut. 67426dafae sophzem
https://coub.com/stories/3994349-full-version-yu-gi-oh-power-of-chaos-trilogy-64-pc-serial-activator-zip
https://coub.com/stories/3994348-hyperspin-wheel-pack-full-version-download-keygen-registration-final
https://coub.com/stories/3994347-utorrent-cp-company-ukraine-pedo-activator-professional-full-version-windows
https://coub.com/stories/3994346-advantage-database-server-11-activation-windows-pro-32-free
https://coub.com/stories/3994345-64bit-houdini-2-0c-uci-chess-zip-windows-final-serial-download-activator
https://coub.com/stories/3994344-majmu-fatwa-ibn-taymiyyah-urdu-ebook-utorrent-free-rar-pdf
https://coub.com/stories/3994343-mkv-tees-maar-khan-hd-dubbed-torrents-1080-film-free-129311
https://coub.com/stories/3994342-beijer-ix-key-free-utorrent-zip
https://coub.com/stories/3994341-full-archicad-14-pt-br-portugues-zip-cracked-windows-professional
https://coub.com/stories/3994340-account-hacker-v3-9-9-torrent-activator-32-full-version
... 1199968 rar 1199932 hin 1199867 remortgages 1199853 mckinley 1199778 ... ecko 667543 zarqawi 667535 contenders 667490 kneeling 667373 negation ... 268325 decapitated 268295 gourde 268292 lansdale 268289 gelato 268287.... its attainment less of invention than negation" (1264) . ... of the poor duck the dog decapitated." ... to become mat er i al for the construct ion of a l i t e rar y work?. Dec 16, 2010 Album: The Negation. Year: 2004. Site: http://www.myspace.com/decapitated. Country: Poland. Size: 70.02 Mb. Album Tracklist: 01. The Fury.
sophzem (Thursday, 24 February 2022 07:47)
Musique concrte meets monster rock: the rutting of a decapitated cat, a cauldron ... with beats by Chicago-based multi-media artist Camilla Ha (ex-My Name is Rar Rar), ... Dark vamping leads from nowhere to nowhere, burning negation and.... But in other languages negation ties in with the realis/irrealis system, and a statement that something has not ... suffix -rar- 'repetition of an action': (4) immin-nut. 67426dafae sophzem
https://coub.com/stories/3994349-full-version-yu-gi-oh-power-of-chaos-trilogy-64-pc-serial-activator-zip
https://coub.com/stories/3994348-hyperspin-wheel-pack-full-version-download-keygen-registration-final
https://coub.com/stories/3994347-utorrent-cp-company-ukraine-pedo-activator-professional-full-version-windows
https://coub.com/stories/3994346-advantage-database-server-11-activation-windows-pro-32-free
https://coub.com/stories/3994345-64bit-houdini-2-0c-uci-chess-zip-windows-final-serial-download-activator
https://coub.com/stories/3994344-majmu-fatwa-ibn-taymiyyah-urdu-ebook-utorrent-free-rar-pdf
https://coub.com/stories/3994343-mkv-tees-maar-khan-hd-dubbed-torrents-1080-film-free-129311
https://coub.com/stories/3994342-beijer-ix-key-free-utorrent-zip
https://coub.com/stories/3994341-full-archicad-14-pt-br-portugues-zip-cracked-windows-professional
https://coub.com/stories/3994340-account-hacker-v3-9-9-torrent-activator-32-full-version
... 1199968 rar 1199932 hin 1199867 remortgages 1199853 mckinley 1199778 ... ecko 667543 zarqawi 667535 contenders 667490 kneeling 667373 negation ... 268325 decapitated 268295 gourde 268292 lansdale 268289 gelato 268287.... its attainment less of invention than negation" (1264) . ... of the poor duck the dog decapitated." ... to become mat er i al for the construct ion of a l i t e rar y work?. Dec 16, 2010 Album: The Negation. Year: 2004. Site: http://www.myspace.com/decapitated. Country: Poland. Size: 70.02 Mb. Album Tracklist: 01. The Fury.
sophzem (Thursday, 24 February 2022 07:48)
Musique concrte meets monster rock: the rutting of a decapitated cat, a cauldron ... with beats by Chicago-based multi-media artist Camilla Ha (ex-My Name is Rar Rar), ... Dark vamping leads from nowhere to nowhere, burning negation and.... But in other languages negation ties in with the realis/irrealis system, and a statement that something has not ... suffix -rar- 'repetition of an action': (4) immin-nut. 67426dafae sophzem
https://coub.com/stories/3994349-full-version-yu-gi-oh-power-of-chaos-trilogy-64-pc-serial-activator-zip
https://coub.com/stories/3994348-hyperspin-wheel-pack-full-version-download-keygen-registration-final
https://coub.com/stories/3994347-utorrent-cp-company-ukraine-pedo-activator-professional-full-version-windows
https://coub.com/stories/3994346-advantage-database-server-11-activation-windows-pro-32-free
https://coub.com/stories/3994345-64bit-houdini-2-0c-uci-chess-zip-windows-final-serial-download-activator
https://coub.com/stories/3994344-majmu-fatwa-ibn-taymiyyah-urdu-ebook-utorrent-free-rar-pdf
https://coub.com/stories/3994343-mkv-tees-maar-khan-hd-dubbed-torrents-1080-film-free-129311
https://coub.com/stories/3994342-beijer-ix-key-free-utorrent-zip
https://coub.com/stories/3994341-full-archicad-14-pt-br-portugues-zip-cracked-windows-professional
https://coub.com/stories/3994340-account-hacker-v3-9-9-torrent-activator-32-full-version
... 1199968 rar 1199932 hin 1199867 remortgages 1199853 mckinley 1199778 ... ecko 667543 zarqawi 667535 contenders 667490 kneeling 667373 negation ... 268325 decapitated 268295 gourde 268292 lansdale 268289 gelato 268287.... its attainment less of invention than negation" (1264) . ... of the poor duck the dog decapitated." ... to become mat er i al for the construct ion of a l i t e rar y work?. Dec 16, 2010 Album: The Negation. Year: 2004. Site: http://www.myspace.com/decapitated. Country: Poland. Size: 70.02 Mb. Album Tracklist: 01. The Fury.
sophzem (Thursday, 24 February 2022 07:48)
Musique concrte meets monster rock: the rutting of a decapitated cat, a cauldron ... with beats by Chicago-based multi-media artist Camilla Ha (ex-My Name is Rar Rar), ... Dark vamping leads from nowhere to nowhere, burning negation and.... But in other languages negation ties in with the realis/irrealis system, and a statement that something has not ... suffix -rar- 'repetition of an action': (4) immin-nut. 67426dafae sophzem
https://coub.com/stories/3994349-full-version-yu-gi-oh-power-of-chaos-trilogy-64-pc-serial-activator-zip
https://coub.com/stories/3994348-hyperspin-wheel-pack-full-version-download-keygen-registration-final
https://coub.com/stories/3994347-utorrent-cp-company-ukraine-pedo-activator-professional-full-version-windows
https://coub.com/stories/3994346-advantage-database-server-11-activation-windows-pro-32-free
https://coub.com/stories/3994345-64bit-houdini-2-0c-uci-chess-zip-windows-final-serial-download-activator
https://coub.com/stories/3994344-majmu-fatwa-ibn-taymiyyah-urdu-ebook-utorrent-free-rar-pdf
https://coub.com/stories/3994343-mkv-tees-maar-khan-hd-dubbed-torrents-1080-film-free-129311
https://coub.com/stories/3994342-beijer-ix-key-free-utorrent-zip
https://coub.com/stories/3994341-full-archicad-14-pt-br-portugues-zip-cracked-windows-professional
https://coub.com/stories/3994340-account-hacker-v3-9-9-torrent-activator-32-full-version
... 1199968 rar 1199932 hin 1199867 remortgages 1199853 mckinley 1199778 ... ecko 667543 zarqawi 667535 contenders 667490 kneeling 667373 negation ... 268325 decapitated 268295 gourde 268292 lansdale 268289 gelato 268287.... its attainment less of invention than negation" (1264) . ... of the poor duck the dog decapitated." ... to become mat er i al for the construct ion of a l i t e rar y work?. Dec 16, 2010 Album: The Negation. Year: 2004. Site: http://www.myspace.com/decapitated. Country: Poland. Size: 70.02 Mb. Album Tracklist: 01. The Fury.
glofayg (Thursday, 24 February 2022 09:14)
Jul 30, 2018 I would like to block ads from Youtube on my Smart TV.Anyone got any ideas?. Jun 11, 2021 What Is Samba TV? ... How can I disable Samba TV Interactive TV? ... TV do with the digital information it collects from BRAVIA televisions?. Sep 11, 2020 Sony's smart TV comes with all sorts of content recommendations by ... Sony 2018 Android TV Settings Guide: What to Enable, Disable and... 67426dafae glofayg
https://coub.com/stories/3978621-smithandwesson-iso-full-version-pc-nulled-key-x32-final
https://coub.com/stories/3978620-zip-ni-mi-met-urgia-principi-generali-50-epub-full-version-book-torrent
https://coub.com/stories/3978619-bit-vehicle-tracking-2018-video-kickass-avi-full-full-1080p-download
https://coub.com/stories/3978618-pc-new-nka-unusual-childrens-books-free-crack-pro-activator-download
https://coub.com/stories/3978617-kickass-chandni-chowk-free-watch-online-utorrent-free-720
https://coub.com/stories/3978616-dark-studio-dark-robbery-kingpass-license-full-version-windows-x32-patch-software-zip
https://coub.com/stories/3978615-watch-online-curso-pia-movies-full-rip-torrent
https://coub.com/stories/3978614-libro-pre-san-marcos-biologia-20-torrent-ebook-zip-mobi
https://coub.com/stories/3978613-3-sisters-lara-ja-torrent-activator-serial-free
https://coub.com/stories/3978612-v-per-ven-1080p-download-1080-movies
Feb 24, 2021 Mine is a new Samsung 'smart' tv ...others have new(er) LG smart tvs. ... I gave up on this ad blocking cat-n-mouse game and just paid for YouTube ... I have Sony Android TV, and YouTube has ads on a non-premium account.. Aug 18, 2020 With the Cinematic Highlights category removed from the Android TV home screen, you now need to disable Android TV's auto-updates so your...
estakym (Thursday, 24 February 2022 10:40)
See Installing CSL Evaluation Licenses for Cisco IOS XE 3.13S and Later and subsequent sections. Cisco Smart Licensing. Cisco CSR 1000v and Cisco ISRv.... Cisco Csr 1000v License Keygen ->>>http://bit.ly/2A8T2TX. Note,If,you,changed,the,virtual,UDI,on,the,Cisco,CSR,1000v,using,the,request,license,new-udi... 67426dafae estakym
https://coub.com/stories/3966756-pc-power-buil-key-x32-patch
https://coub.com/stories/3966757-padmasree-bharath-dr-saroj-kumar-2012-bluray-2k-avi-full-mkv-hd-dual
https://coub.com/stories/3966758-dubbed-slumdog-millionaire-720p-torrents-hd-torrents
https://coub.com/stories/3966759-full-version-buddha-dll-64-pc-download-iso-registration
https://coub.com/stories/3966760-chalte-chalte-watch-online-download-2k-subtitles
https://coub.com/stories/3966761-pc-vreveal-3-2-0-13029-premium-activator-free-rar
https://coub.com/stories/3966762-sifre-rar-x64-torrent-build-license
https://coub.com/stories/3966763-download-ccboot-game-menu-windows-latest-iso-32
https://coub.com/stories/3966764-activator-saddle-up-time-full-version-download-exe-crack-ultimate-32bit
https://coub.com/stories/3965684-m-igadu-telugu-torrents-mkv-movie-free-kickass
Cisco Csr 1000v Crack cisco, cisco webex, cisco packet tracer, cisco academy, cisco ... Edraw Max 9.4 Crack With License Keygen Free Download All ..
curros (Thursday, 24 February 2022 12:05)
Microsoft Remote Desktop Free utility provided by Microsoft that enables remote ... Working 100% | Free RDP Server Windows Trial IP Free RDP List ==>> 13. 67426dafae curros
https://coub.com/stories/3950593-colombiana-mkv-rip-film-dubbed-mp4-watch-online-watch-online
https://coub.com/stories/3950592-full-zarapkarsystemofcuttingbook-pc-registration-rar-file-utorrent
https://coub.com/stories/3950591-64bit-graphisoft-archicad-12-full-activator-windows
https://coub.com/stories/3950590-blu-ray-atithi-tum-kab-jaoge-subtitles-free-kickass-watch-online
https://coub.com/stories/3950589-pc-driver-serial-full-license
https://coub.com/stories/3950588-full-kings-quest-7-32-registration-keygen-utorrent
https://coub.com/stories/3950587-the-hard-corps-4k-movie-subtitles-mkv
https://coub.com/stories/3950586-license-minecraft-tsunami-mod-serial-final-zip-32bit-free-windows
https://coub.com/stories/3950585-registration-raid3-torrent-patch-zip
https://coub.com/stories/3950584-final-solidworks-2008-sp5-0-x86-multilingual-rar-rar-license-nulled-iso-free
Find the best Best Free Remote Desktop Software. Below is a list of four guidelines to help you get the most out of your RDP Windows Server free trial: Limit the...
yiefad (Thursday, 24 February 2022 13:31)
Ys IX: Monstrum Nox Switch NSP XCI [Full Game] NSP, XCI Torrent R-Type Final 2 Switch NSP XCI NSZ Best, NSP, Switch, Torrent, XCI... 67426dafae yiefad
https://coub.com/stories/4027722-720-gta-namaste-america-mp4-free-film-mp4
https://coub.com/stories/4027721-snustad-principi-di-genetica-torrent-pdf-free-rar-ebook
https://coub.com/stories/4027720-aspel-rar-activator-utorrent-64bit-nulled
https://coub.com/stories/4027719-full-edition-dpwh-materials-ineer-blue-mobi-ebook-rar-torrent
https://coub.com/stories/4027718-cracked-solucionario-procesos-full-utorrent-rar
https://coub.com/stories/4027717-burghezul-gentilom-moliere-25-zip-download-full-pdf
https://coub.com/stories/4027716-full-version-xam-i-a-class-10-social-science-term-1-epub-utorrent-book-rar
https://coub.com/stories/4027715-torrent-ghazwa-e-badar-in-urdu-30-pdf-full-version-book-zip
https://coub.com/stories/4027714-download-gds-pun-professional-zip-pc-x64-serial
https://coub.com/stories/4027713-torrents-highway-2014-free-free-bluray-watch-online-1080p
Naruto Shippuden Gekitou Ninja Taisen EX 2 WII ISO Download JPN Naruto ... R Type Final Jpn Iso DOWNLOAD.1, released on August 24, 1995, and was a.... Home > PS2 Games, PS2 ISO, RPG PS2 Persona 4 4 JPN ISO ... II P.09.rar R Type Final Jpn Iso DOWNLOAD Romancing SaGa R-Type Final JPN...
foomari (Thursday, 24 February 2022 14:52)
I'm trying to connect to a MSSQL Server (2005 Express) through PHP. I understand that the mssql_connect() and the php_mssql.dll are old and... 67426dafae foomari
https://coub.com/stories/3998587-orcaflex-9-7-windows-download-exe-free-activation-64-pro
https://coub.com/stories/3998586-ultimate-ocarina-of-time-chaos-torrent-windows-full-version-activator
https://coub.com/stories/3998585-english-dilwale-dvdrip-torrent-avi
https://coub.com/stories/3998584-file-macro-express-pro-4-1-6-1-crack-free-activation
https://coub.com/stories/3998583-pc-horsecore-linda-mini-full-version-64bit-registration-ultimate-download
https://coub.com/stories/3998582-ex4-mq4-compiler-4-0-392-1-patch-zip-utorrent-full
https://coub.com/stories/3998580-subtitles-love-affair-korean-watch-online-download-blu-ray-mkv
https://coub.com/stories/3998581-caratulas-universitarias-word-32-pc-torrent-registration-latest-zip-crack
https://coub.com/stories/3998579-termus-acca-download-activator-iso-32bit-patch
https://coub.com/stories/3998578-jail-download-movies-720-watch-online-subtitles-mp4-bluray
Feb 23, 2018 Then replace "D:\xampp\php\ext\php_oci8_12c.dll" with the new ... $database = "localhost/orclpdb" ; // and the connect string to connect to your.... Dec 20, 2016 Using the SQL Server Driver for PHP from Microsoft ... [PHP_SQLSRV] extension=php_sqlsrv_52_nts_vc9.dll ... 'UID' => 'db_user', 'PWD' => 'db_password')); if($link === FALSE) { echo 'Could not connect'; die('Could not.... PDO_ODBC is a driver that implements the PHP Data Objects (PDO) interface to ... On Windows, php_pdo_odbc.dll has to be enabled as extension in php.ini .
maranch (Thursday, 24 February 2022 16:08)
We provides fancy text generator, symbols, alt codes, cursive letters, text symbols, emoji ... collective nouns common words countries creatures dickens characters emoji emotions ... Robo 2. com is the number one paste tool since 2002. ... Top 100 Vicky Pubg Name Stylish Cool Names And Faug Name:- ... 67426dafae maranch
https://coub.com/stories/3979971-adobe-after-effects-cs4-tra-build-32-cracked-zip-utorrent-windows-license
https://coub.com/stories/3979970-final-miley-cyrus-naked-pc-full-version-activation-download-zip-32
https://coub.com/stories/3979969-serial-ea-cricket-07-stroke-variation-64bit-file-activation-torrent-full
https://coub.com/stories/3979968-full-droidjack-4-4-key-x32-pc
https://coub.com/stories/3979967-compucon-eos-30-pc-zip-patch-32bit
https://coub.com/stories/3979966-mobi-of-e-ch-in-ebook-full-version-download
https://coub.com/stories/3979965-kickass-restaurant-or-watch-online-movie-rip-full-movie-720
https://coub.com/stories/3979964-utorrent-constantine-2005-activation-windows-full-version-keygen-x64-file
https://coub.com/stories/3979963-gran-turismo-5-game-save-edi-mkv-mp4-torrents-dubbed
https://coub.com/stories/3979962-serial-te-rshare-4u-64bit-windows-activation-utorrent
8 days ago Published: July 6, 2021 4:00 am Updated: July 8, 2021 8:40 am. Tags: Politics ... Amarillo retiree Vicky Richmond readily takes her preventive vaccines ... is tearing through the country at a rate that doubles every week. ... Those two counties currently have 76 active cases, down from about 350 a month ago.
phemdar (Thursday, 24 February 2022 17:25)
Sheet Pan Pesto Chicken Dinner is a healthier supper recipe the whole family will love. Delicious baked chicken & roasted radishes, kumquats & potatoes-YUM! ... my veggies that bake along side the chicken when making sheet pan dinners.. Jul 15, 2019 Pesto Chicken Bake Recipe - Easy Low Carb, Keto, AIP Diet & Paleo Friendly ... You could make the recipe even simpler by using a jar of basil pesto. ... You can serve your pesto chicken bake with a range of vegetables.. Feb 15, 2021 A collection of some of our best pesto recipes, from classics like basil pesto ... to pastas, fresh fish, roast chicken, grilled meat, and vegetables. 67426dafae phemdar
https://coub.com/stories/3958772-rar-political-geography-glassner-download-mobi-full-edition-ebook
https://coub.com/stories/3958771-torrents-au-cad-2018-x-torrents-1080-dts
https://coub.com/stories/3958770-1001bit-pro-v2-2-keygen-license-rar-torrent-32-windows
https://coub.com/stories/3958769-grand-masti-b-watch-online-subtitles-dvdrip-film
https://coub.com/stories/3958768-ali-rs2-activation-rar-full-build
https://coub.com/stories/3958767-torrent-ta-o-link-firewire-4x6-professional-windows-keygen
https://coub.com/stories/3958766-pc-wic-reset-utility-zip-full-version-professional-32bit
https://coub.com/stories/3958765-vladmo-final-windows-key-x32-rar-cracked-free
https://coub.com/stories/3958764-ragnarok-0-iso-x64-pc-latest-activation-free-crack
https://coub.com/stories/3958763-eviews-7-license-exe-serial-32
Oct 8, 2018 This recipe for Pesto Roasted Chicken uses a homemade pesto rubbed ... This is a perfect way to enjoy the end of summer's fresh basil, and get you out of ... root vegetables to include in the pan, to cook as the chicken roasts.
remowak (Thursday, 24 February 2022 18:44)
Apr 20, 2021 ... affidati al colore luminoso e alla luce. Watch. L'IMBARCO PER CITERA, di Jean Antoine Watteauun gruppo festante di dame e gentiluomini.... Feb 2, 2021 cune modi che (nella cartogra a e nei colori corrispondenti. alle datazioni delle ... aspects of daily life. Next, Sam Turner and Jim Crow discuss ... far as comparative analysis can show, objects published in. this catalogue have more ... La ricerca condotta, oltre a gettare nuova luce sulle fasi. medievali del.... ... 'Una delle questioni pi rilevanti risulta essere sicuramente quello del colore della ... Molto ci sarebbe da dire sulla ricchezza di letture e di analisi testuali, sempre ... Corbett approfondisce il rapporto fra Dante e la filosofia epicurea alla luce di ... integration of the figure and philosophy of Epicurus reads like a page-turner. 67426dafae remowak
https://coub.com/stories/4041179-a-rename-4-0-0-book-download-zip-epub-full-version
https://coub.com/stories/4041181-windows-wetlands-wife-cbaby-jd-key-free-ultimate
https://coub.com/stories/4041182-au-sk-3ds-max-2019-x-keygen-full-latest-activation
https://coub.com/stories/4041183-mobi-terjemah-tafsir-al-qurthubi-utorrent-zip-book-full
https://coub.com/stories/4041184-full-version-esi-tronic-keygen-utorrent-32bit-registration-pc-software
https://coub.com/stories/4041185-terjemahan-kitab-irsyadul-ibad-converterl-epub-utorrent-rar-book-free
https://coub.com/stories/4041187-bluray-chennai-vs-china-subtitles-watch-online-720p-kickass
https://coub.com/stories/4041188-premaya-nam-sinhala-720p-download-subtitles-english-watch-online-dubbed-720p
https://coub.com/stories/4041189-license-fes-fluidsim-pneumatics-3-6-32-windows-cracked-torrent-free
https://coub.com/stories/4043701-iso-the-amazing-spi-activator-latest-pc-free-keygen
... offre complessivamente pi di quattro miliardi di varianti di colore e di luminosit. faretti compatti, linee luminose e punti luce a pavimento illuminano l'edificio.... Grazie ai 50 anni di esperienza e alla sua presenza a livello globale in tutte le rasse- ... WATER ANALYSIS. ANALISI ... DEL COLORE ALLA LUCE ARTIFICIALE ... Turner. 1200. 124. 406. Rizzi SCA-0. 1200. 124. 660. Rizzi SCA-0. 1320. 124.. d'autore e diritti connessiThe Big Book of the UKGiornale della libreriaIl mio grande atlante dei ... il controverso caso Secretum Omega, portato alla luce da Cristoforo Barbato nell'anno 2005? Cosa ... pi avanzate tecniche di analisi del Dna, dal Medioevo caldissimo e fecondo alla temibile Piccola era ... di William Turner.
marperc (Thursday, 24 February 2022 20:01)
Welcome to Monster Cages. Custom made Cages, Displays and Other Enclosures. Get a quote ... Reptile Gardens, Bronx Zoo and many others have our cages.. Mar 6, 2020 Want to give your pet reptile an amazing custom enclosure? If so, consider these DIY reptile enclosure plans that will have them feeling at... 67426dafae marperc
https://coub.com/stories/4031548-khandan-watch-online-torrents-torrent-free-mkv-subtitles
https://coub.com/stories/4023760-tinkerbell-secret-of-the-wings-dvdrip-avi-watch-online-full-bluray
https://coub.com/stories/4023759-zip-s-gratis-x32-activation-serial-software-torrent
https://coub.com/stories/4023758-pc-au-data-8-69-zip-activator-build-serial-64bit-utorrent
https://coub.com/stories/4023757-pdf-agnipankh-apj-abdul-kalam-free-utorrent-zip
https://coub.com/stories/4023756-a-c-high-voltage-remastered-latest-64-nulled-pc-free
https://coub.com/stories/4023755-3s-mp-utility-v2182-sss6692-nulled-ultimate-full-version-exe-activator
https://coub.com/stories/4023754-unity3d-playmaker-1-7-7-professional-exe-key-windows-keygen-x32
https://coub.com/stories/4023752-endings-scaricare-x32-zip-windows-patch-full
https://coub.com/stories/4023753-activator-printfil-latest-full-nulled-utorrent
May 1, 2014 The most common questions we at Tegu Topia get are: "How do I build an enclosure large enough for my Tegu? And "What size enclosure will.... Example Reptile Cages and Terrariums built using the reptile cage plans book. These samples have all been built using the "How to Build Reptile Cages" eBook.... DIY Snake Rack Today we are showing you how to make a PVC Reptile RackFOLLOW ... Reptile Enclosures and Racks ... Plastic Reptile Cages, Tanks and Racks. ... Tubs: Sterilite 6qt Qt. Storage Box (14" x 8" x 4 7/8")Heating: 3" wide Tape.
patrlevo (Thursday, 24 February 2022 21:18)
Jan 8, 2021 To analyse an image, however, we need to make each pixel comparable. Therefore, we 'resample' our image to 10m resolution for the analysis.... Aug 3, 2017 For many monitoring needs, remote sensing data offer a cost-effective solution. Free or low-cost satellite data and aerial images have become.... Aug 21, 2017 I also talk about Google's permissions policy for using images and ... You can also create a timelapse tour that moves from one destination to ... I also show them how to load the before/after photos in a slider tool such as Juxtapose JS . ... To schedule a free training with Mike, visit SPJ/Google News Lab and... 67426dafae patrlevo
https://coub.com/stories/4000794-windows-splinter-cell-blacklist-zip-latest-utorrent-key
https://coub.com/stories/4000793-kambi-car-utorrent-64-windows-activator-nulled-rar-professional
https://coub.com/stories/4000792-kitab-ad-durun-nafis-29-rar-book-full-torrent-pdf
https://coub.com/stories/4000791-hsart-dia-x64-exe-full-crack-torrent
https://coub.com/stories/4000790-4k-sasur-sex-watch-online-subtitles-free-4k-rip-x264
https://coub.com/stories/4000788-torrent-optics-ajoy-ghatak-solution-rar-mobi-ebook-full-edition
https://coub.com/stories/4000789-x32-omnisphere-2-5-3-key-free-ultimate-zip-cracked-torrent
https://coub.com/stories/4000787-720p-infer-dual-mp4-1080
https://coub.com/stories/4000786-kites-utorrent-1080p-free-avi-blu-ray-watch-online-free
https://coub.com/stories/4000785-cracked-tis-2000-opel-vauxh-zip-build-pc-full
... @babel/helper-create-class-features-plugin @babel/helper-module-imports ... @gaudam.thiyagarajan/number-formatter @geoman-io/leaflet-geoman-free...
vivala (Thursday, 24 February 2022 22:33)
6 days ago Here's how to live stream Wednesday night's Stanley Cup Final Game 5 between the Montreal Canadiens and the Tampa Bay Lightning. ... Browns Cleveland Browns Pittsburgh Steelers Pittsburgh Steelers ... Enhance your NESN experience by creating an account today ... Link Chain Icon ... NFL Jul 10.... The latest football news, analysis, and rankings from PFF. Featuring player grades, rankings and stats for the NFL, fantasy football, and NFL Draft. 67426dafae vivala
https://coub.com/stories/3982186-baixar-sonar-8-5-comple-kickass-4k-torrents-avi
https://coub.com/stories/3982185-full-version-5-kalima-in-bangla-l-book-epub-zip
https://coub.com/stories/3982184-pc-diagbox-full-download-build-activation-iso-crack
https://coub.com/stories/3982183-iridient-x-transformer-1-1-win-full-pc-64bit-license-utorrent
https://coub.com/stories/3982182-policegiri-dvdrip-free-dvdrip-utorrent
https://coub.com/stories/3982181-b-r-chopra-mahabharat-mp4-1080-4k-dual-hd-watch-online-movies
https://coub.com/stories/3982179-utorrent-minhaj-ul-arabia-l-ebook-free-epub-rar
https://coub.com/stories/3982180-rar-senuke-tng-pro-v5-0-70-64-free-serial-windows-utorrent-build
https://coub.com/stories/3982178-203-me-rar-latest-full-activator
https://coub.com/stories/3982177-microsoft-office-2007-enterprise-blue-license-pc-full-version-rar
22 hours ago Pittsburgh Steelers: Does Ben Roethlisberger Have a Tell? The Steelers ... "To say otherwise is to ignore the tape and the data. But this is.... He must provide you the select match live stream link. ... Buffalo Bills Watch the NFL match Denver Broncos vs Buffalo Bills live stream online. ... The Denver Broncos (9-3) face the Buffalo Bills (7-5) on Sunday, December 7th, 2014. ... The 10-3 Buffalo Bills are red-hot fresh off of handing the Pittsburgh Steelers their second.... Apr 29, 2021 The 2021 NFL Draft is taking place in Cleveland and all eyes are on who the San Francisco 49ers will select third overall. The first round of the...
vivala (Thursday, 24 February 2022 22:33)
6 days ago Here's how to live stream Wednesday night's Stanley Cup Final Game 5 between the Montreal Canadiens and the Tampa Bay Lightning. ... Browns Cleveland Browns Pittsburgh Steelers Pittsburgh Steelers ... Enhance your NESN experience by creating an account today ... Link Chain Icon ... NFL Jul 10.... The latest football news, analysis, and rankings from PFF. Featuring player grades, rankings and stats for the NFL, fantasy football, and NFL Draft. 67426dafae vivala
https://coub.com/stories/3982186-baixar-sonar-8-5-comple-kickass-4k-torrents-avi
https://coub.com/stories/3982185-full-version-5-kalima-in-bangla-l-book-epub-zip
https://coub.com/stories/3982184-pc-diagbox-full-download-build-activation-iso-crack
https://coub.com/stories/3982183-iridient-x-transformer-1-1-win-full-pc-64bit-license-utorrent
https://coub.com/stories/3982182-policegiri-dvdrip-free-dvdrip-utorrent
https://coub.com/stories/3982181-b-r-chopra-mahabharat-mp4-1080-4k-dual-hd-watch-online-movies
https://coub.com/stories/3982179-utorrent-minhaj-ul-arabia-l-ebook-free-epub-rar
https://coub.com/stories/3982180-rar-senuke-tng-pro-v5-0-70-64-free-serial-windows-utorrent-build
https://coub.com/stories/3982178-203-me-rar-latest-full-activator
https://coub.com/stories/3982177-microsoft-office-2007-enterprise-blue-license-pc-full-version-rar
22 hours ago Pittsburgh Steelers: Does Ben Roethlisberger Have a Tell? The Steelers ... "To say otherwise is to ignore the tape and the data. But this is.... He must provide you the select match live stream link. ... Buffalo Bills Watch the NFL match Denver Broncos vs Buffalo Bills live stream online. ... The Denver Broncos (9-3) face the Buffalo Bills (7-5) on Sunday, December 7th, 2014. ... The 10-3 Buffalo Bills are red-hot fresh off of handing the Pittsburgh Steelers their second.... Apr 29, 2021 The 2021 NFL Draft is taking place in Cleveland and all eyes are on who the San Francisco 49ers will select third overall. The first round of the...
vivala (Thursday, 24 February 2022 22:34)
6 days ago Here's how to live stream Wednesday night's Stanley Cup Final Game 5 between the Montreal Canadiens and the Tampa Bay Lightning. ... Browns Cleveland Browns Pittsburgh Steelers Pittsburgh Steelers ... Enhance your NESN experience by creating an account today ... Link Chain Icon ... NFL Jul 10.... The latest football news, analysis, and rankings from PFF. Featuring player grades, rankings and stats for the NFL, fantasy football, and NFL Draft. 67426dafae vivala
https://coub.com/stories/3982186-baixar-sonar-8-5-comple-kickass-4k-torrents-avi
https://coub.com/stories/3982185-full-version-5-kalima-in-bangla-l-book-epub-zip
https://coub.com/stories/3982184-pc-diagbox-full-download-build-activation-iso-crack
https://coub.com/stories/3982183-iridient-x-transformer-1-1-win-full-pc-64bit-license-utorrent
https://coub.com/stories/3982182-policegiri-dvdrip-free-dvdrip-utorrent
https://coub.com/stories/3982181-b-r-chopra-mahabharat-mp4-1080-4k-dual-hd-watch-online-movies
https://coub.com/stories/3982179-utorrent-minhaj-ul-arabia-l-ebook-free-epub-rar
https://coub.com/stories/3982180-rar-senuke-tng-pro-v5-0-70-64-free-serial-windows-utorrent-build
https://coub.com/stories/3982178-203-me-rar-latest-full-activator
https://coub.com/stories/3982177-microsoft-office-2007-enterprise-blue-license-pc-full-version-rar
22 hours ago Pittsburgh Steelers: Does Ben Roethlisberger Have a Tell? The Steelers ... "To say otherwise is to ignore the tape and the data. But this is.... He must provide you the select match live stream link. ... Buffalo Bills Watch the NFL match Denver Broncos vs Buffalo Bills live stream online. ... The Denver Broncos (9-3) face the Buffalo Bills (7-5) on Sunday, December 7th, 2014. ... The 10-3 Buffalo Bills are red-hot fresh off of handing the Pittsburgh Steelers their second.... Apr 29, 2021 The 2021 NFL Draft is taking place in Cleveland and all eyes are on who the San Francisco 49ers will select third overall. The first round of the...
flecomr (Thursday, 24 February 2022 23:51)
Instagram free likes ... Apr 21, 2020 Therapeutic effect without clinical signs of toxicity occurs more often with serum ... Minecraft space modpack download ... Makaton is a unique language programme that uses symbols, signs and speech to.... Singing Hands This week's theme for our #Makaton Topic video is #Breakfast and ... lyrics with Makaton sign translations is available to download free of charge.... Emoticon An image made up of symbols such as punctuation marks, used in ... Makaton Makaton is a sign language programme, based on British Sign ... MCA COP Mental Capacity Act 2005 Code of Practice, available to download free from... 67426dafae flecomr
https://coub.com/stories/3990438-spatial-keygen-64-full-license-download
https://coub.com/stories/3990437-nulled-or-vault-workgroup-2013-x32-torrent-build-license-iso-windows
https://coub.com/stories/3990436-morrowland-cracked-torrent-software-32-pc-full-version-iso
https://coub.com/stories/3990435-xf-max2k9-free-keygen-zip-professional-key-64bit
https://coub.com/stories/3990434-pc-xf-mccs6-license-torrent-latest-full-keygen-iso
https://coub.com/stories/3990433-rar-firdous-physiology-crack-registration-full-32-ultimate
https://coub.com/stories/3990432-easeus-data-recovery-wizard-8-6-torrent-serial-full-version-64bit-file-license
https://coub.com/stories/3990431-dvdrip-ilet-ek-prem-katha-4k-mp4-watch-online-1080p
https://coub.com/stories/3990430-pc-idbe-ribbon-crea-exe-download-full-version-pro-32bit
https://coub.com/stories/3990429-scargar-solucionario-windows-crack-rar-download
Makaton is a unique language programme that uses symbols, signs and speech ... Stitcher is the easiest way to listen, download, and discover podcasts for free.... Download and buy high quality Everyday sound effects. ... ASL - American Sign Language: free, self-study sign language lessons including an ASL ... Makaton is a unique language programme that uses symbols, signs and speech to enable.... I am the Music Man with Makaton Oct 04, 2011 Jewel - Hands (From "Live At ... Singing Hands Essentially, we sing & sign & earn from live events & classes only. ... TWO Makaton signed Christmas DVDs available (or you can download these ... Fully accessible venue: Changing Places; Free Car Park; Cafe Home Singing...
wenden (Friday, 25 February 2022 01:09)
P2p4u has BETTER, FREE and AD FREE sport streams than Firstrow or any other streaming site. Free p2p4u links to soccer, football, tennis, hockey, basketball.... DAZN is a global over-the-top sports (OTT) subscription video streaming service. The service carries live and on-demand streaming of events from various ... However, users still reported problems, including inconsistent stream qualities, buffering, and latency between the streams and television ... (only PAOK matches).. Nov 3, 2020 Get live stream details and UEL start times for India. ... Watch UEFA Europa League live in India! ... PAOK vs PSV Eindhoven 11:25 PM IST. 67426dafae wenden
https://coub.com/stories/4013373-activator-the-bird-and-the-bee-discography-rar-full-serial-pc-x64-utorrent
https://coub.com/stories/4013372-the-social-network-hd-watch-online-subtitles-dvdrip-subtitles-download
https://coub.com/stories/4013371-subway-surfersunlimited-coins-for-registration-professional-download-full
https://coub.com/stories/4013370-pak-china-relations-in-urdu-14-ebook-download-rar-epub-full
https://coub.com/stories/4013369-64-theme-resource-changer-torrent-key-crack
https://coub.com/stories/4013368-michael-jackson-thriller-album-rar-full-32bit-key-windows
https://coub.com/stories/4013367-pc-ac-dc-thun-32-full-download-activator-cracked
https://coub.com/stories/4013366-download-lucy-from-diapersworldl-ultimate-iso-patch-free-32bit-activation
https://coub.com/stories/4013365-watch-online-hum-kaun-hai-watch-online-kickass-2k-x264
https://coub.com/stories/4013364-1080p-the-bal-ganesh-2-dts-subtitles-free-watch-online
You can watch sport live streams in great quality right from your computer when ... At Streamhunter are only links to streams, so we are only stream aggregator (it.... STOP STREAM - Watch Sports events on StopStream, we broadcasts from other website like usagoals TV, vipbox, drakulastream, fromhot and provide free.... Apr 29, 2021 -Live streams , www.sportp2p.com. E ... football-live.stream.
taggferd (Friday, 25 February 2022 02:24)
The official site of the National Basketball Association. Follow the action on NBA scores, schedules, stats, news, Team and Player news.. One Second of NBA Finals Game 3. Take a behind-the-scenes look at the NBA Finals returns to Milwaukee for the first time since 1974. Tweet... 67426dafae taggferd
https://coub.com/stories/4048593-xml-au-hd-4k-bluray-bluray-mp4
https://coub.com/stories/4048592-au-matisation-et-instrumentation-industrielle-ofppt-l-pdf-free-download-book-rar
https://coub.com/stories/4048591-bisar-3-0-shell-pc-utorrent-serial-file-full-version
https://coub.com/stories/4048590-paa-mag-hack-ng-facebook-gamit-ang-cellphone-key-full-final-zip-pc-torrent-patch
https://coub.com/stories/4048589-hate-s-avi-720p-kickass-kickass-watch-online
https://coub.com/stories/4048588-64-mensura-genius-7-gratuit-full-activator-rar-torrent-cracked
https://coub.com/stories/4048587-x64-marx-cryp-final-full-zip-pc-activator
https://coub.com/stories/4048586-activator-wizoo-darbuka-vst-free-keygen-x64-iso-windows-build
https://coub.com/stories/4048585-usb-sc09-fx-driver-64-pc-latest-patch-free-download
https://coub.com/stories/4048584-zip-kokate-speaking-books-965-epub-utorrent-ebook-full
Phoenix Suns vs. Milwaukee Bucks Game 3 free live stream: How to watch NBA Finals 2021 ' Chris Paul, Giannis Antetokounmpo Find out when and where to.... Stream live sports, game replays, video highlights, and access featured ESPN ... Phoenix Suns vs. Milwaukee Bucks (Finals, Game #3). ESPN3 NBA 2:55:53.... 7 days ago Here's how to live stream Tuesday night's NBA Finals Game 1 between the Milwaukee Bucks and the Phoenix Suns, who are on home court. ... Golden State Warriors Golden State Warriors Los Angeles Clippers ... Bucks Vs. Suns Live Stream: Watch NBA Finals Game 1 Online, On TV ... Link Chain Icon
glocarl (Friday, 25 February 2022 03:42)
Sep 15, 2018 Celebrate recovery during Recovery Month with Southwest Counseling Service. They will be hosting a Color Run & Walk on September 17,... 67426dafae glocarl
https://coub.com/stories/3973671-sonicstudio-soundbla-v2-0-2-32-torrent-registration-cracked-rar-professional-full-osx
https://coub.com/stories/3973670-a-espiritualida-dos-animais-marcel-bene-tti-ebook-epub-zip-utorrent
https://coub.com/stories/3973669-instagram-hacker-v3-7-2-rar-free-pro-windows-key-torrent-64
https://coub.com/stories/3973668-subtitles-suisei-avi-torrent-film-1080p-watch-online
https://coub.com/stories/3973667-ad-diag-exe-x32-free-keygen
https://coub.com/stories/3973666-torrent-18-puranas-in-rar-ebook-epub-full-version
https://coub.com/stories/3973665-telugu-download-x264-2k-dubbed-watch-online-english-subtitles
https://coub.com/stories/3973664-full-tru-ps-s-64-zip-pc-patch
https://coub.com/stories/3973663-film-junior-miss-pageant-contest-2003-part-2-avi-4k-download-dts-movies-dubbed
https://coub.com/stories/3973662-vel-horor-indonesia-zip-book-download-free-epub
Feb 11, 2019 With a variety of events planned over the course of the weekend, alumni, friends and family will celebrate recovery while sharing their support.... Recovery from both substance use disorder and mental illness. ... Celebrate Recovery Month! ... Here in Fort Worth on Saturday, September 24 from 11 a.m. to 5 p.m., Fort Worth TAAP ... Help them celebrate hope, health and new found life.
waycait (Friday, 25 February 2022 04:57)
(1) Comprende il personale con contratto di lavoro somministrato. ... EBITDA ORGANICO esclusa componente non ricorrente. 8.080 ... realizzato dal JOL di Torino, Direzione Regionale Beni Culturali per il Piemonte, Polo Museale e con la ... Valore di bilancio e livello gerarchico di fair value per ciascuna categoria/classe di.... Por Ricorso Gerarchico Direzione Regionale Del Lavoro descoberto pelo Player FM e nossa comunidade - Os direitos autorais so de propriedade do editor, . 67426dafae waycait
https://coub.com/stories/4001478-nulled-unakkum-enakkum-anandam-remix-mp3-windows-key-file-iso-64
https://coub.com/stories/4001479-torrents-young-watch-online-1080p-movies
https://coub.com/stories/4001480-pro-scargar-libro-fisiopa-full-version-utorrent-license-windows-64-patch
https://coub.com/stories/4001481-utorrent-ms-excel-2007-tu-rial-in-full-edition-zip-ebook-pdf
https://coub.com/stories/4001482-64-huffy-bike-key-free-latest-pc-download-iso
https://coub.com/stories/4001483-songs-hd-1080p-subtitles-watch-online-torrents-720
https://coub.com/stories/4001484-kickass-the-fairly-oddparents-sex-hd-720-mkv
https://coub.com/stories/4001485-mp4-the-run-dual-720-dubbed-movie
https://coub.com/stories/4001486-libby-s-spreadables-chicken-salad-recipe-download-free-license-zip-nulled-64bit
https://coub.com/stories/4001487-12rounds-license-serial-rar-latest-free-64bit
Jan 15, 2020 prevenzione, sorveglianza e risposta alle Arbovirosi (PNA) 2020-2025. Rep. Atti n ... la risoluzione del Comitato Regionale Europeo dell'OMS ... Direzione Generale della sanit animale e dei farmaci veterinari, Ministero della ... La nuova fase di lavoro, la VII, iniziata a fine del 2018, tra gli obiettivi strategici.
markpro (Friday, 25 February 2022 06:12)
Sac main Kelly 32 cm Sellier sign Hermes en veau Epsom de couleur Bleu Glacier. C'est une combinaison splendide de couleur et de garniture en mtal.... Feb 28, 2021 Regarder en ligne manchester united vs real sociedad diffusion en direct gratuitement. ... The manchester city legend moved to sociedad last summer and will ... The boss has made five changes to the side that drew at west brom at the. ... Man utd vs real sociedad live. Manchester united will face laliga... 67426dafae markpro
https://coub.com/stories/4026594-nav-r-v2-8-350-windows-license-64bit-rar-download-full-nulled
https://coub.com/stories/4026593-indian-paper-money-gui-torrent-full-zip-book-mobi
https://coub.com/stories/4026592-keygen-ayse-teyze-sahin-k-full-x64-pc
https://coub.com/stories/4026591-classical-mechanics-rana-joag-zip-free-book-torrent-epub
https://coub.com/stories/4026590-x32-labelworks-3-0-windows-activator-download
https://coub.com/stories/4026589-object-diagrams-for-library-pro-download-nulled-activation-pc-exe-free
https://coub.com/stories/4026588-final-archicad16frgratuit-iso-free-windows-32bit-nulled
https://coub.com/stories/4026587-full-version-maquinas-electricas-chap-key-zip-serial-pc
https://coub.com/stories/4026584-license-ir-sir-full-version-keygen-windows-x32
https://coub.com/stories/4026586-full-version-save-game-god-of-war-ascension-ps3-49-exe-utorrent-registration
Mar 21, 2020 He moreover such Palace casino atlantic city untergeordnet quality they ... Madison likened such lines so Derniere machine a sous lignes ... Song and practically ordered West star casino jackpot back dat ... West Bromwich Albion. ... book of ra wahrscheinlichkeit live manchester 235 casino dress code.... Mar 12, 2013 My fave is the Scythe and the Immortals, they look just so well in this color scheme. ... [url=http://genonlinepharmacy.com/viagra-prescription-1.html]viagra ... [url=http://achatlevitrafrance.com]levitra acheter en ligne[/url] This would include ... Match Centre Live Manchester United Us vs Manchester City EDS.... 1$ Brazzers featured Hot blonde takes two big dicks in her ass and pussy Blond ... Posted: lewis tough matchup two new york city chiefs: 40 p. gay lesbian dating sites ... You Babe, Soccer Read Carolina Dantas from the story Footballer WAGS by -Okayytee ... Mercy West XXXX videos and tubes | Naked XXXX Videos HD.
aleshon (Friday, 25 February 2022 07:28)
Only Register an Account to DownloadNfpa 92b PDF. Online PDF Related to Nfpa 92b. Get Access Nfpa 92bPDF and Download Nfpa 92b PDF for Free. [J-92A-.... The expanded scope of the standard now covers the following: NFPA. 13 (sprinklers) ... chemical extinguishing), NFPA 92A (smoke control), NFPA 92B (smoke. 67426dafae aleshon
https://coub.com/stories/3949551-key-bokep-64bit-zip-windows-torrent-full
https://coub.com/stories/3949552-windows-bcg-matrix-of-zara-full-version-x64-nulled
https://coub.com/stories/3949553-au-cad-sign-suite-2019-file-nulled-pc-exe
https://coub.com/stories/3949554-bluray-cat-god-dts-watch-online-full
https://coub.com/stories/3949555-mkv-narcos-season-1-free-dts-hd
https://coub.com/stories/3949556-pam-vel-branth-27-full-edition-book-epub-rar-utorrent
https://coub.com/stories/3949557-dracula-vel-in-full-book-mobi-utorrent-zip
https://coub.com/stories/3949558-bluray-band-baaja-baaraat-torrents-full-avi-watch-online-dvdrip
https://coub.com/stories/3949559-clave-x32-full-download-registration-windows
https://coub.com/stories/3950039-nemotec-64bit-latest-windows-download
nfpa 92b. nfpa 92b standard for smoke management systems in malls, nfpa 92b standard for smoke management systems in malls, nfpa 92a pdf download,...
marfed (Friday, 25 February 2022 08:49)
DraftKings and FanDuel: The two largest online sports betting. ... sisal champions league of legends offshore websites that offer sports betting Diretta calcio italia 458 serie a Maryland. ... Scommesse parma heights. ... Lorenza Fabrizia What is group b strep disease Uc sampdoria x benevento calcio Serie a klasemen. Bonus.... Check the best match plays and goals between Parma 2-5 Atalanta of Serie A ... Results, summary and postgame analysis Match ends, Atalanta 2, Benevento 0. ... Atalanta vs Real Madrid live streaming: Watch Champions League online... 67426dafae marfed
https://coub.com/stories/4004180-plate-n-sheet-v4-full-version-64bit-windows-iso-serial-build
https://coub.com/stories/4004179-official-asus-zenpad-10-z300c-p023-s-activation-pc-full-download-x32-rar
https://coub.com/stories/4004178-exe-fo-abg-bugil-rar-patch-windows-torrent-software
https://coub.com/stories/4004177-senthamil-fonts-serial-registration-file-full-version-torrent-windows-32
https://coub.com/stories/4004176-torrent-mooladhanam-rar-mobi-book-full-edition
https://coub.com/stories/4004175-do-aankhen-barah-haath-1-film-mp4-free-4k-torrent
https://coub.com/stories/4004174-download-darkroom-booth-registration-file-crack
https://coub.com/stories/4004173-full-version-simatic-s7-300-v5-5-build-zip-pc-patch-x32
https://coub.com/stories/4004172-wilcom-embroi-pc-free-exe-patch-latest-utorrent-key
https://coub.com/stories/4004171-the-wolf-of-w-watch-online-dvdrip-avi-dubbed-watch-online-avi-full
Parma's three-year stay in Serie A ended on Monday when they were ... Serie A has launched a new online streaming service that will allow fans to watch up to three matches each round. ... Tv Free WaTcH:Serie A Week 25 AS Roma Vs. Bologna Live Online Soccer Tv. Get ... Benevento (Serie A) on Watch ESPN. The Art...
bentsel (Friday, 25 February 2022 10:09)
Download Sailor Moon Full Episode, you will love it cos it is really interesting. ... Yoruba, Nigerian Films/Movies Download Sailor Moon Full Episode.3gp .mp4 .flv .3gpp ... Download Nonton Anime Jadul Sailormoon Episode 1 Sub Indonesia.... Download Pretty Guardian Sailor Moon Eternal: Der Film | Offizieller Trailer | Netflix ... Download [INDO SUB] SAILOR MOON ETERNAL THE MOVIE NEW CLIP.. Sep 4, 2016 Bishoujo Senshi Sailor Moon Crystal Sub Indo, Download Bishoujo Senshi Sailor Moon Crystal Subtitle Indonesia Batch 360p 480p 720p,... 67426dafae bentsel
https://coub.com/stories/3968476-free-igo-primo-exe-219-16-pc-professional-utorrent-activator
https://coub.com/stories/3968837-x32-easeus-data-recovery-wizard-technician-12-2-0-license-free-patch-rar
https://coub.com/stories/3968826-windows-au-sk-au-crack-activation-exe
https://coub.com/stories/3968542-free-fineprint-x32-utorrent-key-cracked
https://coub.com/stories/3966122-suzanna-perjanjian-di-malam-keramat-pc-nulled-utorrent-full-version-32bit
https://coub.com/stories/3966121-sonarworks-reference-4-studio-rar-full-64bit-keygen-activator-torrent
https://coub.com/stories/3966120-utorrent-winning-the-game-of-s-cks-adam-khoo-ebook-full-zip-pdf
https://coub.com/stories/3966119-school-of-money-by-olumi-em-uel-115-exclusive-pdf-book-zip-free-torrent
https://coub.com/stories/3966118-windows-solution-torrent-serial-rar-activator-32bit
https://coub.com/stories/3966117-aqib-jawahirul-ma-ani-rar-mobi-full-ebook-utorrent
Download Sailor Moon Black Dream Hole Full Movie play in 3GP MP4 FLV MP3 available in 240p, 360p, ... Sailor moon The movie sub indonesia 3 months ago. Apr 24, 2020 The first three seasons of the hit anime 'Sailor Moon' are now available to ... Watch the best Japanese movies and series with English subtitles on Netflix ... Download these free craft and colouring pages featuring the Tokyo...
comher (Friday, 25 February 2022 11:29)
3 game between the Ravens and the Cowboys has been pushed to ... Watch NFL Live Stream Online Free full games including Monday Night Football ... Live Stream, and all the games of Sunday Night Football at the LINK BELOW. ... the network's NFL coverage, including Monday Night Countdown and the NFL Draft.. Seven weeks into the NFL season, ESPN has made it clear it wants its three ... Stream live sports, game replays, video highlights, and access featured ESPN ... 14 @ 7:10 PM ET, ESPN) to begin a Week 1 Monday night double feature. like ... Baseball Tonight: Sunday Night Countdown. ... Enter your website URL (optional). 67426dafae comher
https://coub.com/stories/3992970-con-h-program-kerja-seksi-keagamaan-64-pc-full-version-exe-build-torrent
https://coub.com/stories/3992969-epub-problems-in-mathematics-by-v-govorov-299-torrent-book-free-zip
https://coub.com/stories/3992968-piste-5-05-64bit-full-version-exe-utorrent-keygen-pc-software
https://coub.com/stories/3992967-3ds-max-2011-pc-free-64-software-rar-activator
https://coub.com/stories/3992966-activator-w-boarding-1-2-2-download-pro-rar-64
https://coub.com/stories/3992965-motherma-dubbed-full-4k-dubbed-torrents-mp4
https://coub.com/stories/3992964-grand-theft-au-keygen-x32-torrent-full-activation
https://coub.com/stories/3992963-stag-sans-epub-zip-book-full-download
https://coub.com/stories/3992962-trigo-metria-leigos-free-zip-ebook-torrent-epub
https://coub.com/stories/3992961-subtitles-don-2-2011-mp4-dubbed-full-full-download
"9/25 WWE results in New York City at MSG: Bret Hart tribute night, Nexus vs. ... [dead link] ^ . ... Retrieved March 3, 2017. ... You used to watch him backstage and think, 'that guy is unbelievable', didn't you? ... ://www.pwinsider.com/article/101698/live-ongoing-wwe-payback-ppv-coverage-united-states-title- match.html?p=1 .. Get WeTV App to watch a full episode. CHUANG 2021. VIP Share. CHUANG 2021, produced by Tencent Video, is a variety show of an international boy group...
eerren (Friday, 25 February 2022 12:43)
The North Carolina Tar Heels are also referred to as the Tar Heels. The team has taken home five NCAA Tournament cups in 1957, 1982, 1993, 2005 and the... 67426dafae eerren
https://coub.com/stories/4014227-full-love-express-movies-mkv-blu-ray
https://coub.com/stories/4014228-thrigam-books-in-x264-free-full-1080
https://coub.com/stories/4014229-mobi-datasheet-str-w6554a-full-version-download-rar-book
https://coub.com/stories/4014230-torrent-fo-s-camila-flores-serial-pc-free-license-64bit-exe
https://coub.com/stories/4014226-c-of-duty-mo-utorrent-patch-ultimate-pc-32bit-free
https://coub.com/stories/4014223-lutron-homeworks-illumination-1-professional-key-serial-iso-free
https://coub.com/stories/4014222-rpg-robfeoy-ver-2-0-activator-full-version-rar-file-torrent-cracked
https://coub.com/stories/4014221-dual-thuppakki-blu-ray-watch-online-1080-free-torrents-dvdrip
https://coub.com/stories/4014220-torrent-sultan-the-warrior-mkv-torrent-full-blu-ray-full
https://coub.com/stories/4014219-epub-el-dinero-es-mi-amigo-phil-laut-12-download-free-zip-ebook
All posts tagged "North Carolina A&T vs North Carolina Central Crack Streaming Online Free | NCAA Women's Basketball". Sports6 mins ago...
gennwesl (Friday, 25 February 2022 14:00)
Avira Antivirus Pro 15.0.1925.1249 + Crack Free Download 2019; CCleaner Pro 5.57.7182 Crack + Keygen Free ... Audio Hijack (free version) download for Mac OS X Audio Hijack (was Audio Hijack Pro) drastically changes ... Version: 3.6.2.. Audio Hijack 3.6.2 - Record audio from any application.. Audio ... Audio Hijack Pro 3.3.7 is a powerful application for Mac OS X used for recording audio in any... 67426dafae gennwesl
https://coub.com/stories/4040000-keygen-scargar-torrent-registration-64bit-pc
https://coub.com/stories/4040001-full-do-gry-twierdza-krzyzowiec-extreme-license-final-utorrent-64bit-rar-windows
https://coub.com/stories/4040002-torrent-4-girls-fingerpaint-free-registration-x64-professional-zip-windows
https://coub.com/stories/4040003-soundforge-7-0-sony-mp3-plug-in-2-0-dubbed-avi-blu-ray-movie
https://coub.com/stories/4041023-csi-sap2000-registration-final-full-version-pc
https://coub.com/stories/4041025-pc-aimersoft-key-64bit-nulled-zip-torrent-final
https://coub.com/stories/4041026-baixar-interapp-control-pro-activation-build-torrent-pc
https://coub.com/stories/4041027-free-baixar-controladores-usb-barramen-file-windows-exe-keygen-x64-utorrent
https://coub.com/stories/4041028-abhay-torrent-watch-online-film-1080p
https://coub.com/stories/4041030-bukas-palad-tinapay-ng-buhay-torrent-pdf-full-zip-book
Dec 21, 2016 pavement crack or surface deterioration that ... (7) Sabotage, hijack incidents, and other ... must have Adobe Flash Plugin version 9 or higher, speakers, and sound. ... XIP and Mac OS X. Although it should work on other browsers and ... 3.6.2. Emergency Management and Communications (OEMC) Security.... Audio Hijack 3.2.2 MAC pliki uytkownika n_kristoff przechowywane w serwisie Chomikuj.pl Audio Hijack ... Apple iWork Keynote 6.6.2, Numbers 3.6.2 & Pages 5.6.2 ... DAEMON Tools Ultra v3.1.171 + Crack Mac OS X [cracK_brd] fixed.. Results 1 - 10 of 18 gacordtricwor/audio-hijack-362-crack-macos-macosx - Docker Hub. Celemony Melodyne ... Free Mac OS X Apps filtered by BlogStomp 3.6.2.
laurtevi (Friday, 25 February 2022 15:18)
Features Arcade (MAME 2003) Apr 02, 2018 Download the romset and extract it in MAME roms ... MAME ROMs MAME - MAME - Bios Pack - Planet Emulation. ... MAME 0.202 ROMs (bios-devices).zip ( View Contents) 11-Nov-2018 08:22.. rom pack download Free Download Download Playstation ROMs(PSX/PS1 ISOs ROMs) for ... Mame 0.161 Full Romset Pack (Split Alphabetically . ... file to run like Neogeo will need neogeo.zip (this is a bios file for Neogeo).. mame32 roms zip In order to successfully load zipped ROM sets in these locations you must specify the arcade emulator version which matches... 67426dafae laurtevi
https://coub.com/stories/3958693-full-picbasic-pro-3-0-7-pc-cracked-torrent-x32-activation-latest
https://coub.com/stories/3958692-movie-indian-orfanii-subtitrat-in-ro-watch-online-kickass-avi-subtitles
https://coub.com/stories/3958691-nijeke-ja-bangla-full-zip-pdf-book-download
https://coub.com/stories/3958690-preteendarkpthc-serial-activation-64bit-windows-utorrent-full-rar
https://coub.com/stories/3958689-t-pain-epiphany-full-zip-cracked-utorrent
https://coub.com/stories/3958688-crack-bdcompanylsmlsmo-professional-zip-torrent
https://coub.com/stories/3958687-license-c1240-k9w7-tar-124-25d-ja2-tar-hit-exe-cracked-full-version-build
https://coub.com/stories/3958686-navicat-premium-11-core-free-windows-x64-torrent-iso-keygen
https://coub.com/stories/3958685-rar-terjemahan-syarah-arbaeen-nawawi-utorrent-epub-book
https://coub.com/stories/3958683-iso-au-data-na-srpskom-free-license-ultimate-pc-patch
I found a rom pack at arcade punks that I am currently downloading called ... 56 In 1 Mame 32 0.119 Roms Pack Collection : Adventure; CPS1 Roms Pack ... is a dummy, just click on zip, brings up the whole list to download each one.. We continuously update our ROMS and EMULATORS to Download mame ... packs are compilations of every game in popular game series.zip bios also in this...
ardfol (Friday, 25 February 2022 16:28)
Shinobi life 2 shukaku spawn location. Free Repair Manuals for all Mercedes Models. Mercedes Workshop Owners Manuals and Free Repair Document.... Also Read | Shindo Life (Shinobi Life 2) Codes Apart from Shindo Life spawn time, we have mentioned their locations and rarity as well. Dual Raikiri: LVL: [720].... Code Shinobi Life 2 : How to Get Infinite Spins in Shinobi . Oct 07, 2020 s RASEN SHURIKEN RUSH SPAWN LOCATION Feb 08, 2021 If you don't know the... 67426dafae ardfol
https://coub.com/stories/3984624-kings-720-watch-online-avi-film-watch-online-utorrent
https://coub.com/stories/3984623-windows-star-trek-elite-force-2-torrent-final-free
https://coub.com/stories/3984622-dts-yatra-avi-4k-watch-online-720-full-avi
https://coub.com/stories/3984621-x431-master-rar-windows-utorrent-pro-serial-activator-32-full-version
https://coub.com/stories/3984620-rar-commercial-series-cps-r05-16-az-pmvn4082w-rarl-utorrent-file-free-activation
https://coub.com/stories/3984618-rockstar-mkv-1080p-download-dubbed-watch-online-torrent-blu-ray
https://coub.com/stories/3984617-rar-why-revival-tarries-free-mobi-download-ebook
https://coub.com/stories/3984616-ebook-99-name-of-ah-in-bangla-68-full-edition-download-zip-mobi
https://coub.com/stories/3984615-full-10musume-101111-01-64-download-license
https://coub.com/stories/3984614-book-ufacturing-tech-logy-by-hajra-choudhary-epub-full-version-utorrent
Link do discord - https://discord.gg/Pagq973 Shukaku Jin Spawn Location (Shinobi Life 2) Spawn time: 06:50 PM EST. Actions. Tyler renamed Su Tailed Spirit.... Shindo Life was rebranded from Shinobi Life 2 in November 2020, read more ... A: The Tailed Spirit (boss) spawn at specific locations and at specific times,.... Previous:Previous post:SHINDO LIFE SPAWN TIMES & LOCATIONS. Next:Next post:Roblox All Star Tower Defense Codes (December 2020). Naruto shinobi...
jaqulor (Friday, 25 February 2022)
Barton Zwiebach is once again faithful to his goal of making string theory accessible to undergraduates. Complete and thorough in its coverage, the author... 67426dafae jaqulor
https://coub.com/stories/4013682-mirrors-2008-activator-full-zip-torrent-pc-nulled-32bit
https://coub.com/stories/4013681-loc-kargil-dubbed-mp4-watch-online-subtitles-free-watch-online
https://coub.com/stories/4013680-the-mummy-1080-video-dubbed-dual-watch-online
https://coub.com/stories/4013679-aarambam-mp4-watch-online-bluray-4k-mkv-full-torrents
https://coub.com/stories/4013678-ultimate-keil-mdk-5-download-activator-iso-64-crack-windows
https://coub.com/stories/4013677-x64-fo-s-bianca-rinaldi-na-playboy-pc-download-crack-professional
https://coub.com/stories/4013676-free-w-street-money-never-sleeps-dvdrip-hd-dual
https://coub.com/stories/4013686-32-analisis-literario-pc-download-zip-latest-free-patch
https://coub.com/stories/4015357-sri-ra-a-gita-full-pdf-ebook-utorrent-rar
https://coub.com/stories/4010654-white-house-down-subtitles-hd-torrent-free-mp4-2k-watch-online
Jun 26, 2021 Barton Zwiebach. It features video lectures, detailed self-contained notes and assignments. Unfortunately there are no solutions available for...
dalmfari (Saturday, 26 February 2022 09:58)
Fully compatible with 32 and 64 bit DAWs (32/64 bit VST for OSX and Windows, ... Crack (Win) Download, Slate Digital Complete Bundle v2.4.9.2 Crack (Mac)... 31ebe8ef48 dalmfari
https://wakelet.com/wake/3T0JV53J6xEOyxgxRrVfH
https://wakelet.com/wake/yrFrSK2yDv7ny28o8bpc3
https://wakelet.com/wake/2ao0cyjKeAV7aDh1eB3OK
https://wakelet.com/wake/Q5qe13oYJJ4cfd-cm4f46
https://wakelet.com/wake/u7Wn-wWbBuito6bkZK21I
https://wakelet.com/wake/Tt6rvpJiXFhN6QqSyxRip
https://wakelet.com/wake/OsjTlOCszwP7zLpD_JhUl
https://wakelet.com/wake/0I_ZHnQwHYckFY3JNf5nk
https://wakelet.com/wake/5P9cSf3_YFbTct1Zgw8hS
https://wakelet.com/wake/5vHPcbyT68AERu9tMG66A
Slate Digital Complete Bundle v2.4.9.2 Crack+ Keygen Number Free Download 2021 Slate Digital Complete Bundle v2.4.9.2 Crack presents Virtual Recording...
https://community.tccwpg.com/backhenitti
opailia (Saturday, 26 February 2022 11:20)
... (Full Abacre Hote Management System v2.3.0.16 (Abaqus 6.12-1 + Abaqus 6.11-3 ... Pro Acebyte Utilities Pro 3.0.8 Acebyte Utilities Pro 3.0.9 Acebyte Utilities Pro ... Incl Keygen-Lz0 CPU Speed Professional 3 0 4 6 + Portable CPU-Tweaker 2 ... 1 1 Multilingual SoftPerfect File Recovery 1 2 + Portable SoftPerfect Network.... SoftPerfect Bandwidth Manager 3.0.8 With Crack SoftPerfect Manager:is a full-featured traffic management tool for Windows that offers cost-effective bandwidth... 31ebe8ef48 opailia
https://wakelet.com/wake/TuRLyY91Hnh32ns1huJLt
https://wakelet.com/wake/TQ8K_67uEABRUSTBBP8l8
https://wakelet.com/wake/FJMKKgvbt5QbnLcuIP9-w
https://wakelet.com/wake/yZ45MCA-ZujaE5MEQEwX4
https://wakelet.com/wake/A6pOb6kRxEmuV8ygfCZuF
https://wakelet.com/wake/pke4-uyungGw6JxNylZ6z
https://wakelet.com/wake/-VFzHLujHZFG0E3S4XwZM
https://wakelet.com/wake/RliYhBl0OKhs4HhkeOWam
https://wakelet.com/wake/kJvWAnvhkWIAbBzSHBM5B
https://wakelet.com/wake/dCAQlUAskQXzb6Z4LgSMf
Dec 6, 2020 We recommend interesting sports viewing/streaming and betting opportunities. If you sign up for a service by clicking one of the links, we may.... ... Adobe Premiere Elements 2018 v16.1 Multilingual macOS WiFiSpoof 3.0.8 ... SoftPerfect Bandwidth Manager 3.2.5 Icecream Screen Recorder Pro 5.20 +.... Dec 6, 2020 Las Vegas Raiders' miracle TD stuns the New York Jets: Recap, score, stats and more ... Ruggs III with 5 seconds left, lifting the Raiders to a wild 31-28 victory over the ... You can also get this game on Hulu + Live (free trial) or Sling TV ... Baseball games, live soccer and more on the new streaming service...
https://zeustee.com/tee/funny-unicorn-still-magical-shirt/
strraq (Saturday, 26 February 2022 13:39)
egyptian james herschel holden kris brandt. rhetorius the egyptian james ... James Holden Trans Astrological Pendium Of Rhetorius The Egyptian Pdf Download.. James Herschel Holden is Research Director of the American Federation of Astrologers and has previously translated Books 13-17, 19, 22, 23, and 24 of the... 31ebe8ef48 strraq
https://wakelet.com/wake/ijYLwsAq3kjZ-gfaS2uIq
https://wakelet.com/wake/OOVqIZ6Ue5EaQE-odq4tA
https://wakelet.com/wake/Q7LmwgU3xV3CXZKo68OvG
https://wakelet.com/wake/IHANeRx_QmnnIhOGo4u2Y
https://wakelet.com/wake/f2wygRxNTO4jxqqZqr1wD
https://wakelet.com/wake/P5tELnrloH6B9hzGwx_GH
https://wakelet.com/wake/iwsDjFvu2c69g0lK9_ake
https://wakelet.com/wake/9DI9bGHD8r9DZ_yvYRo5Y
https://wakelet.com/wake/iXpko-zQoApRaXgw8txsZ
https://wakelet.com/wake/2-BtK-XA5FJ1IVt-DwXhK
Download & View Best Books In Astrology as PDF for free. More details. Words: 4,376; Pages: 17. Preview...
https://neobicnobicna.com/u-potrazi-za-tobom-ili-za-drugim-delom-sebe/
neemmon (Saturday, 26 February 2022 14:56)
This page will provide information on how to set up your Easy Grade Pro student ... Click [Import from Another File] found at the bottom of the window.. The Razer Tartarus Pro Keypad has a smooth, convex joystick that is easy to slip off of. ... Razer Synapse Download for PC Download for Mac.. Select your MAC OS at the lop of the list. Canon My Image Garden 3.6.1 is available to all software users as a free download for Windows 10 PCs but also without... 31ebe8ef48 neemmon
https://wakelet.com/wake/981kkzJKhbYmkTYP9XtzB
https://wakelet.com/wake/oos9KLCsPPt_Sxtf_OuQw
https://wakelet.com/wake/jQ7wXi2qxPCTOT4quOlbf
https://wakelet.com/wake/gssRT3mQvumSBit8d7e-_
https://wakelet.com/wake/WuqOm4dRt_jUWb9pDanWI
https://wakelet.com/wake/M8peMz2HOFcA6xeUmfzbE
https://wakelet.com/wake/LX9ayWWPNSI2Y2x4gFv72
https://wakelet.com/wake/pq4uRvgZjUmjnv_mSyWfB
https://wakelet.com/wake/1vyIHAJIJvlnxQkpw08cZ
https://wakelet.com/wake/9rpwMc-hER9aJQO_t45pu
Create and share interactive reports, presentations, personal stories, and more. Sway is an easy-to-use digital storytelling app for creating interactive.... n-Track Studio for Windows and Mac free download. Record songs with a professional quality and easy to use music creation app. Turn your computer into a...
http://itoutsourced.co.za/index.php/component/k2/item/1
cerecla (Saturday, 26 February 2022 16:17)
Jul 27, 2020 UPDATE: The After Effects CS5 (10.0.2) update is now available. ... Color Finesse 3: Incorrectly accepted Color Finesse 2 serial number. ... Suite.13.0.1. ... Redgiant Automatic Duck Ximport AE Redgiant Automatic Duck Media.... HP LaserJet Pro P1102 Series Printer , 3 out of 5 stars from 4 genuine ... and can use it to create a standard sound using effects such as side-chain control. ... This code is extremely useful for audio songs combination. several giant firms use this ... Schutt Youth Shoulder Pad Collar 9.9 9.4 10.0 2: Schutt Sports Mid Fles 4.0.... The DMS AD docket number is in the form Docket No. ... The MLG system on Model A340-200 and A340-300 series airplanes is identical to ... Section 1.179-5T(c)(3) also discusses the effect of a revocation of an election under ... According to the 1995 RED for propamocarb hydrochloride (Estimated Usage of Pesticide, p. 31ebe8ef48 cerecla
https://wakelet.com/wake/vtXEwvEM9vsKlnw_xM7MA
https://wakelet.com/wake/fLDzxyRcMgvQsG97kP3hy
https://wakelet.com/wake/I_TlxoMhM9GD9casVdC3i
https://wakelet.com/wake/VDcWmP2V4dBA4Jej1WT0f
https://wakelet.com/wake/S2uM10dvCc7JvdGlJagtK
https://wakelet.com/wake/CA9sWGAyFyWhijOufK-FR
https://wakelet.com/wake/sGoD7uLJMIlEqfn9-O2pt
https://wakelet.com/wake/46tpZXp3LoNBDskhvIgXo
https://wakelet.com/wake/h7coJkxRDITDEQPhEim20
https://wakelet.com/wake/YPV3gmE0aRzpZfJkPVgSm
by F Garca-Vallejo 2016 Moreover Cytoscape v.2.63 was used to simulate the effects of viral cDNA ... lentiviral alter dramticamente, la topologa de la red de expresin de genes en macrfagos. ... The sequencing of the human genome revealed a controversial number of ... donors were taken and analyzed using GeneSpring GX 10.0.2 (Agilent).. by A ICAL Mercury is $2.00 per number and $12.00 per volume, postpaid. ... However, it was emphasized that theoretical calculations of the effects that changes in ... If it is assumed that the brightest stars are red giants appearing at B ~ 2i9J then with ... Radio Astronomy Observatory,~ Suite 100, 2010 North Forbes Boulevard, Tucson,.... by AP Biotas of Los Angeles County, Science Series no. 42, ... wear data reflect environmental effects, it is possible that ... Colors associated with pit numbers are as follows: orange, 61/67; red, ... example, La Brea has produced more giant short- ... Inc. version 10.0.2). ... Brea rather than Leidy's original suite of fossils.
https://studypal.in/template-excerpt-generated/
yasbene (Saturday, 26 February 2022 17:30)
... europe 30days album pro super beaver river dance ... miki asakura hero album avril lavigne first album cover at last the duets album ... album officialdism melanie martinez doll house full album download zip x ... untitled rar eric clapton blind faith well all right album blankey jet city ... 31ebe8ef48 yasbene
https://wakelet.com/wake/7smT3OLJr0_5V8IJ7AXq_
https://wakelet.com/wake/aO58sX9Sw8SEhSTDtl_qW
https://wakelet.com/wake/o_FbOXW2RFe2QH8YzKzG2
https://wakelet.com/wake/LMXtuNT-jgtQitboJFSYJ
https://wakelet.com/wake/QDInbmuqSS3xE5G0TXIew
https://wakelet.com/wake/484vKjiwqO4OjN-AIB8r_
https://wakelet.com/wake/KiVCfRph8p8weM6Y3sEeo
https://wakelet.com/wake/GksrFUMxnFgbgbXxwUp6B
https://wakelet.com/wake/TysT_hqh2Cxf4tyzusJHC
https://wakelet.com/wake/Lt7WNRxwzYk870F4tFQEl
... daily 0.5 https://www.kmart.com/millennium-leather-ap3312fn-zip-around-1-3- ... ://www.kmart.com/sony-playstation-98174-last-of-us-ps3/p-SPM7843564222 ... 0.5 https://www.kmart.com/liebermans-new-york-city-hudson-river-ny-poster/p- ... .com/pop-culture-graphics-dead-men-can-t-dance-movie/p-SPM8516050502.... I think I just turned a bull loose in a china shop. ga781207 -- That's the last time I take you to the grocery store, ... He was a famous mouser at a glass plant in Gas City, Indiana. ... ga810903 -- Maybe I could be as popular as Nermal if I learned to dance. ... ZIP! - Oh, very well, Garfield. - Have some bacon and eggs, . SPLAT!. 2.1 What the city affords: Sain's rappers and affordance at Kenji Station ... of street musicians (35 months passed between my first and last field diary entries). ... The Awa Odori was first introduced in 1957, and today over 150 dance troupes ... one of his favourite bands, the now famous Blankey Jet City, were helped along.
https://sfhpurple.com/62235
bailxan (Saturday, 26 February 2022 18:43)
Nov 29, 2012 Demand peaked this summer, when more than 400 people regularly sought shelter at night. City shelters overflowed to the point where people.... Jul 13, 2020 Roger Torrent: alleged attack confirms fears about Spanish state ... The popular messaging app claims more than 100 members of civil society, ... human rights activists in Morocco, diplomats, and senior government officials,... 31ebe8ef48 bailxan
https://wakelet.com/wake/1MBIm02IybvjkOS3xeQyt
https://wakelet.com/wake/yx8bglj760mJBZaz2GhVZ
https://wakelet.com/wake/VXJ3rdaZBy8fZv86XnH3M
https://wakelet.com/wake/NdAYd7vkvYOdmbIdSSYqO
https://wakelet.com/wake/Cq4sAR5kHQq17A7NlBEo5
https://wakelet.com/wake/1zSpDVEuJtTtmL17dzI8g
https://wakelet.com/wake/aomowQphKVafFeVQp9K5u
https://wakelet.com/wake/bajpHnxYe9UjFxQggKc9Y
https://wakelet.com/wake/ivanBdIjmUh6WYb6CO27M
https://wakelet.com/wake/srWKD51T8ruoocmxlVgOY
Oct 18, 2018 Hi, I analyzed data from human fecal samples generated with the 16s ... They are not the same thing, and more than one OTU will correspond.... Apr 27, 2010 "Even in our developed United States, water-borne diseases are far more prevalent than people realize. Tracing the sources of pollution so...
https://demonstee.com/tee/nazare-portugal-vintage-retro-surfing-shirt/
benjann (Saturday, 26 February 2022 19:57)
Oct 7, 2014 Searched on Google, problem not yet solved still. I could not find any working solution in Google search results. Also mailed to BlueStacks and.... Oct 5, 2017 Doing simple search across the library and it hangs. I have the zip ... Yeah, I actually guessed right with you using Bitdefender. Anyways it's.... Jun 19, 2018 Analyzing an Integer Overflow in Bitdefender AV: Part 1 The Vulnerability ... We rely of the security software to defend against attackers, so bugs in our ... instruction, another match table is searched for following instructions. 31ebe8ef48 benjann
https://wakelet.com/wake/pFSfR-g7vNnanB0_CkD5G
https://wakelet.com/wake/xT6JD62xbHxv_tu7N5Eo_
https://wakelet.com/wake/O301jHlvW4IdlaEoJD4XK
https://wakelet.com/wake/pmkvptcDJgUk68fQ60LFW
https://wakelet.com/wake/BbfqmCmWVVh8YBfMc48Or
https://wakelet.com/wake/drYHFF7eG4WDdFW222c0U
https://wakelet.com/wake/8RL97Qfpfj-EsBAkeJz1d
https://wakelet.com/wake/59mZlBun9UjlSEeufe-J6
https://wakelet.com/wake/JarBVFOPuo9HVBaegTDDJ
https://wakelet.com/wake/LCep3yK9ZPwD32f4lxGIe
Jan 26, 2013 is default settings for Bitdefender Internet Security 2013 ok ... but the Firewall is simply not upto the mark (if you believe matousec tests and also my ... I searched if zemana anti-logger is compatible with BitDefender in realtime.... dmp file shows up when I search my computer for "BitDefender". As you can imagine, the unrelenting error message is incredibly annoying and.... Sep 25, 2017 I've searched the internet but can't find an answer. Here goes: A problem has occured in BitDefender Threat Scanner. A file containing error information ... Threat Scanner.dmp. You are strongly encouraged to send the file to
http://cup.extreme-attack.eu/index.php?site=profile&id=1&action=guestbook&page=1&type=ASC
filimog (Saturday, 26 February 2022 21:15)
Mar 16, 2021 Locast Wrong City Error. JavaScript is disabled. For a better experience, please enable JavaScript in your browser before proceeding. Aug 20... 31ebe8ef48 filimog
https://wakelet.com/wake/1mbZXwzEvmiM5Nn5YSw-g
https://wakelet.com/wake/CFhIIKyqGeR--5lLeYgWP
https://wakelet.com/wake/VXr4TXYaFmLvhBXDlH0Cv
https://wakelet.com/wake/xMK2fVyItWESseaOQ407x
https://wakelet.com/wake/ob5lDLmRv6dpkMhq3bTEp
https://wakelet.com/wake/U9PTN2b-uOa-AxIpMJGBa
https://wakelet.com/wake/HW5OnoRz0Yl4pBVBnbY_2
https://wakelet.com/wake/DFiHDf9_pgJIX2ladHZvI
https://wakelet.com/wake/9ZdQw0JoaCCEldegcnYwT
https://wakelet.com/wake/-FW5hSnEAtoSd_kTbtVK-
6 Things to Know Before You Sign Up for Locast | Locast Review ... locast tv wrong location locast tv hack locast alternative locast wrong location error...
https://thefancypantskitchen.com/recipe/epic-mezze-platter/
shrunesb (Saturday, 26 February 2022 22:33)
14 games featuring romantic and queer content, including: 10 Visual Novels; 1 Arcade Brawler ...and 1 Shower Simulator! At over $130 value, the bundle's.... Jul 31, 2014 MAC takes on romance novels with the new MAC Novel Romance Collection launching August 21st! Fall in love with sultry shades of color that.... Feb 6, 2014 The main sure thing in a romance novel is the happily ever after. In those books, you can appreciate some of the same highs of true love, but... 31ebe8ef48 shrunesb
https://wakelet.com/wake/U-Y1-bNd1TIt_q0PukfoS
https://wakelet.com/wake/hON3GoVJZI1WVhNUDjpzU
https://wakelet.com/wake/UOHygqeUAUyS2G1RxrJwP
https://wakelet.com/wake/fQy2FJ4xreHgs9osmAKNo
https://wakelet.com/wake/Z0mafcSdEBUjcoxytbRXk
https://wakelet.com/wake/rAm7Wyccp23WqvcZNL1ZO
https://wakelet.com/wake/la8Im7Vt0D4i8fBdAxLdg
https://wakelet.com/wake/BJpAFfOV9at9WqjzKjoQp
https://wakelet.com/wake/4f3-sp-vhA5mfZn4L7395
https://wakelet.com/wake/mNg3__qOgJjW5nbPPXnJq
I gathered over 20,000 Harlequin Romance novel titles and gave them to a neural network, a type of artificial intelligence that learns the structure of text. It's.... Mar 8, 2020 Even those TV series that belong in different genres, such as drama or crime, fantasy or science fiction, usually feature at least one romantic...
https://www.simone.nl/nieuws/stem-op-de-vinyl-top-5/
weltali (Saturday, 26 February 2022 23:56)
Christmas photo newsletter template christmas newsletter templates free word. A christmas border with evergreen and berries. Nativity christmas card template for.... Free Christian Newsletter Templates Magdalene Project Org . Creative Church ... 5 Free Christmas Newsletter Templates For Church Christmas . Free Church.... Is part of free christmas borders for letters to send your letter this letter template gives you see more ideas about a festive twist on my packages to. Frame right plan... 31ebe8ef48 weltali
https://wakelet.com/wake/xU1dC_PB0FKlOzE4l94vf
https://wakelet.com/wake/etViyxdvJ3Tg6Zrni-OXh
https://wakelet.com/wake/fjhDvo9f5oH0Wv-vnEIQe
https://wakelet.com/wake/BEf5IFnll6auUSyKWXKVX
https://wakelet.com/wake/xp0f3EgqyWxD_yL5AU5IC
https://wakelet.com/wake/GR1tZeg1KpANylOK3KrAx
https://wakelet.com/wake/Yel813IQNeyMzcIvzUHZ7
https://wakelet.com/wake/2SRnT_zbKi3bMQfkLLaa_
https://wakelet.com/wake/6fdjn_DFExCDUir9xmnP7
https://wakelet.com/wake/Oro91w5ONZBWhU05FPT2Z
Beautiful Christmas Letters For Customers | What should I write in a business Christmas card? ... What do you write in a Christmas card to a client?,How do you wish someone a ... Free example No. ... Download New year christian messages. Christmas Letter Template Christmas Letter Template Free Christmas Letterhead Pinecones Ribbon Christmas Letterhead 8 5x11 80 Pk Christmas Letterhead...
https://khloemarin.com/gl/module/smartblog/details?id_post=1
pergil (Sunday, 27 February 2022 01:18)
Apr 16, 2020 Apowersoft Phone Manager is a fully-featured mobile device manager on PC, which can transfer and manage mobile data from PC or vice versa.. by MPHUM Veloso Cited by 125 An Application of the Noisy Channel Model: Spell Checking . . . . . 179. 7.6. A Second Application: Language Models for Machine Translation . 180. 7.6.1 Parallel... 31ebe8ef48 pergil
https://wakelet.com/wake/pwpO184LHfCW2STdBWwQi
https://wakelet.com/wake/Pczpq9fuSOWsCpyPBs-jA
https://wakelet.com/wake/yYtAJjbhuiSboufAkE8q3
https://wakelet.com/wake/j9zdFyt3513ftW-3_k2sJ
https://wakelet.com/wake/ldFmTTnY7ZmXEUgMErcri
https://wakelet.com/wake/rZtAl0M8clIRWz8cRQeTL
https://wakelet.com/wake/xng8dz-C0K295MRLud_8j
https://wakelet.com/wake/ZzF-Wp5vOZFBTOK8IL9ah
https://wakelet.com/wake/7IcGJHgTilRTwUTOyZN3Z
https://wakelet.com/wake/TsgqcyNiOK4ThzuWZa_kb
Jun 6, 2021 ApowerManager enables you to backup, organize, transfer and print contacts and messages from the computer without any hassle. iOS users.... ApowerManager is a powerful app that helps you to manage Android from PC with ease. It enables you to connect Android to PC via USB or WiFi. Once linked...
https://www.amelie-paris.com/fr/actualites/636_chagall.html
ivanfax (Sunday, 27 February 2022 02:37)
Astro Spectra Cps 5. 03 Rvn4183. It was created with astro photographers in mind, since it is quite common practice to treat astrophotos in this way before .. ASTRO Digital Spectra and Digital Spectra Plus UHF VHF 800 MHz Mobile ... 6880103W01 CPS Programming Installation Guide ... Software on 3-1/2 in. and 5-1/4 in. floppy disks RVN-4183 Customer ... Insert the command board into the PA accessory connector (J503) before inserting it into the RF board connector (P500). 31ebe8ef48 ivanfax
https://wakelet.com/wake/9yE4WRcnRpjtKPTn_xdLL
https://wakelet.com/wake/Gdi5MKmGTmRd0DJRRTbSe
https://wakelet.com/wake/h1zODi-nx6omgxVNsQ8_G
https://wakelet.com/wake/xaNtlHIpkMW8B9ZeHdUMO
https://wakelet.com/wake/fxJ7JXzADPK2p7YUMQb_K
https://wakelet.com/wake/lnao8wGHPB_5kldsluTOU
https://wakelet.com/wake/8cP1_SmGemkSy_hN8BsZX
https://wakelet.com/wake/QGMl9Bz4XrcL9TIb5X1ph
https://wakelet.com/wake/JK34Ze7-dASyYmcZJs3Hv
https://wakelet.com/wake/ZTJ735IaSEfUzwESkQxaT
Astro Spectra Cps 5.03 Rvn4183 35. Home Ham Radio Programming Radios Motorola RSS . CPS R06.02.03 PASSPORT . RVN4100 replaced .... RVN4183 (.... Dec 2, 2018 astro spectra, astro spectra cps r05.03.00 download, astro spectra plus, astro spectra cps, astro spectra programming cable, astro spectra plus.... May 15, 2018 Astro Spectra Cps 5.03 Rvn4183 https://tlniurl.com/1nyfmx. ASTRO25 Portable CPS R17.01.02 + Tuner R05.04.03...
https://www.organizeworkorhome.com/apps/blog/show/48546143-home-and-tornado-clean-up-?siteId=140823270&locale=en-US
jameiola (Sunday, 27 February 2022 04:01)
This tip is stellar in that it is part stupid frugal trick save money on texting from your cell phone by emailing for freepart productivity you can probably type faster from... 31ebe8ef48 jameiola
https://wakelet.com/wake/1du7ghDqYA-RZGQc-DVPd
https://wakelet.com/wake/eS36oxBTtlHFXrbJko-BX
https://wakelet.com/wake/_FA8uloN3GsKml_RrbKCp
https://wakelet.com/wake/LLKEJuYp3CBhk9piv57-D
https://wakelet.com/wake/lJH-EIIjw8LOiBEiI7JKq
https://wakelet.com/wake/LXfJxorYR2Ys8LhWTKCgS
https://wakelet.com/wake/my7c0Z957Vh-Drn4WA233
https://wakelet.com/wake/t_Dpm5BmPStt-ZucxEP-a
https://wakelet.com/wake/qqGDc2DE6EDxKtR4jnWfz
https://wakelet.com/wake/2G7F0H9xErz7EfA1yGBCJ
Display an image depending on that python script result. However ... Wifi: Kasa Smart WiFi 2 Outlet Outdoor Plug by TP-Link ($19. Home Latest Food & Drink...
http://sanaekainews.sblo.jp/article/60404091.html
egormarm (Sunday, 27 February 2022 05:24)
Dec 1, 2015 qaO9BqkjxFX3ZuoLu1lFR7yi8mtyu0,AQACAAE/FlogMF/21/. El-Goog! Central. hbzfev4o4cgfkimg.onion. Elaboration D mocratique d'une.... comment1, nutcracker lamp, 67940, free monogram fonts wedding, 925, sexy pics.pollyanna ... nudge friut, :[[[, an inspector calls act 1, :P, teen trauma cbt worksheets, fujj, horny afternoon ... 17 2554 21:47:34 ... metal rabbit, dragon, =[[, imgsrc.ru free password download, 607189, thomsonsweddings,.... dnia: 2018-06-09 21:47:58 ... A staff restaurant hot preteen lolita pics A bill passed in the Republican-led House would peg rates to the ... Get a job www.imgsrc.ru A second rescuer said the victim had suffered serious head wounds ... How much does the job pay? jailbait teen Private placements are generally done without a... 31ebe8ef48 egormarm
https://wakelet.com/wake/pqc1X6r4n1qU2vvRcFIyJ
https://wakelet.com/wake/usEjHgBoj_qYYXDNJejL1
https://wakelet.com/wake/7uKJGhLekkCAy-xGyeZ1n
https://wakelet.com/wake/L_DLHOVGzMpFgxgER8cS0
https://wakelet.com/wake/orPrAnvYcu05EdWK8gHG3
https://wakelet.com/wake/Jx8U_8oGVzcsKzS6-3ACi
https://wakelet.com/wake/0rKgPo7Qe4sQmQsgYl3vK
https://wakelet.com/wake/nWCG_miOfH94GK_65O9E3
https://wakelet.com/wake/62HB_XCT-RJg7H4HrxbSS
https://wakelet.com/wake/1bfGXyelQRGxRGHVj7UOJ
Kmart, Msn, Microsoft, Noaa, Diet, Realtor, Motherless.com, Lobby.com, Hot, ... Seixas Evoked Aeros Hobbit Opticians Mostar Teen Contingency Popularized Arable ... Accumulation 21st Compre Napoleon Whitey Holywell Glowering Sunflowers ... Shonna Desantis Signes Origami Pno Kaden Idee Imgsrc.Ru Thrills Pickerel...
http://itcapacitacion.cl/excelencia-en-el-servicio-al-cliente/
patrlaq (Sunday, 27 February 2022 06:48)
Spreadshop was the victim of a cyberattack on July 8, 2021. In an update posted to its website, the platform confirmed that personal user data, including bank.... May 15, 2018 Today I'll describe the 10 most common cyber attack types: ... There are different types of DoS and DDoS attacks; the most common are TCP... 31ebe8ef48 patrlaq
https://wakelet.com/wake/lu5eM1Z1_hO_1MohX0k_q
https://wakelet.com/wake/HjsKhBIJu_Padbg45h7fl
https://wakelet.com/wake/coECFO8tqQ0ObG8s5ZPel
https://wakelet.com/wake/VLwSd7ARUbrajokH6UjUP
https://wakelet.com/wake/C9hVrcWbvPvio_7op2yZt
https://wakelet.com/wake/4HAq7NLO0U5DofZkXQOhT
https://wakelet.com/wake/NxMLm2B1khpH52O1ELh72
https://wakelet.com/wake/5JZHxpnDhbr05ePedltxN
https://wakelet.com/wake/Vh-5AyEdeAphoZNs-W9Wt
https://wakelet.com/wake/DD_Q27tGPDR29GnThIj5R
Jun 22, 2021 Such close calls ratchet up fears about how vulnerable the nation's infrastructure is to cyberattacks. Experts said there are more to come and.... Jun 7, 2021 The last few months have seen a sharp rise in cyberattacks, often ... "Today we announced the seizure of millions of dollars in bitcoin paid by an ... out of the G7 and NATO summits, Sullivan said he hopes there is the start of...
https://donlighting.com/product/torno-table-lamp/
patrlaq (Sunday, 27 February 2022 06:48)
Spreadshop was the victim of a cyberattack on July 8, 2021. In an update posted to its website, the platform confirmed that personal user data, including bank.... May 15, 2018 Today I'll describe the 10 most common cyber attack types: ... There are different types of DoS and DDoS attacks; the most common are TCP... 31ebe8ef48 patrlaq
https://wakelet.com/wake/lu5eM1Z1_hO_1MohX0k_q
https://wakelet.com/wake/HjsKhBIJu_Padbg45h7fl
https://wakelet.com/wake/coECFO8tqQ0ObG8s5ZPel
https://wakelet.com/wake/VLwSd7ARUbrajokH6UjUP
https://wakelet.com/wake/C9hVrcWbvPvio_7op2yZt
https://wakelet.com/wake/4HAq7NLO0U5DofZkXQOhT
https://wakelet.com/wake/NxMLm2B1khpH52O1ELh72
https://wakelet.com/wake/5JZHxpnDhbr05ePedltxN
https://wakelet.com/wake/Vh-5AyEdeAphoZNs-W9Wt
https://wakelet.com/wake/DD_Q27tGPDR29GnThIj5R
Jun 22, 2021 Such close calls ratchet up fears about how vulnerable the nation's infrastructure is to cyberattacks. Experts said there are more to come and.... Jun 7, 2021 The last few months have seen a sharp rise in cyberattacks, often ... "Today we announced the seizure of millions of dollars in bitcoin paid by an ... out of the G7 and NATO summits, Sullivan said he hopes there is the start of...
https://donlighting.com/product/torno-table-lamp/
kamaelyo (Sunday, 27 February 2022 08:15)
Jan 14, 2021 A colossal treasure trove of Warhammer audiobooks. ... As with the other compilations the Warhammer 40k 8th edition Chaos Space Marines.... ... Trine 4: The Nightmare Prince, Tropico 5, Trove, TUG: The Untitled Game, Turok ... Warhammer - Vermintide, Warhammer - Vermintide 2, Warhammer 40,000:.... Results 1 - 48 of 53 ... of a trove of documents Taran Tactical had shared a previous video ... Blood Angels 40k Tactics: Death Company Warhammer 40k Tactica... 31ebe8ef48 kamaelyo
https://wakelet.com/wake/SIz-vRJeL2Mfw6wgYu4UO
https://wakelet.com/wake/CIJxXb_KtFcvlqUMQuDD6
https://wakelet.com/wake/KoAeGfKIHnM3WNZRrMRvj
https://wakelet.com/wake/uo5C_NSP61vqcIEk5mqGV
https://wakelet.com/wake/WBGXJ25KtA9j_-DUWtejk
https://wakelet.com/wake/XMDL4wap8xU7qMOfW9_ef
https://wakelet.com/wake/31Usi37z6LatOtGIZJ4Qi
https://wakelet.com/wake/FJmDkbSv7szR3pohYANAO
https://wakelet.com/wake/ziVsZ6IkbZXBl_tbH1A_q
https://wakelet.com/wake/5uZo0FSh14mNULReTLzOn
"warhammer tomb kings" 3D Models to Print A full set of 10mm Miniatures to be ... Giant Find everything else tagged 3d-print like Ritual Casting Trove, Ritual Casting ... Tomb Kings Top 16 WARHAMMER 40000 STL 3D PRINTING FILES...
http://beatricehoward.com/an-intensive-study-into-neck-vaginas-aka-v-necks/
tricha (Sunday, 27 February 2022 09:42)
Jun 14, 2013 So a few weeks ago I decided to get the girl's bedrooms ready for summer. Toward the end of the school year things really moved into high... 31ebe8ef48 tricha
https://wakelet.com/wake/HcUERFZyjI7Hek9G8SOLU
https://wakelet.com/wake/RhmXB-v_n9cVHsjoYpm3R
https://wakelet.com/wake/-nh0yMExr6sbi1dhGmbVR
https://wakelet.com/wake/lbF7teUSAP5AL5JKueDNb
https://wakelet.com/wake/ECXocYpND-MIkGYDZzTrD
https://wakelet.com/wake/-ZyCiznrpwq47Ac3VgtRD
https://wakelet.com/wake/8B0IaU9aeM8vlEfl89DOu
https://wakelet.com/wake/0URMfwBBe_ptbRqCx-HyY
https://wakelet.com/wake/Vq7RM0T8gukf9e5rHjo5Z
https://wakelet.com/wake/EvEFe8nRywHEJYySA6EV6
Feb 3, 2021 23, 24, 25, 26, 27, 28, 29 ... Free and funny birthday ecard: 40 is the most beautiful age of all. ... If you are looking for a happy birthday wish for your niece then you are ... Happy birthday to the woman whose love, care and kindness played ... Today we are about to celebrate the most beautiful girl's birthday,.... Jun 22, 2020 screenflow for windows cracked. ScreenFlow for PC Windows Download ( Recorder Screen video Free ) ... Read more. Categories Mac, Windows Tags camtasia, screen recorder for pc, screenflow 4, screenflow 7 (download),...
https://pelaburemasperak.com/25-best-collection-decorate-bakers-rack/browse-bakers-rack-vignettesvignettes-bakers/
glynama (Sunday, 27 February 2022 11:00)
A software upgrade fixed the problem. Instead, if you get hit by some moron who was too busy texting, a software upgrade won't prevent that from happening.... Oct 12, 2020 1999 Toyota Camry is a reliable family car that has earned its good ... soft front seats, timing belts, and an upgraded sound system.. Jan 18, 2021 How will I get information updates on weather, sports, ... We recommend using latest version firmware toyota camry software update device. 31ebe8ef48 glynama
https://wakelet.com/wake/2Uno8q76AvNcg1Mouh1SJ
https://wakelet.com/wake/giCLCnEdPJ9BtHyZJorOM
https://wakelet.com/wake/datJQrkiwGy4ie7XPYVVO
https://wakelet.com/wake/vnvKXjbAnvbFN6w8CPnsr
https://wakelet.com/wake/lPBow_p5v2BUF9kO5o_J5
https://wakelet.com/wake/IdTbi9dtjOss73jtoiTeG
https://wakelet.com/wake/h4VcOCT6nitB0E_uI7y8n
https://wakelet.com/wake/-fVTIb2njyANmy-ccoxAU
https://wakelet.com/wake/qRvhfG7T3BS79KiZJMkCb
https://wakelet.com/wake/edpGkYt6TtQdGbc2eNNqE
May 7, 2019 Piggybacking off of this Post here.... Here is a link to the Apple Carplay FAQ and 3 TSB's. The TSB instructions are based on what model of...
https://lipstee.com/trending/be-kind-rewind-shirt/
kalxito (Sunday, 27 February 2022 13:31)
PDF | A research project on the Indonesian ulama gave me the opportunity to visit ... 1950s, Al-Ma`arif followed suit with cheap prints of oft-used kitab, and so did `Abdullah bin ... [18] At present their books do not receive a wider distribution ... observation (1899: 142) that Ibn Hajar al-Haytami's and Shams al-Din al-Ramli's... 877e942ab0 kalxito
https://wakelet.com/wake/Eg9V5utiIcTH8L_e-F7id
https://wakelet.com/wake/fXIvf0xfHUIVK3pxRmt68
https://wakelet.com/wake/9td9n-1zSrPpXVtJPdvfm
https://wakelet.com/wake/-g_oe0ISvLlYHoxaPvAYR
https://wakelet.com/wake/in0w3VKkvY-k_6XCcIJlr
https://wakelet.com/wake/Oaz8gyST4p91PH17RMYOD
https://wakelet.com/wake/mTcH1G9hXmRxOalrrPxS-
https://wakelet.com/wake/wPr6iUX9QDjAZaGNuxFZ4
https://wakelet.com/wake/IFmgA2s1gw5p6DXQ1HiiM
https://wakelet.com/wake/WvOHebroTtkzvQrryqMqq
... Shams Al-ma'arif Al-Kubra (Turkish)/ 27-Sep-2019 10:36 - Shams al-Ma'arif (Printed ... Grimoire.pdf 27-Sep-2019 10:34 891K Al.Toukhi-Red.Magick.pdf 27-Sep-2019 10:34 18M Aleister Crowley - The Book Of The Goetia Of So. ... 10:35 95K al-Buni - Shams al-Maarif - Manuscript 1500.pdf 27-Sep-2019 10:35 467M...
https://xiangyue.homemom.ca/en/album-video-each/922?page=1262#comment-144698
ikeesap (Sunday, 27 February 2022 14:47)
Jul 7, 2008 "Did Crusader ever print or post a basic fuel burn/rpm curve for their ... You can calculate what the 'ideal' fuel consumption would be.... Jun 18, 2014 ... point of maximum fuel efficiency is typically at or close to idle speed. ... could just pick your poisonchoose a speed-fuel consumption figure... 877e942ab0 ikeesap
https://wakelet.com/wake/y4ymWYXMqjAYGRga8xIPN
https://wakelet.com/wake/UI9i5USaL-T9Onep-9Tjw
https://wakelet.com/wake/z5-3x86mJM2Qh7F7Ql9cf
https://wakelet.com/wake/wWIPNmcwvRV5A3ztbfscG
https://wakelet.com/wake/yEPF16KGllTYQBPrTzEpV
https://wakelet.com/wake/jR9aIlJ4GQrgrjuudw6-s
https://wakelet.com/wake/iWlLJA9QBcTHAQweuXyD1
https://wakelet.com/wake/s0G_xTfuelFLso_UK8khN
https://wakelet.com/wake/buKn5GljrtLveI9bBLXlI
https://wakelet.com/wake/xCIrnlxyRsZB1y-8ZM9hG
Boat House Bulletin tests of Stingray boats, performed by MerCruiser. ... Use our Performance Calculator at StingrayBoats.com/performance to compare over ... Our database contains both performance and fuel efficiency test data from engine.... Sep 28, 2020 However, boat fuel consumption has more variables than cars and is harder to calculate. Fortunately, Mercury has done a lot of the hard work in.... Dec 3, 2020 Inboard: mercruiser volvo penta diesel marine engines. calculating fuel consumption | boat gph. I have smartcraft on my boat so i know my...
http://rudolfsfogado.hu/index.php?option=com_easybookreloaded
uryreyg (Sunday, 27 February 2022 15:59)
Watch Online Movies Hindi Best HD Print Clear Voice DVD Video, Watch Bollywood ... The Pushkar Lodge (2020) Hindi Full Movie Online Watch DVD P... Latest entertainment news and gossip from the world of bollywood, Hollywood and regional film industries. Get the latest celebrity news on celebrity scandals,... 877e942ab0 uryreyg
https://wakelet.com/wake/uc7-12yfOiGBzgnLi_Aqq
https://wakelet.com/wake/h_1SVqu6hodzUfiybL_jo
https://wakelet.com/wake/GtDKwbUXwwCFaqt1YqNho
https://wakelet.com/wake/IwrAy7ehDrGXclKxwEeFy
https://wakelet.com/wake/EqMRWI97zz60p6cZ1nOIw
https://wakelet.com/wake/Bmy-s8FVZMtABCRV6ceXg
https://wakelet.com/wake/ANUagdNnSelhuWJuQhB3b
https://wakelet.com/wake/ZYEpTISKKi3tkfdhSSTPG
https://wakelet.com/wake/VqCeEyDVOkjX3NDVDNSng
https://wakelet.com/wake/JQKuTvackT597I3n3gOp6
Shankar Shambhu Songs Download- Listen Shankar Shambhu MP3 songs online free. Play Shankar Shambhu movie songs MP3 by Asha Bhosle and...
https://www.evaluateitbysqm.com/blogs/item/30-save-when-you-shop-at-the-outlet-malls.html
kaulche (Sunday, 27 February 2022 17:15)
HMH Growth Measure is the adaptive and reliable assessment that connects data insights with best-in-class core and supplemental programs. When benchmark.... This section is available only in the 'Complete Report' on purchase. Know your weaker and stronger sections by attempting CMAT practice tests. Please fill out... 877e942ab0 kaulche
https://wakelet.com/wake/wshsE3mOqjuAOpYWk2UzN
https://wakelet.com/wake/2G1vk2kjQZgZuIqjKOxFE
https://wakelet.com/wake/gGHuJ5iaB2lb_4jE6Juh7
https://wakelet.com/wake/oqlYD5mqPZYWa87BbwyeY
https://wakelet.com/wake/eFQtDTDju3qnZR6u2e8Mu
https://wakelet.com/wake/3JDsg4z7LF8Xq3Lii0_gR
https://wakelet.com/wake/xiLEkNtIZSQ_P_quKqKMM
https://wakelet.com/wake/0nYK5YB6-sJETgL086yrp
https://wakelet.com/wake/up6ikYzclApjAdCqkyiCI
https://wakelet.com/wake/Mok7GNwhvfpCDKYIUxq0_
Listening and Reading Assessors use a detailed marking guide which sets out which answers receive marks and how the marks are counted. Assessors use this.... Quarantine Edition 2020. How to clear ... Assessment Test Answers Read. More ... Best Buy,. M... What type of answers are employers looking for during a .
https://inada.ocnk.net/bbs
phembir (Sunday, 27 February 2022 18:28)
That's why I've put together a list of some of the best German storybooks for those ... 280 pages of unconventional German short stories that are perfect for A1-B1 levels. ... Imagine reading a book and coming across the word Schneeeule.. It covers lexis and grammatical structures of the upper range of B1 and B2. More information on telc German exams for medical professionals and examination.... DOWNLOAD THE KEY WORD LIST FOR PART 6 OF THE B1 READING. B1 EXAM LIST ... DOWNLOAD THE OPEN CLOZE EXERCISES IN PDF: Fill in the gaps... 877e942ab0 phembir
https://wakelet.com/wake/o1slqBTskW2ZjrTSEd18P
https://wakelet.com/wake/OAPtloRBUndbPvvjKJJK9
https://wakelet.com/wake/K8R1P0f6WW8MOR-0FNBnm
https://wakelet.com/wake/wMFovbP3qO1_nG6IIhGGE
https://wakelet.com/wake/YYVhafgeKlpLqOxjvYz0q
https://wakelet.com/wake/SBp8ZcKrh0MZzDf0BRY5d
https://wakelet.com/wake/MfboY1IF4H8JnXBQHjR-d
https://wakelet.com/wake/W_nLBYogpUVq1ugMvWCTb
https://wakelet.com/wake/eOCH9UBRw9vRjQ0I-nTRN
https://wakelet.com/wake/O2g_sRtU6KH9ae7Lp8Sl0
For a list of country-specific documents that may be requested in addition to those indicated ... Complete, literal word-for-word, line-by-line certified English translations for all ... Any emailed documents must be submitted as .pdf attachments (not ... German. Graduation Timeline. 4 + 4 or 5 + 4 or 5 = 12 or 13. Timeline varies.... May 29, 2021 Download Vocabulary List now PET (B1) Email This BlogThis! ... you with downloadable PDF worksheets and keys for vocabulary at the B1 (Intermediate ) level. ... B1 German Nouns Eng->Ger->Eng. Gravity. achieve. ... All the words in this section are in the Cambridge PET word list. advantage. afford.
https://www.thesureword.org.uk/component/k2/item/135-developing-effective-interpersonal-skill
mohanny (Sunday, 27 February 2022 19:46)
May 26, 2021 Link live streaming pertandingan lanjutan Serie A Italia giornata ke-31 ... Live Streaming Inter Milan vs Hellas Verona Matchday ke-33 Serie A Italia ... Inter Milan LIVE STREAM (6/13/20): Watch Coppa di Italia, leg 2 online | Time, ... Juventus,Barcolone,Inter milan, Milan, Tottenham Hotspur FC Bayern.... 2. advertisement Parma vs Inter Milan live stream 00:00:00. June 28, 2020 2:00 pm. Goal.com News. Sunday's Serie A predictions including Hellas Verona vs.. Parma (Serie A 2021) Start time : 2:45 p.m. EST TV channel/schedule : N/A - The match isn't ... Share this article 131 shares share tweet text email link FTW Staff. Watch Parma vs Inter Milan live streaming The Internet provides access to ... Parma FC - Inter Milan match for Italy: Serie A starts on 04/03/2021 at 19:45 UTC/GMT. 877e942ab0 mohanny
https://wakelet.com/wake/N9cUSka9C4zvg4GkUQPYz
https://wakelet.com/wake/LV2vGUN3wX8u1gpP3sJHW
https://wakelet.com/wake/kGAY-PEkT5vyPlPI0VQK5
https://wakelet.com/wake/0pPrEiM5GyQEX4AphaPN-
https://wakelet.com/wake/m0F4o2ugrQGGHCoy-ZDJx
https://wakelet.com/wake/YyY748y01psD4z-hMx2XR
https://wakelet.com/wake/24sI_dw_looT4sCnUErJU
https://wakelet.com/wake/k7Q1aT_c89R2rvzGfSyE_
https://wakelet.com/wake/zHajUIRsV5Ra_0SWxC8iw
https://wakelet.com/wake/khKX3_rsJF5wo7hUudn80
0 AC Milan FC Crotone. l Hellas Verona vs FC Crotone - 2:1 Draws Serie A 17/18 ... 40 Berikut link live streaming tv online Inter Milan vs Crotone Serie A Liga.... Feb 24, 2021 Manchester City would get 12M from Hellas Verona for Ivan Ili if the Serie A side ... and subsequently loaned him back to the Serbian club for the following two seasons. ... You can follow us for live updates here: @City_Xtra.. All Euro 2020 tournament mathces live links available 30 minutes before kickoff. ... Stream Hellas Verona vs Lazio live on SportsBay Start time: Sunday, April 11, ... Juventus vs FC Porto: The match will be played on 09 March 2021 starting at ... Inter Milan Jauh di Atas Juventus Prediksi AS Roma Vs Lazio: Adu Gengsi 2...
https://www.amelie-paris.com/fr/actualites/336_la-renaissance.html
kamavalo (Sunday, 27 February 2022 21:04)
iMGSRC.RU host presents Free collection photo / page #114. ... johns2014: Random pix ze, 12, collection, 0 / 61028, 0, 0, 6 years ago. blagoroden_don:.... Dutch replied to Dutch's topic in XVM: English support and discussions ... load: [cfg]/Aslain/minimapAlt.xc 2020-04-10 22:28:11: [JSONxLoader] load:.... Fotki, Estonia / Fotki, Inc. Free registration photo sharing service and communication portal. Yes, Yes, 1,250,000, 50MB for free, unlimited storage for $30/year.Missing: dutch, dutch 877e942ab0 kamavalo
https://wakelet.com/wake/lAK2TZdPEvMLHvg7408BA
https://wakelet.com/wake/C5ZXXF36A6lLRipzeKAL1
https://wakelet.com/wake/bc2gY6XjKqyyDGwOYddLz
https://wakelet.com/wake/nZ74QWtSX9-S-Un_IJffk
https://wakelet.com/wake/ojQtV0gtgmNR5oUsTihHc
https://wakelet.com/wake/s5Won8kQPuic-KkbynrIY
https://wakelet.com/wake/zB2Eh80FO6_bCeEhhjUeL
https://wakelet.com/wake/hvVPP-eCroeNJxqNHEFHW
https://wakelet.com/wake/7B-cnaPY4gVKbbE4wuYCM
https://wakelet.com/wake/LYNHTWxo3vIHGLGdaU20L
Jun 20, 2021 Razgovarajte s nama! vjebenica, gramatika i fonetika hrvatskog jezika ... Download pdf - 1empower a2 elementary workbook [z0xj86yopjln].. a random dutch angel dragon. __FusH__. 10/02/2017 23:04. 1 Like. Favorites. Continue. idk,,. Share:
http://www.radiobez-b.ru/component/kide/-1
orctras (Sunday, 27 February 2022 22:19)
65 Products Download File PDF Coleman Mach Air Conditioner Manual 4800 Series ... Jul 16 2017 My roof mount Coleman TSR Mach 3 AC unit has a bad... 877e942ab0 orctras
https://wakelet.com/wake/eA-kfKNtpntXWyZHulYUJ
https://wakelet.com/wake/0cCEfKbADbMEygAMJtD3y
https://wakelet.com/wake/qku65m_Q2Uc7ilvO8neFW
https://wakelet.com/wake/va80z71mkeEUcf9I-QziJ
https://wakelet.com/wake/JRAuNKIeq7VW8Stywqv6b
https://wakelet.com/wake/lQtpKuE0ezCzjJpVBde3p
https://wakelet.com/wake/869llUSdiVeZLujb-L4L1
https://wakelet.com/wake/JYKxQ4e7GTYsUQmiMfwH3
https://wakelet.com/wake/AffJJi6bT6LHjzto3vfiS
https://wakelet.com/wake/yWRYim8G2Wk_9RNXCN5P4
Jan 16, 2018 Read Book. Coleman Mark. Air Conditioner. Manual money for you worth, acquire ... Manual install Changing. A Coleman Mach. Air Conditioner. On A RV Coleman. Mach 8 A/C and ... Coleman Tsr Rv. Air Conditioner. Manual.... Results 1 - 10 of 10 User manuals, Coleman Air Conditioner Operating guides and Service ... TSR Keeps weather, dirt and tree debris out of RV air conditioners...
https://scandinavian.network/ceigonetsbank
georgert (Sunday, 27 February 2022 23:36)
Shop low prices on groceries to build your shopping list or order online. Fill prescriptions, save with 100s of digital coupons, get fuel points, cash checks, send...Missing: Sweet boys @iMGSRC. 877e942ab0 georgert
https://wakelet.com/wake/Yn8UogwjTEbJKqGVGsQ6s
https://wakelet.com/wake/YC4BbP47qH_zWg53WGBdl
https://wakelet.com/wake/9_BlotGF2Cm2WjyAObsEa
https://wakelet.com/wake/uf9gR_6UuJu5PbiDNAEKL
https://wakelet.com/wake/rLT2qYCiYinq1WqE2fT3j
https://wakelet.com/wake/FPHaL-I17JHG59re67oR0
https://wakelet.com/wake/xkLxlST2KelTZLUbMBCy5
https://wakelet.com/wake/lsLUccqwFCabvGjt1CepH
https://wakelet.com/wake/tNYDRd97DkCd5UHJy_PBT
https://wakelet.com/wake/VTVt9YSxKQV2X1CfAMp0t
Our etched glass mugs are a perfect way to show that special guy or gal that you ... Rendered in 3d Max 10 Post Work in Paint Shop Pro 7 Mass Effect is (c) By ... Mass Effect 3 Gamer.ru: ... 1 N7 Training 2 Equipment 2.1 Armor 2.2 Weapons 3 N7 Special Ops 3.1 N7.... Apr 8, 2014 And feel free to grab the one below it so that more people come party with all of us! ... href="https://www.wineandglue.com" title="Wake Up Wednesdays Features">
https://gardenlocked.com/dramwindzisla
philmarm (Monday, 28 February 2022 00:54)
Oct 27, 2010 Android Native Development Kit Cookbook eBook Packt. ... Book Cover of Joseph Labrecque - Flash Development for Android Cookbook .19.... Apr 5, 2021 Google sought, through Android, to develop a software plat- form for mobile ... categorizes books into an accessible system or a travel guide that arranges ... recipe in hand, the robot then moves to your kitchen and gives it to a... 877e942ab0 philmarm
https://wakelet.com/wake/C4HRr8FHdy2_KnNqqxnuJ
https://wakelet.com/wake/5braUz93_M-FHhTvf5F64
https://wakelet.com/wake/QFUpPBjW8IYFJQWNvtnSn
https://wakelet.com/wake/-FC03c5KL79WBfIgmtq8Z
https://wakelet.com/wake/60dTAcx7fjdExfkGCgbxb
https://wakelet.com/wake/zGXRP-iFnOjduHXRKdtrr
https://wakelet.com/wake/J6jHxc3k4gK-k_B4fj9So
https://wakelet.com/wake/dGE6Tzb2BYyBZ1fdTsvCJ
https://wakelet.com/wake/DKmGveyXoI1835vCPMiCq
https://wakelet.com/wake/Iol0LCQqlmFzqpNgzyNQw
Reto currently works as a Developer Advocate on the Android team at Google, helping Android ... Manual Thread Creation and GUI Thread Synchronization ... alerts, cause vibration, and flash the device's LED, as well as control status bar...
https://seesaawiki.jp/bautatockstic/d/burny%20serial%20number%20check
stanmal (Monday, 28 February 2022 02:14)
Orlando Magic vs. Oklahoma City Thunder Date. January 22, 2020 Event Starts. 7:00 PM Ticket Prices. Get Your Tickets Now! On Sale. On Sale Now Parking.. Video orlando magic vs oklahoma city thunder live stream - Nghe nhc remix, nhc cover hay ht - Nghe Nhc Hay l ni chia s nhng video nhc Remix,.... NBA FRee Oklahoma City Thunder vs Orlando Magic Live Stream NBA Online HD Coverage TV. basketballcoverage-blog.blogspot.com/2011/12/watch-oklaho. 877e942ab0 stanmal
https://wakelet.com/wake/aPJk94o7Kwkh6zBTx5efI
https://wakelet.com/wake/6QWss2NBSezUlHvXtpDfO
https://wakelet.com/wake/kAs9wsDuLt0rzaHv08IAL
https://wakelet.com/wake/jLJC5n37VnleCiqn_05Lb
https://wakelet.com/wake/jlYkmQ7JC5s7bhoYexa-3
https://wakelet.com/wake/CR62FUMZ0giZLHsDGzL-K
https://wakelet.com/wake/v3WUjnwuk_n4PUEPCwXNl
https://wakelet.com/wake/G4zPEpcOmHq-LcJ0O3Fy9
https://wakelet.com/wake/VH_aPiNJYBwJHgRJP3WVF
https://wakelet.com/wake/hM_vMgZxEDlFyyaRuQl9t
Oklahoma City Thunder vs Orlando Magic h2h (2020/12/30) on AiScore Basketball Livescore. ... Match Live. Overview. Chat. Box Score. Odds. H2H.. LIVE Orlando Magic vs Oklahoma City Thunder LIVE | EN VIVO NBA live stream NOW TODAY live | Oklahoma City Thunder vs Orlando Magic live stream NOW.... Live Streaming Oklahoma City Thunder vs Orlando Magic - NBA #LiveStream > Go Live Now :[[ https://is.gd/IVb6zB ]] #nba #LIVE> Date: Today, 1/2/2021.
http://www.reo14.moe.go.th/phpBB3/viewtopic.php?f=6&t=2156189&p=3349978#p3349978
tiblav (Monday, 28 February 2022 03:30)
May 3, 2021 KIK Friend Finder Features It couldn't be easier to find new friends on Kik Messenger ... Simply search for online users on KIK and start chatting.. ... Hot Live Show Online Generator. Find Kik, Snapchat usernames & more! ... How Truecaller Impacts the World. News, email and search are just the beginning.. Stay fresh on the newest features, tips, and bots in the Kik blog. Step 1: Tap ... They were simply running wireshark, found your IP address and ran a lookup on it. 877e942ab0 tiblav
https://wakelet.com/wake/x77dvKwoSl1Hav2nmWLoH
https://wakelet.com/wake/l_CAhV7p-Hrgr2eDhjkqR
https://wakelet.com/wake/Aow-50-BZYYNXi3fTUO7F
https://wakelet.com/wake/GRxcJWIGqXAAXzJJEqIdl
https://wakelet.com/wake/y6xNI54A1-3XNeBdFLg0E
https://wakelet.com/wake/5KFFkrnrG1w01thEjV9TM
https://wakelet.com/wake/jnp9cIpuHxil7HnPQHd_z
https://wakelet.com/wake/gmDlBcv8WciIJiAImnj1_
https://wakelet.com/wake/tM4Oxhz4q_3rAB66IgWfL
https://wakelet.com/wake/ZnuIFMJqCPfeDyZzoMmGL
2 days ago Subscribe to DOODLAND: https://bit.ly/3eREqKx Try not to laugh. These crazy doodles want to rule this world with magic tricks ... Streamed 1 year...
https://valdymoinovacijos.lt/component/k2/item/45-portfolio-content-10
saltlati (Monday, 28 February 2022 04:48)
3 days ago WEIDER 8525 USER MANUAL Pdf Download; Weider 8530 Exercise Chart Exercise I; Page 16 of Weider Home Gym 8530 User; Chart, Wall |.... ... Manual Weider 8530 universal home gym manual weider 8525 manual pdf ... Weider Pro 4100 Exercise Chart PDF exercise manual weider 8530 universal... 877e942ab0 saltlati
https://wakelet.com/wake/fqaXT3i1aITAUMpAPrDTk
https://wakelet.com/wake/izQbjB2nwVUuuTOZ_3Gk7
https://wakelet.com/wake/xBNhQ9ncGQ4KpvyFPziMQ
https://wakelet.com/wake/lY_cddGXSiAUkP91ihr2A
https://wakelet.com/wake/deHVjChEaAzhMkgIc-LjB
https://wakelet.com/wake/ApIXLnurpDIc7PC8F07B6
https://wakelet.com/wake/3W-jY8ks9KPhUsboYHzrI
https://wakelet.com/wake/Qwv7IpMFQCcCP1tqEzdLw
https://wakelet.com/wake/z8q0XH35znYp4k4uB-lQ0
https://wakelet.com/wake/6JPIW1sVvNoOudFjK50um
Joe Weider saw things differently. Tower 200 exercise manual weider 8530 universal home gym manual weider 8525 manual pdf the weider system of.... Gym dumbbells, Joe weider; WEIDER 8525 USER MANUAL Pdf Download; Weider Home Gym | September #5 - Estate; Weider XR 6.1 Multi-Position Weight...
https://lilah-northfield.jimdofree.com/
odwyodel (Monday, 28 February 2022 06:08)
What is it that makes people watch American football ... 3 Things We Learned: FC Barcelona vs Real Sociedad ... Online betting on FC Barcelona. Best odds and bonuses ... Field in the match between Valladolid and Barcelona was so.... Barcelona, second in the la liga, host the third-placed atletico madrid when two sides ... Watch news result real madrid vs atletico madrid live barclays premier league ... With a local guide, visit sites such as the changing rooms, pitch, vip box and ... Atltico madrid real betis live score (and video online live stream*) starts on.... May 2, 2021 VIPBox TV Home | DMCA | Message | Policy. Cookies and Privacy Policy. We use cookies, ip-address for the website and display advertising. 877e942ab0 odwyodel
https://wakelet.com/wake/isWT1M68GlGcs3mCtq0Co
https://wakelet.com/wake/9oMiK2kD6TdlwSRpjc8xT
https://wakelet.com/wake/kSefpbBvUtFGdhm5tI8J2
https://wakelet.com/wake/oSLgaH8O6X71D43Dehi1B
https://wakelet.com/wake/4XEcnetDB1PmXJCr12F-a
https://wakelet.com/wake/uDMHguRWCmqa-rvCYrw-C
https://wakelet.com/wake/j0kgZcGGQsWRPuF35kQba
https://wakelet.com/wake/eDoFlmzaymQvDPzTKfOni
https://wakelet.com/wake/eeamlbCr5-y6ggoE3keRZ
https://wakelet.com/wake/o9KACv6iP3DBM4vA7Gj36
raphinha vs cahill,sports planet kota damansara,statarea soccer,2020 draft predictions nba,5 dragons online real money,basketball usa; ... IntroductionThe case found that Osasuna paid Real Betis a total of 650,000 euros ($702,099), including 400,000 euros to beat their relegation rivals Real Valladolid and another.... Mar 17, 2019 I needs to spend some time learning more or understanding more. Thanks for fantastic ... So wonderfu to find somebody with a few genuine thoughts on this topic. ... the online viewers; tey will take bnefit from it I m sure. ... Pingback: watch bubble and bounce video here ... Pingback: www.vipbox.im.
https://www.americansportsforum.com/tioparrirec
harlxim (Monday, 28 February 2022 07:30)
Read Online Baritone Ukulele Chords Songs ... songs - Ukulele Tabs and ChordsBasic Ukulele Chords For Beginners - Know Your InstrumentUkulele Songs... 877e942ab0 harlxim
https://wakelet.com/wake/W1pda1Fva5MqHhDF2uXOe
https://wakelet.com/wake/lOkfvCRg9pfqz_kWMaMLt
https://wakelet.com/wake/6tfz-kxboiNa4UqFTEa4v
https://wakelet.com/wake/24g1FOOcWAy7fJUoiMebp
https://wakelet.com/wake/wyJs6tpVvoxqpkatQhl6X
https://wakelet.com/wake/xZ3IUIqhCJAL4ZRHqMpR6
https://wakelet.com/wake/YCPF3jtd7yro3WznacUGb
https://wakelet.com/wake/yR1sfMy2IfvNPHbEywXKD
https://wakelet.com/wake/3ySaJeW1me4XGf11CNOjc
https://wakelet.com/wake/k3kZE34n-OZyUxKG6XNgt
... A. The Baritone ukulele is tuned like the top four strings of a guitar, D G B E. ... Online Resources. Chord ... Uke1.pdf. Free Song Websites (with ukulele chords).. UkuChordNamer is the most accurate online ukulele chord naming and identification tool. Tap on the fretboard the notes you are playing to name it.. Included are a chord library, tuner, strumming patters, common progressions, and ... 'Yousician' is a great online tool, not just for ukulele players, but anyone ... The app has a vast free library as well as a premium version to unlock much more.
https://planetapro.jimdofree.com/%D0%B3%D0%BE%D1%81%D1%82%D1%8C%D0%BE%D0%B2%D0%B0-%D0%B3%D0%BE%D1%81%D1%82%D0%B5%D0%B2%D0%B0%D1%8F-guestbook/
hedwcorn (Monday, 28 February 2022 08:54)
Shop the Gucci Official Website. Browse the latest collections, explore the campaigns and discover our online assortment of clothing and accessories. 877e942ab0 hedwcorn
https://wakelet.com/wake/npIbZQKEnsP0nYRi08aok
https://wakelet.com/wake/NwdV5FG2xAK-NaOp0PPsJ
https://wakelet.com/wake/3I79kazx3OAPiCu4tcQGn
https://wakelet.com/wake/x2M9kTzFRzpK_iggRjsqB
https://wakelet.com/wake/ELU5q6_cTYJaZDYyvpVJc
https://wakelet.com/wake/v-0I48sD72WbiA37e7r2x
https://wakelet.com/wake/5kx8VHXaO9hjV5GpthKKw
https://wakelet.com/wake/VPScP0gCfoXJmo_8UFepg
https://wakelet.com/wake/7sUut2gtrIqn6U8--5shx
https://wakelet.com/wake/zRrHEaF9p2GA4DiicNAKs
Dec 1, 2020 Australia has to make a forced change while India remain unchanged. IND vs AUS 3rd ODI live toss time and streaming details. Playing 11s: India...
https://www.thomasafraser.com/apps/blog/show/44524835-honest-interviews
zenpalun (Monday, 28 February 2022 10:13)
Farm Road, Durham, NC 27707-8110. ... (USP) and is an auditing course professor for the MBA in Internal ... such as European Accounting Review and Critical Perspectives on ... South Africa states that "The audit committee should ensure that a ... immediately available to the internal audit staff via Web download and. 877e942ab0 zenpalun
https://wakelet.com/wake/rSNadKsVSp5r3u7hCkTIW
https://wakelet.com/wake/i4PAh1IKGzb_LybP4WD_w
https://wakelet.com/wake/K3XjZ-kPa9QcQN3N5LIHx
https://wakelet.com/wake/9TzyeGGJPxYA_GlUbCabu
https://wakelet.com/wake/dUx-Dhsauhk1aeYffCGWa
https://wakelet.com/wake/uMApJtp7fHIzIKnlIXSh0
https://wakelet.com/wake/vQcxV31AQEi31u8RCjdnJ
https://wakelet.com/wake/Y2ohsgx-YKdIKOe52LJUB
https://wakelet.com/wake/w2er2NGGz3qD7G9xnNAC7
https://wakelet.com/wake/inC7TmiFaav0nwSHWlcua
Apr 1, 2020 As COVID-19 cases around the United States continue to rise, the ... according to a U.S. security official tracking Chinese hacking activity. ... in malicious COVID-19 coronavirus domains in Europe and North ... In the attack, people were lured into downloading a ransomware app ... Ref - Wall Street Journal.... by R Bartlett Cited by 656 of Biomechanics in Sports and European College of Sports Sciences, and an Honorary. Fellow of the ... Appendix 3.1 Further exploration of angletime patterns 112 ... Jumping vertically to achieve maximum height is clearly a task constraint. ... The latter, of course, will require the analyst to be aware of movement principles.. by F Kafka 1971 Cited by 731 Stoker, Metamorphosis, Penal Colony, Country Doctor and the short story: Hunger- ... "The Burrow" and "The Great Wall of China" belong at the summit of Kafka's oeuvre; ... or even contradictory tracks in search of his prey, and content to leave his works ... Europe where islands of urban, wealth, culture, and discontent were...
http://www.ndvadvisers.com/fort-defense-atlantic-ocean-download-mega/
yesizbys (Monday, 28 February 2022 11:40)
DOWNLOADS SHOP CONTACT NEWS SUPPORT ... the ArtsAcoustic BigRock is a emulation of a phaser from the ancient times, read more. ... the ArtsAcoustic Reverb is a professional reverb plugin for vst, pc and mac osx. read more.. ISumsoft Product Key Finder can be installed on Windows XP 7 8 10 ... Jan 27 2019 Find Recover Product Keys for Windows Software iSumsoft Product Key.... {Updated} Windows 7 Serial Key for 32bit/64bit; I have an Win 7 activation key that i want to switch to an; The New 5 Windows 7 Activation Tools in 2020 You... 877e942ab0 yesizbys
https://wakelet.com/wake/0mnk1xBIzQk6mkkLHfSc1
https://wakelet.com/wake/StHJXWlxWAhickhOE7Jhr
https://wakelet.com/wake/QT48Pu1imq9dYsGaYXRwI
https://wakelet.com/wake/E9XuIQGpWHixuAdH_fiYd
https://wakelet.com/wake/-TwayGf3Is0uzRaYxmE-H
https://wakelet.com/wake/CasYhh2Pt6_8SIeK4lut3
https://wakelet.com/wake/OWBD-XTYCrpzs3bmEs2UL
https://wakelet.com/wake/kwKVmrt9UmFgE1TbeUThf
https://wakelet.com/wake/gzVtNsu_Rmo1dKyvkPZbP
https://wakelet.com/wake/LMvjf3z-R4qGFPPs8W1Yu
Mar 2, 2021 ArtsAcoustic Reverb VST [Latest] Free Download. In Summary, If you want to run this app, you need to install the Windows XP/Vista/7/8/8.1/10.... VST/AU/UB. welcome to the ArtsAcoustic Reverb. the ArtsAcoustic Reverb is a high quality reverb for everyday use in a professional studio. this plugin is (unlike...
https://sissycrush.com/read-blog/10457
freiyseu (Monday, 28 February 2022 13:04)
Need money fast? Deposit checks and access funds instantly with approval through your Regions Mobile App when you select Immediate Availability. Regions.... Other Bank(s)-These are any additional accounts set up for direct deposit which require you to ... Download our mobile banking app, and log in. ... The money took a long time to get into PayPal and his bank account (21-days on-hold period.... The fintechs include SoFi, Earnest (owned by Navient), Chime, Varo, Money Lion, Stash ... and a long list of vendors covering residential mortgage loans, student loans, ... accepting deposits, making loans profitably, acquiring customers efficiently, ... a mobile app ecosystem, and a bunch of critical technologies and APIs that... 877e942ab0 freiyseu
https://wakelet.com/wake/eyuhmRkn7UYjHi0_me4s4
https://wakelet.com/wake/cbSi1xlmkZlIqcjtfOAMc
https://wakelet.com/wake/_2lFUrYn6SreIp45kyAXo
https://wakelet.com/wake/UpPbEywu1wGNDJB17pLnB
https://wakelet.com/wake/bISGEOBbNRxRoFuj3ayu4
https://wakelet.com/wake/V_RBBQN_0ZcCUo8Ys5cFf
https://wakelet.com/wake/9JN_t89KrKG1DZM6a8eKB
https://wakelet.com/wake/q00OPGn6tNsYft53SRFo3
https://wakelet.com/wake/4fcf99W-KPQIRZPRUO3-d
https://wakelet.com/wake/sQ4gksky3qh06m4xj3Ei1
Varo and Chime are both online-only banks that offer no-fee checking and savings ... mobile and online banking access to manage accounts and deposit checks.... You can also make direct deposit from Chime account to Cash App using ... name on a regular money transfer as long as the money hasn't yet been picked up.
https://www.hott953.com/apps/blog/show/46169021-drake-signs-dancehall-artist-popcaan-to-ovo-sound-label
walfran (Monday, 28 February 2022 14:32)
129099-BUM-J-0112 SECTION II1: REPLACEMENT PARTS LIST All components, assemblies, accessories, and replacement parts for this furnace are available.... Recreational Vehicles & Park Models. 3. ... Has furnace gas valve and burner orifice been correctly con- ... using DGPH model furnaces with Coleman Blend.. Most common Coleman furnace parts that need replacing Thermocouple. The thermocouple or flame sensor is a small metallic device positioned in the flame path... 877e942ab0 walfran
https://wakelet.com/wake/B4hbl1J9Z_V7d4xegzrc5
https://wakelet.com/wake/5zhXP7pwLCd-ykih-C1C8
https://wakelet.com/wake/j5xjNnXiPu4wr6W0nWKHG
https://wakelet.com/wake/zmloRbJErw4VqsYOWQfbw
https://wakelet.com/wake/85iErgCiKsP3yqdXuBsIQ
https://wakelet.com/wake/WmKYRRvtS0VPdJBGKdMzD
https://wakelet.com/wake/VWPjJILfjci6ZRk6sHUmQ
https://wakelet.com/wake/7OpzgnMnIoiZgHivkHDiP
https://wakelet.com/wake/P8m6-e-YFfKgAxArKfxfA
https://wakelet.com/wake/pL3Uyy1u49MFIryUC9y69
Coleman, Nordyne heat pumps, Interthern. We carry furnace parts for all make or brands of furnaces, new or old. Don't see it here? Call 1-800-479-2754 We ship...
http://www.family-schneider.de/index.php?option=com_phocaguestbook&view=phocaguestbook&id=1&Itemid=55&t=220
caeidri (Monday, 28 February 2022 15:54)
Feb 12, 2017 Elimination Chamber Live Stream: Watch the WWE PPV Online without Cable While all the names aren't locked down yet, we do know that.... Apr 10, 2021 WrestleMania 37, the WWE's 37th premier pay-per-view event, is starting tonight. This annual two-day pro wrestling extravaganza starts at 8... 877e942ab0 caeidri
https://wakelet.com/wake/hg9Ue1aZUdOLC6wubc2uq
https://wakelet.com/wake/rTZvV7-JDmpbq5RIjJ6Mu
https://wakelet.com/wake/e-BtQgtQrwLlMrHZnmZ64
https://wakelet.com/wake/cJIPjj0v3NkkNS_D2TbT0
https://wakelet.com/wake/PPfBmlW6n30glkwIcwu_Y
https://wakelet.com/wake/IgfL3qVwB5yIuTF0J-Z_s
https://wakelet.com/wake/IxNW9ohGZ5e8yaIKpuODI
https://wakelet.com/wake/saSvy_u85Bvjap447fLgq
https://wakelet.com/wake/Esk_GX0Qo47iG48uft3nb
https://wakelet.com/wake/i35LnKIYBiyhdtkmcUcQ1
One event is usually three hours long and features six to twelve matches. Pay-per-view events are a big part of the revenue stream for WWE.. Jun 20, 2021 WWE will hold its last pay-per-view without a live audience on Sunday. Hell in a Cell will mark the final special filmed in the empty WWE...
http://jycdnhj.com/shownews.asp?id=184
clemank (Monday, 28 February 2022 17:11)
Changing Your Address. Method 1. Under Academics (in the top bar of the portal), choose Registration. Then under Helpful Links, select Update My Address.... To change the mailing address for your property tax bill (for parcels located in Cuyahoga County), please complete the form below. In order for us to process the.... Change of Address for Enrolled Providers. Please select the appropriate form based on your provider type. If you have any questions or concerns, please... 877e942ab0 clemank
https://wakelet.com/wake/PvDfbxrsLP2mK-8qx6AAM
https://wakelet.com/wake/VFN9D2V-ZIQw8CR8x1oPx
https://wakelet.com/wake/dQao0r4zfUR-KUi8kqajJ
https://wakelet.com/wake/7xBqXshowpZXkgHt4VJ4W
https://wakelet.com/wake/skQzYfGtl8uz_oOwX7ymS
https://wakelet.com/wake/nnpNuqNZcQpq527oZ3MeE
https://wakelet.com/wake/1NK2A9tIfdATsLYCqAYR6
https://wakelet.com/wake/FlpSGM7WgajL1n-TuhWWW
https://wakelet.com/wake/X4GVwD3-WmvgI6S4FSmk_
https://wakelet.com/wake/eu-MBHON4dRiAfZgPSOps
USCIS Form AR-11/Change of Address Form ... The U.S. Citizenship and Immigration Services (USCIS), Department of Homeland Security (DHS), must be.... use this form to send the Office of the Registrar a request to change your address or telephone number.. Change of Address. Notification to the I.O. of change of member mailing address. USA CANADA. Copyright 2021 by IBEW - Login | Contact Us | Site Map...
https://chihuahua-mini.jimdofree.com/%D0%B3%D0%BB%D0%B0%D0%B2%D0%BD%D0%B0%D1%8F-home/%D0%B0%D0%BA%D1%81%D0%B5%D1%81%D1%81%D1%83%D0%B0%D1%80%D1%8B-%D0%B4%D0%BB%D1%8F-%D1%81%D0%BE%D0%B1%D0%B0%D0%BA/
paeolu (Monday, 28 February 2022 18:33)
Founded in 1984, the Tucson Weekly is the Tucson news source that matters. Politics, culture, arts, music, food and everything else that makes our city great in.... Mortal Kombat X for iOS is now available to download from the App Store.Follow Mortal Kombat X at... 877e942ab0 paeolu
https://wakelet.com/wake/P8mZm19cb9vHPwYW2f2I9
https://wakelet.com/wake/34Of6TyKf5LDPx-uhPpkF
https://wakelet.com/wake/81O2pLcS5TnSLZuX_457S
https://wakelet.com/wake/_LAX8Bm19sLr84Z5XPfRA
https://wakelet.com/wake/is1S8DCDwZDqsx3THcYds
https://wakelet.com/wake/X5_xhANohuvaioaoiusSo
https://wakelet.com/wake/wFHVIiFoii7J6Iw6xrZ2s
https://wakelet.com/wake/gyO6eIbRnplOBpbCOL-oQ
https://wakelet.com/wake/gz0bipoOnnVLeklnyhAel
https://wakelet.com/wake/HSDEa2n7VclEcIClo8Cel
UPDATE April 22nd, 2015 6:57am PST: Mortal Kombat X has soft launched onto Google Play in select regions ...
https://www.vitaldyrehelse.net/apps/blog/show/43888571-sommereksem-hos-hest
wylphi (Monday, 28 February 2022 19:52)
Mar 30, 2010 It's out now and it's official, Mac OS X 10.6.3 was released today by Apple. It is a very crucial update and it implements hundreds of fixes since... 877e942ab0 wylphi
https://wakelet.com/wake/1mI2njVBzvWAkvqAbOYgy
https://wakelet.com/wake/_4GVhVIxGd92obvvq2j6N
https://wakelet.com/wake/iVois7CKTHKki02JPVJl5
https://wakelet.com/wake/i45vU1lypGD56GJzxgbgB
https://wakelet.com/wake/XnvR5pWSvoBGBFjSW75Mx
https://wakelet.com/wake/l0GERQuRB-wfLDmTOBRmU
https://wakelet.com/wake/ifDMKqBwbRxKYCFTwk8wi
https://wakelet.com/wake/8puMbjQuJjMzGTgMH8i9L
https://wakelet.com/wake/Bo-gSs6-eXeRQ6ObA2-MZ
https://wakelet.com/wake/4Syz_svIRgM4PJ9SbZ__E
Sep 29, 2018 By any chance you want to download Mac OS X 10.6.x and 10.7.x Combo updates manually, find out the links here. Download the DMG files...
https://www.hott953.com/apps/blog/show/46036188-gabrielle-union-and-dwyane-wade-welcome-a-baby-girl
daryyam (Monday, 28 February 2022 21:09)
well, just in case there is a "new potential customer" here looking around, I'll kick in my 2 ... Bundle, Roland RD-1000, Synthogy Ivory, Kontakt, Focusrite 18i20, ... with your Serial Number (Help > About Band in a Box will show you your number). ... Authorization is tied to the internal and individual ID number of each machine. 877e942ab0 daryyam
https://wakelet.com/wake/m4u7lvJEnGXk96SRp7ofv
https://wakelet.com/wake/BKggQbjReAhHhZZZ3Rkzq
https://wakelet.com/wake/5-Ic614mTFmnyBsrkDWH5
https://wakelet.com/wake/OYJq7yQqtTM6GFvNgoME1
https://wakelet.com/wake/ARh_-sbyzAiA01fRaVFvO
https://wakelet.com/wake/Er2zn45dLeo5jFwGoY1M1
https://wakelet.com/wake/UcdAot1cD2pH18ZR5hBz8
https://wakelet.com/wake/OZSYwUpgy-VK9IxzNmMnT
https://wakelet.com/wake/JOOXdm3QZthEv_Te_-SKv
https://wakelet.com/wake/FIWdQyqNd1C6lv7H7Rimc
Dec 14, 2020 iZotope RX 7 Audio Editor Advanced VST Free Download with Crack WINDOWS Mac 2019 MacOSX synthogy ivory machine id for keygen. ... Spectrasonics Steven Slate Drums Sugar Bytes SynchroArts Synthogy TAL ... your machine as prompted, then select "Activate A New Product License" and click Next. ... Enter your Serial Number, License Key and iLok user ID (the one you use to ... Direct links for all Ivory II download products can be found below:.
https://sissycrush.com/read-blog/10490
wistglor (Monday, 28 February 2022 22:27)
Ingersoll Rand Gyro-Flo 85 Air Compressor w/ Trailer (parts or repair) $500 . ... 919.150390 Parts Manual Form M-150390 7/13/94 (Very Good Condition) Product Details: - Format: Manual - Binding: 3-Ring Bi-Fold ... 24 outdoor atomic clock... 877e942ab0 wistglor
https://wakelet.com/wake/aG6qeFluXdeX6oNj5kZlq
https://wakelet.com/wake/X46kCf98BzUz7DepZcQ4C
https://wakelet.com/wake/BKWVQUTlWL0orSk980jSN
https://wakelet.com/wake/oCu5qlPEGKkbUXco99rEQ
https://wakelet.com/wake/Lo062VoD9GM0wpACBj72F
https://wakelet.com/wake/1yIiPPi02kTOa7eYeda_e
https://wakelet.com/wake/W-z5ZVkDz5IUituMuIgMc
https://wakelet.com/wake/ULUU9tkfzZLQ2wL_nAv9l
https://wakelet.com/wake/IQnDq2_A4PFdpVhnD0oTp
https://wakelet.com/wake/a9WzleGnYGWE382-DMNJ6
Howa 1500 hact trigger adjustment ... Atomic Number Protons, Electrons and Neutrons in Beryllium. ... The small colored double circles are gluons, which can be seen binding the proton and n ... Rheem gladiator water heater manual.... 1998-2006Haynes Manual on WeldingThe Return of Jake SlaterProgressive Fly Fishing for ... iteration of the car to be sold in the U.S. Paying special attention to technical aspects such ... Robust binding in laminated board to endure hard day-to-day use. ... laws, the concepts of field and waves and the atomic view of matter.
https://adminclub.org/showthread.php?tid=219130&pid=571421#pid571421
amabmae (Monday, 28 February 2022 23:45)
Free download Terraria v1.4.2.2 torrent latest and full version. Terraria is a cool indie sandbox with an admixture of role-playing game in which you have to go... 877e942ab0 amabmae
https://wakelet.com/wake/kouZygjF6i6CvBn8BW0-l
https://wakelet.com/wake/HgU9sHlGWjtILeZja4SIM
https://wakelet.com/wake/apYA-if_8WMX9rhYlDRYs
https://wakelet.com/wake/XkVWa3etTxWmYHZzqZSyQ
https://wakelet.com/wake/Qup28LtN1VjUDS0M_t6gU
https://wakelet.com/wake/SSCIWITtI2OAwd3T4YNs-
https://wakelet.com/wake/oragDb2AKtivXECgmLfGF
https://wakelet.com/wake/Ccaz3M6L97VfpeRsxpfLk
https://wakelet.com/wake/f0zGPKalQBA7gP9eSERxm
https://wakelet.com/wake/PT3I24RhuOQmCGaQjBbr2
Terraria Online is a lite online version of Terraria. Start playing online! No Download. Many more free games.
https://meatbeef18.webs.com/apps/blog/show/48097020-historia-de-electricidad-por-electrodomesticos
wartmanl (Tuesday, 01 March 2022 01:04)
Adobe Media Encoder 2020 software automates the process of creating multiple encoded versions of source files, Adobe Premiere Pro sequences, and Adobe.... Jan 26, 2021 Adobe Premiere Pro 2020 v14.8 Multilingual macOS. Adobe Premiere Pro CC 2020 lets you edit video faster than ever before. Dozens of... 877e942ab0 wartmanl
https://wakelet.com/wake/Qa97pNU2F-vYpwPlAR-V0
https://wakelet.com/wake/UGA3xOv_oJ9AmM_YFpdCl
https://wakelet.com/wake/VpfwHsC5e_fIPnF_H1zs-
https://wakelet.com/wake/K3Qu1Li3idb4zGw0P60rn
https://wakelet.com/wake/Wa_2dkssksNgDYqFWXmgC
https://wakelet.com/wake/hXOxje5CFd3xjwrKx17dq
https://wakelet.com/wake/rCRKrQnGLZ9VqtQljv2mZ
https://wakelet.com/wake/anZ4z8_UktlrM5ht0Wbgc
https://wakelet.com/wake/dxhYAERix0aLtxAE6oDDf
https://wakelet.com/wake/TVtfXGlrftmoKaSUpNSkz
Jan 18, 2021 One of the most complete and professional movie editing software is Adobe Premiere Pro, which professional editors are definitely familiar with.. Jan 9, 2021 Adobe Premiere Pro 2020 Crack v14.6.0.51 Full Version (Pre Activated) [Latest]. Adobe Premiere Pro Crack is an expert program designed by...
https://seesaawiki.jp/wiwhotisa/d/Blonde%20angel%20%40iMGSRC%2eRU
harefat (Tuesday, 01 March 2022 02:18)
The Official Athletic Site of the Clemson Tigers, partner of WMT Digital. The most comprehensive coverage of the Clemson Tigers on the web with highlights,.... Illinois College is a top ranked liberal arts college located in Jacksonville, Illinois known for its Graduate Ready commitment to students.. Get the latest news and information for the Illinois State Redbirds. 2020 season schedule, scores, stats, and highlights. Find out the latest on your favorite... 877e942ab0 harefat
https://wakelet.com/wake/C0kIMzei5EWGsmZeLIyIp
https://wakelet.com/wake/08nzvvlEejjUgx4HJ2hz9
https://wakelet.com/wake/WlU0Mf-vmqXj5EPq_U43U
https://wakelet.com/wake/UbGB8NIjT8ngvJafa2Ufg
https://wakelet.com/wake/VdAZVlgPZM0-i8ncCdSof
https://wakelet.com/wake/p-nW4xD9axlaH9TzeLm-d
https://wakelet.com/wake/uDaXYul2dVSLRrikrnrZm
https://wakelet.com/wake/o0NRUxsMyIIzXZSDX2Yhq
https://wakelet.com/wake/M--z2YTSfp921YGoFr6ib
https://wakelet.com/wake/P2LT_6EBrfi8OC-sFf9DE
City, State or Zip. Search ... Whether you need a long-term stay or short term rehabilitation, we provide around-the-clock licensed nursing care in a supportive.... The official 2020-21 Men's Basketball schedule for the Illinois State University ... Dec 2 (Wed) 5 p.m. ESPN3 WJBC AM 1230 / 93.7 FM / TUNEIN. vs. Greenville.
https://mia.world/elsalasma
ulankar (Tuesday, 01 March 2022 03:33)
Because of the considerable Proof of funds Service Bank Guarantee SBLC ... banks through a single gateway ; Automates your processes thereby reducing cost,.... An SBLC is frequently used in international and domestic transactions where the ... The counselor may be able to negotiate lower payments and interest rates,... 877e942ab0 ulankar
https://wakelet.com/wake/dmmylhqwko3xj1WX5IC-Q
https://wakelet.com/wake/lg6AU2mEEa4woFr_bWmRE
https://wakelet.com/wake/AzPP92_Llo4EG8r580IbR
https://wakelet.com/wake/OLXO7QH7FiVtN9MxK7J6a
https://wakelet.com/wake/InKuf_5uwVjEJqHsh0PKz
https://wakelet.com/wake/aFTkJJS-5uMETYJKFBmaT
https://wakelet.com/wake/NglIlRiG04czXJVmAdxR1
https://wakelet.com/wake/QpwEdufwHFbUOevgQeU4f
https://wakelet.com/wake/pZgo2F0P5o8VW9HmglQEY
https://wakelet.com/wake/fDAMHrLupvCcybBn1Bjbq
FX Rate Calculator. Try our currency converter to get near real-time exchange rates for over 130 currencies. Amount. Currency.
https://mixparlays.com/showthread.php?tid=62250&pid=334681#pid334681
woopatt (Tuesday, 01 March 2022 04:50)
Apr 19, 2017 Download Free Xilisoft Audio Converter Pro 6.5.3 for Mac on Mac Torrent Download.. link: http://www.todotumac.com/2017/10/xilisoft-audio-converter-pro-v653.html.. Buy Audio Converter Pro 6 With Bitcoin - Xilisoft iDevice Magic Platinum PC - Should I Remove It ... Buy Perfect Keylogger for Mac now - secure online purchase! 877e942ab0 woopatt
https://wakelet.com/wake/WPRGefTnhUnKnfgWUeOav
https://wakelet.com/wake/_wzIJk1flNomLltsDpCrb
https://wakelet.com/wake/lokb2tN__JGv5iElVSO57
https://wakelet.com/wake/bTDbao9Sqqpr4dDpmbJRo
https://wakelet.com/wake/D5F-RUCPu6TqY4E0mya8L
https://wakelet.com/wake/qfxpjhRyPxQNG-Ewu207K
https://wakelet.com/wake/0RZuWs-N8QElCdFHcNGDS
https://wakelet.com/wake/pkqlmrWaX86jWcRB4XSZV
https://wakelet.com/wake/gY4X5OhEYU3GALY0W3smo
https://wakelet.com/wake/KYWXsb-KSwOgfNBS326P2
Mar 7, 2016 Xilisoft Audio Converter Pro for Mac is a master program which helps Mac users to convert between audios of different formats, extract audio...
https://mia.world/achinalan
kalyjan (Tuesday, 01 March 2022 07:20)
SOME OLD EXPRESSIONS AND WHERE THEY COME FROM By Tim Lambert I should point out that this list of old sayings gives their most likely origin.. Jul 16, 2015 The word "idiom" originates in the Greek word dios ("one's own") and means "special feature" or "special phrasing." Idioms are peculiar... 877e942ab0 kalyjan
https://wakelet.com/wake/uaUP34a36GiDDPuZQOGRG
https://wakelet.com/wake/DgQ8SFG38ASBxXutBU0qV
https://wakelet.com/wake/-qb7iDp94c5C4i96cTS8s
https://wakelet.com/wake/7IDT9JvZKzQtwmZK5RKku
https://wakelet.com/wake/0wW7zE9l3kkLLw7iBYY4N
https://wakelet.com/wake/1bH7VZ6kgPHTjCKWX_LWI
https://wakelet.com/wake/-b3_w3QReAZyNEemAAMu7
https://wakelet.com/wake/_cRPZsMJqvQWQUBHC8jJ1
https://wakelet.com/wake/uGtqqbwmoU5ov_bltESL7
https://wakelet.com/wake/Qfb0M7CHo8fJreJskllsf
25.05.2021Greek idioms and proverbsComments: The Greeks have imparted wisdom to the world. They could accomplish such a high stage of knowledge and.... ... Balochi Saraiki Hindi Spanish French German Turkish Persian Greek Bengali ... in Gujarati Dictionary, Find English to Gujarati meaning and proverbs meaning. ... CONDEMNED boots on the ground idiom. burn. capital punishment. chair.
https://wissem.jimdofree.com/scripting-os-admin/encrypting-shell-scripts/
kalyjan (Tuesday, 01 March 2022 07:21)
SOME OLD EXPRESSIONS AND WHERE THEY COME FROM By Tim Lambert I should point out that this list of old sayings gives their most likely origin.. Jul 16, 2015 The word "idiom" originates in the Greek word dios ("one's own") and means "special feature" or "special phrasing." Idioms are peculiar... 877e942ab0 kalyjan
https://wakelet.com/wake/uaUP34a36GiDDPuZQOGRG
https://wakelet.com/wake/DgQ8SFG38ASBxXutBU0qV
https://wakelet.com/wake/-qb7iDp94c5C4i96cTS8s
https://wakelet.com/wake/7IDT9JvZKzQtwmZK5RKku
https://wakelet.com/wake/0wW7zE9l3kkLLw7iBYY4N
https://wakelet.com/wake/1bH7VZ6kgPHTjCKWX_LWI
https://wakelet.com/wake/-b3_w3QReAZyNEemAAMu7
https://wakelet.com/wake/_cRPZsMJqvQWQUBHC8jJ1
https://wakelet.com/wake/uGtqqbwmoU5ov_bltESL7
https://wakelet.com/wake/Qfb0M7CHo8fJreJskllsf
25.05.2021Greek idioms and proverbsComments: The Greeks have imparted wisdom to the world. They could accomplish such a high stage of knowledge and.... ... Balochi Saraiki Hindi Spanish French German Turkish Persian Greek Bengali ... in Gujarati Dictionary, Find English to Gujarati meaning and proverbs meaning. ... CONDEMNED boots on the ground idiom. burn. capital punishment. chair.
https://wissem.jimdofree.com/scripting-os-admin/encrypting-shell-scripts/
kalyjan (Tuesday, 01 March 2022 07:21)
SOME OLD EXPRESSIONS AND WHERE THEY COME FROM By Tim Lambert I should point out that this list of old sayings gives their most likely origin.. Jul 16, 2015 The word "idiom" originates in the Greek word dios ("one's own") and means "special feature" or "special phrasing." Idioms are peculiar... 877e942ab0 kalyjan
https://wakelet.com/wake/uaUP34a36GiDDPuZQOGRG
https://wakelet.com/wake/DgQ8SFG38ASBxXutBU0qV
https://wakelet.com/wake/-qb7iDp94c5C4i96cTS8s
https://wakelet.com/wake/7IDT9JvZKzQtwmZK5RKku
https://wakelet.com/wake/0wW7zE9l3kkLLw7iBYY4N
https://wakelet.com/wake/1bH7VZ6kgPHTjCKWX_LWI
https://wakelet.com/wake/-b3_w3QReAZyNEemAAMu7
https://wakelet.com/wake/_cRPZsMJqvQWQUBHC8jJ1
https://wakelet.com/wake/uGtqqbwmoU5ov_bltESL7
https://wakelet.com/wake/Qfb0M7CHo8fJreJskllsf
25.05.2021Greek idioms and proverbsComments: The Greeks have imparted wisdom to the world. They could accomplish such a high stage of knowledge and.... ... Balochi Saraiki Hindi Spanish French German Turkish Persian Greek Bengali ... in Gujarati Dictionary, Find English to Gujarati meaning and proverbs meaning. ... CONDEMNED boots on the ground idiom. burn. capital punishment. chair.
https://wissem.jimdofree.com/scripting-os-admin/encrypting-shell-scripts/
ramaeuj (Tuesday, 01 March 2022 08:41)
Jul 17, 2018 F/s Swarovski Laser Guide 8x30 c/w holster, strap, boxed. Very good condition, no scratches that I can see on the lenses. Please pm for more.... Jan 27, 2016 - Swarovski Laser Guide 8x30 Laser Rangefinder 70002 UA-914.. The top performer among "consumer" laser rangefinders is the Swarovski Laser Guide. Its 8x30 monocular is the best. Past 1000 yards, it ranges deer and man-... 877e942ab0 ramaeuj
https://wakelet.com/wake/Hkn6uHrpY-tTEN6TapkRQ
https://wakelet.com/wake/impFWwodP2Lr0rOEFKEcK
https://wakelet.com/wake/fmurzq6_BMxENPFUKvzQx
https://wakelet.com/wake/FFWmlFsx_jyMX_2_ugVwF
https://wakelet.com/wake/0yFlqDg7JSRk-yQd537Rp
https://wakelet.com/wake/BifUDj543xcNeMxEqFViH
https://wakelet.com/wake/O1U1zLJ1ZRv5XJQfS6TdK
https://wakelet.com/wake/zrnVB-q_x2cm6B1B-sBLn
https://wakelet.com/wake/xDlAJsMCgGhrk-c4QXcZF
https://wakelet.com/wake/kf0G0H8QGdN-OLo6ARDG9
Austrian manufacturer of premium quality rifle scopes, binoculars, spotting scopes, and tripods. Visit our online shop!. Sep 14, 2019 The Swarovski Optik Laser Guide 830 is a monocular rangefinder suitable for wildlife enthusiasts and nature lovers. With a magnification of 8x.... Dec 29, 2020 Swarovski has long manufactured high-quality, compact laser rangefinders. Its current model, the Laser Guide 8x30, features superb glass and...
http://bpimballaggi.it/component/k2/item/1.html
ramaeuj (Tuesday, 01 March 2022 08:42)
Jul 17, 2018 F/s Swarovski Laser Guide 8x30 c/w holster, strap, boxed. Very good condition, no scratches that I can see on the lenses. Please pm for more.... Jan 27, 2016 - Swarovski Laser Guide 8x30 Laser Rangefinder 70002 UA-914.. The top performer among "consumer" laser rangefinders is the Swarovski Laser Guide. Its 8x30 monocular is the best. Past 1000 yards, it ranges deer and man-... 877e942ab0 ramaeuj
https://wakelet.com/wake/Hkn6uHrpY-tTEN6TapkRQ
https://wakelet.com/wake/impFWwodP2Lr0rOEFKEcK
https://wakelet.com/wake/fmurzq6_BMxENPFUKvzQx
https://wakelet.com/wake/FFWmlFsx_jyMX_2_ugVwF
https://wakelet.com/wake/0yFlqDg7JSRk-yQd537Rp
https://wakelet.com/wake/BifUDj543xcNeMxEqFViH
https://wakelet.com/wake/O1U1zLJ1ZRv5XJQfS6TdK
https://wakelet.com/wake/zrnVB-q_x2cm6B1B-sBLn
https://wakelet.com/wake/xDlAJsMCgGhrk-c4QXcZF
https://wakelet.com/wake/kf0G0H8QGdN-OLo6ARDG9
Austrian manufacturer of premium quality rifle scopes, binoculars, spotting scopes, and tripods. Visit our online shop!. Sep 14, 2019 The Swarovski Optik Laser Guide 830 is a monocular rangefinder suitable for wildlife enthusiasts and nature lovers. With a magnification of 8x.... Dec 29, 2020 Swarovski has long manufactured high-quality, compact laser rangefinders. Its current model, the Laser Guide 8x30, features superb glass and...
http://bpimballaggi.it/component/k2/item/1.html
marttant (Tuesday, 01 March 2022 10:07)
Mar 1, 2011 John the Cook is making the best triple-layered cream cake for his friend Dorothy. But when Captain Feathersword can't resist, and takes a huge.... You won't believe your eyes! For the first time ever, Dorothy will have her own plane to travel around the world in search of the perfect rose!. Aug 28, 2012 Barnes & Noble has the best selection of CDs. Buy The Wiggles's album titled Dorothy the Dinosaur's Travelling Show!. 877e942ab0 marttant
https://wakelet.com/wake/sis6hoXrpjErAAbgN0hhS
https://wakelet.com/wake/_gFZBlnnk-mEghgxsJ4-g
https://wakelet.com/wake/pxc8CT-h6hgvjXmshjczw
https://wakelet.com/wake/qzd8UAsOU6EcvQWosgbc_
https://wakelet.com/wake/D12ChwmtfL85_a3XevXHI
https://wakelet.com/wake/zlNHh9EvOmVAzj5NwKOVt
https://wakelet.com/wake/H0e93uMeFOk1dX5Tfutp7
https://wakelet.com/wake/hcpCyrBk82OI4VOOemUb7
https://wakelet.com/wake/0xni3mCDBoVmXEkqoKKtq
https://wakelet.com/wake/OY8u9NmA_-Me4WNLPeTmC
Download The Wiggles Present Dorothy The Dinosaur's Travelling Show! songs online for Free on Wynk Music. Play The Wiggles Present Dorothy The.... Available in the National Library of Australia collection. Author: Polutele, Jodie; Format: Book; 24 p. : ill. ; 21 x 25 cm.. Shop Dorothy the Dinosaur's Travelling Show! [CD] at Best Buy. Find low everyday prices and buy online for delivery or in-store pick-up. Price Match Guarantee.
http://clinicesadra.com/index.php/k2-blog/item/4-custom-pet-gallery-style-with-carousel
oakcomp (Tuesday, 01 March 2022 11:26)
Unboxing of an LG Optical Drive.Subscribe please!:http://www.youtube.com/AppleiTouchTutorials.. Lg lightscribe hl-dt-stdvd Driver Windows. Software CD into the External Super Multi DVD. Rewriter ... LG GE20LU11: 20x External Super-Multi DVD Rewriter. 877e942ab0 oakcomp
https://wakelet.com/wake/-dm1DVjLrVJWooF5u794r
https://wakelet.com/wake/zXmGrWpfOBFEVg38y_IUs
https://wakelet.com/wake/O-XABSSFL_xANch_AUYsh
https://wakelet.com/wake/E7IipVcn_vYK2cgOe3ke7
https://wakelet.com/wake/5qe7szDqkW9mrr0nzutOS
https://wakelet.com/wake/TzR2aanzKQulx9Ow1acOS
https://wakelet.com/wake/nCVr0ddqw-PSL7znuE6Ea
https://wakelet.com/wake/ztC5BbiNORaxQOQUqBIEo
https://wakelet.com/wake/YBOe2d7iGEGkWpgBn4mXD
https://wakelet.com/wake/eSyYv3-N_91qtLSADmDpA
Dec 11, 2020 Hl Dt St Cd Rw Gce 8483b Drivers For Mac ... This firmware upgrade is for firmware versions below 1.05 of the LG Branded ... Icom usb driver for mac. The ROM ... 60 GE20LU10; 13 GE20LU11; 49 GE20NU10; 14 GE20NU11...
https://maarheeze.nu/index.php/component/k2/item/2138-spinningmarathon-voor-fight-cancer-in-maarheeze
elmsta (Tuesday, 01 March 2022 12:38)
(2020) South Indian Full Movie Hindi Dubbed Watch Online Free Download HD ... movie free download 3gp Avengers 2 Full Movie In Hindi Download Hd watch ... hindi movie songs download, 3gp Song Of. The Main Zulm Ko Mitaa Doongi In.... Dec 19, 2020 UFC Fight Night Thompson v Neal: Weigh-Ins ... Neal-led fight card available to stream RIGHT HERE don't miss a single second of face-punching action! ... Prelims matches online begin at 4:00 p.m. ET on ESPN+, before the main ... Get full UFC Vegas 17 play-by-play updates and live coverage here!. Hindi Movie Full Hd p Kuch Dil Ne Kaha -> DOWNLOAD (Mirror #1) fd3bc05f4a Find ... 2 views. Recent Posts See All. IBM SPSS 25 Crack + License Key Free ... dil ne jise apna kaha full movie. in tamil download Main Zulm Ko Mitaa Doongi in... 877e942ab0 elmsta
https://wakelet.com/wake/k7UauUzS45m_g9EBSB004
https://wakelet.com/wake/xMCzYtzTKSPk-Z2Y8JVKe
https://wakelet.com/wake/A0Ebi8waFN2eM6iEMFh73
https://wakelet.com/wake/PcKQU2ulUDtQED6im0g7d
https://wakelet.com/wake/ru_DM542oBgvtnhg9uMuP
https://wakelet.com/wake/kUBZFLU9O_pFW6Xm0CEjV
https://wakelet.com/wake/52_MBpwVTncGT_EeZCGyf
https://wakelet.com/wake/tLmnYys4MjH9pmlcuCJaF
https://wakelet.com/wake/zXSd26wYB4HDAH3QsdyFv
https://wakelet.com/wake/KKCLiYCdgX5W4gBFforLJ
Aug 3, 2016 And in Part II I covered Shakeel's songs from 1954 M Sadiq movie Shabab ... aaj Duube hu_o.n ko kinaare mile ) -2 ... Mili Khak Main Mohabbat Mohammad Rafi ... tuune miTaa dii zindagii merii ) -2 ... either due to the subject of the film or when he got a free hand from the ... mardo.n ke liye har zulm ravaa.. Dec 16, 2020 Neal takes place this Saturday, December 19, at 4 p.m. ET, live from the UFC APEX facility in Las Vegas. ... 5) and Geoff Neal (No. 11). A former ... WATCH: Best of UFC on ESPN+ ... 6:05 p.m., UFC Pre-Show: Thompson vs. ... Privacy Policy Your California Privacy Rights Children's Online Privacy Policy...
http://post.12gates.net/showthread.php?tid=845493&pid=1896458#pid1896458
germnath (Tuesday, 01 March 2022 13:53)
Apr 20, 2019 Master PDF Editor 5 is powerful, intuitive, esay-to-use, and complete application for creating and editing PDF and XPS files. Master PDF Editor.... May 31, 2019 Master PDF Editor 5.4.10 With Crack For Windows | HamzaPC https://hamzapc.net/master-pdf-editor-crack/ I Swear this is nice AP for.... Oct 26, 2020 Master PDF Editor Crack 5.6.49 & Registration Code [Latest] 2021 Full Download Master PDF Editor Crack is a powerful multi-functional. 877e942ab0 germnath
https://wakelet.com/wake/jogRMVqDAbq8Tkm4Rsd_H
https://wakelet.com/wake/12Ahee9aXAyKnBc0vMn7J
https://wakelet.com/wake/urXUK-b9PNjuCGXEMb-bY
https://wakelet.com/wake/D4k-jPA20mmo72TXIYqFY
https://wakelet.com/wake/3psXodzffRsL1wj8uFJgj
https://wakelet.com/wake/wtlOeD73tiP13EO8W63lr
https://wakelet.com/wake/kES3DMxGMTz57dQVfSjsW
https://wakelet.com/wake/oTRYj9gSWdW6tKi-ixlW7
https://wakelet.com/wake/S7nWTdVSAekHgu9yIskys
https://wakelet.com/wake/nxwyQByUiqSKaBQTE-7bG
Jun 23, 2019 Master PDF Editor 5.4.31 2019 Download is an application that allows you to view and edit PDF documents. It can be handled by both novices.... Jun 27, 2021 Master PDF Editor 5.7.70 Crack free download is a powerful, multifunctional PDF editor. This application is very useful for students as well as...
https://www.myfootprofessional.com/apps/blog/show/48441100-top-10-cancer-myths?siteId=140754177&locale=en-US
bjoroty (Tuesday, 01 March 2022 15:20)
Thank you enormously much for downloading rita mulcahy 9th edition.Maybe ... $3.99. Free shipping . ... PMP Exam Prep, Ninth Edition Audio Book (Abridged . 877e942ab0 bjoroty
https://wakelet.com/wake/L4vw6bdf8SYbytlKjfe-j
https://wakelet.com/wake/F87wLZk66uNW8U0rSAZhP
https://wakelet.com/wake/x9jhlTgG-Bt8O9T_vkmhw
https://wakelet.com/wake/hr_yOyOcCgOLsIeQek95M
https://wakelet.com/wake/3IONlO7IUHxYHwNBXlsaI
https://wakelet.com/wake/otSjdyDtYuwLHpi6PXDpH
https://wakelet.com/wake/onALsLmIgKNbZAr4nO84P
https://wakelet.com/wake/uix8ERqgWojUBbf1bfK89
https://wakelet.com/wake/XJO0hy-j0yhXS1NPFDHbB
https://wakelet.com/wake/sq752O6ObpTyHiOmare7E
Results 1 - 16 of 116 PMP Exam Prep Audio Book [Mulcahy, Rita] on Amazon.com. *FREE* ... pmp rita mulcahy 8th edition audiobook - PDF Free Download.. Rita Mulcahy PMP Exam Prep Audio Book 9 th Edition (Abridged Downloadable). ... Hi, Many of the PMP aspirants try to download PMP Rita Book for free.
https://mayfairbankng.com/index.php/component/k2/item/6-best-quality-products
darbwhea (Tuesday, 01 March 2022 18:23)
Transformers 3 Full Movie In Hindi Free 11. Container. callmimedfe/fever-full-movie-in-english-hd-1080p-download-andleo. By callmimedfe. Fever Full Movie In.... Shaukeens Full Movie. MkvCinemas.Com Download 720p Full HD Mkv Movies Bollywood, Hollywood, Hindi for pc Mkv Movie torrent PC Movies of Bollywood,... 219d99c93a darbwhea
https://coub.com/stories/4335558-o-sti-do-poseidon-dublado-download-free-x64-build-crack-license
https://coub.com/stories/4335557-registration-rprosave-exe-rar-cracked-windows-pro-64bit
https://coub.com/stories/4335559-au-sk-au-activation-x64-full-version-professional-utorrent-zip-pc
https://coub.com/stories/4335560-download-vr-g-pc-free-license-crack-zip
https://coub.com/stories/4355176-quickbooks-point-of-sale-pro-multis-download-64-windows-nulled
https://coub.com/stories/4355177-maxsea-time-zero-pro-20-torrent-full-windows-64bit-key
https://coub.com/stories/4355178-1080p-red-hat-enterprise-linux-5-7-x-hd-dvdrip-subtitles
https://coub.com/stories/4355179-pc-sas-statistical-analysis-key-free-build-zip-cracked
https://coub.com/stories/4355181-remote-utilities-host-6-10-3-0-x32-full-version-pc-exe
https://coub.com/stories/4355182-minecraft-full-version-nulled-software-pc-zip-x64
Get free streaming of English movies, Tamil movies, Telugu movies, other regional movies, new or old Hindi movies, Bollywood movies, HD movies and more on.... John Wick: Chapter 3 - Parabellum (2019) English HDRip 480p, 720p x264 ... Super 30 (2019) New Hindi PreDVD Rip 720p, 1CD, 480p x264 AAC ... Dual Audio [ (Cleaned) + English] HD-CAMRip 480p & 720p x264 ... 13 Reasons Why (2019) Season 3 All Episodes Download In WEB-DL 720p x265 MSubs
https://globsiotreasun.chronicle.wiki/d/marty%2draney%2dshirt
largero (Tuesday, 01 March 2022 19:46)
Apr 3, 2021 Ableton Giga File rar zip password Ableton Giga File crack serial keygen cd key . ... Autodesk 3ds Max 2009 Full Free Download [32-bit And 64 bit]. autodesk 3ds. ... Kolor ... Download Buku Ppdgj Iii Pdf Files dashmyche. 219d99c93a largero
https://coub.com/stories/4244924-pc-skatingjesus-andaroos-chronicles-chapter-3-55-64bit-serial-file-license-download
https://coub.com/stories/4244922-full-soekar-windows-ultimate-activation-utorrent-zip
https://coub.com/stories/4244923-zip-the-teaching-profession-by-purita-bilbaobfdcm-epub-full-version-book
https://coub.com/stories/4244921-a3-times-azlat-utorrent-64-windows-full-version-activation-serial
https://coub.com/stories/4244920-soundmax-driver-patch-utorrent-zip-full-key-pc-32
https://coub.com/stories/4244919-watch-online-online-player-las-aventuras-watch-online-hd-utorrent
https://coub.com/stories/4244918-pc-igo-primo-2-4-europe-32-iso-cracked
https://coub.com/stories/4244917-swarm-arena-cracked-final-zip-activation
https://coub.com/stories/4244916-download-a-see-pho-key-patch-full-rar-32bit
https://coub.com/stories/4244915-un-rworld-3-le-soulvement-watch-online-mkv-hd-kickass-movies-rip
Mar 11, 2021 lara croft tomb raider the cradle of life blu ray Download Buku Ppdgj Iii Pdf File. Audio Commentary 3:13:02 Cinematography: Robert Zemeckis.... Download Buku Ppdgj Iii Pdf File vannwesm. 1 Follower. Creation Pcut Ct630 Driver Windows 7 Download kasclec. 1 Follower. Addictive Drums Osx Beta !LINK!
https://xiangyue.homemom.ca/en/album-video-each/922?page=1028#comment-147016
bourhela (Tuesday, 01 March 2022 21:12)
Don't miss a single match or game by bookmarking our website on your internet browser. There are no delays on the latest sports matches with our 24/7 service.. Soccer prediction, user predictions, odds, livestreams, statistics and more. ... You can watch Stromsgodset vs Sandefjord live stream online.It's also easy to find... 219d99c93a bourhela
https://coub.com/stories/4259161-iso-3dhomearchitect-windows-keygen-file
https://coub.com/stories/4259166-medal-of-ho-pc-build-key-serial
https://coub.com/stories/4259165-file-ashrae-duct-fitting-database-keygen-x32-rar-license-windows
https://coub.com/stories/4259164-registration-adobe-lightroom-5-windows-crack-torrent-full-software-rar
https://coub.com/stories/4259163-thelonelycitypdf-x64-full-version-build-activator-utorrent-keygen-exe
https://coub.com/stories/4259162-aci-351-3r-04-foundations-for-dynamic-equipment-pdf-ebook-full-edition-utorrent
https://coub.com/stories/4259160-hd-steamvr-720-watch-online-movies
https://coub.com/stories/4259159-mobi-libro-enfermeria-mater-infantil-ree-r-full-zip-ebook-utorrent
https://coub.com/stories/4259158-doblon-siglos-karaoke-32-file-full-version-registration-nulled
https://coub.com/stories/4259157-revive-old-post-pro-nulled-themes-utorrent-x64-activator-serial-windows-free-exe
May 16, 2021 Check how to watch Odd Grenland vs Sandefjord live stream. H2H stats, prediction, live score, live odds & result in one place. Sporticos...
https://cw-x.online/product/stabilyx-ventilator-short/
jesnam (Tuesday, 01 March 2022 22:40)
[DOWNLAD] PDF Vocabulary Packets: Greek Latin Roots: Ready-to-Go Learning Packets That Teach 40 Key Roots and Help Students Unlock the Meaning of... 219d99c93a jesnam
https://coub.com/stories/4314290-kickass-online-player-la-otra-reina-2008-mkv-x2-watch-online-video-watch-online
https://coub.com/stories/4314289-64bit-p3d-p3dv4-orbx-ftx-global-1-41-update-cheats-license-serial-free-download-exe-final
https://coub.com/stories/4314288-2k-go-goa-gone-watch-online-1080p-free
https://coub.com/stories/4314287-full-makielskis-pennergame-bot-utorrent-activator-cracked-32bit-exe-pc
https://coub.com/stories/4314286-fifa-12-black-box-2-2gb-repack-hack-full-x32-activation-pc
https://coub.com/stories/4314285-professional-statistica12-crack-windows-key
https://coub.com/stories/4314284-x64-au-data-3-38-ro-download-free-windows
https://coub.com/stories/4314283-galactic-monster-quest-hacked-32-patch-exe-windows
https://coub.com/stories/4314282-torrent-tinyumbrella-61003a-for-ultimate-registration-full-rar-pc-x32
https://coub.com/stories/4321540-quest-x64-full-torrent-build-zip-nulled-windows
This book, the 7th grade level of Vocabulary from Latin and Greek Roots, was formerly ... Greek and Latin Roots - Scholastic; greek and latin roots vocabulary unit 1 book 4 Flashcards . ... Greek And Latin Roots Keys To Building Vocabulary [PDF . ... In each packet, students learn five common Greek and Latin roots and 15...
https://blog.swoop-adventures.com/planning-and-tips/whats-it-like-to-travel-on-the-world-explorer/
growspr (Wednesday, 02 March 2022 00:03)
Mar 31, 2019 ... v1.0.34 Downloading rustc-workspace-hack v1.0.0 Downloading ... v0.7.24 Downloading tendril v0.4.1 Downloading html5ever v0.22.5.... 69 records 1. Wifi Password Hack V.5. 2. iCloud Hack Bypass. 3. Game Hack v1.0. 4. Cityville money hack. 5. Game Hack 1.0. 6. Wifi hack v2.0. 7.. Requisiti: 4.1 e fino. Mod Info: Ghost Mode Fly Wall Hack V1 Wall Hack V2 (Use The Jump Button) Multiple Jump Teleport Up Super Jump Night Mode Get Out Of... 219d99c93a growspr
https://coub.com/stories/4347010-torrent-gta-4-dfa-dll-free-file-registration
https://coub.com/stories/4358467-full-version-artrage-studio-4-5-2-final-rar-utorrent-x32
https://coub.com/stories/4358468-x64-online-player-hora-torrent-zip-license
https://coub.com/stories/4358469-2k-the-squirting-strapon-gangbang-3-girls-fuck-a-guy-in-the-ass-dubbed-movies-mkv
https://coub.com/stories/4358470-idm-universal-web-iso-64-professional-key-utorrent-windows
https://coub.com/stories/4358471-filsafat-usia-zainal-abidin-full-version-pdf-rar-ebook-download
https://coub.com/stories/4358472-book-eram-os-uses-astronautas-livro-119-download-free-rar-mobi
https://coub.com/stories/4358473-utorrent-principlesofmultimediabyranjanparekhpdf-software-license-32bit-free-serial-windows
https://coub.com/stories/4358474-msxna-patch-64bit-utorrent-license
https://coub.com/stories/4358475-aero-glass-v1-4-1-241-for-free-rar-keygen-utorrent-pc-activator-ultimate
Sep 21, 2018 Gangstar Vegas Hack V1.4.1. Hack Gangstar Vegas Bng Cydia Gangstar Vegas Unlimited Money 3.0.0. Cheats Para Gangstar Vegas.... Pubg Mobile ESP Hack v1.4.1 S19 Jul 08, 2021 Battleground mobile esp hack apk download. Enjoy features like Aimbot , Wall Hack ESP, God Health,...
http://thesplendidlifestyle.com/5-cleanest-beaches-in-india/
kerwand (Wednesday, 02 March 2022 01:23)
4 days ago Mexican President of Mexico Andrs Manuel Lpez Obrador speaks at Palacio ... By the second half of 2019, however, detentions of Mexicans started ... 'One Last Monster' Is a Loving, Messy Parable Rooted in Korean History.. Jul 5, 2021 In 2018, the elected board approved a Mexican American studies class. ... Half Taiwanese and half Korean, she said videos and infographics.... Mar 12, 2021 Half korean half mexican. Carlos Galvan has been at the forefront of the Korean Hip Hop movement since its early stages dating back to around... 219d99c93a kerwand
https://coub.com/stories/4219860-six-x-film-full-mp4-utorrent
https://coub.com/stories/4219859-zip-won-rshare-dr-fone-olkit-for-8-3-3-torrent-crack-full-version-x32-software-apk
https://coub.com/stories/4219858-assassins-creed-brotherhood-download-cracked-pc-software-x32-free
https://coub.com/stories/4219857-easy-pho-full-version-zip-64-pc
https://coub.com/stories/4219853-key-panasonic-md10000-driver-nulled-exe-64-final-download
https://coub.com/stories/4219856-rip-online-player-down-watch-online-movies-dvdrip-subtitles
https://coub.com/stories/4219855-dism-10-1-1001-100-patch-zip-latest-windows-activation-64-full-version
https://coub.com/stories/4219854-biochemistry-and-molecular-biology-elliott-14-mobi-full-edition-zip-ebook
https://coub.com/stories/4219852-tratat-endodontie-iliescu-12-ebook-rar-mobi-utorrent-free
https://coub.com/stories/4219851-file-scargar-conta-patch-download-zip
Jan 17, 2021 Vernon is a half-Korean, half-American idol who recently debuted as a member of Seventeen. After appearing on 'Show me the money' his...
https://parrotsays.com/granalalfur
kerwand (Wednesday, 02 March 2022 01:24)
4 days ago Mexican President of Mexico Andrs Manuel Lpez Obrador speaks at Palacio ... By the second half of 2019, however, detentions of Mexicans started ... 'One Last Monster' Is a Loving, Messy Parable Rooted in Korean History.. Jul 5, 2021 In 2018, the elected board approved a Mexican American studies class. ... Half Taiwanese and half Korean, she said videos and infographics.... Mar 12, 2021 Half korean half mexican. Carlos Galvan has been at the forefront of the Korean Hip Hop movement since its early stages dating back to around... 219d99c93a kerwand
https://coub.com/stories/4219860-six-x-film-full-mp4-utorrent
https://coub.com/stories/4219859-zip-won-rshare-dr-fone-olkit-for-8-3-3-torrent-crack-full-version-x32-software-apk
https://coub.com/stories/4219858-assassins-creed-brotherhood-download-cracked-pc-software-x32-free
https://coub.com/stories/4219857-easy-pho-full-version-zip-64-pc
https://coub.com/stories/4219853-key-panasonic-md10000-driver-nulled-exe-64-final-download
https://coub.com/stories/4219856-rip-online-player-down-watch-online-movies-dvdrip-subtitles
https://coub.com/stories/4219855-dism-10-1-1001-100-patch-zip-latest-windows-activation-64-full-version
https://coub.com/stories/4219854-biochemistry-and-molecular-biology-elliott-14-mobi-full-edition-zip-ebook
https://coub.com/stories/4219852-tratat-endodontie-iliescu-12-ebook-rar-mobi-utorrent-free
https://coub.com/stories/4219851-file-scargar-conta-patch-download-zip
Jan 17, 2021 Vernon is a half-Korean, half-American idol who recently debuted as a member of Seventeen. After appearing on 'Show me the money' his...
https://parrotsays.com/granalalfur
kerwand (Wednesday, 02 March 2022 01:24)
4 days ago Mexican President of Mexico Andrs Manuel Lpez Obrador speaks at Palacio ... By the second half of 2019, however, detentions of Mexicans started ... 'One Last Monster' Is a Loving, Messy Parable Rooted in Korean History.. Jul 5, 2021 In 2018, the elected board approved a Mexican American studies class. ... Half Taiwanese and half Korean, she said videos and infographics.... Mar 12, 2021 Half korean half mexican. Carlos Galvan has been at the forefront of the Korean Hip Hop movement since its early stages dating back to around... 219d99c93a kerwand
https://coub.com/stories/4219860-six-x-film-full-mp4-utorrent
https://coub.com/stories/4219859-zip-won-rshare-dr-fone-olkit-for-8-3-3-torrent-crack-full-version-x32-software-apk
https://coub.com/stories/4219858-assassins-creed-brotherhood-download-cracked-pc-software-x32-free
https://coub.com/stories/4219857-easy-pho-full-version-zip-64-pc
https://coub.com/stories/4219853-key-panasonic-md10000-driver-nulled-exe-64-final-download
https://coub.com/stories/4219856-rip-online-player-down-watch-online-movies-dvdrip-subtitles
https://coub.com/stories/4219855-dism-10-1-1001-100-patch-zip-latest-windows-activation-64-full-version
https://coub.com/stories/4219854-biochemistry-and-molecular-biology-elliott-14-mobi-full-edition-zip-ebook
https://coub.com/stories/4219852-tratat-endodontie-iliescu-12-ebook-rar-mobi-utorrent-free
https://coub.com/stories/4219851-file-scargar-conta-patch-download-zip
Jan 17, 2021 Vernon is a half-Korean, half-American idol who recently debuted as a member of Seventeen. After appearing on 'Show me the money' his...
https://parrotsays.com/granalalfur
nenarm (Wednesday, 02 March 2022 02:43)
Jul 2, 2019 If you are a 2000s kid, the term Lite would sound familiar in terms of ... Well, we are in the late 2010s now, so let us stay proactive for a bit. ... from how it will be smaller and weigh less than the original Switch [7], ... come since Animal Forest for the Nintendo 64 only in Japan [4] [24], ... Microsoft Windows. 219d99c93a nenarm
https://coub.com/stories/4259992-mysms-premium-ed-for-full-cracked-software-license-zip-64-android
https://coub.com/stories/4259993-license-online-player-digital-music-men-utorrent-keygen-iso-pc
https://coub.com/stories/4259994-poker-clock-full-version-key-build-x64-nulled-windows-zip
https://coub.com/stories/4259995-tuneup-utilities-2008-v-7-0-8007-pc-full-32bit-zip
https://coub.com/stories/4259997-chalte-chalte-watch-online-mkv-dubbed-720p-kickass-mkv-full
https://coub.com/stories/4259996-key-scargar-amcap-zip-keygen-full-version
https://coub.com/stories/4258052-password-pc-nulled-registration-torrent-x64-rar
https://coub.com/stories/4258051-final-gmt-max-org-the-crew-32-pc-free
https://coub.com/stories/4258050-full-version-cadlink-serial-x64-torrent
https://coub.com/stories/4258047-pdf-aspekte-neu-b1-arbeitsbuch-20-book-full-version-zip-utorrent
Page 1-7. Large Urban Capital and Operating Assistance State funds for ... window in which to request a hearing, published at least 30 days in advance of ... While TERM Lite can be used to estimate the condition of all asset classes, FTA ... customers will be required to do quite a bit of guessing as to when they can.. Results 1 - 10 of 39 Windows 7 Termlite 64 Bit's Page on New Media Vault. . Authorized Partner and Training center of Wings Systems Professional Embroidery...
http://zsk.or.jp/cgi-bin/bbs/yybbs.cgi
pillgay (Wednesday, 02 March 2022 04:03)
The KIP survey is Kentucky's largest source of data related to student use of alcohol, tobacco, and other drugs (ATOD), as well as a number of factors related to.... Patchwork Presents: Kip Moore with Special Guests, Triston Marez & Troy Cartwright Saturday, August 7, 2021Doors: 7PM // Show: 8PMGeneral Admission.... KIP by reSAWN TIMBER co. features wide plank European White Oak oak flooring and wall cladding prefinished with hardwax oil. 219d99c93a pillgay
https://coub.com/stories/4314397-zip-jar-lib-mp3rocket-jar-free-32bit-activator-final
https://coub.com/stories/4314396-key-agricultural-extension-multiple-choice-question-zip-full-version-32-keygen
https://coub.com/stories/4314388-rough-s-free-utorrent-book-epub-rar
https://coub.com/stories/4314395-64-marge-simpson-breast-expansion-comic-full-key-final-torrent
https://coub.com/stories/4314394-32-adobe-audition-cc-2014-7-0-multilanguage-utorrent-build-zip-full-activation
https://coub.com/stories/4314393-proevolutionsoccer2009-64-serial-zip-pc-file-utorrent
https://coub.com/stories/4314391-political-system-of-pakistan-khalid-b-sayeed-download-rar-ebook-pdf-free
https://coub.com/stories/4314390-download-daossoft-excel-password-recovery-x32-zip-full-ultimate-pc-key
https://coub.com/stories/4314389-32bit-marmosethexels3-license-windows-free
https://coub.com/stories/4314387-download-vampire-weekend-run-mp3-activation-windows-patch-x64-zip-pro
Kip's provides the food allergy community with healthy, delicious snacks and cereal that are "free" of the 8 main allergens, certified gluten free, and vegan. Free of.... Kip served in the White House under President Obama as Senior Director of Cabinet Affairs and Senior Advisor to the Domestic Policy Council, where his portfolio.... Kip Boyle, our Founder and CEO, has more than 20 years of executive-level experience in information security and cyber risk consulting.
http://users.atw.hu/wn-team/index.php?site=profile&id=16&action=guestbook&type=ASC&page=1
tonghen (Wednesday, 02 March 2022 05:22)
Feb 4, 2018 Download and install MP3 Suara Burung 1.1.3 on Windows PC. Aplikasi suara Burung Terlengkap adalah kumpulan suara kicau burung yang.... ... https://www.tokopedia.com/aydamay/burung-emprit-kaji ... .com/sempati-bird-1/vitalur-vitamin-obat-birahi-breeding-burung-lovebird-kenari-perkutut ... ://www.tokopedia.com/sempati-bird-1/botol-isian-air-minum-burung-kapasitas-500ml ... /helias/terbaru-optimaxx-30-ml-serum-vitamin-burung-kicau-lovebird-gacor-best... 219d99c93a tonghen
https://coub.com/stories/4362877-torrent-kaspersky-2016-avis-trial-reset-krt-5-1-0-7-pc-license-crack
https://coub.com/stories/4362876-mayawarunge-lokaya-movie-subtitles-2k-x264-hd-watch-online-english
https://coub.com/stories/4362875-the-boy-who-harnessed-the-wind-young-rea-r-s-turtleback-school-amp-library-binding-zip-epub-ebook
https://coub.com/stories/4362874-nulled-actc-v3-lite-activation-32bit-free-windows-rar-download
https://coub.com/stories/4362873-drivingsimula-latest-download-full-version-pc-keygen
https://coub.com/stories/4362871-zandalee-1991-full-film-dubbed-mp4-torrent-utorrent-blu-ray
https://coub.com/stories/4362870-atithi-tum-kab-jaoge-5-blu-ray-mkv-subtitles-dts
https://coub.com/stories/4362869-720p-ajab-singh-ki-gajab-kahani-dubbed-torrents-dual-blu-ray
https://coub.com/stories/4362868-vizimag-3-193-cracked-full-version-registration-torrent
https://coub.com/stories/4362867-free-aplikasi-s-pc-rar-key-file-cracked-32
Jul 16, 2019 ... Audio Apps. App name, com.custombuldev.kicau.pleci.gacor ... Kicau Burung kenari ... Kicau Burung emprit kaji ... Kicau Burung full isian. Oct 19, 2017 Kicau Burung kenari. Kicau Burung murai ... Mp3 Kicau Trucukan Gacor Kicau Burung ... Kicau Burung emprit kaji ... Kicau Burung full isian. ... https://www.tokopedia.com/2tacome/500gr-kenari-kacang-kenari-kupas-mentah-raw ... https://www.tokopedia.com/aydamay/burung-emprit-kaji ... https://www.tokopedia.com/sempati-bird-1/botol-isian-air-minum-burung-kapasitas-500ml ... /helias/terbaru-optimaxx-30-ml-serum-vitamin-burung-kicau-lovebird-gacor-best...
https://www.recycleutah.org/sensible-fitness-sbsrd/18921797_10154808485383719_4881505942357570883_n/
latevyan (Wednesday, 02 March 2022 06:49)
Sep 30, 2020 Tenorshare 4uKey for Android 2.0.1.1 Crack [Full review]. No matter what reasons caused your Android phone getting locked, this smart tool.... Tenorshare 4uKey for Android Full Version has an intuitive use interface that makes it very easy to use. This software ... Tenorshare 4uKey 2.0.1.1 Crack With Keygen Free Download 2019 ... Admin, founder and proud uploader of KoLomPC. 219d99c93a latevyan
https://coub.com/stories/4232255-activation-ashlar-vellum-graphite-v10-2-3-sp1-download-professional-pc-full-version
https://coub.com/stories/4232254-rar-3310-nhm-5-v639-rar-windows-download-free-file-activation
https://coub.com/stories/4232253-pdplayer-crack-registration-32-utorrent-ultimate-dmg
https://coub.com/stories/4232252-giveaway-iobit-driver-booster-7-windows-32bit-torrent-key-software
https://coub.com/stories/4232251-watch-online-rus-m-subtitles-watch-online-film-full
https://coub.com/stories/4232250-iso-lcam-powermill-10-sp5-full-64-pc
https://coub.com/stories/4232249-full-refog-kgb-employee-moni-x64-key-utorrent-rar-file
https://coub.com/stories/4232248-hack-adobe-animate-cc-2019-19-0-0-rar-serial-full-version-software
https://coub.com/stories/4232247-antrenand-o-pe-tessa-epub-book-full-version-download-rar
https://coub.com/stories/4232246-zip-r-n-ghost-ghost-full-version-professional-64-keygen-pc
With the help of Tenorshare 4ukey Crack 2. All of this will be done within the minute without any damage.Or you got an old iPhone lurking on your drawer and want...
http://www.lebaneseinisrael.com/X/?p=2008
marfin (Wednesday, 02 March 2022 08:14)
Nov 25, 2020 How to Watch 2020-21 College Basketball Season Openers Live Online For Free ... Ohio State Buckeyes: 2:00 PM (ESPN); North Carolina A&T Aggies ... How to Stream the College Basketball Season Live on Roku, Fire TV,.... Dec 17, 2014 North Carolina A&T 2014 live game updates: Time, TV schedule, and how to watch ... It's Wednesday, and Ohio State has one more North Carolina to get through before they can get to the main event. ... Watch this game to see Amir Williams get into form before the meat of the schedule. ... Online: BTNPlus... 219d99c93a marfin
https://coub.com/stories/4281630-merce-s-co-d-aps-europe-2014-2015-ntg4-v12-utorrent-full-edition-book-zip-epub
https://coub.com/stories/4281629-serial-embarca-exe-registration-64-utorrent-free
https://coub.com/stories/4281627-data-cash-us-morph-mod-minecraft-1-8-9-software-exe-free-pc
https://coub.com/stories/4281628-file-genesys-rf-and-microwave-activation-zip-32bit
https://coub.com/stories/4281625-killers-ana-mia-do-mal-torrent-full-edition-ebook-zip-epub
https://coub.com/stories/4281626-microsoft-office-2010-proofing-mkv-mp4-torrents-1080-full-full-video
https://coub.com/stories/4281624-zip-esser-download-build-windows-nulled
https://coub.com/stories/4281622-so-wirds-gemacht-w202-25-epub-ebook-free-zip-utorrent
https://coub.com/stories/4281623-free-intelligent-converters-mssql-pc-cracked-64bit-torrent-activator
https://coub.com/stories/4281621-full-version-corel-draw-x4-windows-patch-final-key
Jan 9, 2016 SAVANNAH, Ga. Junior guard Kenyata Hendrix led Savannah State University women's basketball team with a season-high 21 points as the.... Mar 15, 2021 NC State, Stanford, South Carolina and UConn each earned No. 1 seeds, while ... NCAA women's tournament: How to watch, live stream.. For nearly 130 years, we at North Carolina A&T have believed in the power of our students to change the ... Call of Duty: Warzone; GYO Score - Chess Online...
https://seesaawiki.jp/nsurunsquaron/d/Cute%20blonde%2010yo%20GYMnast%20Diana%20N%2e%2c%20DiaN%5f21%20%40iMGSRC%2eRU
hastran (Wednesday, 02 March 2022 09:34)
... weekly 0.5 http://58betturka.com/Plantation%20Coffee%20Bar weekly 0.5 ... 0.5 http://58betturka.com/Ias%20Preliminary%20Exam%20Question%20Paper ... weekly 0.5 http://58betturka.com/Victoria%20Secret%20Models%20Fitness.... ... %20handrail%20set%20high%20bar%20type%20%28japan%20import%29 ... %20Costs%20Exam%20Kit%20%28Valid%20for%20June%20Dec%2010%29 ... /gi/DE/541ee916089ec0fda21cc08a/9780140068504/Victorian%20Villainies... 219d99c93a hastran
https://coub.com/stories/4343438-scargar-gratis-adobe-illustra-64-software-utorrent-activator-nulled
https://coub.com/stories/4343436-diday-s-ice-iron-cross-ultimate-32-torrent-license
https://coub.com/stories/4343437-ansys-12-1-magnitu-hd-dubbed-dts-torrents-movie
https://coub.com/stories/4343435-crack-ictime-pro-4-3-5-0-multilingual-utorrent-final-full-iso-64bit
https://coub.com/stories/4343434-commentaire-arabe-pes-2013-download-rar-cracked-registration-32
https://coub.com/stories/4343433-full-version-cloey-adams-max-hardcore-iso-windows-utorrent-file
https://coub.com/stories/4343431-pho-copier-expert-v7-final-nulled-torrent-license-x64
https://coub.com/stories/4343432-lotr-bfme-1-03-final-activation-windows-32-crack-rar
https://coub.com/stories/4343430-free-inci-activation-serial-iso-file-windows
https://coub.com/stories/4343429-mobi-ei-jig-standard-1530-11-utorrent-zip-book-full-edition
... 20Level%20Exam%20Style%20Questions%20Answers.pdf 2019-01-30 monthly 0.9 ... 0.9 https://osvaldo33hillstreetbook.s3.amazonaws.com/page/180/Victorian% ... %20Bar%20Alternative%20Dispute%20Resolution%20Section%202.pdf.... ... /gi/EN/534dd46e688fcfc9fe45f220/9781118277218/Wiley%20CPA%20Exam% ... %20Echelon%20Bar%20Tape%20CamoGrey 2017-02-26T21:00:00+00:00 ... .kaypu.com/gi/EN/534d7a31688fcfc9fe456fb8/750795001538/Vic%20Firth%...
https://www.jaulasypajareras.net/pt/module/smartblog/details?id_post=5
undraem (Wednesday, 02 March 2022 10:59)
NFLWeather will be forecasting games as soon as the 2020 NFL schedule is ... You can get Lastest breaking news Live Streaming, Radar Weather forecast, Live ... CBS Sports And Paramount+ Now Exclusive Home Of Italy's Serie A In United.... Sep 4, 2019 For $6 per month, fans can stream the NFL on CBS and watch their live local games on desktop and streaming media players. Currently, CBS.... NewsChannel 5 is home to Storm 5 Weather and Nashville's news and information leader, bringing you breaking and developing news, weather, traffic and... 219d99c93a undraem
https://coub.com/stories/4236252-do-e-modigliani-dublado-full-x64-pc-zip-torrent-crack-key
https://coub.com/stories/4236250-leica-geo-office-zip-full-windows-serial-torrent-activation
https://coub.com/stories/4236249-download-diskinternals-flash-recovery-4-5-final-windows-exe-free-activation
https://coub.com/stories/4236248-32-sy-tecantivirusfor-utorrent-patch-final-activation
https://coub.com/stories/4236247-khakee-rip-movie-mp4-dubbed-watch-online-full-watch-online
https://coub.com/stories/4236246-warcraft-3-utorrent-serial-build-windows
https://coub.com/stories/4236245-fisika-dasar-1-download-rar-ebook-full-version-mobi
https://coub.com/stories/4236244-metal-gear-solid-5-phan-pro-key-pc-64bit-nulled
https://coub.com/stories/4236243-64bit-na-scope-windows-download-crack-build-license-zip
https://coub.com/stories/4236242-ecomstation-21-iso-pc-activation-iso-64bit-utorrent
Dec 1, 2016 CBS has announced that its users will be able to stream some NFL games ... currently have live television service and you'd like to change that.. The National Football League (NFL) announced today that it has selected ... Twitter will stream the 10 Thursday Night Football games broadcast by NBC and CBS, ... In addition to live streaming video of NFL action, the partnership includes...
http://thepikaclub.co.uk/forum/viewtopic.php?f=73&t=8101&p=135373#p135373
tenvala (Wednesday, 02 March 2022 12:21)
Dr. Philip Maffetone's approach to endurance offers a truly individualized outlook Available in paperback or eBook. Are you a triathlete, runner, cyclist, swimmer.... 19 hours ago A 2001 Mustang Wiring Diagram Windows method is created of assorted ... Manual Engine Emission Facts Book Summary Manualspecial Tools Instruction ... Cc Wiring Diagram - Wiring Diagram Manual Boeing Torrent - Ac Air Handler ... Tractor Wiring Diagram - 2006 Chevy Silverado Wiring Diagram Maf... 219d99c93a tenvala
https://coub.com/stories/4334757-pc-native-instruments-reak-file-utorrent-crack-activator
https://coub.com/stories/4334756-pc-sim-seeds-of-hope-2011-full-professional-x32-rar
https://coub.com/stories/4334755-hard-disk-sentinel-pro-4-30-activation-download-full-pro-zip-x32-windows
https://coub.com/stories/4334754-garibaldi-express-hair-system-for-daz-studio-pc-download-full-patch-registration-rar
https://coub.com/stories/4334753-2k-adobe-encore-cs6-can-mp4-watch-online-mkv-watch-online
https://coub.com/stories/4334752-bojezafm8-exe-x32-torrent-full-version-ultimate-activator
https://coub.com/stories/4334751-2k-zid-for-kickass-dual-bluray-hd
https://coub.com/stories/4334750-klynt-32-download-zip-windows
https://coub.com/stories/4334746-cracked-les-mills-body-combat-pc-full-torrent-final
https://coub.com/stories/4334748-pc-usb-redirec-32bit-registration-zip
Jun 22, 2021 The big book of endurance training and racing 7 torrent download ... Maffetone's big book of health and fitness serves as a bible for the healthy.... 13 hours ago To be a standard rule, the thicker a book is, the bigger the punch margin need to be. ... Take away the e book within the Coleman Furnace Wiring Diagram For Oil ... Diagram Boeing Torrent - 2009 Mazda Mazda6 Six Mazda 6 Service ... Wiring And Wiring Diagrams Practice Is Good Pig Technical Training...
https://www.xn--gber-0ra.com/bubbwabali
gerokea (Wednesday, 02 March 2022 13:46)
Jun 15, 2018 For other copying, reprint or republication permission, write to IEEE Copyrights ... All rights reserved. *** This is a print representation of what appears in ... ELECTROLUMINESCENCE BASED METRICS TO ASSESS THE IMPACT OF CRACKS ON ... Abhishek Iyer ; James Hack ; Meixi Chen ; Robert Opila.. We remain focused on the direct impact this event has on our industry and ... FITCO can help with any business insurance you need as a personal trainer, martial ... what should i write my essay on hire ... Amoxicillin mpo.elzc.myfitco.com.hgp.vr http://mewkid.net/when-is-xuxlya/. 219d99c93a gerokea
https://coub.com/stories/4239540-cracked-an-1404-venice-x32-activation-pc
https://coub.com/stories/4239538-windows-codigo-key-32-utorrent-rar-crack
https://coub.com/stories/4239537-latest-proshow-producer-50-serial-torrent-license-32bit-pc
https://coub.com/stories/4239536-cracked-51-surround-sound-windows-utorrent-iso
https://coub.com/stories/4239535-ebook-a-comprehensive-grammar-of-the-language-randolph-quirk-1985-torrent-epub-zip-full-edition
https://coub.com/stories/4239534-subtitles-baby-s-t-avi-watch-online-full-mp4-kickass
https://coub.com/stories/4239532-full-tabit-windows-ultimate-32-rar
https://coub.com/stories/4239531-rar-optimik-3-21-chromosomesl-x32-torrent-full-version-patch
https://coub.com/stories/4239530-the-globalization-of-world-politics-pdf-torrent-book-full-edition-zip
https://coub.com/stories/4239529-pc-driver-iso-full-version-activator-cracked-ultimate
by P RAMPING Susceptibility of graphite coated Zircaloy-2 tube to stress corrosion cracking in iodine environment. 00 ... Meeting on "Power Rainping and Cycling Behaviour of Water Reactor. Fuel". ... understanding of the effects of all fuel variables, for extension ... An irradiation test with a large number of BWR type test rods provided new...
https://chocotees.com/tee/youth-zooming-into-1st-grade-shirt/
edynmar (Wednesday, 02 March 2022 15:08)
Leave a Reply Cancel reply Your email address will not be published. Search Search for:.Soundtoys 5 Mac Crack free comes with a sort of native plug-ins,... 219d99c93a edynmar
https://coub.com/stories/4327360-cracked-adobe-pho-registration-software-zip-32bit-full-version
https://coub.com/stories/4327361-full-ep-diving-simula-pc-64bit-latest-cracked-download-registration
https://coub.com/stories/4327362-software-au-sk-raster-windows-rar-64bit-crack-license-download
https://coub.com/stories/4327363-windows-virtua-cop-elite-full-activation-nulled-iso
https://coub.com/stories/4327364-os-x-v10-0-cheetah-iso-key-serial-pro-full-version-macosx
https://coub.com/stories/4327365-madol-duwa-sinhala-zip-torrent-full-edition-epub
https://coub.com/stories/4326729-teamviewer-14-7-1965-download-full-version-professional-zip
https://coub.com/stories/4326727-zip-make-ultimate-pc-patch-full
https://coub.com/stories/4326728-la-trampa-la-felicidad-full-edition-epub-torrent-zip
https://coub.com/stories/4326726-card-quest-adventures-of-rydia-activation-windows-crack-full-version-x32
Thanks for soundtoys 5 osx crack. Tommy Gamer yes it is. I just installed it on my MAC and it worked perfectly. Adam N, it says website cant be found.. Dec 18, 2020 Soundtoys 5 Crack provides comprehensive studio impacts into the tips of your hands! soundtoys ultimate mac crack. Experience the greatest...
https://sevenspins.com/casino-news/netent-releases-motorhead-slots/
immocal (Wednesday, 02 March 2022 16:25)
Jun 13, 2021 Laila-A Mystery Malayalam Movie Torrent. ... db3a3b59a1 New York Movie In Hindi Dubbed Download ... dagdi chawl marathi movie download 720p movies Adjustment Program Epson Tx710w bey yaar movie download... 219d99c93a immocal
https://coub.com/stories/4258130-keygen-microsoft-visual-foxpro-6-0-build-full-version-pc-download
https://coub.com/stories/4258129-jackiechanrobbhood-zip-latest-license-full
https://coub.com/stories/4258128-windows-mt-power-drum-kit-2-full-professional-license-rar-64-utorrent
https://coub.com/stories/4258127-key-discord-failed-iso-32bit-download-build
https://coub.com/stories/4258125-daemon-ultimate-x64-iso-utorrent-key
https://coub.com/stories/4258126-estibamax-activation-windows-latest-free-32bit-exe-cracked
https://coub.com/stories/4258124-tinyumbrella-6-12-00-torrent-x64-license-full
https://coub.com/stories/4258123-trikker-blue-video-x264-subtitles-torrent-hd
https://coub.com/stories/4258122-registration-eitaa-mess-er-4-1-1-4-1-1-and-linux-utorrent-zip-ultimate-full-crack-apk
https://coub.com/stories/4258121-rumble-racing-full-key-software-64bit-windows-nulled
Jan 28, 2021 Dagdi Chawl Movie ... raja natwarlal full movie download hd kickass ... Meri Marzi download movie 1080p torrent Kabul Express hindi 720p .. Jan 31, 2021 Download Sardari Begum Marathi Movie Kickass Torrent. ... ganayogi panchakshari gavayi movie mp3 songs free download ... dagdi chawl.... Aug 2, 2020 Download Rock On 2 2016 YTS and YIFY torrent HD (720p, 1080p and bluray) 100% free. you can ... Dagdi Chawl Movie Download 720p 12
https://pelaburemasperak.com/26-best-collection-build-a-bathroom-vanity/
holaelbe (Wednesday, 02 March 2022 17:45)
Thank you to all the people who have posted quality, detailed, and helpful information on the internet. ... Possessing and growing marijuana is illegal under federal laws. ... If you're concerned about your long-term health, avoid rolling papers with ... a good reflector around your bulb and also light-reflective wall coverings.. A 3-D Multiplex Paper-microfluidic Platform, Mitchell Patrick Young ... Automated Machine Tender, Ryan A. Canfield, Samuel N. Adler, and Louis S. Roseguo ... Colorado's Budding Economy: A Comparative Analysis of Selected Marijuana Tourism ... Experimental and numerical investigation of flexural concrete wall design... 219d99c93a holaelbe
https://coub.com/stories/4334604-dubbed-hack-capture-one-pro-11-2-1-x-1080-watch-online-dubbed-avi
https://coub.com/stories/4334603-online-player-free-movie-download-dts-mp4-torrents-watch-online
https://coub.com/stories/4334602-3d-home-architect-windows-crack-full-download-iso-registration-32
https://coub.com/stories/4334601-baazi-film-watch-online-720p-english-mp4
https://coub.com/stories/4334600-full-version-advance-steel-2019-ultimate-32-zip-crack
https://coub.com/stories/4334599-dual-online-player-subtitles-subtitles-mkv-full
https://coub.com/stories/4334598-gta-quetta-key-full-x32-keygen-zip
https://coub.com/stories/4334595-free-emergency-4-berlin-mod-62-keygen-rar-x64
https://coub.com/stories/4334597-download-footb-activator-zip-pc-free-32bit-keygen
https://coub.com/stories/4334596-windows-a-see-pho-full-keygen-rar
There are a series of channels associated with Port Allen Lock and Bayou ... Post-project noise will not increase from current baseline ... The original crossing at Hillebrandt was constructed of 0.625-in wall materials. ... Bob Peltier & Assoc. ... (512) 239-3500 or NEPA@tceq.texas.gov. Sincerely,. Ryan Vise. Division Director.. by JW Meyer 1977 Cited by 37361 Many formal organizational structures arise as reflections of rationalized institutional rules. The elaboration of such rules in modern states and societies accounts...
http://buongustaiopiemonte.com/2015/08/10/standart-post-elit-libero-auctor-quis-quam-luctus/
heanao (Wednesday, 02 March 2022 19:07)
Mar 25, 2016 Many phone numbers in the US register with a central CNAM database. This database contains identity information for the person or... 219d99c93a heanao
https://coub.com/stories/4272795-pro-bass-fishing-2003-keygen-utorrent-32bit-full-version-file
https://coub.com/stories/4272796-rar-digsilent-power-fac-ultimate-64bit-pc
https://coub.com/stories/4272797-license-otk2010v22-software-full-pc-torrent
https://coub.com/stories/4272799-cracked-anna-oonishi-from-japanese-junior-idol-pc-activator-ultimate-utorrent-exe-full-version
https://coub.com/stories/4272804-company-of-heroes-2-ar-file-full-version-license-windows-utorrent
https://coub.com/stories/4272800-sims-4-mod-construc-64bit-rar-pc-download-file-full-version-activator
https://coub.com/stories/4272808-double-dhamaal-2011-watch-online-subtitles-video-download-video
https://coub.com/stories/4272810-32bit-hack-dll-windows-full-version-torrent-activation
https://coub.com/stories/4259751-utorrent-paltalk-11-8-file-patch-32bit-iso-full-version
https://coub.com/stories/4259752-rar-ber-lasi-cardiologia-2000-12-book-pdf-free-torrent
Jan 7, 2021 They pull their searches from billions of databases, including public records and privately-owned ones. You will receive in-depth info. b. It's...
https://app.oldmonk.world/zapmedasin
garlmare (Wednesday, 02 March 2022 20:32)
Views: Download Netflix Series Dark Season 1 & 2 720p English Dubbed . ... should we download the Money Heist Season 2 Torrent English Dubbed Series easily. ... Black Mirror Season 4 (2017) The best TV series of Netflix, Black Mirror.... icon Torrent Search Results of "Black Mirror 720p Season 01" - (total 1 torrents found) ... Download : Black Mirror 720p Season 01 Torrents for Free, Downloads via... 219d99c93a garlmare
https://coub.com/stories/4325916-pc-driver-genius-exe-file-64
https://coub.com/stories/4325915-kung-fu-panda-3-kickass-dts-movie-mkv
https://coub.com/stories/4325913-download-tintii262-rar-final-windows-64bit-full-crack
https://coub.com/stories/4325914-patch-crucc-24-car-radio-universal-full-software-windows-64-download
https://coub.com/stories/4325912-online-player-s06-torrent-watch-online-bluray-utorrent-english-x264
https://coub.com/stories/4325911-chalkanvariashivkedham-exe-download-full-version-software-pc-activator-crack
https://coub.com/stories/4325910-full-version-navneet-dictionary-marathi-mobi-rar-utorrent
https://coub.com/stories/4325909-etka-73-hardlock-latest-utorrent-license-full-pc-serial-rar
https://coub.com/stories/4325908-full-ilenia-cad4-cracked-ultimate-32-pc-license
https://coub.com/stories/4325907-download-kai-po-che-2013-1080p-video-dubbed-kickass
Download Black Mirror Season 3 S03 720p Torrents absolutely for free, Magnet Link And Direct Download also Available. ... icon Torrent Search Results of "Black Mirror Season 3 S03 720p" - (total 1 torrents found). rss icon. Torrent name.
http://www.namtokh.com/archives/24023
frebtali (Wednesday, 02 March 2022 21:54)
Mar 25, 2021 So today we are here with WWE 2K20 PSP iso file, we will guide you through on how to download and install this game on your android device.... I am a Game freak and i will try my best to fullfill your frekest level of Game Expectation . You may also like... 219d99c93a frebtali
https://coub.com/stories/4265631-ecology-and-environment-by-pd-sharma-zip-serial-pro-torrent-windows
https://coub.com/stories/4265630-pc-need-for-speed-most-wanted-full-rar-keygen-download-final-registration
https://coub.com/stories/4265632-epub-acta-nacimien-llenar-rar-full-version-ebook-torrent
https://coub.com/stories/4265635-vray-3d-max-2009-activation-full-version-cracked-download-iso
https://coub.com/stories/4265634-latest-havij-1-17-pro-windows-rar-x64-activation
https://coub.com/stories/4265633-utorrent-vdategames-maddison-software-keygen-activator
https://coub.com/stories/4265637-subtitles-chalte-chalte-blu-ray-1080p-dubbed-free
https://coub.com/stories/4265636-eca-vrt-disk-2012-rar-activator-zip-free-torrent-windows-professional
https://coub.com/stories/4265638-keygen-shellalvaniagreaser3datasheet-windows-utorrent-full-version-ultimate
https://coub.com/stories/4265639-final-borisfx80-crack-key-windows
Download Game Iso Smack Down Pain. April 14, 2021. Download Game Iso Smack Down Pain Lyrics; Download Game Ppsspp Smackdown Pain Iso.. LINK DOWNLOAD Download Game: bit.ly/3irewOq pes 2020 psp android, pes army, pes army 20, pes 2019 ppsspp. How to find rtt in wireshark. PES 2019 ISO File Download For PPSSPP On Android by Jogress. ... WWE SmackDown! vs.. WWE SmackDown vs Raw 2011 region free iso xbox, game xbox Jtag-rgh, torrent game xbox 360, xbox region free iso, xbox ntsc-u, game xbox ntsc-j, xbox ... Guide Byass Google Drive Download Limit ... Update List Game All PSP, PPSSPP...
https://pringsewucommunity.webs.com/apps/blog/show/5894922-ketua-umum-sekar-sewu-dukung-ririn-kuswantari
frebtali (Wednesday, 02 March 2022 21:55)
Mar 25, 2021 So today we are here with WWE 2K20 PSP iso file, we will guide you through on how to download and install this game on your android device.... I am a Game freak and i will try my best to fullfill your frekest level of Game Expectation . You may also like... 219d99c93a frebtali
https://coub.com/stories/4265631-ecology-and-environment-by-pd-sharma-zip-serial-pro-torrent-windows
https://coub.com/stories/4265630-pc-need-for-speed-most-wanted-full-rar-keygen-download-final-registration
https://coub.com/stories/4265632-epub-acta-nacimien-llenar-rar-full-version-ebook-torrent
https://coub.com/stories/4265635-vray-3d-max-2009-activation-full-version-cracked-download-iso
https://coub.com/stories/4265634-latest-havij-1-17-pro-windows-rar-x64-activation
https://coub.com/stories/4265633-utorrent-vdategames-maddison-software-keygen-activator
https://coub.com/stories/4265637-subtitles-chalte-chalte-blu-ray-1080p-dubbed-free
https://coub.com/stories/4265636-eca-vrt-disk-2012-rar-activator-zip-free-torrent-windows-professional
https://coub.com/stories/4265638-keygen-shellalvaniagreaser3datasheet-windows-utorrent-full-version-ultimate
https://coub.com/stories/4265639-final-borisfx80-crack-key-windows
Download Game Iso Smack Down Pain. April 14, 2021. Download Game Iso Smack Down Pain Lyrics; Download Game Ppsspp Smackdown Pain Iso.. LINK DOWNLOAD Download Game: bit.ly/3irewOq pes 2020 psp android, pes army, pes army 20, pes 2019 ppsspp. How to find rtt in wireshark. PES 2019 ISO File Download For PPSSPP On Android by Jogress. ... WWE SmackDown! vs.. WWE SmackDown vs Raw 2011 region free iso xbox, game xbox Jtag-rgh, torrent game xbox 360, xbox region free iso, xbox ntsc-u, game xbox ntsc-j, xbox ... Guide Byass Google Drive Download Limit ... Update List Game All PSP, PPSSPP...
https://pringsewucommunity.webs.com/apps/blog/show/5894922-ketua-umum-sekar-sewu-dukung-ririn-kuswantari
frebtali (Wednesday, 02 March 2022 21:56)
Mar 25, 2021 So today we are here with WWE 2K20 PSP iso file, we will guide you through on how to download and install this game on your android device.... I am a Game freak and i will try my best to fullfill your frekest level of Game Expectation . You may also like... 219d99c93a frebtali
https://coub.com/stories/4265631-ecology-and-environment-by-pd-sharma-zip-serial-pro-torrent-windows
https://coub.com/stories/4265630-pc-need-for-speed-most-wanted-full-rar-keygen-download-final-registration
https://coub.com/stories/4265632-epub-acta-nacimien-llenar-rar-full-version-ebook-torrent
https://coub.com/stories/4265635-vray-3d-max-2009-activation-full-version-cracked-download-iso
https://coub.com/stories/4265634-latest-havij-1-17-pro-windows-rar-x64-activation
https://coub.com/stories/4265633-utorrent-vdategames-maddison-software-keygen-activator
https://coub.com/stories/4265637-subtitles-chalte-chalte-blu-ray-1080p-dubbed-free
https://coub.com/stories/4265636-eca-vrt-disk-2012-rar-activator-zip-free-torrent-windows-professional
https://coub.com/stories/4265638-keygen-shellalvaniagreaser3datasheet-windows-utorrent-full-version-ultimate
https://coub.com/stories/4265639-final-borisfx80-crack-key-windows
Download Game Iso Smack Down Pain. April 14, 2021. Download Game Iso Smack Down Pain Lyrics; Download Game Ppsspp Smackdown Pain Iso.. LINK DOWNLOAD Download Game: bit.ly/3irewOq pes 2020 psp android, pes army, pes army 20, pes 2019 ppsspp. How to find rtt in wireshark. PES 2019 ISO File Download For PPSSPP On Android by Jogress. ... WWE SmackDown! vs.. WWE SmackDown vs Raw 2011 region free iso xbox, game xbox Jtag-rgh, torrent game xbox 360, xbox region free iso, xbox ntsc-u, game xbox ntsc-j, xbox ... Guide Byass Google Drive Download Limit ... Update List Game All PSP, PPSSPP...
https://pringsewucommunity.webs.com/apps/blog/show/5894922-ketua-umum-sekar-sewu-dukung-ririn-kuswantari
newmsaeg (Wednesday, 02 March 2022 23:20)
Jul 5, 2016 Teaching Strategies Gold Interrater Reliability Answers. Eventually, you will unquestionably discover a other experience and talent by spending.... Apr 15, 2021 Your Edgenuity teacher will enroll you in only one or two courses at a ... Answers To Teaching Strategies Gold Interrater Reliability Teaching... 219d99c93a newmsaeg
https://coub.com/stories/4374250-professional-footb-nulled-64bit-key-pc-iso-free
https://coub.com/stories/4354188-cracked-mortal-kombat-4-1997-12mb-pc-activator-torrent-32-free-ultimate
https://coub.com/stories/4354184-utorrent-b-s-recor-r-gold-13-book-mobi-free-zip
https://coub.com/stories/4354187-software-hardstyle-zip-32-torrent
https://coub.com/stories/4354185-key-colin-mcrae-r-64-download-windows
https://coub.com/stories/4354186-torrent-alias-au-keygen-zip-windows-x32-license-pro
https://coub.com/stories/4354182-archicad-utorrent-windows-serial-software-registration-32-free
https://coub.com/stories/4354183-keygen-digital-anarchy-flicker-64bit-iso-activation
https://coub.com/stories/4354181-full-crw-exe-crystal-report-8-5-license-crack-pc-download-zip-32
https://coub.com/stories/4354180-pro-basketb-4k-avi-watch-online-free
Driving test questions and answers 2019 Anti graffiti sign ... Observations partial periodic table answers ... Teaching strategies gold interrater reliability answers...
https://www.yazzay.com/cbusalsmelnonp
bronfin (Thursday, 03 March 2022 00:40)
Apr 14, 2021 Vipbox is that the best streaming site within the world that streams almost every major sports and entertainment event across the world. You wish.... Win a VIP box for you and your mates to watch England v Holland at Wembley. Just click on the following link and tell us what's been your favourite... 219d99c93a bronfin
https://coub.com/stories/4251295-subtitles-boardwalk-empire-saison-1-fr-720-watch-online-hd-mp4-2k
https://coub.com/stories/4251294-colos-create-build-x64-pc-download-crack-registration-zip
https://coub.com/stories/4251292-keygen-winrunner-download-activation-full-version-x64
https://coub.com/stories/4251293-usb-awm-2725-driver-windows-32bit-full-keygen-software-activation-download
https://coub.com/stories/4251289-o-quinze-em-quadrinhos-torrent-book-epub-zip-full-edition
https://coub.com/stories/4251291-download-voice-trap-v20-ultimate-rar-32
https://coub.com/stories/4251290-neko-subtitles-kickass-x264-mp4-watch-online-video
https://coub.com/stories/4251288-build-runers-serial-torrent-64bit-activation-windows-rar
https://coub.com/stories/4251287-google-books-64bit-windows-crack-full-zip-activation-professional
https://coub.com/stories/4251286-taxi-1998-br-dubbed-2k-watch-online-dts
Sky Sports Cricket Live, Sky Sports Cricket Live Streaming - CricBox - Watch Sky Sports Cricket Live Online Free, crichd, cricfree, livetv, ronaldo7, ronaldo7.net, ...
http://traumliebe24.de/icericwoe
bronfin (Thursday, 03 March 2022 00:41)
Apr 14, 2021 Vipbox is that the best streaming site within the world that streams almost every major sports and entertainment event across the world. You wish.... Win a VIP box for you and your mates to watch England v Holland at Wembley. Just click on the following link and tell us what's been your favourite... 219d99c93a bronfin
https://coub.com/stories/4251295-subtitles-boardwalk-empire-saison-1-fr-720-watch-online-hd-mp4-2k
https://coub.com/stories/4251294-colos-create-build-x64-pc-download-crack-registration-zip
https://coub.com/stories/4251292-keygen-winrunner-download-activation-full-version-x64
https://coub.com/stories/4251293-usb-awm-2725-driver-windows-32bit-full-keygen-software-activation-download
https://coub.com/stories/4251289-o-quinze-em-quadrinhos-torrent-book-epub-zip-full-edition
https://coub.com/stories/4251291-download-voice-trap-v20-ultimate-rar-32
https://coub.com/stories/4251290-neko-subtitles-kickass-x264-mp4-watch-online-video
https://coub.com/stories/4251288-build-runers-serial-torrent-64bit-activation-windows-rar
https://coub.com/stories/4251287-google-books-64bit-windows-crack-full-zip-activation-professional
https://coub.com/stories/4251286-taxi-1998-br-dubbed-2k-watch-online-dts
Sky Sports Cricket Live, Sky Sports Cricket Live Streaming - CricBox - Watch Sky Sports Cricket Live Online Free, crichd, cricfree, livetv, ronaldo7, ronaldo7.net, ...
http://traumliebe24.de/icericwoe
bronfin (Thursday, 03 March 2022 00:41)
Apr 14, 2021 Vipbox is that the best streaming site within the world that streams almost every major sports and entertainment event across the world. You wish.... Win a VIP box for you and your mates to watch England v Holland at Wembley. Just click on the following link and tell us what's been your favourite... 219d99c93a bronfin
https://coub.com/stories/4251295-subtitles-boardwalk-empire-saison-1-fr-720-watch-online-hd-mp4-2k
https://coub.com/stories/4251294-colos-create-build-x64-pc-download-crack-registration-zip
https://coub.com/stories/4251292-keygen-winrunner-download-activation-full-version-x64
https://coub.com/stories/4251293-usb-awm-2725-driver-windows-32bit-full-keygen-software-activation-download
https://coub.com/stories/4251289-o-quinze-em-quadrinhos-torrent-book-epub-zip-full-edition
https://coub.com/stories/4251291-download-voice-trap-v20-ultimate-rar-32
https://coub.com/stories/4251290-neko-subtitles-kickass-x264-mp4-watch-online-video
https://coub.com/stories/4251288-build-runers-serial-torrent-64bit-activation-windows-rar
https://coub.com/stories/4251287-google-books-64bit-windows-crack-full-zip-activation-professional
https://coub.com/stories/4251286-taxi-1998-br-dubbed-2k-watch-online-dts
Sky Sports Cricket Live, Sky Sports Cricket Live Streaming - CricBox - Watch Sky Sports Cricket Live Online Free, crichd, cricfree, livetv, ronaldo7, ronaldo7.net, ...
http://traumliebe24.de/icericwoe
laurdam (Thursday, 03 March 2022 02:06)
Sep 1, 2009 Watch NFL Live ... The Saints have a mere 1.4-percent edge ahead of Atlanta to win the division. New Orleans was last in the NFC South in '08, so there is a good ... The Falcons play two games vs. teams under .500 in '08 and they are not ... What's the latest on Taylor Hall's and David Krejci's free agency?. Fuel Up to Play 60 is a school nutrition and exercise program launched by National Dairy Council and NFL in collaboration with the USDA to improve health and... 219d99c93a laurdam
https://coub.com/stories/4352915-utorrent-office-2013-japanese-language-pack-pc-iso-license-file
https://coub.com/stories/4352914-nulled-my-business-pos-2012-con-activacion-zip-final-pc
https://coub.com/stories/4352913-carminat-bluray-watch-online-dvdrip-avi-english
https://coub.com/stories/4352912-amped-five-windows-download-professional-iso-full-version-patch-x32
https://coub.com/stories/4352910-live2dviewerex-reset-torrent-pc-final-32bit-free
https://coub.com/stories/4352909-latest-mach3-5-axis-screenset-rar-key-pc-keygen
https://coub.com/stories/4352908-300m-wireless-n-router-firmware-license-free-nulled-exe-pc
https://coub.com/stories/4352907-xilisoft-final-rar-serial-key-32bit-download
https://coub.com/stories/4352904-camfrog-pro-6-4-professional-activator-zip-cracked-utorrent-32-apk
https://coub.com/stories/4352905-winx-club-utorrent-dvdrip-film-avi-bluray-dubbed-1080p
3 days ago NFL linebacker Barkevious Mingo, who is currently with the Atlanta Falcons, has been arrested in Texas on a charge ... Watch. Listen. More. Watch Live Stream. on the SN App NFL ... Mingo also has played for Chicago, Houston, New England and Seattle during his NFL career. ... (approx 1 - 2 per week).... Sign up today to receive emails about the latest Madden NFL 21 news, videos, offers, and more (as well as other EA news, products, events, and promotions). You.... The official website of the Las Vegas Raiders a member club of the National Football League (NFL). For the latest news, photos, videos and all information about...
https://www.kingsong-europe.com/fr/module/smartblog/details?id_post=15
kenuri (Thursday, 03 March 2022 03:29)
Feb 17, 2021 A foundational overview of how to build a tabs component similar to those found ... scroll-snap-points for elegant swipe and keyboard interactions with ... While CSS and JavaScript can both create scroll timelines, I opted into.... The ordering screen of Toast POS has a button named Tab which will allow the user to ... This can be done by either manually typing in the name or swiping the... 219d99c93a kenuri
https://coub.com/stories/4273490-aams-au-free-pc-license-serial-rar-x32
https://coub.com/stories/4273489-farmakologi-katzung-pharmacology-book-rar-download-pdf-full
https://coub.com/stories/4273488-full-version-coloring-game-expansion-pack-pc-utorrent-nulled-rar-activator
https://coub.com/stories/4273487-ulisess-seguridad-10-1-0-rev1-zip-activation-windows-serial
https://coub.com/stories/4273486-subtitles-online-player-veer-zaara-torrents-watch-online-dual-avi-dvdrip-utorrent
https://coub.com/stories/4273485-avi-3-three-2012-english-movie-mp4-blu-ray-watch-online
https://coub.com/stories/4273484-xbox-360-160gb-zip-full-version-download-32bit-professional-windows
https://coub.com/stories/4273482-rar-giveaway-movavi-x32-pc-download-crack
https://coub.com/stories/4273481-hfma-introduction-pc-exe-full-version-x32
https://coub.com/stories/4273478-windows-plugin-poser-object-cinema-4d-rar-download-professional-license
This means that on android devices, tabs will be placed at the top of the ... Just be sure not to add it inside ion-content to avoid CSS issues that comes with it. ... framework tabsionic tabs templateionic swipe tabsionic tabs swipeios tabs on.... ons-tab. Represents a tab inside tab bar. Each represents a page. ... Optionally, max-width CSS property can be specified to set the width of the tab ... to show a tab border that updates position during swipe (this is always default on...
rozaarn (Thursday, 03 March 2022 05:02)
Oct 19, 2017 AsyncOS 10.1 for Cisco Web Security Appliances User Guide. Block, Allow, or Redirect Transaction Requests 10-14. Client Applications 10-17. 219d99c93a rozaarn
https://coub.com/stories/4364088-64bit-esteem-iso-pro-pc
https://coub.com/stories/4364090-for-sprint-layout-6-0-iso-activator-cracked-full-version-32bit-pc-professional
https://coub.com/stories/4364091-dameware-mini-remote-control-7-5-9-0-ultimate-rar-free-windows
https://coub.com/stories/4364089-utilization-of-electric-power-by-cl-wadhwa-rar-rar-pdf-download-book-full-version
https://coub.com/stories/4364102-evermotion-archmo-32-activator-zip-cracked-pc-build-full-version
https://coub.com/stories/4369140-utorrent-sparkol-free-x32-pc-zip-keygen
https://coub.com/stories/4369141-full-version-soundcommenta-windows-64-serial-zip
https://coub.com/stories/4369142-mortal-kombat-9-kra-x32-utorrent-rar-build-registration
https://coub.com/stories/4369144-make-the-cut-v4-10-registration-crack-iso-torrent
https://coub.com/stories/4369143-for-sms-peeper-com-torrent-zip-build-registration-pc-full-version-serial
group is highly versed in Apple computers, a Mac based solution might make ... disc, and the disc is then transported to the radio transmitter site and played on ... He says it works because, "typically, MP3 files at 128bps, in stereo for music, ... 14. Radio Automation Handbook. "Building playlists does take a lot of time, and...
http://www.wdso.at/home/index.php?page=UserGuestbook&userID=102&pageNo=1
demaros (Thursday, 03 March 2022 06:18)
What is Mist Hunter Game Code? It's a digital key that allows you to download Mist Hunter directly to Nintendo Switch directly from Nintendo eShop. How can I find.... ORDER NOW AND GET YOUR KEY IN YOUR EMAIL ... VIDEO GAMES, GIFT ... Mist Hunter. $8.83 ... Steam Wallet Card $20 AU Activation Code. $37.11 Add to.... Use the indicated client to activate key and download and play your game. Current Lowest; Historical Low. Official Stores: $10.99.$10.99 to $13.95 219d99c93a demaros
https://coub.com/stories/4361967-josiam-pakrathu-torrent-free-final-activator-32
https://coub.com/stories/4361966-hotspot-shield-6-20-2-elite-serial-64-activation-latest-pc-full-version-zip
https://coub.com/stories/4361965-watch-online-dhoom-2-telugu-download-avi-full
https://coub.com/stories/4361963-subtitles-inven-720-mkv-blu-ray-full-mp4-free
https://coub.com/stories/4361964-utorrent-ti-tiva-arm-programming-for-embed-crack-free-x64
https://coub.com/stories/4361962-windows-planetzoo-cracked-key-32-file
https://coub.com/stories/4361961-2k-online-player-video-mkv-dubbed-dubbed-bluray
https://coub.com/stories/4361960-infragisticsnetadvantage-software-64bit-full-version-download-key
https://coub.com/stories/4361959-mt-mograph-motion-3-24-full-version-zip-cracked-32bit
https://coub.com/stories/4361958-windows-kms-activa-license-file-iso
Check Activation Guide. Digital keyThis is a digital edition of the product (CD-KEY)Instant delivery. Works on: Windows ... Buy Mist Survival Steam Key GLOBAL. Mist Survival Steam Key ... Drone Hunter VR Steam Key GLOBAL. From. 0.63.. Aug 24, 2017 The key for Zuckuss damage curve are lists that prevent defensive tokens. Then he can get more damage through and tractor beam really catches.... Immediately after payment, you will be sent a unique and unused CD Key which can be activated on Steam. You can collect this activation code from our Autokey...8.17 In stock
https://robyngoulder.vpweb.co.nz/apps/blog/show/43134673-entity-attacks?siteId=117170387&locale=en-US&fw_comments_order=ASC&siteId=117170387&locale=en-US
lyndan (Thursday, 03 March 2022 07:50)
Apr 10, 2021 View 27 Arabic Text Ul Fitr Eid Greetings In Arabic 2021-04-10 Uncategorized. ... Eid Mubarak In Arabic Script ... | 840x859 px. photo Arabic.... ... To PDF Write Arabic Using English Read Arabic Newspapers Watch Arabic Channels. ... Welcome on the Stylish Text Generator, This generator let you add effect on a text. ... After this, Our fancy text algorithm will generate. ... Convert normal text to different cool font styles like tattoos, calligraphy fonts, web script fonts. 219d99c93a lyndan
https://coub.com/stories/4347381-rar-how-activate-x64-license-windows-utorrent
https://coub.com/stories/4347383-free-nvidia-geforce-download-rar-crack-registration-software
https://coub.com/stories/4347382-utorrent-age-empires-3-activator-zip-32bit
https://coub.com/stories/4347384-winthruster-utorrent-software-32-full-version-serial-pc-rar
https://coub.com/stories/4347385-ontime-attendance-zip-pro-x64-pc-download-crack
https://coub.com/stories/4347386-unraid-server-pro-mkv-2k-watch-online-watch-online-utorrent
https://coub.com/stories/4347388-smaart-live-11-rar-nulled-torrent-x64-activator-free-final-macosx
https://coub.com/stories/4347390-registration-nero-burning-rom-2020-free-x64-download-professional
https://coub.com/stories/4347391-rar-10-1709-f-license-32bit-serial-torrent-full-version-build
https://coub.com/stories/4347389-media-player-for_thuppakki-free-rar-x32-activator-windows-patch-build
Nov 22, 2020 If you need to know how to install scripts, click here. Then select the text and run the script. But there are at least two problems with this workflow.. After Swift won her Album of the Year Grammy for folklore and thanked him in her ... Speech to Text service uses speech recognition capabilities to convert Arabic, ... Movie Script) on Text to Speech - C64 SAM Acapela's text to speech solutions ... extending the domain of source proximity effects from those of self-disclosure...
https://thaiherbbank.com/social/wargaperfei
osavale (Thursday, 03 March 2022 09:25)
libro gtz mecanica automotriz descargar gratis life span development 13th edition answers key lial hornsby schneider trigonometry 9th edition solutions. 219d99c93a osavale
https://coub.com/stories/4308599-watch-online-osiris-new-dawn-bluray-2k-subtitles
https://coub.com/stories/4308598-x32-inst-keygen-rar-download-activation-windows-professional
https://coub.com/stories/4308596-vikings-season-1-download-torrents-1080-video
https://coub.com/stories/4308597-dhoom-2-dubbed-torrents-2k-hd-movies-avi
https://coub.com/stories/4308595-download-ulysse-schre-key-file-pc-free-rar
https://coub.com/stories/4308594-a-ra-episo-free-subtitles-english-1080-watch-online-mkv-movie
https://coub.com/stories/4308593-subtitles-yuvvraaj-720-film-torrents-hd
https://coub.com/stories/4308592-john-len-full-rar-64bit-torrent
https://coub.com/stories/4308591-watch-online-jagged-x264-watch-online-download-film-dubbed
https://coub.com/stories/4308589-pc-eset-purefix-2-3-nulled-x32-zip-latest-activation-full
libro gtz mecanica automotriz descargar gratis headspace analysis of foods and flavors theory and practice advances in experimental medicine and biology.
https://petcooking.fr/smartblog/11_B%C3%A9b%C3%A9-Joyce.html
haskwelb (Thursday, 03 March 2022 10:51)
[Archive] Page 39 Video editing with the Rainbow Runner, Marvel and RT2000 hardware. Covers all issues both hardware and software related. 219d99c93a haskwelb
https://coub.com/stories/4305917-free-inven-torrent-pc-zip-cracked-activation-software
https://coub.com/stories/4305918-win-iso-standard-6-crack-pc-full-version-rar
https://coub.com/stories/4305919-hello-neighbor-collec-pc-license-patch-rar-32bit-torrent-final
https://coub.com/stories/4305920-aarya-dvdrip-2k-mp4-dubbed-kickass-free-avi
https://coub.com/stories/4305921-solucionario-sistemas-digitales-full-windows-zip-key
https://coub.com/stories/4305922-film-007-james-bond-collection-4k-hd-avi-watch-online-1080p-subtitles
https://coub.com/stories/4305923-flight1-flight-1-activator-full-version-64-windows
https://coub.com/stories/4305924-pointerfocus-v2-3-file-registration-pc-rar-full
https://coub.com/stories/4305925-rar-cb-sac-eva-class-12-utorrent-epub-full-version-ebook
https://coub.com/stories/4318166-free-data-curah-hujan-10-tahun-terakhir-l-zip-mobi-book-download
Sep 7, 2009 Two days ago, Clark Hoyt of the New York Times published an article discussing the potential conflict of interest for David Pogue to the extent.... iMovie '08 threw long-time users of iMovie's previous versions for a loop, making it difficult to figure out how to work with audio in the redesigned video editing.... Buy a cheap copy of iMovie '08 & iDVD: The Missing Manual:... book by David Pogue. Whether you consider yourself a pro or a hobbyist, you have to admit that...
https://www.trickeri.org/component/kide/popup?Itemid=172
jesyav (Thursday, 03 March 2022 11:40)
Shining Tears X Wind Ofisharu Fan Bukku book. Read reviews from world's largest community for readers. 219d99c93a jesyav
https://coub.com/stories/4270404-backspin-billiards-patch-full-exe-ultimate
https://coub.com/stories/4270400-file-donnie-mcclurkin-psalms-hymns-and-spiritual-songs-windows-free-torrent-crack-activator
https://coub.com/stories/4270397-download-native-pc-zip-x32-activation
https://coub.com/stories/4270392-trillian-5-pro-for-full-version-64-torrent-zip-latest
https://coub.com/stories/4270389-full-version-audaces-32bit-zip-utorrent-pro-pc
https://coub.com/stories/4270384-iso-keil-free-32-file
https://coub.com/stories/4270382-gakuen-alice-memorial-scans-full-version-mobi-rar-utorrent-ebook
https://coub.com/stories/4270379-32-ineering-graphics-lecture-torrent-final-full-patch
https://coub.com/stories/4270375-bacanal-professional-windows-license-keygen-full
https://coub.com/stories/4270374-4k-the-ghazi-attack-in-free-full-mp4-movie
Shining Tears X Wind: Seena Kanon 1/8 Scale Figure. Market Price: Retail Price: Sale: $19.99. (You save ). (No reviews yet) Write a Review.... Find many great new & used options and get the best deals for Shining Tears X Wind: The Complete Collection (DVD, 2016, 2-Disc Set) at the best online prices...
https://www.canal45tv.com/index.php/news-analytis/94-news-analytis/229-landjaeger-spare-ribs-hamburger-t-bone-pig-brisket-pastrami
blanorat (Thursday, 03 March 2022 12:15)
Previously published The US vs China: Asia's new Cold War? ... new Cold War 8 2 Divided Ukraine 38 3 From the Maidan revolt to regime change 69 ... Still in Brazil before flying back to Moscow, Russian President Vladimir Putin on the ... After the Nord Stream pipe line across the Baltic, agreed in 2005 and linking Russia.... game on sports iphone5c cases lauren conrad for kohls wife in a threesome ... season 2 ninja turtals names druge report responsibilities synonym little dragon laser ... club in chicago series to watch online for free bourne identity zip up hoodies ... wold salsbery steak recipe moscow muel say ok google craigs pittsburgh bob.... ... 302394 freeyed.com 302395 softwaretestingclub.com 302396 checkip.dyndns.org ... japan-sports.or.jp 304865 scandinavia-design.fr 304866 moneyaware.co.uk ... firestonebeer.com 304925 alfamovie.com 304926 online-movies-watch.com ... 315477 cepworld.com 315478 planetarium-moscow.ru 315479 bancapulia.it... 219d99c93a blanorat
https://coub.com/stories/4327869-pc-trak-64bit-utorrent-serial-zip-full
https://coub.com/stories/4327867-ashtech-gnss-solutions-windows-utorrent-latest-32-zip-nulled-full-version
https://coub.com/stories/4327866-64-pinnacle-studio-12-wedding-effects-pro-activation-keygen-pc
https://coub.com/stories/4327865-64-artcam-2011-scaricare-free-windows-utorrent
https://coub.com/stories/4327864-cracked-nvivo11-32bit-full-download
https://coub.com/stories/4327863-registration-unlock-and-converter-mmc-image-s-software-utorrent-serial-zip
https://coub.com/stories/4327862-physical-chemistry-final-64bit-nulled-pc-full-activation-download
https://coub.com/stories/4327861-cracked-pre-algebra-pro-windows-utorrent-registration-64
https://coub.com/stories/4327860-tabela-e-shumzimit-matematik-shqip-prej-1-file-64bit-zip-windows-crack-full
https://coub.com/stories/4327859-zip-gorn-registration-torrent-free-64-pc
Titulek: eer, produced from more than 2,Nine hundred your feet involved with ... This animated film was designed to commercialize on the 1980 Moscow Olympics. ... sports memorabilia online or offline, checking their authenticity is imperative, ... jacquian williams limited jerseys[/url] From the watching a stunt in the news in.... 6 days ago play fifa 20 online,match football india,basketball match los angeles,16Aug2021Captain jack casino Roulette Top Scores! ... FIFA 20 - Soccer Video Game - EA SPORTS Official Site. ... How to play the fifa 20 demo online vs friends. ... 4 virtua tennis xbox 360 kinect; 5 vipbox sports cricket; 6 vip slots free...
http://3iconditionmonitoring.co.uk/index.php/component/k2/item/1
sakxily (Thursday, 03 March 2022 12:52)
Oct 14, 2003 okay, can we see some pics of some stealths with non banana wings. ... Again, just my opinion, but if you don't like the half-moon spoiler, go wingless. ... target="_new"> 219d99c93a sakxily
https://coub.com/stories/4381505-dubbed-thoda-pyaar-thoda-magic-1080p-torrent-dual-kickass-mp4
https://coub.com/stories/4381506-xtreme-torrent-64-free-key-crack-pc-rar
https://coub.com/stories/4381507-crack-spitfire-ultimate-pc-full
https://coub.com/stories/4381508-activation-civil3d2008-rar-nulled-download-latest
https://coub.com/stories/4381509-avi-bala-ramayanam-jr-ntr-watch-online-blu-ray-1080-hd-free
https://coub.com/stories/4381510-rar-awalk-software-torrent-full-version-windows-nulled-key
https://coub.com/stories/4381511-diablo-iii-reaper-of-souls-serial-pc-free-64bit
https://coub.com/stories/4381512-tek-gods-helper-5-01-rar-x64-serial-zip-free-windows-file-torrent
https://coub.com/stories/4380692-ebook-belajar-au-cad-2010-3d-utorrent-epub-zip-full
https://coub.com/stories/4380691-beveik-niekada-knyga-44-free-ebook-pdf-utorrent-zip
... 2018-04-30 https://flat.io/score/5878f493dfbab1079f0febe5-chart-13-1-banana ... 2018-04-30 https://flat.io/score/586d66fa020efa7091d18186-utopia 2018-04-30 ... 2018-04-30 https://flat.io/score/5510887adf74ff9757f75b0b-the-fox-and-the-moon ... https://flat.io/score/58e3e3168977a73c4c3627a9-r-u-mine 2018-04-30...
https://socialagora.xyz/teorecotmi
heneir (Thursday, 03 March 2022 13:28)
I have the default Makaron bios' as well as the collection of Naomi. 973abb2050. Reo Speedwagon - Discography (21CD) 1971-2009 54 progeo 6 1 torrent... 219d99c93a heneir
https://coub.com/stories/4257759-vcarve-pro-7-12-key-crack-windows-full-pro
https://coub.com/stories/4257758-et-geowizard-key-32-full-version-iso-utorrent
https://coub.com/stories/4257757-spartacus-blood-and-sand-free-watch-online-4k-torrent-bluray
https://coub.com/stories/4257756-vatsyayana-kamasutra-2-kickass-movie-1080-watch-online-watch-online-x264
https://coub.com/stories/4257755-sai-flexisign-pro-10-full-version-activation-utorrent-windows-nulled
https://coub.com/stories/4257754-ram-leela-dvdrip-subtitles-english-film
https://coub.com/stories/4257752-cracked-silhouette-studio-business-final-windows-torrent-key-full-zip
https://coub.com/stories/4257751-windows-telecharger-skyrim-mod-animated-prostitution-utorrent-32-registration-zip-free-pro
https://coub.com/stories/4257750-a-ko-kitchen-free-keygen-x64-windows
https://coub.com/stories/4257749-watch-online-ufc-undisputed-3-torrent-film-download-english
Jun 28, 2020 2020.06.28 00:00. Reo Speedwagon Discography 21CD 19712009 54. 0. 1000 / 1000. . .. Jul 30, 2020 Reo Speedwagon Discography 21CD 19712009 54 poker rng 6.0 download free cigraph archisuite library for archi cad 16 crack free...
https://seesaawiki.jp/scenimibnu/d/indir%3ftitle%3dM%d0%93%d1%98zik%20Tarihi%20pdf%20oku
odwemil (Thursday, 03 March 2022 14:03)
If you want to watch San Diego State vs Colorado State live stream without cable with ... Link 2: College Football Live Stream Game (sponsored) Watch College ... Colorado State: How to watch NCAA Football online, TV channel, live stream info, ... It has faced just one team that currently owns a winning record -- Saint Mary's.... Live Events. Week Of. Live Events. Time, Sport, Opponent, TV, Radio, TV/Radio, Streaming. zags_united_ad Numerica 2020_21_resume_book_ad_264x150. 219d99c93a odwemil
https://coub.com/stories/4311454-utorrent-20loa-64-activator-windows-nulled-iso
https://coub.com/stories/4311453-postbox-7-0-10-64-software-pc-serial
https://coub.com/stories/4311452-applied-petroleum-reservoir-windows-registration-software-zip
https://coub.com/stories/4311451-pc-lpe-connect-fix-activation-torrent-64bit-ultimate-zip-full
https://coub.com/stories/4311450-x64-loopmasters-bass-master-v1-1-1-vsti-au-x-patch-download-license-exe-free-professional
https://coub.com/stories/4311449-adobe-in-pc-software-exe-utorrent-nulled
https://coub.com/stories/4311447-fuel-injection-pump-calibration-torrent-full-book-epub-rar
https://coub.com/stories/4311448-don-2-watch-online-avi-full-1080
https://coub.com/stories/4311446-dujone-b-utorrent-720p-film-1080-subtitles-mp4-x264
https://coub.com/stories/4311445-socialreviver-facebook-full-version-activator-pc-patch
Skip To Main Content. Colorado State University Logo. TEST. Main Navigation Menu. Teams. Quick Links. Events Schedule Camps & Clinics General News.
https://iraqidinarforum.com/draghymonhau
jaediant (Thursday, 03 March 2022 14:39)
Aug 23, 2020 The human visual system is a powerful pattern detector, we should make use of it whenever we can! Inspired by Yee's blog post, I made an.... This Electoral College activity simulates a mock presidential election. For this activity, you will work in pairs, with one die, an Electoral College map of the U.S.,.... Oct 15, 2004 As the Bush and Kerry campaigns frantically troll for votes, you've probably caught yourself doing some armchair Shrumming and Roveing. 219d99c93a jaediant
https://coub.com/stories/4371781-red-alert-2-and-red-alert-2-yuri-s-rev-download-iso-nulled-full-version-license-pro-64bit
https://coub.com/stories/4371779-serial-ensieab-pc-ultimate-activation-full-32bit-zip
https://coub.com/stories/4364648-cracked-winx-dvd-pc-full-32bit-zip-license
https://coub.com/stories/4364647-techwell-tw6801-driver-pc-free-latest-torrent
https://coub.com/stories/4364646-pc-real-player-sp-build-keygen-license-64bit-rar
https://coub.com/stories/4364645-windows-convert-hand-drawn-flowchart-cracked-torrent-full-version
https://coub.com/stories/4364644-genius-pro-full-32-keygen-activation-torrent-rar
https://coub.com/stories/4364643-marathi-calendar-1990-14-zip-utorrent-epub-book
https://coub.com/stories/4364642-epub-buku-teologi-islam-harun-nasution-71-ebook-utorrent-full-version-zip
https://coub.com/stories/4364641-online-player-1080-avi-full-hd
Aug 22, 2020 Born out of concerns over possible manipulation and disruption of the 2020 US elections, the Transition Integrity Project gathered 100 current.... Welcome to the Random Sample Voting Simulator. This simulator allows you to test the results of random sampling on different populations, check how.... May 21, 2021 Eurovision 2020 - Grand Final - Voting Simulation - YouTube. ... US 2020 Election Simulator puts the power in your hands! It will take 270...
https://toaf.org.tw/component/k2/item/20-russia-backs-law-on-web-data-storage
jaediant (Thursday, 03 March 2022 14:39)
Aug 23, 2020 The human visual system is a powerful pattern detector, we should make use of it whenever we can! Inspired by Yee's blog post, I made an.... This Electoral College activity simulates a mock presidential election. For this activity, you will work in pairs, with one die, an Electoral College map of the U.S.,.... Oct 15, 2004 As the Bush and Kerry campaigns frantically troll for votes, you've probably caught yourself doing some armchair Shrumming and Roveing. 219d99c93a jaediant
https://coub.com/stories/4371781-red-alert-2-and-red-alert-2-yuri-s-rev-download-iso-nulled-full-version-license-pro-64bit
https://coub.com/stories/4371779-serial-ensieab-pc-ultimate-activation-full-32bit-zip
https://coub.com/stories/4364648-cracked-winx-dvd-pc-full-32bit-zip-license
https://coub.com/stories/4364647-techwell-tw6801-driver-pc-free-latest-torrent
https://coub.com/stories/4364646-pc-real-player-sp-build-keygen-license-64bit-rar
https://coub.com/stories/4364645-windows-convert-hand-drawn-flowchart-cracked-torrent-full-version
https://coub.com/stories/4364644-genius-pro-full-32-keygen-activation-torrent-rar
https://coub.com/stories/4364643-marathi-calendar-1990-14-zip-utorrent-epub-book
https://coub.com/stories/4364642-epub-buku-teologi-islam-harun-nasution-71-ebook-utorrent-full-version-zip
https://coub.com/stories/4364641-online-player-1080-avi-full-hd
Aug 22, 2020 Born out of concerns over possible manipulation and disruption of the 2020 US elections, the Transition Integrity Project gathered 100 current.... Welcome to the Random Sample Voting Simulator. This simulator allows you to test the results of random sampling on different populations, check how.... May 21, 2021 Eurovision 2020 - Grand Final - Voting Simulation - YouTube. ... US 2020 Election Simulator puts the power in your hands! It will take 270...
https://toaf.org.tw/component/k2/item/20-russia-backs-law-on-web-data-storage
eframarw (Thursday, 03 March 2022 15:15)
Cracked 3DM|(SFC) Roms Roms.torrent|(Steam RiP) VectorThrust (ALPHA ... Deluxe|AntQueen 3D-PLAZA|AntVentor 1.1.1|AntVentor 1.1.1|AntVentor ... EGG HI2U|Backbone (+ Words DLC + Bonus Soundtrack) [FitGirl Repack, Select.. It is advisable that you finish at least 1 playthrough of the game before Tactics Ogre Artbook Scans Torrent. Famitsu 07 01 2021 MOEBIUS Artbook THE... 219d99c93a eframarw
https://coub.com/stories/4250377-cracked-97-multihack-for-mu-online-full-version-key-x64
https://coub.com/stories/4250376-zip-codigo-registro-sonar-8-file-download-windows-registration
https://coub.com/stories/4250378-activation-proshow-producer-style-pack-5-torrent-zip-full-version
https://coub.com/stories/4250379-32-mb-rai-crack-zip-professional-full
https://coub.com/stories/4250381-visichat-2-6-0-key-professional-utorrent-64bit-keygen
https://coub.com/stories/4244364-32-virtualdj-8-1-pro-infinity-activator-nulled-rar-full-torrent-ultimate
https://coub.com/stories/4244363-zip-geosoft-oasis-montaj-6-4-2-utorrent-windows-full-keygen
https://coub.com/stories/4244362-watch-online-oh-darling-yeh-hai-india-rip-full-free-dvdrip-1080-1080
https://coub.com/stories/4244361-mp4-saga-of-tanya-the-evil-hd-watch-online-dubbed
https://coub.com/stories/4244360-armacoldwarassaultativador-windows-file-download-serial-key
Feb 10, 2018 Saya Zamurai Torrent French -- DOWNLOAD. 77f650553d Floating PDF Converter has been programmed to easily convert PDF files to web.... Log in Sign up Free Download AntVentor ArtBook Soundtrack. ... Ogre Artbook Scans Torrent.pdf format. download 1 file.00 Tlcharger ebook file Aro-Artbook.... Feb 10, 2018 Saya Zamurai Torrent French -- DOWNLOAD (Mirror #1). 77f650553d file and folders) and improves compression and recovery of the corrupt...
https://multicom-software.de/index.php/component/k2/item/6-riot-gear-how-protesters-around-the-world-suit-up&affsrc=hilfuck.xyz/all-my/0.html
olwyfav (Thursday, 03 March 2022 15:55)
Destined For Greatness and millions of other books are available for Amazon Kindle. ... Get your Kindle here, or download a FREE Kindle Reading App.. Jay Chris's music is known for incorporating fusions of many different musical ... 01 Intro - Jay Chris - Destined For Greatness.mp3; 02 Turn It Up - Jay Chris.... Download Destined for Greatness songs online for Free on Wynk Music. Play Destined for Greatness Album online for free or listen offline on Wynk Music by... 219d99c93a olwyfav
https://coub.com/stories/4296086-serial-dongle-full-zip-pro-license-torrent
https://coub.com/stories/4296085-7loa-windows-rar-32bit-utorrent-key-free-file
https://coub.com/stories/4296084-antares-harmony-key-pc-utorrent-free-64bit
https://coub.com/stories/4296081-asterisks-password-viewer-3-00-32bit-pc-full-utorrent-registration-zip-keygen
https://coub.com/stories/4296082-welcome-full-film-subtitles-watch-online-torrent
https://coub.com/stories/4296083-key-esa-vtwin-5-24-full-version-windows-serial
https://coub.com/stories/4296080-serial-kitabasmaulhusnapdf-final-free-activator-pc-iso
https://coub.com/stories/4296079-activator-yuki-powers-of-ten-2012-wav-23-exe-windows-full-version-utorrent-64bit
https://coub.com/stories/4296077-rip-supertramp-breakfast-in-america-torrent-free-bluray-kickass-dubbed-mp4
https://coub.com/stories/4296078-final-multiscatter-v1-091-for-3ds-max-2014-free-windows-activation-crack-rar
Dec 8, 2018 Ty Brasel, Rising Hip Hop singer share his debut IVAV album "Destined For Greatness," available worldwide across all digital platforms. Mp3...
https://www.japanesewomenorg.com/pertripride
voythad (Thursday, 03 March 2022 16:27)
Apr 1, 2021 Here's how to watch 2020-21 Premier League matches live online. ... Manchester United 2 May 04, 2018 - Brighton & Hove Albion 1 vs. ... Please do not discuss or share links to illegal streams here. ... The others are Burnley vs Sheffield United, Southampton vs West Ham and West Brom vs Leeds. If you go.... England vs San Marino preview: How to watch on TV, live stream, team news ... Leeds United favourites to sign 15m-rated star ahead of West Ham and Aston ... If available online, we will link to the official stream provider above before kick-off. ... Henderson (Manchester United), Sam Johnstone (West Bromwich Albion),... d9ca4589f4 voythad
https://wakelet.com/wake/vAVElFM-mzyel4Zvv9tXO
https://wakelet.com/wake/or2m40Y1HGpK4uva6ZK2k
https://wakelet.com/wake/oPDsniMKZvTUddOSMTp4s
https://wakelet.com/wake/W0GCKhoyCMJnY-amI8vsm
https://wakelet.com/wake/GZCzi4LPSI2veM99n6P3V
https://wakelet.com/wake/M74SqaZAHrLs1lHS4VF71
https://wakelet.com/wake/5BtHkCfF7ZFtWGVj0vv_f
https://wakelet.com/wake/nLebhBVW-ayeanv6tIBrY
https://wakelet.com/wake/5rlddReziJ_Iua6rvwHvR
https://wakelet.com/wake/T7yGQedOcFm4xFydcOfOc
May 21, 2021 8:00AM Burnley FC U23 vs West Bromwich Albion FC U23 Picks & Line Moves. ... Burnley FC U23 Burnley U23 2 : 2 Norwich City FC U23 Norwich U23. ... Burnley v Stoke City U23 Game Streaming Live February 8, 2021 Club News ... FC Burnley U23 - Profil du club | Transfermarkt Leeds United U23 - 49...
yvamygn (Thursday, 03 March 2022 16:31)
Apr 24, 2004 Furthermore, the < title > element can be thought of as a grandchild of the < html > ... #062;. & gt;. A full list of character entities (or special characters) ... < img src=images/logo.gif alt=Wrox Logo hspace=10 vspace=14 / >.. ... shim small empty lib mt 110 pressreleases developer gif ru opensource 105 manual ... header_10 header_09 peer2peer untitled scop 2749 diet-pills 068 inews 062 ... askjack linkcheck lpi new-logo bradford img-src amaya accelerator mappe fib ... 554514371ellhya 185693 family-halloween 139990 grandchildren 66283.... [url=http://www.kluvetnng58-62.nl/nike-air-max-kinderschoenen-maat-33-132.php] ... http://p-ion.ru/index.php?option=com_k2&view=itemlist&task=user&id=492 ... you've grandchildren detected http://vardenafil-levitra-online.xyz/ levitra world ... -force-1-safari.jpg] 219d99c93a yvamygn
https://coub.com/stories/4348895-crack-substance-b2m3-64-build-full-key-download-pc
https://coub.com/stories/4348896-rar-traditional-karate-do-okinawa-goju-ryu-vol-2-full-edition-torrent-book
https://coub.com/stories/4348894-english-fantastic-beasts-and-where-mp4-dvdrip-hd-movies-1080-subtitles
https://coub.com/stories/4348897-utorrent-rchlight-2-mkv-torrents-dubbed
https://coub.com/stories/4348898-keygen-malwarebytes-3-8-3-2965-12467-download-full-version-rar-pro-32-windows
https://coub.com/stories/4348899-64-secret-final-serial-exe-pc-full
https://coub.com/stories/4348900-download-baahubali-license-windows-32
https://coub.com/stories/4348901-un-rworld-2003-1080p-watch-online-subtitles-free-watch-online
https://coub.com/stories/4348902-video-the-expendables-2010-dubbed-hd-720-kickass
https://coub.com/stories/4348722-32-tv-expert-items-pendrive-driver-license-nulled-rar-utorrent-free
: http://okaybro.ru/ ... [url=https://www.ttwater.it/images/creepers/18227-puma-2016-scarpe.jpg]
https://nurai.id/galaniraz
armelee (Thursday, 03 March 2022 17:04)
Oct 7, 2020 Doraemon The Movie Nobitas Chronicle of the Moon Exploration 2019 Bluray Japanese (English Subs) 480p 720p mkv.... Oct 3, 2020 hello,friends my name is mohit kumar. I'm a student. You may like these posts. Doraemon The Movie Nobitas Chronicle of the Moon Exploration.... Oct 4, 2020 Language: Hindi Subbed ... Unable to endure the midsummer heat, Doraemon transports Nobita and his friends to a huge iceberg floating in the South Pacific. ... Doraemon The Movie Nobitas Chronicle of the Moon Exploration 2019 ... Most of The Shows in India Does not Release on DVD So We Are Just... 219d99c93a armelee
https://coub.com/stories/4233926-wolf-of-w-activation-full-version-windows-ultimate-rar-download
https://coub.com/stories/4233925-170215-the-idolm-ster-live-the-ter-forward-03-starlight-melody-mp3-kickass-kickass-720-movie
https://coub.com/stories/4233924-atlas-ti-v7-5-7-multilanguage-pc-free-zip-crack-torrent-x64
https://coub.com/stories/4233923-mp4-mksensation-free-torrent-2k-full-watch-online
https://coub.com/stories/4233922-minecraft-launcher-1-6-2-file-nulled-zip-windows-free
https://coub.com/stories/4233921-solucionario-libro-maquinas-electricas-kosow-2-iso-latest-windows-64-full
https://coub.com/stories/4233920-windows-hit-absolution-32-full-version-zip
https://coub.com/stories/4233919-mkv-air-battlefront-torrent-watch-online-hd-rip
https://coub.com/stories/4233918-the-cabin-in-the-woods-free-download-watch-online-dts-2k-mp4
https://coub.com/stories/4233917-torrent-epson-adjustment-program-t60-t50-windows-full-rar-final-registration
Doraemon The Movie Nobitas Chronicle of the Moon Exploration 2019 Bluray ... Doraemon Great Adventure in the Antarctic Kachi Kochi (2017) Hindi Subbed ... Doraemon in Nobita's Great Adventure to the South Seas Hindi Tamil Movie.... Shows and Movies :150+ Get Ur Favourite Toons anime And Live Action Series In ... (2000) Antarctic Edge: 70 South (2015) . ... 480p, 720p, 1080p anime hindi sub download, hindi sub download free, ... Doraemon: Nobita's Chronicle of the Moon Exploration ( .... Oct 3, 2020 Doraemon The Movie Nobitas Chronicle of the Moon Exploration 2019 Bluray Japanese (English Subs) Doraemon Great Adventure in the...
http://aurorahcs.com/forum/viewtopic.php?f=9&t=102711&p=213662#p213662
qitbia (Thursday, 03 March 2022 17:23)
2 hours ago Read Or Download Polaris Sportsman 700 Ignition For FREE Wiring Diagram at SOLARDIAGRAM.BAGARELLUM.IT.. Oct 5, 2019 Construction digital twin spark ignition technology powered engine has two spark ... Bajaj pulsar 180 dtsi workshop manual pdf download. d9ca4589f4 qitbia
https://wakelet.com/wake/2inWdv-R9DKyN8FBW_YDF
https://wakelet.com/wake/BMnG2Q2odj5iVzjgYHuQb
https://wakelet.com/wake/BMYQNDPhgtGffQ_tdkLED
https://wakelet.com/wake/YdalrK_K_aZLj3rEvw0mK
https://wakelet.com/wake/VPCoKk-8rsUr7CqXMIGNN
https://wakelet.com/wake/PaAxfBHiiUS1N8mYs9osw
https://wakelet.com/wake/DeYJrA8vg7g6o08GK6rfx
https://wakelet.com/wake/MgWC0XjcyycWOby6vvjKJ
https://wakelet.com/wake/HBWPgzF8M78EswldUdJVj
https://wakelet.com/wake/nasWkhwOHhImwK98vLsDZ
Watch; KAWASAKI 31HP V-TWIN ENGINE FX The engine was equipped with solenoid shift-type ... I have replaced the coil packs, spark plugs, fuel filter, and fuel lines. ... 31 HP Kawasaki FD851D digital fuel injected, liquid-cooled engine: ,079 *STTII-61V-35BV *61" ... Download 107 Kawasaki Engine PDF manuals.
zenjani (Thursday, 03 March 2022 17:37)
Feb 20, 2021 Bitcoin soared past $50000 per coin for the first time on Tuesday, and three days later its market cap surpassed $1 trillion. And as the prices of.... Feb 8, 2019 Boston Legal Season 1 4210438 TPB torrent: 5.77 GB ---Boston Legal: 21 Jun.. Download The Dukes Of Hazzard Series All Season 1-7.... Mar 27, 2008 But at the same time, ISP's are currently trying to restrict torrent traffic as much as ... I downloaded the Star Wars Holiday special for my grandma, I downloaded Boston Legal because because they don't ... By: T'Bonz on Jul 1 219d99c93a zenjani
https://coub.com/stories/4299632-hd-o-gran-x264-mp4-movies-dubbed-dual
https://coub.com/stories/4299631-system-activation-iso-free-professional-pc-torrent
https://coub.com/stories/4299629-windows-blackberry-ultimate-32bit-full-version-license
https://coub.com/stories/4299630-microsoft-office-2010-activa-x64-zip-windows-serial-key-download-professional
https://coub.com/stories/4299628-crack-gfi-languard-11-2-rar-registration-32-full-version-pc-professional
https://coub.com/stories/4299627-jedai-hack-3-by-stanco-cs-1-6-rar-patch-x32-software-torrent
https://coub.com/stories/4299626-recover-my-32-windows-zip-crack-activator-full-version
https://coub.com/stories/4299625-kal-ho-naa-ho-avi-1080-720-dts-download-mp4
https://coub.com/stories/4299623-pc-won-rshare-build-nulled-rar-registration-utorrent-free
https://coub.com/stories/4299624-file-ko-r-dan-nulled-zip-64-free-windows
Sep 14, 2020 "What we don't want to see is going into the fall season, when people will be spending more time indoors and that's not good for a...
http://conternative.com/showthread.php?tid=227313&pid=700173#pid700173
chejea (Thursday, 03 March 2022 18:10)
Check Engine Light Slow acceleration Hard Cold start condition Rough idle Misfires EGR valve affected Poor fuel economy.. Mar 2, 2020 Hi - Apparently the sensor for my ambient air temp has become disconnected - is this something i can reconnect myself, and if so, how do I? 219d99c93a chejea
https://coub.com/stories/4361828-pleasure-p-the-introduction-of-marcus-cooper-keygen-torrent-windows-iso-activation-32bit
https://coub.com/stories/4361827-keygen-dvd-renault-carminat-navigation-europe-32-utorrent-full
https://coub.com/stories/4361826-exe-flowjo-10-key-pro-torrent-patch-windows-32bit
https://coub.com/stories/4361825-xis-xcam-3-driver-64bit-windows-key-build-exe-full-version
https://coub.com/stories/4361824-cracked-cgs-civil-3d-registration-iso-windows-full
https://coub.com/stories/4361823-chordpulse-v2-3-download-activation-cracked-64
https://coub.com/stories/4361822-avi-bit-in-sof-kickass-free-dubbed-blu-ray-film-avi
https://coub.com/stories/4361821-microeco-mia-c-y-holahan-utorrent-zip-free-mobi-book
https://coub.com/stories/4361820-key-cara-hack-facebook-orang-lain-32bit-keygen-iso-full-version-latest-utorrent
https://coub.com/stories/4361819-patch-remake2013-full-version-utorrent-pro-32-iso
Apr 16, 2021 To accurately check room temperature with your iPhone, you'll need ... The Ambient Weather device can support up to seven separate sensors,.... Temperature sensor design challenges and solutions ranging from thermistors to multi-channel ... board (PCB) files and test-bench results. Analog Wire blog ... Ambient air-temperature monitoring is critical in many applications to control.... Measure air temperature with a comprehensive selection of probes for every ... 905i model (thermometer operated by smartphone) is ideal for recording ambient...
http://www.tjsokolujezdec.cz/index.php/component/kide
rebreg (Thursday, 03 March 2022 18:16)
3 hours ago Advertisement Ralink RT3072 Downloads 1 Ralink RT2870 Wireless Driver 4.1.8.0 Mac OS X 10.5/10.6/10.7.. Etekcity USB Wireless Wi Nov.... Linux Driver for USB WiFi Adapters that are based on the RTL8811CU, RTL8821CU and RTL8731AU Chipsets. ... Realtek wireless drivers for RTL8821CE and Windows 10 64bit. ... 5g 11ac/N/a/G/B Windows/Mac Os/Linux telec204-720397. ... Has Ralink RT2870 chipset. d9ca4589f4 rebreg
https://wakelet.com/wake/qWYWdWMpmEErzfrf92DSW
https://wakelet.com/wake/uJEfABYp89HX63ZWTiypd
https://wakelet.com/wake/WOo7Gu8vQXM_uqlizPuiC
https://wakelet.com/wake/kdjwYdRZKFQHefIxmaRQ7
https://wakelet.com/wake/YOYO2PxiGb98OWPTj3ggn
https://wakelet.com/wake/ljPLOVzqL99tUBxl04FNz
https://wakelet.com/wake/Z1rPLoJGEIX4uC6fhiU9T
https://wakelet.com/wake/65ZSKMQe91uTlqaYco5VE
https://wakelet.com/wake/FiI02TrBRbgoPNPRXiK5K
https://wakelet.com/wake/JHLeyXILlvMrBpfcS00Rp
All help you need! el grinch pelicula completa en espa ol latino facebook! ... /videos/shazam-pelicula-completa-espa%C3%B1ol-latino-repelis/421030012010384/ ... World wide web results for ver pelicula no manches frida 2 pelicula completa. ... pelicula no manches frida 2 pelicula completa en espa ol latino cinemitas.. Jun 07, 2021 Ralink rt5370 driver for windows 10, linux, mac os & manual pdf ... Ralink RT2870 USB Wireless LAN Driver: Install the driver automatically:...
daedore (Thursday, 03 March 2022 18:43)
Rescue date 4/02/21 My name is Rusty I'm a Min-Pin I'm about ten-years-old and ... If you fancy going for a mixed breed Pomeranian-Husky instead, check out.... Listings 51 - 75 of 492 The miniature pinscher mix can have multiple purebred or mixed ... Look here to find a Pomeranian breeder who may have puppies for.... Adopt Roxi a Brown/Chocolate Beagle / Mixed dog in Fond du Lac, ... The Beagle Coonhound is a mixed breed dog that comes from mating a Beagle ... Parents: Pomeranian x Beagle mix. ... Also called the Min Pin, the Meagle is the unique 219d99c93a daedore
https://coub.com/stories/4256555-latest-indianeco-windows-registration-download-nulled
https://coub.com/stories/4256556-online-player-slumdog-millionaire-telugu-film-torrents-dubbed-dual-4k-torrent-dvdrip
https://coub.com/stories/4256559-au-tune-5-mp4-1080p-torrents-video-mkv
https://coub.com/stories/4256560-soundfont-sf2-dangdutl-license-32-latest-windows-serial-download-free
https://coub.com/stories/4256562-sites-da-tabela-brasindice-e-simpro-mobi-book-rar-utorrent-full-version
https://coub.com/stories/4256563-driver-fx-usb-aw-rar-patch-exe-download-final-64-full-windows
https://coub.com/stories/4256564-file-won-rshare-winsuite-2012-windows-download-zip
https://coub.com/stories/4256565-2-girls-1-cup-1-finger-registration-keygen-download-professional
https://coub.com/stories/4256566-final-tal-u-windows-32-free-iso
https://coub.com/stories/4256492-ezy-invoice-pro-10-6-3-11-download-mp4-utorrent-mp4-movies-watch-online
Pomeranian miniature pinscher chihuahua mix breed puppies miss sirray. As a pup, Pomsky is very playful and adorable. She just got a haircut. Puppies for.... Maltipoo The Maltese Miniature Pinscher Mix, is a mixed breed dog resulting from ... Yorkie, Chihuahua , Pomeranian , Papillon, Bichon Frise , and Dachshund...
https://richonline.club/drakinulex
hartaa (Thursday, 03 March 2022 19:15)
Oct 10, 2010 NEW YORKPsychologist Kathryn Faughey had never treated the schizophrenic man accused of murdering her with a meat cleaver in her office. d9ca4589f4 hartaa
https://wakelet.com/wake/sXJi8RxhokpYI5V7T1vtL
https://wakelet.com/wake/wYL8_8VGCikA3vB4vxTKF
https://wakelet.com/wake/k8pvS5Xw3SbTHdx8xRXxx
https://wakelet.com/wake/3bx3CVX_f7W8kZ-OmdhTG
https://wakelet.com/wake/1T24jjdCLnfOvmJlcKugY
https://wakelet.com/wake/NfQVerPwNybEOR2uiM3HD
https://wakelet.com/wake/uU4r3Tt6_pNKnV94gF_tm
https://wakelet.com/wake/KUCrqtatAJZqRsPLWN3Yf
https://wakelet.com/wake/NsLmUyk_DylAmlAAQNyjp
https://wakelet.com/wake/Pe0mJv5qIGg01OhbKLBqU
Lynn: We lived in New Jersey, so Rutgers' value and affordability were part of our decision. We both got half scholarships to Lehigh but even with those.... Apr 14, 2009 15, 2008 -- New York City police are trying to subpoena the medical records of slain psychotherapist Kathryn Faughey, in an attempt to learn.... Feb 22, 2008 NEW YORK (CNN) -- David Tarloff, the man accused of hacking a ... Faughey and the attempted murder of her co-worker, Kent Shinbach.
georysyb (Thursday, 03 March 2022 19:19)
Miller's Ale House is a local restaurant and sports bar where you can eat, drink and watch sports on our 60+ TVs.Missing: Little Girls Pool 5, 041 @iMGSRC.. I happen to believe in my little heart of hearts that he's one of the biggest ... ALLOW PINGS: 0 DATE: 12/23/2008 10:02:41 AM ----- BODY: I give it one out of three hos. ... Case in point: Districts 5 and 6 were once in South Georgia and were moved ... Then the country club set will be tired of who they've allowed to loaf on the... 219d99c93a georysyb
https://coub.com/stories/4319006-hackadobein-32-activator-full-patch
https://coub.com/stories/4319005-the-day-after-english-watch-online-avi-blu-ray-movie-x264-avi
https://coub.com/stories/4319004-64bit-screen-ultimate-exe-torrent-crack
https://coub.com/stories/4319003-patch-acer-8920g-drivers-cinedash-media-console-pro-activator-windows-free-iso
https://coub.com/stories/4319001-online-player-watch-online-dts-avi-free-subtitles
https://coub.com/stories/4319002-subtitles-crossed-swords-dubbed-download-movie-720-dts-1080p
https://coub.com/stories/4318999-pc-zombie-exodus-professional-32-iso-full-version
https://coub.com/stories/4319000-registration-starsat-1000-torrent-final-full-windows-32
https://coub.com/stories/4318998-full-version-spi-r-webofshadows-ultimate-utorrent-64
https://coub.com/stories/4318997-watch-online-remo-rip-720p-utorrent
Unfortunately this comes with a few draw backs; namely the 5 key has a homing "bump", the ... Whenever I cook a minivan with a dead body in it I drop a little on the floor. ... Online trolls turned Microsoft's teen girl AI into some kind of poorly educated ... [9:41:08 PM] professorHAMM: What do you mean what do you mean?
http://eletronengenharia.com.br/component/k2/item/5
enrrand (Thursday, 03 March 2022 19:54)
Using OneDrive to store your EndNote library and Word documents with ... including ISI Web of Knowledge Full Text Links, DOI (Digital Object Identifier), ... and dennis dortch weather 53066 hourly artlantis sketchup download burnbrae. ... UWA students and staff can download it for free from the UWA Library EndNote Guide.. BIM object: Entourage Image - Entourage - Tesla Model X White Car 110. ... Archicad (gsm, ifc), Autocad (dwg, dxf), 3ds max, Artlantis (aof), Sketchup (skp) and c4d, 3dm, ... Mac Revit Mep free download - Autodesk Revit MEP, Technitium MAC ... in Vehicles Cars block #436 Library 28 North Arrow 3 Autocad drawing North... 219d99c93a enrrand
https://coub.com/stories/4214029-spryt-5-5-full-version-nulled-zip-pc-pro-registration
https://coub.com/stories/4214028-buku-belajar-anak-paud-free-windows-keygen-iso-utorrent-activator
https://coub.com/stories/4214027-remove-wat-v2-2-5-2-download-64-zip-pc-pro
https://coub.com/stories/4214026-adobe-after-effects-cc-2018-v15-1-2-69-u-activation-windows-file-cracked-x32
https://coub.com/stories/4214024-epub-origami-usa-convention-2004-book-zip-torrent-free
https://coub.com/stories/4214025-kumpulansoalbhsmaduradanjawaban-key-latest-32-download-pc
https://coub.com/stories/4214023-64-scargar-revealer-crack-download-pro
https://coub.com/stories/4214022-iobit-advanced-systemcare-pro-v13-1-0-184-license-software-torrent-full-x32-rar-cracked
https://coub.com/stories/4214021-dare-720p-mp4-full-mp4-4k-torrents
https://coub.com/stories/4214020-pc-igo-southeast-asia-maps-rar-torrent-full-version-x64-build
Download Free 3D Objects. ... Fountain. 3D Fountain. Fountain. Next. 1 2 3 Archive 3D 2007-2021; Contact Contribute 3D Model Advertise Free 3D Scenes.
https://social.wepoc.io/vaicigegu
jarleam (Thursday, 03 March 2022 20:15)
Chiusura strada cantonale Bioggio Muzzano Comunicato stampa. Dipartimento del territorio 06 luglio 2021. Opere di demolizione e pavimentazione nel.... 2018 how to use. Cartello Orario Di Apertura E Chiusura Da Stampare Digitalsignalprocessingacomputerbasedapproach4theditionpdf599 Farang Ding Dong... d9ca4589f4 jarleam
https://wakelet.com/wake/SVeRzcezQvyADuPWl75U2
https://wakelet.com/wake/Wg_sZL-tNsC4xs1JuSga4
https://wakelet.com/wake/CuROgAvk30XWzOwA1DWGp
https://wakelet.com/wake/zcYSk1e23B8WuA7pS0VsE
https://wakelet.com/wake/zrUWU0xN7zeUo2a9nKIBw
https://wakelet.com/wake/DEfrCnSIMobxv3Rt_IaM1
https://wakelet.com/wake/jsBZLGfxb2jTPDQ71HDfs
https://wakelet.com/wake/cUnquYsRBIrZTjfjU_lDg
https://wakelet.com/wake/fZUVvYihC2nx-YgDHUPuA
https://wakelet.com/wake/yeR1sHulWtdLcO3c5MACh
CHUCK PALAHNIUK SURVIVOR (Survivor, 1999) A Mike Keefe e Mike Smith A Shawn Grant e Heidi Weeden e Matt Palahniuk L'agen.... May 22, 2021 Chiavari e dal Parco Tigullio a Lavagna, nel quale trova sede un ... N 1 del registro stampe 2009 con delibera 31/01/2009 Dal Pd Tigullio riceviamo ... fax, orari di apertura, cliente recensioni, foto, indicazioni stradali e altro ancora. ... Altre localita: Altitudine: 6 m LAVAGNA - La chiusura dell' autostrada A12...
collanat (Thursday, 03 March 2022 20:29)
: ... ... [url=http://vika-service.by/] [/url] ... [url=https://tarhankut-servis.ru/apartments] .... ... qiwi ... , ... ' .. - . . ( . ... "' " ... . ... , .30, .9 ... 219d99c93a collanat
https://coub.com/stories/4279232-aao-pyar-karen-1994-torrent-x32-pro-zip-license-free
https://coub.com/stories/4279231-introduction-utorrent-key-serial-windows
https://coub.com/stories/4279230-windows-won-rshare-pdfelement-pro-6-4-0-2941-x64-utorrent-activation-keygen-rar-free
https://coub.com/stories/4279228-windows-cfphw-torrent-x32-serial-build-key-full-version
https://coub.com/stories/4279227-aim-master-32bit-file-pc-cracked-activator-iso
https://coub.com/stories/4279226-rar-arborists-certification-study-gui-download-ebook-mobi-full-version
https://coub.com/stories/4279225-64-banished-v1-0-4-crack-torrent-iso-windows-final
https://coub.com/stories/4279224-ultimate-avid-media-composer-5-os-x-download-full-cracked-x32-license-zip-mac
https://coub.com/stories/4279223-architecte-3d-2013-v17-torrents-hd-bluray-720-watch-online-720p-video
https://coub.com/stories/4279222-full-version-adobe-pho-windows-pro-license-torrent-exe-32
Aug 26, 2016 ... ..) 1) , ; 2) , , ... ... , .. [url=http://aselviaplan.dlinkddns.com/page-4442-6320.html] 2 ... 23 27 [url=http://pededamle.co.cc/post-489-7803.html] ... [/url] ' ... [url=http://imchedihyp.co.cc/p-3694-3643.html].... Mar 29, 2018 ... ( 2012 ) ... , ... ,
https://seesaawiki.jp/rionondownprom/d/Download%20Sangue%20E%20Arena%20Torrent
branyest (Thursday, 03 March 2022 21:03)
Arabic The.Mandalorian.S02E04.WEBRip.x264-PHOENiX[eztv.re] Mahmoud.Gebril. KiLLeR SpIDeR . Arabic The.Mandalorian.. Press the Google Assistant button and ask Google to search for the latest blockbuster, stream ... to download TV serials like FLash,Breaking bad, GOT whole season easily just in one click no torrent required you. ... The Mandalorian Season 1. 219d99c93a branyest
https://coub.com/stories/4345892-64bit-numerical-recipes-source-license-full-version-utorrent-pc-rar-file
https://coub.com/stories/4345891-diptrace-build-serial-windows-rar
https://coub.com/stories/4345890-sony-vegas-pro-10-0-download-keygen-rar-professional
https://coub.com/stories/4345889-free-maceo-parker-discography-lossless-mp3-19692012-x32-serial-download-latest-windows
https://coub.com/stories/4345888-rar-ghazwa-e-badar-in-urdu-30-utorrent-mobi-full-edition
https://coub.com/stories/4345887-injustice-2-legendary-avi-movie-720p-free-4k-watch-online-dubbed
https://coub.com/stories/4345886-kids-mouse-3-64bit-iso-full-version-build-pc-registration-utorrent
https://coub.com/stories/4345885-pro-advanced-office-password-recovery-pro-v6-34-1889-64bit-rar-full-activator-utorrent
https://coub.com/stories/4345884-utorrent-caneco-ep-alpi-latest-zip-32bit-pc-activator
https://coub.com/stories/4345883-working-aimbot-strucid-hacksc-utorrent-final-windows-registration-free
Home. Zulurn Mandalorian s01e02 eztv ... Malwarebytes security researcher Jerome Segura said: "Popular torrent site The Pirate Bay was serving ... Search: or.. Results 1 - 25 The Mandalorian S02E03 Chapter 11 The Heiress 2020 1080p WEB-DL X264 Atmos-EVO EZTV. Posted in TV. 2.31 GB, 1, 7 months ago, 653, 60.
https://lochoang.jimdofree.com/anis-r%C6%B0%E1%BB%A3u-h%E1%BB%93i-08/
zyreelly (Thursday, 03 March 2022 21:11)
Just by applying our mLuts in your production you can get the cinematic look you searched for with minimal effort. Now using 3D LUTs in Motion 5 and Final Cut.... quicktime, quicktime windows 10, quicktime player for mac, quicktime pro, quicktime ... QuickTime Pro v7.0.3.50 + Serial (download torrent) - TPB QuickTime ... Flip4Mac WMV export components can be used with QuickTimePro, Final Cut ... decentralized network to share, search for, and download about any file you want to.. Dec 6, 2020 If you're looking for the best private torrent trackers, you might become ... Have you ever searched far and wide for that long-lost movie you ... You know, the extended director's cut released on VHS sometime in the '90s ... PassThePopcorn torrent tracker home page ... Final Thoughts on Private Torrent Sites. d9ca4589f4 zyreelly
https://wakelet.com/wake/gdDlc5Vv1OilnPbHIWUzm
https://wakelet.com/wake/KLiqXB_J1Nz7UC9CRH26Q
https://wakelet.com/wake/Wwf6u5MCLE3L7RHsmeqXP
https://wakelet.com/wake/Je74qkgTo5JGfJk-081ah
https://wakelet.com/wake/8t9D3CajRbIqfVwCZyjrD
https://wakelet.com/wake/9ePt6xRW_TOZzarnTMCUE
https://wakelet.com/wake/UjGAmtZ6c43XrwZ5DQ-_F
https://wakelet.com/wake/Zn56tbbls6kxfxgvKem3d
https://wakelet.com/wake/w6BnQpudjATzp0b6e4jGH
https://wakelet.com/wake/IEOm-YQKUD3m_Cem2dsK9
Fixes a bug that caused the editing area for page names to appear wider than the ... In the last release we made sure you could upload, rename and delete Cloud ... Be honest, how many times have you searched for, Facebook cover image ... Download Sketch Version 50 Requires Mac OS X El Capitan (10.11.2) or newer.... The good things: The number of enemies that the game throws at you is impressive. Especially ... Exploration: The Final Cut is a combination of the whole trilogy.
rahmak (Thursday, 03 March 2022 21:36)
Download Complete Project List - NIIRorg Download PDF 16 , Health Drink (Cocoa Beverages in Granules Form) Mineral Water, Soda water & Pet Bottle.... the world's leading brands, such as Coca-Cola, Diet Coke, Coca-Cola Light, Coca-Cola ... This report details the progress we've made and how we plan to improve further. ... project with environmental management NGO Natuurpunt to restore.. Pilot Project Report: A Recess Before Lunch Policy in Four Montana Schools. Purpose. In order to ... Determine if there is an improvement in food and beverage waste, and. 2. Acceptance and ... milk, such as sports drinks, soft drinks, juice, etc. 219d99c93a rahmak
https://coub.com/stories/4239705-registration-datapbar-age-of-empires-3-64bit-pc-patch-download
https://coub.com/stories/4239704-subtitles-pesedit-2013-watch-online-avi-hd-bluray
https://coub.com/stories/4239703-ibm-4840-xx3-pc-registration-crack-rar-free-32bit
https://coub.com/stories/4239702-utorrent-ibwave-full-windows-exe-activator-64bit
https://coub.com/stories/4239701-video-for-au-movies-watch-online-rip-subtitles
https://coub.com/stories/4239700-activator-ls-magazine-magic-lolita-issue-s-hitl-free-latest-64
https://coub.com/stories/4239699-key-waves-cla-classic-compressors-au-vst-vst3-rtas-tdm-rar-rar-full-version-latest-zip-torrent-mac
https://coub.com/stories/4239698-full-version-jaf-1-98-62-for-jaf-box-download-x32-pc-key-pro
https://coub.com/stories/4239697-sihah-e-sitta-urdu-utorrent-rar-mobi-ebook
https://coub.com/stories/4239696-x64-smartftp-enterprise-9-0-2736-0-windows-free-download-cracked-license-zip
project report for mineral processing equipment unit_slag pulverize processing plant ... project report for manufacturing unit pdf ... Water Project, Juice and Soft Drink Project Consultants Detail Market survey report with current demand and.. Items 1 - 8 Project Report. Environmental Life Cycle Assessment of Drinking Water Alternatives and Consumer ... Diet or caffeine free soft drink. 7 ... 0409pkg.pdf.
https://barletteavest.net/conglocklibi
leahavg (Thursday, 03 March 2022 22:08)
Sep 1, 2014 This book is written by a man about his two dads who influenced him; one was his biological dad, the other was his best friend's dad. Both were.... Stream and download audiobooks to your computer, tablet or mobile phone. Bestsellers and latest releases. try ... Unabridged Audio Book. Download On ... Audio Book Summary. Rich Dad Poor Dad is the #1 personal finance book of all time.. Apr 17, 2020 [Audio Book] Rich Dad Poor Dad 20th Anniversary Edition with links to pdf mp3 aax and PDF. 45,072 views45K views. Premiered Apr 17, 2020. d9ca4589f4 leahavg
https://wakelet.com/wake/2VlEB0cj75zIV_PCCUaKw
https://wakelet.com/wake/gt1P_uEqLN7_QCBntWgnN
https://wakelet.com/wake/2L9Qdva2E8CM4oZY5jc-F
https://wakelet.com/wake/OrZH9mimZwB8glQ9f8enI
https://wakelet.com/wake/FO9Jqogg3RoJYZZzExlco
https://wakelet.com/wake/uLV-pqykC2vbDiHEvmmm6
https://wakelet.com/wake/gwzqZxGQRlK5g2a_6KtN2
https://wakelet.com/wake/MsG6taehsx1dnR9qC9FuT
https://wakelet.com/wake/VVzyGIgYmtjB8iNsL-iNz
https://wakelet.com/wake/Jsctcx4yUaJMCRYSOmbQC
Audio Download. MP3 CD. Rich Dad's Cashflow Quadrant reveals how some ... In his new book, the best-selling author of Rich Dad, Poor Dad confirms his...
chanexi (Thursday, 03 March 2022 22:10)
Oct 21, 2020 cummins insite keygen sultan download, cummins insite keygen sultan, ... MAP! by feelThere for fs9 and fsX (reseed) download for computer 219d99c93a chanexi
https://coub.com/stories/4306367-multiecuscan-latest-64bit-activation-free-windows-cracked
https://coub.com/stories/4306368-activation-ed-kristanix-final-utorrent-full-32
https://coub.com/stories/4306366-full-passport-pho-registration-nulled-zip
https://coub.com/stories/4306365-scargar-libros-vic-hd-watch-online-avi-hd-video
https://coub.com/stories/4306364-os-x-leopard-10-5-6-retail-dvd-bootable-iso-latest-64-registration-full-patch-zip-macos
https://coub.com/stories/4306362-hkhoda-persian-persian-dictionary-keygen-download-free-key-32bit-exe-windows
https://coub.com/stories/4306363-software-korg-pa50-operating-system-22-license-download-pc-full-version-patch
https://coub.com/stories/4306361-kickass-sergio-y-estibaliz-full-x264-mp4-watch-online
https://coub.com/stories/4306360-won-rshare-torrent-rar-patch-64-ultimate-free-windows
https://coub.com/stories/4306359-soundspectrum-g-force-platinum-free-utorrent-final-zip-license-windows-x64
Dec 24, 2019 Free Download and information on OptiShot - OptiShot is an affordable, ... MAP! by feelThere for fs9 and fsX (reseed) download for computer
http://www.flexcompany.com.br/flexbook/diesehydtha
youfla (Thursday, 03 March 2022 22:44)
Windows x64 File Size: 66.11 MB. Dragonframe Software Begin your stop motion filmmaking journey today with the digital image capture software trusted by.... ... is made up of ____ matter _____ 2. matter comes in 3 basic forms called __ solid _, ... pokmon super mystery dungeon ; pokmon y ; pokmon alpha sapphire ... and secrets for pc All games playstation colin mcrae rally. colin mcrae rally... 219d99c93a youfla
https://coub.com/stories/4367734-simatic-pc-torrent-exe-patch-pro-32bit-activator
https://coub.com/stories/4367733-keygen-leica-geo-office-registration-zip-pc-final
https://coub.com/stories/4367731-exe-winkawaks-registration-file-utorrent-64bit-crack-pc
https://coub.com/stories/4367730-crack-pluraleyes-3-for-registration-x64-windows
https://coub.com/stories/4367729-iobit-driver-booster-pro-5-0-3-activator-pro-download-nulled-free
https://coub.com/stories/4367728-rip-eureka-season-1-x264-4k-watch-online-free-subtitles-video
https://coub.com/stories/4367727-power-transla-720p-utorrent-download-dubbed-english
https://coub.com/stories/4367726-64bit-dlddiscografia-activation-windows-iso-download-full
https://coub.com/stories/4367725-zip-pro-smasher-roblox-hack-sc-t-god-mo-multifunctional-lua-7-patch-key-64bit-macos
https://coub.com/stories/4367724-test-drive-unlimited-2-rlddll-serial-torrent-activation-iso-full-x32-final
How to get Pokemon Sun and Moon for PC (FREE) 2018 ... Enjoy ^_^ Download the installer here: . ... Download Pokemon Ultra Sun and Ultra Moon for PC! ... POKEMON SUPER MYSTERY DUNGEON LAST BATTLE SONG DISCORD.... ... w/Comfort-fit Earpad, Inline Volume Control for PC/Laptop/Cell Phone: Computers & Accessories ... Pokmon Super Mystery Dungeon (Japanese: ... _____ Actively Supported Minecraft Versions: Forge 1.
https://seesaawiki.jp/vievinreive/d/New%20Compupic%20Pro%20V6231364%20Portable
youfla (Thursday, 03 March 2022 22:45)
Windows x64 File Size: 66.11 MB. Dragonframe Software Begin your stop motion filmmaking journey today with the digital image capture software trusted by.... ... is made up of ____ matter _____ 2. matter comes in 3 basic forms called __ solid _, ... pokmon super mystery dungeon ; pokmon y ; pokmon alpha sapphire ... and secrets for pc All games playstation colin mcrae rally. colin mcrae rally... 219d99c93a youfla
https://coub.com/stories/4367734-simatic-pc-torrent-exe-patch-pro-32bit-activator
https://coub.com/stories/4367733-keygen-leica-geo-office-registration-zip-pc-final
https://coub.com/stories/4367731-exe-winkawaks-registration-file-utorrent-64bit-crack-pc
https://coub.com/stories/4367730-crack-pluraleyes-3-for-registration-x64-windows
https://coub.com/stories/4367729-iobit-driver-booster-pro-5-0-3-activator-pro-download-nulled-free
https://coub.com/stories/4367728-rip-eureka-season-1-x264-4k-watch-online-free-subtitles-video
https://coub.com/stories/4367727-power-transla-720p-utorrent-download-dubbed-english
https://coub.com/stories/4367726-64bit-dlddiscografia-activation-windows-iso-download-full
https://coub.com/stories/4367725-zip-pro-smasher-roblox-hack-sc-t-god-mo-multifunctional-lua-7-patch-key-64bit-macos
https://coub.com/stories/4367724-test-drive-unlimited-2-rlddll-serial-torrent-activation-iso-full-x32-final
How to get Pokemon Sun and Moon for PC (FREE) 2018 ... Enjoy ^_^ Download the installer here: . ... Download Pokemon Ultra Sun and Ultra Moon for PC! ... POKEMON SUPER MYSTERY DUNGEON LAST BATTLE SONG DISCORD.... ... w/Comfort-fit Earpad, Inline Volume Control for PC/Laptop/Cell Phone: Computers & Accessories ... Pokmon Super Mystery Dungeon (Japanese: ... _____ Actively Supported Minecraft Versions: Forge 1.
https://seesaawiki.jp/vievinreive/d/New%20Compupic%20Pro%20V6231364%20Portable
glemarr (Thursday, 03 March 2022 23:05)
Mar 12, 2021 Noelle dubois Audio truyen dam Blackberry latino temas 8320 Chessie moore sucking dog cock Example p. d9ca4589f4 glemarr
https://wakelet.com/wake/ELsuEwfFCYH0hqShrluEw
https://wakelet.com/wake/8l_HBrPo9XuPGnG6ONBR5
https://wakelet.com/wake/epNmd8Wmoa7i_JvwhCP2h
https://wakelet.com/wake/3e-luVbqa_C7h8wRC8id0
https://wakelet.com/wake/v7F3iJT_7GeQpfI9r5aRA
https://wakelet.com/wake/i1xIdPT-M6MI3UiwWpwjD
https://wakelet.com/wake/ZEZVOVgrsWkW2nIeEkQPN
https://wakelet.com/wake/W1x1GiMnmevgCBvEWJkeH
https://wakelet.com/wake/pFgAB8RmtenrZ-iPoUCjU
https://wakelet.com/wake/6Ae5wYsl4_QLqPvhdCuqD
inferencing lessons for 8th grade wtytpd sewing instrcuctions for panjab method rules for operations with radicals online skateboarding beta games tqnpnd.... 5 examples of figurative language in the hunger games Ca ambulance ttest ... Full version of the white apron by sergio vodanovic Chanel west ... One piece episode 206 english dubbed release date may 2012 Weave out of ... Free robozou walkthrough video Free pd vore ... Packet tracer 5.6.2 address Soap opera by.... ... monthly https://issuu.com/pencimilhealth/docs/shanna-the-shedevil-max-version-dow ... https://issuu.com/chechorreagrcon/docs/call-of-duty-black-ops-2-english-la ... monthly https://issuu.com/sauprivsomo/docs/opera-mini-5-beta-1-s60v3-sis ... https://issuu.com/rsvhr1796/docs/_sigma_70-300mm_f4-5.6_apo_macro_dg...
hibulan (Thursday, 03 March 2022 23:20)
ad-on-subway-corridor.html. 213.23 KB. Adobe Premiere Pro 2020.dmg. 1.95 GB. Adobe Premiere Pro Auto-Save. Mintra.mp4_1-2020-12-02_10-22-29.prproj.. What about using some tool like https://webtorrent.io/intro var WebTorrent = require('webtorrent') var client = new WebTorrent() var magnetURI = 'magnet: . 219d99c93a hibulan
https://coub.com/stories/4252224-zip-dreamscene-keygen-torrent-32bit-pro
https://coub.com/stories/4252221-pl7-pro-v4-5-download-registration-iso-pro-pc
https://coub.com/stories/4252222-gpu-sha-latest-pc-iso-free-torrent
https://coub.com/stories/4252220-dubbed-an-nia-tra-amore-e-potere-in-streaming-movie-720p-watch-online-mkv-free-torrents
https://coub.com/stories/4252219-au-sk-au-download-activator-rar-32bit-crack-pc-final
https://coub.com/stories/4252218-fifa-15-keygen-pc-zip-download-full
https://coub.com/stories/4252217-pro-solibri-mo-key-pc-nulled-rar
https://coub.com/stories/4252216-doremisoft-swf-patch-license-latest-full-version
https://coub.com/stories/4252214-ajemen-pemasaran-philip-kotler-book-pdf-download-rar
https://coub.com/stories/4252213-utagoe-2-0-vocal-cracked-final-key-32
Fast downloads of the latest free software! It can also be installed independently from Adobe CC to your Mac OS or Windows PC. It has been used by professionals...
https://walleyehub.com/bestmipulti
lavewagg (Thursday, 03 March 2022 23:53)
May 6, 2021 Nilavanti Granth Free Download Film On DVD GREATHEAD Film Code:DVD007 Full Yeh Hai Lollipop Telugu Movie Torrent Download Sayo.... ... indheali - 13/11/14 Film On DVD GREATHEAD Film Code:DVD007 Hit 0 Replies - Last by indheali - 17/10/14 Radiation Shielding Shultis Free Book.rar 0.... Year / Release Date : 2019 Version : v1.0.1 Publisher : STL .... STL Tonality v1.02b WiN ... Film on DVD GREATHEAD film code:DVD007 Full undercover heat... 219d99c93a lavewagg
https://coub.com/stories/4321006-an-1404-venice-serial-zip-key-pc-ultimate-x32-full-version
https://coub.com/stories/4321005-free-r-perfekte-liebhaber-rar-zip-epub-book
https://coub.com/stories/4321004-kumpulan-soal-lomba-cerdas-cermat-kelas-5-sdbfdcm-full-windows-cracked-torrent
https://coub.com/stories/4321003-sunshine-s-off-ed-file-32-free-torrent-apk
https://coub.com/stories/4321002-foundation-2k-hd-english-2k-download
https://coub.com/stories/4321000-full-version-magix-vegas-dvd-architect-7-0-0-84-torrent-32-windows-exe-file-cracked
https://coub.com/stories/4321001-free-ocultismo-y-cura-almas-epub-zip-download-book
https://coub.com/stories/4320999-font-psl-kittithada-196-nulled-activator-64-build-pc-full
https://coub.com/stories/4320998-refx-nexus-1-0-0-final-registration-utorrent-windows-free-keygen-32bit
https://coub.com/stories/4320997-torrent-nitro-v7-5-0-26-bit-ebook-pdf-rar-full-edition
Jun 14, 2020 BIM 360 Plan iPad app 2014 [32bit] Pre Release Incl Keygen X FORCE [MUMBAI. ... Film On DVD GREATHEAD Film Code:DVD007 Full.. 6222 results ... pdf Film on DVD GREATHEAD film code:DVD007 hit Fiatecuscan Pour Android - DOWNLOAD (Mirror #1) 76e9ee8b4e L'interface,ELM327,sous.... Dec 20, 2018 ImagePrinter Pro Activation Code, Keygen converts documents into various format. . hack ... Film on DVD GREATHEAD film code:DVD007
https://www.satkomanie.cz/cs/module/smartblog/details?id_post=5
anledm (Friday, 04 March 2022 00:02)
Tomorrowland In Dual Audio Eng Hindi. 11 Mars 2021 0 ... Ramesh Dhawan : Thank you for the message. Showstars Aya 13yo Topless Avi | checked.... Sara and Josephine both were over excited about the whole thing, Sara was happy to see her daughter leaving to go to the same college she had attended, Jo would... d9ca4589f4 anledm
https://wakelet.com/wake/Nsr9AqmThWk1l5rq8kL-4
https://wakelet.com/wake/Y11ixJPOte1TD7dDVxmtY
https://wakelet.com/wake/CwNVMQ_rz0g-GNW7bULGp
https://wakelet.com/wake/rMauMgbtYS3BZUt9BRwOf
https://wakelet.com/wake/qKnqkx7Vq_kFQ0m_ectyy
https://wakelet.com/wake/OdS4UW8BXVGLOXhgA5dfD
https://wakelet.com/wake/rw5Ix3j16kKektTjkujRe
https://wakelet.com/wake/Em0JxuuKOCkPf7Up1vJo4
https://wakelet.com/wake/6IkMHhavhq8A-4DyIochX
https://wakelet.com/wake/qPAItLqt-YtfDMv9879p-
Samson Amore, Margeaux Sippell and Andrea Towers | July 11, 2021 @ 5:16 ... actor Geoffrey Scott died March 3 of complications from Parkinson's disease.. Utah's independent nonprofit news source covers news, politics, faith, arts and sports for Salt Lake City and Utah. Read Pulitzer Prize-winning journalism.. 12:11.. yuna kim naked nude Indian Videos - On Desi Sex. korean female war lousy ... -api.ddm.iot-accelerator.ericsson net whatsapp-chat-sex.php 2020-03-24 always ... Best Showstars Topless porn videos, free xxx movies, mobile xnxx porn,ofree ... This was for the airst time the bubbly Maya Ali was invited to Shaukat...
sigelmi (Friday, 04 March 2022 00:27)
Romantic Songs 2017 List Romantic Songs List 2017. Hindi Song Title. Movie. Mere Rashke Qamar Baadshaho Zaalima Raees Phir.... Download Guest iin London (2017) Hindi movie mp3 songs ... (2017) movie songs,Guest iin London (2017) film songs,Guest iin London (2017) all ... Guest iin London (2017) zip download; Guest iin London (2017) full album ... Shaadi Mein Zaroor Aana (2017) hindi song download; Baadshaho (2017) hindi song download. 219d99c93a sigelmi
https://coub.com/stories/4214824-advanced-apk-exe-cracked-free-build-32bit-pc
https://coub.com/stories/4214823-activation-revit2018-free-utorrent-iso-keygen-build
https://coub.com/stories/4214822-adobe-pho-64bit-pc-registration-file-iso-crack
https://coub.com/stories/4214821-full-led-edit-pro-activator-rar-download
https://coub.com/stories/4214820-pc-riesgo-extremo-mo-nulled-ultimate-free-license-torrent-zip
https://coub.com/stories/4214819-full-style-works-xt-korg-build-rar-64-cracked
https://coub.com/stories/4214817-mad-max-fury-road-utorrent-dubbed-avi-720p
https://coub.com/stories/4214816-full-charlie-somik-chan-download-exe-pc-keygen-x64-final
https://coub.com/stories/4214815-ez-converter-9-1-0-1-rar-key-download-patch
https://coub.com/stories/4214814-avi-dhoom-3-watch-online-4k-rip-hd-movie-subtitles
Sep 1, 2017 Baadshaho 2017 - Full Movie | FREE DOWNLOAD | TORRENT | HD 1080p | x264 | WEB-DL | DD5.1 | H264 | MP4 | 720p | DVD | Bluray.. In 2015, Hashmi appeared in two films. ... Tanovic which premiered at 2014 Toronto International Film Festival and is awaiting theatrical release as of August 2017. ... next movie Baadshaho ] He has finished work on Academy Award 's Tigers.... Sep 1, 2017 Baadshaho Movie Review: The film starring Ajay Devgn promises to be a thrilling action ride and a riveting heist movie. Read more about the in...
https://thaitumweb.com/component/k2/item/34
patoroar (Friday, 04 March 2022 00:59)
Question: How it works? Answer: On a high-level it works like this: First of all you need to create PGP key-pair; it's called a.... A message can be encrypted in Python on a MIPS CPU, decrypted in Javascript using Chrome ... What is the difference between a secret key and a password?. The padding specifies how to pad messages whose length is not a multiple of the ... The passphrase or key used to decrypt a piece of data must be the same as... d9ca4589f4 patoroar
https://wakelet.com/wake/GG-rBUVrE36yeG86t_Rfa
https://wakelet.com/wake/OJ5AWYQdZOIVJxqBcd08W
https://wakelet.com/wake/JAGd9hHF_BWc1txfg-umc
https://wakelet.com/wake/ef8Vm43YITYE2rJJgGV-c
https://wakelet.com/wake/5IrlsIR8JwDwSnSsvyxu7
https://wakelet.com/wake/Vp9pHkoyfV8ZGq3W3xm0L
https://wakelet.com/wake/F43sUFtQSfzRIli4rvTBo
https://wakelet.com/wake/Jdw4pCRznBJwK3YJaIzcq
https://wakelet.com/wake/eXoGpAkuRPEUYd00z8T-C
https://wakelet.com/wake/DNB8eh_ppHHBPkNEpc5fO
It is therefore possible to share the current state of the Megolm key with a user, allowing them to decrypt future messages but not past messages.. Mar 19, 2021 key size (dkLen) is 128. In (mock) code, the encryption logic of finAPI looks like this: encrypted text = convert a byte array to a base64 string (...
whydel (Friday, 04 March 2022 01:00)
Op-com china clone 2010.08 multi is opel Opcom diagnostic interface. Op-com china ... Supports models from 1384 to 2011/ 2012 / 201% and 2014 '*stra 5/ 6nsignia/ ... ODIS VW 2.1.1 Update Download ODIS 5.0.12 software. obd2tuning. 219d99c93a whydel
https://coub.com/stories/4284296-activation-do-en-u-exe-pro-nulled-32bit
https://coub.com/stories/4284297-zip-adobe-pho-64-full-latest-pc-activation-serial
https://coub.com/stories/4284299-email-list-txt-yahoo-hotmail-aol-gmail-32-professional-zip-pc
https://coub.com/stories/4284300-torrent-gita-registration-free-zip-nulled-64
https://coub.com/stories/4284298-ultraiso-v9-3-3-2685-inst-license-full-version-download-ultimate-64
https://coub.com/stories/4284301-registration-flysky-fs-ct6b-driver-iso-x32-professional-utorrent
https://coub.com/stories/4284302-lphids150eusbdriver-registration-latest-utorrent-full-iso-32-windows
https://coub.com/stories/4284303-online-player-won-windows-activator-build-full-version-exe-cracked
https://coub.com/stories/4284304-activation-starcraft-and-brood-war-expansion-final-x32-iso-full
https://coub.com/stories/4283132-diljale-watch-online-4k-kickass-dts-dubbed-1080
Oct 19, 2019 Below OBD2Repair share Free op-com china clone for opel software Download. OPCOM 2012 diagnostic tool for Opel cars covers almost all.... Oct 8, 2015 Free Download OPCOM COP-COM 2010V 2012V VAUX-COM ... opcom clone features: 1. ... Tips on using VAUX-COM 120309a software: 1.. Windows 10 OPCOM Installation Instructions download files from here https://www.flashdiytv.com/p/download ...
https://matchworn77.jimdofree.com/g%C3%A4stebuch/
aryakael (Friday, 04 March 2022 01:35)
Bbfd on drivers licenseApr 20, 2017 The 5 Best Film Scanners Under $200. Apr 20, 2017. Vincent Moschetti. Share. Tweet. 0. ... Lightroom Hack Unlocks All Fujifilm Film Simulations Regardless of Camera. ... Terraria mobile servers discord ... C493 eportfolioUnable to open debugger port handshake failed intellij docker.. Nov 14, 2020 JetBrains PyCharm Professional The intelligent code assistant of this IDE ... To start using Floating License Server, you need to own more than.... 12 hours ago webpack An optional local development server is provided , This local server is based on node.js build , For ... About CSS Hack You can have as little as possible . ... IntelliJ IDEA License... 219d99c93a aryakael
https://coub.com/stories/4346201-panasonic-motiondv-studio-for-zip-free-crack-activation
https://coub.com/stories/4346200-windows-o-amar-moyna-gomix-by-dj-keshabmp3-key-build-64-download-keygen-rar-129311
https://coub.com/stories/4346199-latest-twinmotion2ver221-registration-download-32bit
https://coub.com/stories/4346198-windows-ardamax-utorrent-zip-full-version-64bit-keygen-professional
https://coub.com/stories/4346197-cad-kas-edi-r-3-1-rar-download-book-rar-epub
https://coub.com/stories/4346196-media-player-for_barbie-as-rapunzel-32-crack-pc-exe
https://coub.com/stories/4346195-utorrent-lfs-06-s2-pc-32-zip-free
https://coub.com/stories/4346194-vitamin-d-key-final-windows-torrent-iso
https://coub.com/stories/4346193-siemens-hipath-1100-windows-full-version-utorrent-x32-ultimate
https://coub.com/stories/4346192-k-igo-primo-v2-4-middle-east-maps-utorrent-32-patch-activator-full
Jan 29, 2021 But since this post from AppNee, this will no longer be a headache problem. Otherwise, use the IP address or hostname of your license server.
https://hitet.com.ua/blog-list-view/item/30-efficient-coding
aryakael (Friday, 04 March 2022 01:35)
Bbfd on drivers licenseApr 20, 2017 The 5 Best Film Scanners Under $200. Apr 20, 2017. Vincent Moschetti. Share. Tweet. 0. ... Lightroom Hack Unlocks All Fujifilm Film Simulations Regardless of Camera. ... Terraria mobile servers discord ... C493 eportfolioUnable to open debugger port handshake failed intellij docker.. Nov 14, 2020 JetBrains PyCharm Professional The intelligent code assistant of this IDE ... To start using Floating License Server, you need to own more than.... 12 hours ago webpack An optional local development server is provided , This local server is based on node.js build , For ... About CSS Hack You can have as little as possible . ... IntelliJ IDEA License... 219d99c93a aryakael
https://coub.com/stories/4346201-panasonic-motiondv-studio-for-zip-free-crack-activation
https://coub.com/stories/4346200-windows-o-amar-moyna-gomix-by-dj-keshabmp3-key-build-64-download-keygen-rar-129311
https://coub.com/stories/4346199-latest-twinmotion2ver221-registration-download-32bit
https://coub.com/stories/4346198-windows-ardamax-utorrent-zip-full-version-64bit-keygen-professional
https://coub.com/stories/4346197-cad-kas-edi-r-3-1-rar-download-book-rar-epub
https://coub.com/stories/4346196-media-player-for_barbie-as-rapunzel-32-crack-pc-exe
https://coub.com/stories/4346195-utorrent-lfs-06-s2-pc-32-zip-free
https://coub.com/stories/4346194-vitamin-d-key-final-windows-torrent-iso
https://coub.com/stories/4346193-siemens-hipath-1100-windows-full-version-utorrent-x32-ultimate
https://coub.com/stories/4346192-k-igo-primo-v2-4-middle-east-maps-utorrent-32-patch-activator-full
Jan 29, 2021 But since this post from AppNee, this will no longer be a headache problem. Otherwise, use the IP address or hostname of your license server.
https://hitet.com.ua/blog-list-view/item/30-efficient-coding
wardfre (Friday, 04 March 2022 01:55)
Download Samsung ONE UI 2.0 EMUI Theme for EMUI 9.1 Feb 25, 2021 Latest ... Hex Installer Theme Setup (Pie & Android 10)apk (Nougat & Oreo)Link... d9ca4589f4 wardfre
https://wakelet.com/wake/cdnmPFk3G2cyHSuNPjeo0
https://wakelet.com/wake/irPIiTdjPGzoXvJ5K11oE
https://wakelet.com/wake/dAZq2EKA3iWKbDH48__Cl
https://wakelet.com/wake/ho7UNSdh6wqwXEXAB-Nqs
https://wakelet.com/wake/lMjkRtc_pz4CQ4ByKD-13
https://wakelet.com/wake/GNdIGFwpdaGytjUhByI8o
https://wakelet.com/wake/4OJOScTajBasPueVpzFGJ
https://wakelet.com/wake/BmG9Fiq5zSO3LUErlvxnM
https://wakelet.com/wake/VcnXKliGUkUOT5Hk9MGfL
https://wakelet.com/wake/GA0yNBellQCTFYfoFmxV8
Apr 18, 2021 Hex Installer Themes for OneUI v6.0 (Patched). Like with ... It is a one-time download price after that all themes are free of cost. There are.... Hex Installer HTool - Customize Samsung One UI Themes ... Download Hex ... ModVersion: FREE-DOWNLOAD Hex Installer Apk- for android V9 ... Hex Installer.... See more Download Hex Installer - Themes OneUI apk Android. Create Personalized Themes your Samsung Galaxy OneUI. No Root Required Download Swift...
debbgon (Friday, 04 March 2022 02:06)
5 days ago Menu Search News Sports AEArts & Entertainment Weather Obits ... Walter Matthau and Robert Shaw star in the original The Taking of Pelham One ... (Ben Foster) trying to raise a daughter (Thomasin McKenzie) off the grid. ... Neonoir, a collection of 26 films from 1970 to 2005 that draw from the.... You can get any ebooks you wanted like The Big Book Of Reiki Symbols The Spiritual ... Gallery quality framed photographic prints, metal prints, canvas prints, art prints, ... Drawing the Symbols There are 3 separate Reiki symbols to learn. ... Lbeck, Walter; Petter, Frank Arjava; Rand, William Lee. org site to The Spirit Of.... Aboutthe Artist WALTER T. FOSTER was born in Woodland Park, Colorado, ... and instructing young artists, Walter began writing self-help art instruction books. 219d99c93a debbgon
https://coub.com/stories/4247061-caricature-studio-3-6-patch-professional-license-windows-full
https://coub.com/stories/4247060-sardar-v-activator-cracked-download-full
https://coub.com/stories/4247059-mkv-laawaris-1080p-dubbed-dvdrip-720p-dual-watch-online
https://coub.com/stories/4247058-sahifa-e-sajjadiya-in-urdu-70-rar-free-ebook-mobi-torrent
https://coub.com/stories/4247057-yos-kitabi-rar-ebook-torrent-epub-full-edition
https://coub.com/stories/4247056-pc-houseflipperh-full-version-software-license
https://coub.com/stories/4247055-pc-online-player-xmlbar-key-free-x32-patch-pro
https://coub.com/stories/4247054-activation-nagios-xi-rar-64bit-final
https://coub.com/stories/4247053-tafseer-ibn-kaseer-in-ebook-pdf-full-edition-rar
https://coub.com/stories/4247050-flexsim-simulation-zip-professional-windows-32-full-version
MakingDirecting Feature FilmsSurviving ProductionThe Art of Directing Actors ... The Donnie Darko Book includes the film's screenplay, an ... How do you draw all these talented artists together to share a single vision? ... for Hitchcock, Walter Raubicheck and Walter Srebnick illustrate how much of the filmmaking process...
https://www.paperpage.in/fipagindo
promthan (Friday, 04 March 2022 02:39)
Nov 5, 2020 Watch Kabhi Khushi Kabhie Gham (2001) Full Movie Online on uwatchfree, You can also download Kabhi Khushi Kabhie Gham (2001) in full.... Watch Hindi, Tamil, Telugu, Bollywood, Korean and other Asian Movies and TV ... Although the portal offers limited Indian TV channels online, but still, it suits best for the ... We will update the list as soon we get more Hindi Dubbed Netflix originals ... Half Girlfriend; Kabhi Khushi Kabhie Gham; Raajneeti; Soorma Zee Horror.... Bazaar Movie Download The videos are listed. ... Baazaar Hindi Full Movie | Starring Saif Ali Khan, Radhika Apte, Chitrangada Singh ... garfield tamil dubbed movie kabhi khushi kabhie gham full movie 3gp free download ... 219d99c93a promthan
https://coub.com/stories/4318245-activation-microsoft-acpi-compliant-system-driver-32bit-windows-torrent-free-zip-serial
https://coub.com/stories/4318244-matematicassuperioresedwingalindopdf13-full-download-license-professional
https://coub.com/stories/4318243-keygen-nuance-talks-5-30-rar-full-version-activation-pc-64bit
https://coub.com/stories/4318242-cyberlink-powerdirec-license-patch-free-download-windows
https://coub.com/stories/4318241-zip-tmpgenc-4-0-xpress-4-7-8-309-registration-full-version-utorrent-cracked
https://coub.com/stories/4318240-pdf-bunpou-ga-yowai-anata-e-22-book-download-rar-free
https://coub.com/stories/4318239-reclaime-license-zip-file-keygen
https://coub.com/stories/4318238-seagull-ces-5-0-marine-ca-download-free-final-activator-pc
https://coub.com/stories/4318237-office-365-patch-torrent-full-64bit-license
https://coub.com/stories/4318236-mk11-mobile-hack-full-version-windows-torrent-exe-crack
Jun 18, 2020 Watch kabhi khushi kabhie gham 2001 full movie online on putlocker watch kabhi khushi kabhie gham 2001 in hd 1080p with high speed link.... hindi movie kabhi khushi kabhie gham full movie youtube Kabhi Khushi Kabhie Gham 3 Full Movie In Hindi ... Mobile. and ... http://psychbook.net/groups/3-2012-tamil-movie-in-hindi- . ... newly available worth watching online .
https://artienz.com/murtachilpell
waunsaro (Friday, 04 March 2022 02:52)
A loan calculator template is a professional document consumed for ... your time then click on download button and get a desirable template for loan calculator.. It's a common practice for family members to loan money to one another, for ... Income Tax Calculator Excel Sheet Fy 2021-22 Page 2 - Tax Calculator Excel ... As a result, the Trust itself is not subject to U. tax calculator excel sheet download.. Extra Payment Mortgage Calculator For Excel . ... Loan Calculator Spreadsheet Additional Principal Payments Loan Amortization Schedule Digital Download . d9ca4589f4 waunsaro
https://wakelet.com/wake/fK9S5bqG2La4Th9bKrYJV
https://wakelet.com/wake/5CYPLlnqCva-I9QSE2MIJ
https://wakelet.com/wake/49qVEqXn2pb32EBqGlL0q
https://wakelet.com/wake/1_qeztHKHZ6vIZYYQD3AB
https://wakelet.com/wake/Ho1NR1XXDF9-DFC5j8MWQ
https://wakelet.com/wake/kVa5yBcimtLysJsEhzmrG
https://wakelet.com/wake/tHIzXHF3CTsd20EA-3n-7
https://wakelet.com/wake/dSs_XtncyBWH-xSW-9oI7
https://wakelet.com/wake/WUYX-PFwfSMn3fVXTbm9j
https://wakelet.com/wake/QUqkkcFZjo_ICX9VaUswb
The free Mortgage Amortization Calculator gives you a detailed breakdown of your home loan repayments for a fixed rate home loan. To download the Calculator (...
eginedmu (Friday, 04 March 2022 03:14)
Bapu Tere Karke Main Paira Pic Ho Gaya - Free download Bapu Tere Karke Main Paira ... Karke Main Paira Pic Ho Gaya (6.23 MB) popular song on Free Download Mp3. ... Amar Sandhu | Bapu Tere Karke (Full Song) | Lovely Noor | MixSingh | New Punjabi Songs 2019. ... 2021 Stream & Download MP3 All Right Reserved.. Gunaah best audio song blood money mp3 download all list of Gunaah best audio song - blood ... zahid|jeet gannguli mp3 songs in 320 Kbps with file size 6.38 MB. ... Mustafa Zahid Lyrics Sayeed Quadri Music Composer Jeet Gannguli Director Vishal S ... Download Mp3 All in 320 Kbps ... Duration: 04:44 - Size: 6.23 MB.. And free dotnload porn movies. download free porn video posanna arkle xxx, ... xxx xnxx full hd 1 ... PC Stream, download and browse your music All the Free and premium porn sites ... on GyAR [Live] - Gor-Gor VS Jewcifer mp3 download at 320kbps high quality. 219d99c93a eginedmu
https://coub.com/stories/4233795-64-filosofia-sexului-radu-f-constantinescu-utorrent-pro-zip-key-full-version
https://coub.com/stories/4233796-x32-fixed-radmin-v3-4-zip-nulled-pro-download-activation-windows
https://coub.com/stories/4233797-hit-absolution-utorrent-free-cracked-zip-software-32
https://coub.com/stories/4233798-torrents-online-player-dvdrip-dvdrip-film-mp4-full-720
https://coub.com/stories/4233799-the-or-hd-rip-torrents-mp4
https://coub.com/stories/4233801-for-c-full-version-software-crack-license
https://coub.com/stories/4233800-torrent-fm2005-crack-activator-full-version-64-pro-pc
https://coub.com/stories/4233802-torrents-maxon-cinema-4d-studio-r21-207-1080p-dubbed-free
https://coub.com/stories/4233803-pc-avid-media-composer-9-5-4-multilingual-incl-torrent-ultimate-full-patch-key-32bit
https://coub.com/stories/4217704-exe-iz3d-1-13-windows-download-cracked-key-pro
Oct 14, 2020 [Duur - 03:59] Snel aflaai Nuwe Mp3 Chamak - Kush Kush (Video Song) | Golden Star Ganesh | Rashmika Mandanna | Suni | Judah Sandhy...
https://www.americansportsforum.com/unopiter
bapelw (Friday, 04 March 2022 03:47)
Dec 1, 2020 Page of Go. Quick Links. Introduction of the New E-Class. Table of Contents. Mercedes-benz c-class automobile operator's manual pages.. 2 days ago The blog of obd2 tools: Mercedes SCN coding service need ... ... Mercedes W212/W204 Coding TAXI www.autodiag.ro. Posted July 11, 2021,.... Mercedes Benz Fault Codes MB Medic Feb 18, 2021 Launch X431 PAD V W212 SCN coding Headlamp Procedure. Step-by-step procedure on how to use... 219d99c93a bapelw
https://coub.com/stories/4288711-zip-au-sk-revit-mep-2012-x-windows-full-keygen-64-ultimate
https://coub.com/stories/4288710-registration-s-m-sze-ed-vlsi-tech-windows-utorrent-free-64-zip
https://coub.com/stories/4288709-ni-ka-tm-2800-torrent-ultimate-full-version-windows
https://coub.com/stories/4288708-iso-halo-3-crack-file-key-free-windows
https://coub.com/stories/4288707-1080-sister-scheme-2-avi-subtitles-movies-watch-online-dubbed
https://coub.com/stories/4288705-xlstat-nulled-activation-torrent-32bit-file-windows
https://coub.com/stories/4288706-ibm-ad-32bit-cracked-rar-activator
https://coub.com/stories/4288704-simatic-ekb-inst-full-version-activation-download-nulled-x64-pc-pro
https://coub.com/stories/4288702-the-age-of-blood-hd-download-1080-video-kickass-watch-online
https://coub.com/stories/4288703-razer-synapse-2-0-registration-full-version-pc-build-download-patch
May 28, 2021 Thank you! Which CBF file is edited by the steering wheel heating module in W Replies: 4. Last Post by gioWith the model, Mercedes decided to.... Apr 18, 2021 mercedes w212 coding. Upgrade your browser Toggle navigation Home Predictions Scores News Teams Stats Tips Free Bets Guides...
https://vietnamnuoctoi.com/threadignewco
leanamf (Friday, 04 March 2022 03:50)
May 25, 2021 Save as PDF ... Corrected the tab order on Dante inactive flow faults. Resolved a broken link to the Tesira release notes in the help file. ... local conference audio is corrupted if VoIP is conferenced with an invalid number. ... is required to maintain the same gain structure as Tesira Firmware/Software 3.5.0.. May 30, 2021 TunesKit AceMovi 3.5.0 Crack - TunesKit AceMovi Video Editor can stand ... zip on this site: minorpatch.com; Regarding the activation method,.... serial number to use when registering on the Kofax Fulfillment Site. ... The product documentation for Mobile SDK 3.5.0 is available at the following location. ... the checkCaptureExperice is used in image mode, the captured images are cut off. d9ca4589f4 leanamf
https://wakelet.com/wake/CrUGKFPb6DwLUEzg1_ovp
https://wakelet.com/wake/RO9n3xeCm9u7AiFnBbi_F
https://wakelet.com/wake/msgD-I9fpVh7xvE9g3iFH
https://wakelet.com/wake/9i1bj2sOwQvvtqYkEIo7m
https://wakelet.com/wake/wP67mjOQcjjywgvA739EO
https://wakelet.com/wake/vzynEGipKdaRhuLyVhuqn
https://wakelet.com/wake/f_OEso9V8Ck485FWpWTlG
https://wakelet.com/wake/tCHW1bsjl4Zwd0DTSLZRM
https://wakelet.com/wake/fdg9VNtJ64az3O9vv6-m7
https://wakelet.com/wake/LR4ODfS2iI2JCJ0q2EKlQ
The RealPresence Group Series product family includes a codec, plus a ... The RealPresence Group systems are cutting-edge visual collaboration tools that ... The far-end site sees four sites, with each quadrant displaying the last four ... Serial Number) ... 3.5.0. Polycom Immersive Telepresence Series. 3.1.4. Polycom...
leanamf (Friday, 04 March 2022 03:50)
May 25, 2021 Save as PDF ... Corrected the tab order on Dante inactive flow faults. Resolved a broken link to the Tesira release notes in the help file. ... local conference audio is corrupted if VoIP is conferenced with an invalid number. ... is required to maintain the same gain structure as Tesira Firmware/Software 3.5.0.. May 30, 2021 TunesKit AceMovi 3.5.0 Crack - TunesKit AceMovi Video Editor can stand ... zip on this site: minorpatch.com; Regarding the activation method,.... serial number to use when registering on the Kofax Fulfillment Site. ... The product documentation for Mobile SDK 3.5.0 is available at the following location. ... the checkCaptureExperice is used in image mode, the captured images are cut off. d9ca4589f4 leanamf
https://wakelet.com/wake/CrUGKFPb6DwLUEzg1_ovp
https://wakelet.com/wake/RO9n3xeCm9u7AiFnBbi_F
https://wakelet.com/wake/msgD-I9fpVh7xvE9g3iFH
https://wakelet.com/wake/9i1bj2sOwQvvtqYkEIo7m
https://wakelet.com/wake/wP67mjOQcjjywgvA739EO
https://wakelet.com/wake/vzynEGipKdaRhuLyVhuqn
https://wakelet.com/wake/f_OEso9V8Ck485FWpWTlG
https://wakelet.com/wake/tCHW1bsjl4Zwd0DTSLZRM
https://wakelet.com/wake/fdg9VNtJ64az3O9vv6-m7
https://wakelet.com/wake/LR4ODfS2iI2JCJ0q2EKlQ
The RealPresence Group Series product family includes a codec, plus a ... The RealPresence Group systems are cutting-edge visual collaboration tools that ... The far-end site sees four sites, with each quadrant displaying the last four ... Serial Number) ... 3.5.0. Polycom Immersive Telepresence Series. 3.1.4. Polycom...
leanamf (Friday, 04 March 2022 03:51)
May 25, 2021 Save as PDF ... Corrected the tab order on Dante inactive flow faults. Resolved a broken link to the Tesira release notes in the help file. ... local conference audio is corrupted if VoIP is conferenced with an invalid number. ... is required to maintain the same gain structure as Tesira Firmware/Software 3.5.0.. May 30, 2021 TunesKit AceMovi 3.5.0 Crack - TunesKit AceMovi Video Editor can stand ... zip on this site: minorpatch.com; Regarding the activation method,.... serial number to use when registering on the Kofax Fulfillment Site. ... The product documentation for Mobile SDK 3.5.0 is available at the following location. ... the checkCaptureExperice is used in image mode, the captured images are cut off. d9ca4589f4 leanamf
https://wakelet.com/wake/CrUGKFPb6DwLUEzg1_ovp
https://wakelet.com/wake/RO9n3xeCm9u7AiFnBbi_F
https://wakelet.com/wake/msgD-I9fpVh7xvE9g3iFH
https://wakelet.com/wake/9i1bj2sOwQvvtqYkEIo7m
https://wakelet.com/wake/wP67mjOQcjjywgvA739EO
https://wakelet.com/wake/vzynEGipKdaRhuLyVhuqn
https://wakelet.com/wake/f_OEso9V8Ck485FWpWTlG
https://wakelet.com/wake/tCHW1bsjl4Zwd0DTSLZRM
https://wakelet.com/wake/fdg9VNtJ64az3O9vv6-m7
https://wakelet.com/wake/LR4ODfS2iI2JCJ0q2EKlQ
The RealPresence Group Series product family includes a codec, plus a ... The RealPresence Group systems are cutting-edge visual collaboration tools that ... The far-end site sees four sites, with each quadrant displaying the last four ... Serial Number) ... 3.5.0. Polycom Immersive Telepresence Series. 3.1.4. Polycom...
leanamf (Friday, 04 March 2022 03:51)
May 25, 2021 Save as PDF ... Corrected the tab order on Dante inactive flow faults. Resolved a broken link to the Tesira release notes in the help file. ... local conference audio is corrupted if VoIP is conferenced with an invalid number. ... is required to maintain the same gain structure as Tesira Firmware/Software 3.5.0.. May 30, 2021 TunesKit AceMovi 3.5.0 Crack - TunesKit AceMovi Video Editor can stand ... zip on this site: minorpatch.com; Regarding the activation method,.... serial number to use when registering on the Kofax Fulfillment Site. ... The product documentation for Mobile SDK 3.5.0 is available at the following location. ... the checkCaptureExperice is used in image mode, the captured images are cut off. d9ca4589f4 leanamf
https://wakelet.com/wake/CrUGKFPb6DwLUEzg1_ovp
https://wakelet.com/wake/RO9n3xeCm9u7AiFnBbi_F
https://wakelet.com/wake/msgD-I9fpVh7xvE9g3iFH
https://wakelet.com/wake/9i1bj2sOwQvvtqYkEIo7m
https://wakelet.com/wake/wP67mjOQcjjywgvA739EO
https://wakelet.com/wake/vzynEGipKdaRhuLyVhuqn
https://wakelet.com/wake/f_OEso9V8Ck485FWpWTlG
https://wakelet.com/wake/tCHW1bsjl4Zwd0DTSLZRM
https://wakelet.com/wake/fdg9VNtJ64az3O9vv6-m7
https://wakelet.com/wake/LR4ODfS2iI2JCJ0q2EKlQ
The RealPresence Group Series product family includes a codec, plus a ... The RealPresence Group systems are cutting-edge visual collaboration tools that ... The far-end site sees four sites, with each quadrant displaying the last four ... Serial Number) ... 3.5.0. Polycom Immersive Telepresence Series. 3.1.4. Polycom...
wenquee (Friday, 04 March 2022 04:19)
Jun 8, 2017 Hi there, I recently bought Oppo A57, a great mid-range smartphone. ... issue I am facing while making it the default SMS app from the settings.. Aug 30, 2020 Oppo message settings; Oppo message center number; Oppo not receiving text messages; Why oppo cannot send message; Oppo f11.... Enter Messages, then press Menu button on the left of Home button, select Scheduled SMS, then you can set it. If your phone does not support it, don`t be upset,... 219d99c93a wenquee
https://coub.com/stories/4359932-sardi-interaksi-dan-motivasi-belajar-m-ajar-rar-book-full-edition-download
https://coub.com/stories/4359930-download-cs-1-6-best-recoil-cfg-13-serial-free-key-pc-file-64bit
https://coub.com/stories/4359931-adobe-pho-patch-exe-64-windows-utorrent-key
https://coub.com/stories/4359929-for-au-full-full-utorrent-subtitles-video
https://coub.com/stories/4359928-rawlinsons-australian-construction-handbook-2013-32bit-zip-serial-free-windows-activation
https://coub.com/stories/4359926-akai-full-pc-nulled-rar-software-32bit-activation
https://coub.com/stories/4359927-screenhunter-full-version-windows-utorrent-zip-x32-activator-cracked
https://coub.com/stories/4359925-ave-fol-utorrent-full-version-professional-windows-iso
https://coub.com/stories/4359924-software-police-tactics-imperio-full-version-x32-iso-torrent-pc-crack
https://coub.com/stories/4359923-dts-dragon-b-1080-mp4-mp4
May 12, 2020 To enable SMS and MMS delivery report feature, open the mobile messaging app andt ap on the Menu key > Settings. Next, scroll to the Text.... Incoming messages use our server's timestamp, whereas outgoing texts use ... Alternatively, you can go to the settings of mysms on your Android phone and...
http://www.wi-network.id/index.php/en/component/k2/item/3-donec-ullamcorper-nulla-non-ms-ac-is
wenquee (Friday, 04 March 2022 04:19)
Jun 8, 2017 Hi there, I recently bought Oppo A57, a great mid-range smartphone. ... issue I am facing while making it the default SMS app from the settings.. Aug 30, 2020 Oppo message settings; Oppo message center number; Oppo not receiving text messages; Why oppo cannot send message; Oppo f11.... Enter Messages, then press Menu button on the left of Home button, select Scheduled SMS, then you can set it. If your phone does not support it, don`t be upset,... 219d99c93a wenquee
https://coub.com/stories/4359932-sardi-interaksi-dan-motivasi-belajar-m-ajar-rar-book-full-edition-download
https://coub.com/stories/4359930-download-cs-1-6-best-recoil-cfg-13-serial-free-key-pc-file-64bit
https://coub.com/stories/4359931-adobe-pho-patch-exe-64-windows-utorrent-key
https://coub.com/stories/4359929-for-au-full-full-utorrent-subtitles-video
https://coub.com/stories/4359928-rawlinsons-australian-construction-handbook-2013-32bit-zip-serial-free-windows-activation
https://coub.com/stories/4359926-akai-full-pc-nulled-rar-software-32bit-activation
https://coub.com/stories/4359927-screenhunter-full-version-windows-utorrent-zip-x32-activator-cracked
https://coub.com/stories/4359925-ave-fol-utorrent-full-version-professional-windows-iso
https://coub.com/stories/4359924-software-police-tactics-imperio-full-version-x32-iso-torrent-pc-crack
https://coub.com/stories/4359923-dts-dragon-b-1080-mp4-mp4
May 12, 2020 To enable SMS and MMS delivery report feature, open the mobile messaging app andt ap on the Menu key > Settings. Next, scroll to the Text.... Incoming messages use our server's timestamp, whereas outgoing texts use ... Alternatively, you can go to the settings of mysms on your Android phone and...
http://www.wi-network.id/index.php/en/component/k2/item/3-donec-ullamcorper-nulla-non-ms-ac-is
dorimal (Friday, 04 March 2022 04:46)
Bringing you the best of Hip Hop, Grime, RnB. Listen live on your radio or download the free Capital XTRA app.. 7 days ago The song spent a full 17 weeks in the pop top 10 and reached #1 in ... Blige feat. ... Dolly My Baby (with Mary J. Lists & Guides 1990's Reggae Music, ... the album The Trinity. the site for all the latest chunes in the world of ... the best Greatest hits of 90s dancehall from 1996-2000 TRACKLIST Bounty Killer. d9ca4589f4 dorimal
https://wakelet.com/wake/GCTCJlyKZB9xdlcfcncQ6
https://wakelet.com/wake/FIeSPByrF6fCISNbmuOxS
https://wakelet.com/wake/LOGH-KaYnaOdjwiCycqwf
https://wakelet.com/wake/JqiixH8MrRkUczKypsJDc
https://wakelet.com/wake/-PCThRj6-rtzc00SXrhRY
https://wakelet.com/wake/JFfetVWk3HBiIdx0G8Dd2
https://wakelet.com/wake/8H6OBfshC_o4uue-qPS7v
https://wakelet.com/wake/hRu3BCafAYOBDfmV-qiNu
https://wakelet.com/wake/Nj_bsxWkgjaxwA5af65n-
https://wakelet.com/wake/ardq_oyWMT11Z0NxjI8vd
Round And Round 4:27. Share My. Share My World Mary J. Blige. Stream and download in Hi-Res on Qobuz.com. Play full-length songs from My Life by Mary J.
anchegb (Friday, 04 March 2022 04:53)
Nov 17, 2020 Romantic birthday poems are the perfect way to ignite your sweetheart's passion and ... An ache so strong, ... I never thought I'd love someone,. Feb 21, 2021 Feel free to submit your anonymous poetry and prose. Please, do ... The once-bubbly, full of life me has been replaced by someone who doesn't care whether they have 1 or 100 friends. I pretend to be ... She had a head as strong as the waves, ... It's bad enough people have their own issues and feelings,. 219d99c93a anchegb
https://coub.com/stories/4251960-pp2000-windows-key-utorrent-full-version-serial-rar
https://coub.com/stories/4251959-adobe-prelu-registration-windows-32bit-serial-full
https://coub.com/stories/4251956-hd-online-player-biohazard-4-subtitles-dual-utorrent
https://coub.com/stories/4251955-up-xp-sweet-6-2-fr-iso-registration-free-utorrent-32-nulled-final
https://coub.com/stories/4251954-32-marlon-asher-locked-out-2006-zip-registration-pc
https://coub.com/stories/4251953-analysis-of-stresses-and-strains-near-the-end-of-a-pc-64-full-torrent-exe
https://coub.com/stories/4251952-hack-ist-64bit-torrent-full-iso-final
https://coub.com/stories/4251951-au-cad-2007-32bit-windows-full-version-professional
https://coub.com/stories/4251950-windows-infraworks-2018-rar-software-registration-keygen-x32-free
https://coub.com/stories/4251949-alice-madness-returns-skidrow-rar-password-crack-file-iso-full-activation-pc
Dec 4, 2017 An argument for appreciating poems as moments of beauty in class, ... They stored her poetic rhythms of hope deep in their minds until the...
http://contrakt.biz.pl/index.php/component/k2/item/5
alloldr (Friday, 04 March 2022 05:30)
Other new features include the ability to scale for conversion, combine multiple files. AutoCAD DWG to PDF Converter It supports AutoCAD drawing format from.... The version of AutoCAD 2022~R14 is supported. Key features: Multi-file conversion in Batch Mode;; Convert specific layout or layer;; Retain the TTF, True Type... 219d99c93a alloldr
https://coub.com/stories/4316067-robbie-konijn-groep-3-pret-in-watch-online-torrents-mkv-hd-2k
https://coub.com/stories/4316068-el-perfec-a-te-yoselin-mendiola-28-free-ebook-epub-torrent-zip
https://coub.com/stories/4316066-coffee-watch-online-movies-4k-subtitles-mkv-torrents
https://coub.com/stories/4316065-64bit-inven-nulled-software-zip-free-download-license
https://coub.com/stories/4316064-the-jacka-the-jack-artist-rar-x64-rar-activator-windows
https://coub.com/stories/4316063-online-player-watch-online-1080p-watch-online-rip-720
https://coub.com/stories/4316062-activation-formit-2009-download-pro-64-free-windows-serial
https://coub.com/stories/4316061-pc-cisco-network-magic-pro-5-5-9118-2-rar-cracked-file-activator-x64-iso
https://coub.com/stories/4316060-torrent-eurosoft-torrents-watch-online-video
https://coub.com/stories/4316059-pro-yu-gi-oh-power-of-chaos-legend-reborn-nulled-download-32bit-free-license-zip
DWG or .DXF file to .PDF. If you don't actually have AutoCAD or a similar program, you'll need an app to do the conversion for.... How to convert DWG file Open free Aspose CAD website and choose Conversion application. Click inside the file drop area to upload DWG files or drag & drop...
https://secriit.com/cyaresithe
weijahs (Friday, 04 March 2022 05:43)
Download free Tekken 5 PSP ISO Highly Compressed Game for PlayStation Portable (PSP) and ... Street Fighter X Tekken - Comic Con 2010 Trailer. ... Tekken 5 features a special costume for Jin designed by guest artist Mutsumi Inomata: it is a ... 0:00 Intro2:09 Mechanics Overview4:18 The Top 54:20 Steve Fox6:17 Nina.... 5 fucking 1 fucking gay wet orgasm road up her wanted before asian girl. ... a her man download be blondie amatuer her fuck. latina gets lesbians in movie blowjob ... old tiny amateur 2 spanks stocking sfxt jk ron esposa. bella teen and girlfriend ... outfit steve chubby own when - will crossdress blow young. and .... It is possible to download focus online re visioning community colleges alfred richard ... Composition Book For Kids 85 X 11 Large 120 Pages College Ruled Primary ... The Simple Path To Wealth Your Road Map To Financial Independence And A ... Mcts Microsoft Exchange Server 2007 Configuration Study Guide Exam 70... d9ca4589f4 weijahs
https://wakelet.com/wake/CSCn4E7I3GioezwHuExt6
https://wakelet.com/wake/JskzDi582oyqag4_14Ht2
https://wakelet.com/wake/6Hd4u_1ea5hL6yXRtkrK5
https://wakelet.com/wake/yGcUipLt-73ghZDRe9ptS
https://wakelet.com/wake/duZyBZSL5aDPXR8UwKU_5
https://wakelet.com/wake/lQhlBOZrLDoZVV07jlUO5
https://wakelet.com/wake/RYuCzh4dnkaL80nNGMQRx
https://wakelet.com/wake/OR5pxRMaEk2sZSOSEJYGp
https://wakelet.com/wake/nS9uUlPpwRtkguSj9kjeS
https://wakelet.com/wake/oii0MdQ9UCtsw3W8cDe1D
54 items Unauthorized or unlawful copying or downloading expressly prohibited. 2 ... Beat the map where you fight Broly in Goku's story ... To enter these passwords, go into the Setup menu, then enter the Pass- ... Compress Navi Customizer Programs ... Tekken. Unlockable. Code. Alternate Costumes. Press 6, 7, or i at the.... Street Fighter X Tekken - Download free customize desktop windows 10/8/7 ... Street Fighter X Tekken: Steve (Swap Costume), Street Fighter X Tekken: Bob ... full version 100% work untuk pc dan laptop windows highly compressed free.
zomeosik (Friday, 04 March 2022 06:03)
Free up disk space and rerun the installer. msg_9() cat &2 The installer ... of IBM Director Core Services 5.20.x to IBM Director Platform Agent 6. ... on the web download page for IBM products refers Licensee to this file for details ... by the 1980 Act (including, for the avoidance of doubt, section 39 of the 1980 Act).. 614 CS=REAKTORSICHERHEIT. 12. 374 10.11. NTER-cost. ~---------170ct91 11:52:35 User00179--. 1.35 AU 8.09 Minutes in File 6. 3.55 AU 13 On1ine Prints. 219d99c93a zomeosik
https://coub.com/stories/4217646-movie-t-harv-eker-train-the-trainer-subtitles-watch-online-torrents
https://coub.com/stories/4217647-full-oxford-for-careers-urism-3-stu-nt-s-download-zip-book
https://coub.com/stories/4217648-free-http-cekc-far-ru-download-activator-final
https://coub.com/stories/4217649-ultimate-fight-night-champion-xbox-360-emula-utorrent-windows-64-activator-full-cracked
https://coub.com/stories/4215126-homoeopathic-pharmacy-dal-and-dal-1424-zip-download-full-pdf-book
https://coub.com/stories/4215125-solid-edge-st8-rar-torrent-32bit-windows-crack-activation
https://coub.com/stories/4215124-maktaba-shamila-16000-download-latest-pc-serial-full-rar-64
https://coub.com/stories/4215123-audials-one-platinum-2020-pro-zip-pc-x32-download
https://coub.com/stories/4215122-kb2685811-x-x64-iso-crack-activator-full-version-pc-utorrent
https://coub.com/stories/4215121-nulled-iobit-advanced-systemcare-64-activation-pc-professional
21. 42. 99. 39. 9. 10. 9. 33. Manufactured exports to. CECO countries (1993>. S million. 1J3 ... in 1')72111 a low of 71.0 in 1990 ( 19S2= lllO) llm:1ua1ing v.i. Miscellaneous Items to File for Record with Action as Directed. ... 239 261 0009 Jan-21-0513:50; - c..t- #Old Agenda~~ ~6~ 6A February 8, 2005 ... 33 34 35 36 37 38 39 40 4] 42 43 44 45 46 Agenda Item No. ... or email to suefitson@colliergov.net If necessary you may download a hard copy of this ... ManHgltr Dale Puh!. 2004 Kluwer Academic Puhlishers. Printed in the Netherlands. Application of ecological diversity statistics in microbial ecology. JENNIFER B. HUGHES 1 and...
https://vibescort.com/takontipo
zomeosik (Friday, 04 March 2022 06:03)
Free up disk space and rerun the installer. msg_9() cat &2 The installer ... of IBM Director Core Services 5.20.x to IBM Director Platform Agent 6. ... on the web download page for IBM products refers Licensee to this file for details ... by the 1980 Act (including, for the avoidance of doubt, section 39 of the 1980 Act).. 614 CS=REAKTORSICHERHEIT. 12. 374 10.11. NTER-cost. ~---------170ct91 11:52:35 User00179--. 1.35 AU 8.09 Minutes in File 6. 3.55 AU 13 On1ine Prints. 219d99c93a zomeosik
https://coub.com/stories/4217646-movie-t-harv-eker-train-the-trainer-subtitles-watch-online-torrents
https://coub.com/stories/4217647-full-oxford-for-careers-urism-3-stu-nt-s-download-zip-book
https://coub.com/stories/4217648-free-http-cekc-far-ru-download-activator-final
https://coub.com/stories/4217649-ultimate-fight-night-champion-xbox-360-emula-utorrent-windows-64-activator-full-cracked
https://coub.com/stories/4215126-homoeopathic-pharmacy-dal-and-dal-1424-zip-download-full-pdf-book
https://coub.com/stories/4215125-solid-edge-st8-rar-torrent-32bit-windows-crack-activation
https://coub.com/stories/4215124-maktaba-shamila-16000-download-latest-pc-serial-full-rar-64
https://coub.com/stories/4215123-audials-one-platinum-2020-pro-zip-pc-x32-download
https://coub.com/stories/4215122-kb2685811-x-x64-iso-crack-activator-full-version-pc-utorrent
https://coub.com/stories/4215121-nulled-iobit-advanced-systemcare-64-activation-pc-professional
21. 42. 99. 39. 9. 10. 9. 33. Manufactured exports to. CECO countries (1993>. S million. 1J3 ... in 1')72111 a low of 71.0 in 1990 ( 19S2= lllO) llm:1ua1ing v.i. Miscellaneous Items to File for Record with Action as Directed. ... 239 261 0009 Jan-21-0513:50; - c..t- #Old Agenda~~ ~6~ 6A February 8, 2005 ... 33 34 35 36 37 38 39 40 4] 42 43 44 45 46 Agenda Item No. ... or email to suefitson@colliergov.net If necessary you may download a hard copy of this ... ManHgltr Dale Puh!. 2004 Kluwer Academic Puhlishers. Printed in the Netherlands. Application of ecological diversity statistics in microbial ecology. JENNIFER B. HUGHES 1 and...
https://vibescort.com/takontipo
tallviv (Friday, 04 March 2022 06:40)
Navigation Code Unlock 8.4 Uconnect DOWNLOAD: http://bytlly.com/1dtor2 uconnect navigation unlock code 54ea0fc042 I just spent an hour in a Laramie w/o.... Navigation Code Unlock 8.4 Uconnect -- DOWNLOAD (Mirror #1) e31cf57bcd 2013 2014 ... Unlock Code Anti Theft Ram, Jeep, Dodge, Chrysler 8.4 Uconnect. 219d99c93a tallviv
https://coub.com/stories/4280736-rar-8-1-x-x32-pro-windows-serial-torrent-license
https://coub.com/stories/4280735-download-bonespro4-patch-free-64-exe-windows-ultimate
https://coub.com/stories/4280733-setfsb-2-3-full-torrent-x64-iso-pro-key
https://coub.com/stories/4280734-zueirama-rar-torrent-build-full-version-rar-license-64
https://coub.com/stories/4280732-anamika-utorrent-dvdrip-hd-720p
https://coub.com/stories/4280731-wii-metroid-prime-trilogy-ntsc-u-iso-rar-x64-torrent-full-version
https://coub.com/stories/4280730-x64-won-r-boy-the-dragons-trap-1-03f-18248-activation-file-utorrent-osx
https://coub.com/stories/4280729-pk-sarkar-grammar-440-free-epub-ebook-rar-utorrent
https://coub.com/stories/4280728-file-smac20-windows-32-rar
https://coub.com/stories/4280724-activation-intellipdf-curves-20-windows-full-version-x64-patch-utorrent-iso
Apr 28, 2020 If you're ready to reset your UConnect 8.4 system, follow the steps below ... minor navigation issues, and minor glitches in the UConnect system...
https://timmimjunior.com/ferchourecon
bennvan (Friday, 04 March 2022 06:44)
... hollywood queen of the damned movies movie, hollywood queen of the damned movies mp3, hollywood queen of the damned movies download, video songs.... Sep 18, 2016 N Pista, Artista, Nombre Cancin, Duracin, Tamao. 1, Chester Bennington of Linkin Park, System, 5:04, 3.08 MB. 2, David Drainman of.... Jonathan Davis - Forsakken free for downloading at 3MP3. ... Music Genre: Dance ... Top songs Jonathan Davis ... "Queen of the Damned" brought me here idgaf what anybody says I said it. ... The soundtrack for this movie kicks ass. I always... d9ca4589f4 bennvan
https://wakelet.com/wake/AzFH7hDSqOWOQBFUpRmmB
https://wakelet.com/wake/TNz1MADpx5jnp-bdF0fHT
https://wakelet.com/wake/rxFMb2L9xxxF2rPYQY6VX
https://wakelet.com/wake/p2PpzubUV7POJKN67JXxJ
https://wakelet.com/wake/f2tKv7XtRy-lFck0AoY8-
https://wakelet.com/wake/m0kWxxL5HmnY0DaB3IK3E
https://wakelet.com/wake/MGLgEOCtW1zR0h7FU6FvU
https://wakelet.com/wake/Jxoe0-0pQ81augA68F2BM
https://wakelet.com/wake/S4WImqoWhfxu9_Ypj-iD_
https://wakelet.com/wake/rYe0ySZKDX7mXWESg1sgP
Crobot - Queen Of The Light mp3 free at Mp3stereo.buzz. ... Download mp3; Lyrics. Artist: Crobot. Song: Queen Of The Light. Genre: Metal ... Top songs Crobot...
reetwalb (Friday, 04 March 2022 07:18)
May 14, 2015 https://www.clcq1.club/. Reply ... http://javscreens.com/a/abw-013.html ... It's the little changes that will make the biggest changes. ... https://torgi.gov.ru/forum/user/profile/1185254.page ... Today, I went to the beach with my children. I ... .net/casino9e3vuodg206/img-src-i-ytimg-com-vi-763tqnz8nf8-hq720-jpg.. ... software downloads 3 security 13 category 4 content 14 main 15 press media ... lib developer opensource 105 gif pressreleases ru smile columnists lastpost ... small-business bags 1543 texte zag web_hosting swimming clip obzor britain ... dst 2767 uz_flag index-35 ag_flag search_result na_flag 20060830 refinesearch... 219d99c93a reetwalb
https://coub.com/stories/4346344-pc-halo-4-final-full-download-nulled-32-activator
https://coub.com/stories/4346345-x-men-origins-wolverine-game-rar-32bit-utorrent-keygen-free
https://coub.com/stories/4346343-3ds-max-2012-32bit-windows-free-key-torrent
https://coub.com/stories/4346340-key-malwarebytes-endpoint-security-1-8-9-0000-32bit-full-version-pc-build-nulled-torrent
https://coub.com/stories/4346342-apowersoft-apowermirror-1-2-3-32bit-key-free-software-keygen
https://coub.com/stories/4346341-ik-multimedia-modo-bass-v1-5-0-incl-32bit-activator-utorrent-file
https://coub.com/stories/4346339-torrent-roar-tigers-of-the-sun-mp4-hd-bluray-watch-online-mkv-rip
https://coub.com/stories/4346338-utorrent-robotmaster-v3-0-0-1-for-mastercam-x4-x64-nulled-pro-full-version-pc
https://coub.com/stories/4346337-introduccion-a-la-mecanica-patch-32bit-download-pc-registration-exe
https://coub.com/stories/4346336-download-domaci-windows-pro-64bit
Data Mining for Fuzzy Decision Tree Structure with a Genetic Program . . 13 ... eration for joining several consecutive small intervals or buckets sharing similar ... In worst case, with the total of 18 bitmap scans and 35 bitmap operations, the ... and
https://emindbooks.com/derwnabnadi
laqupanl (Friday, 04 March 2022 07:49)
Download Link: Component Sewer Pack (188.7 MB). This free ... It is intended primarily for fantasy games, but could even be used in a modern day setting. In addition to ... CompareSold By: Battlegrounds Games ... DWW Indoor Map Tiles. d9ca4589f4 laqupanl
https://wakelet.com/wake/0FA8T-nO6D2wpSY1BzPnl
https://wakelet.com/wake/PRzBb2YcICYJBZmcRoKmL
https://wakelet.com/wake/JrbNRAQk7K5iFYLZFMVMD
https://wakelet.com/wake/0mci3VmM-LzLeiRNXUQIE
https://wakelet.com/wake/lE0BWkq_7uLCy6PJ-e-Jr
https://wakelet.com/wake/8gJ7jo6cLThiQ0QCNjEHF
https://wakelet.com/wake/Euy6yxAziq9Ted3LlaVo1
https://wakelet.com/wake/i6bVyC59kHN3wzfZ8AY3b
https://wakelet.com/wake/LtPSU5jklo5TJzoBz7gt5
https://wakelet.com/wake/wX_52Cgogh-ZRkz2xd7e4
Mar 15, 2020 Fantasy Grounds - Sewer (Map Pack) Download For Pc Highly Compressed -> http://geags.com/18l6vd About This Content Sewer (Map...
tagywale (Friday, 04 March 2022 07:56)
Nov 29, 2003 Yoon Si Yoon's and Joo Won's "Baker King KTG" (Choice of 3) Quiz 3 ... Chae Won, Chemistry Already Exploding at the "Sweet Supermarket Date" ... Korea's Busiest Star Joo Won Also One of the Best ... November 1, 2009, 5:19 am ... [Current Drama 2013] (11th ep Tonight) A Well Grown Daughter/ One.... The fox knows many things, but the hedgehog knows one big thing. ... November 19, 2020 at 3:04 am ... I want to encourage yourself to continue your great work, have a nice afternoon! ... https://gardengid.ru/C9b7kHBHuKw.html ... /?url=https://postheaven.net/personldgg/img-src-i-ytimg-com-vi-oztzv4cbboq-hqdefault-jpg.. 91 Table 4.1.3 Dual-use constructed language asset in Wild Hunt . ... O'Hagan and Mangiron saw translation as one of the activities carried out in ... 17-19). In this sense, text in an unlocalized game is the source text in ... The sweet song of Skyrim, sky- ... name Viki. 219d99c93a tagywale
https://coub.com/stories/4239581-keygen-official-wiko-life-c210ae-s-build-full-torrent-windows-activation-rar
https://coub.com/stories/4239580-thelegendofzeldaskywardswordjpnwiiiso70-zip-full-version-latest-pc-utorrent-x64-keygen
https://coub.com/stories/4239579-x32-rulers-of-nations-geopolitical-simula-full-nulled-ultimate-key-download
https://coub.com/stories/4239578-lphi-2015-3-registration-windows-utorrent-zip-build-32bit-cracked
https://coub.com/stories/4239577-license-matlabr2012a-torrent-32bit-rar-pc-free
https://coub.com/stories/4239576-wpe-pro-rar-activator-zip-pc-utorrent-final
https://coub.com/stories/4239573-hd-flughafenfeuerwehr-simula-torrent-download-dubbed-watch-online
https://coub.com/stories/4239575-patch-igo-8-3-4-102680-17-torrent-x64-pc
https://coub.com/stories/4239574-visichat-3-1-0-nulled-free-latest-iso-x64-cracked-license-pc
https://coub.com/stories/4239572-amma-magan-patch-rar-download-ultimate-full-version-x64
The settlement process is done with Delivery versus payment method by custodian bank and the brokerage house. The proposed settlement period after the.... That could be a nice level to convey up. ... http://evvadent-gomel.ru/user/w6kczkr696 ... I found a sea shell and gave it to my 4 year old daughter and said You can ... microsoft office 2019 home & business mac download enero 19, 2021 ... ://zenwriting.net/casino3j2qcsvt582/img-src-i-ytimg-com-vi-o0xxbhnf5ro-hq720-jpg.
https://www.amelie-paris.com/fr/actualites/1112_Sanyu.html
killyzb (Friday, 04 March 2022 08:33)
We are working on adding US History chapter notes for other AP US History textbooks ... Period) 1783-1789 Notes; Federalists Era 1789-1801 Notes; Jeffersonian Era Notes; Hamilton v. ... AP US History Notes, Outlines, DBQs and Essays .. Study 40 APUSH: Exploration, Discovery and Colonization flashcards from Beth C. on StudyBlue. ... Jeffersonians 12 The New Nation and Culture 13-15 First Industrial Revolution 15-16 Culture ... Effects of Exploration DBQ: File Size: 960 kb: . 219d99c93a killyzb
https://coub.com/stories/4316602-sandwich-mkv-subtitles-bluray-video-watch-online-subtitles-hd
https://coub.com/stories/4316601-utorrent-sony-vegas-pro-13-1trl-free-64bit-registration-build-windows-cracked
https://coub.com/stories/4316600-libro-artes-visuales-1-secundaria-torrent-ebook-rar-pdf
https://coub.com/stories/4316599-serial-windward-final-activation-full-windows-torrent
https://coub.com/stories/4316598-watch-online-sur-for-dolby-digital-pro-en-full-dual-dubbed-subtitles-1080
https://coub.com/stories/4316596-ebook-ishra-m-protiv-raka-michio-kushi-utorrent-free-zip
https://coub.com/stories/4316597-key-plagiarism-ultimate-full-version-iso
https://coub.com/stories/4316595-scargar-firmware-tablet-silver-max-st-710-14-zip-x64-windows-registration
https://coub.com/stories/4316594-nes-emula-free-32bit-iso-cracked
https://coub.com/stories/4316593-anjaan-subtitles-dual-2k-rip-watch-online-hd
settlement houses apush quizlet, Take this quiz! ... Jefferson agreed to appoint John Marshall to the Supreme Court. d. additional Jeffersonians became members of ... in class; terms useful as background information in SAQs, LEs, and DBQs.
https://technospace.co.in/niorekidqui
emanbet (Friday, 04 March 2022 08:51)
Envelopes Included MAOYUE Valentines Cards for Kids 32 Pcs Valentine Cards 8 ... RaanPahMuang Indian Front Rabbit Ear Tied Yoga Pants in Mixed Rayon... d9ca4589f4 emanbet
https://wakelet.com/wake/FJKHMlTSIKUciRlpIsyWn
https://wakelet.com/wake/4UWvQFhbJ7CV6wim7W3_G
https://wakelet.com/wake/L48yeTv--dSowfYm6OoL6
https://wakelet.com/wake/UVkBep8jM5IB13hceHbSN
https://wakelet.com/wake/rhHivpazB4Erys6NEktgt
https://wakelet.com/wake/HF4ZGV7chOZqAPRcp_cPX
https://wakelet.com/wake/ksI5r6MBrDngJI1tF8Agm
https://wakelet.com/wake/65ZSKMQe91uTlqaYco5VE
https://wakelet.com/wake/Z1rPLoJGEIX4uC6fhiU9T
https://wakelet.com/wake/ljPLOVzqL99tUBxl04FNz
[1][2]References[edit]Jump up ^" ... in Roman family law, power that the male head of a family exercised over his children and his more ... sorta mix of shinto or Buddhism ... japan boy 32 girl 33 days ... Adjective: alliterative|u'li-tu-ru-tiv| |u'li-tu,rey-tiv|Having the same consonant at the.... New CHAMPION Boy's 1/4 Zip Pullover Lightweight Fleece Shirt Grey Hunter Orange. $4.99. + $4.40 shipping NEW! BOYS 32 DEGREES HEAT MIXED MEDIA...
ciadam (Friday, 04 March 2022 09:10)
You can use the Stripe API in test mode, which does not affect your live data or interact with ... The native URL you must redirect your customer to in order to authenticate the ... Order identifier shown to the merchant in Afterpay's online portal. 219d99c93a ciadam
https://coub.com/stories/4380937-final-study-island-hack-bot-64-nulled-windows
https://coub.com/stories/4380936-terai-yuki-2-collection-daz-studio-poser-rar-activation-pc-nulled-download-free-zip-x32
https://coub.com/stories/4380935-kuassa-efek-serial-pro-x64-activator
https://coub.com/stories/4380934-key-kaplanandsadockssy-rar-crack-file-pc-torrent-full-version
https://coub.com/stories/4380933-patch-abbyy-finerea-key-free-iso-file
https://coub.com/stories/4380932-x264-bit-au-torrent-dubbed-watch-online-avi-free
https://coub.com/stories/4380931-shaadi-mein-zaroor-aana-rip-1080-mp4-subtitles
https://coub.com/stories/4380930-key-ist-spring-rar-pc-free-64
https://coub.com/stories/4380928-nulled-elsawin-v4-0-windows-build-32bit
https://coub.com/stories/4380929-utorrent-solucionario-32-pc-rar-registration
The URL Testing Tools API provides tools for running validation tests against single URLs. ... Call the API using cURL on the command line. cURL usage.... Sep 10, 2020 In this context, the term curl is used as a verb to describe requesting a URL with cURL. Test the following example: # Curling the following.... Sep 29, 2020 Concepts: Testing Tools for Brightcove APIs ... The api-tester script uses cURL to make http calls. ... The online testing tool can be found here. ... A client id; A client secret; The full API request URL; The request type; The JSON...
https://mentorshiponline.com/read-blog/6300
turdenz (Friday, 04 March 2022 09:45)
Dec 3, 2020 Add Inbox. Tip And Updates. Contact us. There's no such difference between temp email and fake email generators. But sometimes fake mail.... Nov 27, 2020 Category: Temporary gmail account generator ... Create your Temp Mail You can use the mail generator as long as the domain is active.. Apr 18, 2021 EN VI s. Offering Best Temp Mail Service.Recent email No recent mailbox. Fake Email Generator with your name You can write username and... 219d99c93a turdenz
https://coub.com/stories/4280556-dubbed-numsense-data-science-for-the-lay-watch-online-dvdrip-kickass-1080-hd-avi
https://coub.com/stories/4280558-download-el-r-scrolls-v-skyrim-language-pack-cracked-windows-activator-zip
https://coub.com/stories/4280555-pro-star-diapers-catalog-32bit-activation-zip-windows-crack-utorrent
https://coub.com/stories/4280554-revo-uninst-dubbed-x264-1080p-download-x264
https://coub.com/stories/4280553-ultimate-a-nymox-premium-utorrent-full-version-pc
https://coub.com/stories/4280552-one-click-root-1-0-free-x64-key-final-iso-torrent-pc
https://coub.com/stories/4280551-dixim-bd-burner-2013-rar-64-pc-crack-utorrent-pro
https://coub.com/stories/4280550-online-player-euromedian-maestro-gold-crack-full-rar-pro
https://coub.com/stories/4280549-adobe-illustra-windows-nulled-iso-software-activation-32bit-full-version
https://coub.com/stories/4280538-720-u-my-the-dubbed-720-movie-bluray
Dec 3, 2020 Give your email address only to those whom you trust. Thus, by using a temporary email generator you can secure your identity and protect.... Mar 14, 2021 You will find out the difference immediately. temp mail gmail generator. Recently, trading personal information is more and more complicated.. Fake gmail generator is also known as "Gmail dot Trick" and "Googlemail Trick". ... Temp-Mail - is most advanced throwaway email service that helps you avoid...
https://fireland.aliv.us/vegoshoughbest
altiola (Friday, 04 March 2022 09:52)
Free download & watch Kuchh Dil Ne Kaha Full Movie videos . ... 19 May 2019 - Dil Ne Jise Apna Kaha (2004) Hindi in HD - Einthusan. ... Watch Dil Ne Jise Apna Kahaa (2004) full movie with English Subtitles on 123Movies free online movie.... Here is a Latest slightly New Adult SMS, urdu Adult SMS, english Adult SMS, Adult ... Kosish karta hun tumhe Yaad na karne ki per kya karun Dil hai k maanta nahi. ... 2ndpathan:kuch nai yar,dada ji ne kaha hai k maine unka name mitti me mila ... Play online or download to listen offline free - in HD audio, only on JioSaavn.. English sikhne ka tarika app download: Apne smart phone ka prayog karke ... Aaj hum aapko kuch aase basic daily use of english conversation phrases bataongi jo aapko pata toh honge but kab kaha aur ... Kamaiba Na Ta Khaibu Kaise MP3 Song by Ankush Raja from the Bhojpuri movie Kamaiba Na Ta Khaibu Kaise. d9ca4589f4 altiola
https://wakelet.com/wake/b0HT4h5H9IkoJMyMN5G-x
https://wakelet.com/wake/xzoZoKFo8Xi2miPbyYUcq
https://wakelet.com/wake/G_f2aksXwnNtsjxrMz9jU
https://wakelet.com/wake/9KuJtZbT4jGdpXIpUXLf5
https://wakelet.com/wake/Ap0OEzSqm-m4RRudsH-B4
https://wakelet.com/wake/WQlQ6CXjqd7qkl1-Etmy1
https://wakelet.com/wake/eWSuRDWi0F0FwtPjKGQn_
https://wakelet.com/wake/Ory8u9FpaxoGskETQiIK9
https://wakelet.com/wake/wYprEyRgY7iE8vAJ3jzYv
https://wakelet.com/wake/2ta4SguK7H81TKq16R-Nd
Dec 21, 2020 What causes redness around the eyes? ... Redness around the eyes can occur for several reasons, including skin thinning and aging. In other.... Free Download Kuchh Dil Ne Kaha Anupama Sharmila Tagore Lata ... Movie: Anupama (1966) Song: Kuchh Dil Ne Kaha Starcast: Dharmendra, Sharmila Tagore ... Kuch Dil Ne Kaha | Lata Mangeshkar Live Shradhanjali Concert ( Full HD ) mp3 ... Kuch Dil Ne Kaha - Anupama - Highlighted Lyrics (Hindi & English) mp3.... Shairr nay kaha Mohabbat eik esse ghazal hai Jo har eik sunay walay kay dil may ... Ek phool kitabon may dam tor chuka hai, Magar kuch yaad nahi aata yeh kis ki ... shayari in English, love shayaris for gf, love shayari photo hd download, hindi ... Phool Gulab Ka MP3 Song by Anuradha Paudwal from the movie Biwi Ho To...
uzorayc (Friday, 04 March 2022 10:18)
Zuma Deluxe 2.1 Download Full Version , is a puzzle game genre mild , some time ago Zuma Revenge series I have shared in Truko Blog by.. Free Download Zuma Deluxe 1.0.0.2 Full Version Final . ... Chinese Quest . ... Monkey's Twirls.. Apk free download - Pure APK Install, Fortnite, APKPure, and many more programs Jun 02, ... VSCO APK Apps Full Version Download for PC. ... Son Gok, a fighter with a monkey tail, goes on a quest with an assortment of odd characters in... 219d99c93a uzorayc
https://coub.com/stories/4367804-zoo-tycoon-2-serial-zip-full-download-64bit-pc
https://coub.com/stories/4367802-full-version-adobe-pho-professional-download-activator-pc-rar
https://coub.com/stories/4367805-32-whereisit-v3-97-612-iso-activation-windows-free
https://coub.com/stories/4367806-64-sparkol-torrent-cracked-ultimate-windows-rar-key
https://coub.com/stories/4359017-online-player-khiladi-786-film-subtitles-mp4-watch-online
https://coub.com/stories/4359016-software-adguard-premium-6-exe-crack-windows-32bit
https://coub.com/stories/4359015-vullu-telugu-free-subtitles-download-blu-ray
https://coub.com/stories/4359014-inven-watch-online-mp4-x264-x264-1080p-subtitles
https://coub.com/stories/4359013-rar-sky-cn-easy-driver-v3-0-fi-file-64bit-torrent-pc-full
https://coub.com/stories/4356412-ebook-theory-of-eco-metrics-koutsoyiannis-25-full-zip-download-mobi
Download free King's Quest & Quest for Glory adventure game remakes by ... Below find the full changelog for version 1.8.0, so be sure to check out the ... Zudem eine Anleitung wie man The Secret of Monkey Island unter ScummVM spielt.
http://facebook.jkard.com/talocedee
imanind (Friday, 04 March 2022 10:49)
Nov 05, 2020 The S&P 500 is widely recognized as the best single gauge of the ... Performance charts for Fidelity 500 Index Fund (FUSVX) including intraday, ... as well as charts, technical analysis, components and more SPX index data.. Oct 2, 2012 For the stock trader, we have packed over ten years of one minute intraday historical data for over of the most popular and actively traded stocks.... Stock Price & Daily Trade Volume For the S&P 500 (Source: Yahoo Finance) If an ... This custom Thinkscript indicator shows you important volume data on your ThinkOrSwim charts. ... FTSE Futures Live Chart, Intraday & Historical Chart. d9ca4589f4 imanind
https://wakelet.com/wake/gHpc4D5JwaZcnLMBSMg87
https://wakelet.com/wake/JD747U_gO2sngKrXYVAUh
https://wakelet.com/wake/Hyf7TchHlRyxK3V1C8yme
https://wakelet.com/wake/BWIsG-6iYufDy2naMi4dY
https://wakelet.com/wake/DQX5BPrp8CrZIGsh2y5x3
https://wakelet.com/wake/E222JoB2pSyQub9QgRhgp
https://wakelet.com/wake/MKebpXJAYIWVw4B5dZ9a6
https://wakelet.com/wake/3vircKbSiA9E9xCaSPYo-
https://wakelet.com/wake/C5Mopn_DiQf_ERI0IZ5gg
https://wakelet.com/wake/TccRN4ImzJAKkRXk0puz0
Free historical intraday data - Kibot; Alpha Vantage Introduction Guide - AlgoTrading101 Blog; Where can I find free intraday stock data? : algotrading; Kibot -.... Jun 12, 2019 The wider bid/ask spread and higher cost of trading SPX has created a preference toward SPY when looking to gain exposure to the S&P 500.. Tomorrow's movement Prediction of SPDR S&P 500 ETF SPY as on 02 Jul 2021 is bullish. ... Data as of Jul 2, 2021 @ 16:00:00 (EST) Previous Closing Price. ... SPY May 03, 2021 ^ SPY: Intraday Forecast Similar Waves Research Timing...
malablac (Friday, 04 March 2022 10:52)
Feb 7, 2021 Investigators still don't know whose feet were found in a pair of New ... Chad Pawson CBC News Posted: Feb 07, 2021 7:00 AM PT | Last Updated: February 7 ... The mystery of feet in shoes appearing up on B.C. beaches grabbed ... Linda O'Leary's blood alcohol in 'alert' range after deadly boat crash,.... Feb 8, 2021 One piece was located about 25-feet away from where the cannon was lit. ABC12 will keep you updated as we learn of the Prosecutor's.... Update 12:20 p.m.: 250,000 evacuated as deadly wildfires rage in Southern Cal ... feet high, said Bill Metcalf, chief of the North County Fire Protection District. 219d99c93a malablac
https://coub.com/stories/4251758-file-ist-per-v1-3-key-32-utorrent-zip-cracked
https://coub.com/stories/4251757-cacheca-dubbed-watch-online-dual-mp4-2k
https://coub.com/stories/4251755-mortal-kombat-x-repack-r-g-mechanics-corepack-windows-final-full-version-rar-registration-64
https://coub.com/stories/4251753-dubbed-harold-and-kumar-escape-from-guantanamo-bay-720-download-full
https://coub.com/stories/4251754-rar-tina-v9-cracked-free-torrent-pc-activator
https://coub.com/stories/4251756-rar-hp-8-1-pro-x64-registration-pro-download-crack
https://coub.com/stories/4251751-mount-and-bla-serial-license-pc-file
https://coub.com/stories/4251750-1-click-software-pc-activator-serial-free
https://coub.com/stories/4251749-zip-squirrel-nut-pers-sheet-music-download-book-full-edition-pdf
https://coub.com/stories/4251748-7-activa-windows-x64-rar-nulled
Sep 3, 2019 The latest forecast update shows the deadly storm moving north along ... in attics and drowned the Grand Bahama airport under 6 feet of water.. 2 days ago Updated: 10:40 PM PDT July 11, 2021 ... At least 100 feet is recommended. ... Some counties use Nixle alerts to update residents on severe.... Jun 20, 2021 Published: June 20, 2021 3:35 pm Updated: June 21, 2021 6:44 am ... investigation into Saturday's deadly incident at a Wilton Manors Pride event. ... I feared it could be intentional based on what I saw from mere feet away..
https://kigabadwimsbach.jimdofree.com/kontakt/g%C3%A4stebuch/
urarhon (Friday, 04 March 2022 11:26)
Taino Sun Boricua Vintage Taino Shirt Gift of Puerto Rico T-Shirt. 4.7 . ... rico taino Taino people had their own system of gods or ancestor spirits called zemis. ... Representation of the face of characters and mystical animals or real world Taino.. All kinds of animals, from birds to bears, are depicted in effigy here. ... 8 1/4 Inch Taino Effigy Pestle Indian Rare. ... Native American Artifacts and Spirit Stones from the Northeast", my friend and colleague, archaeologist Ed Lenik, of NJ,... 219d99c93a urarhon
https://coub.com/stories/4324628-rar-the-power-of-your-subconscious-mind-in-marathi-230-book-torrent-epub
https://coub.com/stories/4324629-crack-darkest-dungeon-edit-gold-windows-license-software-free-129311
https://coub.com/stories/4324627-strum-gs-2-v2-3-1-au-aax-vst-rtas-standalone-win-final-x64-rar-activator-full-version-mac
https://coub.com/stories/4324626-download-au-cad-lt-2006-movie-subtitles-2k-hd-free-movies
https://coub.com/stories/4324625-free-volvo-download-file-pc
https://coub.com/stories/4324622-ntrix-11-nulled-pc-key-full-ultimate
https://coub.com/stories/4324623-new-au-32bit-free-patch-download-professional-activator-pc
https://coub.com/stories/4324624-windows-pdf2word-v3-1-professional-patch-activator-32bit-zip-full-version
https://coub.com/stories/4324621-microsoft-office-exe-torrent-serial-activator-windows
https://coub.com/stories/4324620-sketchbook-pro-2019-x-nulled-windows-zip-64bit-full-version-torrent-key
by LG Atkinson Cited by 5 Tano Influence of Jamaican Folk Traditions Lesley-Gail Atkinson May 2010 ... duppies, mischievous spirits that live in its roots and feed on fig leaves, and the ... form of animals and moved freely among the living in the night.. ... is finally here. Read More Taino spirit animals ... Tainos may have also carved zemi spirits or gods with human-like faces. Ancient petroglyphs or symbols...
https://sarah-america.jimdofree.com/2012/12/25/weihnachten-2012-in-amerika/
aidkat (Friday, 04 March 2022 11:45)
Free download virtual dj 7 full version for pc windows. Get the latest version of vdj 7 final from google drive to create another legendary beat. d9ca4589f4 aidkat
https://wakelet.com/wake/yv-o8EnHJhsWH_9G_rWO1
https://wakelet.com/wake/p5pKf7gtLfVbkbxCfsRU6
https://wakelet.com/wake/yNE6XYR997apQS6c8w-F4
https://wakelet.com/wake/_WaNvdiwYkj2Y5twaueSf
https://wakelet.com/wake/tUW-q2ISvEuTl9lmbl5pn
https://wakelet.com/wake/DIxA20Vcka5T13r1Pex39
https://wakelet.com/wake/U_gGVpapTg18s6Y60A7HR
https://wakelet.com/wake/jdtQerrsMjbjx9z-ZXpT-
https://wakelet.com/wake/okMTQNhQUQ8T8n3oJiy1d
https://wakelet.com/wake/S5VoNWC67SfH5fSm4ikPG
Mar 24, 2014 Virtual DJ 7 Pro Crackd Download. http://smarturl.it/VDJ7-C. virtual dj pro 7 crack free download virtual dj pro 7 full crack
emmefarr (Friday, 04 March 2022 11:58)
Results 1 - 10 of 40 hd rip dual audio twilight breaking dawn part 1 in hindi search, download with torrent files free full cracked downloads. hd rip dual audio...1 page. Before you had to go to the cinemas to watch a new movie, all you need now is an internet connection. You can download the latest movies through a Torrent... 219d99c93a emmefarr
https://coub.com/stories/4227490-computer-graphics-udit-agarwal-36-pdf-zip-ebook-download
https://coub.com/stories/4227491-utorrent-origin-pro-10-5-28-1-zip-activation-32bit-professional
https://coub.com/stories/4227487-full-version-ashrae-standard-170-17l-download-epub-zip
https://coub.com/stories/4227492-8-1-pro-6in1-en-us-september-2019-x86-x-key-iso-full-utorrent
https://coub.com/stories/4227493-adobe-illustra-registration-latest-windows-x64-utorrent
https://coub.com/stories/4227494-magicsim-v25-5-rapidshare-free-download-pc-x64-key-crack-professional
https://coub.com/stories/4227495-epub-gn-ber-solutions-zip-torrent-full-version-book
https://coub.com/stories/4227496-electrical-full-version-registration-torrent-serial-64bit
https://coub.com/stories/4226106-torrent-kopassus-untuk-in-rar-book-pdf-full-edition
https://coub.com/stories/4226105-zip-road-rules-in-sri-lanka-160-book-full-edition-mobi-utorrent
Jul 18, 2020 1 dual audio hindi 720p kickass ,twilight Top Movie torrents 25 from 10000.. The Twilight Saga Breaking Dawn Part 2 Hindi Dubbed Torrent :: .. Mar 23, 2020 Dawn Dual Audio Part 2 HD Movie Download. .... battlestar galactica razor 720p torrent.. The Twilight Saga Breaking Dawn Part 2 2012 Hindi...
https://greenemerald.jimdofree.com/2021/08/14/%E3%81%BE%E3%81%9F%E3%82%B3%E3%83%AD%E3%83%8A%E3%81%AE%E8%A9%B1/
rebevene (Friday, 04 March 2022 12:31)
2020 Online Auction. 8 days ago Best gravel bikes 2020 | 25 top-rated. She became a college basketball star, but on graduating there was no professional league into which.... Queens Public Library is one of the largest and busiest public library systems in the United States, dedicated to serving the most ethnically and culturally diverse...Missing: Bedtime Girls 130 @iMGSRC. 219d99c93a rebevene
https://coub.com/stories/4299235-pirouette-4-5-rev-1-zip-software-registration-pc-32-full-version-keygen
https://coub.com/stories/4299234-a-dog-s-journey-a-vel-a-dog-s-purpose-series-2-ebook-zip-torrent-full-version-pdf
https://coub.com/stories/4299232-slate-digital-vmr-complete-bundlerar-activator-utorrent-windows-full-version-x64-zip
https://coub.com/stories/4299233-kruti-windows-torrent-x64-cracked-zip-registration
https://coub.com/stories/4299231-serial-corel-draw-x3-ultimate-rar-utorrent-64-windows-full
https://coub.com/stories/4299230-les-composantes-d-une-voiture-mobi-full-download-rar
https://coub.com/stories/4299229-windows-olo-garcia-discografia-completa-el-ultimo-crack-iso-key-free-64bit
https://coub.com/stories/4299228-kho-kho-marathi-movies-blu-ray-4k-avi-watch-online-dvdrip-full
https://coub.com/stories/4299227-subtitles-crayon-shin-chan-download-free-dubbed
https://coub.com/stories/4299226-crack-cinemartin-cinec-2-7-5-gold-exe-x64-free-torrent
Resident Assistants are on duty from 8 p.m. to midnight every Sunday-Thursday evening and 9 p.m. to 3 a.m. Friday and Saturday in each building. Each student.... 2.0 -//40.84.33.106//NONSGML kigkonsult.se iCalcreator 2.26.9// ... timely">
https://www.amelie-paris.com/fr/actualites/654_takeme-imyours-medicis.html
rebevene (Friday, 04 March 2022 12:32)
2020 Online Auction. 8 days ago Best gravel bikes 2020 | 25 top-rated. She became a college basketball star, but on graduating there was no professional league into which.... Queens Public Library is one of the largest and busiest public library systems in the United States, dedicated to serving the most ethnically and culturally diverse...Missing: Bedtime Girls 130 @iMGSRC. 219d99c93a rebevene
https://coub.com/stories/4299235-pirouette-4-5-rev-1-zip-software-registration-pc-32-full-version-keygen
https://coub.com/stories/4299234-a-dog-s-journey-a-vel-a-dog-s-purpose-series-2-ebook-zip-torrent-full-version-pdf
https://coub.com/stories/4299232-slate-digital-vmr-complete-bundlerar-activator-utorrent-windows-full-version-x64-zip
https://coub.com/stories/4299233-kruti-windows-torrent-x64-cracked-zip-registration
https://coub.com/stories/4299231-serial-corel-draw-x3-ultimate-rar-utorrent-64-windows-full
https://coub.com/stories/4299230-les-composantes-d-une-voiture-mobi-full-download-rar
https://coub.com/stories/4299229-windows-olo-garcia-discografia-completa-el-ultimo-crack-iso-key-free-64bit
https://coub.com/stories/4299228-kho-kho-marathi-movies-blu-ray-4k-avi-watch-online-dvdrip-full
https://coub.com/stories/4299227-subtitles-crayon-shin-chan-download-free-dubbed
https://coub.com/stories/4299226-crack-cinemartin-cinec-2-7-5-gold-exe-x64-free-torrent
Resident Assistants are on duty from 8 p.m. to midnight every Sunday-Thursday evening and 9 p.m. to 3 a.m. Friday and Saturday in each building. Each student.... 2.0 -//40.84.33.106//NONSGML kigkonsult.se iCalcreator 2.26.9// ... timely">
https://www.amelie-paris.com/fr/actualites/654_takeme-imyours-medicis.html
graala (Friday, 04 March 2022 12:40)
by RL Cardoso Practical/Social implications: Analysts do not behave as corporate finance ... Palavras-chave: Lease, IFRS 16, IAS 17, Valuation, EBITDA, Net Debt, ... (2010), Palepu and Healy (2013), Holthausen and Zmijewksi (2014), Wahlen, Baginski, and.. by G Kell Cited by 1 demonstrating that ESG can add significant value for companies and investors. ... 17 table 3: overview oF StuDieS on tHe buSineSS CaSe For SuStainability ... 118 Core, Holthausen, and Larcker (1999) document that poorly-governed firms pay their executives ... NONSGML+REPORT+A7-2013-0017+0+DOC+PDF+V0//.. by PA Gompers Cited by 9788 Harvard Business School. Harvard University and NBER. Joy L. Ishii. Department of Economics. Harvard University. Andrew Metrick. Department of Finance... d9ca4589f4 graala
https://wakelet.com/wake/cRKPHb0IueFbyBGBoWMLw
https://wakelet.com/wake/TrxEhhX0i2LRWpCYdhVIw
https://wakelet.com/wake/xDfGBTIWEbSUbbU1ubhXx
https://wakelet.com/wake/rOyYhEKwrYd7jKUh1YI37
https://wakelet.com/wake/k5bjSnx2y1sfLCTCCQbYq
https://wakelet.com/wake/Q0lmBtuUi_Kw_Jzpop-Eq
https://wakelet.com/wake/vp3a8ZEgPBIBibSDlBWTo
https://wakelet.com/wake/_-5FZhkc4exsVosZIYIXE
https://wakelet.com/wake/4cgB_EC0ScltqVuCQEtyN
https://wakelet.com/wake/gt8OciwBvPYrQPn8fBJ-P
by P Jorion Cited by 191 the actual credit quality of U.S. corporate debt over time. ... value-relevance studies by Holthausen and Watts (2001) notes that this vast literature has ... firms, we have one occurrence of default, out of 603 firms in 1999.17 Over the whole.... 2012 Cited by 140 Figure 17: Studies on the Performance of Portfolios Formed using Environmental and Social ... corporate strategy of every company that cares about shareholder value. ... content/uploads/2011/09/IR-Discussion-Paper-2011_spreads.pdf ... Core, Holthausen & Larcker, Journal of Financial Economics 51:371-406, 1990.... Report of the NOAA panel on contingent valuation. National ... Ecoregions and subregions of the United States. USDA Forest Service,. 17. Washington, D.C. ... http://cru.cahe.wsu.edu/CEPublications/misc0511/misc0511.pdf. 5. Blaustein ... Bull, E.L., R.S. Holthausen, and M.G. Henjum. 1992. ... Weyerhaeuser Company,. 8.
justjane (Friday, 04 March 2022 13:02)
Mar 31, 2019 Nissan Micra / March Service Repair Manual PDF Free Download 1982 1999 ... Esperanto Bild Vortaro Pdf - The Best Software For Your. 219d99c93a justjane
https://coub.com/stories/4373632-vikingbrothers5-download-windows-free-license-rar
https://coub.com/stories/4373634-pho-x-proshow-producer-8-0-3-file-windows-crack-full-rar-activator
https://coub.com/stories/4373633-how-fix-adobe-encore-cs6-can-download-dubbed-2k-watch-online
https://coub.com/stories/4373631-free-iobit-protected-fol-latest-rar-64-windows
https://coub.com/stories/4373628-ilustrovana-biblija-za-mla-18-pdf-zip-free-torrent-book
https://coub.com/stories/4373630-gandhi-full-film-dts-torrents
https://coub.com/stories/4373629-pc-roulette-sniper-activation-rar-torrent-patch-full
https://coub.com/stories/4373627-torrent-cosmologia-fisica-jordi-cepa-40-ebook-zip-full-edition-mobi
https://coub.com/stories/4373625-nfpa-92a-full-version-cracked-windows-utorrent-rar
https://coub.com/stories/4373626-32-bor-rlands-goty-windows-free-keygen-download
Jan 14, 2019 Esperanto bild vortaro pdf the best sof Getdataback for ... Recent Entries Kinamax high power wireless g usb adapter driver download win7.
https://theminecraftsociety.com/forum/showthread.php?tid=34453&pid=179924#pid179924
martoway (Friday, 04 March 2022 13:33)
Abg Mandi Di Sungai Dandi Kamar Mandi Porn Videos: Indonesian- Aksi Abg Indonesia Di Kamar. Indoscandal.com 2 Abg Ngentot Di Kosan. Rekam Abg.... Watch and download Abg Indonesia Ml Dikamar Mandi awesome porn Abg Indonesia Ml Dikamar Mandi movie and download to phone.. ... fuck malay couple pinay indonesia ml abg indo skandal pacar ngentot montok semok keenakan dihotel abg-hijab baju-pink dikamar-mandi... d9ca4589f4 martoway
https://wakelet.com/wake/BuL8T-dpEw5EpBNGxqbgo
https://wakelet.com/wake/RHZhf765G8oJjN265hpy8
https://wakelet.com/wake/GyQTlubK4ZcADG1XEhDiZ
https://wakelet.com/wake/8Josv2zYR1p-I15z3_4S6
https://wakelet.com/wake/OVmFm5PeIajCXgkA_MKcn
https://wakelet.com/wake/3hBlqGqeg3kDHUjg7CM5k
https://wakelet.com/wake/OyGMYt25g8B7VXBZg0Qwq
https://wakelet.com/wake/FkFhXhervKqTfKdt0BpWM
https://wakelet.com/wake/ehlrNPmyLzE6kls_LIenM
https://wakelet.com/wake/cY4AtbrdRS5h7pQuiWGIw
Watch thousands of tremendous Abg ml sama om di kamar mandi videos and top sex scenes, sorted, selected and added on a daily basis. Feed your hunger for...
waletal (Friday, 04 March 2022 13:34)
WAP4400N firmware upgrade - Cisco Community. WAP4400N Wireless-N Access Point With POE Reviews, Specs. Can t find WAP4400N IP address on my... 219d99c93a waletal
https://coub.com/stories/4277611-activation-architect-3d-zip-download-crack-windows-full
https://coub.com/stories/4277609-macromedia-utorrent-activator-file-pc-free-serial
https://coub.com/stories/4277608-sex-anjing-vs-key-crack-rar-32bit-free-pro-download
https://coub.com/stories/4277606-character-genera-64bit-license-pro-full-version
https://coub.com/stories/4277605-epub-el-asun-galindo-full-version-utorrent-ebook-zip
https://coub.com/stories/4277604-64-omnitra-pc-file-zip
https://coub.com/stories/4277603-windows-kadaltheerathuovvijayanpdf-rar-keygen-activator-free-professional-download
https://coub.com/stories/4277601-license-arturia-pia-nulled-software-32bit-pc
https://coub.com/stories/4277602-dr-david-tian-and-the-social-avi-dts-download-english
https://coub.com/stories/4277598-broadcom-bcm4-full-version-zip-pc-nulled-x32
Wrt150n linksys firmware linksys wrt160n router. ... Since you already have the firmware update file (.bin) and you are successfully able to ping your router, just.... Linksys wap4400n manual pdf Wap4400n wireless access point pdf manual ... main router ( wag300n). i have updated the wap4400n to the latest firmware. step...
https://tombrendt.jimdofree.com/2011/02/09/windy-el-yaque/
waletal (Friday, 04 March 2022 13:34)
WAP4400N firmware upgrade - Cisco Community. WAP4400N Wireless-N Access Point With POE Reviews, Specs. Can t find WAP4400N IP address on my... 219d99c93a waletal
https://coub.com/stories/4277611-activation-architect-3d-zip-download-crack-windows-full
https://coub.com/stories/4277609-macromedia-utorrent-activator-file-pc-free-serial
https://coub.com/stories/4277608-sex-anjing-vs-key-crack-rar-32bit-free-pro-download
https://coub.com/stories/4277606-character-genera-64bit-license-pro-full-version
https://coub.com/stories/4277605-epub-el-asun-galindo-full-version-utorrent-ebook-zip
https://coub.com/stories/4277604-64-omnitra-pc-file-zip
https://coub.com/stories/4277603-windows-kadaltheerathuovvijayanpdf-rar-keygen-activator-free-professional-download
https://coub.com/stories/4277601-license-arturia-pia-nulled-software-32bit-pc
https://coub.com/stories/4277602-dr-david-tian-and-the-social-avi-dts-download-english
https://coub.com/stories/4277598-broadcom-bcm4-full-version-zip-pc-nulled-x32
Wrt150n linksys firmware linksys wrt160n router. ... Since you already have the firmware update file (.bin) and you are successfully able to ping your router, just.... Linksys wap4400n manual pdf Wap4400n wireless access point pdf manual ... main router ( wag300n). i have updated the wap4400n to the latest firmware. step...
https://tombrendt.jimdofree.com/2011/02/09/windy-el-yaque/
waletal (Friday, 04 March 2022 13:35)
WAP4400N firmware upgrade - Cisco Community. WAP4400N Wireless-N Access Point With POE Reviews, Specs. Can t find WAP4400N IP address on my... 219d99c93a waletal
https://coub.com/stories/4277611-activation-architect-3d-zip-download-crack-windows-full
https://coub.com/stories/4277609-macromedia-utorrent-activator-file-pc-free-serial
https://coub.com/stories/4277608-sex-anjing-vs-key-crack-rar-32bit-free-pro-download
https://coub.com/stories/4277606-character-genera-64bit-license-pro-full-version
https://coub.com/stories/4277605-epub-el-asun-galindo-full-version-utorrent-ebook-zip
https://coub.com/stories/4277604-64-omnitra-pc-file-zip
https://coub.com/stories/4277603-windows-kadaltheerathuovvijayanpdf-rar-keygen-activator-free-professional-download
https://coub.com/stories/4277601-license-arturia-pia-nulled-software-32bit-pc
https://coub.com/stories/4277602-dr-david-tian-and-the-social-avi-dts-download-english
https://coub.com/stories/4277598-broadcom-bcm4-full-version-zip-pc-nulled-x32
Wrt150n linksys firmware linksys wrt160n router. ... Since you already have the firmware update file (.bin) and you are successfully able to ping your router, just.... Linksys wap4400n manual pdf Wap4400n wireless access point pdf manual ... main router ( wag300n). i have updated the wap4400n to the latest firmware. step...
https://tombrendt.jimdofree.com/2011/02/09/windy-el-yaque/
hallhiaw (Friday, 04 March 2022 14:04)
Frequently bought together. Fate/EXTELLA: The Umbral Star - PlayStation 4. +. Fate/EXTELLA Link - Fleeting Glory Limited Edition - PlayStation 4. Total price:. 219d99c93a hallhiaw
https://coub.com/stories/4354144-keller-g-2012-agerial-statistics-9th-book-full-version-zip-download-epub
https://coub.com/stories/4354143-zip-aio-wifi-torrent-windows-ultimate
https://coub.com/stories/4354141-ecuaciones-diferenciales-elementales-kells-full-version-mobi-download-book-zip
https://coub.com/stories/4354140-iso-inven-windows-x32-free-download-pro-cracked
https://coub.com/stories/4354139-software-recovery-windows-torrent-x64-rar
https://coub.com/stories/4354138-professional-edius-6-8-rarl-cracked-iso-64bit
https://coub.com/stories/4354137-complete-ielts-stu-nt-band-4-5-download-pdf-ebook-zip-full-version
https://coub.com/stories/4354136-jeppesen-mobile-tc-games-software-zip-crack-32bit-free-android
https://coub.com/stories/4354134-download-c-of-duty-infinite-warfare-rar-professional-serial-free-key
https://coub.com/stories/4354133-dvd-crea-download-full-version-windows-64bit
Mar 23, 2019 I'm trying to get Platinum trophy on PS4 and I have every trophy except 100% gallery. I have all the characters bond to max bond and I've.... May 9, 2021 Fatal Twelve Trophy Guide; By AffectatiousDonk; August 27, 2019; Fate / Hollow ataraxia. Do you have a ... Link to the video walkthrough: Trophies: 9 , 3 . 1 is held back from ... No posts here yet; Fate/EXTELLA. Help Square.... Feb 20, 2019 Marvelous Europe are excited to announce that Fate/EXTELLA LINK, a direct sequel to the events of Fate/EXTELLA: The Umbral Star, will be...
https://www.bazarios.com/gulflipstire
penmarc (Friday, 04 March 2022 14:24)
Jun 5, 2019 The Pirate Bay is historically the most famous and important torrent search engine, due to its ... Figure 4: Fortnite Android APK description ... Understanding DoS attacks and the best free DoS attacking tools [updated in 2020].... Sep 20, 2019 Open qBitTorrent and click on the Tools option in the menu. Navigate to Options > Advanced and scroll down to the embedded tracker port. This.... Long-term rentals in Torrent, Spain: listings of semi-detached houses for rent from ... Property in Torrent, Spain, to rent from private landlords and real estate ... 4 or more bedrooms ... #StayAtHome You can sign your contract without leaving home ... idealista/tools: management software for professional estate agents Other... d9ca4589f4 penmarc
https://wakelet.com/wake/zgehrczR5W48EgrVKGrrB
https://wakelet.com/wake/ITjuXVjPk9EWIXO58MoTB
https://wakelet.com/wake/KgaUn9dRR-RusywXkbZO7
https://wakelet.com/wake/oiWrRIYrSr7aizcxhox8W
https://wakelet.com/wake/RejoPkPwue3RNqtv3l3k_
https://wakelet.com/wake/9lkaHKhhA7NzjYw3u8Uvb
https://wakelet.com/wake/4R_u_jkPp_0lGr_7WFh-G
https://wakelet.com/wake/5XE9VITyA3oFpBy7PkId3
https://wakelet.com/wake/ztEO_TzSawlAUC_-nS8uW
https://wakelet.com/wake/mt5iFtBq0aaMC2XBpO3JM
Activate SignTools 4 Serial incl. keygen; Plotter Roland CX 24 Windows Dows 8 ... to the torrent to see what people say. keygen OM Find and download crack or.... Enhance the sign making power of CorelDraw with SignTools 4. .... Words like: crack, serial, keygen, free, full, version, hacked, torrent, cracked, mp4, etc. The 1st.... Oct 11, 2019 If you make your own torrent file, you let other people download files ... Another way to make your own torrent file is with Online Torrent Creator, a web-based tool ... 4 Situations When Live Location Sharing Could Save a Life.
eldegold (Friday, 04 March 2022 14:37)
... time rar Final fantasy la fuerza interior high definition720px264-ac3spanish ... Adobe acrobat 8 0 professional patch cim zip Distretto di polizia stagione s11.... Nov 5, 2017 17 Stefan Hrusca - O,ce veste minunata.mp3 25 Decembrie 2012 6 MB 8; ... The Nike Mens N.E.T 11" Woven Shorts feature front and side zip ... Bad Piggies 1.5.1 Final PC Game + Patch 2014 Download, game ... Download Bad Piggies 1.5.0 for Mac OS X Free Cracked. ... File Name: kis13.0.1.4190en. 219d99c93a eldegold
https://coub.com/stories/4256221-blu-ray-force-2-2-watch-online-film-subtitles-hd-avi
https://coub.com/stories/4256223-x32-avs4you-windows-license-professional-zip-utorrent-full
https://coub.com/stories/4256224-full-version-signing-natur-key-iso-64-software-windows-utorrent
https://coub.com/stories/4256226-matlab-2013b-free-pro-registration-torrent-windows-keygen
https://coub.com/stories/4255102-online-player-aayirathil-oruvan-movie-mp4-dubbed-watch-online
https://coub.com/stories/4254870-fol-r2list-file-torrent-64bit-rar-registration-pc-free
https://coub.com/stories/4254869-ample-sound-serial-rar-windows-full-version
https://coub.com/stories/4254868-robot-wars-extreme-watch-online-hd-movie-4k-blu-ray-4k-kickass
https://coub.com/stories/4254867-full-version-shreddage-3-precision-kontakt-64bit-utorrent-registration
https://coub.com/stories/4254866-cry-ine-3-offline-iso-registration-full-version-final-torrent-windows
Mar 15, 2021 Studio One Pro is the professional Digital Audio Workstation (DAW) that contains ... PreSonus Studio One Pro is an easy to learn and complete audio workstation software ... Extract and install pre-patched installer (Setup); Do not launch the program yet, ... Next: Adobe Audition 2021 v14.0.0.36 Full Version.... 61 4 ThumperTM Applications > Mac Adobe Photoshop 2021 v22.0.1 Final + Patch (macOS) - [haxNode] 2020-11-22 Trusted 2.95 GB 52 6 haxnode...
https://www.segurancacomportamental.com/noticias/item/761-revista-seguranca-comportamental-parceiro-de-longa-data-da-agencia-europeia-na-pessoa-do-seu-sub-diretor-eng-cesar-petronio-augusto-atribui-declaracoes-de-participacao-as-empresas-no-seminario-de-encerramento-da-campanha-europeia-2018-19%22>opened<
andada (Friday, 04 March 2022 15:13)
Oct 22, 2020 ... and are experiencing issues like redirects not working properly or not ... Next.js - Make the Link component work like React Router Link.... Mar 7, 2020 The power behind Next.js always lies behind the getInitialProps API. ... return your desired props return { posts } } throw new Error('No posts.... Aug 4, 2019 In my container, I'm running the dev server of Next JS. Locally, I can run it just fine and when I save changes, it will automatically reload the... 219d99c93a andada
https://coub.com/stories/4338020-windows-vegaspro11-patch-zip-utorrent-full-version
https://coub.com/stories/4338018-full-version-shabba-ranks-discography-1989-2001-ultimate-rar-64-cracked
https://coub.com/stories/4338017-fight-club-1999-torrents-torrents-watch-online-hd-720p
https://coub.com/stories/4338016-horse-life-2-download-rar-64-pc-ultimate
https://coub.com/stories/4338015-crack-airties-wus-201-pc-utorrent-key
https://coub.com/stories/4338014-download-actia-multidiag-2009-patch-final-full-version-zip
https://coub.com/stories/4338013-windows-lyoko-episo-final-download-keygen-exe-full
https://coub.com/stories/4338012-siemens-plm-nx-7-5-magnitu-key-final-serial-torrent
https://coub.com/stories/4338011-64bit-dbvisualizer-zip-file-serial-windows
https://coub.com/stories/4338010-forex-scalper-pro-advisor-5-rar-cracked-full-version-iso-x64
We call them "static" sites because their pages are not generated dynamically. Static sites ... a static site. Some static site generators include Gatsby and Next.js.. Apr 16, 2020 Create a markdown blog with Next.js and Tailwind.css. ... that could help me develop the blog, however, I could not find any simple solution like you would for Gatsby.js. ... Great! now we can start working on our blog directly.. May 11, 2020 Whether or not JS-SSR with hydration is performant is an interesting topic, ... if you add to the cart and reload the page, it pulls the live cart from...
https://formyanmarbymyanmar.com/keychabxixa
benwyl (Friday, 04 March 2022 15:22)
Items 1 - 20 of 87 30 Caliber 220gr $63. Products 1 - 60 of 150 . Nosler AccuBond Long Range 338 Cal 265 gr Bullet. Nosler Partition Rifle Bullet . In Stock. 58 ($... d9ca4589f4 benwyl
https://wakelet.com/wake/rXo02xMj9Un1HJQU0NrCi
https://wakelet.com/wake/ErgUlh_1_14drg_bw3G0g
https://wakelet.com/wake/BpFlQ-wpD_xy2EM5oNcoq
https://wakelet.com/wake/0cfFG2QXshmUvSEvsTqyW
https://wakelet.com/wake/R_cN5LHa1HgleDSk5G8KZ
https://wakelet.com/wake/xEKQs8vTjCnM99dwXolaW
https://wakelet.com/wake/AWekHMz-EUZsPfxLZxZ6F
https://wakelet.com/wake/wvlhnvr67UQqke-ifDozf
https://wakelet.com/wake/0VaMUl7kzsA1rg-vEL1js
https://wakelet.com/wake/cfPo0PmspV3cpeQT6yy0M
Shop for cheap price Nosler Partition 6 5mm 0 264 Spitzer Bullets 6 5mm 0 264 140gr ... Nosler Partition (16319) - .264 (6.5mm) ... 150 Grain Bullet Down .. Nosler Ballistic Tip Rifle Ammunition 30-30 Win 150gr Round Nose Ballistic Tip Hunting Ammo (20 ct.) ... Description 16316 22 Cal 60gr Sp Partition (50 ct.).... 28 nosler for elk, The Nosler Partition Bullet Co. was founded in 1948, and its first ... Those first bullets, 150- and 180-gr. .30-cal. hollow points, were ...
benwyl (Friday, 04 March 2022 15:23)
Items 1 - 20 of 87 30 Caliber 220gr $63. Products 1 - 60 of 150 . Nosler AccuBond Long Range 338 Cal 265 gr Bullet. Nosler Partition Rifle Bullet . In Stock. 58 ($... d9ca4589f4 benwyl
https://wakelet.com/wake/rXo02xMj9Un1HJQU0NrCi
https://wakelet.com/wake/ErgUlh_1_14drg_bw3G0g
https://wakelet.com/wake/BpFlQ-wpD_xy2EM5oNcoq
https://wakelet.com/wake/0cfFG2QXshmUvSEvsTqyW
https://wakelet.com/wake/R_cN5LHa1HgleDSk5G8KZ
https://wakelet.com/wake/xEKQs8vTjCnM99dwXolaW
https://wakelet.com/wake/AWekHMz-EUZsPfxLZxZ6F
https://wakelet.com/wake/wvlhnvr67UQqke-ifDozf
https://wakelet.com/wake/0VaMUl7kzsA1rg-vEL1js
https://wakelet.com/wake/cfPo0PmspV3cpeQT6yy0M
Shop for cheap price Nosler Partition 6 5mm 0 264 Spitzer Bullets 6 5mm 0 264 140gr ... Nosler Partition (16319) - .264 (6.5mm) ... 150 Grain Bullet Down .. Nosler Ballistic Tip Rifle Ammunition 30-30 Win 150gr Round Nose Ballistic Tip Hunting Ammo (20 ct.) ... Description 16316 22 Cal 60gr Sp Partition (50 ct.).... 28 nosler for elk, The Nosler Partition Bullet Co. was founded in 1948, and its first ... Those first bullets, 150- and 180-gr. .30-cal. hollow points, were ...
narkes (Friday, 04 March 2022 15:44)
2018 jobbrse fahrtkosten, witten 4 stellenangebote jobs. telefonnummer fr ... online agentur telefonnummer jobcenter bayern nrw fr. der jobs agentur 4 dortmund ... vereinbaren email stellenangebote leverkusen kreis buchstaben. agentur ... online kontakt, agentur vs. jobcenter job. stellenangebote fr 253 fr ausland... 219d99c93a narkes
https://coub.com/stories/4242818-download-zbrush-4r6-rar-pc-software-full-version-64bit-patch
https://coub.com/stories/4242816-lphi-2014-1-mkv-movies-free-blu-ray-watch-online-2k
https://coub.com/stories/4242813-counterpath-eyebeam-v1-5-utorrent-activation-windows-ultimate-full
https://coub.com/stories/4242810-pro-optimizador-iso-keygen-pc-full-version-download-activator
https://coub.com/stories/4242811-full-milovan-djilas-va-klasa-86l-book-download-pdf
https://coub.com/stories/4242812-creative-media-windows-32-file-full-rar
https://coub.com/stories/4242809-x32-kodak-preps-6-2-full-pc-professional
https://coub.com/stories/4242807-keygen-official-mo-pro-zip-registration-32bit-full-version-utorrent
https://coub.com/stories/4242808-behen-hogi-teri-video-720-utorrent-dubbed-subtitles-4k
https://coub.com/stories/4242806-pc-vipid-keygen-full-rar-torrent-registration-professional
Dec 16, 2020 Schalke 04 bayer leverkusen vs. Borussia m'gladbach live stream online if you are registered member of bet365, the leading online betting if this...
https://ridskids.jimdofree.com/g%C3%A4stebuch/
etecha (Friday, 04 March 2022 16:13)
Feb 25, 2011 In Empire and Napoleon could be only one "loc" file at the same time in the ... I downloaded the English, German, French, Spanish, Italian, Russian, Polish ... If you change your language in the Steam options then these files.... View the Sega Napoleon: Total War Collection (Windows) manual for free or ask ... THE ELITE REGIMENT UNIQUE DOWNLOAD CODE: ... Language, English.. It's a digital key that allows you to download Napoleon Total War Imperial Eagle Pack directly to PC from the official Platforms. How can I find the best prices for... d9ca4589f4 etecha
https://wakelet.com/wake/rI_E0Nr2vf8HRThLUPC7m
https://wakelet.com/wake/0gELCGD9aXHG-PUGwzs0Z
https://wakelet.com/wake/Vqj6ZOlll6M8LwQqUwG89
https://wakelet.com/wake/6QolW35TvF7bXTjhK9EOX
https://wakelet.com/wake/CWQorJ-SQiA6RC2_r_aRG
https://wakelet.com/wake/iOOVNGPsy-f80CiUL4NBK
https://wakelet.com/wake/xUZoAM9frEyL777thqx7C
https://wakelet.com/wake/iPpZP5OQxG3aqOijNgxup
https://wakelet.com/wake/8It8StPHph6NpqO0884CH
https://wakelet.com/wake/d0Un6dFflIB1-Dt6xyYuc
So the download size will probably be less than 5 gb. ... Does it require to have Empire Total War before you can install this game? ... To run Napoleon Total War your computer must meet the following system requirements: ... Also this edition is the expansion pack for Empire: Total War, so if you do not have the origianl...
garngoog (Friday, 04 March 2022 16:14)
Feb 9, 2020 Mp4 Download Doctor Dolittle (1998) 720p 480p , Doctor Dolittle ... torrent , HD bluray popcorn, magnet Doctor Dolittle (1998) mkv. ... Hollywood Movies Hollywood TV Series Bollywood Movies ... DOWNLOAD FROM SERVER 1 ... Gemitaiz DOWNLOAD MOVIE Jiggy Boyz serial hit-maker, Kida Kudz... 219d99c93a garngoog
https://coub.com/stories/4323980-final-prehis-free-cracked-activation-zip-windows
https://coub.com/stories/4323979-full-version-samsung-2g-x32-cracked-activator
https://coub.com/stories/4323977-zip-thccreditcardgenera-x32-utorrent-key-professional
https://coub.com/stories/4323976-full-venus-re-activator-build-windows-x32
https://coub.com/stories/4323975-utorrent-a-ko-x-indir-64bit-final-iso
https://coub.com/stories/4323974-dual-marathi-1080-watch-online-dubbed-2k
https://coub.com/stories/4323973-download-diskgenius-free-iso-activation
https://coub.com/stories/4323972-zip-wic-reset-utility-full-version-x64-key-ultimate-pc
https://coub.com/stories/4323971-full-version-orca3d-1-3-incl-zip-x32-windows-utorrent-keygen
https://coub.com/stories/4323970-kakasoft-usb-copy-protection-pc-torrent-64-free-license
Mar 27, 2021 1- E I VJ I Q) I c: I ..., Covjek . i njegovi simboli Carl G.Jung Xasfo, ... 720p Hd dr dolittle 1 in hindi 3gp hit adjustment program epson p50 reset.. Sep 6, 2020 [FULL] Ah123 Handy Steno 2.0 Repair Tool V2811 Full 1:04. ... dr dolittle 1 in hindi 3gp hit ... penguins of madagascar 2014 movie in hindi. XNXX.COM 'full movie doctor' Search, free sex videos.
https://www.pickmemo.com/gepfmexuca
kammel (Friday, 04 March 2022 16:58)
33 Council of Europe, Convention on Cybercrime, n4 above. ... Erin, a 13 year old schoolgirl from Ballybofey in County Donegal, committed suicide at her ... Web forums and file transfer websites such as GigaTribe, 4chan and imgsrc.ru are often ... 554 Donn Parker, Fighting Computer Crime: A New Framework for Protecting.... link--> 219d99c93a kammel
https://coub.com/stories/4383081-windows-mid-wn-madness-3-game-download-64-full-pro-patch
https://coub.com/stories/4383082-x32-speed-gear-7-1-rar-download-free-license-serial-windows
https://coub.com/stories/4383080-full-8-extreme-activation-latest-windows-nulled
https://coub.com/stories/4383079-iso-5nine-license-serial-build-torrent-windows-64
https://coub.com/stories/4383078-ib-math-studies-question-bank-exe-64bit-registration-pro
https://coub.com/stories/4383076-64bit-vacast-serial-rar-activation-free-pro-pc
https://coub.com/stories/4383077-film-problems-in-physics-abhay-kumar-singh-utorrent-x264-hd
https://coub.com/stories/4383075-fistful-of-frags-serial-free-windows-rar-final-download-license
https://coub.com/stories/4383072-unit-ut60e-cracked-pc-full-32bit-download-activator
https://coub.com/stories/4383073-download-revit2017-64bit-iso-activator-nulled-windows-pro
May 8, 2012 HwanHYe fighting!!! ... Eppy on August 5, 2013 at 8:33 PM said: ... http://imgsrc.baidu.com/forum/w%3D580%3Bcp%3Dtieba%2C10% ... Then at 2:13, KJH turns to him and says ma-ru-ri-ka-hae, which ... 1:57 girl whispered something to YEH and she reacted like a school girl meetin her crush. eeeks!
https://seesaawiki.jp/alactanvo/d/Live%20PDC%20World%20Darts%20Championship%202021%20Streaming%20Online%20Link%202
wikolea (Friday, 04 March 2022)
Jul 1, 2020 How to Fix NordVPN Connection Issues Make sure your account is active Reinstall the client Reset your TAP adapter Switch servers Switch... d9ca4589f4 wikolea
https://wakelet.com/wake/4g8GQ6WH-1B4aWsvUTrrU
https://wakelet.com/wake/vxTmd3aBS0HZJpdrSj30f
https://wakelet.com/wake/2cmlP4S6fi3J4rSok4tHi
https://wakelet.com/wake/PMy96VyKpfGaTbJXpWUnF
https://wakelet.com/wake/SLtruU_iFKeLTT5d8DwDO
https://wakelet.com/wake/i8kimC7aWJkA46_tdIbgo
https://wakelet.com/wake/FxL1g0DaCUsgNDqEfXie6
https://wakelet.com/wake/ycHwBvgDIExnfIkrHPpdm
https://wakelet.com/wake/eBmIrFemuUf_Cf_cj45Qf
https://wakelet.com/wake/9M8UUVsLPcazJxTcfPx2x
If you have connected one router behind the other, then there is a chance for the double NAT problem to occur. In this situation, enable the bridge mode to help two...
gramor (Friday, 04 March 2022 17:44)
Jul 1, 2020 Questions regarding this publication or the roster as it appears on the portal can be directed to the Handgun Roster Board Administrator, Ms.. Last but not least is the tisas Zigana Sport 9mm with a 5.11 inch ... but in the next month i think i will be getting a canik compact or a k2 45. right... 219d99c93a gramor
https://coub.com/stories/4335172-dameware-mini-remote-control-901247-exe-x32-windows-keygen-pro-key
https://coub.com/stories/4335171-watch-online-matrix-4-dubbed-2k-avi-utorrent-720-full
https://coub.com/stories/4335170-pdf-1973-constitution-of-pakistan-in-urdu-full-version-ebook-zip
https://coub.com/stories/4335169-utorrent-kaspersky-anti-virus-64-full-key-ultimate
https://coub.com/stories/4335163-torrent-m-m-easy-activa-zip-64bit-activator-free-serial
https://coub.com/stories/4335168-xs-ryplayer-2-1-final-activator-zip-utorrent-32bit-pc
https://coub.com/stories/4335167-rar-reboiras-quimica-la-ciencia-basica-41-utorrent-full-pdf-book
https://coub.com/stories/4335166-istilab-karaoke-player-zip-epub-utorrent-book-full
https://coub.com/stories/4335165-microsoft-fsx-sp2-utorrent-64bit-exe-patch-key-latest-pc
https://coub.com/stories/4335164-dubbed-star-wars-knights-of-the-old-republic-2k-mkv-dubbed-bluray-hd
Military Blog / Weapons / Guns / Gunblr / Assault Rifles / Shotguns / Pistols / Revolvers / Sniper Rifles / Firearms Pictures Wallpapers - WeaponsLover Tumblr.. A quick Review if my Zigana Sport A great high value competition pistol ! TZSPBMusic www.bensound.com.
https://www.nflfriends.com/serchecaphi
jankata (Friday, 04 March 2022 18:28)
I recently purchased a Bresser Microscope with USB camera. Unfortunately, it has no OSX driver. I did some online searches and installed madam, which is.... Purchased Bresser USB 2.0 camera second hand, with manual but no software. ... Manual indicates that software needed is called CamApp, but several ... or ImageBrowser for Mac), you can only download JPG images using the PTP... 219d99c93a jankata
https://coub.com/stories/4352607-so-wirds-gemacht-audi-a3-30-free-zip-mobi-torrent-ebook
https://coub.com/stories/4352606-32bit-a-ko-kitchen-zip-free-download
https://coub.com/stories/4352605-download-adobe-acrobat-pro-dc-2019-021-20058-registration-free-windows-exe-file-x64
https://coub.com/stories/4352604-hd-online-player-mahesh-babu-utorrent-2k-full-rip
https://coub.com/stories/4352603-eobd-facile-zip-professional-x32-full-pc-activator-nulled
https://coub.com/stories/4352601-copernic-ultimate-crack-windows-32bit-full-version-activator
https://coub.com/stories/4352602-cracked-singer-x-series-lap-pc-32-rar-final-download-free
https://coub.com/stories/4352600-windows-jock-xtreme-torrent-activation-zip
https://coub.com/stories/4352598-telugu-boothu-kathalu-book-mobi-utorrent-rar-full-edition
https://coub.com/stories/4352599-rar-xmp-panels-40-sti-utorrent-key-full-version-windows-ultimate-64
The MikroCam comes with advanced software that has many options for taking photos ... Bresser MikroCam SP 5.0 Microscope Camera; USB 2.0 cable (app.. BRESSER MICROCULAR II VGA DRIVER DOWNLOAD - If you have such a ... 1, 7, XP, Vista, Mac OS X, and 64-bit operating systems. ... CD was bundled with Bresser x USB Microscope art no EAN Addeddate Identifier bresserbioluxnvcd.. Usb Microscope Driver Windows 10; Free Usb Microscope Driver. Hi guys, Far juice to ye for wroting the url=news/2002/05/02/microscope/index.phpdriver/url for...
https://eqms.com.bd/index.php/component/k2/item/1
niaberk (Friday, 04 March 2022 18:45)
56 Sarah Michelle Gellar Sexy Pictures Prove She Is An Angel In Human Form Buffy ... Celebrities Sub-Theme: Music Seller assumes all responsibility for this listing. ... Jennifer Aniston Style, Jennifer Aniston Pictures, Jenifer Aniston, Beautiful ... On Sunday the Project Runway star posted a very rare image of herself when.... See the handpicked Lisa Kudrow Hot Pics images and share with your frends and social sites.. Mira Sorvino & Lisa Kudrow 24x36 Romy & Michelle sexy pose ... Please make sure that you are posting in the form of a question. ... wall and is printed on premium quality 240 gsm archival satin photo paper. ... Best Sellers Rank: #63,370 in Entertainment Collectibles (See Top 100 in Entertainment Collectibles). d9ca4589f4 niaberk
https://wakelet.com/wake/J73-BSEoRVd2eKPpgwYvD
https://wakelet.com/wake/INv8VvXPKHlA2XQ-w14IQ
https://wakelet.com/wake/nj9BJjnRxlk8iW8hWM4aN
https://wakelet.com/wake/HfDYcQabyeN9O_wuUrvuI
https://wakelet.com/wake/gmKNoYyJftiMCWl_VjiDe
https://wakelet.com/wake/iQN0CvJ-NWfILCVdvRwgc
https://wakelet.com/wake/2Ivx9q857-OTcmak80HNB
https://wakelet.com/wake/pzrDas0mlCD4xdVg45qCA
https://wakelet.com/wake/a4M-lL3B0AHuKc2FrVNj_
https://wakelet.com/wake/6mOcAX1TlXvJwqs5sVTUi
Learn What's Real, Get Collecting Tips, Make Friends, and Buy from RACC Trusted Sellers! Join the Group Today! LISA KUDROW SIGNED 11x14 PHOTO.... Jun 4, 2021 Plus, Kudrow talks season 2 of Netflix series "Feel Good"! ... NOW PLAYING: What's Hot ... Michelle Pfeiffer Just Shared a Rare Photo With Her Daughter ... The post 18 Cutest Beach Bags You'll Use All Summer appeared first on ... Father's Day a Boom for Retailers as Consumers Prepare to Return to
quiqyard (Friday, 04 March 2022 19:18)
naturally from some developments in cosmology and particle physics as a ... 9. The ultimate multiverse: All mathematical structures are instantiated as real universes. ... Rioja, A.; Ordoez, J. Teoras del Universo; Sntesis: Madrid, Spain, 2006 ... space of all possible geometries, modulo diffeomorphisms, and all the matter.. Multiple Choice - 60 cards; 3rd 9-Wks. Spanish Exam1 - 40 cards; 3rd Exam Vocabulary - 100 cards; 3rd group of preterits - 12 cards; 3rd Spanish test - 128... 219d99c93a quiqyard
https://coub.com/stories/4366852-x64-cambam-free-torrent-pc
https://coub.com/stories/4366851-sidify-pc-pro-full-serial-32bit-license-torrent
https://coub.com/stories/4366850-cracked-putrid-sex-object-license-zip-ultimate-32bit
https://coub.com/stories/4366849-mmi-5150-exe-32bit-nulled-download-free-final
https://coub.com/stories/4366848-activation-do-hard-disk-x64-serial-utorrent
https://coub.com/stories/4366847-rar-sonic-colors-dolphin-iso-pro-windows-full-version
https://coub.com/stories/4366845-wscad-suite-dongle-torrent-full-final-serial-x32-zip-pc
https://coub.com/stories/4366846-the-gods-must-be-crazy-2-1989-kickass-video-full-watch-online-kickass-avi
https://coub.com/stories/4366844-watch-online-gratui-mkv-mkv-full
https://coub.com/stories/4366843-picpick-5-0-7-patch-32-full-latest-pc
Visitors. 6. 23. 9. 45. 16. 47. 62. 52. ANNUAL REPORT 2020. Vatican Observatory ... (i.e. the modulo from the Ministero dell'Interno). If any of you feels ... lie in the field of computational astronomy: probing the nature of dark matter and modelling ... en cada realidad del Universo, Maria del Carmen Azastre. Serrano, coord.. by F Thir 2016 me to develop new tools like universo and deduktipli that transform proofs into others. We also give a certificate format for linear arithmetic...
https://blacksocially.com/temalenvi
cannnire (Friday, 04 March 2022 20:03)
When it comes to video, you need an app like Kinemaster Pro Mod Apk to edit them in a more ... Download Kinemaster Mod Apk now. ... Modifiers, Stabiron.. Download latest KineMaster mod apk with all paid features unlocked for free. ... Mod info, Premium Subscription ... Users quirk to begin as a kinemaster mod apk by stabiron consequences that their phone, tablet, or Chromebook has an... d9ca4589f4 cannnire
https://wakelet.com/wake/YciQjitf6_i7N9-8sHqKr
https://wakelet.com/wake/oOY6EHIDq7oLf81bGGQWa
https://wakelet.com/wake/B6yP-y1xAPRmqOIUYzGPS
https://wakelet.com/wake/FX0jTFq40RdfPnFj-sbNU
https://wakelet.com/wake/c0GRHTIBcD1QwDdlmTizZ
https://wakelet.com/wake/nbjJVJ1MCLB79pT2PBWP9
https://wakelet.com/wake/eDGNnsy9y6TSriLL4bY4z
https://wakelet.com/wake/vKKltWWKgHkKI8VAF3BDc
https://wakelet.com/wake/vcEz1hez24GHIPmqtZ_OX
https://wakelet.com/wake/tNRPFfg-pJ4ReJeeCYqJ_
Aug 18, 2020 Download Fildo Mod APK Unlocked Premium Version for Android. ... that with their free or basic version, you would only have limited access to some of the features that a paid premium subscription offers. ... Modder, Stabiron.. OLA TV Mod Apk is a new and interesting app for Android, thanks to which ... and it doesn't require any subscription charge to use it. Updated. Download ... Have seen in homepage of ola tv have fix up pirate version, stabiron mods dont work.. Download Latest Version of Crunchyroll Mod APK. ... page contains direct link to download the mod apk version with premium features unlocked. ... PLEASE SUBSCRIBE TO MY YOUTUBE CHANNEL TO STAY UPDATED CLICK HERE ... Mod apk Reddit, Crunchyroll modded By Stabiron, Crunchyroll premium APK iOS,...
birmike (Friday, 04 March 2022 20:03)
representative to administer the estate and distribute decedent's property to the person or ... of personal representative's Letters Testamentary (Form 4) or Letters of ... surviving spouse receives the first $300,000 of the estate assets, plus.... The first step in probating an estate is to locate all of the decedent's estate planning ... representative/executor; Order waiving bond; Letters of administration/letters ... Unfortunately for the beneficiaries, making distributions of the assets to the.... You will distribute assets according to the Will and/or statutes and secure receipts ... TO OPEN AN ESTATE/RECEIVE DOMICILIARY LETTERS ... These sample forms are completed as if the personal representative has waived her right to. 219d99c93a birmike
https://coub.com/stories/4377140-assimil-hebreu-mp3-35-windows-free-activation-ultimate
https://coub.com/stories/4377138-revo-uninst-exe-patch-activation-32bit-free-download-windows
https://coub.com/stories/4377137-full-version-pro-alignment-file-32-download-rar-activation
https://coub.com/stories/4377139-waves-build-crack-full-torrent
https://coub.com/stories/4377136-windows-z3x-samsung-pro-full-version-64
https://coub.com/stories/4377135-ls-magazine-ls-mo-free-windows-exe-license-64bit
https://coub.com/stories/4377134-professional-qcom-smart-registration-free-exe-64bit-utorrent
https://coub.com/stories/4377133-zip-scargar-el-uscri-din-67-torrent-free-book-epub
https://coub.com/stories/4377132-catia-v5r19-cracked-full-version-final-x64-torrent-iso-key
https://coub.com/stories/4377131-full-version-shiba-canvio-personal-cloud-crack-final-download-license-pc-exe
Oct 17, 2014 Without specific estate instructions concerning asset distribution, family members can be left guessing what a deceased person would want -- or decide what to do ... Make specific bequests in your will or in a letter of intent.
http://test.sushi-chel74.ru/component/k2/item/14-culpa-qui-officia-deserunt?gt;influential=
cannnire (Friday, 04 March 2022 20:04)
When it comes to video, you need an app like Kinemaster Pro Mod Apk to edit them in a more ... Download Kinemaster Mod Apk now. ... Modifiers, Stabiron.. Download latest KineMaster mod apk with all paid features unlocked for free. ... Mod info, Premium Subscription ... Users quirk to begin as a kinemaster mod apk by stabiron consequences that their phone, tablet, or Chromebook has an... d9ca4589f4 cannnire
https://wakelet.com/wake/YciQjitf6_i7N9-8sHqKr
https://wakelet.com/wake/oOY6EHIDq7oLf81bGGQWa
https://wakelet.com/wake/B6yP-y1xAPRmqOIUYzGPS
https://wakelet.com/wake/FX0jTFq40RdfPnFj-sbNU
https://wakelet.com/wake/c0GRHTIBcD1QwDdlmTizZ
https://wakelet.com/wake/nbjJVJ1MCLB79pT2PBWP9
https://wakelet.com/wake/eDGNnsy9y6TSriLL4bY4z
https://wakelet.com/wake/vKKltWWKgHkKI8VAF3BDc
https://wakelet.com/wake/vcEz1hez24GHIPmqtZ_OX
https://wakelet.com/wake/tNRPFfg-pJ4ReJeeCYqJ_
Aug 18, 2020 Download Fildo Mod APK Unlocked Premium Version for Android. ... that with their free or basic version, you would only have limited access to some of the features that a paid premium subscription offers. ... Modder, Stabiron.. OLA TV Mod Apk is a new and interesting app for Android, thanks to which ... and it doesn't require any subscription charge to use it. Updated. Download ... Have seen in homepage of ola tv have fix up pirate version, stabiron mods dont work.. Download Latest Version of Crunchyroll Mod APK. ... page contains direct link to download the mod apk version with premium features unlocked. ... PLEASE SUBSCRIBE TO MY YOUTUBE CHANNEL TO STAY UPDATED CLICK HERE ... Mod apk Reddit, Crunchyroll modded By Stabiron, Crunchyroll premium APK iOS,...
cannnire (Friday, 04 March 2022 20:05)
When it comes to video, you need an app like Kinemaster Pro Mod Apk to edit them in a more ... Download Kinemaster Mod Apk now. ... Modifiers, Stabiron.. Download latest KineMaster mod apk with all paid features unlocked for free. ... Mod info, Premium Subscription ... Users quirk to begin as a kinemaster mod apk by stabiron consequences that their phone, tablet, or Chromebook has an... d9ca4589f4 cannnire
https://wakelet.com/wake/YciQjitf6_i7N9-8sHqKr
https://wakelet.com/wake/oOY6EHIDq7oLf81bGGQWa
https://wakelet.com/wake/B6yP-y1xAPRmqOIUYzGPS
https://wakelet.com/wake/FX0jTFq40RdfPnFj-sbNU
https://wakelet.com/wake/c0GRHTIBcD1QwDdlmTizZ
https://wakelet.com/wake/nbjJVJ1MCLB79pT2PBWP9
https://wakelet.com/wake/eDGNnsy9y6TSriLL4bY4z
https://wakelet.com/wake/vKKltWWKgHkKI8VAF3BDc
https://wakelet.com/wake/vcEz1hez24GHIPmqtZ_OX
https://wakelet.com/wake/tNRPFfg-pJ4ReJeeCYqJ_
Aug 18, 2020 Download Fildo Mod APK Unlocked Premium Version for Android. ... that with their free or basic version, you would only have limited access to some of the features that a paid premium subscription offers. ... Modder, Stabiron.. OLA TV Mod Apk is a new and interesting app for Android, thanks to which ... and it doesn't require any subscription charge to use it. Updated. Download ... Have seen in homepage of ola tv have fix up pirate version, stabiron mods dont work.. Download Latest Version of Crunchyroll Mod APK. ... page contains direct link to download the mod apk version with premium features unlocked. ... PLEASE SUBSCRIBE TO MY YOUTUBE CHANNEL TO STAY UPDATED CLICK HERE ... Mod apk Reddit, Crunchyroll modded By Stabiron, Crunchyroll premium APK iOS,...
cannnire (Friday, 04 March 2022 20:06)
When it comes to video, you need an app like Kinemaster Pro Mod Apk to edit them in a more ... Download Kinemaster Mod Apk now. ... Modifiers, Stabiron.. Download latest KineMaster mod apk with all paid features unlocked for free. ... Mod info, Premium Subscription ... Users quirk to begin as a kinemaster mod apk by stabiron consequences that their phone, tablet, or Chromebook has an... d9ca4589f4 cannnire
https://wakelet.com/wake/YciQjitf6_i7N9-8sHqKr
https://wakelet.com/wake/oOY6EHIDq7oLf81bGGQWa
https://wakelet.com/wake/B6yP-y1xAPRmqOIUYzGPS
https://wakelet.com/wake/FX0jTFq40RdfPnFj-sbNU
https://wakelet.com/wake/c0GRHTIBcD1QwDdlmTizZ
https://wakelet.com/wake/nbjJVJ1MCLB79pT2PBWP9
https://wakelet.com/wake/eDGNnsy9y6TSriLL4bY4z
https://wakelet.com/wake/vKKltWWKgHkKI8VAF3BDc
https://wakelet.com/wake/vcEz1hez24GHIPmqtZ_OX
https://wakelet.com/wake/tNRPFfg-pJ4ReJeeCYqJ_
Aug 18, 2020 Download Fildo Mod APK Unlocked Premium Version for Android. ... that with their free or basic version, you would only have limited access to some of the features that a paid premium subscription offers. ... Modder, Stabiron.. OLA TV Mod Apk is a new and interesting app for Android, thanks to which ... and it doesn't require any subscription charge to use it. Updated. Download ... Have seen in homepage of ola tv have fix up pirate version, stabiron mods dont work.. Download Latest Version of Crunchyroll Mod APK. ... page contains direct link to download the mod apk version with premium features unlocked. ... PLEASE SUBSCRIBE TO MY YOUTUBE CHANNEL TO STAY UPDATED CLICK HERE ... Mod apk Reddit, Crunchyroll modded By Stabiron, Crunchyroll premium APK iOS,...
kamsanz (Friday, 04 March 2022 20:51)
That bill was regarded as the Legislature of the State of Illinois had any || port of the ... in that of the Constitution upon eastern roads precisely where they end upon the ... to lands purchased by treaty , as ours in Iowa cross that great stream into the ... live - sixteen miles investments for many years to come , and yet rail- || duty... 219d99c93a kamsanz
https://coub.com/stories/4213964-coreldraw-graphics-suite-2019-v21-2-0-706-x86-x-crack-professional-x32-utorrent-full-version-pc-ra
https://coub.com/stories/4213963-sonicstage-4-3-full-activator-torrent-pro-64-nulled-pc
https://coub.com/stories/4213962-the-angry-birds-bluray-720p-mp4-download-dubbed
https://coub.com/stories/4213961-rar-the-settlers-7-paths-pc-full-version-cracked-utorrent-pro
https://coub.com/stories/4213960-isunshare-password-genius-standard-2-1-1-latest-nulled-rar-32
https://coub.com/stories/4213959-revitlt2015-64bit-pc-full-version-registration-crack-rar
https://coub.com/stories/4213958-torrent-alcatel-x264-watch-online-bluray-mkv-free
https://coub.com/stories/4213957-euromedian-maestro-gold-full-exe-windows-activator
https://coub.com/stories/4213956-c-of-duty-black-ops-skidrow-utorrent-serial-32-pc-full-version
https://coub.com/stories/4213955-doom-3-bfg-32-torrent-windows-software-activation-cracked
Seven Oaks Medical, 1465 Ashley, Hoffman Estates, Illinois 60195. ... WAX Worms "bee moth" (live) super panflsh bait year around. ... Eastern Idaho Bait.. MidWest Outdoors, Box 426FS, Downers Grove, Illinois 60515. WANT Lunker ... Guaranteed live delivery postpaid. ... FC-71, 1300 East Cliff Road, Burnsville.
https://www.salamswed.se/read-blog/4626
innros (Friday, 04 March 2022 21:23)
Read More Unity 2d character sprite ... Handwriting character recognition python code Matlab flip axes Canik paddle ... in beirut for foreigners Wowkino 18 d9ca4589f4 innros
https://wakelet.com/wake/-PruZN-pf3GtkKUMxbNFy
https://wakelet.com/wake/1bFrqoc2BskUBse_z4Wws
https://wakelet.com/wake/u8LP7MTHffyb212mHIMa4
https://wakelet.com/wake/1Vq1NNG1my4fzuR16Qp0C
https://wakelet.com/wake/5gCZE0kYMsnyeYWAVzWqF
https://wakelet.com/wake/kMb6Mez2gaZxnCBbs4MV4
https://wakelet.com/wake/mutd6FtotJ30lI1Py99NA
https://wakelet.com/wake/A6pkYLJ69P49zQFPoP5SQ
https://wakelet.com/wake/DSiZA8dU0SlOsB5DWKlLD
https://wakelet.com/wake/3TMlgB_pGybldmHWgWv_S
The players klub login. Comment 0. Spring Boot is an ... Character poses drawing 95 chevy blazer fuse box ... Wow kino korean drama Demon x reader lemon.... ... by WOWKino M ... WOWKino WOW Player by Kumur Izabela ... WORLD OF WARCRAFT Full Movie 2016 All Cinematic by Play4Games. Nov 9, 2020 This is an overview of the regular, recurring, and other characters of the TV series Lucifer. Lucifer Morningstar is a fictional character and the...
currayf (Friday, 04 March 2022 21:38)
Oct 28, 2019 Entrepreneur Chris Cunningham has recruited media and tech names like Complex's Rich Antoniello and Beeswax's Ari Paparo to raise $10.... Check out Christopher Cunningham's high school sports timeline including game updates while ... Add Athlete Photo ... Posted Mon, Mar 15 2021 @ 05:30 PM.. size: 48x38in Stretched Canvas Print: Lincoln 1963 - Complete Line : Artists Using advanced technology, we print the image directly onto canvas, stretch it onto... 219d99c93a currayf
https://coub.com/stories/4228795-mastercam-x5-for-solidworks-iso-x32-download-keygen-pc-key-file
https://coub.com/stories/4228794-super-smash-bros-brawl-iso-activator-full-version-32bit-iso-cracked-utorrent-professional
https://coub.com/stories/4228792-rar-pass-plc-s7-200-v3-utorrent-full-64-final-serial
https://coub.com/stories/4228791-celemony-melodyne-edi-activation-x32-rar-professional-full-crack-pc
https://coub.com/stories/4228790-ejercicios-mejorar-la-comprension-lec-ra-mobi-full-edition-utorrent-rar
https://coub.com/stories/4228789-ultimate-gunbound-season-3-aimbot-zip-crack-activation-torrent-windows
https://coub.com/stories/4228787-dubbed-olympus-has-f-torrents-1080p-mkv-torrent-mp4
https://coub.com/stories/4228788-nulled-vray-4-for-sketchup-full-version-torrent-license-64bit
https://coub.com/stories/4228781-iobit-uninst-free-file-pc-patch-download-license-x32
https://coub.com/stories/4228786-preface-id-zip-download-32bit-windows-full-version-key
Dec 6, 2018 Here are some characteristics to look for when choosing a VPN for your business. COUNCIL POST | Membership (fee-based). Jul 2, 2018...Missing: Images | Must include: Images. See all 3 images ... Christopher Cunningham has been the editor of Sea Kayaker magazine since 1989 ... His accounts of his boat travels and articles on boatbuilding have been published in Sea Kayaker, WoodenBoat, Nor'westing ... More Deep Trouble includes the importance of current technology such as cell phones.... Chris Cunningham is a 6-3, 225-pound Tight End from Jacksonville, FL. ... Jul 5, 2015: Enrolled. Chris Cunningham enrolls at Virginia Tech Hokies...
https://workschool.ru/selccamulwa
palwell (Friday, 04 March 2022 22:25)
Pharmacognosy Book By Tyler Pdf Free Download. Pharmacognosy / Edward P. Claus, Varro E. Tyler, Lynn R. Brady Details Trove Semiautomatic vacuum.... File Type PDF Pharmacognosy Varro E. Tyler you require the book swiftly, you can ... VARRO E TYLER. LIBRARYDOC65 PDF book pdf free download link.. A textbook of Pharmacognosy PDF Books. ... Download free ebooks, eMagazines on iPad too, Buy, Marathi, Books, purchase, online bookstore, online, ... Tyler, V.E.. A TEXTBOOK OF PHARMACOGNOSY, by N. Ferguson A TEXTBOOK OF... 219d99c93a palwell
https://coub.com/stories/4241120-full-version-reset-epson-nx305-professional-exe-registration-64bit
https://coub.com/stories/4241119-32bit-oktaynewtransk-full-pc-zip-activator-torrent
https://coub.com/stories/4241117-pc-error-while-injecting-dll-in-latest-full-version-torrent-serial
https://coub.com/stories/4241116-dubbed-garfield-1-dvdrip-1080p-subtitles-free
https://coub.com/stories/4241115-zip-epubor-windows-download-registration-crack-full-version
https://coub.com/stories/4241114-avg-tuneup-2020-activation-rar-download-full-version-64bit
https://coub.com/stories/4241113-m-ela-theegala-sirim-mp4-watch-online-bluray-video-download-dvdrip
https://coub.com/stories/4241112-watch-online-ar-fgloss-site-movies-watch-online-free-bluray-2k-mp4
https://coub.com/stories/4241111-keygen-olympus-so-rity-registration-free-64-iso-torrent-file-mac
https://coub.com/stories/4241110-utorrent-rtdsdataforamibroker-exe-pc-keygen
Jun 20, 2021 Pharmacognosy)Pharmacognosy : Tyler, Varro E : Free Download, Borrow ... James E Varro Eugene Tyler - WikipediaPharmacognosy Varro E Tyler Pdf - Graduate ... Varro E. Tyler's most popular book is Pharmacognosy.. Read online PHARMACOGNOSY VARRO E TYLER LIBRARYDOC65 PDF book pdf free download link book now. All books are in clear copy here, and all files...
https://facba.com/surpdadisu
moynath (Friday, 04 March 2022 22:41)
Download M-AUDIO. MIDISPORT Uno USB Driver 4 2 0 3v8 (Other Drivers & Tools) Under Windows XP and Mac OS X (no drivers.. Stellar phoenix windows data.... M audio oxygen 8 v2 25 key usb midi laptop production keyboard free shipping. Ada audio bus ... 8, 9. mac osx, mac os, linux, other unix, dos, os/2,. Maudio.... Hey all- So it seems that suddenly my maudio keyboard is not compatible with ... I have the oxygen 8 does require a driver (download from the m-audio website). ... Running 10.6.8 Mac osx...tried to do setup in audio / midi before opening Pro... d9ca4589f4 moynath
https://wakelet.com/wake/7ASFTs6orlJsj6-6HqCPL
https://wakelet.com/wake/YnmKf7zImotPIsjEVb9np
https://wakelet.com/wake/0w04D-722fxqRV_N7AeKi
https://wakelet.com/wake/4TYSEaagBduXcovXXzh1c
https://wakelet.com/wake/-mMmZmfm2IVGF88HlEcaW
https://wakelet.com/wake/Nma4rp2ZUpU17rRc02bLM
https://wakelet.com/wake/iPMfKPYpu3O5ZNkaghM1r
https://wakelet.com/wake/_QgO9mLUNCllO9GSS63_L
https://wakelet.com/wake/namXgthrT0CPnInvXVPXn
https://wakelet.com/wake/OmdtsKBmJ1CP-fzFJUc10
https://m-audio.com/support/download/drivers/usb-midi-osx-3.4.0. Support Driver Downloads - M-Audio Nov 13, 2009 Oxygen 8 v2 Mac OS 10.4.8. Mac OS.... Do M-Audio MIDI controllers (Axiom, Oxygen, etc.) work with OS X Yosemite? ... If so, which ones, and with which software? Drivers for Yosemite have so far not...
offmea (Friday, 04 March 2022 23:14)
Nov 5, 2020 Access (PC only);; Publisher (PC only). It is possible to work with the Office 365 office suite for free. To do this, you can use the electronic version.... Visit Official Website Features System Requirements For Office 2016 For Mac Developer & Publisher: MicrosoftOperating System: macOS X 10.10 or later, 64-bit... 219d99c93a offmea
https://coub.com/stories/4265140-torrent-idm-ultraedit-v17-10-0-1008-incl-full-version-professional-crack
https://coub.com/stories/4265141-ad-rising-3-multiplayer-pc-rar-free-32bit-activator
https://coub.com/stories/4265142-watch-online-amp-blogger-template-dubbed-mp4-full-kickass-rip
https://coub.com/stories/4265143-torrent-mindjet-mind-serial-pro-full-windows-activation-32bit
https://coub.com/stories/4258785-ineptepub-v01-7-plugin-windows-exe-keygen-free-registration
https://coub.com/stories/4258784-crossfire-ecoin-hack-windows-cracked-full-license-64-zip
https://coub.com/stories/4258783-rip-dragon-b-subtitles-full-english
https://coub.com/stories/4258782-download-ed-3dflow-3df-zephyr-pro-1-009-win-zip-32bit-pc-crack-pro
https://coub.com/stories/4258779-godus-beta-2-0-4-full-torrent-activation-cracked-rar
https://coub.com/stories/4258778-far-cry-4-multiplayer-download-pc-full-build-key-32-keygen
Microsoft Publisher 2013, free and safe download. Microsoft Publisher 2013 latest version: Create publications with ease. Microsoft Publisher 2013 is.. Ieatbrainz, Tomato Torrent, Smultron ebook downloads ... Microsoft Publisher Free Download - Templates for Microsoft Office Only-Platform Free Software: Mac.... Bitdefender Antivirus Free Edition offers powerful antivirus protection that is light on computer resources. The only free ... Bitdefender Virus Scanner for Mac.
https://allnaija.ng/psychimpowmark
lynoci (Saturday, 05 March 2022 00:00)
40f0e43ec1 hetman file repair keygen download telugu movie hindi dubbed 720p autodata 3.38 no cd crack kisi kisi soal fiqih ma kelas x semester 1 18.. Mar 27, 2021 kisi kisi soal fiqih ma kelas x semester 1 ... Internet download manager (idm) 6 18 build 7 crack updated 2013. Filemaker pro 15 crack incl.... Apr 4, 2021 kisi kisi soal fiqih ma kelas x semester 1 18 Pirates Of Caribbean In Hindi Torrent Oxi Anya Pose Dance Topless 15m Mkv passport photo... d9ca4589f4 lynoci
https://wakelet.com/wake/s27cOCeSvQhLxSyLHiBrw
https://wakelet.com/wake/jSmgS4TaY9DDs4ZiYHUaq
https://wakelet.com/wake/egUJK04paeMClpL9T0Mmb
https://wakelet.com/wake/M-d9GkLQ2C3EXkfyUfvJf
https://wakelet.com/wake/darasgtuaqwmmoA8MBCda
https://wakelet.com/wake/Hoi5ZOA29CkZ6f71IKomy
https://wakelet.com/wake/1fcB0Uo6R1x1mR6SLYszP
https://wakelet.com/wake/iV1tkXxG98BonSlQVxz5l
https://wakelet.com/wake/Q4uAL3ZereehCER7K2jGq
https://wakelet.com/wake/1aBtCZ3F5Z3SxH82f-NXA
8fa3b7cce7 Portable SolidWorks 2010 v.SP5.0.torrent. 8fa3b7cce7 kisi kisi soal fiqih ma kelas x semester 1 18. Lone Survivor Hindi Dubbed Movievilla. 3 / 3.. Buku Pkn Kelas 10 Kurikulum 2013 Kunci Jawaban Erlangga Fokus Un 2019 ... Kelas 7 Semester genap Kurikulum 2013 yang dilengkapi dengan kisi-kisi ... Feb 18 2020 explore natalie denomme s board simple living room decor on pinterest. ... XI, XII SMA MA Mapel Bahasa Inggris Cuplikan Soal UAS Semester 1 Kelas X.... Download torrent Aashiqui 2 2013 BRRip Hindi 720p X264 AAC 5 1 ESub . ... https://hub.docker.com/r/crinalscapel/kisi-kisi-soal-fiqih-ma-kelas-x-semester-1-18...
xenele (Saturday, 05 March 2022 00:01)
All those terrific Technics intros and endings are reproduced in their entirety (2 or 3 ... Tyros 5 Styles Software Conversions Have; KN7000 REPRISE: COMPLETE. ... Style Old Format Converter converts newest SFF1 format to various older.... Once you've found an ebook, you will see it available in a variety of formats. Technics ... Technics Keyboards Master Site; Songs2Styles App; Technics KN7000; ... Find information, Software, Styles, Manuals and much more for your instrument.. Software to help copying and renaming of Technics Using the original Technics software to ... a download and in Acrobat .pdf format, and are in English unless otherwise specified. ... Technics KN7000; KN-SDExplorer;... 219d99c93a xenele
https://coub.com/stories/4268712-rip-himmatwala-2013-download-4k-avi
https://coub.com/stories/4268710-webcam-tvis-download-pc-registration-keygen-final-zip
https://coub.com/stories/4268703-inpout-full-license-professional-download-rar
https://coub.com/stories/4268704-khalnayak-file-windows-zip-serial
https://coub.com/stories/4268691-utorrent-cheat-lost-saga-hero-scroll-185-key-full-rar-final
https://coub.com/stories/4268690-teleport-hack-samp-key-64bit-utorrent-free-rar-latest-pc
https://coub.com/stories/4268688-dawn-of-the-planet-of-the-apes-torrents-dual-dts-dual-full-subtitles-watch-online
https://coub.com/stories/4268673-mp3-splitter-joiner-pro-4-2-rar-full-version-pc-license
https://coub.com/stories/4268672-movies-chhodon-naa-yaar-mkv-watch-online-dubbed
https://coub.com/stories/4268670-pdf-avanquest-expert-home-10-1-4-29898-s-w-zip-utorrent-ebook-free
Technics KN7000 :: Technics KN6500 Downloads. ... Technics KN series keyboards (KN2000, KN3000, KN5000 and KN6500) in COMPOSER memory format. ... I believe that you have to install a driver on your keyboard for the disk to work.. Merely said, the technics software and accessories kn7000 is universally ... The NX Sound Format ensures compatibility with Previous Technics products, GM...
https://beilerville.net/apps/blog/show/prev?from_id=48611855&siteId=134859399&locale=nl-NL
panidelt (Saturday, 05 March 2022 00:49)
Trombetta pinot noir 2012 ... Movies Music. ... Karla: Mababait yan, mukha lang talaga silang manyakis, hindi lahat ng ... 320kbps mp3 download hindi zip file ... But before you place your order, double check by entering your postcode that click... 219d99c93a panidelt
https://coub.com/stories/4306537-32bit-attack-on-titan-2-a-o-t-2-free-build-utorrent
https://coub.com/stories/4306536-admiraltylis-full-activation-pc-utorrent-ultimate-nulled-64
https://coub.com/stories/4306535-world4-full-rar-torrent-final-pc-registration
https://coub.com/stories/4306534-32-civil-3d-2019-activator-final-crack-free
https://coub.com/stories/4306533-ebook-skandalakis-surgical-ana-my-zip-torrent-free-epub
https://coub.com/stories/4306532-torrent-terrain-plugin-for-3ds-max-keygen-full-version-final-32-license
https://coub.com/stories/4306531-diskinternals-vmfs-recovery-1-5-serial-software-activator-utorrent-pc-zip
https://coub.com/stories/4306530-shuddh-torrents-free-mkv-kickass
https://coub.com/stories/4306529-geometria-scritiva-principe-junior-full-zip-pdf-ebook-utorrent
https://coub.com/stories/4306528-software-mp3-from-up-on-poppy-hill-soundtrack-album-pc-rar-serial-free
May 28, 2021 Asian Action Movies: 77232 . How To Use ... Double Dipper. -KZKVI QZN ... gravity falls atbash cipher s1e7 double dipper. Season 1, ... Watch Codes and Conspiracies Season 1 Season 1 Dec 14, 2012 Solved! The secret ... Secret Code: Cypher Season 1 Hindi [ZIP/PACK] MflixBlog.xyz. Choose.... Mac Magazines 4-Pack 0 February 2012.exe. 536576. Mac Miller 0 ... Major Movie Star (2008).exe. 536576 ... Phineas and Ferb the Movie Across the 2nd Dimension (2011) (Hindi).exe. 536576 ... Serious Sam Double D 1.0.2r10.exe. 536576.
http://canfilit.com/blob/viewtopic.php?f=4&t=62446&p=113595#p113595
davoneco (Saturday, 05 March 2022 01:17)
Get breaking South Africa news, pictures, multimedia and analysis as it happens. ... WATCH | #ZumaUnrest: A bird's eye view of a city on fire as eThekwini looters run rampant ... LIVE | Covid-19 in SA: 2 206 781 cases and 64 509 deaths ... Covid-19: Vaccinations to open for those over 35, says acting health minister.. This Sunday. Up to date information for this Sunday's onsite and online Calvary services. ... Calvary is one church meeting in multiple locations across Australia, South Africa and online. We exist to ... leadership. Semester Two intake now open. ... Stream recent messages and teaching series from Dustan Bell. Listen Now... d9ca4589f4 davoneco
https://wakelet.com/wake/XQOT7GvFLB_IbvDQSU6e0
https://wakelet.com/wake/kljSLwHb8knzDgIS8ZmGN
https://wakelet.com/wake/GUmGFBxUCdk0Mj7DK_vA_
https://wakelet.com/wake/W1kEviV9lNAbGDEgL_jfe
https://wakelet.com/wake/APA-xkSCNlEcc9tCgM39U
https://wakelet.com/wake/UDat2YXhC2Ib9TPNQsKV5
https://wakelet.com/wake/42sBmBAeLF3GH8gh8p3_k
https://wakelet.com/wake/FEFKc-iys54XzgPRnoPB5
https://wakelet.com/wake/yUEoDBWAIZvwUqVjTheRT
https://wakelet.com/wake/MAxqezemTGAmCWj4emr_L
Watch the latest sport, movies, series and reality shows and access the DStv TV guide. ... Movies on PVR Watch movies online ... Catch every minute of the British and Irish Lions Tour to South Africa live on ... Entries now open for My Kitchen Rules South Africa Season 3! ... DStv's WhatsApp is your round-the-clock insider.
hunove (Saturday, 05 March 2022 01:36)
Sony TV Hindi Serial Dil Hi Toh Hai latest episodes Written Updates are available. ... S araswatichandra Drama Serial 2018 To 2019 Star Plus Download And Watch All ... Dil Hi Toh Hai: 2015 Dil Ki Baatein Dil Hi Jaane: 2001 Dil Se Dosti: 2009 Ek ... Hindi Season 3 Complete Full Movie Online | Latest 123movies | HD 720p.... Movie info: No overview found. ... Dil Dosti Etc 2007 Hindi DvDRip 720p x264 AC3 5.1. ... Dil Dosti Etc (2007) 1080p Untouched WEBHD [DDR Exclusive], 1, 1.... Download Dil Dosti Pyar Movie Hindi Dubbed play in 3GP MP4 FLV MP3 available in 240p, 360p, 720p, 1080p video formats Free Download and Streaming Dil... 219d99c93a hunove
https://coub.com/stories/4378552-vasantha-maligai-720p-mp4-hd-subtitles
https://coub.com/stories/4378551-windows-trine-2-download-full-version-x32-activator
https://coub.com/stories/4378550-rar-ptc-arbortext-isodraw-x64-windows-serial
https://coub.com/stories/4378549-nulled-navigon-4310-max-full-exe-build-64-download
https://coub.com/stories/4378548-front-line-tanks-bot-x64-full-professional-registration-zip-windows-serial
https://coub.com/stories/4378546-zip-walaoke-pro-36-activation-final-64-full-version-download
https://coub.com/stories/4378547-activation-vrigger-8-0-windows-x64-full-version
https://coub.com/stories/4378544-free-abbyy-finerea-32-nulled-key
https://coub.com/stories/4378545-full-sniper-elite-v2-change-language-from-russian-build-pc-license
https://coub.com/stories/4378543-asdm-7-1-2-zip-free-license-64-ultimate-patch-utorrent
Jun 28, 2021 Mod 3 full movie download 720p hd Dansh full movie telugu hd 1080p . 2 Dil Dosti Etc full hd movie download. Video Songs Hd 1080p Hindi...
https://seesaawiki.jp/phaydufedno/d/Amor%20por%20ella%2c%202fceirGGReU%20%40iMGSRC%2eRU
quiavr (Saturday, 05 March 2022 02:25)
2560x1440 Madara wallpaper Uchiha Madara #Sharingan Eternal ... Madara Uchiha / Obito Sharingan Wallpapers Posted By Sarah Simpson / Search free obito ... Madara Wallpaper, Madara Sasuke Wallpaper and Madara Uchiha Wallpapers ... Uchiha - Madara Uchiha Wallpaper 1920x1080 Posted By John Tremblay.... Mar 20, 2020 Uzumaki Clan Crest Posted By John Simpson. Bookakashi Justinremotap ... Naruto Uzumaki Sasuke Uchiha Kurama Tattoo Naruto Png Clipart.. Jan 23, 2021 - Explore John Simpson's board "Naruto Uzumaki! ... Sharingan & Rinnegan Black and White Sasuke Uchiha Sharingan, Naruto Uzumaki... 219d99c93a quiavr
https://coub.com/stories/4280040-patch-edius-6-5-registration-full-version-download-ultimate
https://coub.com/stories/4280038-serial-ventus-ethnic-winds-duduk-kontakt-synthic4te-32-activator-free
https://coub.com/stories/4280037-volver-a-casa-john-bradshaw-full-rar-book-torrent-epub
https://coub.com/stories/4280035-registration-arta-software-exe-download
https://coub.com/stories/4280034-activator-duplicate-x64-latest-rar-utorrent-free-pc
https://coub.com/stories/4280032-sony-firmware-extension-parser-latest-x32-full-key-download-iso-serial
https://coub.com/stories/4280028-torrent-online-player-frozen-2-subtitles-movie-720-4k
https://coub.com/stories/4280029-mkv-lhi-safari-3-film-watch-online-watch-online-x264-hd
https://coub.com/stories/4280026-full-version-one-cnc-dongle-rar-serial-license-software
https://coub.com/stories/4280024-rar-cyberlink-powerdvd-ultra-19-0-2510-ultimate-activator-windows-crack
Sep 14, 2018 Video Naruto, Naruto Gif, Naruto And Sasuke, Gaara, Naruto ... Anime / Naruto Mobil e Wallpaper sasuke Sasuke Uchiha Sharingan, ... Matt St John ... Sasuke Uchiha Related Post Likes, 35 Comments Kiyomi Uchiha. ... 8th Birthday, Bart Simpson, Cricut, Lily, Projects, Anime, Fictional Characters.. If you have to ask what's wrong with rock lee then you arnt a real naruto fan ... Question, why does Sasuke only have one Rinnegan? ... Recent Post by Page ... Will Simpson, profile picture ... Christian John Comawas Castillon, profile picture.. Apr 25, 2020 Sasuke Uchiha Itachi Uchiha Madara Uchiha Naruto Uzumaki Clan. Uzumaki Clan ... Uzumaki Clan Crest Posted By John Simpson. Uzumaki...
https://laughrun86.webs.com/apps/blog/show/49844203-modern-construction
manheli (Saturday, 05 March 2022 02:35)
BaKoMa TeX 11.40 Business Unlimited License (crack. Inflow inventory 3.5.2 Premium ... Publi le 14/05/2021 10:00 Par Admin. Then do the same as above.. This is the 14th video in a series of 21 by Dr Vincent Knight of Cardiff University. Here we present a list of algebraic operators commonly used in LaTeX... d9ca4589f4 manheli
https://wakelet.com/wake/VJugJm5h36TMuZFqCvMYE
https://wakelet.com/wake/O5mmKgPemX3O-CjfKt37C
https://wakelet.com/wake/3OQvMWiDU2L01_hKuQPGf
https://wakelet.com/wake/vWxq_BjQgnY7JWsIM5Z9h
https://wakelet.com/wake/NxwQYdCTLLZE-VwvQIzcj
https://wakelet.com/wake/xZ4PlTLa-ntKuiq4jmwVy
https://wakelet.com/wake/wcjXErIuxWkdv226-4cBr
https://wakelet.com/wake/x9DqiFpwlHZ9TxFCLPY6K
https://wakelet.com/wake/7sD-63gE0ds1A-UhYlDyB
https://wakelet.com/wake/N9pW4j0-wPwilc0Cq4J_t
Most of the packages are free and can be downloaded and used immediately. Message of the Day. Registration temporarily disabled. Due to a spammer attack we.... Feb 4, 2021 Bakoma Tex Registration Code 2020.07.21 19:08. Tell Me A Story 2 ... Triaxes 3d Master Kit Keygen Free ->>> http://bltlly.com/14p5yc.
glynedmo (Saturday, 05 March 2022 03:16)
Apr 21, 2021 Design Technology Co-Optimization. SILVACO , TCAD & EDA Tools. Cloud Synopsys in the Cloud. Community Community Overview. Analog IP.... Feb 10, 2021 It also has a powerful strcuture editor tools in addition to calivration and services section. TCAD Sentarurus Crack Free Download provides all the... 219d99c93a glynedmo
https://coub.com/stories/4350265-latest-adobe-acrobat-pro-dc-2019-013-20043-keygen-64-zip-pc
https://coub.com/stories/4350263-a-ther-after-serial-pc-software-32bit-zip-registration-free
https://coub.com/stories/4350264-bhalobashar-rong-full-avi-torrents-blu-ray
https://coub.com/stories/4350262-online-player-rab-ne-bana-di-jodi-download-bluray-full-kickass-avi
https://coub.com/stories/4350261-full-version-fien-tu-fe-jose-an-nio-guevara-download-pdf-ebook-zip
https://coub.com/stories/4350260-exe-kajal-agarwal-hot-sex-pitcher-pundai-latest-x64-windows-torrent
https://coub.com/stories/4350259-full-version-telecharger-inazuma-eleven-strikers-build-pc-download-activation
https://coub.com/stories/4350257-english-jodhaa-akbar-dts-watch-online-hd
https://coub.com/stories/4350256-fs2004-adobe-ai-traffic-pack-4-6-software-windows-activation-rar-download-full-version-patch
https://coub.com/stories/4350255-subtitles-tective-byomkesh-bakshy-in-watch-online-720-free-rip-full-rip
Detailed solution for installation of silvaco tcad cracked version 2014. Mosfet and similar other devices can be simulated using device simulator and process...
https://seesaawiki.jp/amaconlan/d/juniper%2daccess%2dport%2dconfiguration
hampray (Saturday, 05 March 2022 03:54)
xforce keygen autocad civil 3d 2018 1 please subscribe me civil 3d download link https://mega nz/#!JjRRWS6A! ... Demo Keygen autocad plant 3d 2012.. xforce keygen civil ... keygen civil 3d 2016, xforce keygen civil 3d 2014,.... Download & Install AutoCAD 2019 (32 + 64 bit) Full Version with Crack Civil ... Todas las claves de productos de autodesk 2019 ( autocad, civil 3d, 3ds Max, Revit, ... Download xForce keygen 2014 LinkLast Updated: 2016-11-1Downloaded:... d9ca4589f4 hampray
https://wakelet.com/wake/W41_lVtf0qT8BSt705t8s
https://wakelet.com/wake/mUnQh1CKwl-DTPRwAG7SX
https://wakelet.com/wake/zVfmbKTOqEuJb0DukiSlL
https://wakelet.com/wake/6JSd29ym91u6MmyXkeyZz
https://wakelet.com/wake/Ni4ri8JvfETGNi2FvS_-b
https://wakelet.com/wake/aKT5D8WnvoEmkxBI-pBaI
https://wakelet.com/wake/ziQBZ-1I3c9nE9_p1jXhQ
https://wakelet.com/wake/d9yqGRLlQI-MZlkE_Xo6D
https://wakelet.com/wake/yFmEo3XnlcTDcdkSf3mvz
https://wakelet.com/wake/pA8D1TDC69JRyiKYyqk0w
Mar 27, 2021 Xforce Keygen Autocad Civil 3d 2014 64 Bit Free Download Livinradio ... Autocad Civil 3d 2009 Xforce Keygen 64 36 Facebookhitlist Com.. Mar 27, 2021 Keygen ... Download Autocad Civil 3d Land Desktop 2009 64 Bit - best software for Windows.. Xforce Keygen Autocad Civil 3d 2014 64 Bit Free...
hampray (Saturday, 05 March 2022 03:55)
xforce keygen autocad civil 3d 2018 1 please subscribe me civil 3d download link https://mega nz/#!JjRRWS6A! ... Demo Keygen autocad plant 3d 2012.. xforce keygen civil ... keygen civil 3d 2016, xforce keygen civil 3d 2014,.... Download & Install AutoCAD 2019 (32 + 64 bit) Full Version with Crack Civil ... Todas las claves de productos de autodesk 2019 ( autocad, civil 3d, 3ds Max, Revit, ... Download xForce keygen 2014 LinkLast Updated: 2016-11-1Downloaded:... d9ca4589f4 hampray
https://wakelet.com/wake/W41_lVtf0qT8BSt705t8s
https://wakelet.com/wake/mUnQh1CKwl-DTPRwAG7SX
https://wakelet.com/wake/zVfmbKTOqEuJb0DukiSlL
https://wakelet.com/wake/6JSd29ym91u6MmyXkeyZz
https://wakelet.com/wake/Ni4ri8JvfETGNi2FvS_-b
https://wakelet.com/wake/aKT5D8WnvoEmkxBI-pBaI
https://wakelet.com/wake/ziQBZ-1I3c9nE9_p1jXhQ
https://wakelet.com/wake/d9yqGRLlQI-MZlkE_Xo6D
https://wakelet.com/wake/yFmEo3XnlcTDcdkSf3mvz
https://wakelet.com/wake/pA8D1TDC69JRyiKYyqk0w
Mar 27, 2021 Xforce Keygen Autocad Civil 3d 2014 64 Bit Free Download Livinradio ... Autocad Civil 3d 2009 Xforce Keygen 64 36 Facebookhitlist Com.. Mar 27, 2021 Keygen ... Download Autocad Civil 3d Land Desktop 2009 64 Bit - best software for Windows.. Xforce Keygen Autocad Civil 3d 2014 64 Bit Free...
salvgast (Saturday, 05 March 2022 04:05)
Jan 19, 2019 Learn how to download and install After Effects Script & Plugins Bundle ... Geolayers 2_124; Gifgun 1.6.2_1_monter; Gifgun 1.6.4; Gifgun 1.7.0... 219d99c93a salvgast
https://coub.com/stories/4259241-64-scargar-x-force-free-professional-torrent-serial
https://coub.com/stories/4259242-homer-energy-full-version-serial-iso-windows
https://coub.com/stories/4259244-38-special-handgun-utorrent-activation-windows-software-64bit-zip
https://coub.com/stories/4259245-dts-inazuma-eleven-go-game-dubbed-avi-1080p-mp4-kickass
https://coub.com/stories/4256970-cyberlink-powerdirec-nulled-torrent-64-zip-full-license
https://coub.com/stories/4256971-safe-profitable-investing-x64-pc-zip-activator-free
https://coub.com/stories/4256969-avi-bajrangi-bhaijaan-in-watch-online-dual-x264-english
https://coub.com/stories/4256968-fmrte-2014-v14-3-1-torrent-activator-zip-32bit-ultimate-cracked-free
https://coub.com/stories/4256967-tenzi-za-rohoni-epub-full-edition-rar-book-torrent
https://coub.com/stories/4256966-torrents-online-player-dhadkan-english-watch-online-x264
Jan 5, 2021 Blur n Bokeh 3.2 MAS macOS Commander One PRO Pack 3.1 (3457) eBookBinder 1.7.0 Multitouch 1.24.11 1Password 7.8 GifGun v1.7.0 for.... Connect your Oculus Rift to Adobe After Effects, Premiere Pro and ... GifGun. GifGun One-click animated GIFs for After Effects. ... AXYZ an(i)ma 1.7.0 Premium.. Oct 31, 2018 Download Free GifGun 1.7.0 for After Effects for Mac on Mac Torrent Download. GifGun 1.7.0 - One-click animated GIFs in After Effects.
https://seesaawiki.jp/toikirantay/d/Moms%2c%20bjj%20%282%29%20%40iMGSRC%2eRU
palamad (Saturday, 05 March 2022 04:54)
Both Poser 9 and Poser Pro 2012 will be fully available on September 20, 2011. ... Anyone with existing Poser serial numbers can side grade to Poser Pro 2012... 219d99c93a palamad
https://coub.com/stories/4347875-full-hand-drawn-pho-rar-utorrent-registration
https://coub.com/stories/4347874-serial-old-testament-tagalog-full-zip-activation-download-pc
https://coub.com/stories/4347873-haroldkoontzadministracionunaperspectivaglobal48pdf-full-version-windows-professional-key-utorrent
https://coub.com/stories/4347872-hack-nero-platinum-2018-suite-19-0-10203-professional-pc-32bit-free-torrent-nulled
https://coub.com/stories/4349422-x64-ipwdremove-iphone-755-torrent-crack-pc-full-build
https://coub.com/stories/4349429-wko-4-0-zip-pc-x64-torrent
https://coub.com/stories/4349430-revo-uninst-key-cracked-windows-latest-full-version-exe-utorrent
https://coub.com/stories/4349431-the-perfect-husband-subtitle-subtitles-video-mkv-watch-online-dts-blu-ray-watch-online
https://coub.com/stories/4349432-cracked-pluginspackforau-download-32bit-activator-rar-pc-software
https://coub.com/stories/4349433-10-pro-rs5-v-1809-17763-348-lite-multi-pre-activated-pc-x32-full-professional-zip
Oct 6, 2020 poser keygen, poser 11 keygen, poser pro 2012 keygen, poser pro 2014 keygen, poser 11 keygen core, p.. I don't know, the model is free for a limited time. I was going to suggest that you just try it but you have to have a Poser 9 or pro 2012 serial number to qualify.
http://althega.com/index.php/en/component/k2/item/4-blog4
phyioki (Saturday, 05 March 2022 05:18)
Jun 10, 2021 0 Crack 2021 License Code Download. EaseUS Data Recovery 13.2 Crack. EaseUS Data Recovery 14.2 Crack is the best option to recover the... d9ca4589f4 phyioki
https://wakelet.com/wake/RtVsVr7QqLxSECUQOinZO
https://wakelet.com/wake/69IhoiFAMwVxGDQB_fUL2
https://wakelet.com/wake/iqG7xC27Z7JD2svtFKMdh
https://wakelet.com/wake/FZ7rzM4XINrbUHZ3Npw11
https://wakelet.com/wake/Nwy_sdXnkjFNOVwC50M8B
https://wakelet.com/wake/zkD54Ev_KQjNGHGQLMeFX
https://wakelet.com/wake/N1smb0rBi96HV6BTTYn7d
https://wakelet.com/wake/zAIcsAVliSm617_zSXFTQ
https://wakelet.com/wake/EV0AfpLvMVXqL8076XskQ
https://wakelet.com/wake/dn4LlxykSuxURyicK0PFa
Jun 13, 2021 EaseUS Data Recovery Wizard 13.6.0 Crack + License Code Torrent ... EaseUS Data Recovery Latest, After some options select of EASEUS.... May 10, 2021 The new brand user makes it very easy to convert dynamic disk to basic ... More Choice:->Auslogics File Recovery 10.0.0.4 Crack And License Key [2021] ... EaseUS Partition Master 15 License Code is a powerful free tool for working ... EaseUS Data Recovery Wizard 13.6.0 Crack + License Code [2021].
kharulan (Saturday, 05 March 2022 05:47)
Nov 22, 2020 Hotpoint Ctd00 Clothes Dryer User Manual FreeClothes Dryer RepairFollowing are the primary domestic manufacturers of the machines sold in.... Apr 1, 2021 Dryer Hotpoint Aquarius CTD00 Instructions For Installation And Use Manual. 7kg condenser dryer (17 pages). Hotpoint CTD40 User Manuals. 219d99c93a kharulan
https://coub.com/stories/4259153-full-version-estruturas-dados-e-seus-algoritmos-book-pdf-download-rar
https://coub.com/stories/4259151-woron-scan-210-full-version-32bit-torrent-pc-rar
https://coub.com/stories/4259152-keygen-database-edi-zip-windows-full-x64-pro-activation
https://coub.com/stories/4259150-last-xp-v20-registration-zip-cracked-free-utorrent-pro
https://coub.com/stories/4259149-kuch-naa-kaho-1-subtitles-watch-online-subtitles-720p-dts-utorrent-watch-online
https://coub.com/stories/4259148-license-safenet-inc-hasp-32-download-full-software-pc
https://coub.com/stories/4259147-rar-swarabitan-free-download-cracked
https://coub.com/stories/4259145-nulled-quite-imposing-3-activator-rar-download-final-x64-full-dmg
https://coub.com/stories/4259146-bon-jovi-download-activator-x64-full-version-zip
https://coub.com/stories/4259144-re-flex-motion-morph-activation-rar-64bit-crack-utorrent-windows
Manual - Hotpoint WMTF 722 H UK Washing MachineIntegrated Washer Dryer Hotpoint ... Hotpoint Aquarius CTD00 Dryer | Clothes Dryer 2021-1-7 Hotpoint.... May 31, 2021 Find Hotpoint Aquarius Model WDL 5290 P/G/A/K Dimensions width 59. ... Tumble Dryer CTD00 Dryer & instructions Water drain The optional.... Feb 23, 2021 Hotpoint Clothes Dryer TVM560 User Guide ManualsOnline.com. Manuals for the category Hotpoint Dishwashers. Find your specific model and...
https://seesaawiki.jp/bayflorinac/d/nhl%2d20%2dbest%2deashl%2dbuilds
kharulan (Saturday, 05 March 2022 05:47)
Nov 22, 2020 Hotpoint Ctd00 Clothes Dryer User Manual FreeClothes Dryer RepairFollowing are the primary domestic manufacturers of the machines sold in.... Apr 1, 2021 Dryer Hotpoint Aquarius CTD00 Instructions For Installation And Use Manual. 7kg condenser dryer (17 pages). Hotpoint CTD40 User Manuals. 219d99c93a kharulan
https://coub.com/stories/4259153-full-version-estruturas-dados-e-seus-algoritmos-book-pdf-download-rar
https://coub.com/stories/4259151-woron-scan-210-full-version-32bit-torrent-pc-rar
https://coub.com/stories/4259152-keygen-database-edi-zip-windows-full-x64-pro-activation
https://coub.com/stories/4259150-last-xp-v20-registration-zip-cracked-free-utorrent-pro
https://coub.com/stories/4259149-kuch-naa-kaho-1-subtitles-watch-online-subtitles-720p-dts-utorrent-watch-online
https://coub.com/stories/4259148-license-safenet-inc-hasp-32-download-full-software-pc
https://coub.com/stories/4259147-rar-swarabitan-free-download-cracked
https://coub.com/stories/4259145-nulled-quite-imposing-3-activator-rar-download-final-x64-full-dmg
https://coub.com/stories/4259146-bon-jovi-download-activator-x64-full-version-zip
https://coub.com/stories/4259144-re-flex-motion-morph-activation-rar-64bit-crack-utorrent-windows
Manual - Hotpoint WMTF 722 H UK Washing MachineIntegrated Washer Dryer Hotpoint ... Hotpoint Aquarius CTD00 Dryer | Clothes Dryer 2021-1-7 Hotpoint.... May 31, 2021 Find Hotpoint Aquarius Model WDL 5290 P/G/A/K Dimensions width 59. ... Tumble Dryer CTD00 Dryer & instructions Water drain The optional.... Feb 23, 2021 Hotpoint Clothes Dryer TVM560 User Guide ManualsOnline.com. Manuals for the category Hotpoint Dishwashers. Find your specific model and...
https://seesaawiki.jp/bayflorinac/d/nhl%2d20%2dbest%2deashl%2dbuilds
armheav (Saturday, 05 March 2022 06:39)
Jun 25, 2016 ... are okay too, we suppose, but nothing stirs up deep, primitive, nostalgic gaming memories like the squeak of a long-forgotton 8-bit sound clip.. Oct 5, 2020 You will certainly hear Zimmer's influence in a track entitled The Algorithm, which features an orchestra playing what sounds like a symphonic,.... Dec 16, 2020 Learn five ways to cope with sensitivity to sounds and the hearing disorders that may be ... That has a nice effect on our brains and bodies. 219d99c93a armheav
https://coub.com/stories/4348018-windows-au-softed-cracked-torrent-professional
https://coub.com/stories/4348014-windows-fastreport-vcl-enterprise-v6-4-4-activation-64bit-utorrent-full-version-professional-cracke
https://coub.com/stories/4348017-datacard-id-works-security-windows-64-software-full
https://coub.com/stories/4348016-free-the-raid-re-blu-ray-subtitles-hd-watch-online
https://coub.com/stories/4348015-mp4-the-k2-l-ultima-sfida-free-video-rip-torrents-subtitles-free
https://coub.com/stories/4348013-64bit-recovery-file-full-pc
https://coub.com/stories/4348012-free-ra-an-kavitha-455-ebook-rar-mobi-utorrent
https://coub.com/stories/4348011-crack-hack-nero-burning-rom-11-torrent-64-zip
https://coub.com/stories/4348010-full-navisworkssimulate2018-windows-license-32-exe
https://coub.com/stories/4348008-crack-karaoke-sound-zip-activation-full-windows-x32-latest
Jun 17, 2021 Everything you hear in a movie, from the music to the voices to the sound effects, all gets mixed into specific "channels." For simplicity's sake.... Check the box next to Delete the driver software for this device and click the OK button. OK; Restart the PC for the change to take effect. After restarting, Windows.... Large Collection of Sound Effects. Great sounds for video clips, games, commercials, apps. Free to use.
https://lochoang.jimdofree.com/anis-r%C6%B0%E1%BB%A3u-h%E1%BB%93i-08/
ophnam (Saturday, 05 March 2022 06:42)
Mineralization: Conversion of organic nitrogen to ammonium; Nitrification: ... intermediate product in the conversion of ammonium to nitrate (nitrification). ... major benefit of the legume rotation lasts only during the first year following the legume rotation. ... This knowledge allows you to predict whether net mineralization or net... d9ca4589f4 ophnam
https://wakelet.com/wake/XQfa4DJyfqulherXPVKO1
https://wakelet.com/wake/ub3Us2_KtufuFN6UsZ43L
https://wakelet.com/wake/d1dHXV2kUlBMLqyOn--aJ
https://wakelet.com/wake/l5I4LwKL-mNDih503coax
https://wakelet.com/wake/ue37uetqeE0gKIGEGwKUA
https://wakelet.com/wake/nG2m9Z0EmBmyhtx3n1aW3
https://wakelet.com/wake/s_V5dJ3dN5358tLcmaWpe
https://wakelet.com/wake/4NEaLwFbc6CXjI8GCA2aO
https://wakelet.com/wake/PgrTJIiObJeQihBdTO1YD
https://wakelet.com/wake/yFxIsuqB2iCvCFGJVad6S
CH3CH = C(CH3)2 + HBr Write the structure of the major organic product in each of the following reactions:. by RM Khan 2007 Cited by 372 This allowed us to predict the pleasantness of novel molecules by their ... an analogous physicochemical space from chemical descriptors, and then test for any ... The reaction time was longer for odorant pairs that were closer in ... led us to conclude that the major axis of perception reflects the major axis of.... JES is the flagship journal of The Electrochemical Society. Published continuously from 1902 to the present, JES remains one of the most highly-cited journals in...
ramlav (Saturday, 05 March 2022 07:29)
53969 items Advanced Office Password Recovery Pro v6.34.1889 Crack + Portable. ElcomSoft Advanced Office Password Recovery 6.32.1622 Portable.rar.... Advanced Office Password Recovery 6.34.1889 February 19th, 2019 free dwonload with crack - WorldSrc. ... V6.34.1889. s 7/8/10 x32, ... How Install the crack:.. Elcomsoft Advanced PDF Password Recovery Pro v5.0.6 ML with Key-BRD ... Advanced Office Password Recovery v6.34.1889 Crack ~ [APKGOD], 6, 1, Feb. 219d99c93a ramlav
https://coub.com/stories/4260195-planit-edgecam-2012-r1-zip-full-version-32-patch-utorrent-activator
https://coub.com/stories/4260194-organic-chemistry-reagents-and-their-functions-book-zip-utorrent-epub-free
https://coub.com/stories/4260193-quickbooks-2015-utorrent-ultimate-full-x32-rar-registration
https://coub.com/stories/4260192-terrorist-takedown-2-activation-download-pc-patch-full-version-rar
https://coub.com/stories/4260191-revit-2016-trial-hd-movies-watch-online-dvdrip-mkv
https://coub.com/stories/4260190-activator-red-giant-tra-ultimate-torrent-windows-exe-keygen
https://coub.com/stories/4260188-cakewalk-sonitus-fx-plugin-suite-vst-dx-v3-3-1-0-doa-32-key-keygen-rar-torrent-windows
https://coub.com/stories/4260189-serial-assassin-s-creed-2-skidrow-64bit-pc-ultimate-registration
https://coub.com/stories/4260187-luxury-house-re-watch-online-mkv-video-dts-watch-online
https://coub.com/stories/4260186-x64-fl-pth-of-field-plugin-for-after-effects-zip-build-windows
Advanced Office Password Recovery Pro v6.34.1889.... Dec 16, 2020 0 RC Nulled Crack Themes WHMCS stands for Web Host Manager Complete . ... Advanced Office Password Recovery Pro v6.34.1889 Crack
https://www.hott953.com/apps/blog/show/42989239-foxy-brown-dissing-ashanti-over-spragga-benz
quinlaqu (Saturday, 05 March 2022 08:07)
Note : Please Update (Trackers Info) Before Start "Good Company v0 8 5-GOG" Torrent Downloading to See Updated Seeders And Leechers for Batter Torrent... d9ca4589f4 quinlaqu
https://wakelet.com/wake/NoW1Ob99voWGBXkKel7rX
https://wakelet.com/wake/KKzq2Oi4wMUNawvqYqIqE
https://wakelet.com/wake/a5hwFGVOcvyl4VKK3jioe
https://wakelet.com/wake/02TwtrUfPSV4kIimLwP1z
https://wakelet.com/wake/gmUWbkTpLgRrfDIFtH2eg
https://wakelet.com/wake/6o-XYxaAkyo1sqsjB7c3D
https://wakelet.com/wake/2thO5GjyIc1lyn6NcTwGJ
https://wakelet.com/wake/7V7Plca__MFUPdt3gjM_X
https://wakelet.com/wake/yyDCY3rgeJbyIoO5ql2bn
https://wakelet.com/wake/qDIQ6RX03drEO0zqNnyom
Original GFE List CC 1 - 3: Less than 1 Year old and 1 - Good 2 - Fair 3 - Poor Line ... VS131 POL 20 131 75 MONARCH BOAT CO WORK BOAT 165I/OMERC/EZ ... GENERATOR 9084-M 9085-S 9086-A. 16,891.00 4 93 YES V-C 05 VEH GOV. ... 9078-S 4,000.00 4 300 V085 R&G 10 085 88 Olathe Equipment Trailer, 5 TN,.... Find many great new & used options and get the best deals for HO 1:87 ... See all condition definitions Brand: Sylvan Scale Models MPN: V-085.... pp( poed q hd lw: e s o u d s be edy fo b jp o well~s-ggessve: l: g o v e g coucl o EO ... Oho Gov. B ob b f old coges- ; sol beg, o o he Aug. bo bou h e hes he co** P"e ... Cll bo 12, 8 hp V 085 *. y exs offs fv. s{ fc W V e h.c w *. good hp, v Blek Xg...
kalofre (Saturday, 05 March 2022 08:21)
Athens - Agios Kosmas Marina Athens - Alimos Marina Athens - Delta Kallithea Marina Athens - Flisvos Marina Athens - Glyfada Marina Athens - Zeas Marina. . Submit malware for free analysis with Falcon Sandbox and Hybrid Analysis technology. ... >CliniqueClive ... />Marina de Bourbon 219d99c93a kalofre
https://coub.com/stories/4343337-blu-ray-cw-cardcap-full-4k-dubbed-rip-download
https://coub.com/stories/4343336-camera-lens-blur-x32-windows-exe-pro-license-download-cracked
https://coub.com/stories/4343335-peter-griffin-voice-changer-ultimate-zip-utorrent-pc
https://coub.com/stories/4343334-tal-club-utorrent-32bit-full-license
https://coub.com/stories/4343332-sony-vaio-windows-exe-x64-torrent
https://coub.com/stories/4343333-havij117pro-file-download-pc-serial
https://coub.com/stories/4343331-elite-dangerous-32bit-pc-cracked-activation-software-full-version
https://coub.com/stories/4343330-aisi-movies-movies-free-utorrent-torrents
https://coub.com/stories/4343329-download-teori-komunikasi-massa-mcquail-golkes-pdf-zip-book-full-version
https://coub.com/stories/4343328-leica-cyclone-7-4-1-3087-x86x-full-professional-pc-32bit
Oct 18, 2013 Gerhard Weikum. Max Planck Institute for Informatics, Saarbruecken, Germany ... Marina Krotofil and Alvaro A. Crdenas. Femtocell Security in...
https://www.maarheeze.nu/index.php/component/k2/item/5449-moederdagactiviteiten-marishof
adaray (Saturday, 05 March 2022 09:10)
LMA faculty carefully guide each student taking piano lessons to their full potential while teaching a lifelong love of music. Our caring, professional faculty make.... Virtual MIDI Piano Keyboard is a MIDI events generator and receiver. It doesn't produce any sound by itself, but can be used to drive a MIDI synthesizer (either... 219d99c93a adaray
https://coub.com/stories/4254678-keygen-dungeon-siege-legends-of-aranna-32bit-activation-utorrent-full-version
https://coub.com/stories/4254677-full-version-super-hit-maker-5-1-zip-utorrent-windows
https://coub.com/stories/4254674-file-gratis-32bit-pc-full-version
https://coub.com/stories/4254675-premiere-pro-cc-2015-zip-activator-windows-professional-full-version
https://coub.com/stories/4254673-avid-sibelius-8-3-0-64bit-activation-keygen-pc-rar
https://coub.com/stories/4254672-pc-ciel-gestion-commerciale-evolution-9-1-full-torrent-latest-key-zip
https://coub.com/stories/4254668-gpspro-download-software-rar-windows-activator-x64
https://coub.com/stories/4254670-morphomso1300e2driver-keygen-64bit-zip-utorrent-windows-free-key
https://coub.com/stories/4254669-subtitles-twilight-saga-breaking-dawn-part-2-movies-watch-online-subtitles-dvdrip-utorrent
https://coub.com/stories/4254667-latest-dj12678-rar-torrent-free-patch-registration
Sep 9, 2012 I came across a lot of informative posts, but by far the most helpful app I came across was a virtual piano chord/scale creator, by Colm.... Former headhunter and executive search consultant. Master's degree in music from New England Conservatory. Full time performer/song writer/recording artist.
http://harouni-urologie.com/component/k2/item/26-rehabilitation%3Ebest
adaray (Saturday, 05 March 2022 09:10)
LMA faculty carefully guide each student taking piano lessons to their full potential while teaching a lifelong love of music. Our caring, professional faculty make.... Virtual MIDI Piano Keyboard is a MIDI events generator and receiver. It doesn't produce any sound by itself, but can be used to drive a MIDI synthesizer (either... 219d99c93a adaray
https://coub.com/stories/4254678-keygen-dungeon-siege-legends-of-aranna-32bit-activation-utorrent-full-version
https://coub.com/stories/4254677-full-version-super-hit-maker-5-1-zip-utorrent-windows
https://coub.com/stories/4254674-file-gratis-32bit-pc-full-version
https://coub.com/stories/4254675-premiere-pro-cc-2015-zip-activator-windows-professional-full-version
https://coub.com/stories/4254673-avid-sibelius-8-3-0-64bit-activation-keygen-pc-rar
https://coub.com/stories/4254672-pc-ciel-gestion-commerciale-evolution-9-1-full-torrent-latest-key-zip
https://coub.com/stories/4254668-gpspro-download-software-rar-windows-activator-x64
https://coub.com/stories/4254670-morphomso1300e2driver-keygen-64bit-zip-utorrent-windows-free-key
https://coub.com/stories/4254669-subtitles-twilight-saga-breaking-dawn-part-2-movies-watch-online-subtitles-dvdrip-utorrent
https://coub.com/stories/4254667-latest-dj12678-rar-torrent-free-patch-registration
Sep 9, 2012 I came across a lot of informative posts, but by far the most helpful app I came across was a virtual piano chord/scale creator, by Colm.... Former headhunter and executive search consultant. Master's degree in music from New England Conservatory. Full time performer/song writer/recording artist.
http://harouni-urologie.com/component/k2/item/26-rehabilitation%3Ebest
adaray (Saturday, 05 March 2022 09:11)
LMA faculty carefully guide each student taking piano lessons to their full potential while teaching a lifelong love of music. Our caring, professional faculty make.... Virtual MIDI Piano Keyboard is a MIDI events generator and receiver. It doesn't produce any sound by itself, but can be used to drive a MIDI synthesizer (either... 219d99c93a adaray
https://coub.com/stories/4254678-keygen-dungeon-siege-legends-of-aranna-32bit-activation-utorrent-full-version
https://coub.com/stories/4254677-full-version-super-hit-maker-5-1-zip-utorrent-windows
https://coub.com/stories/4254674-file-gratis-32bit-pc-full-version
https://coub.com/stories/4254675-premiere-pro-cc-2015-zip-activator-windows-professional-full-version
https://coub.com/stories/4254673-avid-sibelius-8-3-0-64bit-activation-keygen-pc-rar
https://coub.com/stories/4254672-pc-ciel-gestion-commerciale-evolution-9-1-full-torrent-latest-key-zip
https://coub.com/stories/4254668-gpspro-download-software-rar-windows-activator-x64
https://coub.com/stories/4254670-morphomso1300e2driver-keygen-64bit-zip-utorrent-windows-free-key
https://coub.com/stories/4254669-subtitles-twilight-saga-breaking-dawn-part-2-movies-watch-online-subtitles-dvdrip-utorrent
https://coub.com/stories/4254667-latest-dj12678-rar-torrent-free-patch-registration
Sep 9, 2012 I came across a lot of informative posts, but by far the most helpful app I came across was a virtual piano chord/scale creator, by Colm.... Former headhunter and executive search consultant. Master's degree in music from New England Conservatory. Full time performer/song writer/recording artist.
http://harouni-urologie.com/component/k2/item/26-rehabilitation%3Ebest
fynnnoe (Saturday, 05 March 2022 09:30)
Risk Rating of major roads in South East Europe Risk Maps .......................... 7. 1.3.2 ... 1.2.1 Risk Mapping. SENSoR has used the ... Mini roundabout. 7.. Overlap of the motorway route with the climate zones defined in Romania . ... 1.2.1. Longitudinal profille. The longitudinal profile was designed based on technical criteria and ... Where appropriate, SBR mini-treatment plants will be located. d9ca4589f4 fynnnoe
https://wakelet.com/wake/jy1K_oWvVZUwuZVj08ZpV
https://wakelet.com/wake/lk5Lm0kZ6shui2htLwUOJ
https://wakelet.com/wake/rSNYs9DPnuxUH88qoovCk
https://wakelet.com/wake/Rjuf5OzP5rwvfxb1GU-qn
https://wakelet.com/wake/t1cBGANjnn0Jj2-qZ_drm
https://wakelet.com/wake/drtiYRn4n_pm93Mm8iLks
https://wakelet.com/wake/VnNq3bdklEVbvcKOHMJXk
https://wakelet.com/wake/wgY2VG6mdu1Mrbe0-x30o
https://wakelet.com/wake/2PkR1pY80KgqoX3dVCzXv
https://wakelet.com/wake/Kr6T57CFzDrlpuzugwWDS
Mar 31, 2015 A-1.2.1. APPENDIX B: WORK IN ROAD RESERVES. Procedure for Wayleave Application Form. B-2-1 ... E-7.1.4. APPENDIX E7.2 ROADS & STORMWATER DETAIL DESIGN ... RD-123. Typical Layout of Mini-Circle. RD-130.. Motorway, Trans-European Railway and the Euro-Asia Transport Links projects, that facilitate multi- ... 1.2.1. Primary and secondary sources. Concerning the resources available for transport infrastructure financing, at the most ... way of mini.
froroma (Saturday, 05 March 2022 09:59)
Watch the Golden State Warriors at the Chicago Bulls with NBA League Pass. Broadcast restrictions may apply.. Watch NBA Live: Golden State Warriors vs Chicago Bulls live streaming and TV information. Chicago Bulls have won their last four matches in succession.. Mar 29, 2021 Both the teams are placed at 10th spot in points table to their respective Conferences. Bulls are on 3 games losing streak while Warrior have lost... 219d99c93a froroma
https://coub.com/stories/4340562-boris-red-for-edius-7-zip-full-version-key-torrent
https://coub.com/stories/4340559-x-men-the-last-stand-subtitles-mp4-blu-ray-hd-full-watch-online-subtitles
https://coub.com/stories/4340560-zip-fol-r-lock-7-8-0-full-version-64bit-download-pc
https://coub.com/stories/4340561-universal-torrent-patch-windows-full-rar-license
https://coub.com/stories/4340558-hd-b-ali-gangster-dual-subtitles-1080
https://coub.com/stories/4340556-isilo-6-10-for-registration-pc-cracked-full-version
https://coub.com/stories/4340557-book-cai-sanchez-semiologia-cardiovascular-full-epub-download-rar
https://coub.com/stories/4340555-karta-pacjenta-podologia-free-mobi-torrent-ebook
https://coub.com/stories/4340554-x64-scargar-driver-micronics-w313-activation-free-serial-rar
https://coub.com/stories/4340553-utorrent-or-cfd-2012-key-32-cracked-exe-pro-pc
Mar 11, 2021 Kate Scott will become first woman to handle Warriors' play-by-play duties on a ... broadcast team for Golden State's March 29th game against the Bulls by ... for the St. Louis Blues and Chicago Blackhawks game last March 8, and ... game in 2016 and then becoming the first woman to do play-by-play for a...
https://seesaawiki.jp/asliyrano/d/my%2dhusband%2dsaid%2di%2druined%2dhis%2dlife
panaflem (Saturday, 05 March 2022 10:49)
by JB Knudsen Cited by 206 Java Cryptography Extensions (JCE), showing you how to use security providers ... Java was designed to enable small programs, applets, to be downloaded and run ... In practice, a provider is a collection of algorithm classes headed up by.. Home of the Legion of the Bouncy Castle and their Java Cryptography resources and open ... A set of tools for generating signed PDF documents, as well as certificates. ... Java Cryptography Extensions : Practical Guide for Programmers. One can practice these Electronics & Communication Engineering interview questions ... No need to worry about downloading in-complete Ebooks or PDF files in Electronics ... Cryptography & Network Security Questions and Answers ... 1000 Java Problems-Algorithms-Solutions 1000 Python Problems-Solutions 1000... 219d99c93a panaflem
https://coub.com/stories/4249453-serat-babad-tanah-jawi-full-ebook-utorrent-mobi-rar
https://coub.com/stories/4249454-utorrent-whatyousayiswhatyougetdongossettpdf-latest-key-full-version-pc-exe-nulled
https://coub.com/stories/4249455-pc-apr-h4s-platinum-7-4-11-610-hacking-4-studying-19-crack-activator-file-free-utorrent
https://coub.com/stories/4249456-citylights-torrents-2k-full-dts-film-movies
https://coub.com/stories/4249457-64-corel-draw-x6-language-pack-italian-download-patch-activation-professional
https://coub.com/stories/4249458-book-pwd-maharashtra-red-download-full-version-rar
https://coub.com/stories/4249459-senha-crack-pc-registration-utorrent-32
https://coub.com/stories/4249461-32bit-multi-loa-rar-activation-pc-latest-patch-free
https://coub.com/stories/4249462-rar-clave-activation-free-32-ultimate-torrent-pc
https://coub.com/stories/4253890-mp4-bitter-passion-tagalog-1080p-dts-kickass-mkv
Develop a greater intuition for the proper use of cryptography. This book teaches the basics of writing cryptographic algorithms in Python, demystifie.. Practical Cryptography Niels Ferguson Bruce SchneierWiley Publishing, Inc. Executive Publisher: Robert Ipsen Executi.... May 22, 2021 In this tutorial, we're going to learn about the Digital Signature mechanism and how we can implement it using the Java Cryptography...
https://stockmanshollow.com/board/viewtopic.php?f=5&t=280&p=264017#p264017
tasmerc (Saturday, 05 March 2022 10:56)
3 days ago There are two pages that the Super Dark Mode cannot darken: + The new tab: you need to install dark theme for Chrome to make it dark. + The... d9ca4589f4 tasmerc
https://wakelet.com/wake/UhSsjoPwjyPdQxRXooFiY
https://wakelet.com/wake/TQ5y5K-LLDYR9G9Xi38Mk
https://wakelet.com/wake/2B25-2NDA8hRwUmxew9E-
https://wakelet.com/wake/ZALXnuki7XeJQNtcRJ4lr
https://wakelet.com/wake/0dlKjpotdyFQFhqYsdpL1
https://wakelet.com/wake/DJaRXPUHzdqarisDg4Pga
https://wakelet.com/wake/R29_OOKtftYPZOD55kBwl
https://wakelet.com/wake/x0oneULuBhuXYxgy6Zjrx
https://wakelet.com/wake/vuVgin-qiA4d0T0-A3m-w
https://wakelet.com/wake/BPodqQ-RunzppIuxvivZA
Taskbar puts a start menu and recent apps tray on top of your screen that's accessible at any time, increasing your productivity and turning your Android tablet.... Updated March 2021. The on-screen keyboard enables you to enter text and perform keyboard shortcuts using a mouse, trackpad, or other input device.
keeelv (Saturday, 05 March 2022 11:40)
Here on SofaScore livescore you can find all Buffalo Bills vs Pittsburgh Steelers previous results sorted by their H2H matches. Links to Buffalo Bills vs. Pittsburgh.... Dec 13, 2020 Pittsburgh Steelers at Buffalo Bills: Live stream, how to watch, odds, time ... While the Bills (9-3) probably can't realistically get the No. ... games the lone setback being the "Hail Murray" game against the Arizona Cardinals. 219d99c93a keeelv
https://coub.com/stories/4332145-techsmith-camtasia-studio-9-0-4-torrent-full-pro-patch-key
https://coub.com/stories/4332144-objective-first-stu-nts-answers-torrent-zip-full-edition-ebook-pdf
https://coub.com/stories/4332143-sonic-generations-v1-0r4-update-registration-nulled-x32-pc
https://coub.com/stories/4332140-veer-zaara-mp3-songs-exe-utorrent-full-version-pro-pc
https://coub.com/stories/4332141-4k-online-player-the-prince-of-egypt-720-subtitles-video-x264-watch-online-full
https://coub.com/stories/4332137-blu-ray-dil-tu-hi-bata-watch-online-1080-hd-video
https://coub.com/stories/4332139-rangku-biologi-sma-full-version-ebook-epub-torrent-rar
https://coub.com/stories/4332138-iso-resi-latest-license-windows
https://coub.com/stories/4332136-pastel-partner-torrent-key-windows-pro-rar-free
https://coub.com/stories/4332135-rar-very-pdf2word-v3-1-free-pc-torrent-32bit
Dec 12, 2020 Listen live. Fans can listen to the action on the Bills Radio Network, featuring Steve Tasker and the voice of the Bills, John Murphy. Bills Radio...
https://tombrendt.jimdofree.com/2011/04/13/el-yaque-new-politics/
alorays (Saturday, 05 March 2022 12:18)
I think that you can do with a few pics to drive the message home a little bit, but other than ... dice (20-04-2014 08:43): ... Current market Rumor : women Considered A Necessity Today ... a href="http://www.probusinesstv.ru/chanel718/new-chanel5949.html" > /a>. d9ca4589f4 alorays
https://wakelet.com/wake/jH9fg87ZR2T676iYcfdGC
https://wakelet.com/wake/R5CawHkyouONL-xRDGid5
https://wakelet.com/wake/BlbJ_JHa_z79AtrI_1k7U
https://wakelet.com/wake/_hgN51VcV1yYejWeskybI
https://wakelet.com/wake/FGYVBIesaQb0zyLXMuWJD
https://wakelet.com/wake/3HaIZCag8rAHY4n-j9Ks_
https://wakelet.com/wake/72URjQFPNuem2dyds4lwk
https://wakelet.com/wake/pAyEVLOFNvQAZKsITRF7g
https://wakelet.com/wake/OM55Q-xSHqBE_acrw-BDU
https://wakelet.com/wake/b6P3seuj5Bt-GjZ4c_mKO
Jun 23, 2021 ... Kyrat's Bell ... 61B43DB8 147499 Inbox messages download failed. ... BBE44DD9 276931 GHOST BEAR (RARE) B62B085E 276932 This strange and ... Like what... marrying little girls? ... I hope you're wearing a diaper gora!. A project to install 13 "little free libraries"/book exchanges across Cambridge made ... I am sure the women at the YWCA would even love to see a better site out the ... 42.361473 -71.115972 PB4(June-December 2017) P085 Parks & Recreation ... (October 2014-April 2015) P43 Parks & Recreation Light sensors and surface.... It can be very useful when potty training a child. They are nothing like a diaper or a pull up. They do not keep the child dry like a diaper does or even pull-ups do.Missing: Girls | Must include: Girls
zsolree (Saturday, 05 March 2022 12:28)
michael kors outlet The Boston Herald is reporting Allen was requesting three years ... Timothy http://www.balunywa.net/usa/?key=Cheap-Nike-Bags-For-Girls I think all ... http://www.donkk.ru/forum/go.php?http://www.ugg-boot-outlet.com ... vente bikini village 2014 ... ralph lauren swimwear ... ImgSrc=ExpressAuto-Large.. Germany 3 1 L'Alliance Francophone 19 5576308454.249586 ... b> ... United States 473 2 Argonautic Life Support Systems 584 47853.355217 ... If you are old-school, new-school or just think anime girls &/or guys are hot, this... 219d99c93a zsolree
https://coub.com/stories/4243118-panelinha-rita-lobo-29-mobi-download-rar-book-full
https://coub.com/stories/4243116-adobepdfinf-download-nulled-rar-full
https://coub.com/stories/4243117-epub-uchs-ne-2-download-rar-ebook-full
https://coub.com/stories/4243115-rulers-of-nations-2-torrent-activator-pc-nulled-exe
https://coub.com/stories/4243114-usb-firmware-crack-pc-x32-full-utorrent
https://coub.com/stories/4243113-x264-pa-me-muevo-2k-subtitles-watch-online-dual-2k
https://coub.com/stories/4243112-daossoft-excel-password-remover-torrent-x32-full-version-pro-key
https://coub.com/stories/4243110-license-mo-rola-mtr2000-cps-build-free-keygen-pc
https://coub.com/stories/4243111-pirates-of-the-caribbean-watch-online-2k-mp4-free
https://coub.com/stories/4243108-smart-dll-missing-fixer-pro-4-6-5-software-x64-license-serial-exe
... %A5-ym074962-p-91.html"> .... Editor's NotesA cropped, pastel color t-shirt with logo printed on front. The side of the bottom hem can be tied into a ribbon. Wear it as a cover up over swimsuit or...$54.00. ... middle;height:225px">
https://thaitumweb.com/index.php/component/k2/item/8
safrkhar (Saturday, 05 March 2022 13:14)
Rheem RTGH-95DVN Tankless Water Heater Rheem Condensing. ... C 1210 ES NG Tankless Water Heater Natural Gas Toto SW584#12 Washlet S350e ... on a steep state censible 510e water heater nvidia physx sdk allen bradley slc 500.... Car Seat Evenflo LiteMax 35 Owner's Manual Rear-facing child restraint system, ... State Censible 510e Gas Water Heater Manual Free Flute Sheet Music Pdf.... Residential water heaters up to 52 gallon capacity, a brochure with generic earthquake bracing instructions can be obtained from: Office of the State Architect, 400 P Street, Sacramento, ... The State Industries Censible 510E water heater is a tankless model designed for commercial or residential use and powered by gas. 219d99c93a safrkhar
https://coub.com/stories/4330665-registration-au-cad-2006-full-latest-iso-nulled-32
https://coub.com/stories/4330664-nulled-runtime-error-at-1-0-can-exe-pc-activator-file-torrent
https://coub.com/stories/4330662-pho-calendar-crea-final-64bit-rar-windows-activation-torrent
https://coub.com/stories/4330663-terjemahan-kitab-minhajul-muslim-l-book-mobi-download-free
https://coub.com/stories/4330661-rar-emulador-torrent-windows-nulled-full-version
https://coub.com/stories/4330660-neat-cut-x32-crack-free-torrent-macos
https://coub.com/stories/4330659-windows-longbow-converter-for-au-activator-64-full-exe-129311
https://coub.com/stories/4330658-720-australia-full-dubbed-dual-kickass-watch-online-english
https://coub.com/stories/4330657-movie-hey-bro-hd-kickass-mkv-subtitles-watch-online-1080p
https://coub.com/stories/4330653-watch-online-always-2011-movies-utorrent-mp4-mkv-subtitles
State Select Gs640ybrt Manual Residential Gas. Outdoor Model No. State Censible 510E Hot Water Heater Model #PRV 40 PORT6 - Propane gan, 40 gallon,.... State 510e sensible manualidades :: for Mobile google manual on ... I have an old (1991) State Censible gas-fired water heater, model # PRV 40 NORT6 F,...
https://www.maarheeze.nu/index.php/component/k2/item/5037-nieuwe-bestemming-baronie-van-cranendonck
berknath (Saturday, 05 March 2022 13:36)
Take just a few minutes to register your product, and enjoy the benefits: Free Technical Support; Special offers and promotional pricing (email opt in required).... Download the guide to tap into the true power of HR. ... Our human capital management (HCM) software gets you out of the weeds, our focus on ... A single source of truth for all employee data makes your life so much easier just imagine ... I don't have to worry about a change in tax code or child support garnishment.. Dec 1, 2013 In Beyond Capital he was to develop this further in terms of a full-scale ... of the activation of capital's absolute limits associated with the destruction of the ... of social metabolism, a metabolism prescribed by the natural laws of life itself. ... On the role of isolation as the key to abstraction in a dialectical... d9ca4589f4 berknath
https://wakelet.com/wake/E-WMJDeFgz1LWENL-nePE
https://wakelet.com/wake/xw2P3m4_yFCCZ_OiZbim-
https://wakelet.com/wake/ncFSIt-0kYNeuKjN9mV_x
https://wakelet.com/wake/1NE2gL0phUS-ALYlS6Psh
https://wakelet.com/wake/2oPi3o_tGGwHOOhsHy-tc
https://wakelet.com/wake/8RvKxj-nMrcVtO8TIKuPE
https://wakelet.com/wake/COVL_-jT__QdBSG_sE3SX
https://wakelet.com/wake/Gkykiddzc8rTEQAiigork
https://wakelet.com/wake/4WuDTkkeIQ0PF_LujBLXr
https://wakelet.com/wake/tXzaDEMboLdwbDqi_ygfz
by JW Moore 2017 Cited by 170 Download by: [142.105.209.61] ... markets and capitalism independently of the web of life, then mobilize indicators of the ... The Capitalocene, then, is a key conceptual and methodological move in rethinking ... activation the work of science, power and capital is a co-produced reality, bundling the.. Each person is a real-life user of Clubhouse. Usually, it's someone who has had ... How much of my data does Clubhouse want for registration? You have to give...
marque (Saturday, 05 March 2022 14:01)
Oct 25, 2018 Opinion: Donald Trump embraces 'nationalism' of the worst kind. Image without a caption. President Trump at a campaign rally with Sen.. Jul 24, 2020 Families trust nursing homes to provide their aging loved ones professional round-the-clock care when they are no longer able to care for them. 219d99c93a marque
https://coub.com/stories/4240318-full-shin-chan-dubbed-subtitles-download
https://coub.com/stories/4240317-license-hello-neighbor-beta-3-dna-hack-torrent-exe-crack-free-professional-windows
https://coub.com/stories/4240314-marketing-research-naresh-malhotra-5th-epub-book-full-edition-download-zip
https://coub.com/stories/4240315-key-stellar-phoenix-latest-utorrent-32-windows
https://coub.com/stories/4240313-zip-cancionero-danilo-montero-vocion-download-book-full-mobi
https://coub.com/stories/4240312-geometers-sketchpad-5-05-windows-full-version-cracked-32bit-ultimate-zip-torrent
https://coub.com/stories/4240311-watch-online-pandaga-chesko-1080p-mkv-subtitles-video-dvdrip
https://coub.com/stories/4240310-ja-rule-the-last-temptation-key-64-latest-utorrent
https://coub.com/stories/4240309-crack-mi-lta-di1610-driver-torrent-64bit-full
https://coub.com/stories/4240308-x64-medal-of-ho-build-zip-key-cracked
Mar 27, 2019 Prominent Apple blogger calls the MacBook's butterfly keyboards the ... that refused to type the letter G unless I pressed very hard on the key.. Jul 5, 2018 All across the Internet, blogs, web forums and comment sections are similarly littered with panicked cries for relief from Hell Itch victims.. Jul 13, 2020 A job loss is one of the worst financial shocks most families will face, ... One way to know is to look at different types of economic hardship, such...
https://talkotive.com/read-blog/10847
jeafior (Saturday, 05 March 2022 14:52)
3 , 36 ... [b] ?[/b] ... http://remmont.com/reise-nach-irland-download-ebook-pdf-reise-nach-irland ... kompoz.me.... Boat Only Rental (3 person) : ... works 100 deenspnlfritos http://topkmarte.ugu.pl/wohepegyw/ravenloft-night-of-the-walking-dead-pdf.html ... apk http://discpricper.7m.pl/posts/35-skachat-draivera-dlja-nokia-s6-01.html ... ? . 219d99c93a jeafior
https://coub.com/stories/4327899-dubbed-the-antaheen-watch-online-full-subtitles-english-x264-video
https://coub.com/stories/4327898-activation-transformers-f-pc-crack-utorrent-full-version-64bit
https://coub.com/stories/4325199-barten-rar-torrent-ultimate-x32-serial-free
https://coub.com/stories/4325198-kickass-ju-on-s-mp4-avi-720p-dubbed
https://coub.com/stories/4325196-smoke-2019-32bit-torrent-full-activator-pc-serial
https://coub.com/stories/4325195-full-version-aida-windows-torrent-crack-zip-key-final
https://coub.com/stories/4325194-fsx-eiresim-belfast-city-egac-v1-1-64bit-latest-full-version-crack-windows
https://coub.com/stories/4325193-mkv-bob-esponja-pelicula-mp4-torrents-english-subtitles
https://coub.com/stories/4325192-windows-solucionario-welty-fundamen-download-32-final-crack-zip
https://coub.com/stories/4325191-x64-adobe-animate-cc-2019-19-0-0-full-torrent-windows-activator-keygen
Jun 27, 2021 https://narcom.ru/redirect.php?https://tubepatrol.org/videos/sex-hd-seal-pak/ sex hd vida0s.... Oct 14, 2014 24 , , ,...
https://pixel-mustangs.jimdofree.com/startseite/unser-g%C3%A4stebuch/
raidchar (Saturday, 05 March 2022 14:59)
Jun 4, 2021 The Western Michigan University softball team picks up a 4-3 win vs. Ball State (courtesy of Ashley Huss-WMU Photographer) ROSEMONT, IL (WKZO AM/FM) The Western Michigan ... Live Stream on pac-12.com or on the Pac-12 Now app . ... Western New Mexico University - 2021 Softball Schedule. 2-2. d9ca4589f4 raidchar
https://wakelet.com/wake/0QvNcGiiADbpLrYbK-9EI
https://wakelet.com/wake/B7xA8pBqHugzZibBPu3Xf
https://wakelet.com/wake/zX8sWOUer_N8y13v_BUAA
https://wakelet.com/wake/pQjhZNG5gGiu8vTgYcZf_
https://wakelet.com/wake/PwhZ8MwMkcA3LzkEqc_jq
https://wakelet.com/wake/vCNdylITePE0vKRkYdVBR
https://wakelet.com/wake/9ER-Cz3bzRmDAPkfWBz2h
https://wakelet.com/wake/JxR9PTdiSMn56Y95J2h4Q
https://wakelet.com/wake/aHaT3kHxtfJtlO4Qa6CBT
https://wakelet.com/wake/ohIaB-fXgRy2q79DZ3ZU-
The official 2020 Softball Roster for the Michigan State University Spartans ... Monarch: 4: Ashley Michelena: Sr. Chelsea Little League will offer multiple divisions in tee ball, baseball and softball for the 2021 season. ... Live Stream on watchespn. ... Additional Links View PDF Central Michigan (1-4) -vs- South Dakota (2-5).... Still time to sign up for our 2021 Youth Camp!! Grades 1-8 can register online! Reserve your spot today! .... Western Michigan Broncos vs Kent State Golden Flashes College Basketball betting odds, ... Watch Here http://sport.dicobian-hd.online/hs-boysbasketball.php?live= ... the Western Michigan Broncos (4-11) into a matchup against the Ball State ... Stories Additional Links View PDF Kent St. 80 (4-3,1-2 MAC) vs Western Mich.
drafin (Saturday, 05 March 2022 15:42)
Carlos de Vilanova. Remedios naturales para aumentar la testosterona: Cmo mejorar la salud sexual y la energa masculina. Stephen Harrod Buhner. Dejar ir. 219d99c93a drafin
https://coub.com/stories/4240615-windows-alrassamalarabiv31r1-crack-key-full-64
https://coub.com/stories/4240614-rab-ne-bana-di-jodi-4-4k-watch-online-watch-online-torrents
https://coub.com/stories/4240613-mobile-cellular-telecommunications-by-william-cy-lee-book-mobi-utorrent-free-zip
https://coub.com/stories/4240611-big-brother-torrents-2k-watch-online-dubbed-watch-online
https://coub.com/stories/4240612-key-microsoft-office-2010-outlook-x86-thethingy-pc-rar-free-keygen-software
https://coub.com/stories/4240610-keygen-rtt-teorie-vraestel-final-free-download-32-windows
https://coub.com/stories/4240609-ckinfo-v113rar-torrent-registration-free-x64-zip
https://coub.com/stories/4240608-dubbed-rave-reports-11-watch-online-mp4-video-720
https://coub.com/stories/4240607-nfs-the-run-game-cracked-windows-32-free-build
https://coub.com/stories/4240606-file-nne-meter-download-64-keygen-full-activation
DAS DE PESCA GRATIS. Tanto los ... liberacin cuidadosa de especies populares de tamao ... de lagos y arroyos; puede encontrarla en formato PDF en lnea. ... comercial y sean transportados por pescadores deben ir acompaados de ... No se permite dejar desechos en el hielo. d. ... (CAMINO RED FEATHER LAKES):.. Padres y tutores legales no podrn dejar a sus nios solos en un ... descargar mercanca o bajar pasajeros, o paran antes de ... a un callejn o camino muy cerrado, pueden ir muy ... asegrese de apretar el botn de liberacin o de jalar de.. Dejar suficiente distancia entre su vehculo y el vehculo de adelante. ... conductores para condiciones especficas del camino y peligros ms adelante, ... Al ir detrs de un conductor que sealiz su intencin de hacer un giro, o que ha ... el freno de mano, pero sostenga el botn de liberacin del freno de manera que...
https://jaidenbwad609.webs.com/apps/blog/show/44592355-what-does-ace-mobile-mechanics-mean-
deefolk (Saturday, 05 March 2022 16:17)
Jul 3, 2021 Ac3 torrent download; true grit 2010 (english) pdvd (xvid) torrent ... Here you download movies in best quality and dual audio like, hindi-english some. ... the walls of a maximum security prison in the shawshank redemption. ... Do not miss to watch movie the green mile (1999) online for free with your family. d9ca4589f4 deefolk
https://wakelet.com/wake/hXKwjhy-OiV_tt1Z9_Tab
https://wakelet.com/wake/kDShJD0Pb17nIOocCstoz
https://wakelet.com/wake/9H9tvZsuJ5wiKNolzjjjW
https://wakelet.com/wake/TktrzHjEDVa9n15Uq_V0W
https://wakelet.com/wake/Dw9HAl5pAC9hsJRpTrNtK
https://wakelet.com/wake/7qfnpDucUdhLUJlUObgVm
https://wakelet.com/wake/TuygDGzRsIbAvVHI8EKXO
https://wakelet.com/wake/ubtogo06BBux_DFt-s0cd
https://wakelet.com/wake/Tizrk7sMDJJW7uJAucYCl
https://wakelet.com/wake/6Ex69w_BDex0nYspIb5L6
Money Train 1995 Free Download 720p Bluray Movie Info Full Name: Money ... Download File Money Train 1995 720p Blu Ray mp4 File: Money. ... 01:49:58, avg.bitrate: 2231 kb/s Audio: aac, 48000 Hz, 5:1 (eng) Money Train 1995 720p ... BluRay 278 The Shawshank Redemption (1994) 279 The Shining (1980) 280 The.... Aug 25, 2017 Download Sherlock Season 1-4 (2010-2017) 720p (English) of each episode ... Download Movie 2011 Sherlock Holmes: A Game of Shadows Direct link. ... Ano de Lanamento: 2011 Idioma Original: Ingls Audio: Dual Audio ... The Shawshank Redemption BRRip (1994) 849MB x264 MKV [Multi Links].
tamjak (Saturday, 05 March 2022 16:27)
Similar Games Camping Mama Outdoor Adventures (USA) NDS ROM SpongeBob To Nakamatachi Toybot No Kougeki (6rz) (Japan) NDS ROM Hello Kitty... 219d99c93a tamjak
https://coub.com/stories/4334483-pc-le-ore-rivista-hard-crack-license-torrent
https://coub.com/stories/4334482-32bit-eca-vrt-dvd-2011-rar-ultimate-free-crack-license
https://coub.com/stories/4334481-gsa-seo-in-full-registration-exe-torrent
https://coub.com/stories/4334480-movies-ram-leela-4k-video-torrent-watch-online-dubbed
https://coub.com/stories/4334479-activator-test-drive-unlimited-2-rar-professional-64bit-pc-torrent
https://coub.com/stories/4334478-3dt-compose-v02-for-wedding-rar-zip-windows-key-keygen-professional-x32
https://coub.com/stories/4334477-video-flight-of-the-phoenix-in-dubbed-mkv-full-watch-online-free-1080
https://coub.com/stories/4334475-zip-grammar-of-p-k-y-sarkar-full-epub-torrent-ebook
https://coub.com/stories/4334476-zygor-gui-final-torrent-32bit-cracked-license-pc
https://coub.com/stories/4334473-zip-stanari-u-slonu-coffre-hoc-insani-torrent-ebook-full-version-pdf
Play 0603 - Crash Boom Bang! for Free on your PC, Android, iOS, or any other ... Camping Mama - Outdoor Adventures 3395 - Jewel Quest - Expeditions (DE).... Jun 18, 2020 Camping Mama: Outdoor Adventures ... Cooking Mama World Combo Pack Volume 1 NDS ROM Info: ... Download Links: Game Size 33 MB. (DSi Enhanced) (EU); 5826 Camping Mama - Outdoor Adventures (US); 5918 ... 1.41) and provided for your system update purpose, please download here. ... GEI V2.1, we have added a new patch geiplus.nds inside the kernel of GEI V2.1.
https://braskbrask68.webs.com/apps/blog/show/47829996-cara-untung-main-togel-misteritogel
virpas (Saturday, 05 March 2022 17:13)
May 19, 2017 Newbie Audio Engineering + Production Question Zone Comping workflow ... Pro Tools actually has a tool for this, you can right click and rate each track. ... whether the singer's voice happened to crack - in a good way - on take number 4; ... Pro Tools 9 Software, Version 9, VG Discs, Fast Free ShipUS $107.. It can be run as a stand-alone application or as a plug-in within Pro Tools (or any DAW). ... In Pro Tools, locate the audio track that you wish to apply the Melodyne ... "right" vocal comp was pieced together from several days worth of recording.. With Pro Tools, you can make music with up to audio and 1, MIDI tracks and ... From trimming clips and reshaping sounds with a single click, to comping ... Download Pro Tools and get hold of the best audio workstation Vote 1 2 3 4 5 6 7 8 9... 219d99c93a virpas
https://coub.com/stories/4255366-book-vastu-shastra-books-in-13-full-mobi-rar
https://coub.com/stories/4255364-mobi-ed-sheeran-digital-booklet-full-edition-book-zip-utorrent
https://coub.com/stories/4255363-ra-beauty-re-64-activation-windows-utorrent
https://coub.com/stories/4255362-dts-ereadrone-the-fpv-simula-mp4-english-kickass-watch-online-720-rip
https://coub.com/stories/4255360-kon-boot-usb-2in1-zip-windows-utorrent-activation-full-64bit
https://coub.com/stories/4255361-cyme-cymgrd-v6-3-r3golkes-torrent-full-version-key-rar
https://coub.com/stories/4255359-utorrent-illwinter-s-floorplan-genera-activator-x64-keygen-pc
https://coub.com/stories/4255358-64bit-exiland-assistant-3-4-nulled-rar-free-macos
https://coub.com/stories/4255357-activation-power-geez-amharic-2010-32bit-torrent-zip
https://coub.com/stories/4255355-credit-wizard-1-1-rar-cracked-pro-free-download
Build guides for Senna on MOBAFire. Find Senna guides from summoners and champion builds based on stats for all League of Legends (LoL) champions.. Criar Site Grtis Pro tools 8 m powered ilok crack download links are externally hosted. ... Hardware-independent native systems: Pro Tools 9 Pro Tools 9, released in November 2010, dropped the requirement of ... "Track Comping". Sound on...
https://www.choiceconsultingllc.net/component/k2/item/10-vitae-vulputate-augue-lacinia-faucibus
elmielik (Saturday, 05 March 2022 17:34)
Jul 18, 2013 Math 240. Spanning sets. Linear independence. Bases and. Dimension. Span, Linear ... A set of functions 1f1,f2,...,fnl is linearly independent on.. Linear independence of functions The definition of linear dependence and the ability to determine whether a subset of vectors in a vector... d9ca4589f4 elmielik
https://wakelet.com/wake/k6_euUPX7laLLeubmKn9J
https://wakelet.com/wake/mjpY3PWpifW8eowYM_y2l
https://wakelet.com/wake/sWpNvOegXax0J9M7yy_O_
https://wakelet.com/wake/1-1jWhAOMx2-s-GjffKfR
https://wakelet.com/wake/UOmZYwGaiKb6eRhY6_eGD
https://wakelet.com/wake/z_7SsTaS0U433hTG-OpT8
https://wakelet.com/wake/JEZuGAHaIsolStT-8R3jT
https://wakelet.com/wake/xM8WX3pThRptjws3MAc7-
https://wakelet.com/wake/Y-Vkruj186pccSszWemrj
https://wakelet.com/wake/BvDuyfZG5I6jdK4qoxrvt
The functions f and g are linearly independent on I if they are not linearly ... If we calculate (2) for an exponential function z = Aerx, A a constant, we have z = Aerx.... Otherwise S is linearly independent. Page 3. Examples of linear independence. Vectors e1 = (1,0,0), e2 = (0 ... Show that functions ex, e2x, and e3x are linearly...
begsha (Saturday, 05 March 2022 17:59)
Read Sheetz reviews, including information from current and former employees on salaries, benefits, and more. Find out what life is like at Sheetz, then browse.... Sheetz Employee Handbook Online. Eventually, you will unquestionably discover a new experience and completion by spending more cash. still when? get you... 219d99c93a begsha
https://coub.com/stories/4352228-inpa-5-0-6-and-ediabas-7-3-0-cracked-utorrent-activator-full-version-zip-windows
https://coub.com/stories/4352227-watch-online-bajrangi-bhaijaan-1-2-3-dts-4k-torrent-subtitles
https://coub.com/stories/4352225-subtitles-super-hap-film-dvdrip-torrents-mp4-dual
https://coub.com/stories/4352226-free-bionic-com-pro-download-rar
https://coub.com/stories/4352224-full-quickbooks-pos-2013-beast-62-key-patch-pc-rar
https://coub.com/stories/4352222-opencanvas-6-x64-rar-download-activation-free-latest
https://coub.com/stories/4352223-book-babica-v-supergah-16-download-free-mobi-rar
https://coub.com/stories/4352221-full-version-biomedical-instrumentation-by-arumugam-l-book-download-rar-mobi
https://coub.com/stories/4352220-32-smart-array-p410i-patch-free-rar-key
https://coub.com/stories/4352218-torrent-gran-turismo-5-activation-patch-64-windows
Jan 19, 2021 Employee Handbooks. Candidates view five interactive sections in sequence, including an interactive survey to help determine if Sheetz is right.... Download : Sheetz Employee Handbook at wu.filery.site.
https://clubgimnasticocriollo.webs.com/apps/blog/show/10281693-reportaje-la-semana-copa-alcalde-wmm-2011
yanctal (Saturday, 05 March 2022 19:00)
Always and Forever. Front Cover. Lurlene McDaniel. Random House Childrens Books, 2004 - Juvenile Fiction - 166 pages. 3 Reviews. Sixteen-year-old Melissa.... Her first book was "Kickaroo: The Soccer Playing Kangaroo." But she realized that writing for picture books was not what she wanted to do, so she wrote "Will.... Publisher: Random House Children's Books, Special Attributes: EX-LIBRARY. ISBN: 9780553494198, EAN: 9780553494198. Author: Lurlene McDaniel... d9ca4589f4 yanctal
https://wakelet.com/wake/17x_Bq8KsQC-wD15DrNjJ
https://wakelet.com/wake/o2Oz4G78z2xORzYCsAHLs
https://wakelet.com/wake/eNJziz6yLXw11gUK0pJVn
https://wakelet.com/wake/LUI6EcMHHt1QZOuv4rmeT
https://wakelet.com/wake/tibGm2zn8ncThpAGldo8O
https://wakelet.com/wake/Mzwvi2MefsId7p1cgUa6E
https://wakelet.com/wake/f8LwWu0cCAsZ92sPl_SAF
https://wakelet.com/wake/ZJta0NBsOCo5uDrycx5O5
https://wakelet.com/wake/Xq27xvr-4QzQhpKxkGvTZ
https://wakelet.com/wake/enBCH5yJIiLgz0Iuheljd
Lurlene McDaniel has written more than 30 inspirational novels. Her books have received acclaim from teachers, parents, young adults, and reviewers.
yanctal (Saturday, 05 March 2022 19:01)
Always and Forever. Front Cover. Lurlene McDaniel. Random House Childrens Books, 2004 - Juvenile Fiction - 166 pages. 3 Reviews. Sixteen-year-old Melissa.... Her first book was "Kickaroo: The Soccer Playing Kangaroo." But she realized that writing for picture books was not what she wanted to do, so she wrote "Will.... Publisher: Random House Children's Books, Special Attributes: EX-LIBRARY. ISBN: 9780553494198, EAN: 9780553494198. Author: Lurlene McDaniel... d9ca4589f4 yanctal
https://wakelet.com/wake/17x_Bq8KsQC-wD15DrNjJ
https://wakelet.com/wake/o2Oz4G78z2xORzYCsAHLs
https://wakelet.com/wake/eNJziz6yLXw11gUK0pJVn
https://wakelet.com/wake/LUI6EcMHHt1QZOuv4rmeT
https://wakelet.com/wake/tibGm2zn8ncThpAGldo8O
https://wakelet.com/wake/Mzwvi2MefsId7p1cgUa6E
https://wakelet.com/wake/f8LwWu0cCAsZ92sPl_SAF
https://wakelet.com/wake/ZJta0NBsOCo5uDrycx5O5
https://wakelet.com/wake/Xq27xvr-4QzQhpKxkGvTZ
https://wakelet.com/wake/enBCH5yJIiLgz0Iuheljd
Lurlene McDaniel has written more than 30 inspirational novels. Her books have received acclaim from teachers, parents, young adults, and reviewers.
yanctal (Saturday, 05 March 2022 19:01)
Always and Forever. Front Cover. Lurlene McDaniel. Random House Childrens Books, 2004 - Juvenile Fiction - 166 pages. 3 Reviews. Sixteen-year-old Melissa.... Her first book was "Kickaroo: The Soccer Playing Kangaroo." But she realized that writing for picture books was not what she wanted to do, so she wrote "Will.... Publisher: Random House Children's Books, Special Attributes: EX-LIBRARY. ISBN: 9780553494198, EAN: 9780553494198. Author: Lurlene McDaniel... d9ca4589f4 yanctal
https://wakelet.com/wake/17x_Bq8KsQC-wD15DrNjJ
https://wakelet.com/wake/o2Oz4G78z2xORzYCsAHLs
https://wakelet.com/wake/eNJziz6yLXw11gUK0pJVn
https://wakelet.com/wake/LUI6EcMHHt1QZOuv4rmeT
https://wakelet.com/wake/tibGm2zn8ncThpAGldo8O
https://wakelet.com/wake/Mzwvi2MefsId7p1cgUa6E
https://wakelet.com/wake/f8LwWu0cCAsZ92sPl_SAF
https://wakelet.com/wake/ZJta0NBsOCo5uDrycx5O5
https://wakelet.com/wake/Xq27xvr-4QzQhpKxkGvTZ
https://wakelet.com/wake/enBCH5yJIiLgz0Iuheljd
Lurlene McDaniel has written more than 30 inspirational novels. Her books have received acclaim from teachers, parents, young adults, and reviewers.
yanctal (Saturday, 05 March 2022 19:02)
Always and Forever. Front Cover. Lurlene McDaniel. Random House Childrens Books, 2004 - Juvenile Fiction - 166 pages. 3 Reviews. Sixteen-year-old Melissa.... Her first book was "Kickaroo: The Soccer Playing Kangaroo." But she realized that writing for picture books was not what she wanted to do, so she wrote "Will.... Publisher: Random House Children's Books, Special Attributes: EX-LIBRARY. ISBN: 9780553494198, EAN: 9780553494198. Author: Lurlene McDaniel... d9ca4589f4 yanctal
https://wakelet.com/wake/17x_Bq8KsQC-wD15DrNjJ
https://wakelet.com/wake/o2Oz4G78z2xORzYCsAHLs
https://wakelet.com/wake/eNJziz6yLXw11gUK0pJVn
https://wakelet.com/wake/LUI6EcMHHt1QZOuv4rmeT
https://wakelet.com/wake/tibGm2zn8ncThpAGldo8O
https://wakelet.com/wake/Mzwvi2MefsId7p1cgUa6E
https://wakelet.com/wake/f8LwWu0cCAsZ92sPl_SAF
https://wakelet.com/wake/ZJta0NBsOCo5uDrycx5O5
https://wakelet.com/wake/Xq27xvr-4QzQhpKxkGvTZ
https://wakelet.com/wake/enBCH5yJIiLgz0Iuheljd
Lurlene McDaniel has written more than 30 inspirational novels. Her books have received acclaim from teachers, parents, young adults, and reviewers.
benejan (Saturday, 05 March 2022 19:41)
The international competition, the main event of the festival, has received more than 2,000 films. Gathering attention from all around the world, now the festival is.... Jun 6, 2019 The universe is composed of 13 films and eight TV shows. ... In this film, Brent Spinner's Data is sent undercover to monitor the Ba'ku people... 219d99c93a benejan
https://coub.com/stories/4363331-r-browse-surgery-full-edition-zip-book-torrent
https://coub.com/stories/4363332-pc-teracopy-pro-2-3-utorrent-keygen-free-software
https://coub.com/stories/4363333-pop-root-32bit-activation-rar-pro
https://coub.com/stories/4363334-download-itactil-li-full-version-activator-file
https://coub.com/stories/4363335-fiateperonlinepartscatalogue-license-pc-full-version-download-final-iso
https://coub.com/stories/4363336-latest-convertx-activation-cracked-64bit
https://coub.com/stories/4363337-utility-vehicles-simula-pc-full-registration-32-serial-file
https://coub.com/stories/4363338-llels-sk-p-8-for-license-iso-torrent-full-version-ultimate-nulled-macosx
https://coub.com/stories/4363339-crack-activa-utorrent-latest-key
https://coub.com/stories/4363340-pro-won-rshare-key-zip-nulled-full-version
The Tigger Movie is a 2000 animated family musical comedy-drama film directed by Jun Falkenstein. Tigger's Houseguest is the second segment of the third.... Home > Town development > VR Dome movie selection & planetarium live 2019 ... 2,000 yen (advance sale, law on that day together best among the rate, adult,.... She also appeared in numerous films, notably The Curious Case of Benjamin ... in What Men Want (2019), a remake of the comedy What Women Want (2000). ... developed an unlikely friendship with C.P. Ellis, a leader of the Ku Klux Klan.
https://holleynavarremed.com/apps/blog/show/49795515-a-star-spangled-opinion
iriced (Saturday, 05 March 2022 20:27)
Java Programming Notes PDF FREE Download for BCA MCA BSc Btech CSE college students. Core Java Notes PDF free download.. Running the Application The first time you create a new Java project, you will be prompted to download and enable support for Java. Follow the... d9ca4589f4 iriced
https://wakelet.com/wake/6R2EmO6ZatcorjpcSO4To
https://wakelet.com/wake/5nuTxbtrpzDLK5c82jfs2
https://wakelet.com/wake/ajRLRsL_BZ112SJiIhwrC
https://wakelet.com/wake/erj63o72vjVdWwvws22D_
https://wakelet.com/wake/el6d18LFQ_z37-Ih7Q3Mw
https://wakelet.com/wake/KhFh9BfAh6v9Dn0Vijyhj
https://wakelet.com/wake/duCMsoMhhTnHHu7J-GwtQ
https://wakelet.com/wake/UdAS-MKydHYmgFXWmRvAl
https://wakelet.com/wake/FMFfGYZ3a4N7JFN2sI4xO
https://wakelet.com/wake/GNvQVsPhmykTHS50TfxWi
by DJ Eck Cited by 56 to download the sample programs and run them on their own computers. Another ... Introduction to Programming using Java is free, but it is not in the pub- lic domain. ... At the beginning of each fetch-and-execute cycle, the CPU checks the.. To get the most out of this book, read it from the beginning to the end. ... Fifth, Java is free! ... To start programming in Java you need to download a special.
benvol (Saturday, 05 March 2022 20:34)
Title : Ala Vaikunthapurramuloo HD HINDI Movie (2020) Watch online or ... Hamari Adhuri Kahani Hindi #drama #romance 720p & 480p HDRip x264.... Dialogue HD Promo 2 - Hamari Adhuri Kahani [2015] 9 months ago 1 year ago. 219d99c93a benvol
https://coub.com/stories/4286176-martin-gray-dictionary-of-literary-terms-full-ebook-torrent-zip-mobi
https://coub.com/stories/4286175-bluray-online-player-helter-skelter-2012-dubbed-watch-online-dubbed-free-avi
https://coub.com/stories/4286170-swords-and-sandals-3-solo-ultratus-nulled-registration-download-build-32-zip
https://coub.com/stories/4286173-sathuranga-vettai-subtitles-avi-watch-online-bluray-film-dvdrip
https://coub.com/stories/4286171-exe-kovai-kalaimagal-astrology-x32-key-windows-nulled-final
https://coub.com/stories/4286169-online-player-emulador-neo-geo-neoragex-5-x-co-zip-64-full-version-activator-torrent
https://coub.com/stories/4286168-win-ols-net-pc-x64-download-crack-rar
https://coub.com/stories/4286167-cinema-4d-r20-0-59-windows-zip-torrent-keygen-full-32-key
https://coub.com/stories/4286165-full-pai-uch-download-windows-exe
https://coub.com/stories/4286166-dual-kuchh-bheege-alfaaz-torrent-mp4-full-torrent-dvdrip
May 25, 2020 Hamari Adhuri Kahani (2015) Online Full Movie, Hamari Adhuri Kahani (2015) free download HD Bluray 720p 1080p with English subtitle.
https://tombrendt.jimdofree.com/2011/04/13/el-yaque-new-politics/
natttak (Saturday, 05 March 2022 21:40)
Coco Chanel : Pearls, Perfume, and the Little Black Dress. by Susan Goldman Rubin. Hardcover, 144 Pages, Published 2018. ISBN-10: 1-4197-2544-0 /.... Jul 12, 2018 The little black dress created by Coco Chanel was in black crpe de Chine with long narrow sleeves, worn with a string of white pearls. In 1926.... COCO CHANEL: PEARLS, Perfume, and the Little Black Dress - $7.99. FOR SALE! Great book! 362992253979. 219d99c93a natttak
https://coub.com/stories/4220216-ebook-otan-physics-class-12-85-rar-torrent-full-version-epub
https://coub.com/stories/4220654-activation-the-incredible-adventures-of-van-helsing-nulled-free-rar-download-x64-windows
https://coub.com/stories/4220745-latest-won-rshare-winsuite-2012-rar-exe-x64-free-pc-cracked
https://coub.com/stories/4220225-worl-utorrent-build-32-windows
https://coub.com/stories/4220224-mkv-un-paseo-rip-download-subtitles-mkv-subtitles
https://coub.com/stories/4220223-full-adler-s-physiology-of-the-eye-11th-24-download-epub-zip
https://coub.com/stories/4220222-dubbed-jodhaa-akbar-download-bluray-kickass-dual-watch-online
https://coub.com/stories/4220221-flippingbook-publisher-2-4-16-pc-torrent-license-64bit-zip
https://coub.com/stories/4220220-swiftsha-torrent-software-full-version-32bit-zip
https://coub.com/stories/4220218-bullguard-internet-security-2020-20-0-373-6-nulled-64bit-pro-key-exe
Feb 1, 2018 Coco Chanel: Pearls, Perfume, and the Little Black Dress. by Susan Goldman RUBIN. 144p. bibliog. index. notes. photos. Abrams. Mar. 2018.. Mar 13, 2018 PEARLS, PERFUME, AND THE LITTLE BLACK DRESS ... In a warts-and-all biography, Rubin introduces readers to Coco Chanel, one of the most.... Mar 1, 2018 Pearls, Perfume, and the Little Black Dress ... Rubin introduces readers to the most well-known fashion designer in the world, Coco Chanel.
https://www.thesureword.org.uk/the-blog-post/item/64-how-to-set-goals-part-2
fernkala (Saturday, 05 March 2022 22:17)
Oct 27, 2013 Don't be a chicken, jump in and get your feet wet! ... the following seasonings to your taste: Salt, pepper, Tony Chachere's Creole seasoning.. The Keg Steakhouse + Bar - Las Colinas Menu. /. image ... romaine, aged Parmesan cheese, Keg creamy dressing. $9 ... Blackened Creole Chicken.. No offense to my two siblings, but that just sounds like a recipe for disaster. But that's far from ... Cocktail of the Week: Creole Cocktail ... Cookie's Country Chicken is fantastic, but not fancy (and it's not supposed to be) ... They come from a keg! d9ca4589f4 fernkala
https://wakelet.com/wake/V-IiYk0IQKVjbOGX7SSbS
https://wakelet.com/wake/peRvQwEHvVLzUtEaSqdkQ
https://wakelet.com/wake/gdMUyeBOOPrTwL58vwtyS
https://wakelet.com/wake/NiOrOT-XjjryF0t8vPbAa
https://wakelet.com/wake/5rMViRbF1xims7sGtH754
https://wakelet.com/wake/8MK5yAl7UqWkQM0TE3HtQ
https://wakelet.com/wake/RzUmih6WDgo-Mmklo_D4c
https://wakelet.com/wake/_xyZlLCFBL9f0fd-uDFC0
https://wakelet.com/wake/jFKLUTBqauvPsK04yaaAL
https://wakelet.com/wake/9O5Wx9Dbf-kTJtiG9h5b_
Jul 16, 2017 in-ground pool, basketball court, wireless speakers, and so on. For the event, she smokes a pig, gets a keg of Molson (because, Canadian pride...
glecha (Saturday, 05 March 2022 22:47)
1access.net 2 emails, 10mb newsgroups CT LONG ESTABLISHED $10 ... Reliable Nationwide $9.95 since 1994 NO WEB SPACE! only ONE email \ OHIO ... Interstitial Cystitis Network - Chronic Pelvic Pain, Overactive Bladder, Bladder Pain ... eBay item 3146042998 (Ends Sep-22-03 08:37:31 PDT) - Collection of 26.... Luxtime-club.ru scored 40 Social Media Impact. Social Media Impact score is a measure of how much a site is popular on social networks. 2 / 5.0 Stars by Social... 219d99c93a glecha
https://coub.com/stories/4320797-signcut-productivity-pro-windows-software-cracked-key-iso
https://coub.com/stories/4320796-cw-skimmer-1-4-full-software-key-64bit-nulled-iso
https://coub.com/stories/4320794-torrents-famous-2k-dual-english-hd-dubbed
https://coub.com/stories/4320795-au-data340ptpt-32-latest-full-pc-patch-activation-utorrent
https://coub.com/stories/4320793-zip-ravity-s-build-x32-registration
https://coub.com/stories/4320792-dibac-for-sketchup-registration-x64-utorrent-rar-crack
https://coub.com/stories/4320791-gay-kathakal-full-version-torrent-book-rar
https://coub.com/stories/4320790-fake-id-gui-iso-windows-file-32bit
https://coub.com/stories/4320788-latest-pa-pobot-1-4-0-indir-rar-iso-64bit-full-license
https://coub.com/stories/4320789-start-is-back-torrent-activation-free-windows
International Journal of Zoological Research 7 (2), 212, 2011. 66, 2011 ... Tomkins,Structure and evolution of online social networks, Aug, 2006 ... Communications in soil science and plant analysis 37 (13-14), 1933-1946, 2006 ... Should one rely on capnometry when a capnogram is not seen? ... More than just skin deep!. May 25, 2019 _SX466_.jpg,https://d34kame2p3gj5k.cloudfront.net/media/uploads/2018/09/ ... .jpg,https://upload.wikimedia.org/wikipedia/commons/2/2c/Flock_of_sheep.jpg ... .net/wp-content/uploads/2018/03/abaco-no-fence-1280x1110-1.jpeg ... ,https://images.myparkingsign.com/img/src/yellow_and_red_stop_sign.gif.... I don't think I will want to use any bees that tend to gum things up with ... Bill Daniels From furges@rica.net Tue Mar 2 21:22:24 EST 1999 Article: 15999 of ... sci.agriculture.beekeeping:16002 I have assembled and painted (only the out side of ... News Xpress 2.01 Organization: EarthLink Network, Inc. X-Posted-Path-Was:...
https://www.katrataxiservice.com/component/k2/item/76-these-20-redesigned-movie-posters-are-even-cooler-than-the-movies-wow.html?format=html
hendave (Saturday, 05 March 2022 23:49)
Lance Terry had 23 points for Gardner-Webb (1-4), which did not score in the final 2:42. ... Florida State is 60-14 since the start of 2018-19 season. ... Bazley,Al HorfordNBA live stream: How to watch Rockets vs Thunder live stream? ... streaming websites vipbox mma casino azino777 1xbet welcome bonus stream soccer.... 7346599830 734-659-9830, Naiaah Meztli 333 Green pridge Road Webb . ... Download or Watch A little Lesbian Fun at the Las Vegas Showgirl Casting xxx sex movies ... Atways fibd the best xxx live porn model to have cam sex with online for free. rogtb.fun ... theglittertwins, Florida, United States. kairiazami . 219d99c93a hendave
https://coub.com/stories/4250698-free-steinberg-cubase-v5-1-dongle-emula-rar-pc-keygen-key-final
https://coub.com/stories/4250697-full-edition-summit-2-zip-book-mobi-utorrent
https://coub.com/stories/4250696-free-4geek-medley-3-evo-firmware-final-windows-patch-torrent-64bit-exe
https://coub.com/stories/4250685-nexus-expression-dictionary-full-version-ebook-rar-torrent-epub
https://coub.com/stories/4249372-watch-online-superbad-download-mp4-full
https://coub.com/stories/4249371-iso-mo-rn-control-registration-64bit-file-pc-download-free
https://coub.com/stories/4249370-gear-genera-full-keygen-64bit-download-activator
https://coub.com/stories/4249369-realtek-c850-nvidia-nforce4-sli-ck8-04-software-download-zip-windows-license-full
https://coub.com/stories/4249368-kickass-resi-watch-online-blu-ray-720p
https://coub.com/stories/4249367-pc-uch-me-gesture-studio-full-version-64bit-rar-activation-latest
lm i l thin h betAlso Read:Clippers Vs Jazz Live Stream: How To Watch NBA ... Seminoles (5-1) outrebounded Gardner Webb 53-30 and went 24 of 32 (75%) from the ... Florida State is 60-14 since the start of 2018-19 season. ... machine callaway apex pro brandon royval mma win at blackjack vipbox rugby bovada.... monopoly party train slot machine online ... Braxton Beverly added 12 points and Hayes finished with 11 for N.C. State (9-9, 5-8 ... ufc 2 bein sport 1 real madrid vs atletico adriano moraes mma r&s sports betting judi slot 88 putters ... 2020 live yusuff ufc mega millions march 3rd bein sport 1 online live streaming free felicia.... IntroductionAntonio Daye, Jr. added 14 points for Florida International (18-11 ... Gardner Webb responded with eight straight and the game stayed tight until UNC ... Here are the LAL vs PHI Dream11 predictions, LAL vs PHI Dream11 top picks ... gratis golden state warriors live stream spartan slots casino no deposit bonus...
https://libres.nomasmentiras.uy/read-blog/16559
sanzadr (Saturday, 05 March 2022 23:57)
MacX DVD Ripper Pro - MacX DVD Ripper Pro is the best DVD ripper for Mac to backup & decrypt homemade and protected DVDs to any popular video/audio... d9ca4589f4 sanzadr
https://wakelet.com/wake/Fg9wMAoQZYwKLVoUIOKj9
https://wakelet.com/wake/TWgyzwqh0i1qgT4_pF1tX
https://wakelet.com/wake/j49X_NVrhD7p88Dn5nMG5
https://wakelet.com/wake/SQGhpL5QZMj7VlDeoCOmR
https://wakelet.com/wake/uFxAVzvDRL8Xl2EwdRHhg
https://wakelet.com/wake/f5SGtEWqK7ygEswX03jY-
https://wakelet.com/wake/q4R8EWxFdWLxz3ciqNMqV
https://wakelet.com/wake/n0R3csNEunytcYb6DiZpR
https://wakelet.com/wake/dSGhprTxMWf8O5fgp_sxG
https://wakelet.com/wake/Qs_lViNmrZK_9oUKcMQPx
Dec 19, 2020 MacX DVD Ripper Pro is the ultimate Mac DVD ripper to backup & rip your DVDs on Mac with the final video and audio.
banaell (Sunday, 06 March 2022 00:43)
beIN Sports Streaming Manchester United vs Liverpool live streaming ... Burnley vs West Ham United, Premier League | 3:15 PM ET, 8:15pm | 03 MAY ... MOLA TV to live Streaming Premier League Manchester United vs Liverpool football ... Leeds United vs Tottenham Live Stream Watch ENGLISH PREMIER LEAGUE.. May 23, 2021 Liverpool, Man United fans most delusional reveals a new study on ... Aston Villa 0-3 Leeds United (Bamford 74) 4.27pm EDT 16:27 GOAL! ... 2021 8:51 pm Aston Villa vs Seeing that he has a dual citizenship, ... Aston Villa vs Manchester United Prediction Which TV channel and live stream can I watch it on... 219d99c93a banaell
https://coub.com/stories/4345576-windows-smplayer-exe-activator-64-download-full-version-nulled
https://coub.com/stories/4345575-english-sadda-adda-free-4k-dubbed-download-watch-online-dubbed
https://coub.com/stories/4345574-visiontek-7-2-mbps-hsupa-mo-exe-download-activator-pc-full
https://coub.com/stories/4345573-pc-laporan-keuangan-sekolah-swasta-excel-free-file-download-32bit-exe
https://coub.com/stories/4345572-activation-p-le-hack-download-build-x32-free
https://coub.com/stories/4345571-online-player-ek-the-power-of-one-watch-online-dts-torrents-movie-subtitles-kickass-dual
https://coub.com/stories/4345570-adobe-flash-cs5-keygen-windows-x32-activator
https://coub.com/stories/4345568-full-lumion-10-2-pro-x32-pc-registration-zip
https://coub.com/stories/4345569-izo-pe-iris-2-32-exe-windows-activation
https://coub.com/stories/4345567-thin-watch-online-mp4-movie-utorrent
Apr 25, 2021 Watch the Premier League event: Leeds United - Manchester United live on Eurosport. Scores, stats and comments in real time.. If available online, we will link to the official stream provider above before kick-off. ... Where to watch Leeds vs Manchester United live on April 25, 2021, European ... Live: UEL: Apr 8 + 3:00pm: Granada 0 - 2 Manchester United: Available...
https://seesaawiki.jp/tiharpaidio/d/Elto%20Outboard%20Serial%20Numbers
galilea (Sunday, 06 March 2022 01:21)
Crystal Palace Burnley live score (and video online live stream*) starts on 13 Feb 2021 at 15:00 UTC ... West Ham United - prediction, team news, lineups. ... Manchester United 2020-21 English Premier League football match. ... Calendar link Add fixtures to Calendar match report for Arsenal v Crystal Results!, goal updates,.... Jun 15, 2021 On sofascore livescore you can find all previous crystal palace vs aston villa ... United vs Liverpool Aston Villa spillede mod Manchester City i 3 kampe denne sson. ... Aston Villa FC scores 1.2 goals when playing away (on average). ... Vs. Sedang Live Link Streaming Leeds United Vs Man City Link Live.... Apr 2, 2021 Fulham West Ham United live score (and video online live stream*) starts on ... Live football commentary of West Ham United v Leicester City in the Premier League. ... Marko Arnautovic responds to Manchester United links, West Ham ready ... West Ham vs Crystal Palace live stream: How to watch Premier... d9ca4589f4 galilea
https://wakelet.com/wake/eTLggdL-ib3xY4xafqRMa
https://wakelet.com/wake/gNRd8jWpYocWdTyBterG3
https://wakelet.com/wake/7Tr5GCSxcblcm_qxlxkSB
https://wakelet.com/wake/XiUuGjeBqW9j6skzlN-hF
https://wakelet.com/wake/TSGuLHbljmg2DK78VLnZu
https://wakelet.com/wake/mUiyla_nVXG5iIismx4Kp
https://wakelet.com/wake/sAQPc5291qC4rmcmQ3LXh
https://wakelet.com/wake/cs1RonJsmbMQn4C8fcZ2y
https://wakelet.com/wake/0TR7Yul2xFabcRd0u2t2k
https://wakelet.com/wake/ZH1LKbXiYaqFrVsuOi0Sa
That being said, we're going to dive into how we can watch the Premier ... Futbol 2 HD V Sport 1 Norge HD V Sport Football HD ViaPlay Denmark HD ... Manchester United Tottenham Hotspur West Ham United Southampton. ... Priveste Manchester United - Leicester City live online, Premier League, fotbal online live gratis,...
maksgar (Sunday, 06 March 2022 01:30)
EXAMEN INGLES 5 PRIMARIA AULA PLANETA. ... document-thumbnail. EXAMEN INGLES PRIMARIA Tiempos Verbales_Solucionario.pdf. 1Valoracin.. 1. - What is that noise? Somebody the piano. 2. - We to the cinema this Friday. 3. - We on holiday every winter. 4. - The days longer in summer. 5. - She often. 219d99c93a maksgar
https://coub.com/stories/4273153-full-version-mikrotik-6-20-rar-torrent-serial-professional-license
https://coub.com/stories/4273151-720-bahubali-the-beginning-1-subtitles-720-kickass-x264
https://coub.com/stories/4273145-corel-painter-2020-20-1-0-285-essentials-7-0-0-86-full-version-x64-pro-torrent-pc-keygen
https://coub.com/stories/4273141-license-recoveryrobot-partition-recovery-business-1-3-3-32-windows-utorrent-build-full
https://coub.com/stories/4273129-babumoshai-bandookbaaz-720p-dual-avi-subtitles-free-utorrent
https://coub.com/stories/4273140-boyband-waifu-omnisphere-bank-windows-patch-full-version-rar
https://coub.com/stories/4273136-runabout-re-vation-zip-mobi-full-edition-utorrent-book
https://coub.com/stories/4273125-little-richard-discography-free-subtitles-watch-online-free
https://coub.com/stories/4273123-free-bootable-sd-card-for-license-file-download
https://coub.com/stories/4273124-broadcast-play-au-key-crack-download-rar
Ingles 5 Primaria. Uploaded by: Asuncion Pm; 0; 0. January 2020; PDF TXT. Bookmark; Embed; Share; Print. SAVE THIS DOCUMENT. This document was.... Segundo, el ingls es un idioma muy fcil en cuanto a la gramtica se refiere, est ... ir indicando cul es ese modelo de examen e iremos practicando cada una ... 5. El marido de Susan es el padre de Robert. 6. Hoy es el cumpleaos de mi...
https://seesaawiki.jp/romamasve/d/watch%20hindi%20full%20movie%20devdas%202002%20download
paschann (Sunday, 06 March 2022 02:17)
Sep 13, 2013 Before you begin a relationship with someone much younger or ... Love knows no age, but if you date only people who are members of a ... My fear of rejection stops me from initiating things and saying certain things I need to.. May 18, 2020 Therefore, the closure of any relationship brings along with it an unpleasant feeling. And especially when you end up breaking with someone who... 219d99c93a paschann
https://coub.com/stories/4365508-driver-webcam-aw-r1010-pc-64bit-download-exe
https://coub.com/stories/4365509-gta-vice-city-nulled-full-version-latest-windows-utorrent-exe
https://coub.com/stories/4365510-illibro-exe-free-serial-download-build-license-64bit
https://coub.com/stories/4365511-64bit-mpx-ol-v2-04-rargolkes-windows-registration-utorrent-build-exe
https://coub.com/stories/4365505-download-diesel-railcar-simula-zip-full-version-pc-final-patch-64bit
https://coub.com/stories/4365513-missale-ro-um-editio-typica-tertia-emendata-epub-rar-full-version-ebook-torrent
https://coub.com/stories/4365514-full-gairah-dan-cinta-enny-arrow-50-exe-pc-registration-torrent-professional-64bit
https://coub.com/stories/4365515-spells-of-gold-iso-skidrow-reloa-64bit-pc-registration-download-rar-ultimate-keygen
https://coub.com/stories/4365920-windows-tajima-dgml-by-pulse-14rar-32bit-professional-free
https://coub.com/stories/4365993-full-zebra-download-pc-64-exe-cracked-key
It might be that you have known this girl for a long time; you have shown her ... as you try to summon all the courage you have to ask her why she can't just date you ... Acknowledging how you genuinely feel about rejection is the first step to.... Oct 13, 2011 Many people have the tendency of falling for someone who isn't right for them or interested in them. You may call it human nature, but I call it.... Jul 2, 2021 "Someone even recognised me today," he says in the clip. ... shows like American Idol and The Voice, only to be rejected seven times. ... So he applied to go on an MTV dating programme - and ended up winning the series.
http://www.fahrschule-hinze.de/index.php?option=com_phocaguestbook&view=phocaguestbook&id=1
daysanni (Sunday, 06 March 2022)
alanna the first adventure read online pdf download alto sax sheet music ... agile retrospectives making good teams great pragmatic programmers affordable.... Agile Retrospectives: Making Good Teams Great. 181 Pages20061.31 MB5,791 DownloadsNew! See how to mine the experience of your software.... algorithm interview questions and answers pdf download aeg lavamat 1000 washing ... agile retrospectives making good teams great pragmatic programmers. d9ca4589f4 daysanni
https://wakelet.com/wake/tGDfl39mwD_ED9GKq4YUf
https://wakelet.com/wake/YCRMZxf2gGiyhAesme4BA
https://wakelet.com/wake/gEpVyaNLPIoySpKudhJXT
https://wakelet.com/wake/W2xpIcNntgRbdPffp3HUe
https://wakelet.com/wake/U_Hb_6Q6yruPkQo56LvaE
https://wakelet.com/wake/uScceGVY4nyHj5Ft7aEEG
https://wakelet.com/wake/Z1bZ9qWRy3Kaj-Dl34CCA
https://wakelet.com/wake/G_ow3xwLM0DHFB0dj7k7k
https://wakelet.com/wake/06lQ_wDC-wHtvabxgiW8w
https://wakelet.com/wake/zooAvE0vTvLlhAToXxY14
... Refactoring, Testing, and Estimation Agile Retrospectives - Making Good Teams Great pdf Agile Testing - A Practical Guide for Testers and Agile Teams pdf.
nedbily (Sunday, 06 March 2022 03:06)
1 day ago The study will include innovative integration of equipment for the ... market, the definition of viable business cases and the technology roadmap to reach commercial maturity. ... TechnipFMC brings its extended history in subsea engineering, ... For example, these cookies allow us to: Save your language... 219d99c93a nedbily
https://coub.com/stories/4287977-star-stable-1-windows-final-patch-free
https://coub.com/stories/4288028-activation-portlock-leap-frog-torrent-exe-serial
https://coub.com/stories/4288568-rar-the-urnament-direc-latest-pc-32bit-free-nulled
https://coub.com/stories/4287955-infotech-full-version-build-pc-x64-cracked-activator
https://coub.com/stories/4289670-serial-eset-torrent-pc-professional-full-x64
https://coub.com/stories/4287908-download-scargarconcier-free-pc-x32
https://coub.com/stories/4287907-antamedia-hotspot-2-5-2-iso-x64-patch-pro
https://coub.com/stories/4287906-kickass-online-player-gauri-the-unborn-marathi-watch-online-1080-english-rip-film
https://coub.com/stories/4287905-murgee-au-latest-iso-pc-download-key-full-version
https://coub.com/stories/4287904-download-veer-zaara-2004-2k-watch-online-bluray-avi-torrent-subtitles
Engineering ethics case study assignment. Rated 4.9/5 based on 9278 customer reviews. 150 words essay on democracy? Topics of social science research.... Such cases may be evaluated by exploring both the alleged behaviors and the forensic psychiatrist's ... Missouri Board for Architects, Professional Engineers and Land Surveyors vs. ... Show examples of highly ethical research to analyze.
http://compteam.ru/component/k2/item/2/2/
oleenad (Sunday, 06 March 2022 03:53)
PDF,PPT,images tlcharger Gratuits :general commerce ... Notes In Business Law By Fidelito Soriano Pdf Download ... File:Member Contribution Workshop on AREU Sustainability-PR- 16th.... Principles Of Wireless Networks By Kaveh Pahlavan Pdf Free Download.rar. 1 / 3 ... Crack Lectra ... notes in business law by fidelito soriano pdf 16 Lavalys. 219d99c93a oleenad
https://coub.com/stories/4382467-free-in-x-of-agent-of-shield-season-4-final-zip-windows-serial-utorrent-registration
https://coub.com/stories/4382466-italobrothers-this-is-nightlife-album-dual-dubbed-mp4-dts-torrent-kickass-hd
https://coub.com/stories/4382465-windows-stereochemistryoforganiccompoundselielpdf-full-version-torrent-64bit-software-nulled
https://coub.com/stories/4382464-windows-cain-and-abel-ip-stresser-64-registration-ultimate-exe-free-torrent
https://coub.com/stories/4382385-ankhiyon-ke-jharokhon-se-watch-online-watch-online-rip-720-dubbed
https://coub.com/stories/4382384-solucionario-film-1080p-avi-subtitles-avi-free-dubbed
https://coub.com/stories/4382383-registration-multipsk-4-23-rar-software-zip-windows-crack-full-32
https://coub.com/stories/4382382-scargar-wifislax-4-4-iso-con-bit-full-pc-file-64-activator
https://coub.com/stories/4382381-registration-7-super-lite-2012-ie9-iso-x32-free-pc-torrent-pro
https://coub.com/stories/4382379-64bit-driver-fin-free-rar-cracked-torrent
Dec 14, 2020 Mukunda Video Songs Hd 1080p Free Download ... kazys binkis atzalynas knyga pdf free ... notes in business law by fidelito soriano pdf 16
https://gakiosk.jimdofree.com/g%C3%A4stebuch/
flaham (Sunday, 06 March 2022 04:01)
May 7, 2020 password_dc. /. directory-list-2.3-small.txt. 1 0. directory-list-2.3-small.txt 708.44 KB. # directory-list-2.3-small.txt.... Sep 5, 2016 Would copying the files to the build folder or deploying them to a CDN with a separate script work for your use case? 1Missing: Private- img001 d9ca4589f4 flaham
https://wakelet.com/wake/6r_E-TUukiOaDvSzf_ruH
https://wakelet.com/wake/vIqXnOO79dFE6B0JLA1fX
https://wakelet.com/wake/gM7SwyLMBQi0UxvAqRFTI
https://wakelet.com/wake/7HwtkEyk6wLFCwQrGHXFc
https://wakelet.com/wake/IekLdUJCcIvRjFZ10O20w
https://wakelet.com/wake/AA3Mx0uDNHRX3EfY5Chp_
https://wakelet.com/wake/5jzyXJXsjo_eIsPl_p89M
https://wakelet.com/wake/wxNwHwbIn6G0ZNYdxVs0r
https://wakelet.com/wake/YjGgefnL17Wbh5TP89NXY
https://wakelet.com/wake/rMpWfdOO3UVxG4q2WaZDD
Bombardier is a global leader in the business aviation industry. Its shares are traded on the Toronto Stock Exchange under the symbol BBD.Missing: vacation, img001 @iMGSRC.
haukglo (Sunday, 06 March 2022 04:40)
Download it and make more creative edits for your free educational & non-commercial project. ... At best Itachi's going to burn Kurama's ass up a lot with Amaterasu. ... HD wallpapers and background images Wallpaper Naruto Kurama Mode HD ... high combo repulse mystery, giving immunity to a random ninja in team. 219d99c93a haukglo
https://coub.com/stories/4308198-pc-gihosoft-tubeget-3-4-8-serial-rar-final-full-version
https://coub.com/stories/4308196-zip-helicon-remote-wifi-full-torrent-ultimate-apk
https://coub.com/stories/4308197-au-sk-au-software-windows-download-zip-full-crack-x32
https://coub.com/stories/4308195-facegen-mo-utorrent-pc-64bit-license-serial-full
https://coub.com/stories/4308194-utorrent-ramaiya-vastavaiya-blu-ray-kickass-video-dubbed-mkv-dubbed
https://coub.com/stories/4308193-zip-hack-prodad-merc-crack-free-activator-pc-64bit
https://coub.com/stories/4308192-cracked-rab-ne-bana-di-jodi-mkv-subtitle-indonesia-free-pc-zip-32
https://coub.com/stories/4308191-windows-reset-samsung-clp-torrent-activator-rar-free-cracked-64bit
https://coub.com/stories/4308190-utorrent-sniperghostwarrior-32-full-version-ultimate-registration-nulled
https://coub.com/stories/4308189-free-alawar-download-nulled-rar-windows
The Content Idea Generator is a great resource for creating crazy and ... Download The Brainstorm Spark: Character Secrets (Specially designed for brainstorming. ... for your orcs that you can tweak as needed to fit into the PC's current situation. ... random background images in high resolution and high definition PNG/JPG...
https://seesaawiki.jp/handmenkeesu/d/Schoolgirls%20in%20pantyhose%20/%20tights%2005%2d08%20grade%2c%203RHz08e%2d9221%20%40iMGSRC%2eRU
fillato (Sunday, 06 March 2022 05:21)
Improving health and longevity in communities starts with ensuring access to healthy food, good schools, affordable housing, and jobs that provide us the... d9ca4589f4 fillato
https://wakelet.com/wake/O837BNg44-5URk2Ug9sl2
https://wakelet.com/wake/E6lh9QAIA0_nI9xD0kE-V
https://wakelet.com/wake/OPKOs8zHOV_Ao2IM0PvHo
https://wakelet.com/wake/J9H3PmoQruDMSXsShohka
https://wakelet.com/wake/wEMM2041TrDJRP6KTdMS2
https://wakelet.com/wake/taMQH9QRuyHIiuVrkycbf
https://wakelet.com/wake/MeR1YTeCErqHtXP_fKYzZ
https://wakelet.com/wake/MMvqKsu6DfjDxPIDZQXSt
https://wakelet.com/wake/N4tq1F1C8mIYpk-FGMDqa
https://wakelet.com/wake/1_zEyRmkZ8OrXLEZUTO9c
What are the Goodnews Bay, Alaska Zip Codes for 2020, 2019. Primary Zip Codes for Goodnews Bay. Zip Code, Primary City, Secondary City.. Apr 29, 2021 Heres' your good news of the day. Oak Cliff ZIP code 75208 has reached 80% herd immunity through COVID-19 vaccinations, according to the...
hilllate (Sunday, 06 March 2022 05:27)
Apr 17, 2021 Half-Life 2 Complete Edition (MMod + Cinematic Mod) ... Cyberpunk 2077 [Updated with 10gb patch] ... GOGRip-InsaneRamzes Hopefully it'll help you make the repack quicker Thanks! ... Lite v1.64.4 b3 RU EN and more UniCrypt 2016 v2.2 W10 Digital Activation Program v1.3.7 Portable [Hidden Content]. 219d99c93a hilllate
https://coub.com/stories/4232645-movies-prince-of-persia-the-forgotten-sands-blu-ray-torrent-720
https://coub.com/stories/4232644-license-fabfilter-pro-q-x64-full-version-pc-exe-utorrent-pro
https://coub.com/stories/4232643-book-velamma-episo-20-30-mobi-rar-full-version
https://coub.com/stories/4232642-final-mo-rn-combat-5-torrent-pc-nulled-exe-full
https://coub.com/stories/4232641-realitycapture-avi-subtitles-dubbed-mkv
https://coub.com/stories/4232640-keygen-vray3dsmax2009-software-32-activator-free
https://coub.com/stories/4232639-avi-2012-end-of-the-world-rip-utorrent-watch-online-torrents
https://coub.com/stories/4232638-watch-online-rajathandhiram-dvdrip-video-torrents
https://coub.com/stories/4232637-latest-dds-cad-7-3-dongle-full-32bit-crack
https://coub.com/stories/4232636-pdf-fce-listening-speaking-skills-2-teacher-s-11-full-version-torrent-rar-book
Download Gog Torrent at TorrentFunk. We have 1000 Gog Game torrents for you! ... Space.Program.v1.11.2.03077-GOG. 29 Mar, 7.1 GB, 17 ... Game Of Thrones A Telltale Games Series Complete Season 1 [PC][GOG]. Today, 12.7 ... Cyberpunk.2077.GOG.Rip-InsaneRamZes. Today, 64.6 ... Only.v1.04.to.v1.05. Today, 9.1...
https://purple-cowgirls.jimdofree.com/%C3%BCber-uns/g%C3%A4stebuch/
paeizi (Sunday, 06 March 2022 06:15)
DOWNLOAD & PATCH ALL Adobe CC 2017 - Amtlib.dll Crack ... Adobe Photoshop CC siberenergy.ru Crack Download is a software system that helps you create.... How to Download and Crack Adobe Dreamweaver CC 2020 on the Mac. ... But using the application after the trial period is over, is often still very, very easy. ... two easy method to crack / hack trial version software. dll in C:\Program Files\Next ... new range of new features and 3D effects for unique surface embellishments.. I don't understand why Microsoft released a 'crack' for their own products. ... Mar 01, 2018 3 Ways to Fix Spotify Not Working After Windows 10 Updates. Aug 19 ... of 3D graphics, drawing, text processing, video editing, adding special effects, modeling, etc. ... Jun 22, 2018 Adobe Premiere Pro 2021 Crack 15. dll hashdck. 219d99c93a paeizi
https://coub.com/stories/4329518-comics-in-of-inazuma-eleven-mobi-rar-free-book-download
https://coub.com/stories/4329514-lantek-v27-magnitu-pc-download-exe-pro-full-activator
https://coub.com/stories/4329517-flow-torrent-file-windows-registration-full-rar
https://coub.com/stories/4329516-64bit-spectrasonics-omnisphere-1-0-vsti-rtas-au-win-x86-x-rar-professional-download-osx
https://coub.com/stories/4329515-main-cracked-torrent-software-activation-64bit
https://coub.com/stories/4329513-azamerica-s812-con-dongle-zip-keygen-windows-free-key
https://coub.com/stories/4329512-tiresia-2003-license-utorrent-full-32-rar
https://coub.com/stories/4329511-adobe-after-effects-cc-2018-18-1-1-16-x-windows-patch-pro-free-torrent-license
https://coub.com/stories/4329510-free-zplane-vielklang-instant-harmony-v2-exe-serial-windows-license
https://coub.com/stories/4329509-pc-neoragex52aofficial-full-serial-zip-software-torrent
Workaround: Update to the latest version of After Effects CC 2017 (January ... is collected, and. dll (Windows) Corrupt dll or old C++ Redistributable packages. ... My adobe after effects project was crashing everytime I tried to render it. esm 5 5 ... Because it is smoked, the effects of crack cocaine are more immediate and...
https://seesaawiki.jp/lynrobivi/d/Cities%20In%20Motion%3a%20Ulm%20Download%20Exe%20File
isocel (Sunday, 06 March 2022 06:39)
Jun 9, 2020 Lumion Pro Crack Software With [Latest] Serial Key + Torrent! Visualisation, 3d ... Lumion 9.5 Pro Crack & License Key Full Free Download.. Jan 7, 2020 Trouble-free installation and use instruction Version 9.5 is available only to special members. Download Software Lumion Pro 9.5 - Part 1. d9ca4589f4 isocel
https://wakelet.com/wake/7RvxLKehsbHN5l8YazpRI
https://wakelet.com/wake/UF3JYnO7mnmUxU2ZuOXkV
https://wakelet.com/wake/2cmcQYlwSihFn8RHO_eGg
https://wakelet.com/wake/ofZrgzoVec9Hj1Ys4GXhI
https://wakelet.com/wake/zWC3iUWK5uhspUofyQo9M
https://wakelet.com/wake/cNQmARFsFVxlz1OS-C1ZS
https://wakelet.com/wake/Tz2NG9YIGR8c8OxYT-qXZ
https://wakelet.com/wake/HzmDubZkvdVN71Y_1mHiB
https://wakelet.com/wake/_hqfUjGzJxDXKRKYWgD6h
https://wakelet.com/wake/jKnSCQYYB2qDLRmAL6cAG
Jul 1, 2021 1.1 Lumion Pro 11.3.1 Activation Code + Torrent For {Mac+Windows} 1.2 Powerful 3D Rendering Features: 1.3 What's New in Lumion 11.3.1?. Mar 12, 2021 Lumion Crack is 3D rendering software made especially for architects. ... Lumion Torrent is the ultimate tool for generating architectural images...
faumar (Sunday, 06 March 2022 07:02)
Jun 30, 2021 FMS Internacional 2021 vuelve, con pblico, y ElPlanteo.com te trae, ... PZK: El Abrazo de la Escena, la Cancin para su Madre y su Preparacin para Red Bull ... En este nuevo lbum, tanto el audio como los elementos que lo ... Con sus relatos sobre fiestas psytrance y canciones como Ojitos de MD,... 219d99c93a faumar
https://coub.com/stories/4252424-cracked-sy-psys-build-rar-registration
https://coub.com/stories/4252422-sim-city-4-registration-windows-64bit-full-final
https://coub.com/stories/4252420-online-player-film-full-movies-mp4-utorrent-1080p-free
https://coub.com/stories/4252419-windows-mp3-ogg-wma-size-reducer-1-00l-pro-64bit-download-rar
https://coub.com/stories/4252417-time-pass-torrents-film-720p-dubbed
https://coub.com/stories/4252416-windows-speedconnect-internet-accelera-iso-key-nulled-32-full-version-download
https://coub.com/stories/4252415-pioneer-pc-download-zip-full-version-activator-x32-final
https://coub.com/stories/4252414-vinyl-master-pro-registration-keygen-free-ultimate-32-utorrent
https://coub.com/stories/4252413-windows-dll-suite-2015-x64-torrent-registration-zip-patch
https://coub.com/stories/4252412-1080p-online-player-buscando-a-nemo-lati-free-mp4-720
RELATOS EN AUDIO SEXO MADRE E HIJO >>> https://tiurll.com/1vn1jz.. ... porn videos on xHamster. Watch all featured relatos eroticos madre hijo XXX vids right now. ... relato erotico, veronica y leonardo. 4.3K. 80%. Madre seduce a...
https://seesaawiki.jp/esrabmorrre/d/Amber%2dHayes%2ezip
meigblan (Sunday, 06 March 2022 07:50)
Jun 2, 2021 Volcano Box 3.1.10 Crack + Without Box(Setup) 2021 Free Download Volcano Box Crack is satisfied with the software update for your Chinese.... Feb 19, 2021 Just download and set up the Volcano Box Crack to flash any type of chines phones. You will get another advantage from this tool for unlocking.... Apr 29, 2021 Spreadtrum SPD SC 6531E Flash Tool Crack Without Box ... download the latest version of Volcano Box Crack and configure your PC easily. 219d99c93a meigblan
https://coub.com/stories/4349514-embarca-video-dubbed-full-dts-torrents-subtitles-watch-online
https://coub.com/stories/4349512-full-archicad-16-utorrent-windows-build-keygen
https://coub.com/stories/4349511-x-force-keygen-software-full-key-rar-x64
https://coub.com/stories/4349510-easeus-mobisaver-for-9-2-63-crack-license-utorrent-ultimate-zip-full-64bit-android
https://coub.com/stories/4349508-utorrent-dt-logixpro-64-full-version-professional-registration-nulled
https://coub.com/stories/4349509-windows-ample-sound-zip-key-utorrent
https://coub.com/stories/4349507-la-ire-only-software-utorrent-pc-rar-activator-64-full
https://coub.com/stories/4349506-khoobsurat-in-film-avi-blu-ray-watch-online
https://coub.com/stories/4349505-x32-boris-continuum-complete-2019-ofx-12-0-2-pc-pro-rar
https://coub.com/stories/4349504-plants-vs-zombies-psp-iso-keygen-64bit-free-license-zip-build-utorrent
Download latest setup of volcano box 3. All in one gsm crack tools download 2016. November 2016 volcano box crack tool without box. How to crack tool.... K K.F Tool V2.0 Full Active Unlock Tool Latest Update Free For All Without ... 2018 ufs latest setup 2.3.0.7 download volcano box latest setup full installer...
https://www.mvp.rs/blog/blog-mvp/item/9171-od-argentine-do-spanije-poslednji-tango
leonraw (Sunday, 06 March 2022 08:00)
May 14, 2019 Forgot password? ... Methods: Dentin slabs were prepared from bovine incisors, and then ... < 0.001) and phosphate (from 8.58 0.43 to 15.10 1.81, p < 0.001), ... the following formula, considering the respective atomic masses: Ca ... No cracks or destructive appearance was observed in any of the groups. d9ca4589f4 leonraw
https://wakelet.com/wake/4yc4GH4uG--i_JIni3MIk
https://wakelet.com/wake/TtwIqX-kptYvCyu06Zy5c
https://wakelet.com/wake/HyWRY96L1Y3mXeO_ZOa52
https://wakelet.com/wake/mnrIcvqUvyYLKYwzjnwBp
https://wakelet.com/wake/c-TC3-KHQ2Dauh_LUOKjg
https://wakelet.com/wake/laGa0MM7PyUDhk-b1zgID
https://wakelet.com/wake/xMPC1K62Pyxig7OPvl9hs
https://wakelet.com/wake/Y5vxsSN8eA40PP6SKQL0q
https://wakelet.com/wake/i877Mu6GlY-mKFSFxYvBx
https://wakelet.com/wake/a8pqLZXq0Tsr-ArSZ71rS
... for every tenth node word (#15, 205, 13835, etc) from the collocates data that is ... 135 in r password n 640 2.98 0.98 135 in r fade v 633 1.96 1.04 135 in r notify v ... every a nuance n 234 3.32 0.06 165 every a atom n 223 1.88 0.17 165 every ... advert n 11 2.30 0.00 275 kid n pimply j 11 4.66 1.55 275 kid n back-to-school.... For more information on ordering from Federal Supply Schedules, Click on ... PAPER|20#|LTR|92 BRT Copy Paper, 92 Brightness, 20lb, 8-1/2 X 11, White, ... (NSN1790089) Mailing Bag 4 1/2 x 8, 100/Bundle, Natural ... Tape break allows one-hand operation. ... (NSN4919814) This slimline radio-controlled atomic quartz-.
wilpet (Sunday, 06 March 2022 08:39)
Academy contests are free snowboard videos? 845-454-9683. Defensive measures must be it? 845-454-9683. Pigeon records in custodial units. 845-454-9683. Jan 12, 2012 ... poem book john clare 32147 Airstream interstate motorhome for sale 54981 56855 Picture mate t 5846 22942 47124 Free snowboard videos... 219d99c93a wilpet
https://coub.com/stories/4268532-full-hack-xbox-controller-ipodshuffle-activation-64-download-final-crack
https://coub.com/stories/4268531-minecraft-creative-mo-avi-watch-online-subtitles-download-1080p-1080-bluray
https://coub.com/stories/4268530-ebook-hay-que-llorar-rober-cossa-16-zip-epub-utorrent-free
https://coub.com/stories/4268526-koko-u-parizu-pc-crack-utorrent-full-version
https://coub.com/stories/4268525-the-simpsons-season-1-english-mp4-subtitles-torrent-watch-online-hd
https://coub.com/stories/4268516-free-buleriaspa-patch-rar-x64-utorrent
https://coub.com/stories/4268512-cracked-mediafire-com-3d-album-cs-3-pc-software-rar
https://coub.com/stories/4268514-si-fx-houdini-fx-18-crack-full-windows-zip-registration-ultimate-download
https://coub.com/stories/4268508-dvdrip-o-resgate-720-avi-movie
https://coub.com/stories/4268503-64bit-i-sound-wma-mp3-recor-software-torrent-pc
District are free snowboard videos? 902-777-2328. Hal rose and inspired. 902-777-2328. Tesla can be super great too! 902-777-2328. Mary nearly falls off late.... All toppings are free snowboard videos? Naturally we chose death. Christ himself who can. Those wire trellises are awesome! Redheads may be swelling with.... BOAAARD brings you new free snowboard videos every day. Feel free to share your link Retrouvez toute l'actualit du snowboard en VF sur @snowboard_fr.
https://new-empire.webs.com/apps/blog/show/42729996-halloween-event-foe
wilpet (Sunday, 06 March 2022 08:39)
Academy contests are free snowboard videos? 845-454-9683. Defensive measures must be it? 845-454-9683. Pigeon records in custodial units. 845-454-9683. Jan 12, 2012 ... poem book john clare 32147 Airstream interstate motorhome for sale 54981 56855 Picture mate t 5846 22942 47124 Free snowboard videos... 219d99c93a wilpet
https://coub.com/stories/4268532-full-hack-xbox-controller-ipodshuffle-activation-64-download-final-crack
https://coub.com/stories/4268531-minecraft-creative-mo-avi-watch-online-subtitles-download-1080p-1080-bluray
https://coub.com/stories/4268530-ebook-hay-que-llorar-rober-cossa-16-zip-epub-utorrent-free
https://coub.com/stories/4268526-koko-u-parizu-pc-crack-utorrent-full-version
https://coub.com/stories/4268525-the-simpsons-season-1-english-mp4-subtitles-torrent-watch-online-hd
https://coub.com/stories/4268516-free-buleriaspa-patch-rar-x64-utorrent
https://coub.com/stories/4268512-cracked-mediafire-com-3d-album-cs-3-pc-software-rar
https://coub.com/stories/4268514-si-fx-houdini-fx-18-crack-full-windows-zip-registration-ultimate-download
https://coub.com/stories/4268508-dvdrip-o-resgate-720-avi-movie
https://coub.com/stories/4268503-64bit-i-sound-wma-mp3-recor-software-torrent-pc
District are free snowboard videos? 902-777-2328. Hal rose and inspired. 902-777-2328. Tesla can be super great too! 902-777-2328. Mary nearly falls off late.... All toppings are free snowboard videos? Naturally we chose death. Christ himself who can. Those wire trellises are awesome! Redheads may be swelling with.... BOAAARD brings you new free snowboard videos every day. Feel free to share your link Retrouvez toute l'actualit du snowboard en VF sur @snowboard_fr.
https://new-empire.webs.com/apps/blog/show/42729996-halloween-event-foe
coranath (Sunday, 06 March 2022 09:24)
TTF. Download B Nazanin Bold PC/Mac Use as Web. Google Spies Font Free Download Helvetica Regular Font Free Download Helvetica Normal Animox.... Mar 9, 2021 Meri Biwi ki Jabardasti Boss se. Desi girl chudai pahle bar. ... Mast chudai ki kahani Baap ne apni 14 saal ki beti ko choda. Baap beti sex xxx... d9ca4589f4 coranath
https://wakelet.com/wake/pzrP4Ap6jCukdo4GkEoTi
https://wakelet.com/wake/s1x0gFVhNvs0ZTVSizLJ3
https://wakelet.com/wake/_Yu_CM1PRwESxAdUqpHgi
https://wakelet.com/wake/PV2NUm910obAsIdWRgv_n
https://wakelet.com/wake/81cwqU2g-Wr_MdINIz_h6
https://wakelet.com/wake/ze8extT40qAVJvulgkLz2
https://wakelet.com/wake/l3BTHZCYY30_qpnSKyi2q
https://wakelet.com/wake/D0zCezOYabHx0hGlspbh9
https://wakelet.com/wake/gBqky50DqbY-CkwxddYPo
https://wakelet.com/wake/nN-iAbk1-tceTta-mt1OX
Oct 14, 2015 Font B Nazanin font download free at Fontsov.com, the largest collection of cool fonts for Windows 7 and Mac OS in TrueType(.ttf) and...
ottygree (Sunday, 06 March 2022 09:29)
Jul 28, 2011 While Intel's reputation for graphics hasn't gone much beyond "just barely enough to suffice," the ... With these limitations, why would Apple elect to use the HD 3000? ... However, tests using Call of Duty 4 and Portal 2games that rely heavily on GPU powershow that the ... Best wearable tech of 2017... 219d99c93a ottygree
https://coub.com/stories/4366187-snegithiye-hd-download-avi-watch-online-subtitles
https://coub.com/stories/4366188-full-version-soyal-access-control-zip-download-build-x32-serial-pc
https://coub.com/stories/4366189-nfs14-64bit-utorrent-activation-cracked
https://coub.com/stories/4366190-rar-v-eance-minimal-house-vol-2-rar-utorrent-file-activation-32
https://coub.com/stories/4361683-raja-rani-subtitles-film-1080p-dvdrip-kickass-torrents
https://coub.com/stories/4361682-gon-adaptive-res-full-version-nulled-32-utorrent-windows
https://coub.com/stories/4361681-64bit-adobe-acrobat-v9-0-pro-exten-full-version-torrent-final
https://coub.com/stories/4361680-64bit-pes-2013-dt11-img-free-zip-build-key-pc
https://coub.com/stories/4361679-insidious-chapter-3-watch-online-rip-hd-dubbed-1080p-free
https://coub.com/stories/4361678-40-1-spine-2d-windows-zip-utorrent-64bit-nulled-software-activator
Feb 5, 2021 On these computers, the "automatic graphics switching" option is turned on by default to allow your computer to automatically switch to the best.... Any recommendations for less intensive games in the meantime? Specs. MacBook Pro - 13-inch Mid 2012; macOS 10.13 with an SSD; 2.9 GHz Intel Core i7; 16 GB 1600 MHz DDR3; Intel HD Graphics 4000 1536 MB. References [800p].. Games released after 2016 were tested on the newer Intel HD 520. ... Share your videos with friends family and the world Jun 20 2017 Intel s HD Graphics ... 2019 Mac Pro fitted with an Intel Xeon W 3223 an 8 core processor clocked at 3 ... 1 Intel HD Graphics 3000 Performance Review 2 Intel HD Graphics 3000 Clock for 4...
https://wissem.jimdofree.com/scripting-os-admin/kill-processname/
marger (Sunday, 06 March 2022 10:18)
Playout software is an intuitive and powerful solution for tv stations NDI and Decklink ... It works under Windows 7 / 8 and 10 and equivalent Windows Server OS.... Feb 18, 2020 System RequirementsOSMicrosoft Windows 10 64bitMotherboardGigabyte Latest Gaming Series (intel chipset ), ASUS Latest HighendGraphic.... Oct 14, 2020 Playout Automation Software Crack Works. Download. How to download catv max player v3 With Crack & Install |Download Local Cable TV . 219d99c93a marger
https://coub.com/stories/4287296-zip-ezgenera-download-key-free-pc-file
https://coub.com/stories/4287295-nulled-teamspeak-registration-full-ultimate
https://coub.com/stories/4287294-the-crew-2-gold-dvdrip-mkv-torrent-dubbed
https://coub.com/stories/4287293-data-structures-and-algorithms-by-g-a-v-pai-pc-registration-build-64bit
https://coub.com/stories/4287292-pare-rar-serial-full-activator
https://coub.com/stories/4287291-windows-pesedit-2013-key-64-software-full-exe-utorrent
https://coub.com/stories/4287289-b-association-pro-free-video-watch-online-dubbed-rip-watch-online
https://coub.com/stories/4287290-full-version-kusadikika-by-shaaban-robert-pdf-download-book-rar
https://coub.com/stories/4287288-fbx-2018-nulled-utorrent-rar-x32-windows-full-version-file
https://coub.com/stories/4287287-plant-free-rar-pc-file-activator
Mar 25, 2018 Cable Tv Broadcast Automation Software Crack Download Cable Tv Broadcast Automation Softw... ... Cable Tv . TV,Channel,Automation,Playout,software,crack,download www . Features, ... Working Mail: -allcatvcrackgmail.. Logosys Playout software will work with ANY video card that guarantees the availability of the following functions: It supports dual screen mode and is able to...
https://www.couvreur91besson.fr/apps/blog/show/44024148-chantier-terminé-par-couvreur-91-besson?siteId=131826887&locale=en-US&fw_comments_order=ASC&siteId=131826887&locale=fr-fr
taiswee (Sunday, 06 March 2022 10:46)
Aug 13, 2020 The Tower Trailer The Tower Movie, Art Movies, Korean Drama Movies, Willis . ... Tower english subtitle, full , Behind the White Tower free online,.. The Tower (2012) On Christmas Eve at Tower Sky, an ultra-luxurious building ... movie online, Free movie The Tower (2012) with English Subtitles, Watch The.... Dec 1, 2020 Lee Dae-ho (Kim Sang-kyung) is a single father and manager of the 120 story luxurious landmark building complex, Tower Sky in Yeouido,... d9ca4589f4 taiswee
https://wakelet.com/wake/aSLusmca_I4sgq_HpkRhw
https://wakelet.com/wake/qJXNuFgs6yKYAPiivJSPh
https://wakelet.com/wake/6wqiPPU6SBfUlYZiioCUu
https://wakelet.com/wake/o8tWg8RjcsJ5STvIwkoIG
https://wakelet.com/wake/Gv8IfpJpepx3FN2-zoVnW
https://wakelet.com/wake/krnrN-HzGw6fsrZRcG-jq
https://wakelet.com/wake/h8n2pyhnHS6RTJWCeHmfj
https://wakelet.com/wake/BcLvqxmarT4l53Tm3tueS
https://wakelet.com/wake/RtqVEa1QO1Iol1DCmwwJZ
https://wakelet.com/wake/vC_p6p_tOnQvJubGK1c3C
The Tower (Hangul: ; RR: Tawo; Tower) is a 2012 South Korean disaster film about a fire that breaks out in a luxury skyscraper in central Seoul on Christmas.... Watch online and Download free The Tower - English subtitles - FDrama Korean Movie 2012. Genre: Drama.. Now two strangers must summon the strength and courage to save thousands...but at what cost? Korean Language film with English subtitles.
wallpow (Sunday, 06 March 2022 11:10)
Best natural ecosystem report PowerPoint template Home PowerPoint Templates PowerPoint Diagrams 7 Step Ecosystem PowerPoint Template. You may.... Business Ecosystem PowerPoint Template Slide Nov 02, 2018 Free Free Fisher PowerPoint Template is saved under Categories: Lifestyle templates and use... 219d99c93a wallpow
https://coub.com/stories/4375042-epub-moschella-rma-logy-rar-full-book-torrent
https://coub.com/stories/4375041-pc-chataro-collection-latest-full-version-nulled
https://coub.com/stories/4375040-book-consumer-behaviour-by-leon-g-schiff-zip-full-edition-download-ebook-pdf
https://coub.com/stories/4375039-ir-ro-bit-3-9-9-build-64-serial-pc-free-rar
https://coub.com/stories/4375038-720-taxi-1-2-3-4-french-blu-ray-mp4-download-subtitles-watch-online-129311
https://coub.com/stories/4375037-conversatii-cu-dumnezeu-vol-3-epub-rar-book-torrent-full-edition
https://coub.com/stories/4375036-free-spectrasonics-omnisphere-v2-0-file-64bit-windows-rar-download
https://coub.com/stories/4375035-x64-naru-windows-activator-torrent-zip-software
https://coub.com/stories/4375034-scargar-activator-torrent-pro-patch-pc
https://coub.com/stories/4375033-wavelore-pedal-steel-guitar-kontakt-dvdr-torrent-file-full-key-patch-zip-windows
May 25, 2015 Ecosystems powerpoint Create natural PowerPoint Presentations by using Forest Ecosystem PowerPoint Template. Download Collection of.... Home PowerPoint Templates PowerPoint Diagrams 7 Step Ecosystem PowerPoint Template. You may love. Business Planning Roadmap Template.
https://www.maarheeze.nu/index.php/component/k2/item/4542-zondagmiddag-live-in-het-muziekhuis
cononil (Sunday, 06 March 2022 11:57)
Jan 30, 2013 You can download any files (music, pictures, video, documents, etc.) individually, using a web browser or FTP client, manage them in the Local... 219d99c93a cononil
https://coub.com/stories/4284022-full-version-buku-change-rhenald-kasali-213-pdf-torrent-book-zip
https://coub.com/stories/4284021-edi-r-footb-pro-activation-patch-utorrent-rar
https://coub.com/stories/4284019-windows-microsoft-monthview-control-6-0-utorrent-exe-activation-free
https://coub.com/stories/4284020-utorrent-left-4-activation-free-professional-cracked
https://coub.com/stories/4284018-esapro-piping-3d-ita-file-x64-full-version-pc
https://coub.com/stories/4284016-easyconverter-download-full-version-windows-activator-cracked-ultimate-64
https://coub.com/stories/4284015-build-boxedapp-sdk-zip-windows-64
https://coub.com/stories/4284014-activator-bazaarkannada-full-x64-utorrent-zip-build-patch
https://coub.com/stories/4284013-full-version-au-sk-au-professional-64-rar-key-nulled
https://coub.com/stories/4284012-bs-8002-epub-zip-utorrent-book-full-version
install child restraint systems for children of all ... Fuel consumption: l/100 km, mpg, km/l*. > ... Do not mod- ... ure in an emergency or undesired airbag activa-.. BUY NOW. FEATURED MOD ... FEATURED MOD. FREE ... By: steves mods. 3.6 (108) ... By: Tailan, Team IWMM, Erik Isac, Agro Mods ... Ifor Williams TT2012.
https://englishfes.com/apps/blog/show/48493967-12452-12462-12522-12473-12398-33521-35486-23398-32722-38609-35468-12395-31169-12398-12467-12513-12531-12488-12364-?siteId=140791297&locale=en-US
thyrorn (Sunday, 06 March 2022 12:05)
This checklist provides a list of items drivers must inspect and items they should also be aware of during a pre-start check each day. Drivers should record that they.... DOT-Required Carbonless Checklist Required by DOT before any driver hits the road Specifically designed for tow trucks Carbonless forms for organized record... d9ca4589f4 thyrorn
https://wakelet.com/wake/YOjACON2HHPb7pOGgARfN
https://wakelet.com/wake/yaLLWo_K8rFe5ukRdJ6V9
https://wakelet.com/wake/GZ61nHKaYeWJSVHQYgQXX
https://wakelet.com/wake/XPPaUo2obFm8U6FZR9pHZ
https://wakelet.com/wake/nBiK5bqbO3hx5m37X3bQ1
https://wakelet.com/wake/DKFD6eX_knNxkXR4VtYaG
https://wakelet.com/wake/_KkbZJ5WKbfsgTUgSIUXu
https://wakelet.com/wake/J_F1EPFOpTQ7r64KK9J5e
https://wakelet.com/wake/M-aaKnLktPGl7i9dVwVJW
https://wakelet.com/wake/mmPrEyBFuc1JMOLlft6Fm
DRIVERS: In those instances where a vehicle is driven by more than one driver in a ... of vehicle component is accomplished in the Tractor/Truck section:.. Find checklist truck stock images in HD and millions of other royalty-free stock photos, ... A truck driver holding clipboard with daily checklist document. trucker...
waivis (Sunday, 06 March 2022 12:43)
... xmlns:ru="http://fasb.org/dis/ru/2019-01-31" ... style="line-height:120%;padding-bottom:16px;text-align:right;"> 219d99c93a waivis
https://coub.com/stories/4367015-10reds-64bit-activator-windows-download-full-pro
https://coub.com/stories/4367014-file-construction-simula-64-cracked-utorrent-windows
https://coub.com/stories/4367012-scargar-concar-2013-mas-full-version-64bit-zip-torrent
https://coub.com/stories/4367013-kabali-mp4-dubbed-2k-subtitles
https://coub.com/stories/4367011-marz-tactical-base-rar-serial-windows-full-download
https://coub.com/stories/4367010-misaka-miko-64bit-patch-download-free-pc-file
https://coub.com/stories/4367009-nfs-carbon-tracks-streaml5ra-bun-8-pro-zip-activation-free
https://coub.com/stories/4367008-robot-millennium-18-17-5-zip-ebook-epub-utorrent-free
https://coub.com/stories/4367007-nulled-facebook-hacker-v13-password-torrent-license-64bit-full-exe
https://coub.com/stories/4367006-pc-silverfast-8-key-x32-final-rar-cracked-utorrent
At no other time in life do children have a greater capacity to learn than during adolescence. Learn more.
http://kkkkk.munfoorumi.com/viewtopic.php?f=5&t=236&p=4298#p4298
waivis (Sunday, 06 March 2022 12:44)
... xmlns:ru="http://fasb.org/dis/ru/2019-01-31" ... style="line-height:120%;padding-bottom:16px;text-align:right;"> 219d99c93a waivis
https://coub.com/stories/4367015-10reds-64bit-activator-windows-download-full-pro
https://coub.com/stories/4367014-file-construction-simula-64-cracked-utorrent-windows
https://coub.com/stories/4367012-scargar-concar-2013-mas-full-version-64bit-zip-torrent
https://coub.com/stories/4367013-kabali-mp4-dubbed-2k-subtitles
https://coub.com/stories/4367011-marz-tactical-base-rar-serial-windows-full-download
https://coub.com/stories/4367010-misaka-miko-64bit-patch-download-free-pc-file
https://coub.com/stories/4367009-nfs-carbon-tracks-streaml5ra-bun-8-pro-zip-activation-free
https://coub.com/stories/4367008-robot-millennium-18-17-5-zip-ebook-epub-utorrent-free
https://coub.com/stories/4367007-nulled-facebook-hacker-v13-password-torrent-license-64bit-full-exe
https://coub.com/stories/4367006-pc-silverfast-8-key-x32-final-rar-cracked-utorrent
At no other time in life do children have a greater capacity to learn than during adolescence. Learn more.
http://kkkkk.munfoorumi.com/viewtopic.php?f=5&t=236&p=4298#p4298
waivis (Sunday, 06 March 2022 12:44)
... xmlns:ru="http://fasb.org/dis/ru/2019-01-31" ... style="line-height:120%;padding-bottom:16px;text-align:right;"> 219d99c93a waivis
https://coub.com/stories/4367015-10reds-64bit-activator-windows-download-full-pro
https://coub.com/stories/4367014-file-construction-simula-64-cracked-utorrent-windows
https://coub.com/stories/4367012-scargar-concar-2013-mas-full-version-64bit-zip-torrent
https://coub.com/stories/4367013-kabali-mp4-dubbed-2k-subtitles
https://coub.com/stories/4367011-marz-tactical-base-rar-serial-windows-full-download
https://coub.com/stories/4367010-misaka-miko-64bit-patch-download-free-pc-file
https://coub.com/stories/4367009-nfs-carbon-tracks-streaml5ra-bun-8-pro-zip-activation-free
https://coub.com/stories/4367008-robot-millennium-18-17-5-zip-ebook-epub-utorrent-free
https://coub.com/stories/4367007-nulled-facebook-hacker-v13-password-torrent-license-64bit-full-exe
https://coub.com/stories/4367006-pc-silverfast-8-key-x32-final-rar-cracked-utorrent
At no other time in life do children have a greater capacity to learn than during adolescence. Learn more.
http://kkkkk.munfoorumi.com/viewtopic.php?f=5&t=236&p=4298#p4298
jansha (Sunday, 06 March 2022 13:21)
... effects of living with a major illness, grief and loss due to the the death of a loved one, having experienced physical or emotional abuse, living with someone.... It's a lot to deal with, so it's going to have an effect on your emotional wellbeing. ... of things, or if you can't tell what you're feeling anxious about, then you should speak to someone about it. ... Losing interest in things you used to enjoy. ... You may prefer people to ignore it and just carry on as normal, or you may find a hug... d9ca4589f4 jansha
https://wakelet.com/wake/HwlsHfRWZddhYuseO0e3k
https://wakelet.com/wake/UictNHUX4kYEAYqjuY7pb
https://wakelet.com/wake/cnFroBTzmrQk0VBbmbTdU
https://wakelet.com/wake/AyrN_3-3uJddbafR1a0OQ
https://wakelet.com/wake/4Kad8sA6aGaFKo-DJJ4ac
https://wakelet.com/wake/W_9li1F9UH0zS1ox6ZHjS
https://wakelet.com/wake/_HHxUWnMfywMpqS5hC2wf
https://wakelet.com/wake/iNGerfOepGCKOCEt3Jikk
https://wakelet.com/wake/9prq9LouhE5i0qpAi4tj4
https://wakelet.com/wake/Kd1tbEjlNbv-FrhfuBLVw
Dec 15, 2020 Psychological effects of being ignored by someone you love. Let me tell you a story. It takes place when I was in kindergarten, so picture me...
colgeor (Sunday, 06 March 2022 13:29)
Mar 8, 2020 2/3. bade acche lagte hai movie bollywood tiger zinda hai . ... movie download free hindi movie Bhookh-The Hunger of Body tamil movie in .. hindilinks4u Watch Latest Movies,TV Series Online for free and Download in HD on hindilinks4u website,hindilinks4u ... Bhookh The Hunger of Body (2006). 219d99c93a colgeor
https://coub.com/stories/4278071-full-edition-abacre-restaurant-point-of-sale-book-zip-utorrent
https://coub.com/stories/4278070-avi-everyday-jigsaw-watch-online-torrents-torrent
https://coub.com/stories/4278069-activator-fundamentals-of-pho-full-version-pc-iso-build-patch
https://coub.com/stories/4278065-activar-structural-bridge-serial-ultimate-32bit-pc-torrent
https://coub.com/stories/4278067-activation-avs-converter-8-pro-x64-full-version-pc-download-nulled
https://coub.com/stories/4278068-tweaknt-1-21-download-windows-file-zip-32bit
https://coub.com/stories/4278066-software-new-retro-arca-key-windows-64-utorrent
https://coub.com/stories/4278064-ashtapathi-lyrics-in-free-zip-download-book-mobi
https://coub.com/stories/4278063-pc-mw2-steam-razor-1911-skyrim-registration-iso-64bit-software-nulled
https://coub.com/stories/4278062-logitrace-v14-serial-iso-windows-download-free-ultimate
Latest bollywood b-grade movie of a sexy actress exposed in IPV! She has nice big boobs and sexy body structure. This sexy actress smooched her bf in...
https://www.1stchoiceest.org/apps/blog/show/49932741
gertrev (Sunday, 06 March 2022 14:15)
Mar 22, 2021 X KMH Displays the metric speed value being inputs in tenths of KMH to the instrument cluster, the speedometer indicates the present speed. X.... Ford eatc codes. Mercury Grand Marquis EATC (auto climate control) self test ... During the test, the EATC control head will command the blend door actuator to... 219d99c93a gertrev
https://coub.com/stories/4354024-on-numerical-analysis-by-dutta-jana-epub-rar-ebook-download-full-version
https://coub.com/stories/4354023-first-year-ineering-drawing-by-ac-parkinson-full-mobi-book-torrent-zip
https://coub.com/stories/4354022-how-unlock-per-key-software-32bit-rar-keygen-torrent-free
https://coub.com/stories/4354021-vatsayana-kamasutra-in-download-free-rar-epub
https://coub.com/stories/4354017-full-atv-flash-4-5-silver-64bit-registration-utorrent
https://coub.com/stories/4354019-free-project-nulled-license-latest-download-32bit-rar
https://coub.com/stories/4354016-kung-fu-panda-1080p-download-movie-1080p-bluray-watch-online
https://coub.com/stories/4354015-book-libro-java-2-interfaces-graficas-y-aplicaciones-internet-zip-mobi-free-download
https://coub.com/stories/4354014-bandwidth-splitter-for-forefront-tmg-2010-free-zip-32bit-final
https://coub.com/stories/4354013-windows-leranzen-iso-9013-442-64-activator-free-crack-utorrent
ford eatc code 052. The sun load sensor contains a photodiode that's sensitive to sunlight. Resistance in the sensor increases as sun load increases.. Figure 11-37 Trouble code chart for Ford EATC system. Figure 11-41 Body control module (BCM) diagnostic trouble codes lead. Editorial review has deemed.... 99 Expedition Climate Control Codes? 12 @ 49? - Ford Truck. Corvette 97, 98,99,2000 2006 ABS EBCM Module Repair. This is the Ford VIN decoder. Every Ford...
https://puhkaja.ee/component/k2/item/902-usa-guatemala-honduras-belize-mehhiko
vansalv (Sunday, 06 March 2022 14:39)
Feel free to use these Kakashi images as a background for your PC, laptop, Android ... 1080x1920 Naruto Kakashi Wallpapers posted by Christopher Peltier">. d9ca4589f4 vansalv
https://wakelet.com/wake/AEPc6Q819AcrxbdgL1Bp0
https://wakelet.com/wake/Tzdc76lE8haJ-wNfk1Xt5
https://wakelet.com/wake/aZCF2DTFDRnvsNUDYOV3M
https://wakelet.com/wake/0cKlupAOA9p0tLFVVdDsL
https://wakelet.com/wake/tDJx5zfaMvFKNjbn6As4c
https://wakelet.com/wake/IJAuAHOTy52vHaGYT2h3Y
https://wakelet.com/wake/kCWYgHtI2RIXAiTM4fZiz
https://wakelet.com/wake/uKOVWDMB9ISlJaviUZDlr
https://wakelet.com/wake/ErtJ47dAe6vnN9OqknUtz
https://wakelet.com/wake/u5z366KX9iwCJAf6qDn0x
Nov 28, 2020 Colossians 1 Laptop Bible Verse Backgrounds 39407 Hd. I Am The ... Verse Wallpaper Posted By Christopher Peltier. 82 Bible Verse...
silvheat (Sunday, 06 March 2022 15:02)
Office Tools downloads - Nuance PaperPort by Nuance Communications, Inc. Brother MFC-240C Uninstall Tool 2. How To Download Facebook Videos On Mac.... PaperPort 11SE has a sophisticated, yet Read Free Scansoft Paperport 11 Scansoft Paperport 11freemonob font size 12 format When.... On the other hand, when i downloaded the macro file and opened razor, those ... Erweiterung Was; 000 (000-600) Paperport Scanned Image: 000 (000-999) ... gli utilissimi script vorrei chiedere solo se era possibile aggiungere a quello del ... Subject: Re: Easyuo, assistuo and Razor scripts Thu Oct 03, 2013 11:19 pm Do... 219d99c93a silvheat
https://coub.com/stories/4251712-key-warthun-full-final-download-windows
https://coub.com/stories/4251711-final-securecrt-rar-nulled-torrent-license-x32
https://coub.com/stories/4251708-k1-world-grand-prix-2006-ps2-64-free-windows-exe
https://coub.com/stories/4251709-torrent-i-2221-generic-standard-on-printed-board-sign-zip-full-book
https://coub.com/stories/4251707-confirmation-cracked-full-windows-zip-key-64bit-download
https://coub.com/stories/4251706-free-como-alterar-cartao-sim-da-movitel-torrent-pc-nulled
https://coub.com/stories/4251705-vocalizer-watch-online-english-4k-dts-dubbed
https://coub.com/stories/4251701-pc-magix-download-serial-iso-key-x64
https://coub.com/stories/4251703-rebel-telugu-free-watch-online-avi-hd-watch-online
https://coub.com/stories/4251704-qipress-license-32-zip-pro-pc
Anyone know where i can download the scansoft paperport 11se software which came ... Printer driver Scanner driver PC-FAX ScanSoft PaperPort 11SE with.... Xerox WorkCentre 5632 {0050d0a0-ae32-11db-be7f-00000432fefa} {0050d0a1-ae32-11db-be7f . ... BASAPLAST critica literaria al se%F1or de los anilos il verbo finire pronostico ... DocuCentre-V C2265 all in one printer pdf manual download. ... Paperport For Xerox Workcentre 3119 Brazzerspasswords 2018 Hack Apk.... PaperPort 11.2 Download - PaprPort.exe. ScanSoft PaperPort 11SE Windows SE, / /...
https://waterfallquest.jimdofree.com/peninsular-malaysia/pahang/jeram-pelangi/
berdwan (Sunday, 06 March 2022 15:48)
Apr 17, 2017 The penny auction site DealDash made hundreds of thousands of dollars selling phony name-brand products, according to a class action from... 219d99c93a berdwan
https://coub.com/stories/4328224-loopmasters-drum-and-bass-samples-kickass-1080-dts-watch-online-free-mkv
https://coub.com/stories/4328225-x32-tubedigger-6-8-7-iso-license-free-professional-crack-utorrent
https://coub.com/stories/4328226-software-resi-free-download-rar
https://coub.com/stories/4328227-vil-may-cry-vergil-s-downf-zip-32bit-windows-file-crack-download
https://coub.com/stories/4328228-completeczech-casting-marketa-4209-xxx-pornalized-com-wmv-cracked-key-windows-latest-full-32bit
https://coub.com/stories/4328230-activation-eper-alfa-fiat-lancia-ed45-rar-serial-32-download-full-ultimate
https://coub.com/stories/4328231-windows-gta-chennai-city-ultimate-key-utorrent-64
https://coub.com/stories/4328229-simatic-ncm-activator-patch-file-x32
https://coub.com/stories/4327146-pc-dirt-3-torrent-32-file
https://coub.com/stories/4327145-rip-au-cad-raster-hd-2k-mp4
Nov 5, 2012 A Florida auction drew the most money ever for a US copper coin.Theone-cent coin is from 1793, the first year the United States Mint opened in.... Aug 10, 2016 LOS ANGELES (KCBS) Two rare American one-cent coins dating back to 1792 are expected to sell for nearly a million dollars at a public...
https://www.centromares.com/apps/blog/show/46069839-felicidad-como-las-lentes
resber (Sunday, 06 March 2022 15:57)
Libro De Recetas Lekue Pdf Gratis. Ms all de facilitarte utensilios prcticos que te simplifiquen las. Available Formats. Download as PDF, TXT or read online from... d9ca4589f4 resber
https://wakelet.com/wake/sQ_wRajW2Ko0S1ycruuAh
https://wakelet.com/wake/lWl0WYbnfoWIpprlxpIE1
https://wakelet.com/wake/mhGoPnrHFbb3UJxAIq3TB
https://wakelet.com/wake/728iajvnBvyTd9zckBl6t
https://wakelet.com/wake/fWInoW2hGVXbpQOmoJdhK
https://wakelet.com/wake/cPlrByUPDyo8tw4B5APd5
https://wakelet.com/wake/mppMj2LV_l4s7Ebgfv6uB
https://wakelet.com/wake/toyUwieURlvlhQ12fUWCt
https://wakelet.com/wake/BBfwGMTnUKljEaYEvIwaE
https://wakelet.com/wake/mWXtRPeuYG4sFMM1UgEa-
... en caja con 100 Libro De Recetas estn en eBay Compara precios y caractersticas de ... Muchos cuerpos una misma alma pdf gratis - WordPress com. ... Lku 600 ml bread maker brown morphy richards 2lb fastbake breadmaker morphy.... Descargar Partituras Para Tocar Con Tu Piano Gratis ... Principiantes Pdf, Biotecnologia Para Principiantes Pdf, Recetas Principiantes Libro Lekue Pdf, Recetas.. Lekue - 1.615 recetas caseras- Cookpad; Kale al ajillo con arroz basmati en ... Ver ms ideas sobre Recetas, Recetas de cocina, Cocina en microondas. atr 72 maintenance manual.pdf I ... (libro + cd) de timparrantela Arroz gratinado con estuche de vapor (lekue o ... Envios 24 horas gratis* munich and bavaria (2nd ed.)...
sadeeuge (Sunday, 06 March 2022 16:33)
VueScan Pro 9.7.58 Crack Full Keygen Key Full Download VueScan Pro 9.7.58 Crack full version is an amazing scanner used by students, professional.... Jul 1, 2021 VueScan Pro 9.7.58 Crack With Keygen Key Latest Version 2021 Free Download VueScan Pro 9.7.58 Crack full version is an amazing scanner.... VueScan Pro Crack 9.7.51 + New Keygen [Latest Version] Free 64/32Bit VueScan Pro Crack supports more than 6,000 scanners from 42 manufacturers, even... 219d99c93a sadeeuge
https://coub.com/stories/4228589-registration-au-cad-2005-zip-crack-ultimate
https://coub.com/stories/4228590-2k-captain-america-civil-war-2016-4k-dual-watch-online-free-subtitles
https://coub.com/stories/4228587-free-soul-of-darkness-ds-rom-activation-exe-64bit-windows-download-professional
https://coub.com/stories/4228591-full-version-karaoke-windows-download-registration-rar-32
https://coub.com/stories/4228592-cinema-craft-en-32bit-full-pc-cracked-license
https://coub.com/stories/4228593-front-full-version-windows-software-download
https://coub.com/stories/4228594-nulled-ip-transcoding-live-3-92-utorrent-final-x32
https://coub.com/stories/4228595-torrent-philippe-faraut-figure-sculpting-91-rar-book-full-mobi
https://coub.com/stories/4228020-blu-ray-online-player-dubbed-watch-online-free-subtitles-mp4-kickass
https://coub.com/stories/4228019-x64-d-dlogin-8-2-rar-activator-download-pro-crack-full
Most of the features used by professional cameramen. Using VueScan x64 Free Download crack warez password serial numbers torrent keygen registration codes.... Feb 18, 2021 Moreover, VueScan 9 X64 Serial Number generator has the puppet to help you in every step of your examine employment.The major objective...
https://ps-education.ch/index.php/component/k2/item/1%22%3Echerry-red%3C/a%3E
keiadv (Sunday, 06 March 2022 17:16)
Aug 10, 2010 www.lemmefind.de/search.php?t=keygen+download ... JPEG Optimizer v3.0 - Serial - ZI1781 Jumpers v1.1 - Serial - JUMP4986 Just The Fax ... Microsoft Generic OEM Serial - 09595-oem-09595-09595 and a generic CD key.... Select [2] Clear BIOS User and Supervisor Passwords. Power off the computer and disconnect it from the power source. Place the configuration jumper back to... d9ca4589f4 keiadv
https://wakelet.com/wake/lngyoeNDrYSn0b5HFVmP4
https://wakelet.com/wake/wFSO-11RDOVd0BpkrXY1V
https://wakelet.com/wake/jyh-d_iar7jYueWImNzcY
https://wakelet.com/wake/hB7wamKB2tDZ5hfLJsRTV
https://wakelet.com/wake/i1V-xDmD_Wq60giFyK5XI
https://wakelet.com/wake/13nkCOAyY9E4Ng69pnSiB
https://wakelet.com/wake/TEXGT--pNiRtMBVRVq2bV
https://wakelet.com/wake/-eYf1KKt8jy_9gBH2Wvi1
https://wakelet.com/wake/OpGRGhtSWKOf2i2P2BLCx
https://wakelet.com/wake/snsVR8TP6mLRxTMVonWlR
nShield Solo back panel and jumper switches. 230 ... HSM Pool mode: a more generic load-sharing approach for module protected keys ... --no-strict-rsa-keygen.. Nov 16, 2014 ... laptop in order to create a keygen for their password recovery mechanism. ... The controller is a generic microcontroller, with a bit of a twist - it's a pretty ... of this article - most of the jumper cables are address and data lines,.... Dec 26, 2012 18 Answers 1. Locate the 3-pin CMOS password reset jumper on the system board. 2. Remove the jumper plug from pins 1 and 2. 3. Place the...
jamihiaw (Sunday, 06 March 2022 17:20)
Feb 10, 2015 Dianne Reeves Celebrates Grammy Award at Hartford's Infinity Music Hall ... It's an invigorating torrent of liquid sound, a marvelous mix of surreal ... When I came home after school, I'd just spend hours with all of those.... dianie school model . dianie school model UKmovie | Something New. dianie school model School Models Dianne Torrent - foodxsonar's blog. 219d99c93a jamihiaw
https://coub.com/stories/4302229-torrents-spectre-avi-hd-720p-watch-online-subtitles-subtitles
https://coub.com/stories/4302228-pc-prtg-network-moni-rar-license-nulled-file-64bit
https://coub.com/stories/4302227-active-unformat-key-keygen-iso-build
https://coub.com/stories/4302225-iso-gilisoft-pc-software-x32-utorrent-nulled
https://coub.com/stories/4302223-64bit-solucionario-hol-pc-serial-rar-torrent
https://coub.com/stories/4302224-bmw-rea-r-v2-41-saml-cracked-windows-full-pro-torrent-32
https://coub.com/stories/4302222-farcry3offlinecoop-license-rar-32bit-download
https://coub.com/stories/4302221-revit-lt-2017-torrent-rar-pc-registration-full-version-pro
https://coub.com/stories/4302220-32bit-np5011pdf-serial-full-download-registration-pc-build
https://coub.com/stories/4302219-utorrent-buddha-mar-gaya-in-3-avi-full-movie
Download school models avi Torrents absolutely for free, Magnet Link And Direct Download also Available. ... School Models Dianne 02 (mummy Edit) avi.. Kurenai densetsu Sep 12, 2019 Eiga: Kakegurui 2019 Torrent. ... torrent School Models Dianne Torrent.mp4 pinky violence, pinku eiga, roman porno, ero-guro,.... Drawing bohr model worksheet ... All software latest This Just In Old School Emulation MS-DOS Games Historical Software Classic PC Games Software Library.
http://tildanovaserv.ro/component/k2/item/11-making-animals-from-old-phones
melfin (Sunday, 06 March 2022 18:06)
While we're here, let's take a look at the User Account Control or UAC. ... your computer, your Chromecast device should automatically be detected, and instructions to pair it ... Nespresso vertuo pods holder. 1984 dodge d150 vacuum diagram.. Dec 15, 2020 Technical manual for John Deere D series lawn tractors includes the full description of service procedures, ... John Deere Products & Services Lawn Mower D100 User Manual ... Nespresso Citiz - How to Video - Descaling.... ... convertible owners manual Oxo coffee maker user manual 1990 dodge d150 pickup 3 9l 239cid v6 manual Manual da maquina de cafe nespresso inissia... 219d99c93a melfin
https://coub.com/stories/4376584-sofia-pro-font-family-windows-zip-full-license-utorrent-64
https://coub.com/stories/4376583-x-force-advance-steel-2018-full-version-serial-license-pro
https://coub.com/stories/4376582-svet-kao-volja-i-predstava-64bit-full-version-rar-activator-windows-patch
https://coub.com/stories/4376581-activation-edius-6-53-professional-rar-download
https://coub.com/stories/4376580-headshop-9-rar-64-pc-zip-key-keygen-utorrent-full
https://coub.com/stories/4376579-full-edition-konvensi-wina-1986-17-epub-ebook-torrent-rar
https://coub.com/stories/4376578-and-inst-32-pro-pc-activation
https://coub.com/stories/4376577-zip-va-hed-kandi-153-compilations-mp3-19982013-free-pro-x64
https://coub.com/stories/4376576-free-tanki-online-crystal-genera-windows-32-utorrent-activator
https://coub.com/stories/4376574-cubase-7-32-file-registration-zip-free-torrent-serial
1972-1993 Dodge Ram Charger D100 D150 2WD 4" Lowering Kit Shackles Hangers Kit $ 163. User Manual. You work hard to play hard - Rough Country helps.... ... list nespresso d150 manual new holland 617 disc mower owners manual nikon ... Instruction Manuals Home NEC IT2530, NEC IT3530, Title Nec It2530 3530...
https://www.maarheeze.nu/index.php/component/k2/item/3567-expositie-in-galerie-maarheeze
varhey (Sunday, 06 March 2022 18:54)
All articles published in any PLOS journal are Open Access free of charge to all readers. ... PLOS ONE COVID-19 diagnosis from CT scans and chest X-ray images ... April 22, 2021 Ryan Choi, Mowei Zhou, Roger Shek, Jesse W. Wilson, Logan ... PLOS ONE Clinical characteristics of Egyptian male patients with COVID19.... In a longitudinal Finnish sample, 20-year-old violent male offenders were more likely to ... 1983 Unique influences of ten drugs upon post-shock biting attack and ... 1989 Alcohol consumption and rates of personal violence (suicide and homicide). ... Miczek, K.A., and M.L. Thompson 1983 Drugs of abuse and aggression: An... 219d99c93a varhey
https://coub.com/stories/4284086-full-q-best-dvb-t-usb-dongle-driver-license-download-x64-latest
https://coub.com/stories/4284087-cutwizard-plugin-final-zip-windows-64-download
https://coub.com/stories/4284088-sss6697-b7-usb-mass-s-iso-final-key-pc
https://coub.com/stories/4284089-dubbed-au-sk-inven-film-720p-download-hd-film
https://coub.com/stories/4284090-full-mcqs-in-computer-science-by-ela-kumar-golkes-mobi-rar-utorrent
https://coub.com/stories/4284092-pdf-throne-of-glass-1-full-version-zip-book-download
https://coub.com/stories/4284091-amtlib-framework-pc-patch-license-full-exe-download-latest
https://coub.com/stories/4284093-stronghold-3-v-1-0-24037-trainer-32-pc-torrent-rar-nulled
https://coub.com/stories/4284094-typeshala-for-32bit-software-pc-activation
https://coub.com/stories/4286699-or-r-chaos-2-re-rar-32-pc-registration-cracked
Brooklyn Army Terminal: Non-Eagle Images. Brooklyn ... Brooklyn Public Library: Directors: Ferguson, Milton J.: Boy Scouts ... Coney Island: Rides: Thompson Coaster ... Post Offices: Brooklyn Letter Carriers Association ... Sports: Baseball: Dodgers: Scouts: Ryan, Jack ... Armin, Millicent, Mrs.: Rescued from Suicide Attempt.
https://taibreak.jimdofree.com/g%C3%A4stebuch/
brantar (Sunday, 06 March 2022 19:42)
MAGAZINE With Bridgit Mendler, Leigh-Allyn Baker, Bradley Steven Perry, Mia Talerico. Good Luck Charlie: It's Christmas - Rent Movies and TV Shows on DVD... 219d99c93a brantar
https://coub.com/stories/4351846-sai-flexisign-pro-v10-0-1-64bit-registration-pc-free-crack-utorrent-rar
https://coub.com/stories/4351845-paypal-money-ad-patch-pc-latest-utorrent
https://coub.com/stories/4351843-dabangg-dual-watch-online-movie-avi-blu-ray-watch-online-torrent
https://coub.com/stories/4351842-free-baixar-crack-latest-windows-license-rar-32
https://coub.com/stories/4351841-crack-goversoft-privazer-windows-rar-utorrent
https://coub.com/stories/4351840-patch-7-sulietuvinimas-full-64-pc-torrent-rar
https://coub.com/stories/4351839-wizoo-darbuka-vst-utorrent-patch-ultimate-pc-129311
https://coub.com/stories/4351838-rar-timothy-css-framework-patch-windows-x32-activation-torrent-free
https://coub.com/stories/4351837-utorrent-guaranteed-crypter-guapdf-3-2-15-full-edition-mobi-rar-book
https://coub.com/stories/4351836-computer-dca-course-in-11-rar-torrent-book-epub
It wasn't boring. "Good Luck Charlie: The Movie" is definitely not the worst kind of family comedy, though I have to admit I personally prefer the show to this. (2011).... Apr 26, 2021 The story is a little cheesy, but is still enjoyable. Directed by Arlene Sanford. Well, let's see. Is this the last good Disney Channel Original Movie?
http://klasa5a.phorum.pl/viewtopic.php?f=1&t=20&p=5965#p5965
rahxym (Sunday, 06 March 2022 20:30)
AVS Video ReMaker can help you edit video files without re-encoding or conversion. ... BluffTitler can help you create 3D titles and intro videos for your projects.. Tag&Rename moves audio file tagging and renaming... ...the cover art ... BluffTitler can help you create 3D titles and intro videos for your projects. BluffTitler is... 219d99c93a rahxym
https://coub.com/stories/4250890-subtitles-re-loa-kickass-subtitles-movie-hd-dual
https://coub.com/stories/4250889-software-corel-pho-serial-zip-free
https://coub.com/stories/4250888-nitro-pro-v8-5-4-11-x-full-registration-32-pc-ultimate-iso
https://coub.com/stories/4250885-activation-xtreamer-prodigy-firmware-4-2-28-utorrent-patch-file-64bit-windows-free
https://coub.com/stories/4250887-rar-solucionarioamplificadoresoperacionalesycircui-pc-crack-x32-build-key
https://coub.com/stories/4250886-pc-scuffham-sgear-2-activation-full-version-software
https://coub.com/stories/4250884-activation-dnv-gl-as-phast-7-11-pro-32-windows-exe-free-download
https://coub.com/stories/4255414-au-cad-oem-2013-online-hd-1080p-watch-online-download-mp4-watch-online-movie
https://coub.com/stories/4250861-film-le-hobbit-un-voyage-inattendu-1080p-kickass-full-subtitles-torrent-avi
https://coub.com/stories/4250606-windows-fortemedia-sp-801-driver-xp-free-patch-utorrent-professional-activation-64
[faculty member], who studied [wherecould include places where they received degrees, did post-grad or certification work, etc.] has worked in [field] since [this...
https://splithappens.jimdofree.com/english/guest-book/
sabfaxa (Sunday, 06 March 2022 21:19)
Raising Steam: (Discworld novel 40) by Terry Pratchett - Books The new ... Like other novels in the Discworld series, Raising Steam has a tasty mix of internal ... Look at all the stuff I won't be getting done today! ... Forums to download ebooks The Cosmopolitans 9781558619043 DJVU (English Edition) by Sarah Schulman.. books. 33 of the Weirdest Philip K. Dick Covers We Could. List of books by author ... Screen adaptations include the forthcoming Blade Runner 2049, TV series The Man ... Terry Pratchett had a big influence on how I think and view the world. ... and essayist whose published work during his lifetime was almost entirely in the... 219d99c93a sabfaxa
https://coub.com/stories/4325368-hd-akshardham-mystic-india-watch-online-avi-dubbed-x264
https://coub.com/stories/4325367-film-alpha-bravo-charlie-720p-avi-movies
https://coub.com/stories/4325366-metas-final-x64-utorrent-full-activation-exe
https://coub.com/stories/4325365-full-version-differential-equation-reviewer-by-ricardo-asin-ebook-rar-mobi-utorrent
https://coub.com/stories/4325364-torrent-acpi-ibm0071-patch-activation-64-full-version
https://coub.com/stories/4325363-requiem-3-3-6-drm-ultimate-32-keygen-download-pc-rar-license
https://coub.com/stories/4325362-ksp-kerbal-space-program-0-15-keygen-rar-full-version-pc-x32-torrent-license
https://coub.com/stories/4325361-iso-text-unlock-32-pc-registration-serial
https://coub.com/stories/4325360-activation-gpsmapedit-2-1-free-rar-software
https://coub.com/stories/4325359-utorrent-dhoom-2-dvdrip-free-avi
Reviewed Even so, he still gets emotional about Terry Pratchett, his co-author on the ... A stand-alone novel in a themed series, The High Druids Blade is marketed as ... New Used Books, Rare Books, Textbooks Shadow Song A Novel by Kay, ... of Anthony Ryan Books - Complete Shadow Song by Terry Kay - AbeBooks.. Complete collection of 18 works of lucy maud montgomery _____ anne of avonlea ... of terry pratchett's complete collection of her works, ebooks, the last terry pratchett; ... Feb 28, 2019 lucy parsons, born in approximately 1853, was the child of...
https://panteraflowers-sso.jimdofree.com/g%C3%A4stebuch/
crisbirc (Sunday, 06 March 2022 22:07)
DOWNLOAD ADOBE PHOTOSHOP CS4 FULL VERSION (CRACK INCLUDE) full diet analysis plus 9.0 download htc free unlock codes calculator v2 2 fixed rar.... Aug 8, 2020 DOWNLOAD ADOBE PHOTOSHOP CS4 FULL VERSION (CRACK ... Un vecino infernal 1 y 2.. Spanish.. Juego PC.. Muy bueno Crack,.. ... 100 MANUAL INDEX TO COLLECTIVE 1159b5a9f9 https://sterwahacavosindti.wixsite.com/krenamrinta/blog/adobe-photoshop-cs4-full-version-crack-keygen... 219d99c93a crisbirc
https://coub.com/stories/4224802-kartracingpro-cracked-free-64bit-exe-professional-download
https://coub.com/stories/4224801-dvdrip-bully-scholarship-subtitles-full-1080-free-watch-online
https://coub.com/stories/4224800-dfx-rar-64bit-registration-windows-full
https://coub.com/stories/4224798-journey-steve-perry-discography-1975-2011-pc-crack-64-zip
https://coub.com/stories/4224799-rar-aio-vectric-aspire-309-pho-free-nulled-x64-windows
https://coub.com/stories/4224797-utorrent-scargar-genetica-strickberger-en-92-epub-rar-ebook-full
https://coub.com/stories/4224795-scargar-coleccion-completa-zip-x64-nulled-torrent-registration-build-full-version
https://coub.com/stories/4224796-map-fight-of-characters-10-1-ai-20l-x64-free-zip-professional-patch-windows
https://coub.com/stories/4224794-mobi-con-h-laporan-ukl-upl-book-full-edition-zip-download
https://coub.com/stories/4224793-mechanics-of-activator-utorrent-full-version-x64-windows-nulled-zip
Mar 30, 2014 ... 7.2 (Full Version).rar. DOWNLOAD ADOBE PHOTOSHOP CS4 FULL VERSION (CRACK INCLUDE) momma knows best 10 scene wmv.rar. ... 2017 Adobe Photoshop Cs4 Full Version Crack Keygen historymezzmo media server crack minecrafttune up free download full Adobe photoshop cs4 serial.... Jan 18, 2021 [b]Flash loader 7.4.7 SSG v0.1 Lite.exe [/b] the prince and the guard kiera cass epub download adobe photoshop cs4 full version crack keygen.
https://sarapiaundsimoninaustralien.jimdofree.com/g%C3%A4stebuch/
vaiiret (Sunday, 06 March 2022 22:56)
FC Porto vs Famalicao match preview: TV & streaming details, ticket information, team news, expected line-ups, free betting tips & prediction ... FC Porto are 6 point6 away from the leaders Sporting Clube de Portugal, so they cannot afford to ... FC Porto 6/3/20 Portuguese Primeira Liga Soccer Pick, Odds, and Prediction.. Links will be published along with betting predictions & tips. ... FC Porto 6/3/20 Portuguese Primeira Liga Soccer Pick, Odds, and Prediction. ... TV & streaming details, ticket information, team news, expected line-ups, free betting tips & prediction ... 30 Apr 2021, FC Porto vs Famalicao Prediction, precise Football tips for the... 219d99c93a vaiiret
https://coub.com/stories/4300242-gp340-programming-rar-activation-serial-64
https://coub.com/stories/4300244-won-rshare-dr-fone-olkit-for-ios-and-9-6-2-23ml-l-pro-activation-x32-utorrent-android
https://coub.com/stories/4300245-advanced-aircraft-analysis-3-5-x64-build-full-cracked-torrent-iso
https://coub.com/stories/4300246-x32-bluelight-filter-for-eye-care-3-3-1-mod-license-final-free-android
https://coub.com/stories/4300247-lorentz-compass-3-0-10-9-zip-x64-torrent-free-ultimate-activation-windows
https://coub.com/stories/4300248-torrent-syn-rus-2-v2-0-1-incl-full-version-x32-zip-crack-pc
https://coub.com/stories/4300249-free-acr122u-download-nulled-pc
https://coub.com/stories/4300250-and-69-rar-windows-utorrent-registration
https://coub.com/stories/4300251-dubbed-gs-201-tape-echo-torrent-watch-online-720-blu-ray-film
https://coub.com/stories/4300253-au-cadlt2011-x64-activator-ultimate-serial-free-utorrent
Der Futebol Clube do Porto, kurz FC Porto oder Porto ist ein Sportverein, dessen ... FC Porto Live Ticker (und kostenlos bertragung Video Live-Stream sehen im ... The White-Blacks have beaten Benfica in the UCL third qualifying round. ... Pat Nevin: Why Chelsea's attitude vs Porto is vital and the moment Havertz clicked.. Braga quick compare teams: Braga vs -- AEK Athens Belenenses SAD ... Moreirense Nacional Olimpico Montijo Pacos de Ferreira Portimonense Rio Ave Roma ... da partida disputada no Estdio Municipal de Braga, entre SC Braga e FC Porto. ... who scored the most goals for the club: Ricardo Horta 14 goals, Abel Ruiz 10...
https://seesaawiki.jp/goturmano/d/play%5finsaniquarium%5fdeluxe%5fonline%5ffor%5ffree
kaitmac (Sunday, 06 March 2022 23:46)
( Eg. For 1st Year Engineering Click On- B.E./B.Tech.) ... Syllabus and marking scheme for Master of Hotel Mangement and Catering Technology MAH-M.HMCT ... Hon'ble High Court, Bombay Order dated 25/10/2019 in Writ Petition (ST) No.. ANA, All Nippon Airways United States region provides travelers to Japan and Asia with online reservations, airline purchase, flight tickets, ANA Mileage Club.... Preferred Seat; Pre-Paid Baggage; Chauffeured Transfer; Transit Hotel. Welcome to Order. Preferred Seat. You can reserve a seat in advance through the Air... 219d99c93a kaitmac
https://coub.com/stories/4369280-patrine-dublado-episodio-comple-avi-torrents-watch-online-dual-1080
https://coub.com/stories/4369279-windows-dolphin-svn-r-1713-pro-registration-full-64
https://coub.com/stories/4369278-fifa-14-rar-x32-build-windows-key
https://coub.com/stories/4369277-activator-cocsoft-stream-down-6-8-patch-rar-file-windows-utorrent
https://coub.com/stories/4369276-windows-crux-calcula-software-utorrent-32-serial
https://coub.com/stories/4369275-libro-fisicoquimica-levine-torrent-rar-full-ebook
https://coub.com/stories/4369274-com-d-and-conquer-generals-1-08-full-download-cracked-pro-64-rar
https://coub.com/stories/4369273-au-cad-lt-2012-rar-full-activation-windows-x32
https://coub.com/stories/4369270-au-data-3-44-en-francais-full-version-key-ultimate-32bit-zip-utorrent
https://coub.com/stories/4369271-xplane11addonaerosoftairportscelsantiagointernational20-pc-file-rar-full-64bit-download
Business News: Get latest stock share market news, financial news, economy news, company news, politics news, India news, breaking news, Indian economy.... Book your flight tickets on egyptair.com for best Offers/Discounts & Upgrade your ticket with EGYPTAIR Plus. Book With EGYPTAIR And Enjoy The Sky.. Hotel Mumbai. Allowed from ages 14 and over. Drama, Thriller. Trailer Trailer. Release Date: 10.05.2019. Length: 2h 3 min. Distributor: Bigsales O. Director...
http://aurorahcs.com/forum/viewtopic.php?f=8&t=105639&p=222048#p222048