Dr. Jaudy explains the causes of bloating.
In this article, I will discuss several of the causes of bloating, specifically chronic bloating and its association with several conditions.

What Is Bloating?
Although sometimes used interchangeable, bloating and abdominal distension are two different, yet related, symptoms. Bloating is a sense of gassiness or the sense of having distension in the abdominal region, although actual distension does not have to occur. 1 Abdominal distension may result from bloating, but this can only be determined from accurate measurement of abdominal girth. 1
Most people experience bloating after eating a heavy meal, such as during the holidays. However, many people experience bloating consistently and after eating regular meals. If no underlying cause can be determined (such as irritable bowel syndrome), then it is considered ‘functional bloating’. The Rome III criteria for functional bloating includes 1:
- Recurrent feeling of bloating or distension at least 3 days per month
- Symptom onset at least 6 months prior to diagnosis
- Presence of symptoms for at least 3 months
- Insufficient criteria to establish a diagnosis of any other functional gastrointestinal disorder (such as irritable bowel syndrome or functional dyspepsia)
We’ll talk more about this shortly, but for now, let’s discuss the causes of bloating.
What Are the Causes of Bloating?
Although overeating is a common cause of bloating, many people experience bloating on a regular basis, even after normal eating. When bloating is due to overeating, it is usually transient, meaning that it occurs after overeating and then goes away. When bloating is chronic or occurs after normal eating, then we are talking about some type of digestive disorder.
The main cause of bloating is decreased digestion due to decreased enzyme secretions (proteases, lipases, amylases, nucleases), decreased blood flow to the gut (mesenteric ischemia) 2, and decreased fermentation in the gut.
Enzyme Secretions
Approximately seven liters of fluid (ions, digestive enzymes, bile, and mucous) is secreted by the digestive system per day. In general, secretions are stimulated by the parasympathetic nervous system and inhibited by the sympathetic nervous system.
Blood Flow to the Gut
In order to function properly (motility, secretions, propulsion of gas, etc.), the organs of the gut (stomach, liver, pancreas, large and small intestines, etc.) require proper blood flow. If the blood flow to the gut is disrupted for any reason, this can lead to dysfunction in the gut, which may cause numerous symptoms including bloating.
Fermentation
Microorganisms that live in the gut (gut flora) secrete enzymes that human cells do not. This enables the fermentation, which is the chemical breakdown of carbohydrates into simpler, usable compounds, of carbohydrates that are undigested. Alterations in levels of gut flora can cause increases or decreases in fermentation, which can lead to a number of symptoms, including bloating.
Conditions that Cause Bloating
Many conditions can lead to bloating including (but not limited to):
- Irritable bowel syndrome (IBS) 3
- Lactose intolerance 4
- Food allergies 5
- Functional gastrointestinal disorders 6
- Gastroesophageal reflux (GER) 7
- Constipation 7
- Splenic-flexure syndrome 8
- Problems with menstruation 9
- Polycystic ovarian cysts 10
- Intestinal parasites 11
- Bowel or intestinal obstruction 12
- Gastric dumping syndrome (GDS) and rapid gastric emptying 13
- Dysglycemia 13
- Plus others
All these causes are the result of gradual failure of the neuroimmunological and neurophysiological cellular signaling. There is a problem in the electrochemical system between the brain, the ganglia, the plexi, and the organs on the cellular level.
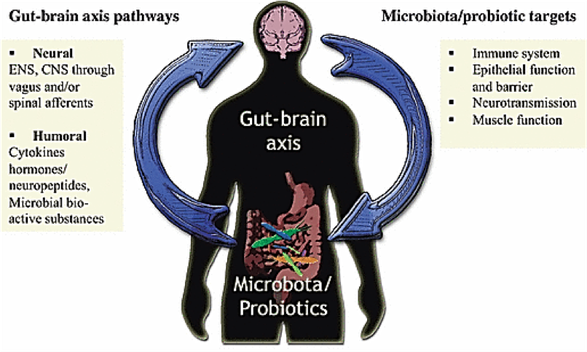
The Brain-Gut Connection
Doctors Matthew Grundfast and Michael Komar state that: “It is the integration of intestinal motor, sensory, autonomic, and central nervous system activity interacting through the brain-gut axis that is responsible for normal gastrointestinal function.” 14 What this means is that the brain and the gut are intimately connected through electrochemical pathways and they communicate with each other bi-directionally (the brain communicates with the gut and the gut communicates with the brain). 15 – 25 Any problems in the signaling from the gut to the brain can lead to problems in signaling from the brain to the gut and vice versa. This can lead to abnormal secretions, decreased blood flow to the gut, and abnormal fermentation in the gut, which can cause bloating.
Problems in brain-gut communication are described in a number of disorders including:
- Irritable Bowel Syndrome (IBS) 15 20 25
- Functional Gastrointestinal Disorders 17 22
- Gastrointestinal Sensory Disorders 19
- Abdominal Pain Syndromes 21
- Inflammatory Bowel Diseases (Ulcerative Colitis and Crohn’s Disease) 26
- Ulcers 27
- Anxiety and Depression 28
- Obesity 29
- Skin problems 30 31
- Mood disorders 32
- And many others
The brain controls the gut and the physiological state of the gut affects the brain. This information shows that gastrointestinal symptoms, such as bloating, can have devastating impacts on your health.
For more information, read my article on Irritable Bowel Syndrome or my article on Inflammatory Bowel Diseases.
References
- Lacy BE, Gabbard SL, Crowell MD. Pathophysiology, evaluation, and treatment of bloating: hope, hype, or hot air?. Gastroenterology & hepatology 7.11 (2011): 729.
- Herbert GS, Steele SR. Acute and chronic mesenteric ischemia. Surgical Clinics of North America 87.5 (2007): 1115-1134.
- Houghton LA, et al. Relationship of abdominal bloating to distention in irritable bowel syndrome and effect of bowel habit. Gastroenterology 131.4 (2006): 1003-1010.
- Swagerty Jr DL, Walling AD, Klein RM. Lactose intolerance. American family physician 65.9 (2002): 1845-1850.
- Houghton LA, Whorwell PJ. Towards a better understanding of abdominal bloating and distension in functional gastrointestinal disorders. Neurogastroenterology & Motility 17.4 (2005): 500-511.
- National Institutes of Health (NIH). Indigestion. Accessed November 10, 2014. Available at: http://digestive.niddk.nih.gov/ddiseases/pubs/indigestion/
- National Institutes of Health (NIH). Constipation. Accessed November 10, 2014. Available at: http://digestive.niddk.nih.gov/ddiseases/pubs/Constipation/
- Salvioli B, et al. Origin of gas retention and symptoms in patients with bloating. Gastroenterology 128.3 (2005): 574-579.
- Sharma P, et al. Problems related to menstruation amongst adolescent girls. The Indian Journal of Pediatrics 75.2 (2008): 125-129.
- Orenstein H, et al. Polysymptomatic complaints and Briquet’s syndrome in polycystic ovary disease. Am J Psychiatry 143.6 (1986): 768-771.
- Amin OM. Seasonal prevalence of intestinal parasites in the United States during 2000. The American journal of tropical medicine and hygiene 66.6 (2002): 799-803.
- National Institutes of Health (NIH) Medline Plus. Intestinal Obstruction. Accessed November 10, 2014. Available at: http://www.nlm.nih.gov/medlineplus/ency/article/000260.htm
- National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDKD). Accessed November 10, 2014. Available at: http://digestive.niddk.nih.gov/ddiseases/pubs/dumping-syndrome/Dumping_Syndrome_508.pdf
- Grundfast MB, Komar MJ. Irritable Bowel Syndrome. Osteopathic 84 (2000): 1247-1257.
- Mach T. The brain-gut axis in irritable bowel syndrome–clinical aspects. Medical Science Monitor 10.6 (2004): RA125-RA131.
- Horváth VJ, et al. Diabetic Gastroparesis: Functional/Morphologic Background, Diagnosis, and Treatment Options. Current diabetes reports 14.9 (2014): 1-9.
- Jones MP, et al. Brain–gut connections in functional GI disorders: anatomic and physiologic relationships. Neurogastroenterology & Motility 18.2 (2006): 91-103.
- Woods SC, Benoit SC, Clegg DJ. The brain-gut-islet connection. Diabetes 55.Supplement 2 (2006): S114-S121.
- Mertz H. Role of the brain and sensory pathways in gastrointestinal sensory disorders in humans. Gut 51.suppl 1 (2002): i29-i33.
- Honig A, et al. Acute tryptophan depletion affects brain-gut responses in irritable bowel syndrome patients and controls. Gut 53.12 (2004): 1794-1800.
- Mayer EA, Tillisch K. The brain-gut axis in abdominal pain syndromes. Annual review of medicine 62 (2011).
- Koloski NA, et al. The brain–gut pathway in functional gastrointestinal disorders is bidirectional: a 12-year prospective population-based study. Gut61.9 (2012): 1284-1290.
- Wang PYT, et al. Upper intestinal lipids trigger a gut–brain–liver axis to regulate glucose production. Nature 452.7190 (2008): 1012-1016.
- Terryberry JW. "Brain-Gut Axis."
- Orr WC, et al. Sleep and gastric function in irritable bowel syndrome: derailing the brain-gut axis. Gut 41.3 (1997): 390-393.
- Hollander D. Inflammatory bowel diseases and brain-gut axis. Journal of physiology and pharmacology 55 (2004): 183-190.
- Tache Y. The peptidergic brain-gut axis: influence on gastric ulcer formation. Chronobiology international 4.1 (1987): 11-17.
- Taché Y, Bernstein CN. Evidence for the role of the brain-gut axis in inflammatory bowel disease: depression as cause and effect?. Gastroenterology 136.7 (2009): 2058.
- Das UN. Obesity: genes, brain, gut, and environment. Nutrition 26.5 (2010): 459-473.
- Arck P, et al. Is there a ‘gut–brain–skin axis’?. Experimental dermatology 19.5 (2010): 401-405.
- Bowe WP, Logan AC. Acne vulgaris, probiotics and the gut-brain-skin axis- back to the future?. Gut pathogens 3.1 (2011): 1-11.
- Neufeld KA, Foster JA. Effects of gut microbiota on the brain: implications for psychiatry. Journal of psychiatry & neuroscience: JPN 34.3 (2009): 230.
Additional Resources
- Azpiroz F, Malagelada JR. Abdominal bloating. Gastroenterology 129.3 (2005): 1060-1078.
- Konturek SJ, et al. Brain-gut axis and its role in the control of food intake. Journal of physiology and pharmacology 55.2 (2004): 137-154.
- Bercik P, Collins SM, Verdu EF. Microbes and the gut‐brain axis. Neurogastroenterology & Motility 24.5 (2012): 405-413.

Write a comment
Health Kidney (Wednesday, 23 August 2017 09:23)
I would like to thank you for the efforts you have made in writing this article. I am hoping the same best work from you in the future as well. Thanks...
https://www.naturalmattressmatters.com/healthy-mattress/ (Saturday, 20 January 2018 04:20)
I really impressed after read this because of some quality work and informative thoughts . I just wanna say thanks for the writer and wish you all the best for coming!.